Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Brown L, Courville E. Cat scratch disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lymphnodescatscratch.html. Accessed July 16th, 2025.
Definition / general
- Majority of cases are caused by Bartonella henselae acquired via arthropod vector (cat flea) or inoculation by cat scratch (Pediatr Infect Dis J 2021;40:S11)
- Cutaneous red papule 3 - 10 days after contact that may become crusted or pustular, with subsequent development of regional lymphadenopathy 1 - 2 weeks later
- Histology is characterized by necrotizing stellate abscesses surrounded by palisading histiocytes
- Usually resolves spontaneously; rare cases may require treatment with antimicrobial therapy
Essential features
- Typically self limited lymphadenitis caused by Bartonella henselae and transmitted by cats
- Cutaneous lesion followed by usually localized lymphadenopathy
- Lymph node histopathology characterized by necrotizing stellate abscesses surrounded by palisading histiocytes
- Organism stains with Warthin-Starry or specific immunohistochemistry; confirmation by serology or PCR
ICD coding
- ICD-10: A28.1 - cat scratch disease
Epidemiology
- Adults or children can be affected but the highest incidence is in children 14 and under (Emerg Infect Dis 2016;22:1741)
- Considered the most common cause of benign lymphadenopathy in young people (Ocul Immunol Inflamm 2014;22:148)
- Estimated annual incidence of 4.7/100,000 population (Emerg Infect Dis 2016;22:1741)
- Incidence is higher in the southern United States and in the winter (thought to possibly be due to holiday adoption of kittens) (Emerg Infect Dis 2016;22:1741)
Sites
- Skin: cutaneous red papule or wheal that may become crusted or pustular
- Lymph nodes, most commonly upper extremity, followed by cervical and inguinal; patients may have involvement of 1 or multiple lymph node sites (Pediatr Infect Dis J 2021;40:S11)
- Liver, spleen or bone
- Rarely, CNS, eye, hematologic involvement / complications (Eur J Intern Med 2005;16:610)
- Parinaud oculoglandular syndrome: follicular conjunctivitis and regional lymphadenopathy, possibly caused by direct conjunctival inoculation (Ocul Immunol Inflamm 2014;22:148)
Etiology
- Majority of cases are caused by Bartonella henselae, harbored by kittens and young cats; transmitted between cats by the cat flea (Am J Clin Pathol 1994;101:607)
- Up to 100% of cat fleas harbor Bartonella and it can also often be detected in cat saliva, blood, skin, claws and feces
- Most important risk factors are owning a kitten and being bitten, scratched or licked by a kitten harboring fleas; however, up to 25% of patients with cat scratch disease do not report contact with cats
Clinical features
- Cutaneous nonpruritic red papule: 3 - 10 days after contact that may become crusted or pustular (Ocul Immunol Inflamm 2014;22:148)
- Lymphadenopathy, often of cervical or axillary nodes, develops in 1 - 2 weeks; lymphadenopathy is essentially universal but 85% have involvement of only a single node
- May have necrotizing granulomas in liver, spleen or bone
- Fever and constitutional symptoms may be present (Am J Dis Child 1985;139:1124)
- Rare complications in ~10%, including granulomatous conjunctivitis, thrombocytopenic purpura, CNS disease (Eur J Intern Med 2005;16:610, Infect Dis Clin North Am 1987;1:575, Am Fam Physician 2011;83:152)
Diagnosis
- PCR (J Clin Microbiol 2005;43:3800)
- Serology or immunofluorescence (Clin Diagn Lab Immunol 2003;10:686)
- Culture is not practical, as Bartonella are fastidious organisms that are difficult to culture (Pediatr Infect Dis J 2021;40:S11)
Radiology description
- Regional lymphadenopathy
- Liver and spleen granulomas
Prognostic factors
- Self limited disease in most; may take 2 - 6 months for lymphadenopathy to regress (Infect Dis Clin North Am 1987;1:575)
- Immunocompromised patients may present with disseminated disease or other diseases / syndromes associated with Bartonella, such as bacillary angiomatosis (BMJ Case Rep 2021;14:e239932, Am J Clin Pathol 2004;121:S71, Eur J Clin Microbiol Infect Dis 2021 Apr 12 [Epub ahead of print])
Case reports
- 16 year old boy with tender cervical lymphadenopathy (Arch Pathol Lab Med 2005;129:1065)
- 32 year old HIV infected woman with B. quintana and M. tuberculosis coinfection (J Infect 2003;46:244)
- 53 year old man with cat scratch disease encephalopathy (BMJ Case Rep 2018;2018:bcr2017223647)
- 59 year old heart transplant patient with disseminated cat scratch disease (Transpl Infect Dis 2017;19)
Treatment
- Treatment neither required nor recommended for immunocompetent patients / uncomplicated disease (Antimicrob Agents Chemother 2004;48:1921)
- Antibiotics (doxycycline, rifampin) could be considered if disseminated or complicated disease (Antimicrob Agents Chemother 2004;48:1921, Pediatr Infect Dis J 2021;40:S11)
Clinical images
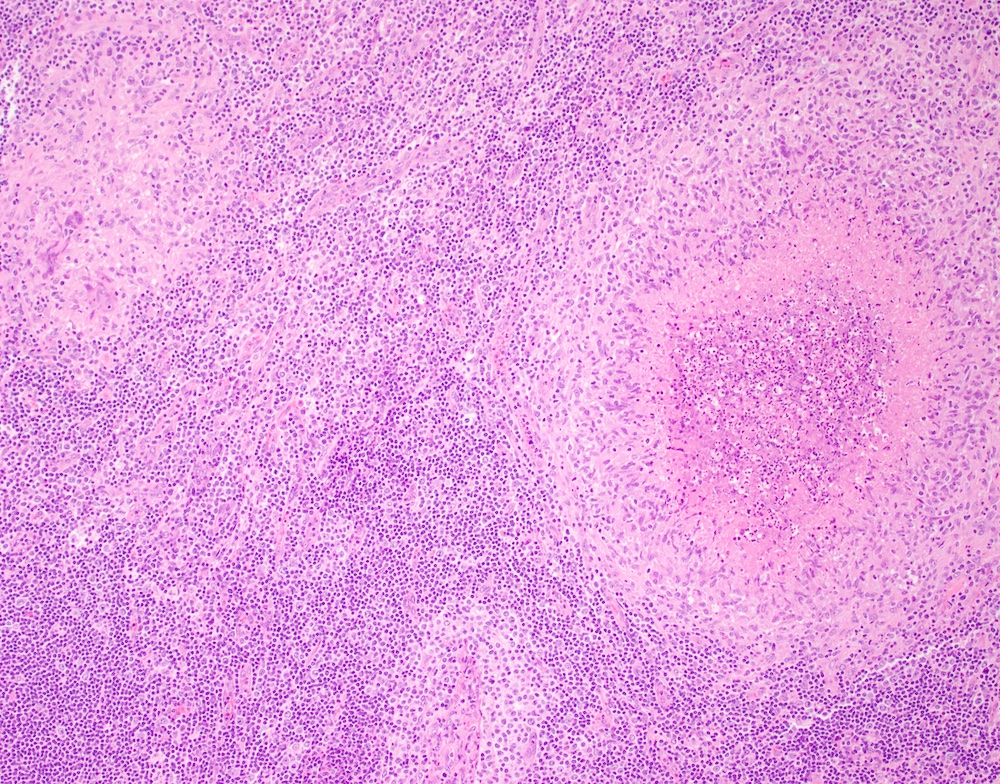
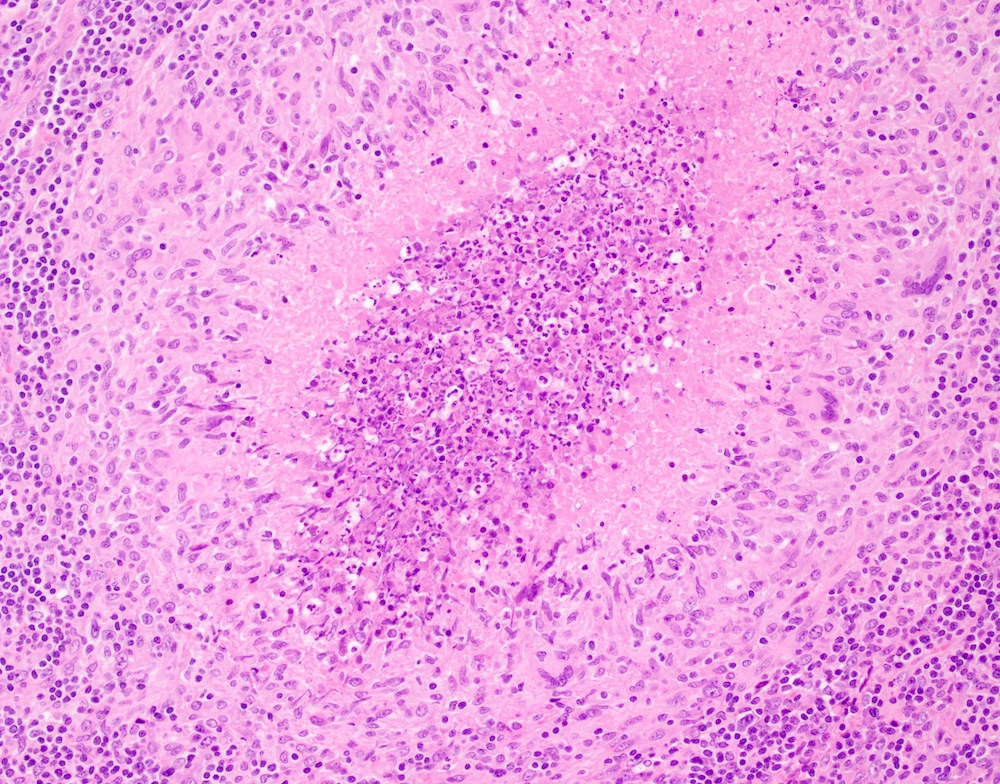
Microscopic (histologic) description
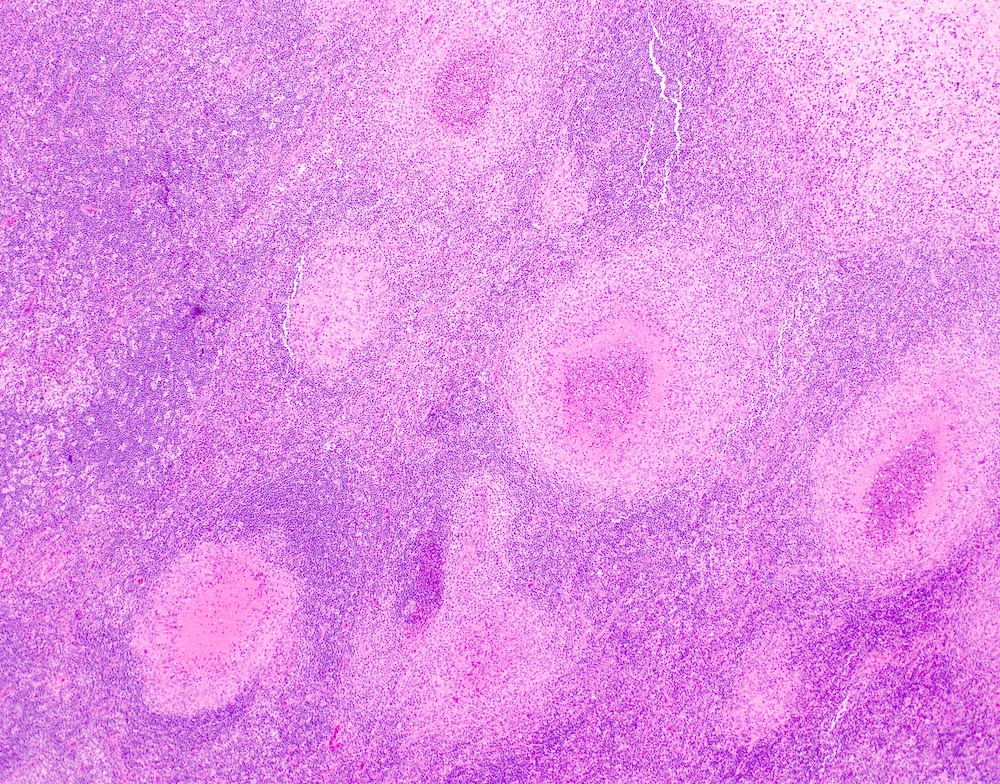
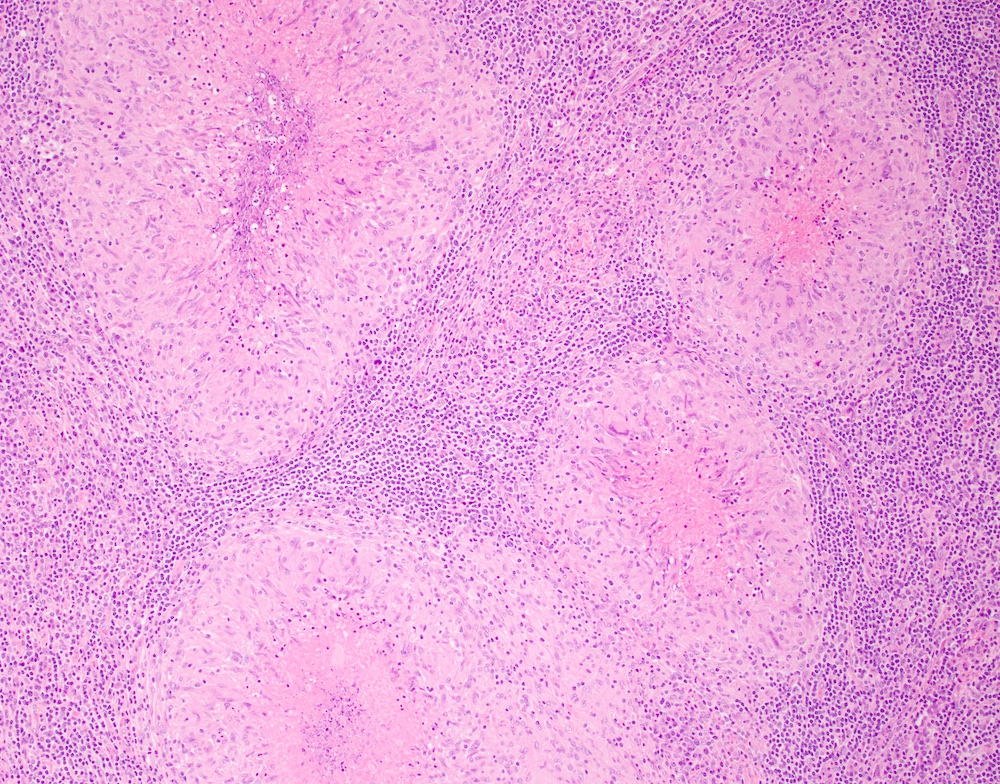
- Early: histiocytes and follicular hyperplasia, microabscesses localized adjacent to the thickened capsule (Am J Clin Pathol 2004;121:S71)
- Intermediate: capsulitis and subcapsular granulomas
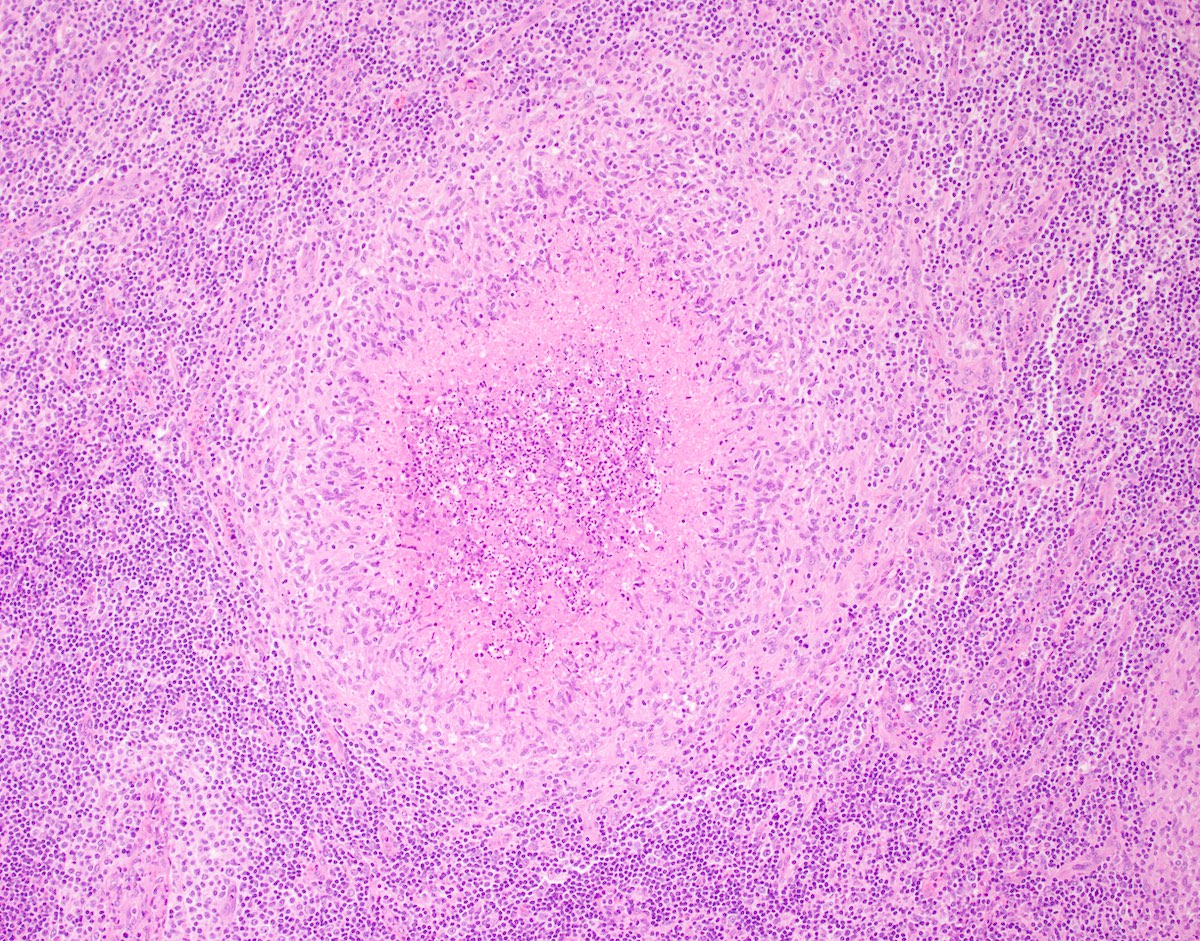
- Late: necrosis and abscesses, often stellate, surrounded by palisading histiocytes (Int J Dermatol 1978;17:656)
- Paracortical vascular proliferation (Am J Clin Pathol 2004;121:S71)
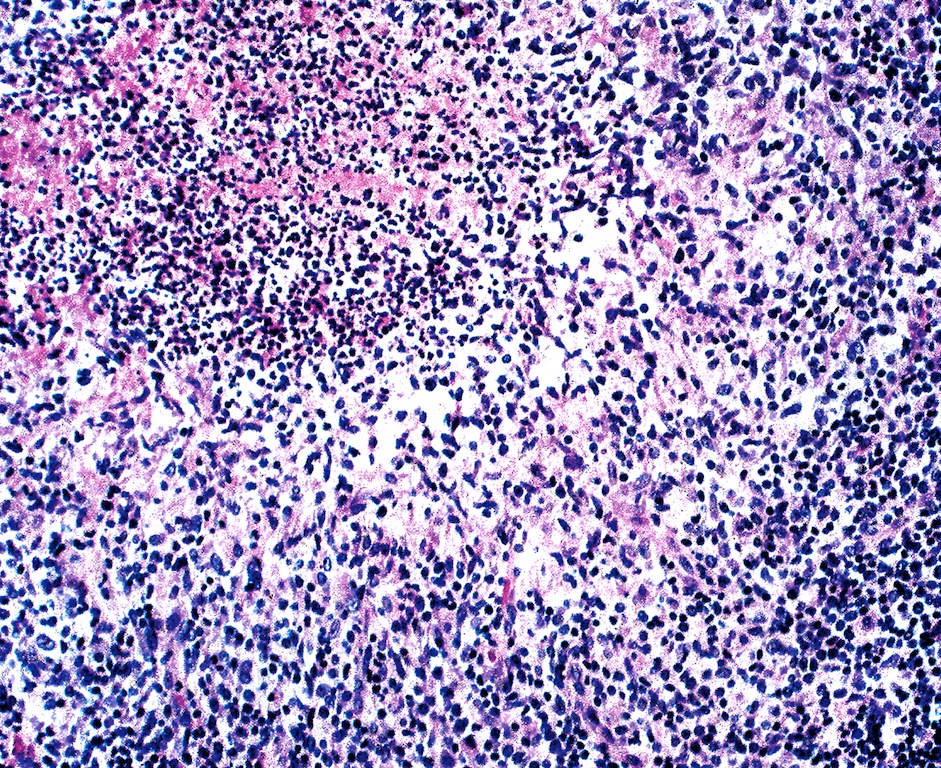
- Sinuses are often packed with monocytoid B cells but no epithelioid cells are present (Am J Clin Pathol 2004;121:S71)
- Small rods may be present with silver stain around small blood vessels and lymphatics; most readily identified early in disease (Science 1983;221:1403, Am J Clin Pathol 2004;121:S71)
- Skin shows dermal necrosis surrounded by histiocytes
- Also multinucleated giant cells, lymphocytes and eosinophils
- References: Calif Med 1955;82:25, Am Fam Physician 2011;83:152
Microscopic (histologic) images
Cytology description
- Similar to histologic features (granulomas, epithelioid histiocytes, neutrophils, necrosis, polymorphous lymphocytes) (Acta Cytol 1985;29:542, Diagn Cytopathol 1996;15:108)
Positive stains
- Warthin-Starry or other silver stains
- B. henslae immunohistochemistry (Am J Clin Pathol 2009;131:250)
- Combined use of Warthin-Starry and IHC may yield higher sensitivity than either alone (Appl Immunohistochem Mol Morphol 2020;28:781)
Negative stains
- Gram stain has limited utility, as Bartonella usually does not stain well (Am J Clin Pathol 2009;131:250)
Electron microscopy description
- Extracellular bacteria form small groups within bundles of collagen fibrils
- Bacteria are gram negative pleomorphic rods, with thick and homogeneous cell walls (Am J Clin Pathol 1987;87:739)
Molecular / cytogenetics description
- Causative organism may be detected by PCR (J Clin Microbiol 2005;43:3800)
Sample pathology report
- Cervical lymph node, excision:
- Necrotizing granulomatous lymphadenitis (see comment)
- Comment: The lymph node architecture is distorted by frequent stellate necrotizing granulomas with occasional multinucleated giant cells. Bacterial structures are identified by both Warthin-Starry stain and immunohistochemistry for B. henselae. The overall features are in keeping with cat scratch lymphadenitis, a condition that is generally self limited in immunocompentent patients.
Differential diagnosis
- Lymphoma, particularly classic Hodgkin lymphoma:
- May demonstrate granulomatous inflammation but will have Hodgkin / Reed-Sternberg cells and mixed inflammation, including eosinophils and plasma cells
- Sarcoidosis:
- Granulomas usually small and tight without suppuration
- Other infectious agents capable of causing granulomatous lymphadenitis:
- Kikuchi syndrome:
- No neutrophils
- Kimura disease:
- Eosinophils predominate, rather than neutrophils
Practice question #1
A 10 year old girl presents with an enlarged, tender axillary lymph node. An excisional biopsy is performed with findings shown. Which of the following is a likely clinical history for this patient?
- Asthma, peripheral blood eosinophilia and elevated serum IgE
- Drenching night sweats, petechial rash and peripheral blood cytopenias
- Fever, pharyngitis, splenomegaly and positive monospot (heterophile antibody) test
- Low grade fever and fatigue, new kitten in the household
Practice answer #1
D. Low grade fever and fatigue, new kitten in the household. The image shows multiple well formed suppurative granulomas. A relatively common cause of these morphologic findings is cat scratch disease, lymphadenitis transmitted by cats, almost always caused by B. henselae. Most patients with cat scratch disease are under the age of 18 and have recent exposure to a cat, with tender lymphadenopathy appearing in the draining lymph nodes from the site of a scratch. Fever, pharyngitis, splenomegaly and positive monospot (heterophile antibody) test (answer C) describes the classic presentation of infectious mononucleosis. Drenching night sweats, petechial rash and peripheral blood cytopenias (answer B) is more suggestive of a malignant process. Asthma, peripheral blood eosinophilia and elevated serum IgE (answer A) can be seen in Kimura disease.
Comment Here
Reference: Cat scratch disease
Comment Here
Reference: Cat scratch disease
Practice question #2
Practice answer #2
A. Cat scratch lymphadenitis. The image demonstrates lymphadenopathy with suppurative granulomas, a feature that can be seen in cat scratch lymphadenitis. Special stains (silver stain) or organism specific immunohistochemistry on tissue sections may be helpful. Clinical correlation (anatomic distribution of lymphadenopathy, presence of risk factors, such as contact with cats, etc.) and infectious disease workup (serologic studies and culture) are helpful. Kimura disease demonstrates prominent eosinophilic infiltration. Progressive transformation of germinal centers is characterized by indistinct germinal centers invaded by mantle zone cells. Treponema pallidum lymphadenopathy is characterized by plasmacytosis and capsular fibrosis.
Comment Here
Reference: Cat scratch disease
Comment Here
Reference: Cat scratch disease