Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Ly TY, Walsh NM. Sarcoidosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorsarcoidosis.html. Accessed September 24th, 2025.
Definition / general
- Multisystem granulomatous disorder with cutaneous involvement in up to 35% of cases
Essential features
- Multisystem granulomatous disorder with cutaneous involvement in up to 35% of cases
- Etiology is unknown
- Disease development and progression may be related to disordered immune response to extrinsic antigens in genetically susceptible individuals
- Clinically heterogeneous and can mimic other dermatological conditions
- Histologically characterized by discrete, nonnecrotizing granulomas with minimal lymphocytic inflammation involving the dermis or subcutaneous tissue
- Diagnosis of exclusion; particularly with respect to infection
Epidemiology
- Variable worldwide prevalence and can affect any age and race
- More common in northern Europe, Canada, U.S. and Australia; rare in Asia (Curr Opin Pulm Med 2020;26:527)
- Higher incidence among women and people of Afro-Caribbean descent (Ther Adv Chronic Dis 2018;9:227)
- Peak onset in third to fifth decades (Ther Adv Chronic Dis 2018;9:227)
Sites
- Skin: up to 35% of cases, with one - third having skin involvement as the first manifestation of disease (Dermatol Clin 2015;33:389, Clin Dermatol 2007;25:303)
- Lung: occurs in 90 - 95% of cases, most commonly bilateral hilar lymphadenopathy (J Am Acad Dermatol 2012;66:699.e1, J Am Acad Dermatol 2012;66:719.e1)
- Lymph nodes: peripheral lymphadenopathy in 10% of cases (J Am Acad Dermatol 2012;66:719.e1)
- Ocular: up to 50% in European and American populations and 50 - 90% in Japanese cases (J Am Acad Dermatol 2012;66:719.e1)
- Cardiac: up to 27% show involvement at postmortem and is a significant cause of mortality (J Am Acad Dermatol 2012;66:719.e1, Circulation 1978;58:1204)
- Central nervous system: up to 15% (J Am Acad Dermatol 2012;66:719.e1, Proc R Soc Med 1967;60:1169)
Pathophysiology
- Granulomatous inflammation is characterized by Th1 mediated immune response
- Antigen presenting cells recognize and internalize putative agents to form major histocompatibility complex (MHC) peptide complexes that are recognized by CD4+ T cells
- Cellular immune response is elicited with secretion of tumor necrosis factor alpha (TNF alpha), interferon gamma (IFN gamma), IL1, IL2, IL6, IL12, IL15, IL18 and macrophage inflammatory protein 1 (J Am Acad Dermatol 2012;66:699.e1, J Eur Acad Dermatol Venereol 2010;24:747, Curr Opin Rheumatol 2000;12:71)
Etiology
- Unknown
- May represent a chronic immunological response in a genetically susceptible individual that has been exposed to an undetermined extrinsic antigen (J Am Acad Dermatol 2012;66:699.e1, J Eur Acad Dermatol Venereol 2010;24:747)
Clinical features
- Familial clustering suggests genetic susceptibility in some cases
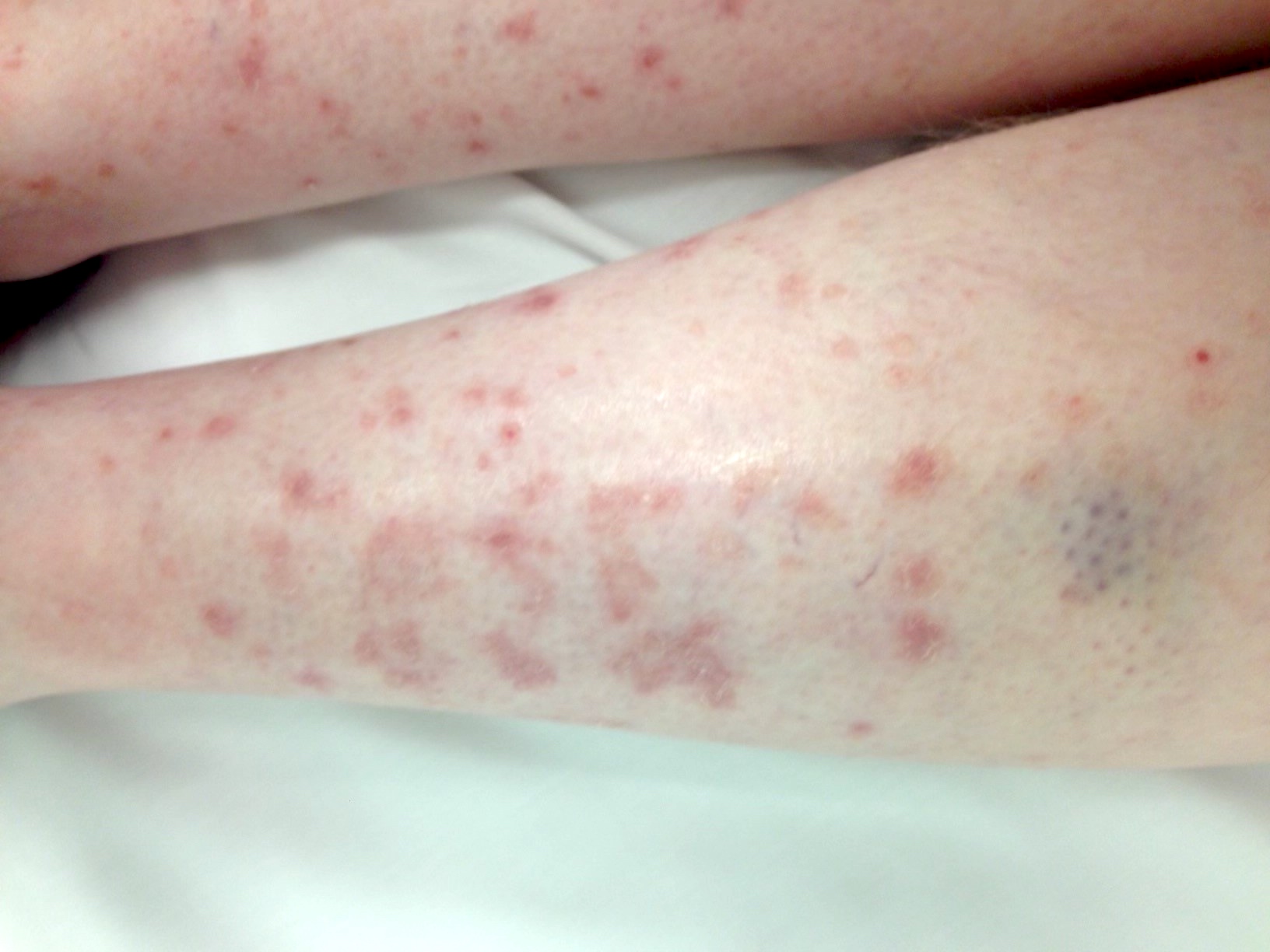
- Cutaneous manifestations are variable and can mimic other dermatological conditions
- Clinical morphology can range from papules and plaques (sometimes annular) to subcutaneous nodules
- Skin from any anatomic site may be affected
- Presentations include
- Acute and usually self limiting variant (Löfgren syndrome characterized by erythema nodosum, bilateral hilar adenopathy, fever and polyarthralgia)
- Chronic form involving skin only (20 - 40% of cutaneous sarcoidosis cases lack systemic involvement)
- Systemic chronic variant affecting multiple organs
- Lupus pernio is a chronic and disfiguring variant characterized by indurated lesions of the nose, cheeks and ears
- Scar sarcoidosis is characterized by development of lesions in surgical scars, tattoos, skin piercings and other sites of trauma
- Erythema nodosum occurs in up to 40% of patients with sarcoidosis (Medicine (Baltimore) 2017;96:e7595)
Diagnosis
- Diagnosis of exclusion
- Thorough history and physical exam (including ophthalmic evaluation) to assess for potential occupation / environmental exposures or associated systemic symptoms and signs
- Chest Xray, pulmonary function tests and cardiac investigations
- Reference: Cells 2021;10:766
Laboratory
- Skin biopsy to rule out infection and other inflammatory conditions
- Elevated serum angiotensin converting enzyme (ACE), elevated calcium, elevated erythrocyte sedimentation rate (ESR)
Radiology description
- Bilateral hilar lymphadenopathy on chest radiography is common
- Other less common findings: pulmonary infiltrates, fibrosis, bullae, cysts, emphysema
- Occasionally, bone lesions and cysts
- Reference: AJR Am J Roentgenol 2020;214:50
Prognostic factors
- Acute variant (Löfgren syndrome) is associated with good prognosis (Arch Dermatol 1997;133:882, Am J Respir Crit Care Med 1999;160:736)
- Chronic cutaneous sarcoidosis (particularly facial lesions) has a less favorable prognosis, with increased risk of pulmonary fibrosis and eye involvement (Am J Clin Dermatol 2008;9:155)
- Lupus pernio is associated with prolonged course, multisystem involvement (lung and upper respiratory tract, eye, bone cysts) and poor prognosis (Curr Probl Pediatr 2000;30:149)
Case reports
- 13 year old girl with livedo reticularis-like eruption (JAAD Case Rep 2019;5:392)
- 44 year old woman with Löfgren syndrome (BMJ Case Rep 2021;14:e239239)
- 49 year old woman with diabetes (CMAJ 2016;188:674)
- 52 year old woman with firm plaques (JAAD Case Rep 2019;5:810)
- 58 year old woman with morpheaform plaque (JAAD Case Rep 2021;14:30)
Treatment
- First line (limited or mild disease): topical and intralesional corticosteroids
- Systemic immunomodulators: tetracycline class antibiotics, antimalarials and other agents
- Systemic immunosuppressive and immunomodulatory agents: prednisone, methotrexate, TNF inhibitors and other biologic therapies
- References: Front Immunol 2020;11:545413, Eur Respir J 2021;58:2004079,
Clinical images
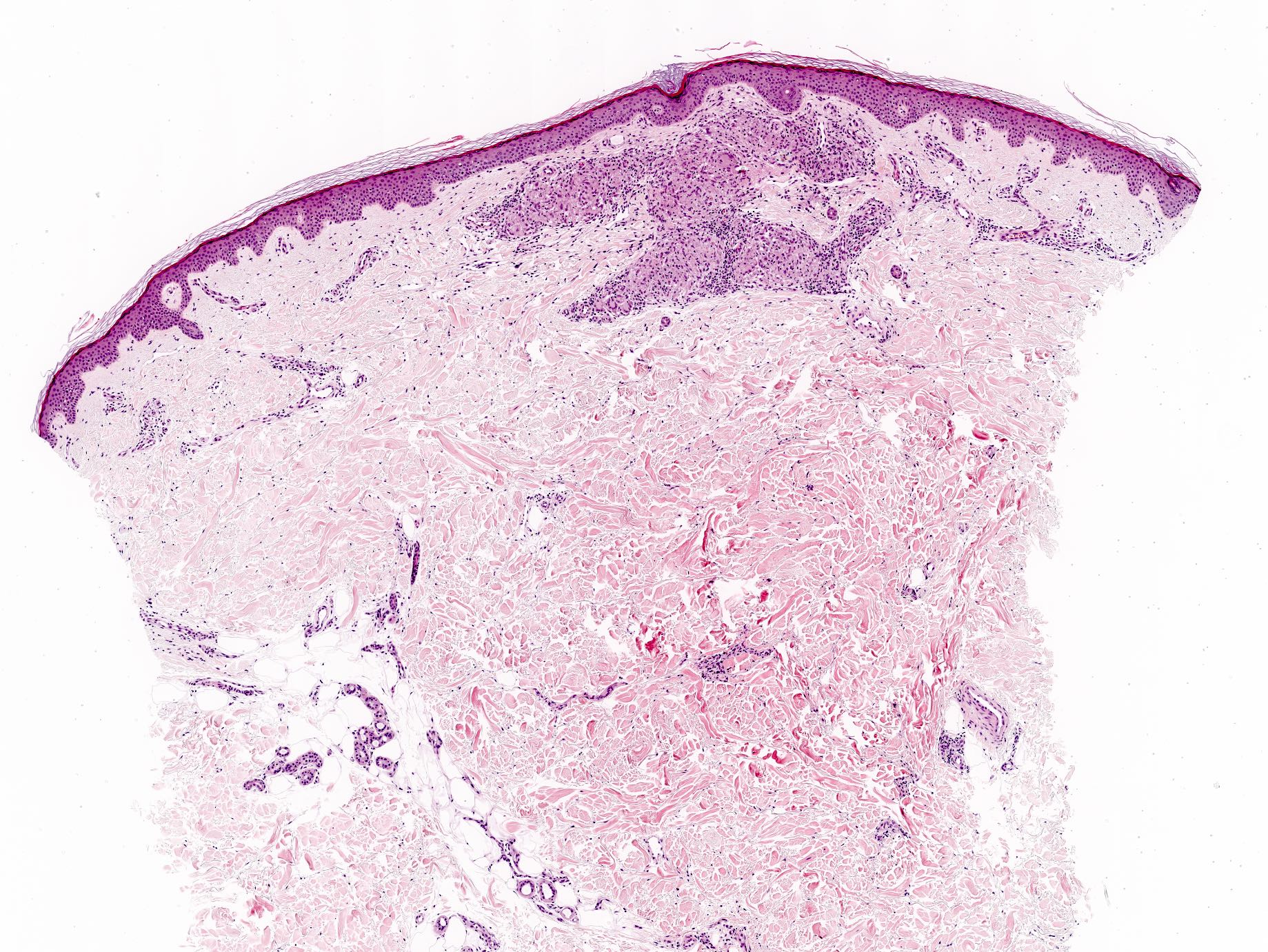
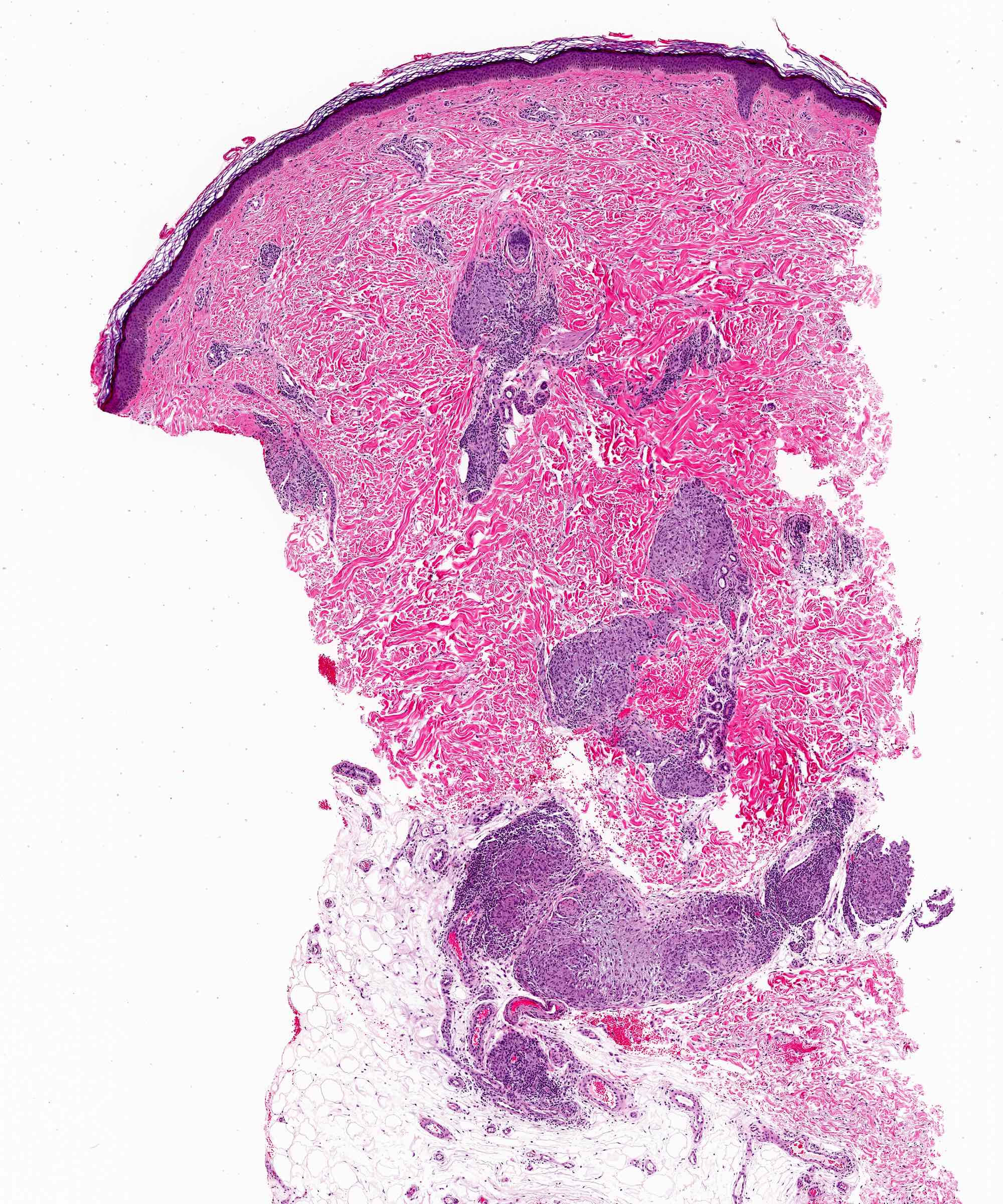
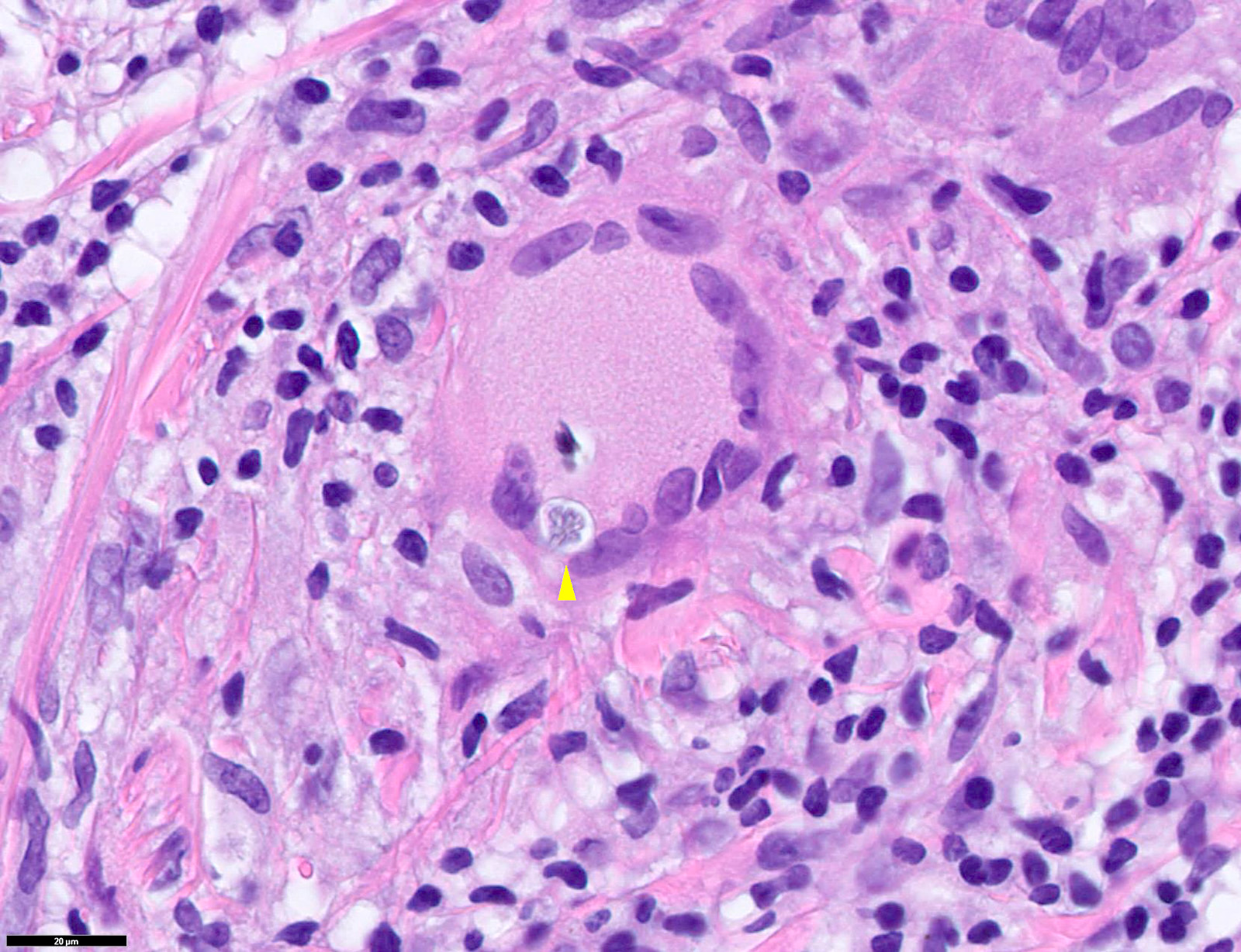
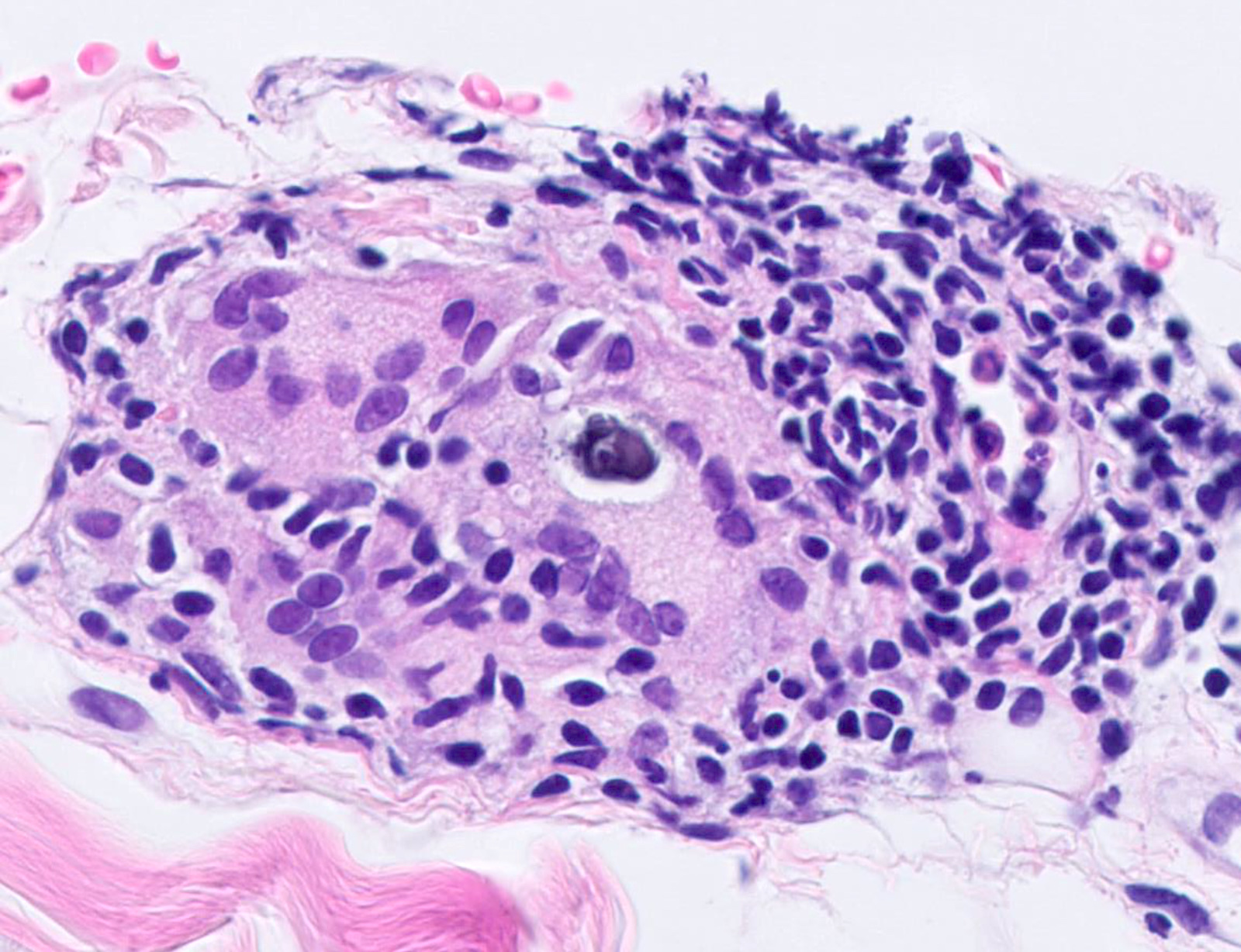
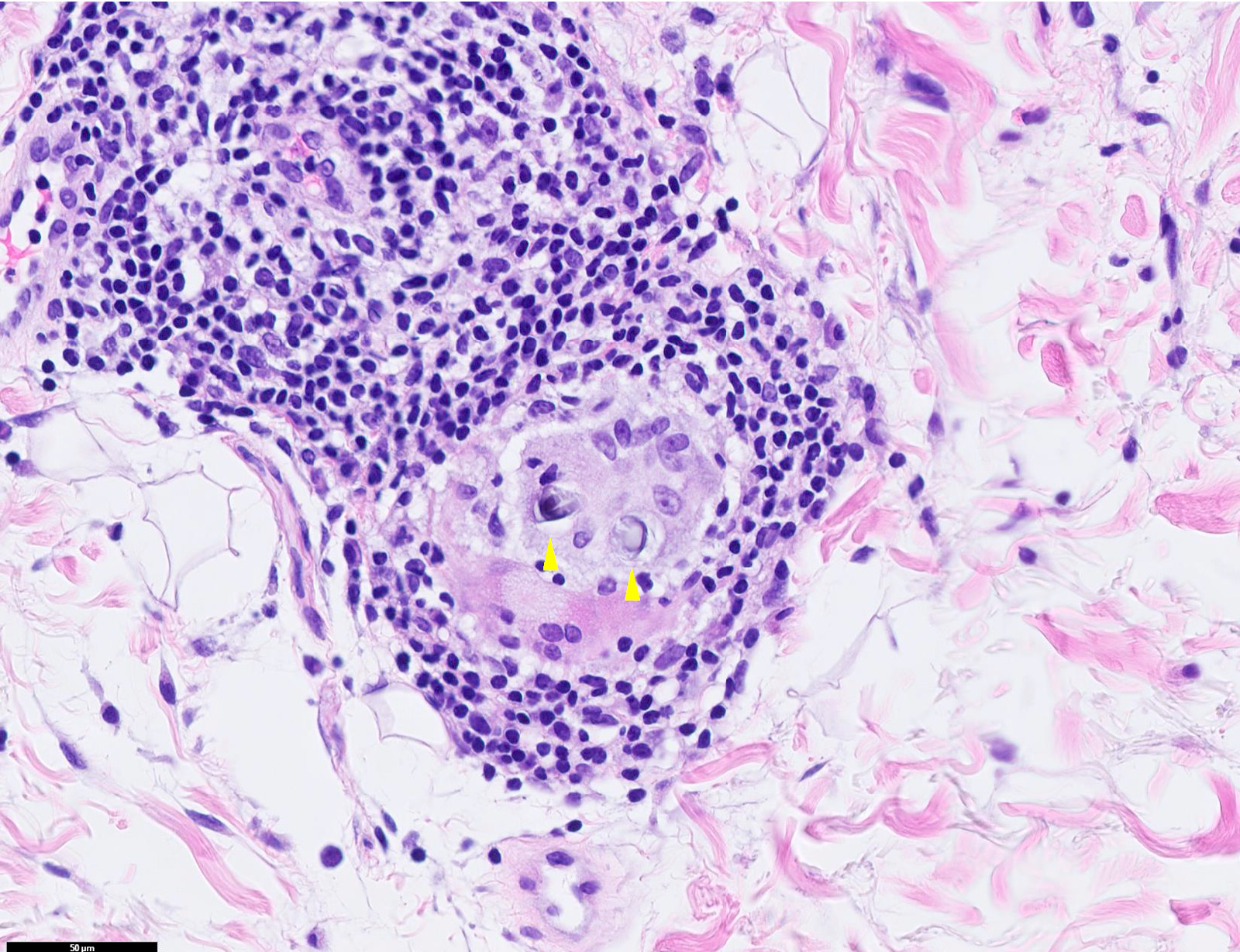
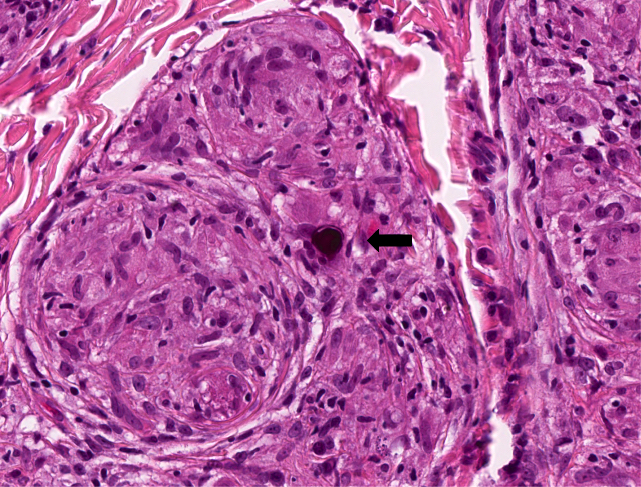
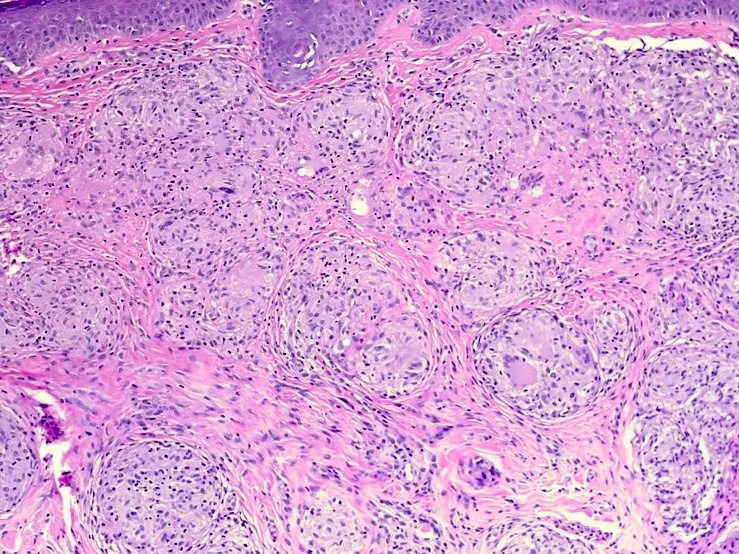
Microscopic (histologic) description
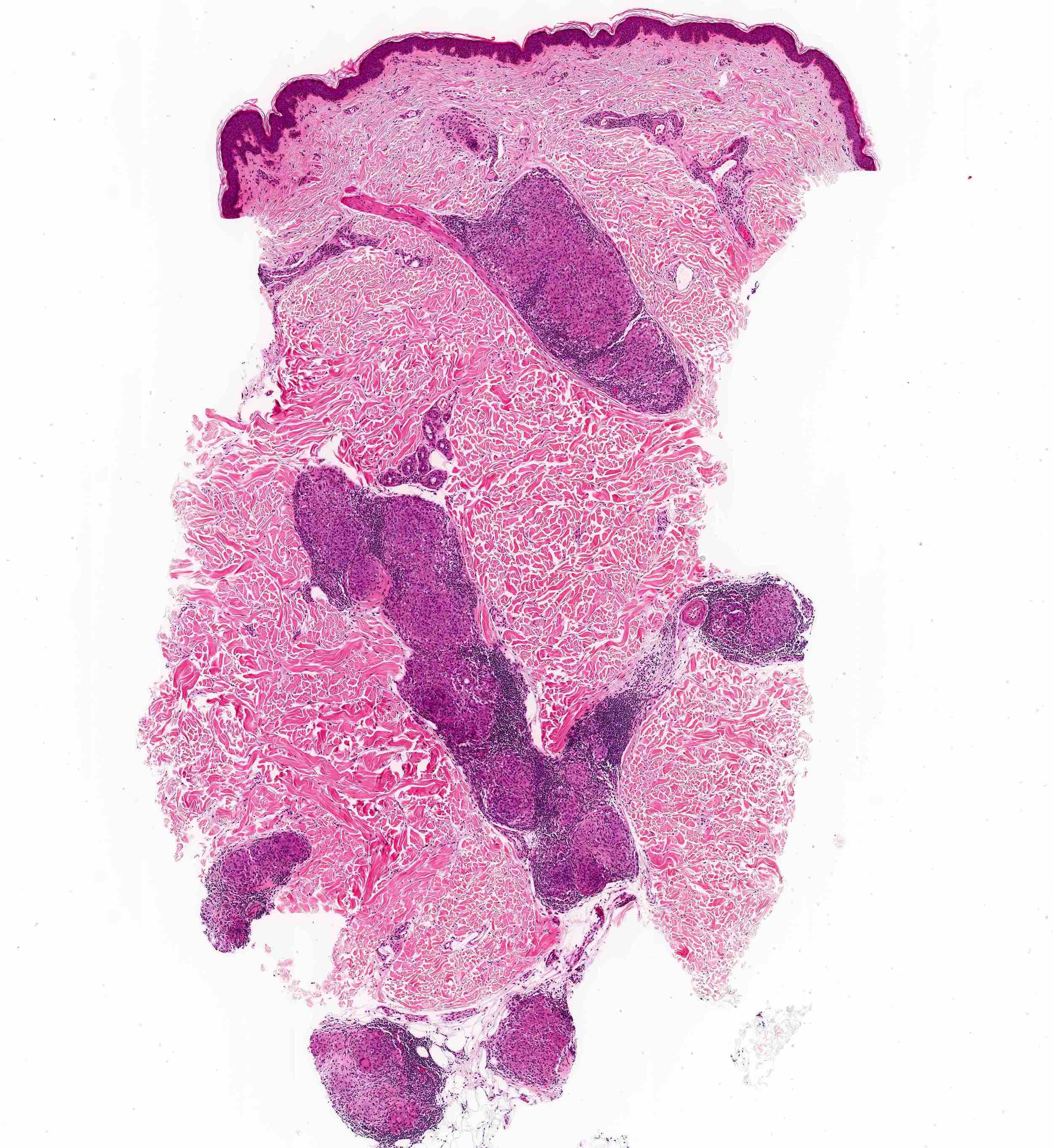
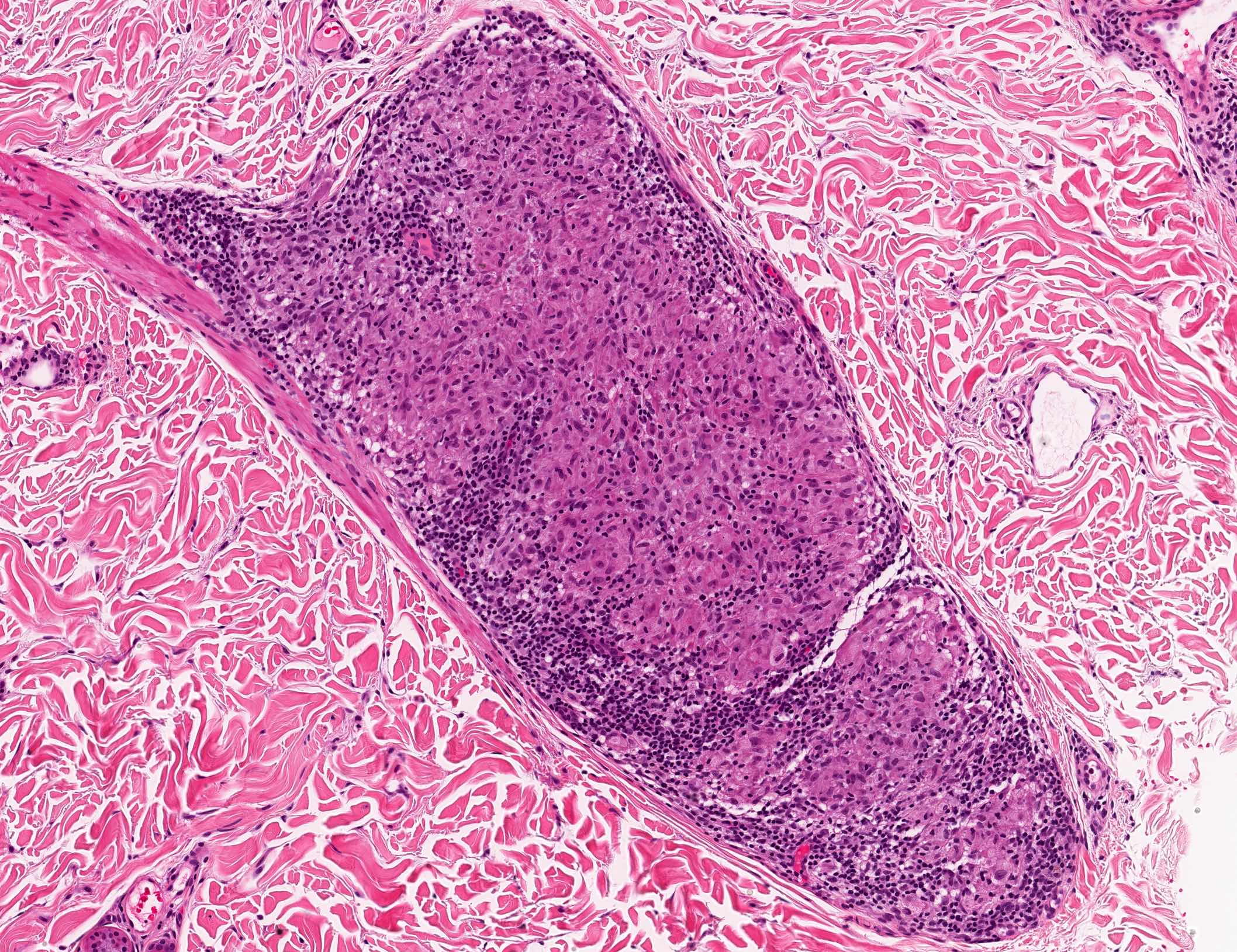
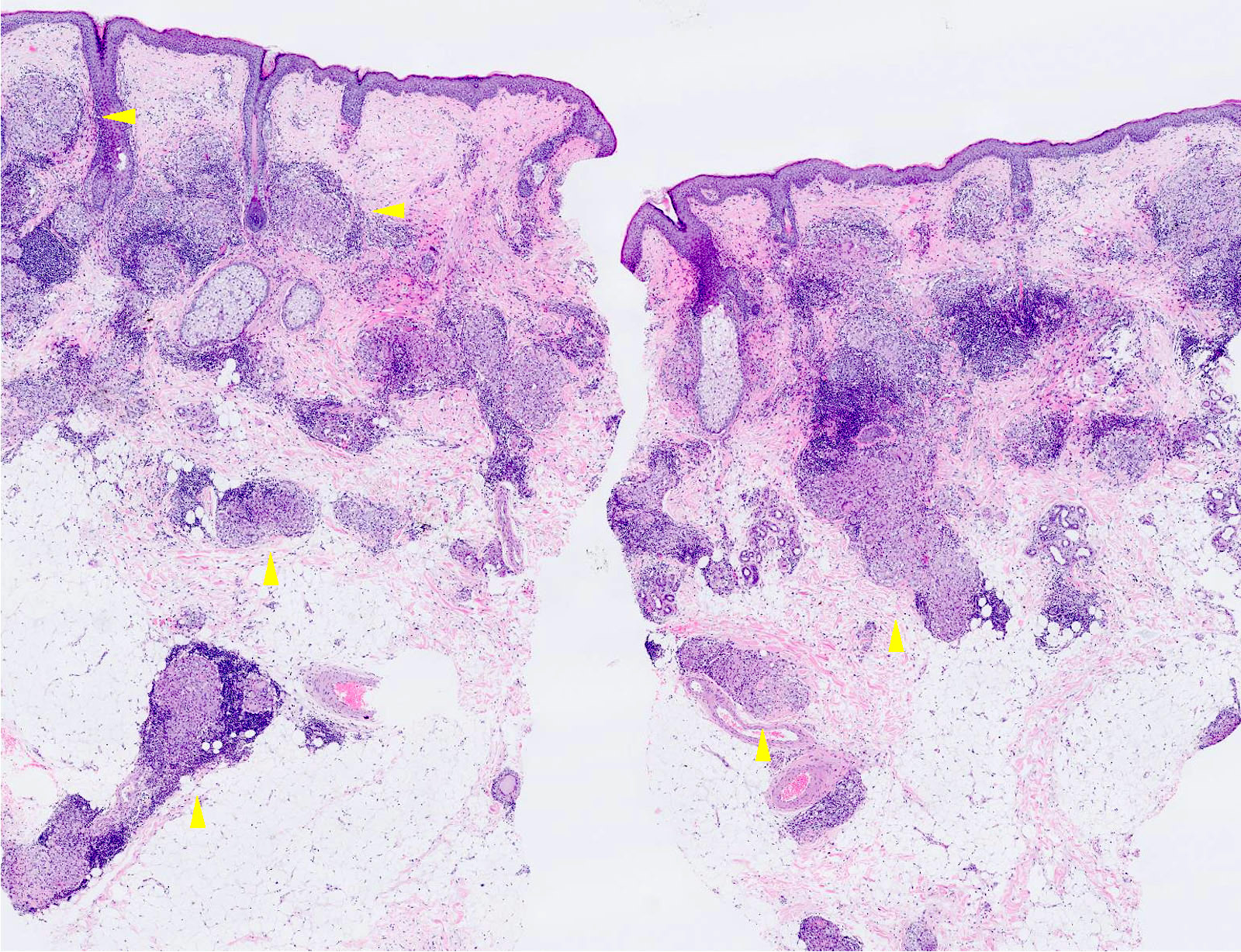
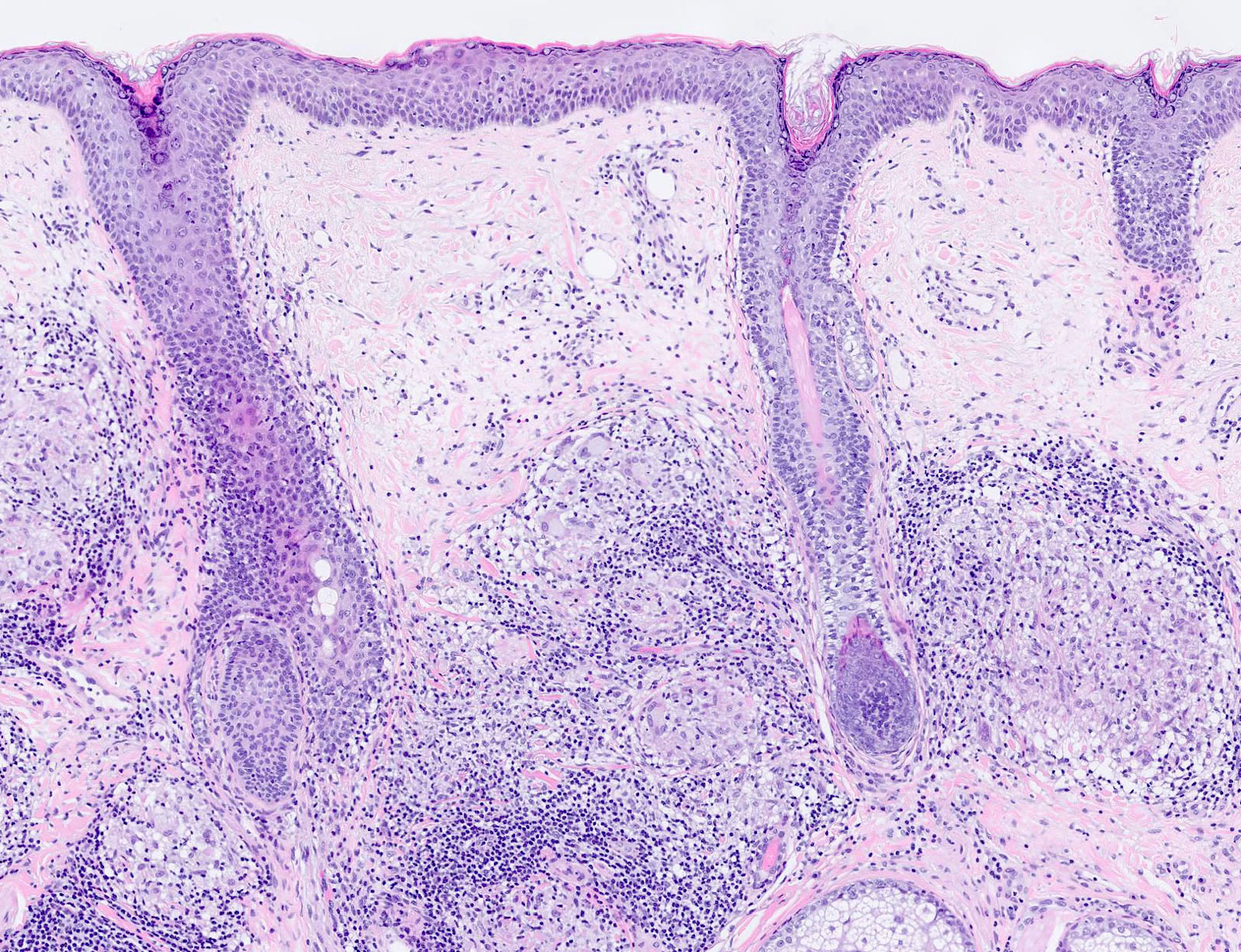
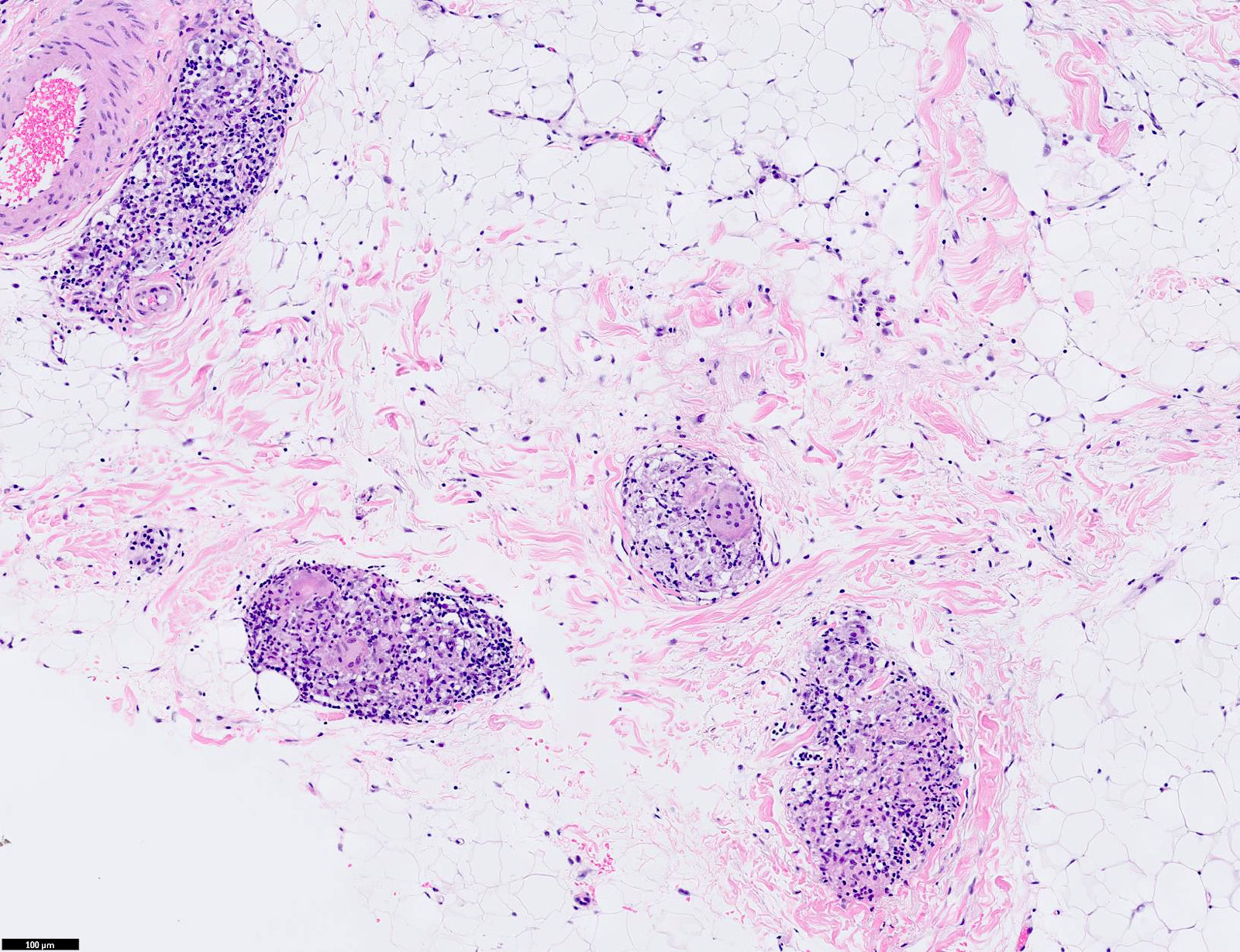
- Nodular, diffuse or angiocentric pattern of granulomatous inflammation in superficial or deep dermis with or without involvement of the subcutis
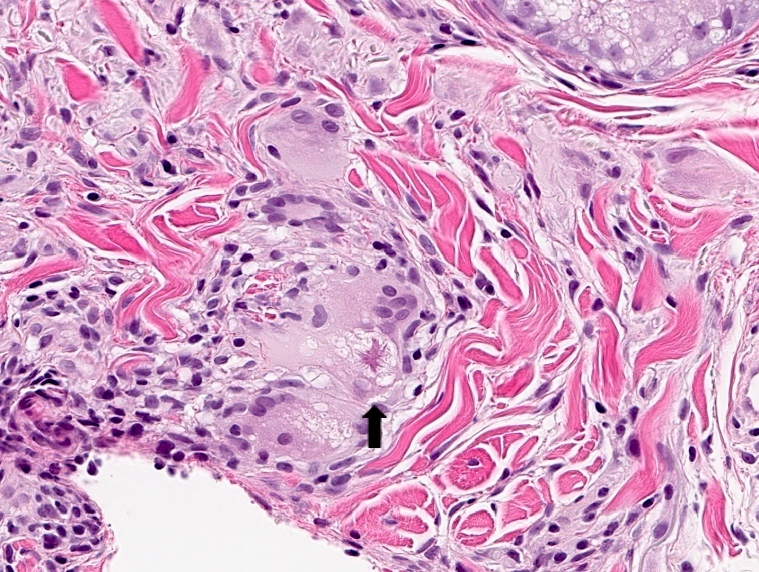
- Perineural granulomas can also be seen and are more frequently encountered than realized (J Cutan Pathol 2015;42:465)
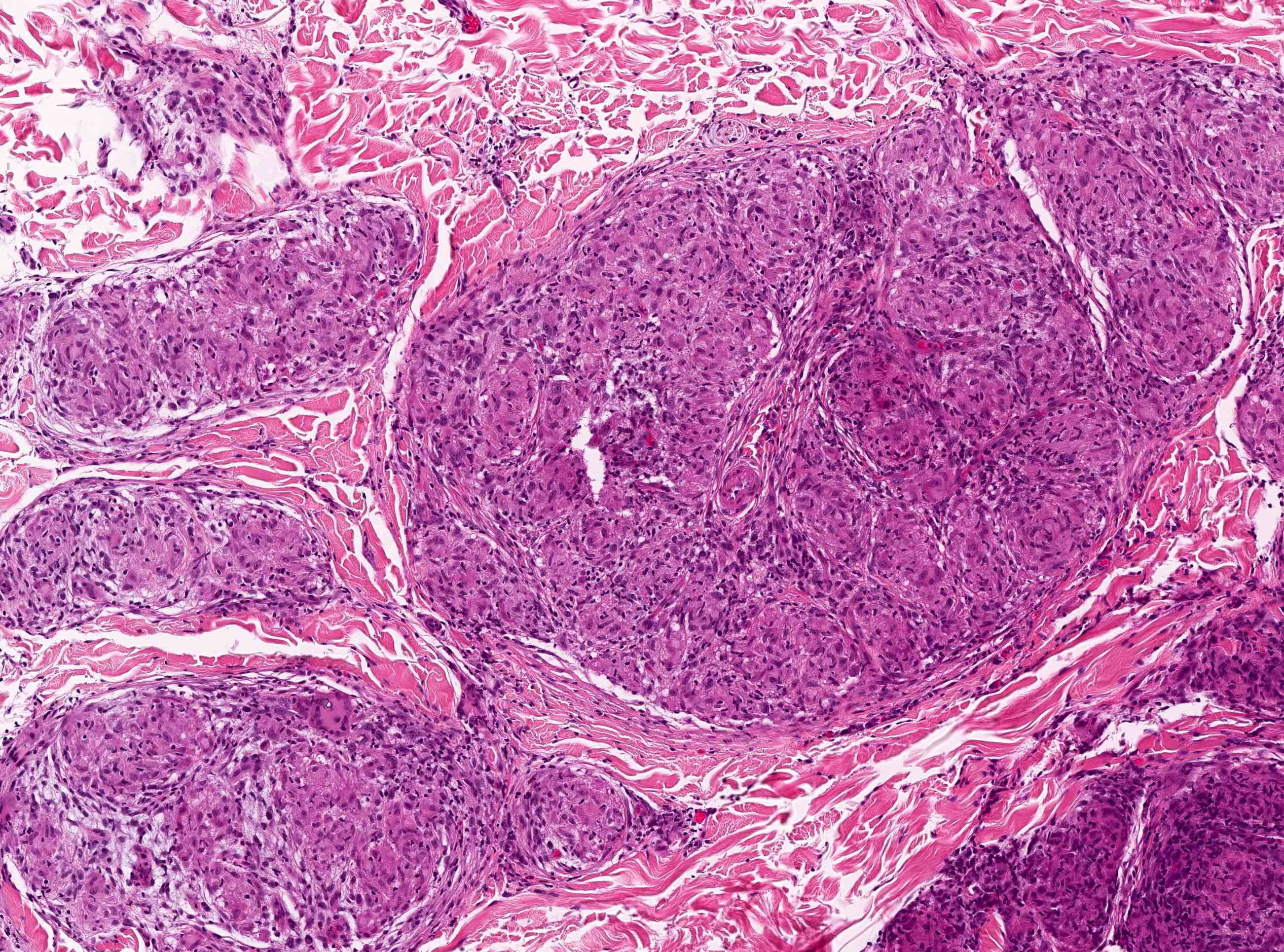
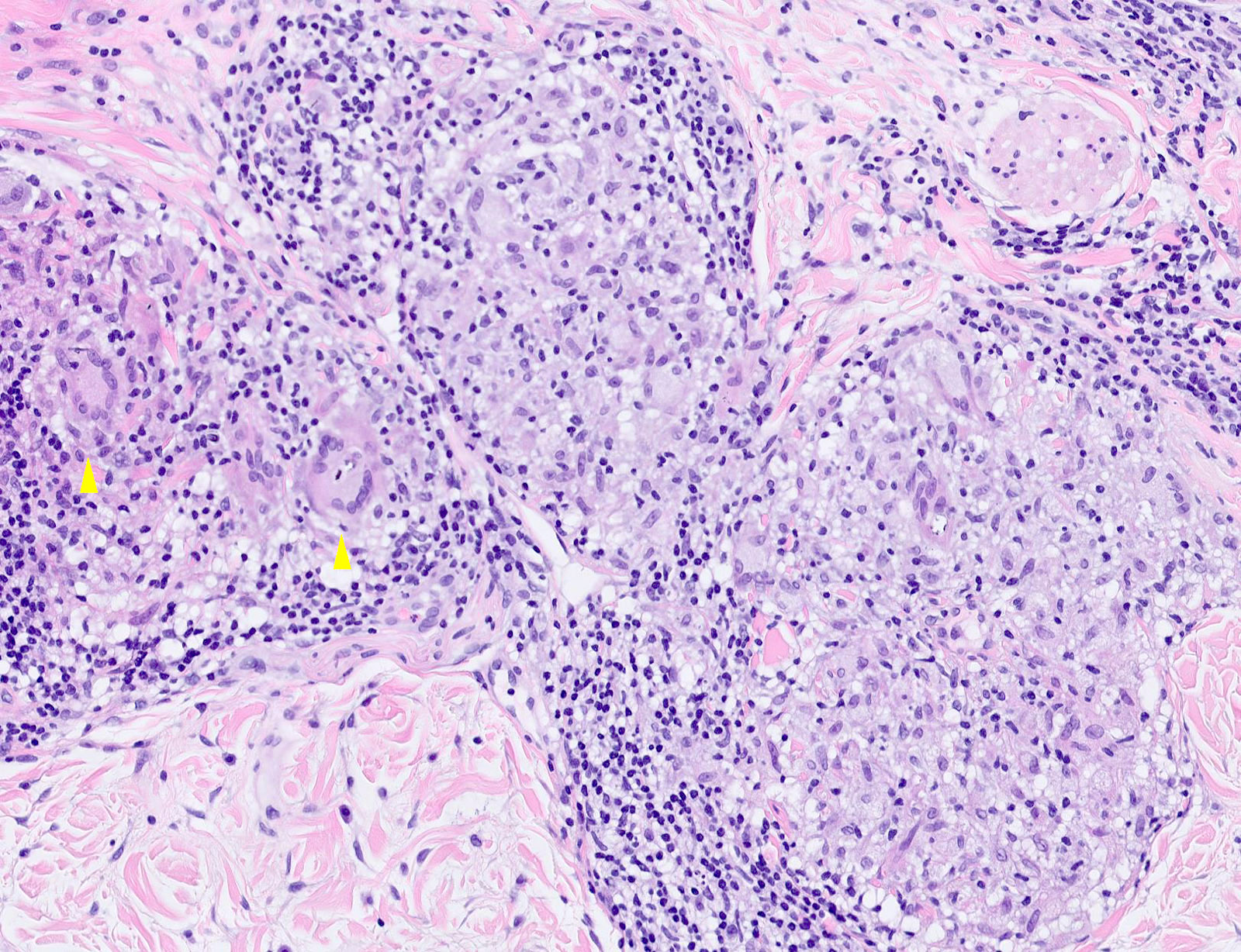
- Discrete or confluent nonnecrotizing granulomata composed of epithelioid histiocytes with abundant eosinophilic cytoplasm
- Variable number of Langhans or other giant cells
- Limited lymphocytic cuff surrounding granulomata (so called naked granulomas)
- Small foci of fibrinoid necrosis sometimes present but geographic or caseating necrosis is rare
- Typically, normal epidermis
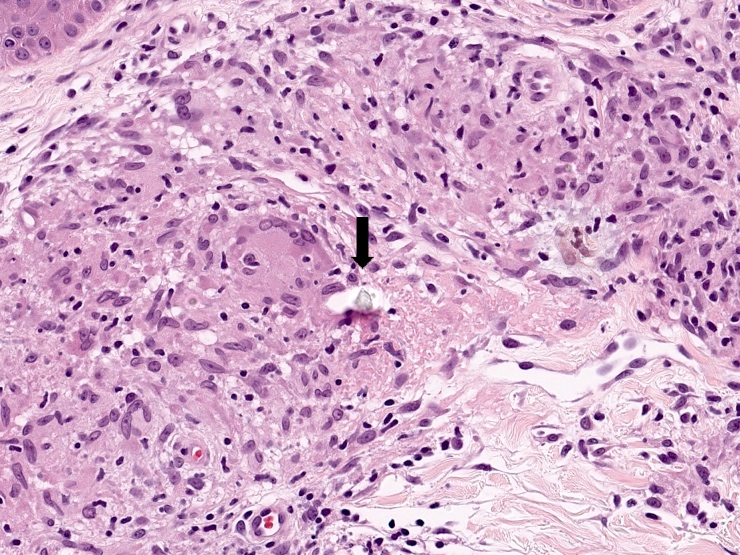
- Intracytoplasmic inclusion bodies may be seen but none are specific or pathognomonic
- Schaumann body: basophilic, calcified, laminated round structure
- Asteroid body: intracytoplasmic eosinophilic star shaped structure
- Foreign material is present in at least 5% of cases and does not exclude sarcoidosis (Arch Dermatol 2001;137:485, Arch Dermatol 2001;137:427, Am J Dermatopathol 1993;15:203)
Microscopic (histologic) images
Contributed by Thai Yen Ly, M.D., Jijgee Munkhdelger, M.D., Ph.D. and Andrey Bychkov, M.D., Ph.D.
Positive stains
Negative stains
- Fungal stains: periodic acid-Schiff (PAS), Gomori methenamine silver (GMS)
- Acid fast stains: fite, Ziehl-Neelson (ZN)
Sample pathology report
- Skin, punch biopsy:
- Granulomatous dermatitis, sarcoidal type (see comment)
- Comment: Special stains for fungal organisms (PAS and GMS) and mycobacteria (fite) are negative. The pattern of the granulomatous infiltrate, in the appropriate clinical context, would be consistent with sarcoidosis. Clinical pathologic correlation is recommended.
- Note: As sarcoidosis is a diagnosis of exclusion, a descriptive diagnosis is appropriate.
Differential diagnosis
- Infection:
- Concomitant neutrophilic infiltrate may be present
- Fungal organisms on PAS or GMS stains
- Mycobacteria on fite or Ziehl-Neelsen stains
- Positive culture
- Clinical features of infection
- Concomitant neutrophilic infiltrate may be present
- Foreign body reaction:
- Presence of foreign material
- Irregularly distributed giant cells with haphazardly arranged nuclei
- Cutaneous Crohn's disease:
- Usually perianal / genital distribution
- Ill defined granulomata
- Mixed inflammation is common (lymphocytes, eosinophils, plasma cells)
- Epidermal ulceration may be present
- Clinical history of Crohn's disease
- Granulomatous cheilitis (Melkersson-Rosenthal syndrome):
- Subtle and poorly formed granulomata
- Characteristic facial, lip and oral mucosal swelling with or without facial nerve palsy and fissured tongue
- Granulomatous rosacea (including perioral and periorbital dermatitis):
- Perifollicular distribution of granulomatous inflammation
- Tuberculoid granulomata (less circumscribed, more confluence, prominent lymphoplasmacytic inflammation) rather than sarcoidal granulomata
- Background of prominent vascular ectasia
- Characterized by persistent erythema and recurrent episodes of flushing, edema, papules and pustules
- Tuberculoid leprosy:
- Elongated sausage shaped granulomata around nerves
- PCR studies may be helpful
- Localized lesion on trunk or limb with associated sensory impairment
- Necrobiosis lipoidica:
- Features altered collagen (necrobiosis), lymphoid aggregates and lymphoplasmacytic infiltrate
- Association with diabetes mellitus
- Granuloma annulare (sarcoidal variant):
- Palisading or interstitial pattern of more typical granuloma annulare may also be present to suggest the diagnosis
- Increased dermal mucin
- Beryllium and zirconium:
- Granulomata are indistinguishable from sarcoidosis
- History of exposure
Additional references
Practice question #1
A 45 year old woman presents with fever, polyarthralgia, bilateral hilar adenopathy, erythema nodosum and an erythematous papular skin eruption on the face. Punch biopsy of a facial lesion is shown the image above. What is the most likely diagnosis?
- Granuloma annulare
- Granuloma faciale
- Rheumatoid nodule
- Sarcoidosis
- Xanthelasma
Practice answer #1
D. Sarcoidosis. Given the microscopic findings and clinical context, the most likely diagnosis is sarcoidosis (acute variant Löfgren syndrome). The image shows well formed, nonnecrotizing and nonpalisading sarcoidal granulomata. Granuloma faciale is considered a localized form of vasculitis with an eosinophil rich infiltrate that is not granulomatous. Rheumatoid nodules feature palisading granulomatous inflammation around pink fibrinous material that can mimic necrosis. Granuloma annulare is another palisading granulomatous process associated with increased dermal mucin. Xanthelasma features loose, ill defined aggregates of foam cells in the dermis.
Comment Here
Reference: Sarcoidosis
Comment Here
Reference: Sarcoidosis
Practice question #2
Regarding sarcoidosis, which of the following statements is true?
- Associated foreign material may be present and does not exclude sarcoidosis
- Asteroid body inclusions are a diagnostic feature
- Fungal organisms are sometimes seen on special stains
- Geographic necrosis is a common finding
- Schaumann body inclusions are a diagnostic feature
Practice answer #2
A. Associated foreign material may be present in some cases of sarcoidosis (e.g., scar sarcoidosis) and does not exclude the diagnosis of sarcoidosis. Schaumann and asteroid body inclusions are not specific or pathognomonic for sarcoidosis and can be seen in other conditions such as tuberculosis, tuberculoid leprosy and berylliosis. Prominent geographic necrosis is rare but small foci of fibrinoid necrosis are sometimes evident in sarcoidosis. The presence of fungal organisms confirms infection and is incompatible with sarcoidosis, which is a diagnosis of exclusion.
Comment Here
Reference: Sarcoidosis
Comment Here
Reference: Sarcoidosis