Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Immunofluorescence description | Immunofluorescence images | Negative stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Li A, Kazlouskaya V. Pemphigus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorpemphigus.html. Accessed May 13th, 2024.
Definition / general
- Pemphigus is a group of acantholytic conditions caused by autoantibodies against various epidermal cell junction proteins, commonly presenting with flaccid blisters, erosions or scaling
Essential features
- Group of acantholytic conditions including 4 main forms: pemphigus vulgaris, pemphigus foliaceus, paraneoplastic pemphigus and a newly described IgA pemphigus
- Caused by IgG or IgA autoantibody against epidermal antigens (commonly desmoglein 1 and desmoglein 3)
- Most frequent clinical presentation: flaccid bullae or crusted erosions involving skin or mucosa
- Prototypic histopathological feature: intraepidemal acantholysis with intact basal layer (tombstone sign) and intraepidermal eosinophils
- Direct immunofluorescence shows intercellular IgG / IgA and C3
ICD coding
- ICD-10: L10 - L10.9 - pemphigus
Epidemiology
- Pemphigus vulgaris:
- Most common form (80%) in pemphigus group
- Incidence ranges from 0.76 to 16.1 per million, with higher incidence among Ashkenazi Jewish, Indian, Southeast European and Middle Eastern populations (J Am Acad Dermatol 2016;75:925, Immunol Res 2018;66:255)
- Average age of onset: 40 - 60 years
- May affect neonates via transplacental autoantibody transmission (JAMA Dermatol 2021;157:220)
- Pemphigus foliaceus:
- Average age of onset: 40 - 60 years
- Most common form of pemphigus in Brazil, Tunisia and Finland (J Invest Dermatol 1995;104:302)
- Endemic pemphigus foliaceus in Brazil and Tunisia may be associated with environmental factors
- Affects females, younger patients (J Invest Dermatol 1995;104:302)
- Paraneoplastic pemphigus constitutes up to 5% of total pemphigus cases (J Invest Dermatol 2019;139:469)
Sites
- Skin, mucosae, nails (paronychia)
Pathophysiology
- IgG or IgA autoantibody against epidermal antigens (Exp Dermatol 2005;14:861, Clin Rev Allergy Immunol 2018;54:1):
- Pemphigus vulgaris: IgG to desmoglein 1 (skin) or desmoglein 3 (mucosa)
- Pemphigus foliaceus: IgG to desmoglein 1
- Paraneoplastic pemphigus: IgG to desmoplakin I, desmoplakin II, plectin, periplakin, envoplakin, BP230 or A2ML1
- IgA pemphigus: IgA to desmocollin 1 (subcorneal pustular dermatosis [SPD] variant); IgA to desmoglein 1, desmoglein 3 (intraepidermal neutrophilic [IEN] variant)
- Compensation theory: desmoglein 1 compensates for desmoglein 3 in the skin of patients with mucosal lesions and vice versa (J Clin Invest 1999;103:461)
- Cell mediated toxicity plays a role in paraneoplastic pemphigus with T cells attacking epidermis resulting in lichenoid inflammation
Etiology
- Association with human leukocyte antigen class II: HLA-DR4 and HLA-DR14, HLA-DRB1 0402, 1401, 0503, 0302 (Front Med (Lausanne) 2018;5:226)
- Endemic pemphigus foliaceus: Simulium nigrimanum (black fly) is a possible vector
- Drug induced pemphigus:
- Thiol drugs (e.g. penicillamine, captopril)
- Penicillamine → pemphigus foliaceus
- Nonthiol drugs (e.g. penicillin, cephalosporin, enalapril, rifampin, NSAID) (Br Med J 1976;2:1423)
- Thiol drugs (e.g. penicillamine, captopril)
- Paraneoplastic pemphigus:
- B cell lymphoproliferative disorders, Castleman disease, Waldenström macroglobulinemia, carcinomas (bronchus, pancreas, liver, uterus, breast, thyroid, liver), thymoma, sarcoma (N Engl J Med 1990;323:1729)
Clinical features
- Pemphigus vulgaris:
- Mucosal erosions (oral or genital), painful flaccid blisters
- Hoarseness if larynx or pharynx are involved
- Rarely isolated crusted lesions on the scalp, paronychia, foot ulcers and macroglossia
- Mucosal erosions (oral or genital), painful flaccid blisters
- Pemphigus vulgaris variants:
- Pemphigus vegetans:
- Neumann type (severe) and Hallopeau type (mild)
- Affects intertriginous areas, blisters evolving into hypertrophic vegetations and pustules, cerebriform tongue (Ankara Univ Hekim Fak Derg 1988;15:137)
- Pemphigus vegetans:
- Pemphigus foliaceus:
- Affects seborrheic areas (face, scalp, upper trunk)
- Crusted superficial erosions
- Pemphigus foliaceus variants:
- Pemphigus erythematosus (Senear-Usher syndrome):
- Plaques with crusted erosions on the face (malar areas)
- Patients may have underlying lupus erythematosus
- Endemic pemphigus foliaceus: small blisters, erosions or papules (J Dermatol 2015;42:18)
- Pemphigus herpetiformis:
- Usually a variant of pemphigus foliaceus, rarely of pemphigus vulgaris
- Urticarial plaques and vesicles in herpetiform pattern
- Pemphigus erythematosus (Senear-Usher syndrome):
- Paraneoplastic pemphigus:
- Mucosal involvement (severe stomatitis and conjunctivitis)
- Erythema multiforme-like (targetoid) lesions on the palms and soles
- Lichenoid lesions
- Bronchiolitis obliterans
- IgA pemphigus:
- Small superficial blisters / pustules arranged in annular / arcuate plaques with crusting in the center; mucosae are usually not involved (Oncol Lett 2014;8:62)
- Superficial flaccid pustular blister (SPD variant)
- Generalized crusted macules with peripheral pustules (IEN variant)
- Signs:
- Nikolsky sign: induction of blister / erosion by slight friction
- Asboe-Hansen sign: lateral extension of intact blister with gentle pressure
Diagnosis
- Made on clinical, histopathologic, immunopathologic and serologic findings (Turk Patoloji Derg 2016;32:91)
- Histopathology
- Biopsy for H&E taken from the edge of the blister
- Immunopathology
- Direct immunofluorescence (most sensitive)
- Biopsy taken from the perilesional skin
- Serology
- Enzyme linked immunosorbent assay (ELISA) (see Laboratory)
- Indirect immunofluorescence (J Invest Dermatol 1980;75:183)
- Immunoblotting and immunoprecipitation (less used)
- Endoscopy may help identify extraoral mucosal lesions (Clin Endosc 2014;47:452)
- Paraneoplastic pemphigus may utilize chest Xray, CT scans, pulmonary function tests and cancer screening
Laboratory
- Indirect immunofluorescence: intercellular deposition of IgG or IgA
- Pemphigus vulgaris and variants:
- IgG against desmoglein 3 or desmoglein 1 and 3
- Monkey esophagus used as a substrate
- Pemphigus foliaceus and variants:
- IgG against desmoglein 1
- Guinea pig used as a substrate (J Invest Dermatol 1987;88:545)
- Paraneoplastic pemphigus:
- IgG against envoplakin, periplakin, desmoglein 1 and desmoglein 3
- Rat bladder used as a substrate for plakin
- IgA pemphigus:
- IgA against desmocollin 1 (SPD variant)
- IgA against desmoglein 1, desmoglein 3 (IEN variant)
- Pemphigus vulgaris and variants:
- Enzyme linked immunosorbent assay (ELISA):
- Pemphigus vulgaris (IgG against desmoglein 3 or 1)
- Pemphigus foliaceus (IgG against desmoglein 1)
- Paraneoplastic pemphigus (antibodies against envoplakin and periplakin)
- IgA pemphigus (IgA and sometimes IgG to desmocollin 1, desmoglein 1 and desmoglein 3)
- Immunoblotting and immunoprecipitation (rarely used today)
- Other findings:
- Possible autoimmune related thrombocytopenia, neutropenia and anemia
Radiology description
- Bronchiolitis obliterans in pemphigus paraneoplastica presents with reduction of vessels and areas of bronchiectasis
Radiology images
Prognostic factors
- Historically, 5 year mortality > 90%
- Improved with oral steroids and steroid sparing treatments (Int J Dermatol 2005;44:470)
- Pemphigus foliaceus has better prognosis than pemphigus vulgaris
- Poor prognosis factors (J Eur Acad Dermatol Venereol 2010;24:947):
- Younger age at presentation
- Mucosal involvement at presentation
- Relapses
- Paraneoplastic pemphigus (Arch Dermatol 2012;148:1165):
- 5 year survival is about 40%
- Poor prognosis factors: erythema multiforme-like lesions, bronchiolitis obliterans, extensive involvement
Case reports
- Newborn boy with extensive vesiculobullous lesions on the anterior side of his chest and abdomen, born from mother with known pemphigus vulgaris (Rev Paul Pediatr 2019;37:130)
- 6 year old girl with widespread annular lesions with superficial pustules (Indian J Dermatol Venereol Leprol 2016;82:439)
- 30 year old woman with 3 year history of vegetative and ulcerated lesions on the oral mucosa (Niger J Clin Pract 2018;21:1238)
- 44 year old woman with multiple pruritic annular plaques and dyspnea (JAAD Case Rep 2016;2:436)
- 45 year old man with chronic lymphocytic leukemia developed severe stomatitis and cutaneous blisters (J Med Case Rep 2018;12:252)
Treatment
- Rituximab is a first line in moderate and severe cases (J Eur Acad Dermatol Venereol 2020;34:1900)
- Systemic steroids are treatment of choice if rituximab is not available
- Systemic immunosuppressive medications (azathioprine, mycophenolate mofetil, methotrexate, cyclosporine and dapsone) are used as steroid sparing agents
- Local skin care
- Prevention of secondary infection (especially herpes simplex virus)
- Intravenous immune globulin, immunoadsorption, plasmapheresis, extracorporeal photopheresis or cyclophosphamide for refractory cases
- Dapsone may be used as a first line agent for IgA pemphigus (Indian J Dermatol 2012;57:495)
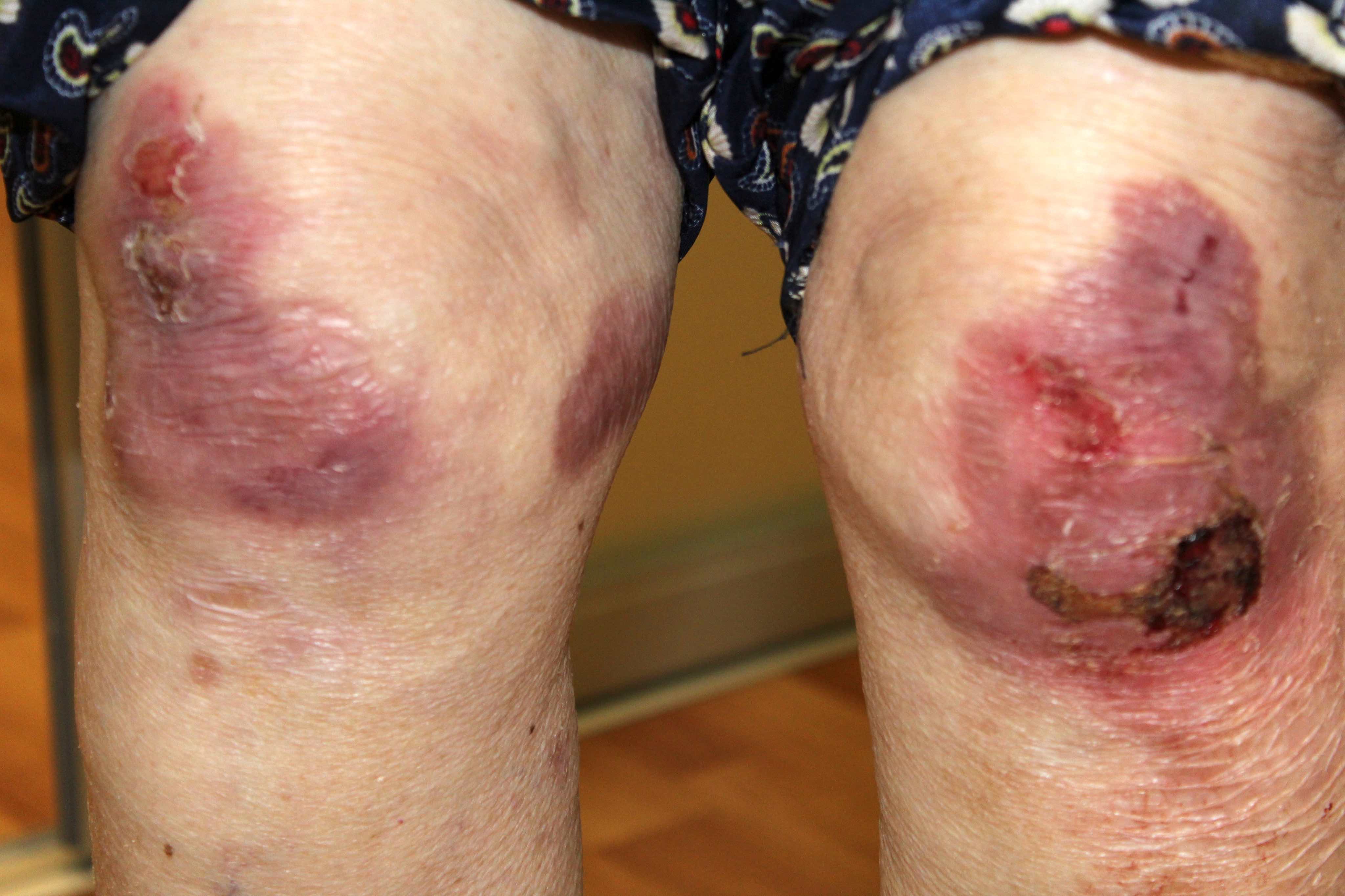
Clinical images
Contributed by Natalia Zhovta, M.D., Yi C. Lai, M.D., Maria Hannaway, M.D., Jamerson Loyal, M.D., Iryna Tsikhanouskaya, M.D., Ph.D., Timothy Patton, D.O. and Juliana Jung, M.D.
Pemphigus vulgaris:
Pemphigus foliaceus:
Paraneoplastic pemphigus:
IgA pemphigus:
Images hosted on other servers:
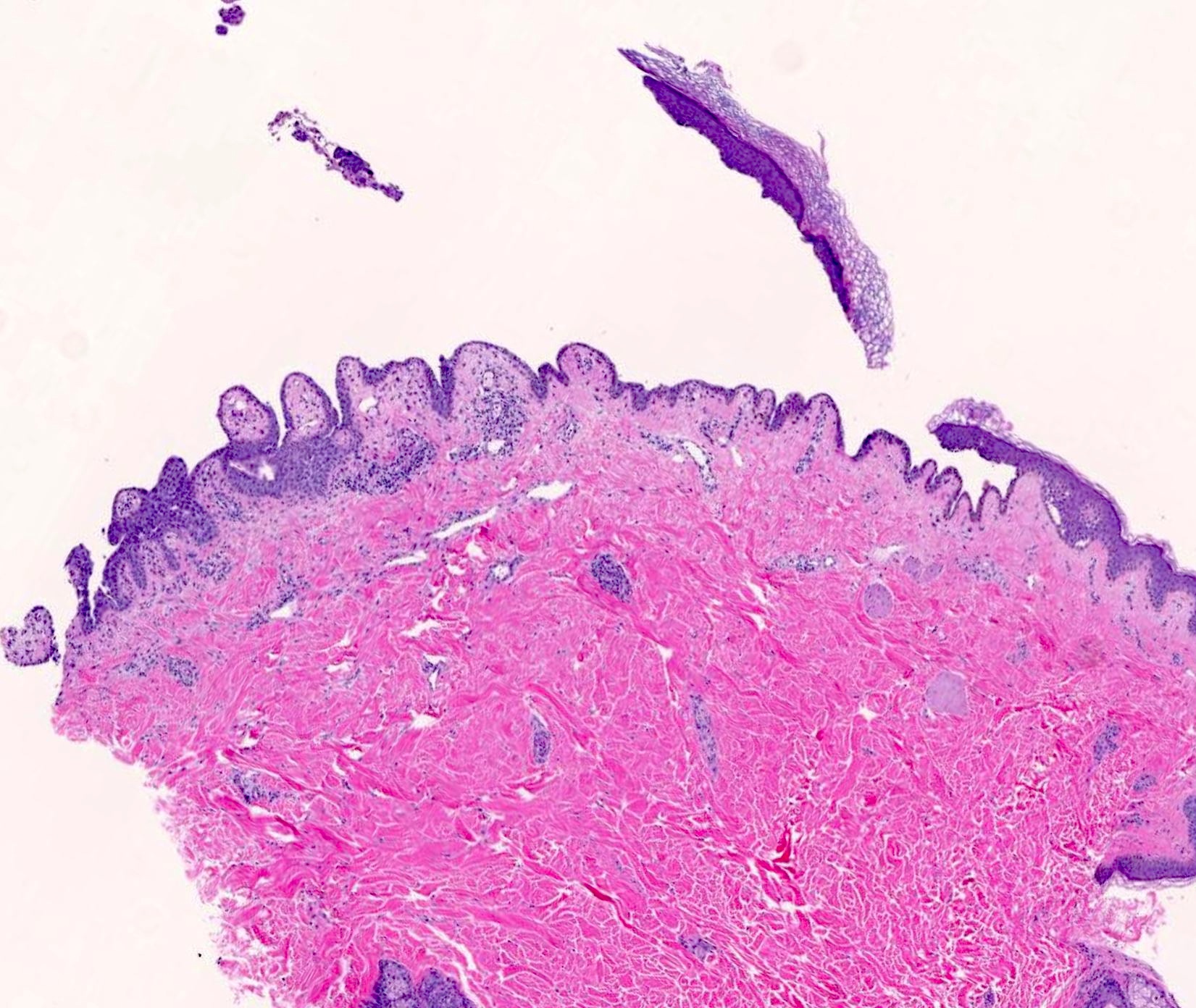
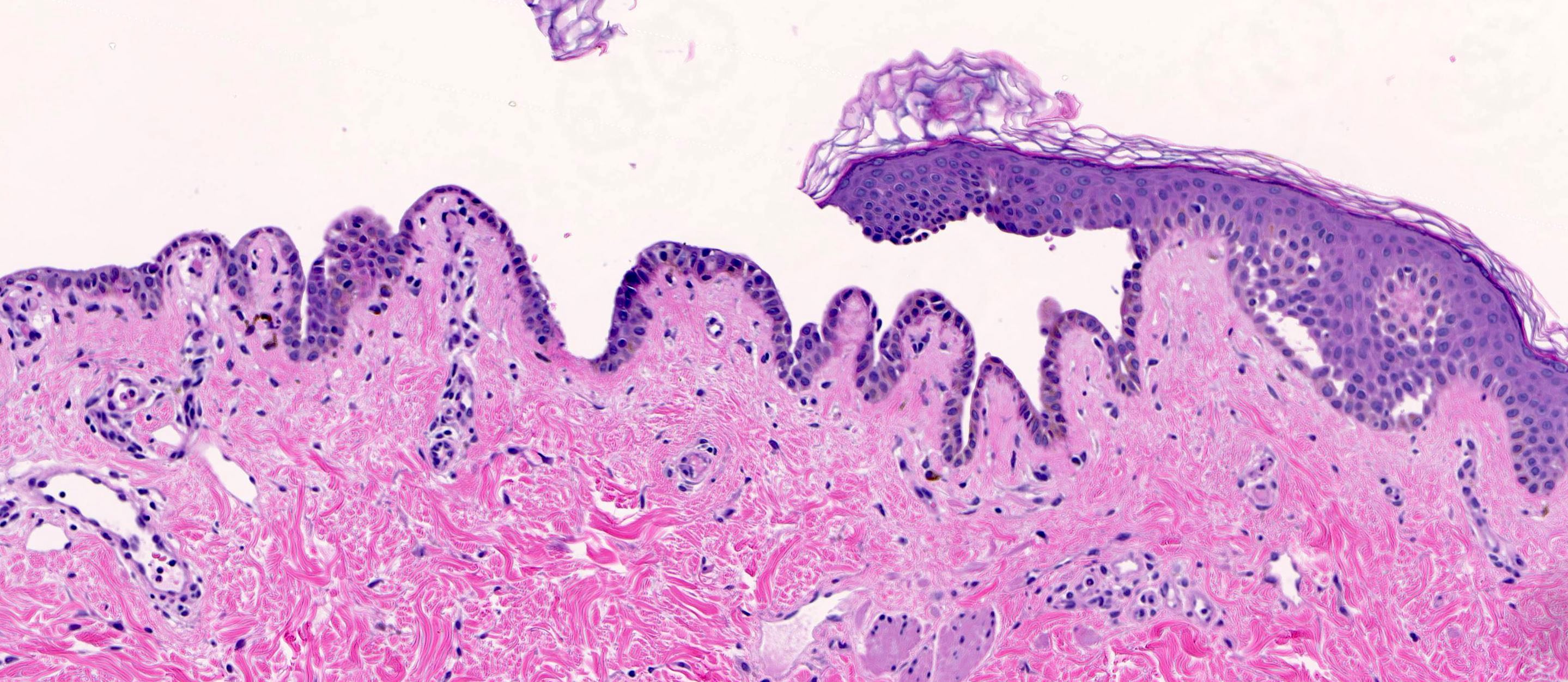
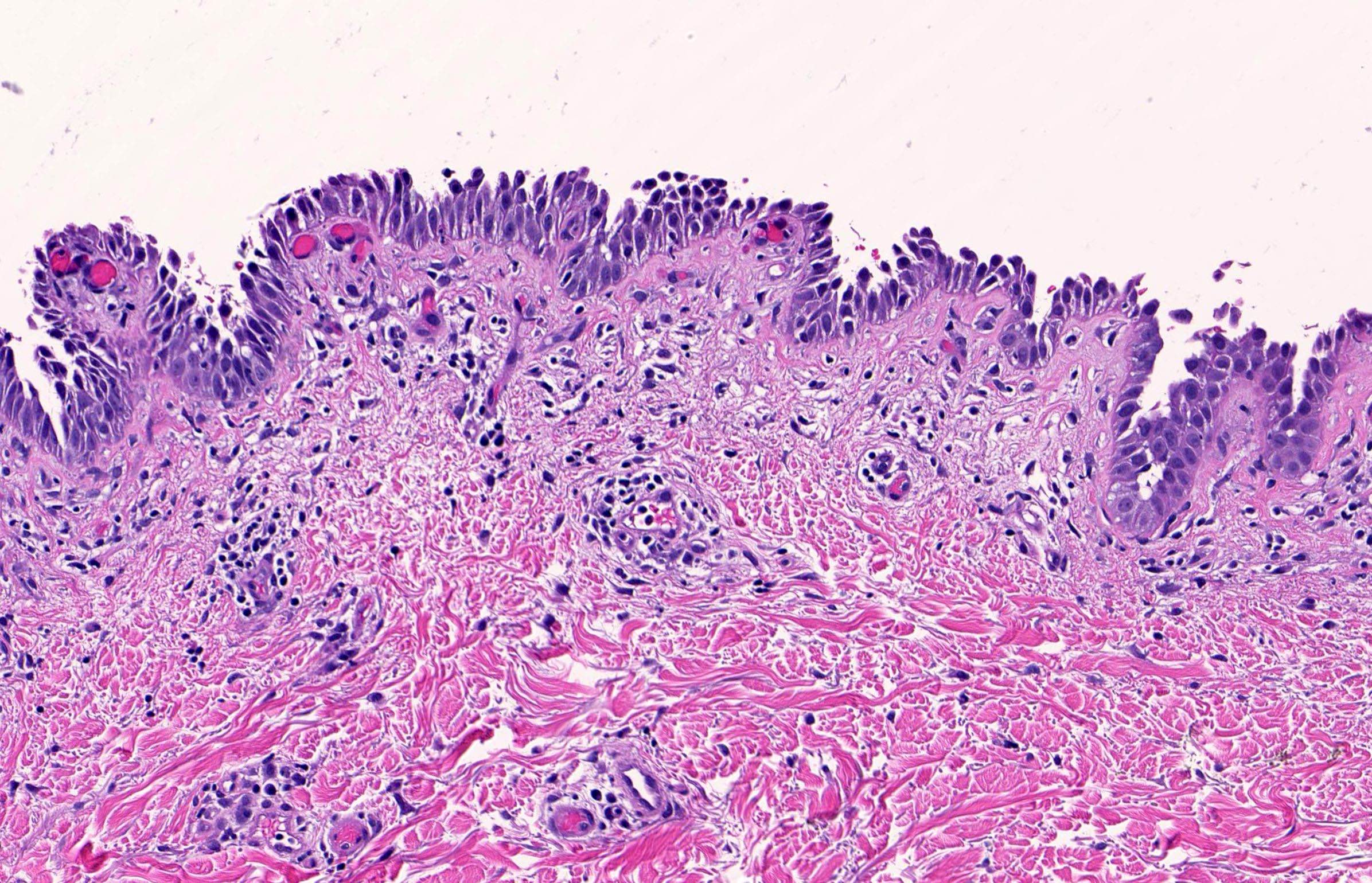
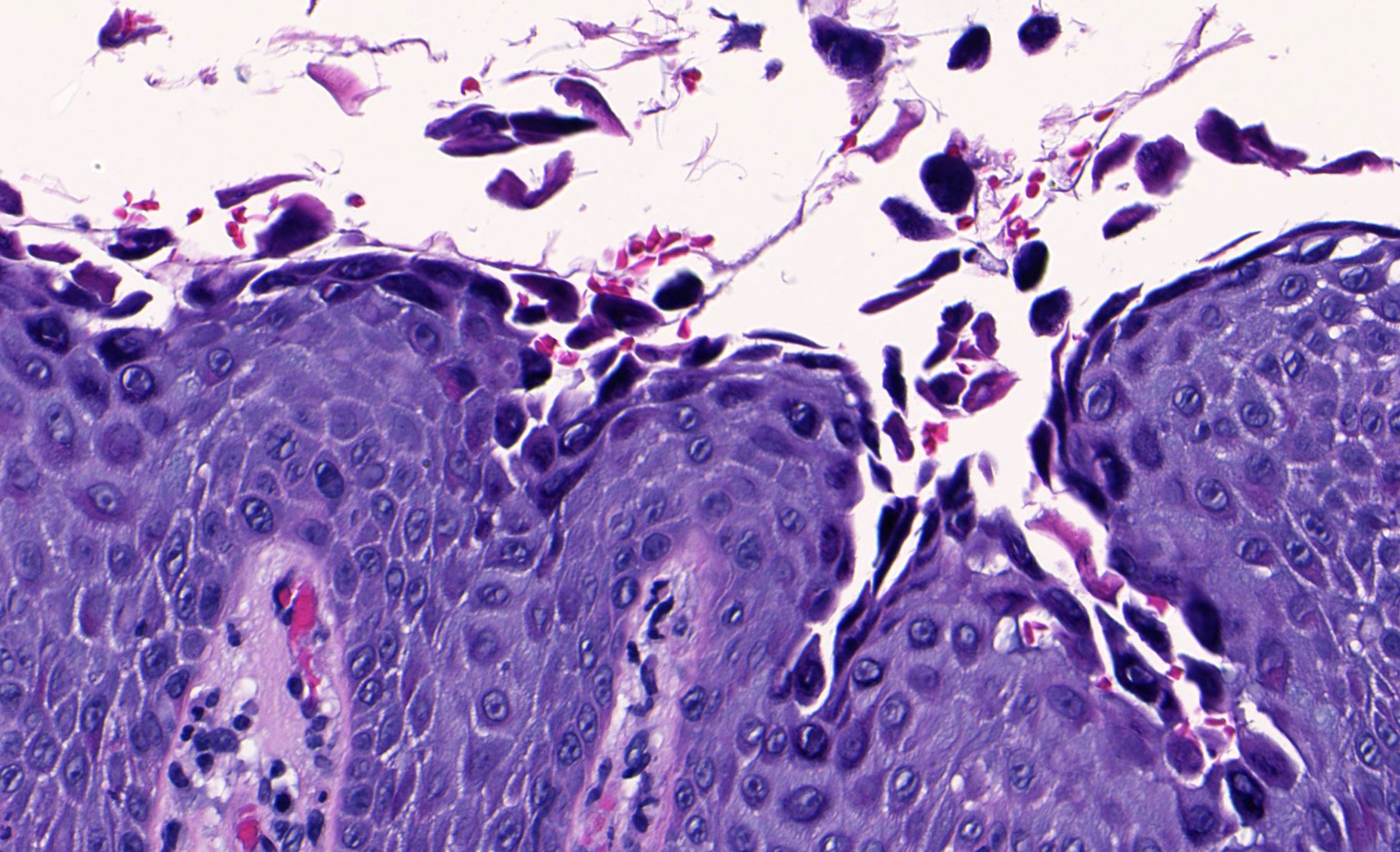
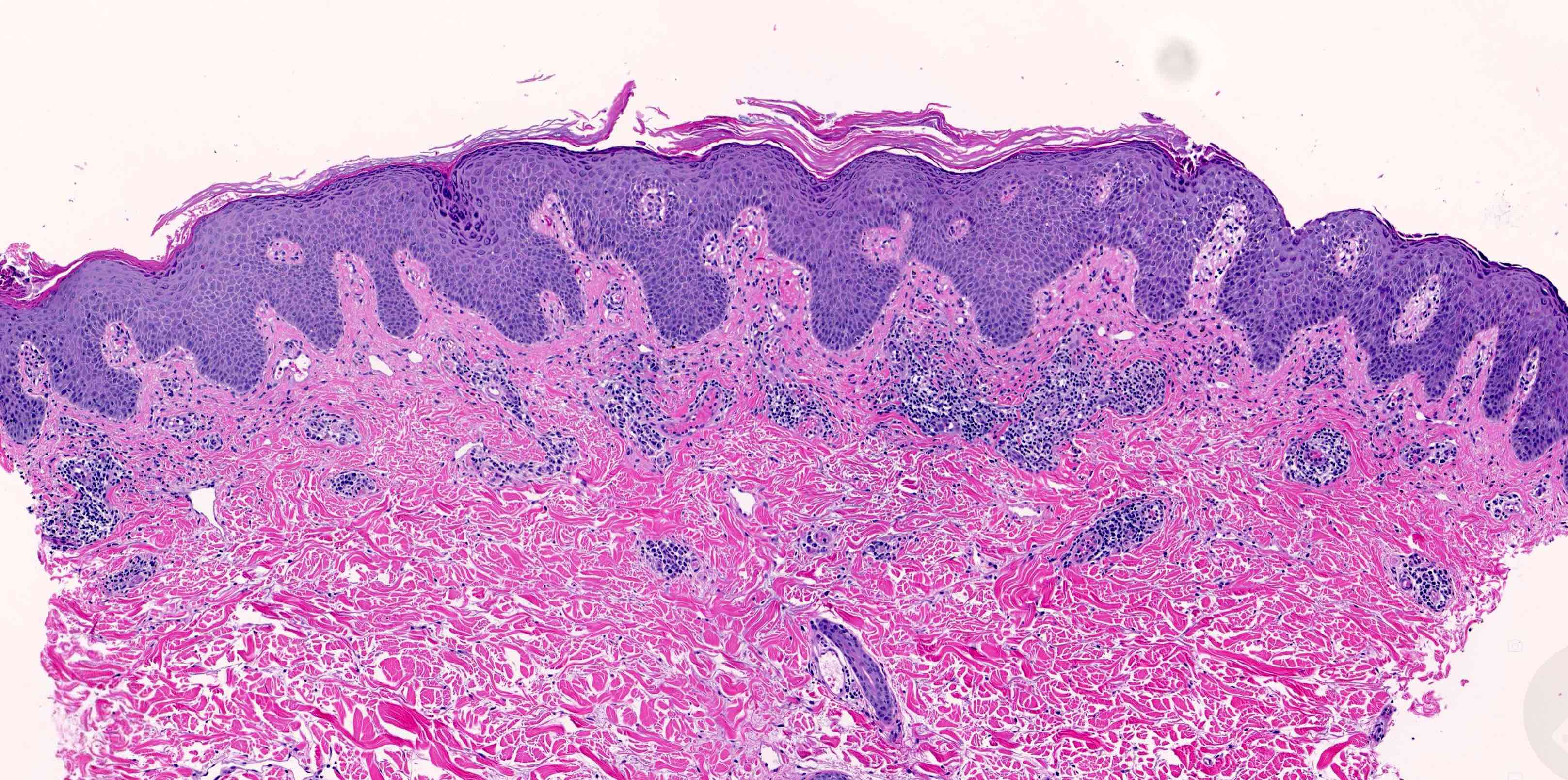
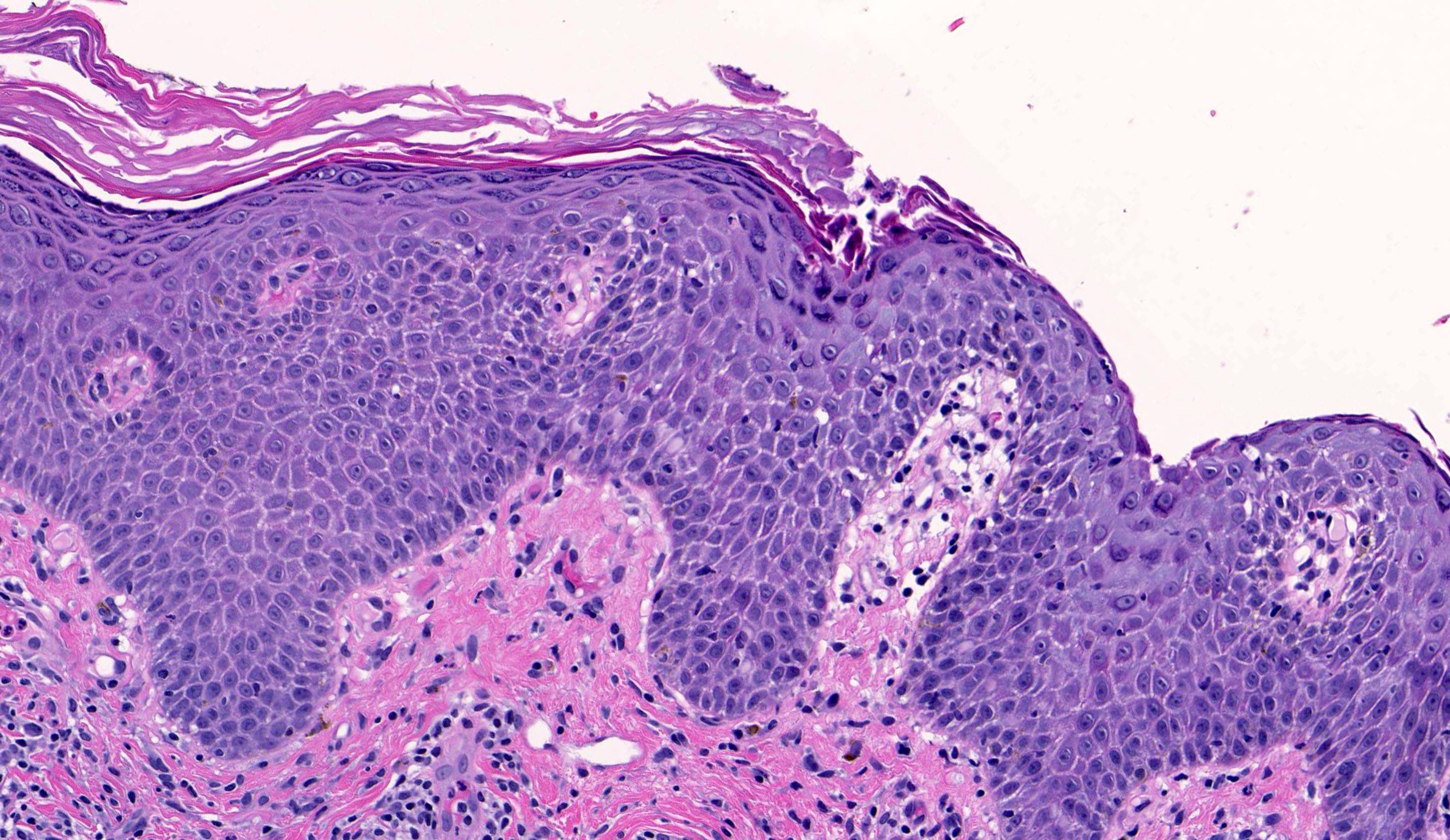
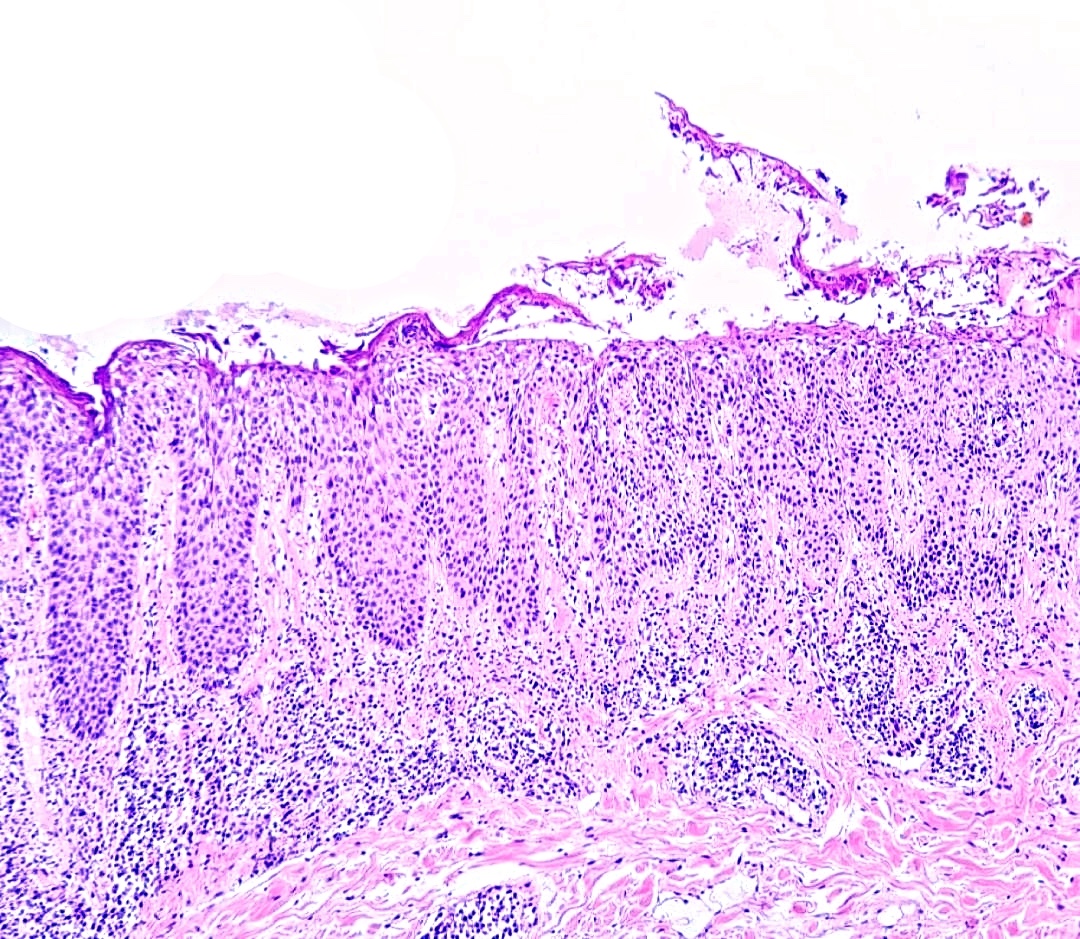
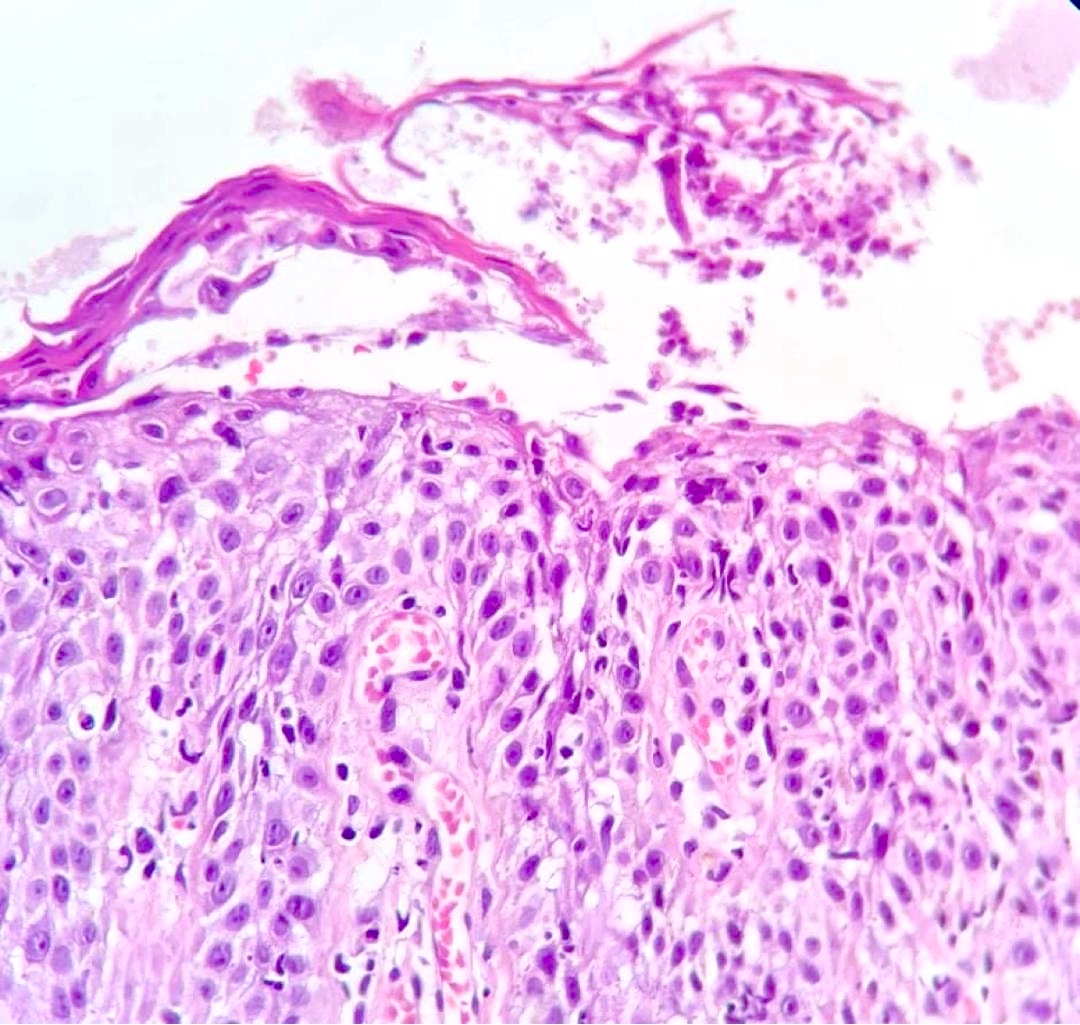
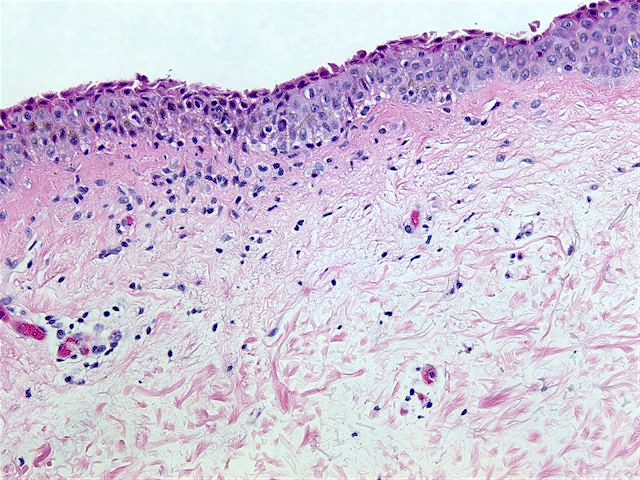
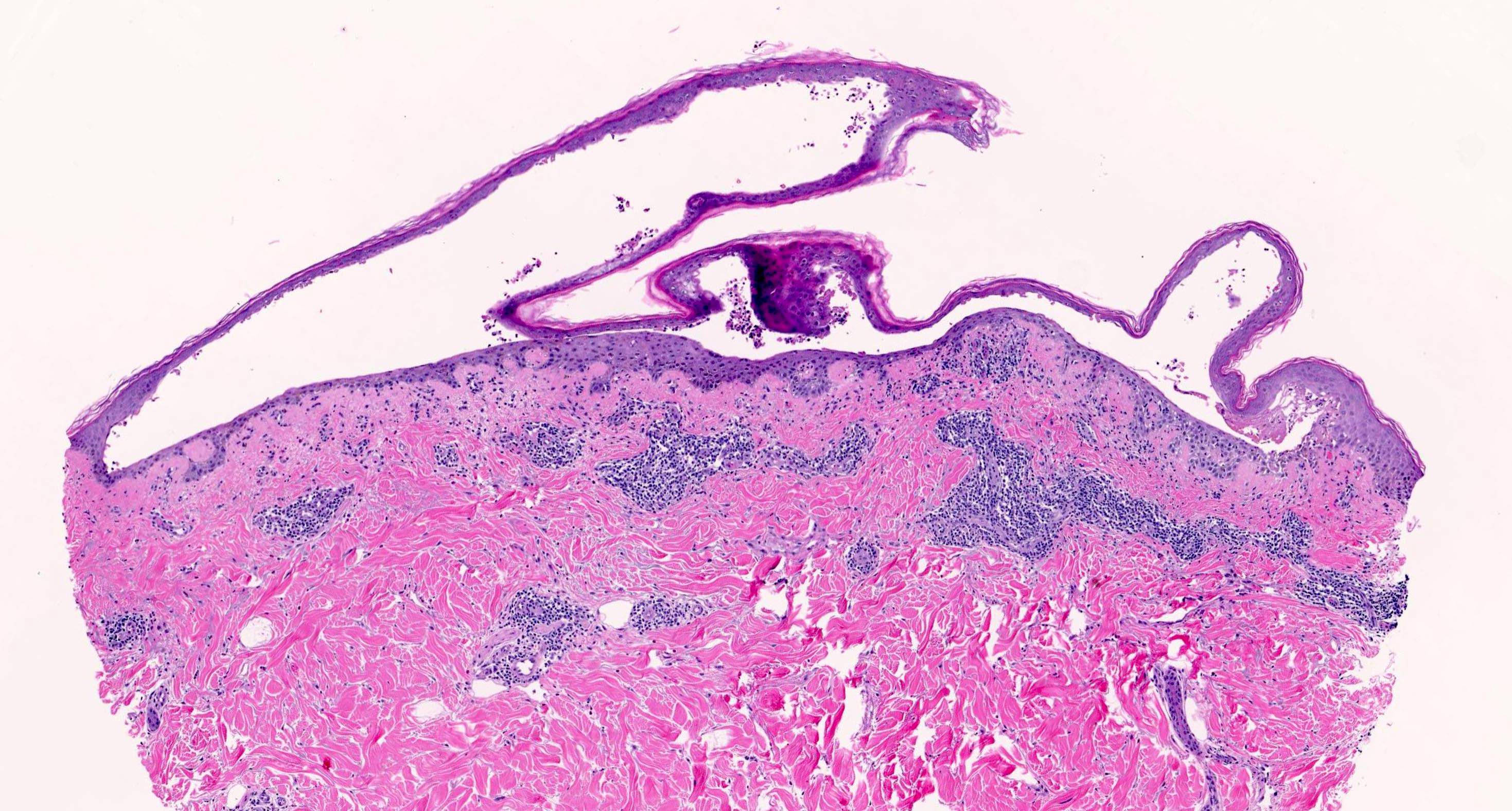
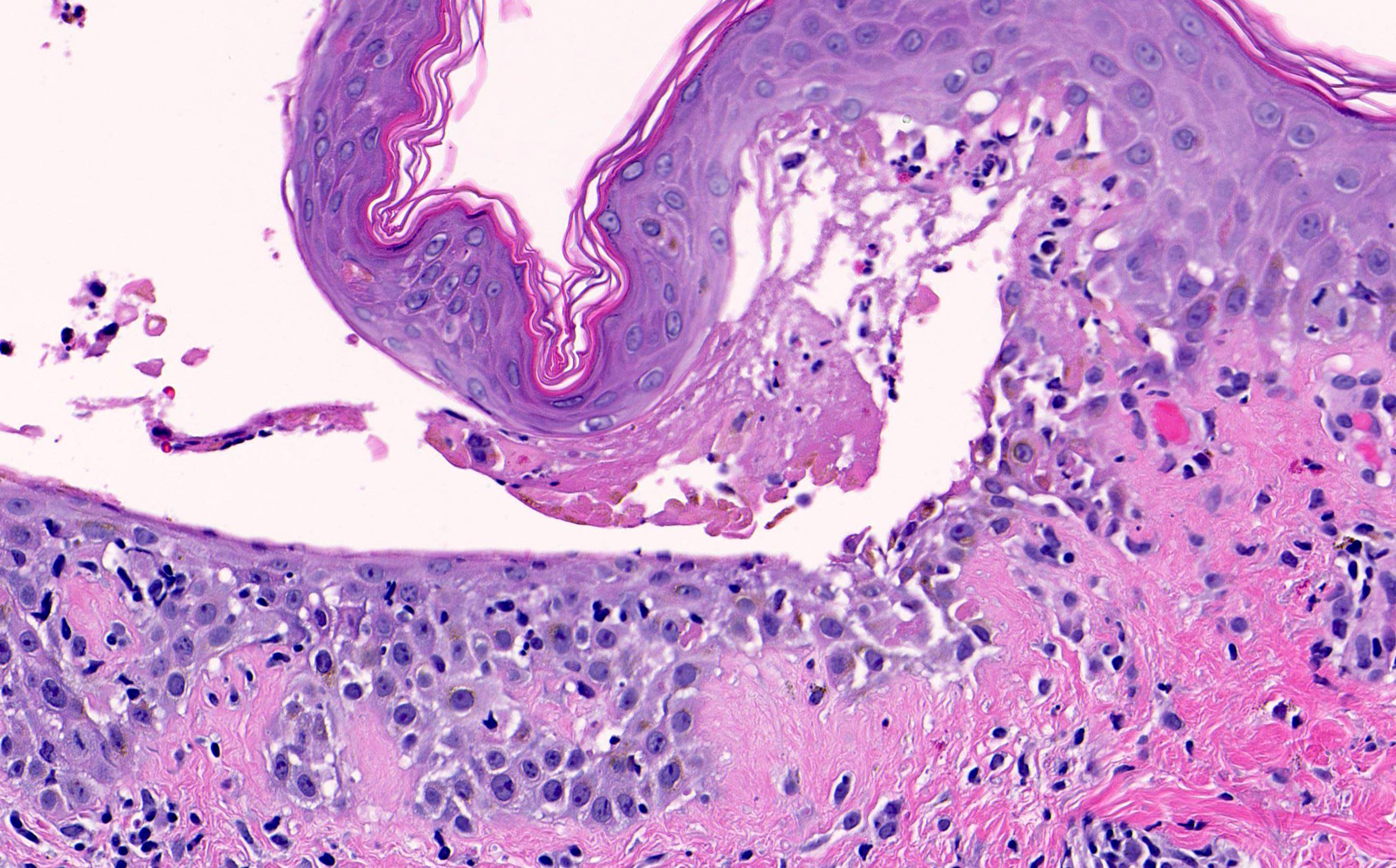
Microscopic (histologic) description
- Pemphigus vulgaris:
- Suprabasal acantholysis
- Basal layer remains attached (tombstone sign)
- Intraepidermal vesicles with round acantholytic keratinocytes
- Intraepidermal eosinophils and sometimes neutrophils
- Follicular involvement
- No significant dyskeratosis
- Miniaturization of the sebaceous glands in the scalp lesions (also seen in pemphigus foliaceus) (J Cutan Pathol 2017;44:835)
- Pemphigus vegetans:
- Subtle suprabasal acantholysis
- Hyperplastic epithelium, pseudoepitheliomatous hyperplasia
- Intraepidermal eosinophils, microabscesses
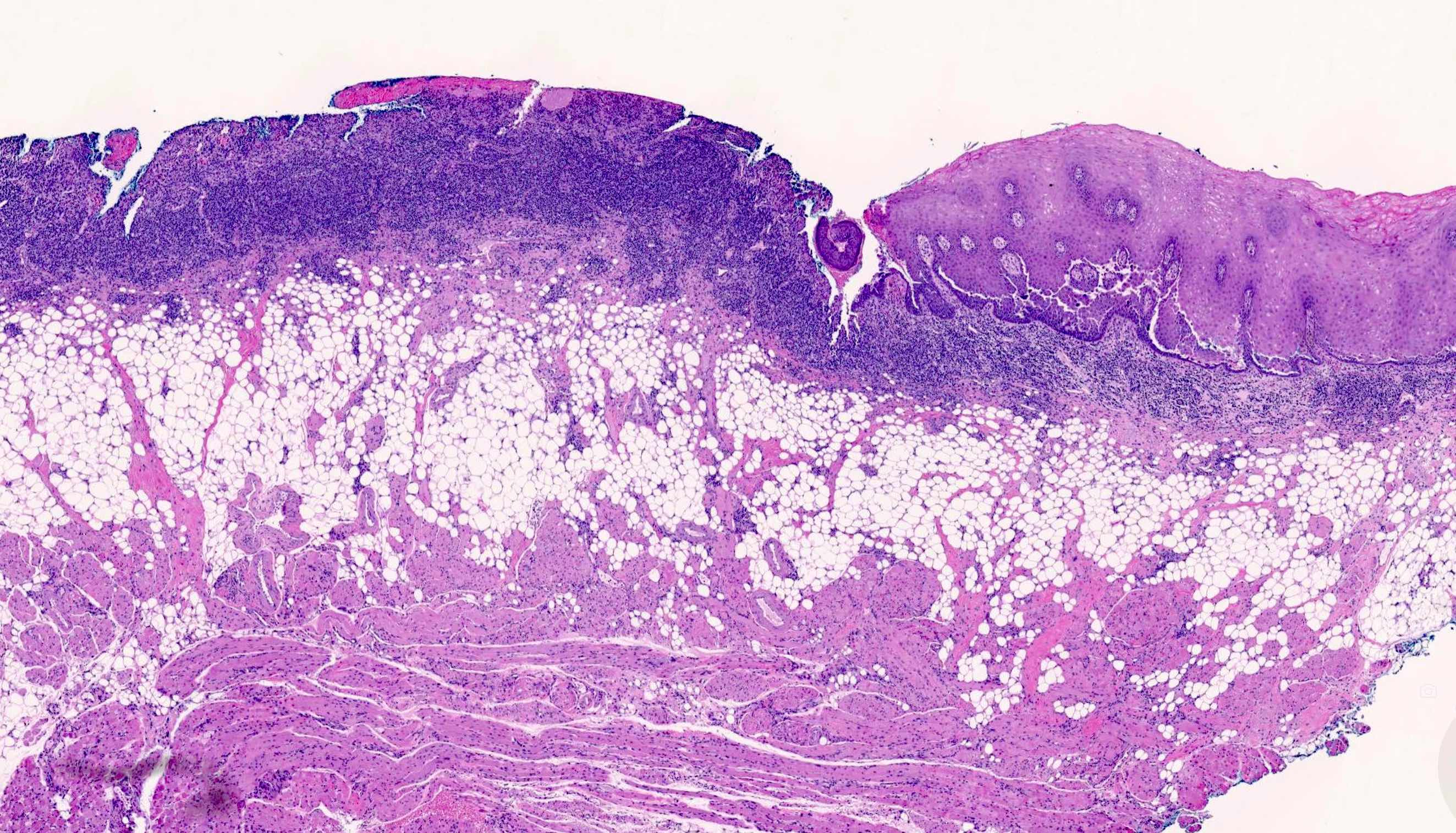
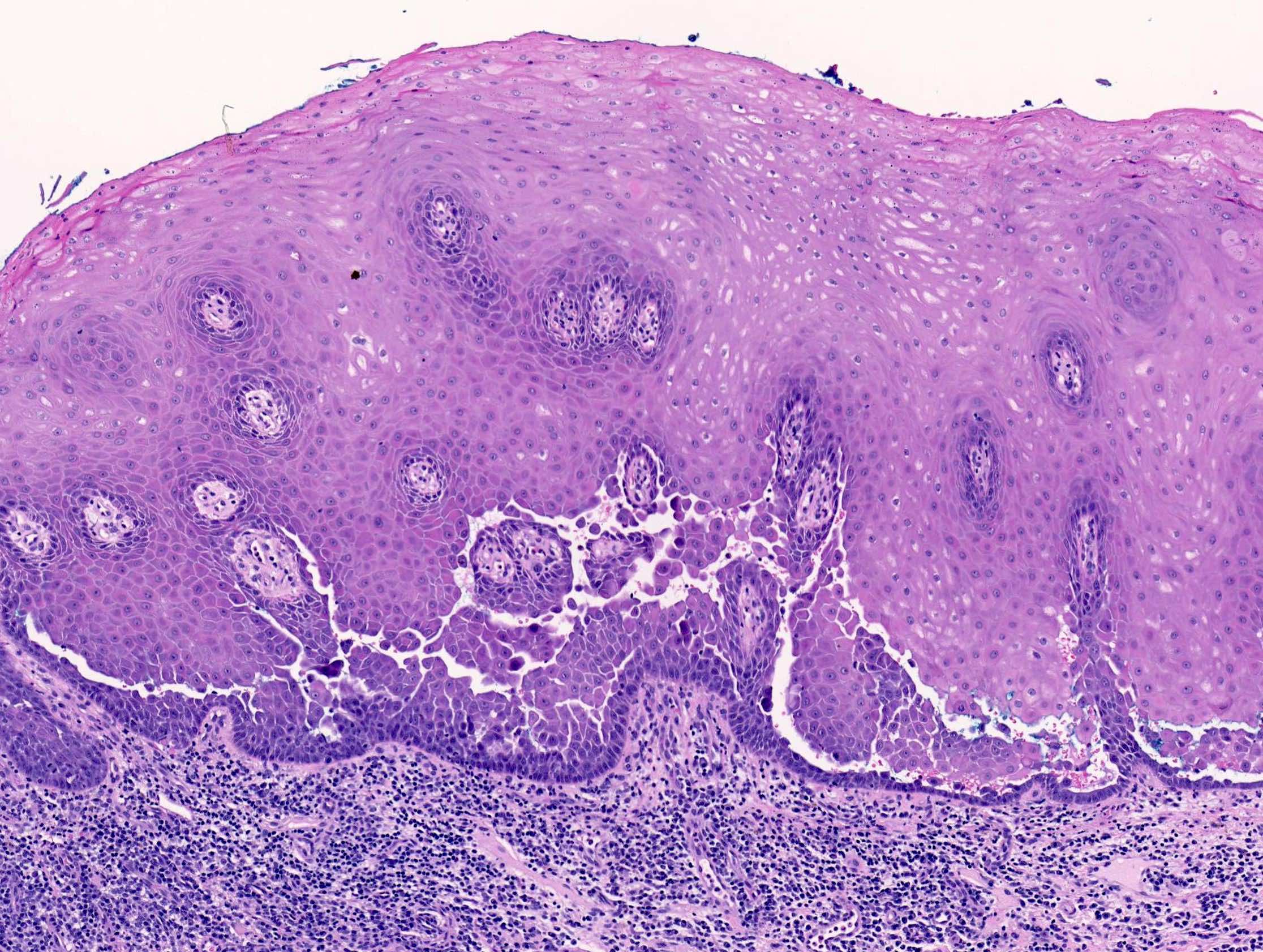
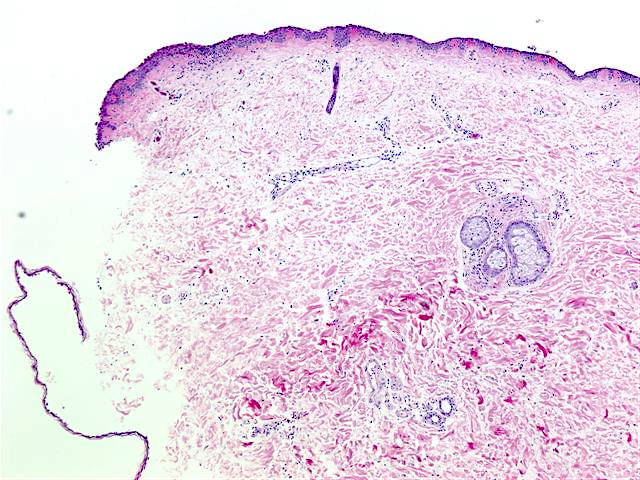
- Pemphigus foliaceus, endemic pemphigus foliaceus, pemphigus erythematosus:
- Subcorneal acantholysis; minority of cases may have acantholysis in the lower layers of the epidermis (J Cutan Pathol 2014;41:880)
- Rarely intact blisters
- Detached stratum corneum may show granular keratinocytes as cling ons
- Neutrophilic exocytosis
- Intraepidermal eosinophils
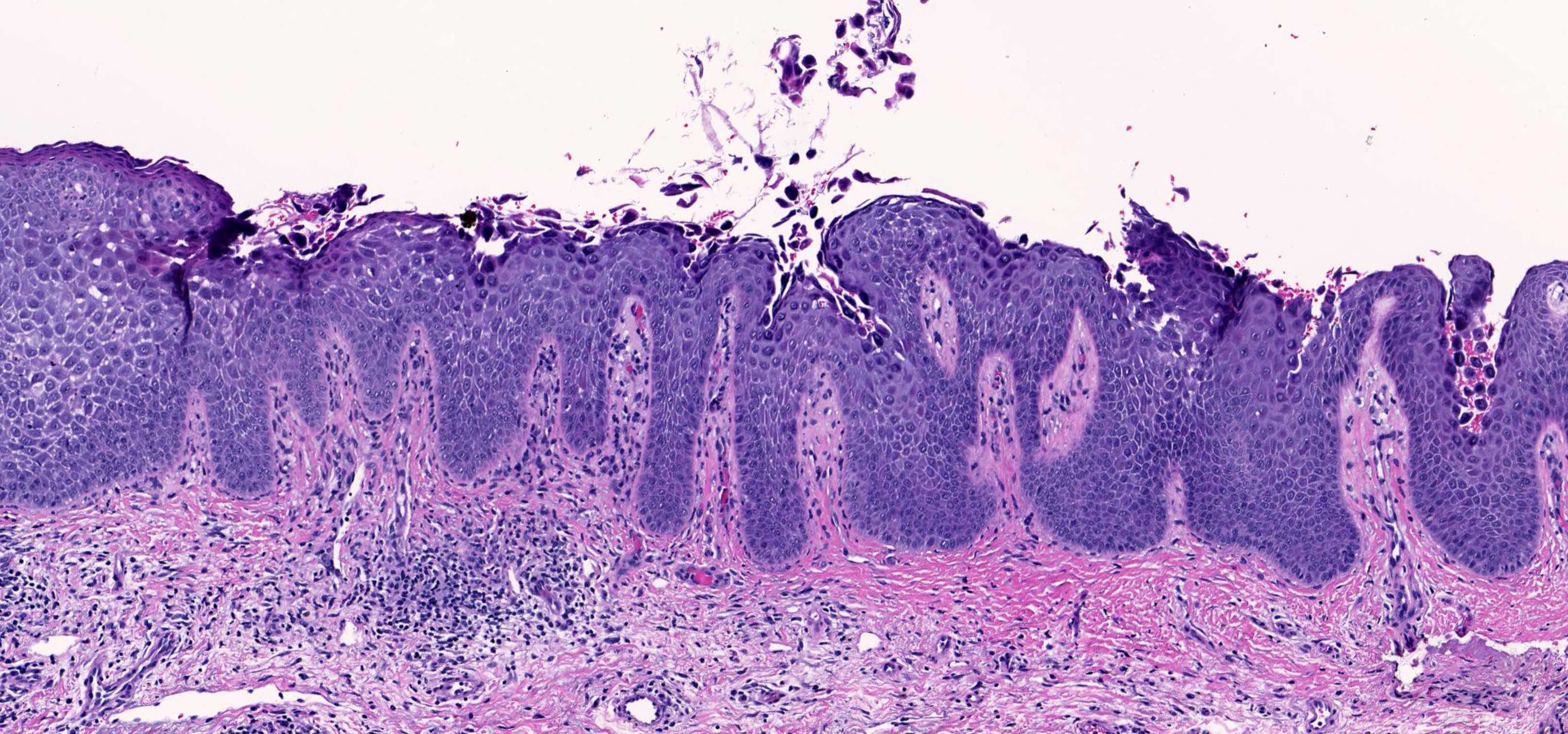
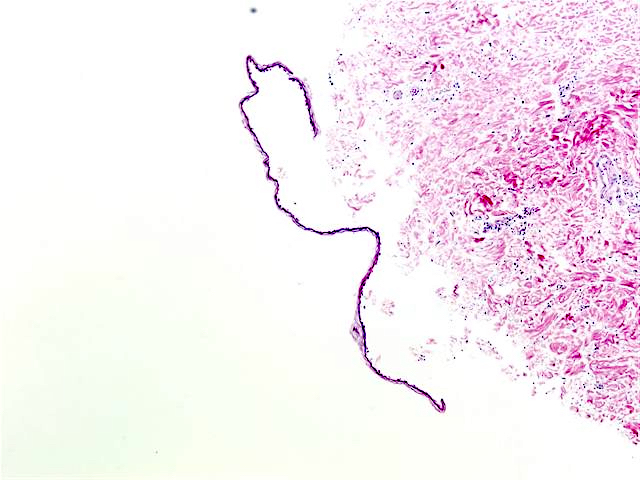
- Paraneoplastic pemphigus:
- Variable
- Features of pemphigus vulgaris
- Lichenoid and vacuolar interface changes
- Dyskeratosis and spongiosis
- Rare eosinophils
- IgA pemphigus:
- Subcorneal pustules (subcorneal pustular dermatosis variant)
- All layer epidermal pustules (intraepidermal neutrophilic variant)
Microscopic (histologic) images
Contributed by Viktoryia Kazlouskaya, M.D., Ph.D., Juliana Jung, M.D. and Case #56
Pemphigus vulgaris:
Pemphigus foliaceus:
Paraneoplastic pemphigus:
Cytology description
- Rarely used but may be helpful as a quick tool or if other diagnostic resources are limited
- Tzanck smears from the erosions or blister bottom (Sci Rep 2020;10:18314)
- Acantholytic cells are larger round cells with large nucleus surrounded by clear halo and inconspicuous nucleoli
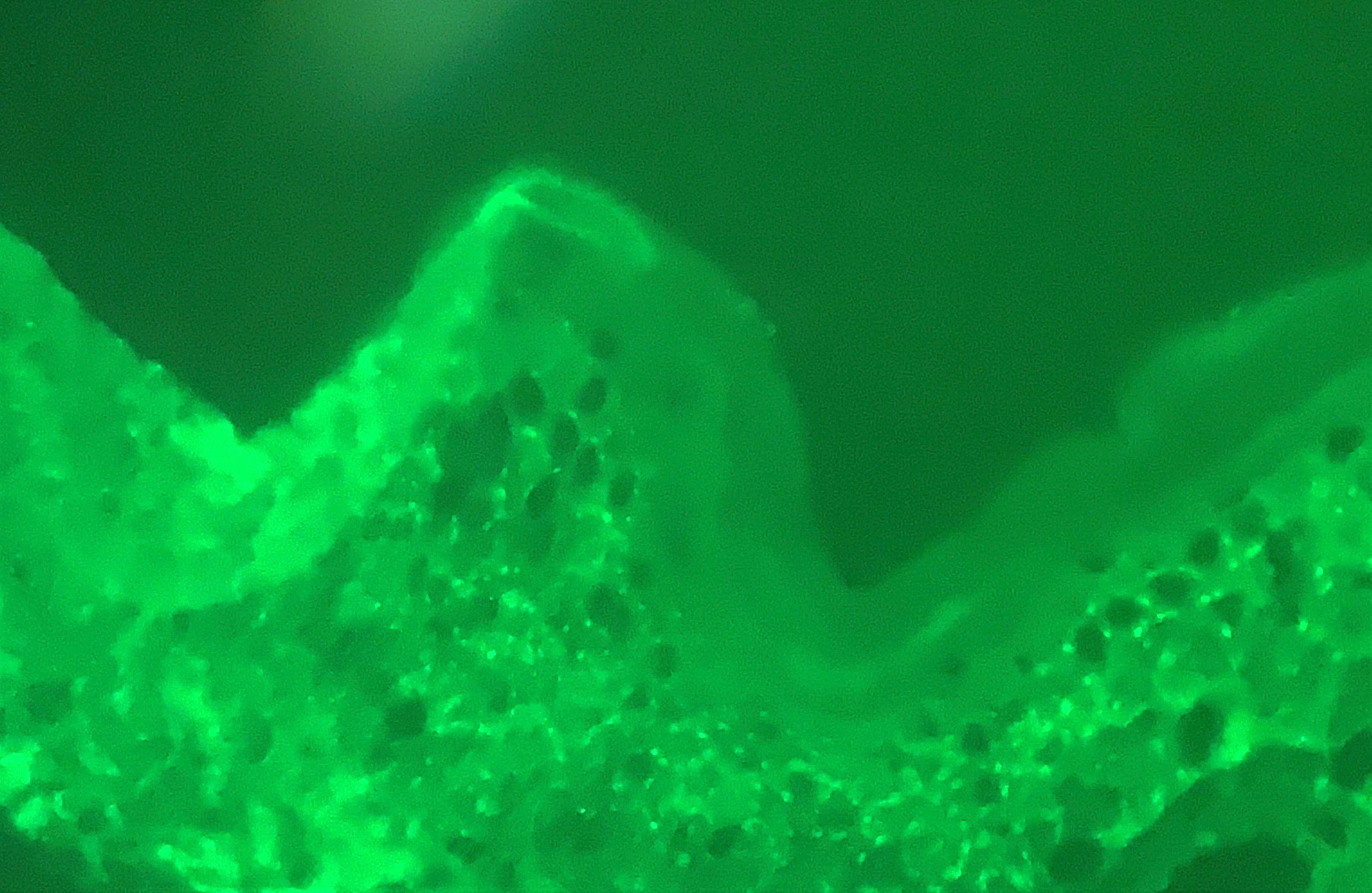
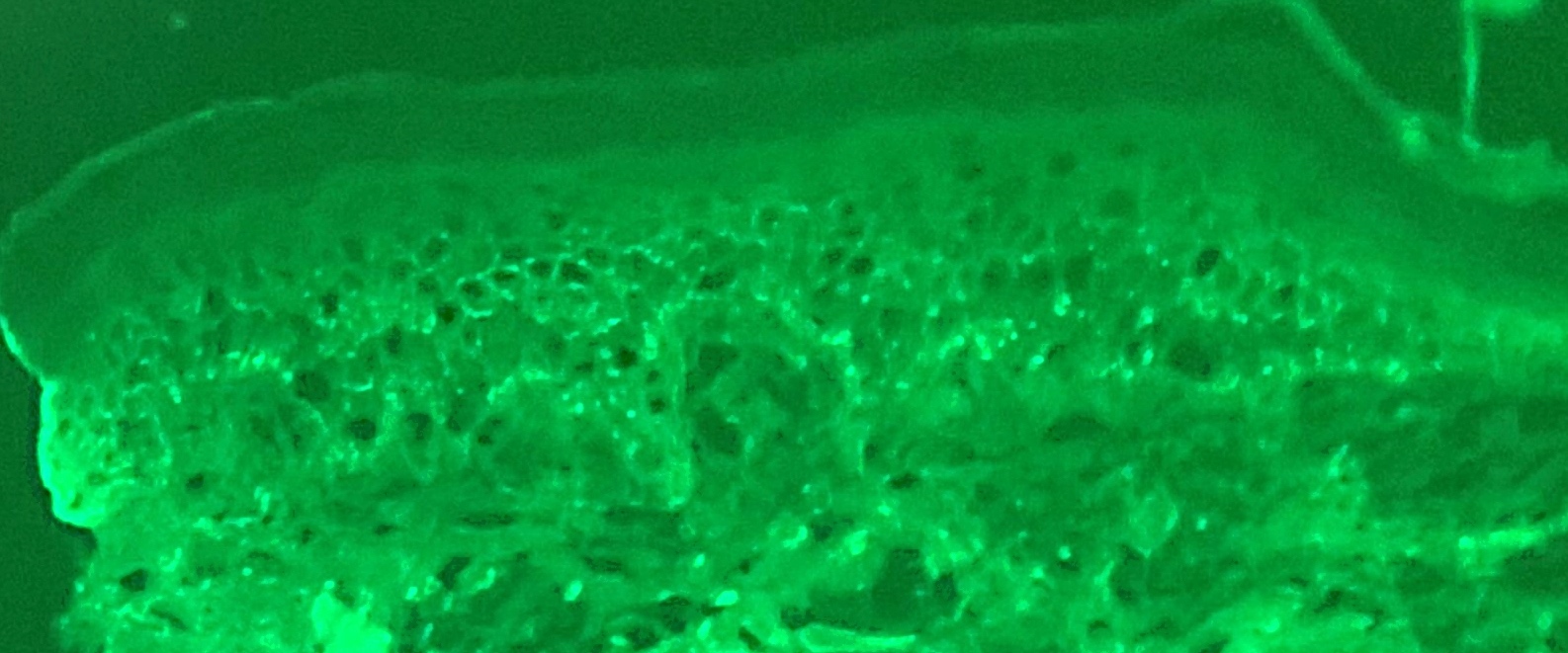
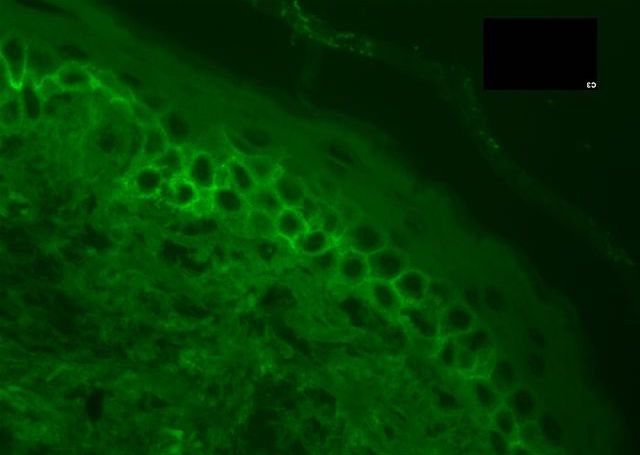
Immunofluorescence description
- Pemphigus vulgaris: intercellular IgG and C3 in the epidermis (chicken wire pattern) and adnexal epithelium (J Int Oral Health 2015;7:59)
- Pemphigus foliaceus: intercellular pattern, stronger fluorescence in the upper epidermis
- Paraneoplastic pemphigus: linear or granular IgG at dermal epidermal junction; in 50% of cases, intercellular deposition is also seen
- Pemphigus erythematosus: granular IgG at dermal epidermal junction
- IgA pemphigus: intercellular IgA in the upper epidermis (SPD variant) or lower epidermis (IEN variant)
Immunofluorescence images
Electron microscopy description
- Dilatation of intercellular space, stretched desmosomes, acantholytic cells
Sample pathology report
- Skin, punch biopsy:
- Intraepidermal acantholysis, suggestive of (or consistent with) pemphigus vulagaris (see comment)
- Comment: Examination of the specimen shows intraepidermal acanthosis in the lower portions of the epidermis and spongiosis with eosinophil and neutrophil exocytosis. There is a perivascular infiltrate with eosinophils in the dermis. Neither fungal microorganisms nor basement membrane changes are seen with interpretation of PAS histochemical stain.
- Skin, punch for immunofluorescence:
- Intercellular epidermal IgG and C3 deposition (see microscopic and comment)
- Comment: IgG and C3 immunofluorescence is seen throughout the epidermis with the intercellular pattern suggestive of pemphigus vulgaris but correlation with clinical findings is necessary.
- 5 immunofluorescence stains are scored subjectively on a scale from 0 - 3+
- Staining results:
- IgG: 2+, intercellular epidermal
- IgM: 0, negative
- IgA: 0, negative
- C3: 2+, intercellular epidermal
- Fibrin: 0, negative
Differential diagnosis
- Pemphigus vulgaris:
- Grover disease:
- Apparent dyskeratosis, focal acantholysis, follicular acantholysis is rare, usually a small lesion, negative immunofluorescence (J Cutan Pathol 2019;46:6)
- Clinically, itchy nonfollicular papules on the trunk of middle age and elderly patients
- Darier disease:
- Apparent dyskeratosis, epidermal hyperplasia, follicular acantholysis is rare, negative immunofluorescence
- Clinically, congenital, autosomal dominant, starts in adolescence, presents with crusted papules on the intertriginous areas and scalp
- Warty dyskeratoma:
- Verrucous epidermal hyperplasia, exoendophytic silhouette, apparent dyskeratosis, negative immunofluorescence
- Clinically, solitary nodule
- Hailey-Hailey disease:
- Psoriasiform hyperplasia, exuberant crust may be present, apparent dyskeratosis, follicular involvement is rare, acantholytic cells throughout the full thickness of the epidermis (brick wall look), negative immunofluorescence
- Grover disease:
- Pemphigus foliaceus:
- Bullous impetigo:
- Evidence of bacteria, negative immunofluorescence, more common in children, clinical presentation and history
- Staphylococcal scalded skin syndrome:
- May be indistinguishable with pemphigus foliaceus, clinical correlation is required
- Fungal infections:
- Positive fungal stain, negative immunofluorescence
- Bullous impetigo:
- Pemphigus vegetans:
- Pyostomatitis vegetans:
- Neutrophilic rather than eosinophilic abscesses
- Infections:
- Positive fungal, bacterial stains, negative immunofluorescence
- Pyostomatitis vegetans:
- Paraneoplastic pemphigus:
- Lichenoid conditions (mainly erythema multiforme, lichenoid drug eruptions):
- Focal areas may be indistinguishable, usually no acantholysis, negative immunofluorescence
- Lichenoid conditions (mainly erythema multiforme, lichenoid drug eruptions):
- IgA pemphigus:
- Sneddon-Wilkinson disease:
- May be indistinguishable, negative immunofluorescence
- Sneddon-Wilkinson disease:
Board review style question #1
What are the expected histopathological features of the condition in the above image?
- Acantholytic dyskeratotic cells and parakeratotic columns with negative direct immunofluorescence
- Dilapidated brick wall appearance with negative direct immunofluorescence
- Focal acantholysis with various pattern and negative direct immunofluorescence
- Intraepidermal acantholysis with chicken wire pattern IgG on direct immunofluorescence
Board review style answer #1
D. Intraepidermal acantholysis with chicken wire pattern IgG on direct immunofluorescence
The image demonstrates crusted erosions and bullae on the scalp and chest and is consistent with pemphigus vulgaris. Histopathological features of pemphigus vulgaris include intraepidermal acantholysis and chicken wire pattern IgG on direct immunofluorescence. Answer A is incorrect because acantholytic, dyskeratotic cells and parakeratotic columns are seen in Darier disease, which typically presents as keratotic plaques and papules. Answer B is incorrect because dilapidated brick wall appearance is seen in Hailey-Hailey disease, which typically presents in intertriginous areas. Answer C is incorrect because focal acantholysis with various patterns is seen in Grover disease, which typically presents as small papules on the chest.
Comment Here
Reference: Pemphigus
The image demonstrates crusted erosions and bullae on the scalp and chest and is consistent with pemphigus vulgaris. Histopathological features of pemphigus vulgaris include intraepidermal acantholysis and chicken wire pattern IgG on direct immunofluorescence. Answer A is incorrect because acantholytic, dyskeratotic cells and parakeratotic columns are seen in Darier disease, which typically presents as keratotic plaques and papules. Answer B is incorrect because dilapidated brick wall appearance is seen in Hailey-Hailey disease, which typically presents in intertriginous areas. Answer C is incorrect because focal acantholysis with various patterns is seen in Grover disease, which typically presents as small papules on the chest.
Comment Here
Reference: Pemphigus
Board review style question #2
A patient presents with oral, ocular and polymorphous skin lesions. Biopsy shows suprabasal acantholysis and lichenoid changes. What is the most likely underlying etiology?
- B cell lymphoproliferative disorders
- Contact allergen
- Idiopathic autoantibody
- Thiol drug
- Viral infection
Board review style answer #2
A. B cell lymphoproliferative disorders
Suprabasal acantholysis with lichenoid changes and oral and conjunctival involvement is characteristic of paraneoplastic pemphigus, with B cell lymphoproliferative disorders as the most common underlying cause. Answer B is incorrect because contact allergic pemphigus has been reported with histopathology analogous to pemphigus vulgaris but not paraneoplastic pemphigus. Answer C is incorrect because idiopathic autoantibody is consistent with primary pemphigus variants. Answer D is incorrect because thiol drug is reported to cause drug induced pemphigus. Answer E is incorrect because viral infection has not been linked with paraneoplastic pemphigus-like lesions.
Comment Here
Reference: Pemphigus
Suprabasal acantholysis with lichenoid changes and oral and conjunctival involvement is characteristic of paraneoplastic pemphigus, with B cell lymphoproliferative disorders as the most common underlying cause. Answer B is incorrect because contact allergic pemphigus has been reported with histopathology analogous to pemphigus vulgaris but not paraneoplastic pemphigus. Answer C is incorrect because idiopathic autoantibody is consistent with primary pemphigus variants. Answer D is incorrect because thiol drug is reported to cause drug induced pemphigus. Answer E is incorrect because viral infection has not been linked with paraneoplastic pemphigus-like lesions.
Comment Here
Reference: Pemphigus
Board review style question #3
Which of the following is true regarding pemphigus foliaceus?
- Caused by desmoglein 3 autoantibody
- Has worse prognosis than pemphigus vulgaris in general
- Involves the lower half of the epidermis
- More prevalent than pemphigus vulgaris in general
- Rarely affects mucosa
Board review style answer #3
E. Rarely affects mucosa
The mucosa expresses less desmoglein 1 compared with desmoglein 3 and is typically spared in pemphigus foliaceus. Answers A and C are incorrect because pemphigus foliaceus characteristically demonstrates desmoglein 1 autoantibodies and affects the superficial epidermis of the skin. Answers B and D are incorrect because pemphigus foliaceus is generally less common than pemphigus vulgaris and has a better prognosis.
Comment Here
Reference: Pemphigus
The mucosa expresses less desmoglein 1 compared with desmoglein 3 and is typically spared in pemphigus foliaceus. Answers A and C are incorrect because pemphigus foliaceus characteristically demonstrates desmoglein 1 autoantibodies and affects the superficial epidermis of the skin. Answers B and D are incorrect because pemphigus foliaceus is generally less common than pemphigus vulgaris and has a better prognosis.
Comment Here
Reference: Pemphigus