Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gonzalez RS. Low grade myofibroblastic sarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuelowgradmyofibroblasticsarcoma.html. Accessed May 14th, 2024.
Definition / general
- Rare tumor composed predominantly of malignant myofibroblasts
Essential features
- Deep intramuscular tumor of head and neck (tongue and oral cavity) and extremities (1.5 - 17 cm), rarely abdominopelvic (J Clin Pathol 2008;61:301)
- Commonly recurs, only rarely metastasizes; recurrences may be higher grade
- No corresponding high grade myofibroblastic sarcoma; such a tumor would fit under the designation of undifferentiated pleomorphic sarcoma
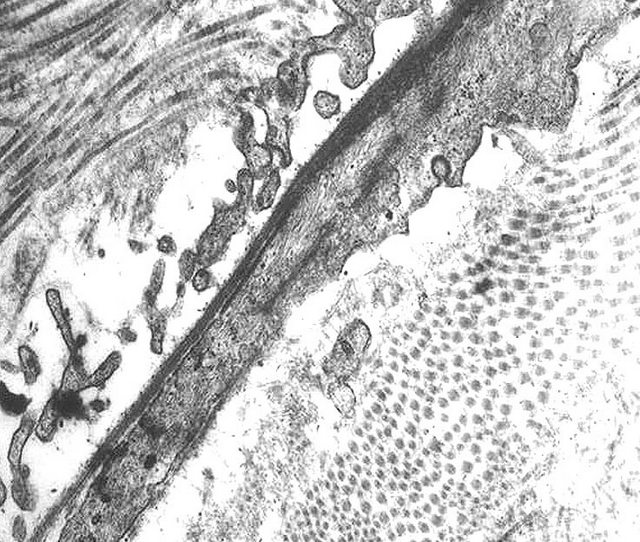
- No uniformly accepted criteria for diagnosis; some authors suggest electron microscopy appearance is the gold standard (Int J Surg Pathol 2013;21:29)
Terminology
- Also called myofibrosarcoma
Epidemiology
- Any age but predominantly patients in their 30s or 40s; slight male predominance
Case reports
- 49 year old woman with laryngeal mass (Case #310)
Treatment
- Complete excision
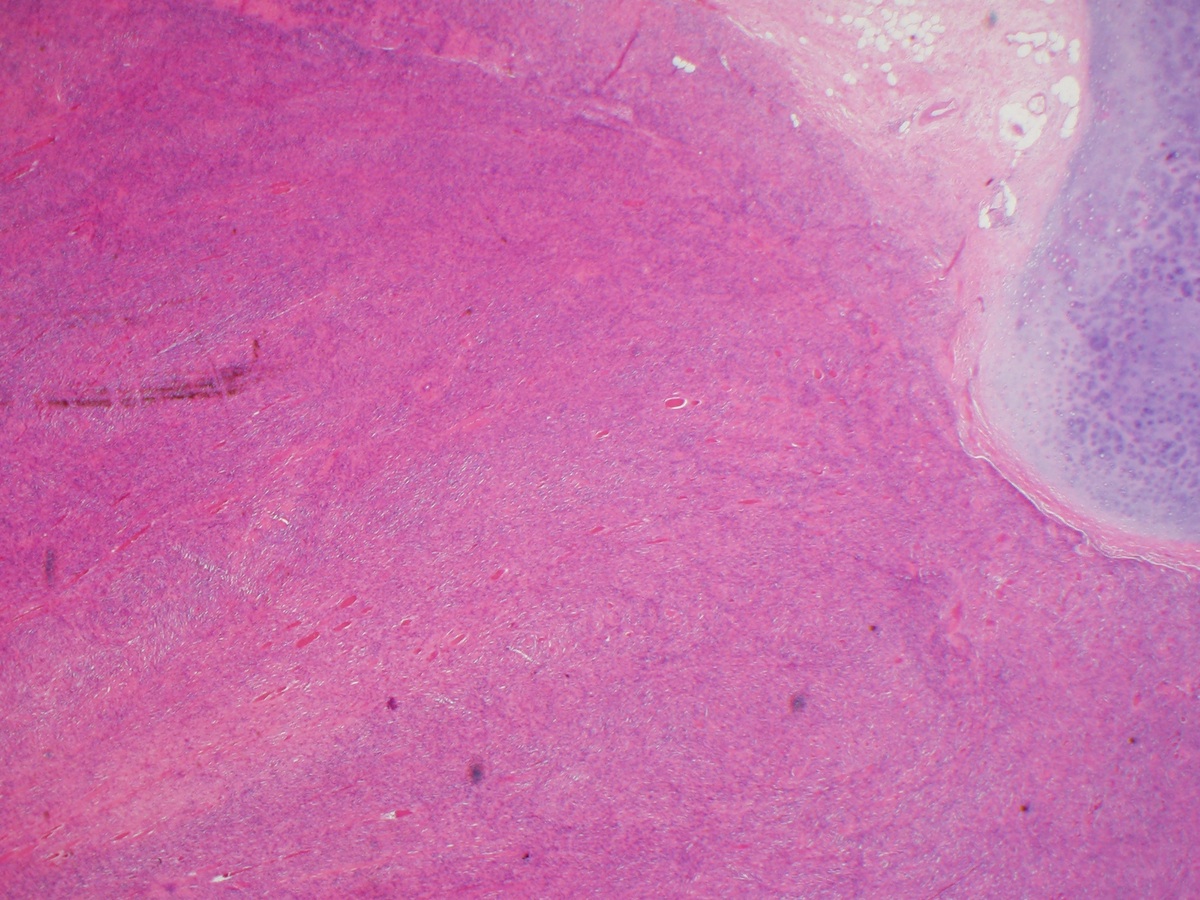
Gross description
- Firm, pale, fibrous cut surface, ill defined margins
Microscopic (histologic) description
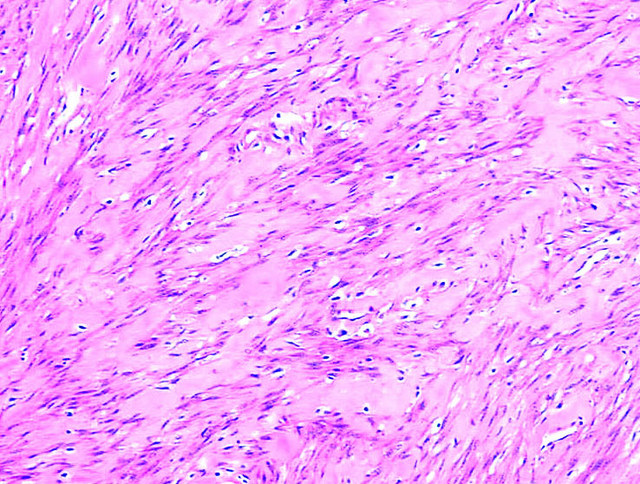
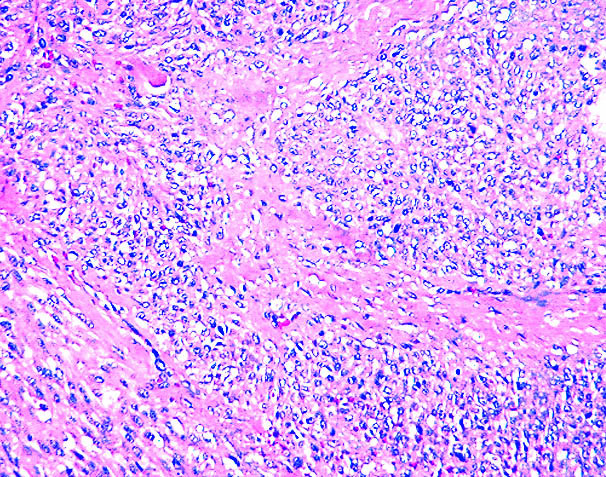
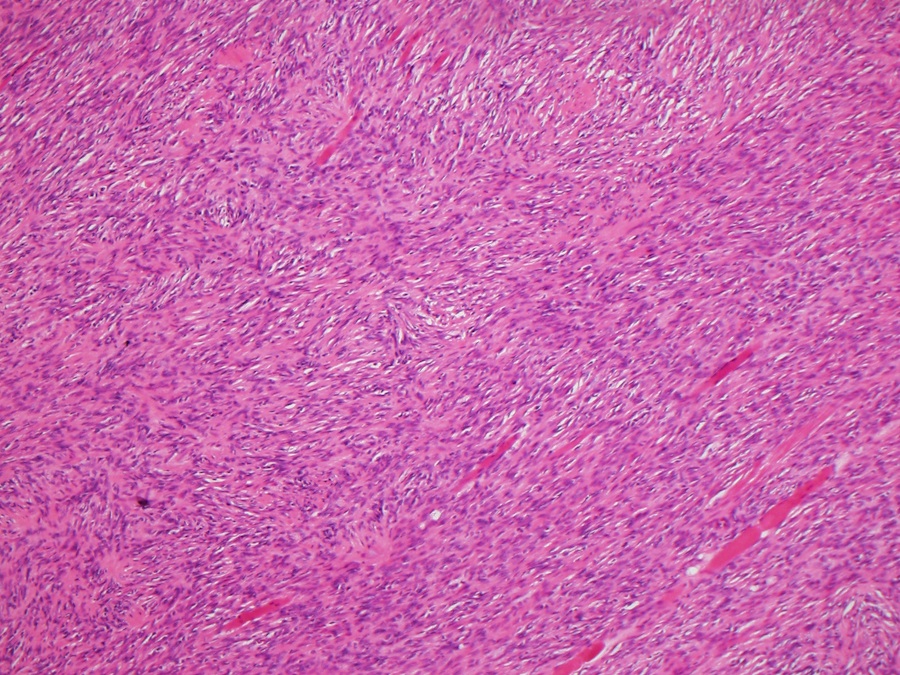
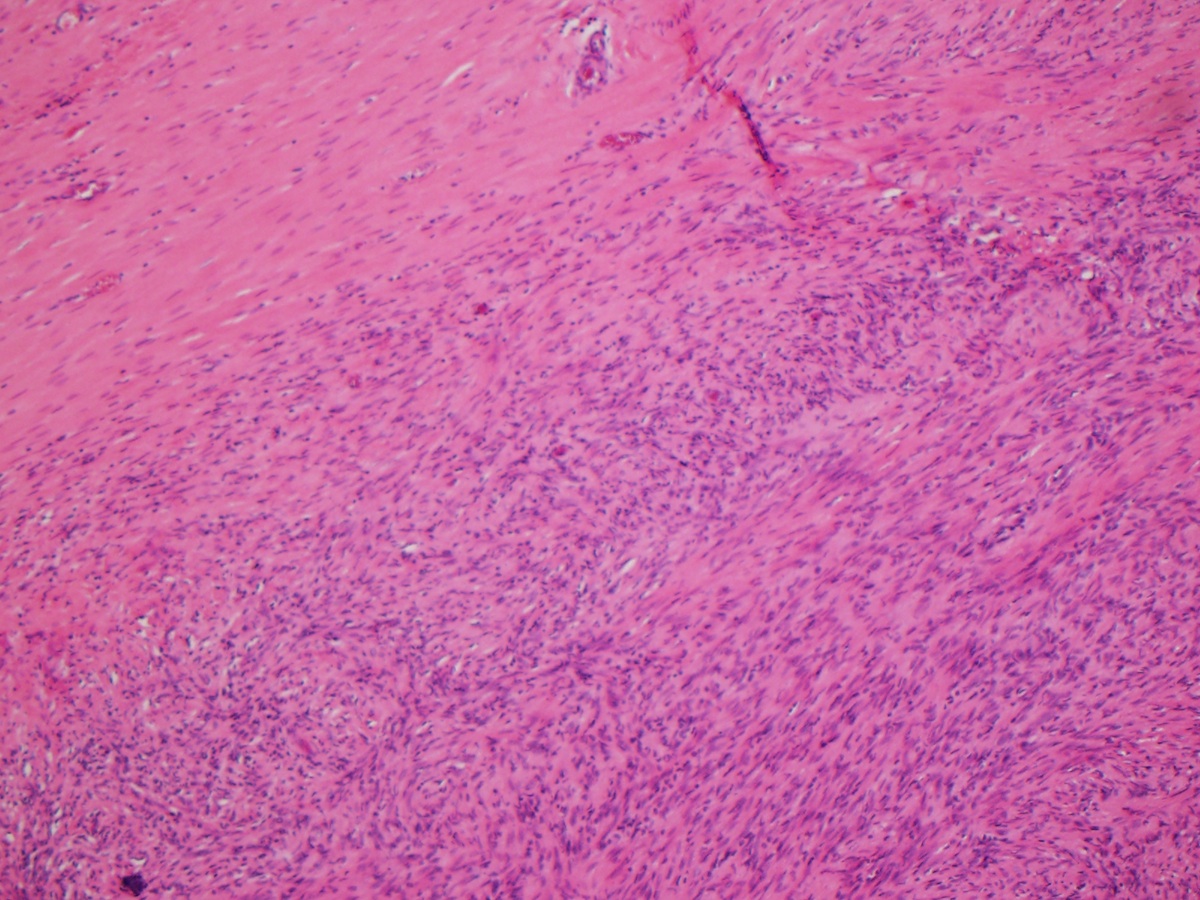
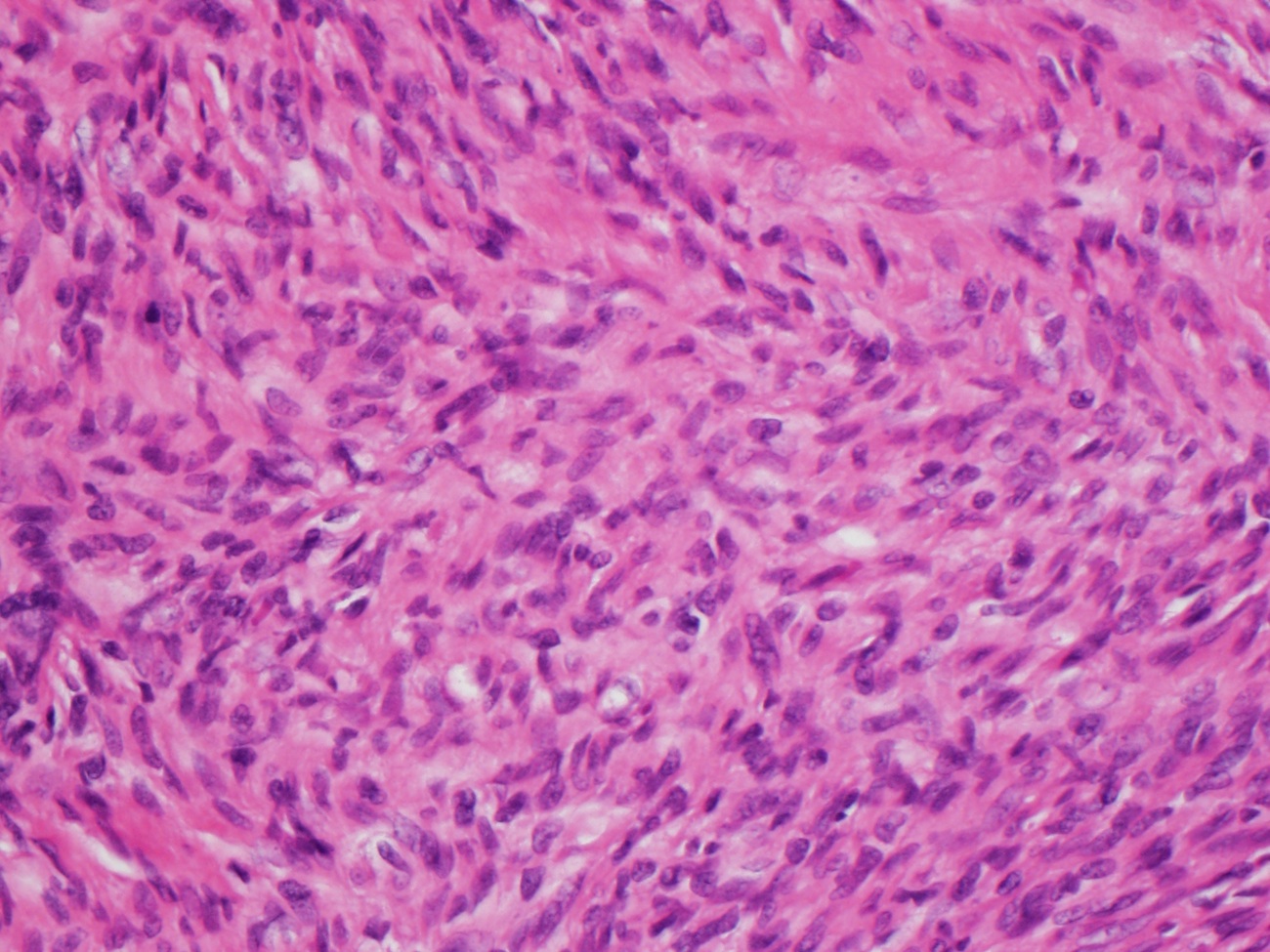
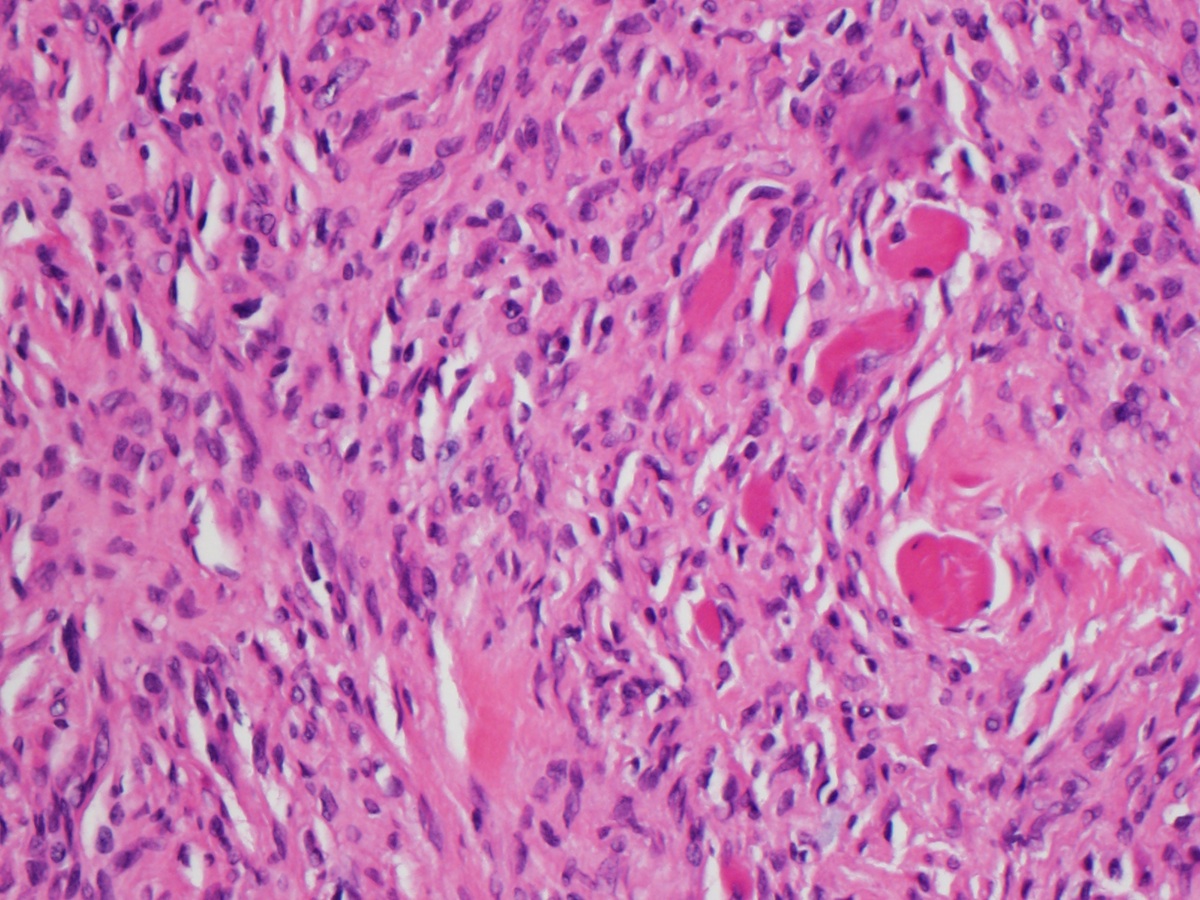
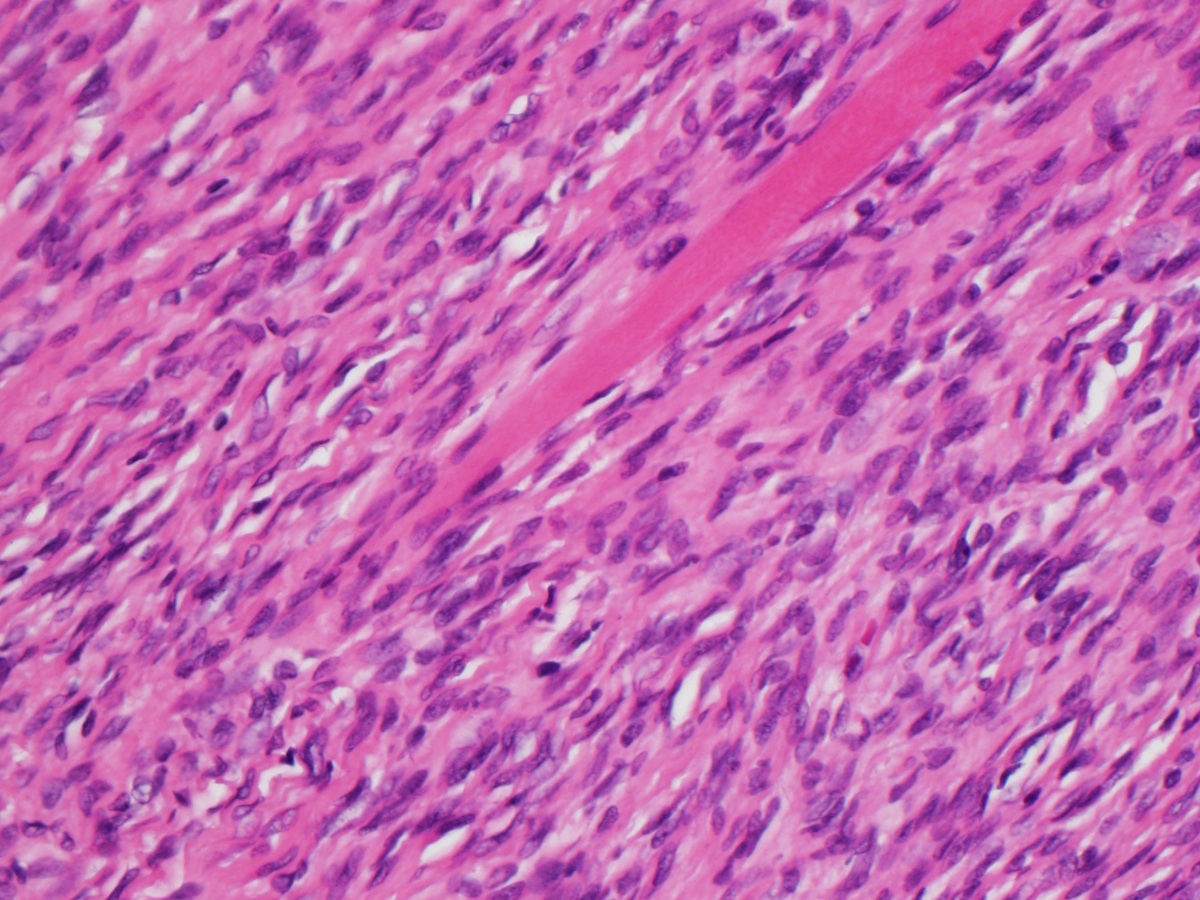
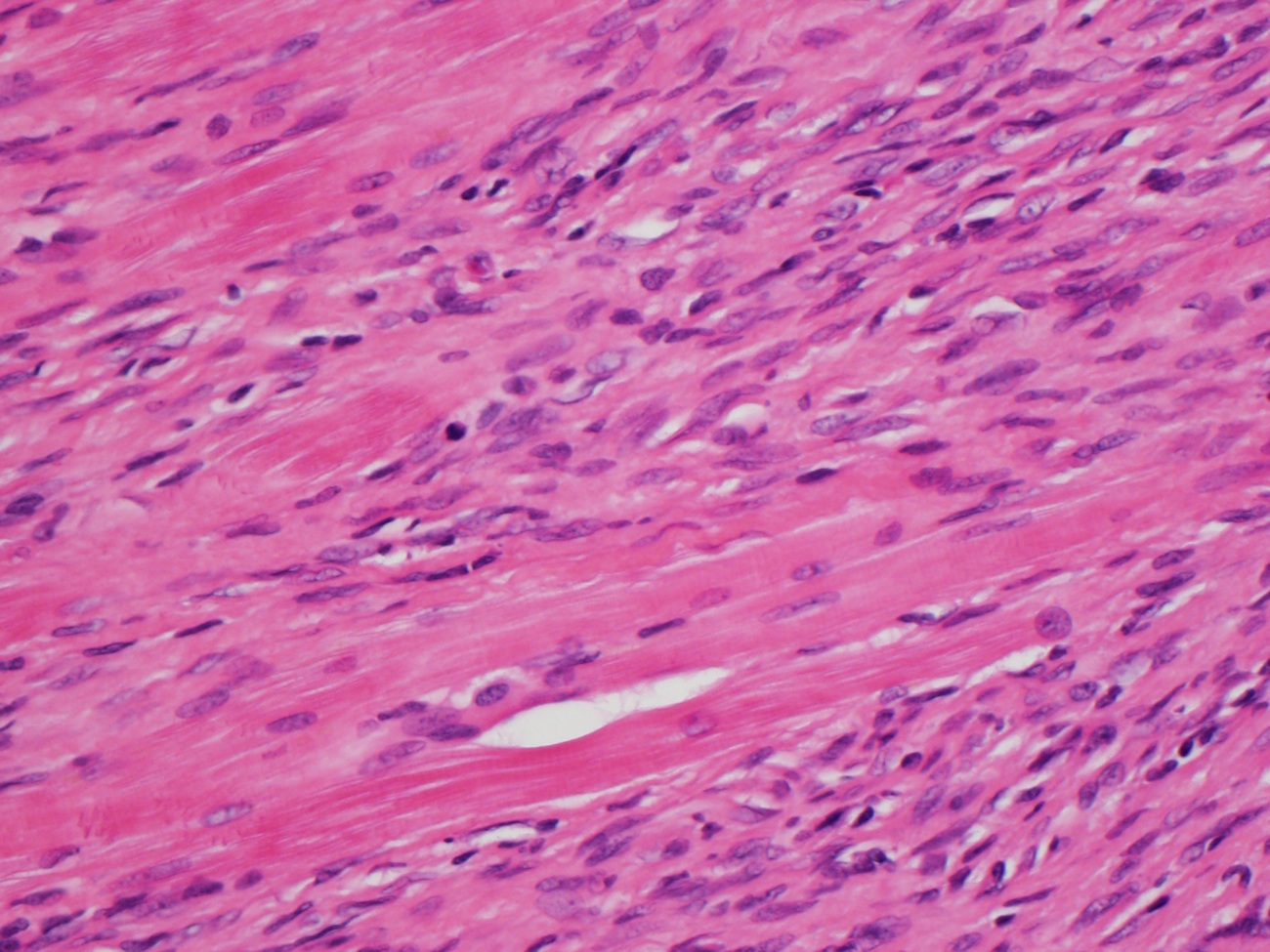
- Circumscribed to diffusely infiltrative with fascicles or storiform growth of spindled tumor cells
- Cells have ill defined pale eosinophilic cytoplasm, fusiform nuclei that are elongated or wavy with evenly distributed chromatin or round and vesicular with indentations and small nucleoli
- At least focal moderate nuclear atypia with hyperchromasia and irregular nuclear membranes
- Collagenous matrix with prominent hyalinization
- May have numerous thin walled capillaries
- 1 - 6 mitoses/10 high power fields
- No histiocytic giant cells or prominent inflammation
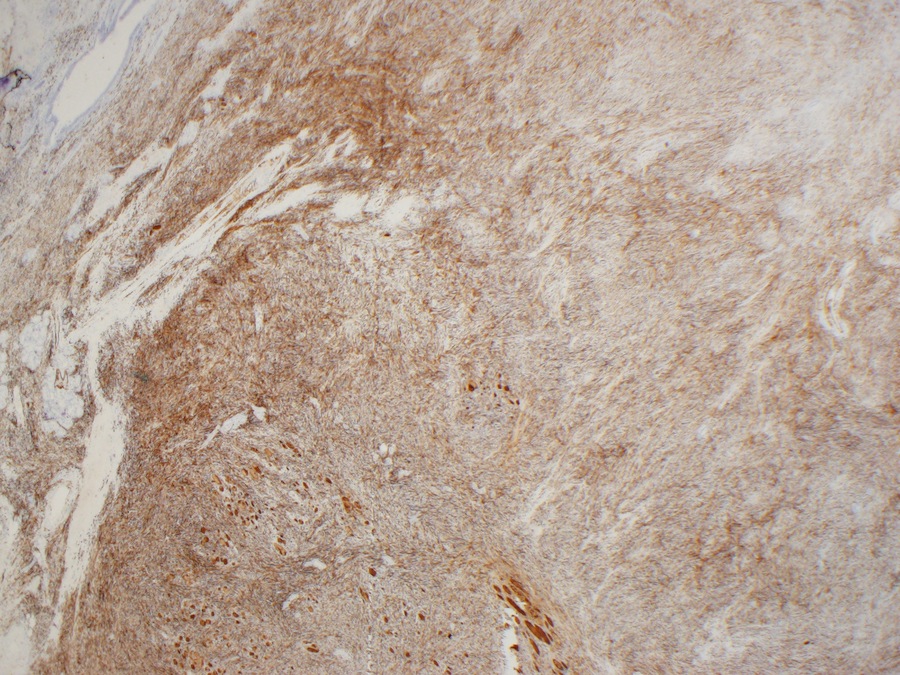
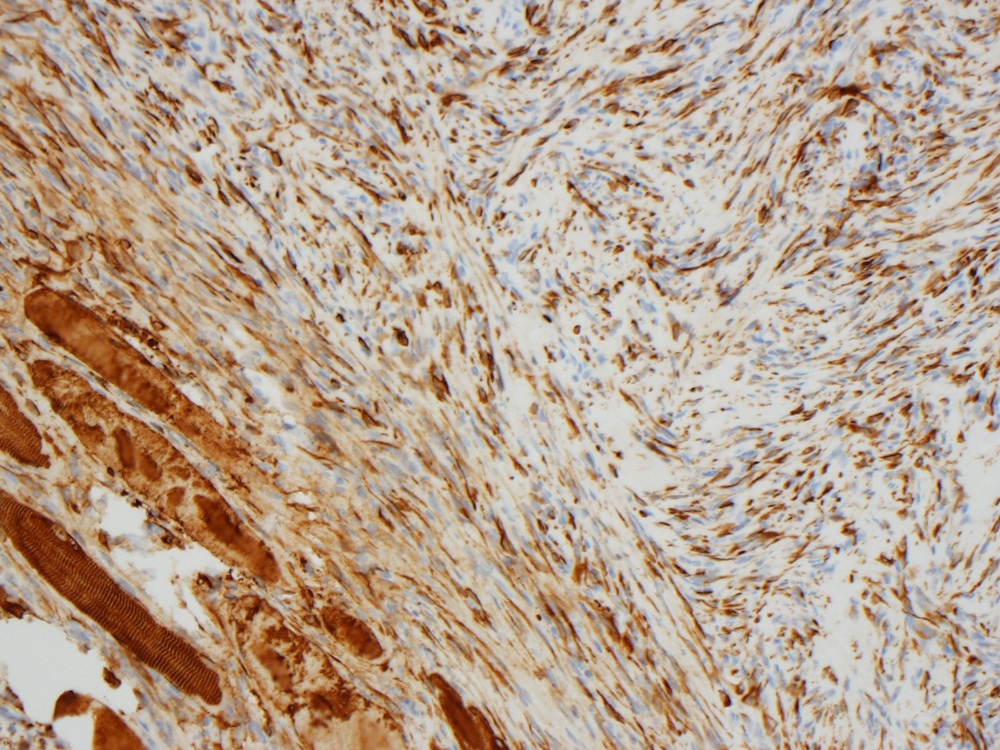
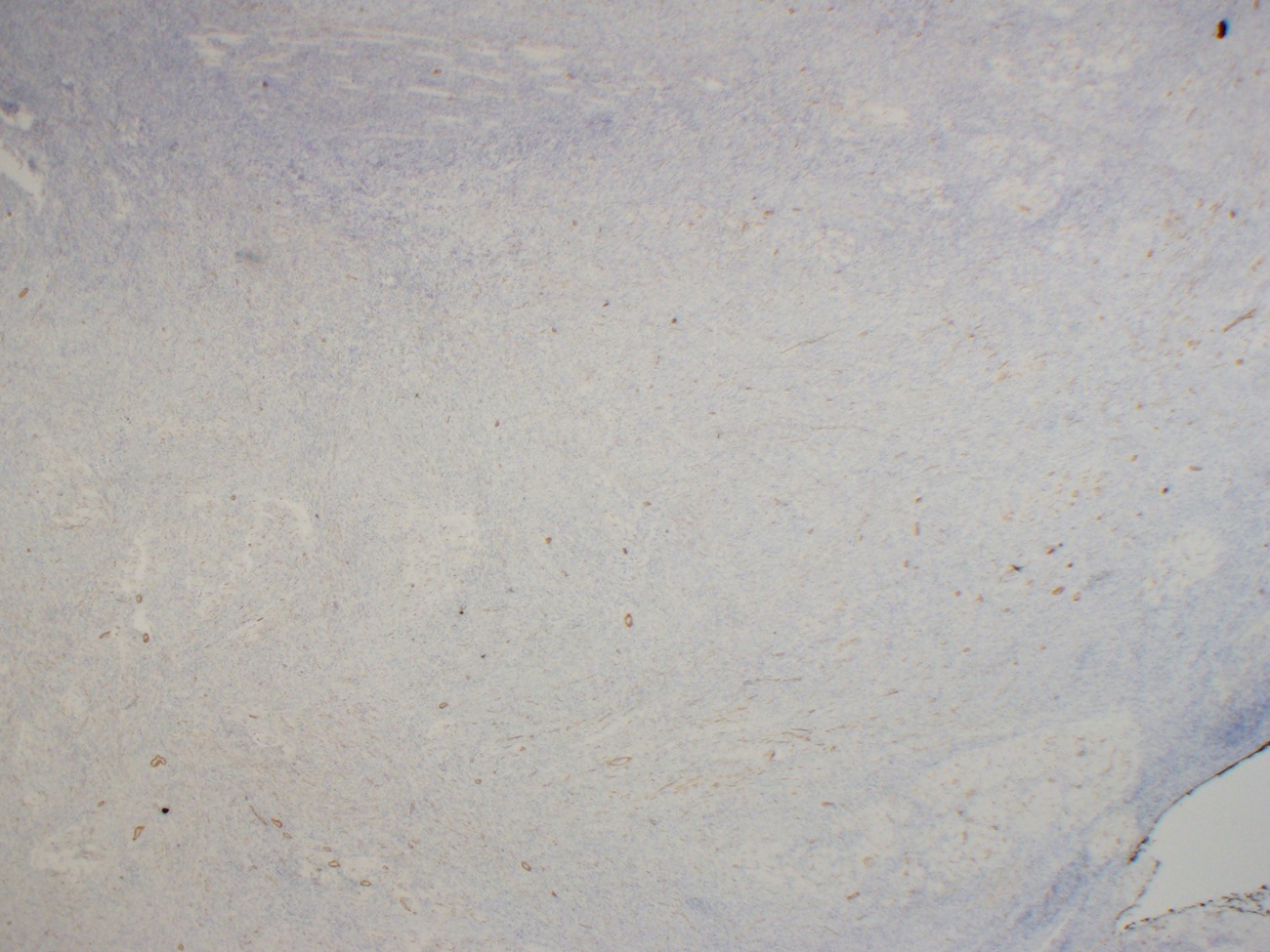
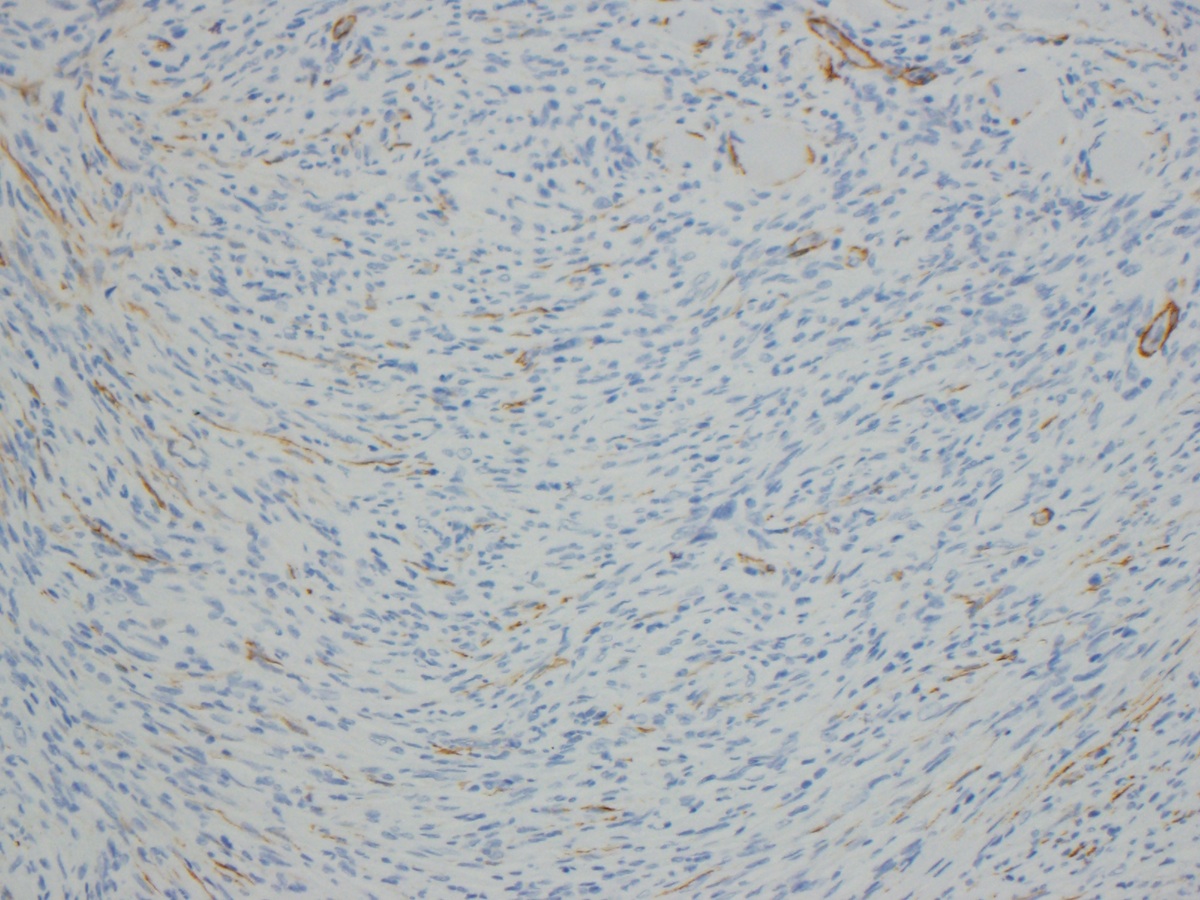
Microscopic (histologic) images
Positive stains
- At least 1 myogenic marker (desmin, calponin, tram track pattern for smooth muscle actin or muscle specific actin)
Negative stains
- S100, EMA, h-caldesmon, ALK, CD34
Electron microscopy description
- Myofibroblastic features of indented and clefted nuclei, variable rough endoplasmic reticulum, discontinuous basal lamina, fibronexus junctions (Ultrastruct Pathol 2008;32:97)
Molecular / cytogenetics description
- Gains at 1p11 → p36.3 (66%), 12p12.2 → p13.2 (45%), 5p13.2 → p15.3 (31%), +22 (28%), loss at 15q25 → q26.2 (24%) (Am J Clin Pathol 2009;131:701)
Sample pathology report
- Tongue, resection:
- Low grade myofibroblastic sarcoma (3.8 cm) (see comment)
- Margins of resection unremarkable.
- Comment: Immunohistochemical stains for SMA and desmin are positive. The overall histologic and immunohistochemical findings are most consistent with low grade myofibroblastic sarcoma.
Differential diagnosis
- Fibromatosis:
- Minimal nuclear atypia, usually negative for myogenic markers (but may sometimes express them focally)
- Fibrosarcoma:
- May have focal (not diffuse) myofibroblastic differentiation; herringbone fascicular pattern, a diagnosis of exclusion that should be made with much hesitation (Histopathology 2006;49:152)
- Inflammatory myofibroblastic tumor:
- Tumor of myofibroblasts with prominent lymphoplasmacytic infiltrate scattered among tumor cells, usually less atypia than myofibroblastic sarcoma, often ALK+ (Hum Pathol 2008;39:846)
- Leiomyosarcoma:
- Alternating fascicular pattern, more eosinophilic cytoplasm, more strong and diffuse staining for myogenic makers, usually dense cytoplasmic actin staining rather than tram track pattern
- Myofibroma / myofibromatosis:
- Often multiple and often in children (although solitary lesions and lesions in adults are both common as well), usually zonated with peripheral myoid nodules with intervening central cellular spindle areas with ectatic "hemangiopericytic" vessels; more diffuse or atypical forms of myofibroma may be very difficult to distinguish from myofibroblastic sarcoma (zonation is helpful feature)
- Nodular fasciitis:
- Not infiltrative, not deep, < 3 cm usually, lacks chromosomal anomalies seen in myofibroblastic sarcoma (although recently a recurrent translocation resulting in MYH9-USP6 gene fusion has been described in many cases of nodular fasciitis) (Lab Invest 2011;91:1427)
- Solitary fibrous tumor (SFT):
- Diffusely positive for CD34, usually patternless haphazard arrangement of cells, usually no atypia (except in malignant SFT)
Additional references
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following is true about low grade myofibroblastic sarcoma?
- It is more common than high grade myofibroblastic sarcoma
- It is paradoxically negative for muscle markers by immunohistochemistry
- It often metastasizes to the liver
- It should show at least focal nuclear atypia
Board review style answer #2
D. It should show at least focal nuclear atypia
Comment Here
Reference: Low grade myofibroblastic sarcoma
Comment Here
Reference: Low grade myofibroblastic sarcoma