Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Warmke L, Meis J. Papillary endothelial hyperplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuemasson.html. Accessed May 13th, 2024.
Definition / general
- Benign, reactive proliferation of endothelial cells (nonneoplastic)
- First described in 1923 by French physician Pierre Masson, who described an atypical papillary endothelial proliferation in an ulcerated hemorrhoid, which was originally considered to be a vascular neoplasm, in a 68 year old man
- Recognized as a reactive process in 1932 by Henschen
- Term intravascular papillary endothelial hyperplasia was first used by Clearkin and Enzinger in 1976 (Arch Pathol Lab Med 1976;100:441)
- 3 types: primary (pure form) arising in a dilated vessel, secondary (mixed form) arising in a pre-existing vascular lesion and rare extravascular form typically arising in hematoma (Am J Dermatopathol 1983;5:539)
Essential features
- Benign intravascular proliferation of reactive endothelial cells, forming numerous papillae most often lined by a single layer of plump endothelial cells
- Associated thrombotic material is frequently present
- Small, well circumscribed lesion without necrosis, marked cytologic atypia or infiltrative growth pattern
Terminology
- Also known as Masson tumor
- Intravascular papillary endothelial hyperplasia (IPEH)
Epidemiology
- Slight female predominance (1.3:1) (Ear Nose Throat J 2021 Jun 10 [Epub ahead of print])
- No known ethnic predilection
- Average age: 31 years (range, 9 months to 78 years) (Am J Dermatopathol 1983;5:539)
Sites
- Intravascular location is most common
- Can occur in any blood vessel
- Most commonly in subcutis of fingers (Am J Dermatopathol 1983;5:539)
- Frequently in subcutis of head, neck and upper extremities
- Does not tend to involve the overlying skin
Pathophysiology
- Pathogenesis still unknown
- Favored to be an exuberant form of organizing thrombus rather than a primary tumor, arising in the context of venous stasis
- Development takes place in several stages, including endothelial cell growth within a thrombus, production of collagenases by the endothelial cells, partial digestion of the thrombus and the formation of papillary structures (Cir Esp 2017;95:235)
- Hypoxia inducible factor 1 alpha (HIF1α) and vascular endothelial growth factor (VEGF), proteins associated with thrombus remodeling and angiogenesis, are highly expressed in cellular cores (Int J Clin Exp Pathol 2013;6:2912)
- Elevation of basic fibroblast growth factor (bFGF), which is released by macrophages due to traumatic vascular stasis, stimulates endothelial cell proliferation (J Hand Surg Am 1994;19:559)
Etiology
- May represent an alteration in the process of thrombosis
- Thrombus hypothesis: thought to result from hyperplastic endothelial proliferation caused by development and recanalization of a thrombus within a blood vessel
- Slight female predominance may have hormonal influence (Case Rep Dent 2014;2014:934593)
- Preceding trauma has been reported in occasional patients (Am J Dermatopathol 1983;5:539)
Clinical features
- Slow growing mass lesion or swelling
- Firm, subcutaneous nodule or papule
- Ovoid, rounded or lobulated shape
- Superficial location
- Bluish or reddish discoloration of the overlying skin
- May be tender or painless (Dermatol Online J 2016;22:13030)
- Often incidental finding within thrombosed dilated blood vessels or vascular tumors
Diagnosis
- Nonaggressive features on imaging studies
- Final diagnosis on histologic examination of excision specimen
- Assess for pre-existing vascular lesion (secondary form) (Arch Pathol Lab Med 1993;117:259)
Radiology description
- Ultrasound
- Well circumscribed mass
- Lobulated
- Hypoechoic
- MRI
- Well defined lobulated lesion
- High T2 signal peripherally (Skeletal Radiol 2016;45:1467)
- Variable central enhancement and signal intensity
- Majority (73%) associated with a dominant vessel (Skeletal Radiol 2016;45:1467)
Prognostic factors
- Benign clinical course
- Secondary form follows course of pre-existing vascular lesion
- No patient with pure form had a recurrence (Am J Dermatopathol 1983;5:539)
Case reports
- 19 year old man with enlarging mass in right shoulder (Arch Pathol Lab Med 1993;117:259)
- 29 year old woman with cecal mass (Surg Case Rep 2022;8:179)
- 32 year old woman with submucosal vulvar lesion (Dermatol Online J 2016;22:13030)
- 37 year old woman with submandibular gland lesion (Ear Nose Throat J 2021 Jun 10 [Epub ahead of print])
- 65 year old woman with mandibular lesion (J Craniofac Surg 2022;33:e431)
Treatment
- Treated by simple local excision
Clinical images
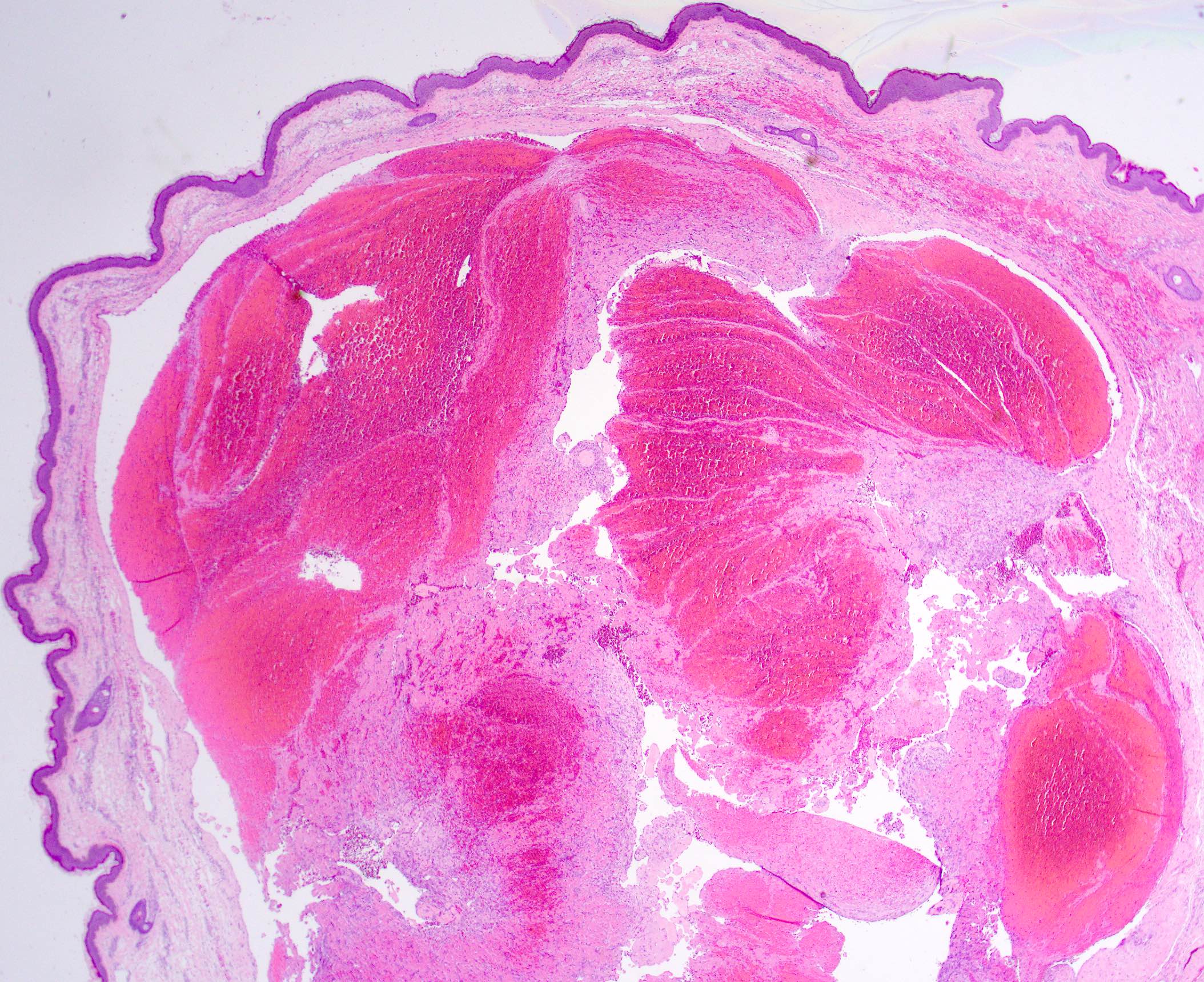
Gross description
- Well circumscribed lesion
- Purplish red multicystic mass
- Associated hemorrhage and clotted blood
- May be surrounded by a fibrous pseudocapsule
- Small lesion (usually < 5 cm) (Dermatol Online J 2016;22:13030)
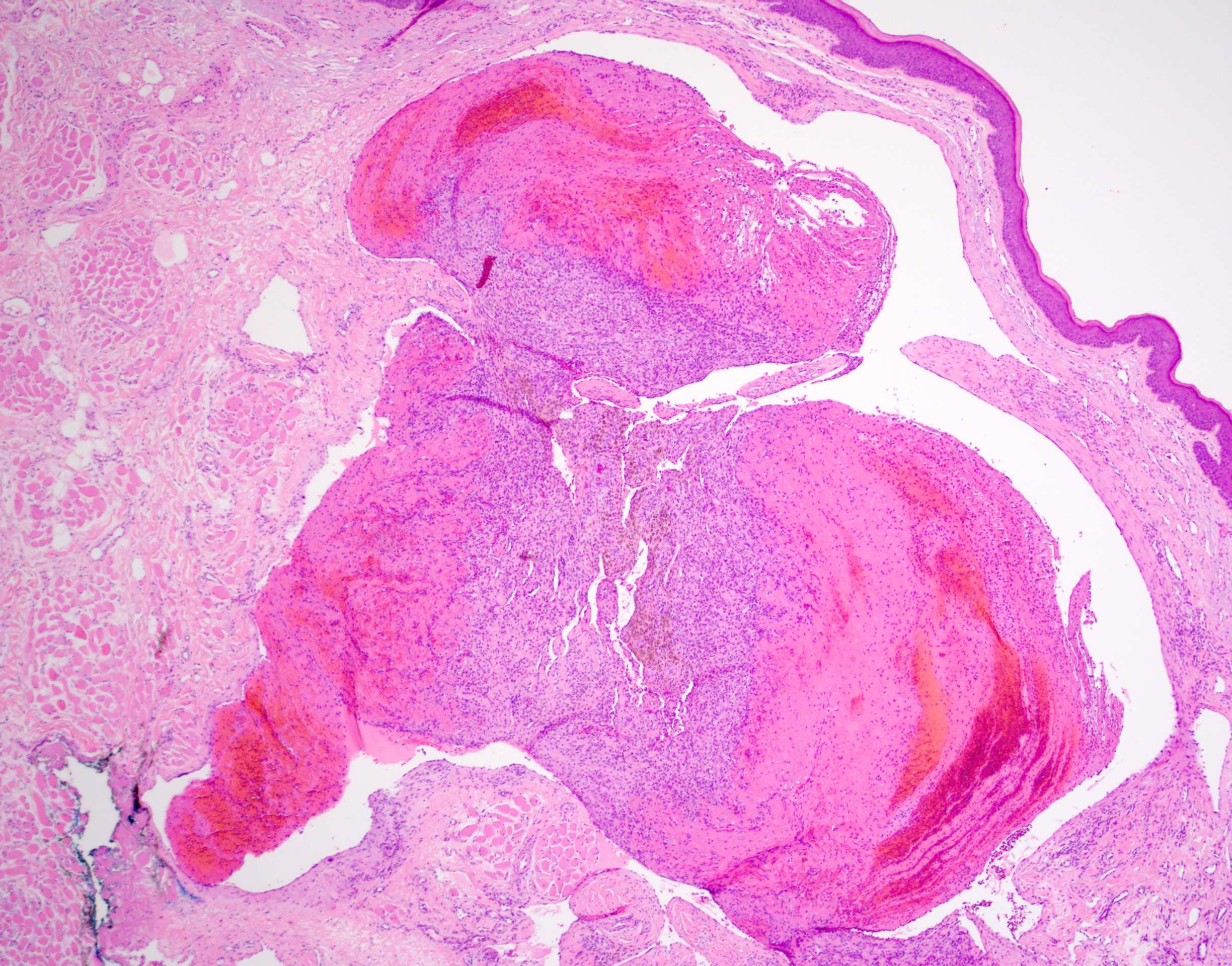
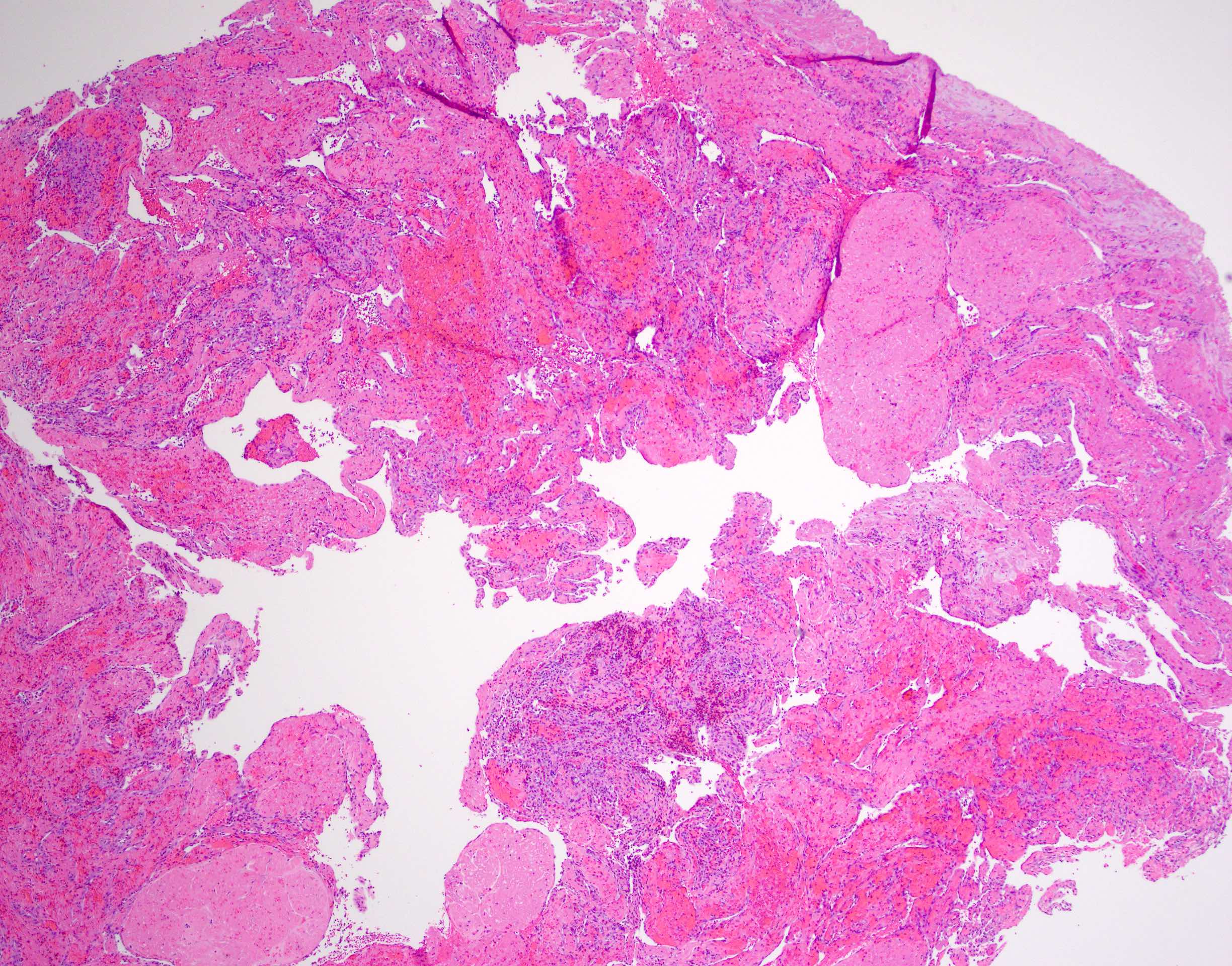
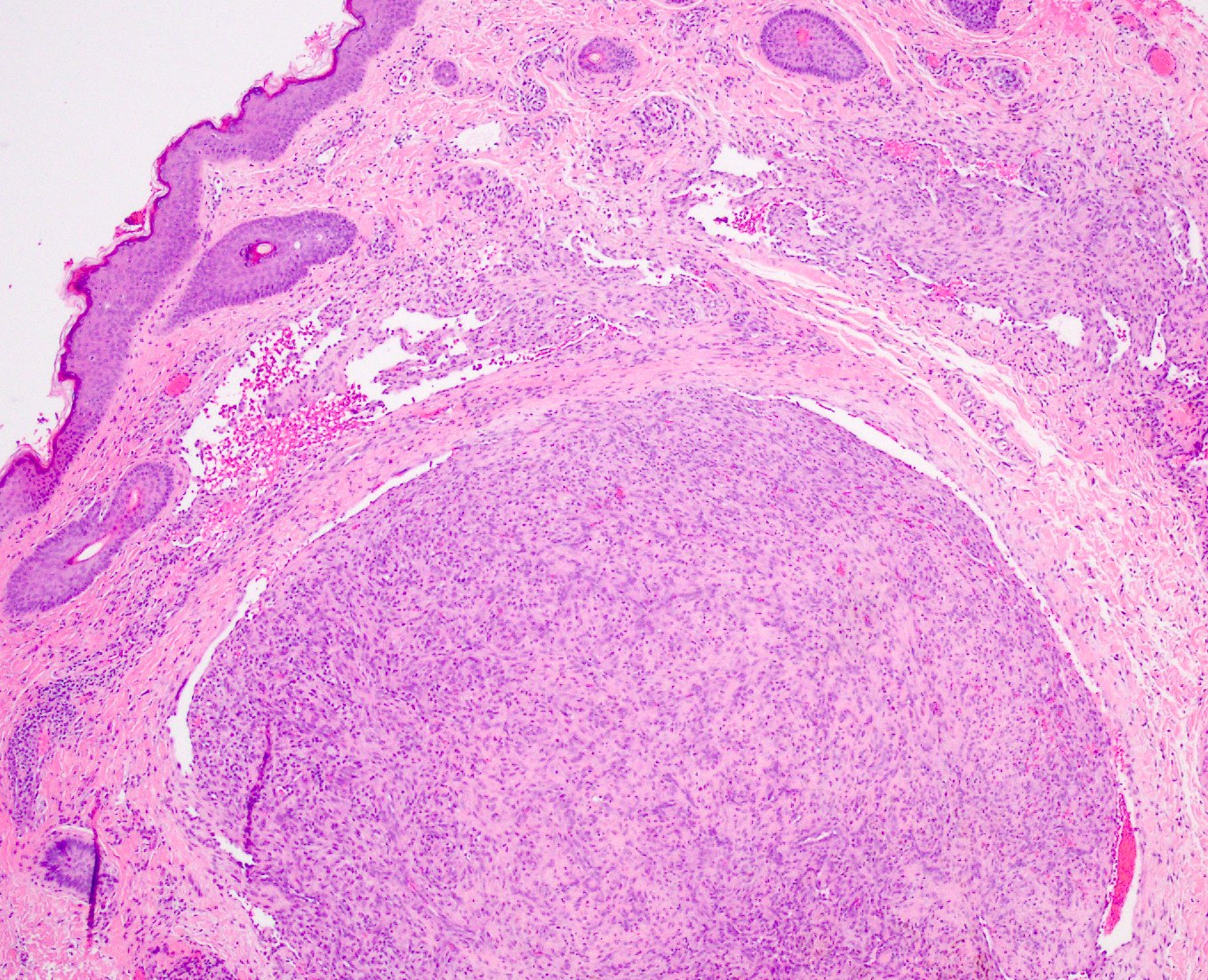
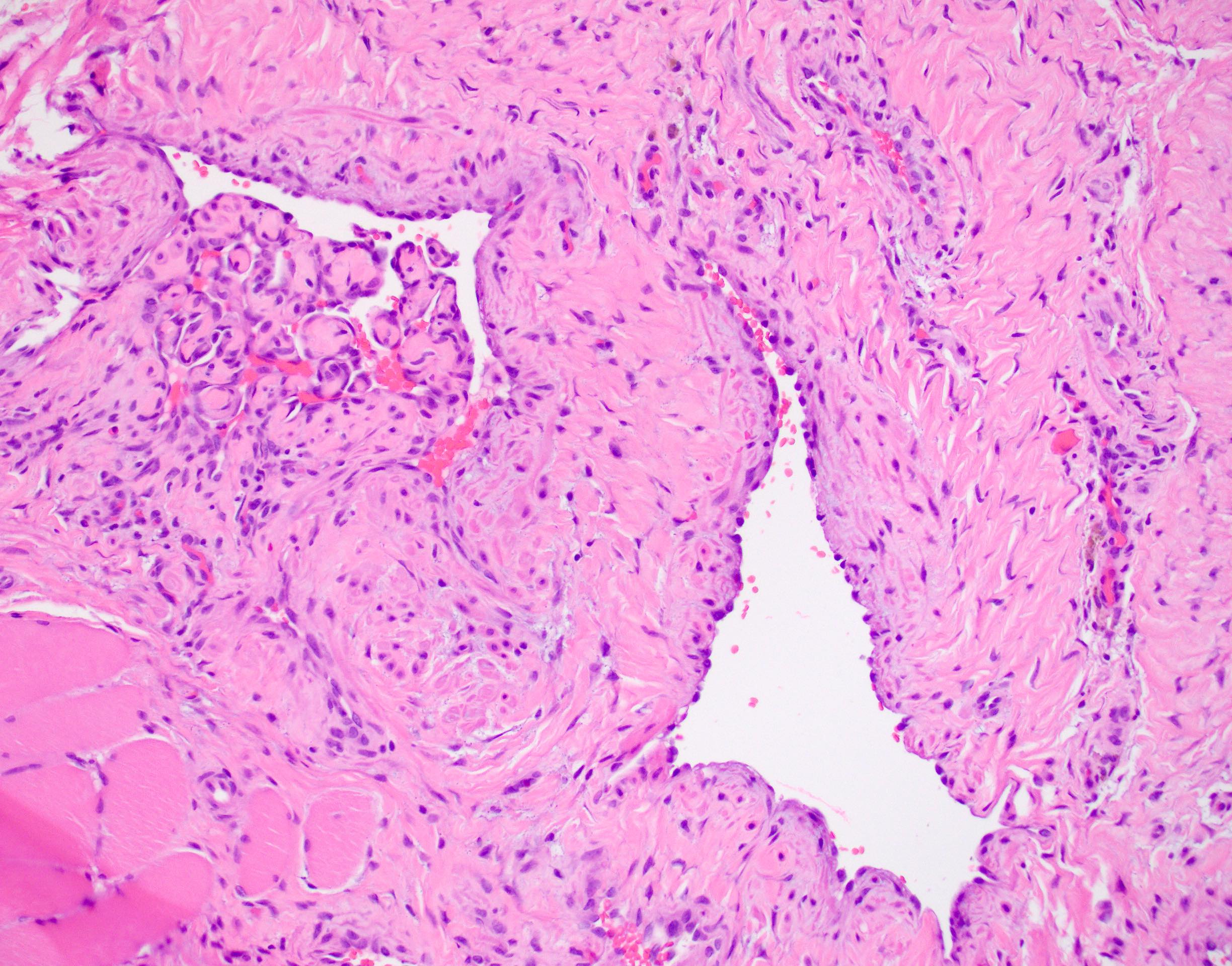
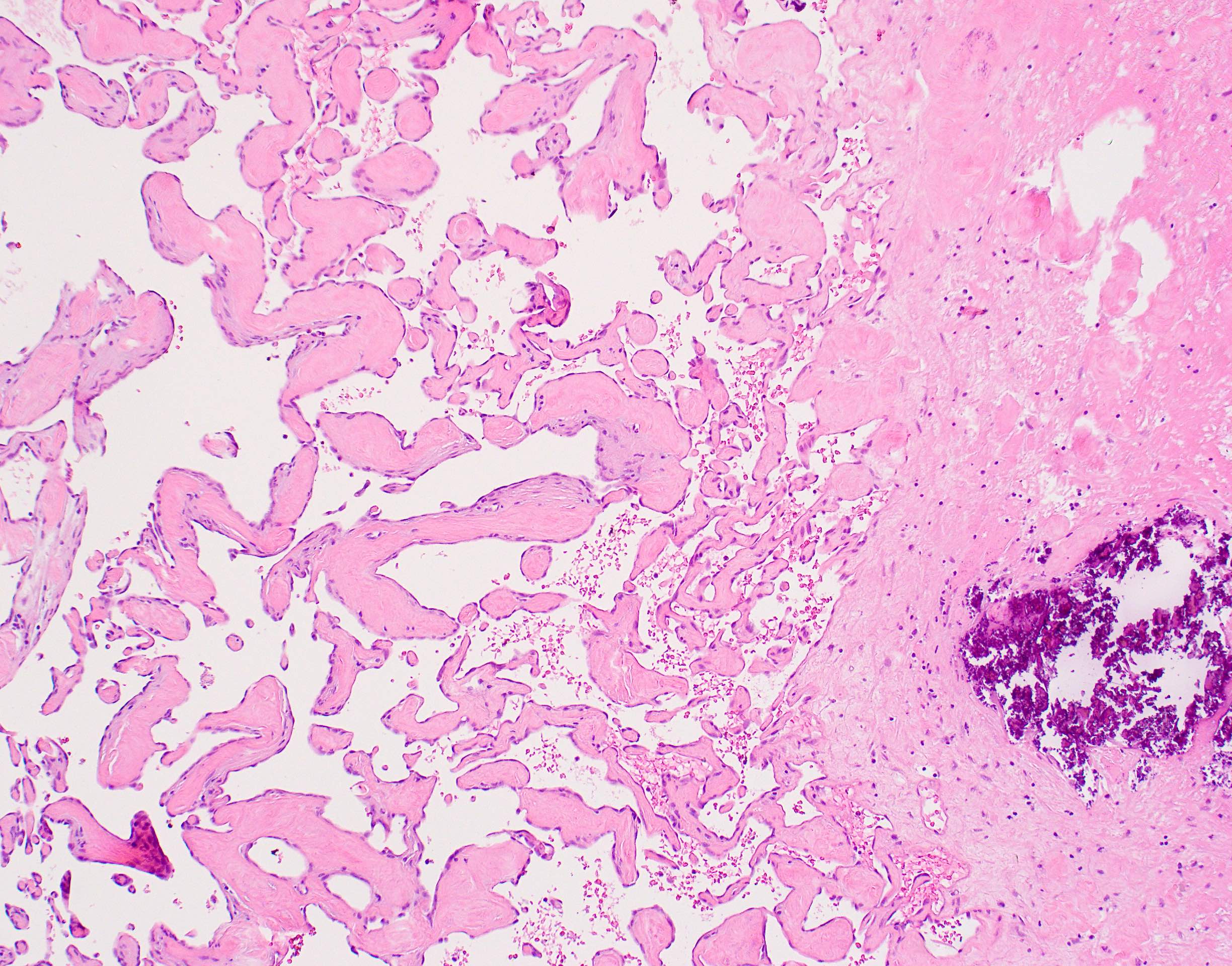
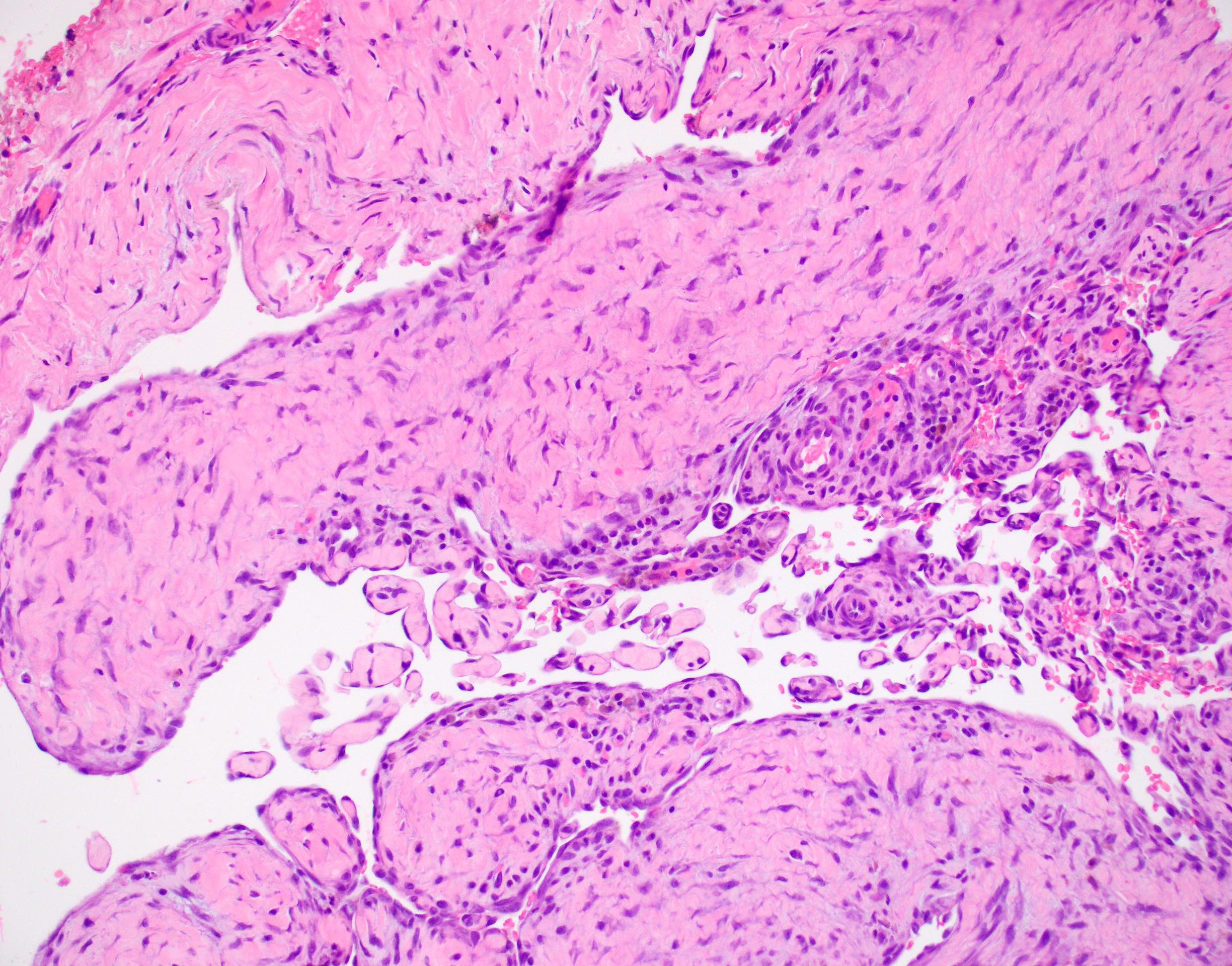
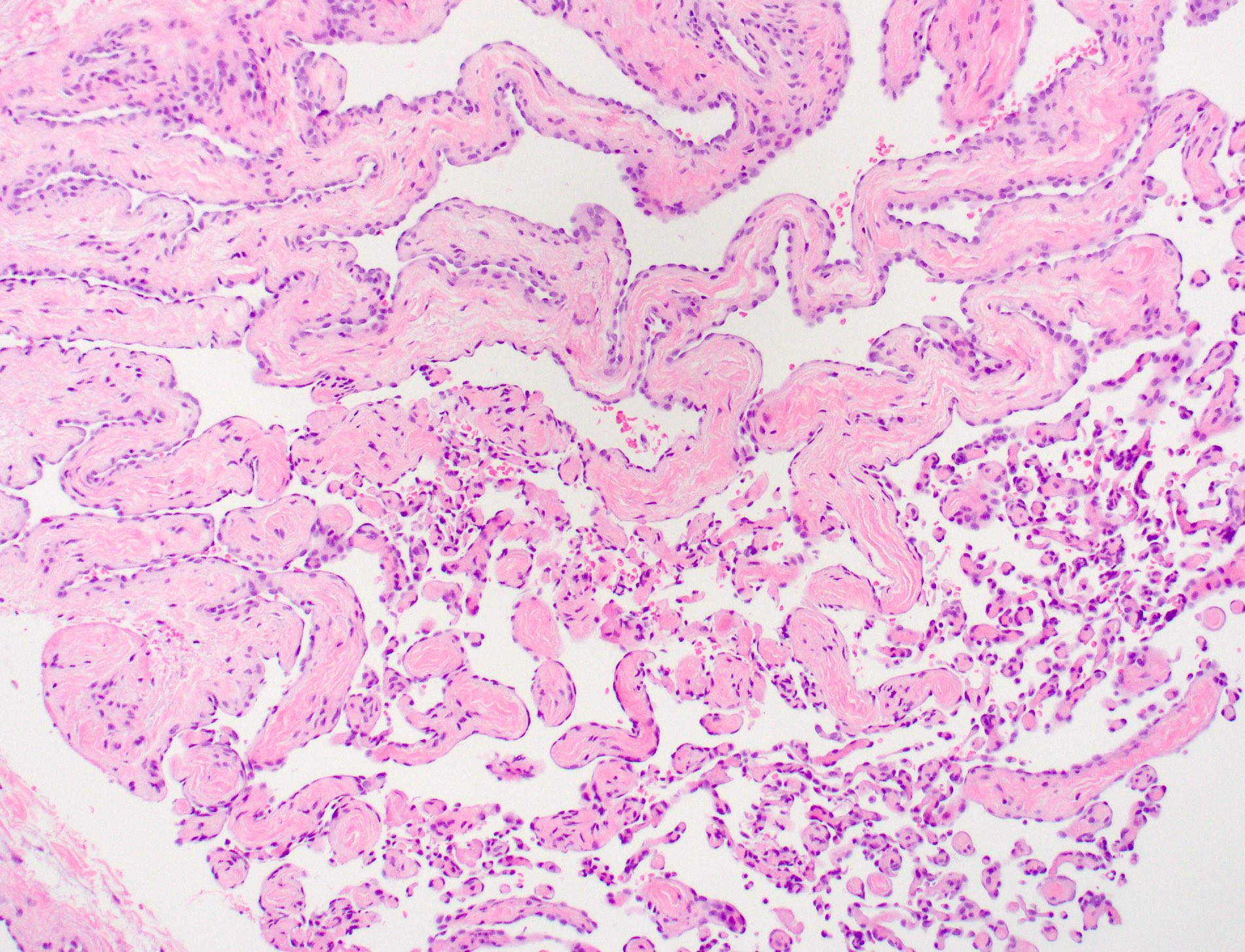
Microscopic (histologic) description
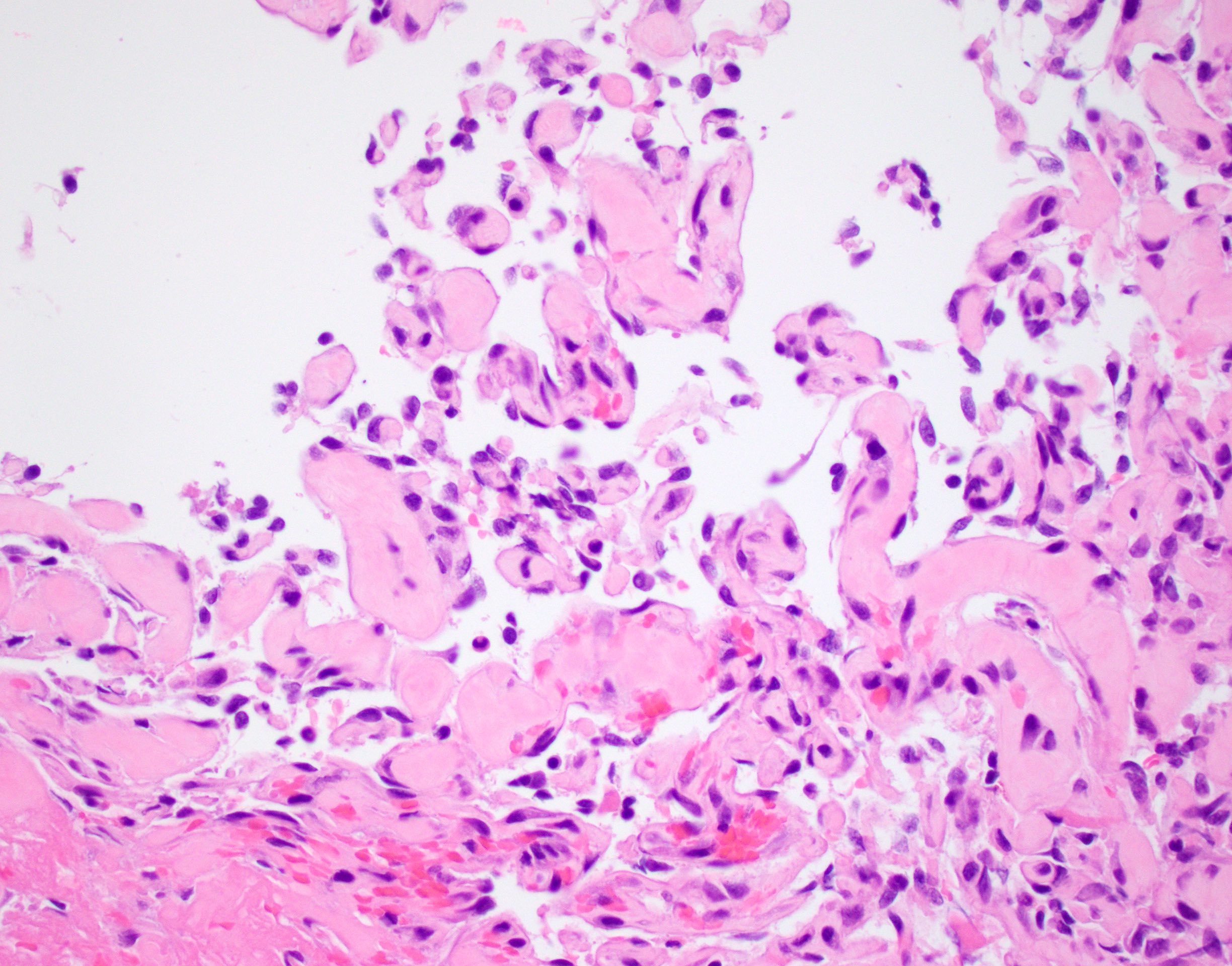
- Papillary structures within vascular spaces (Case Rep Pathol 2020;2020:4348629)
- Numerous papillae with cores of fibrin or fibrous connective tissue
- Papillae lined by a single layer of plump endothelial cells
- Piling up of endothelial cells is unusual
- Slight nuclear atypia and rare mitotic figures may be seen
- Associated thrombi of different sizes and stages of organization often present
- Absence of tissue necrosis
- No atypical mitotic figures
- No extensive high grade cytologic atypia
- Mixed form arises in vessels with abnormalities such as arteriovenous malformations, hemangiomas and pyogenic granulomas (Cir Esp 2017;95:235)
- Extravascular form associated with trauma related hematomas
Microscopic (histologic) images
Virtual slides
Cytology description
- Cytologic features are varied and not diagnostic (Acta Cytol 2012;56:199)
- Hemorrhagic and fibrinous background
- Scattered spindle cells with capillary network
- Hyaline cores surrounded by lesional cells (Acta Cytol 1990;34:175)
- No necrosis or marked cytologic atypia
- Rare mitotic figures may be present but no atypical forms
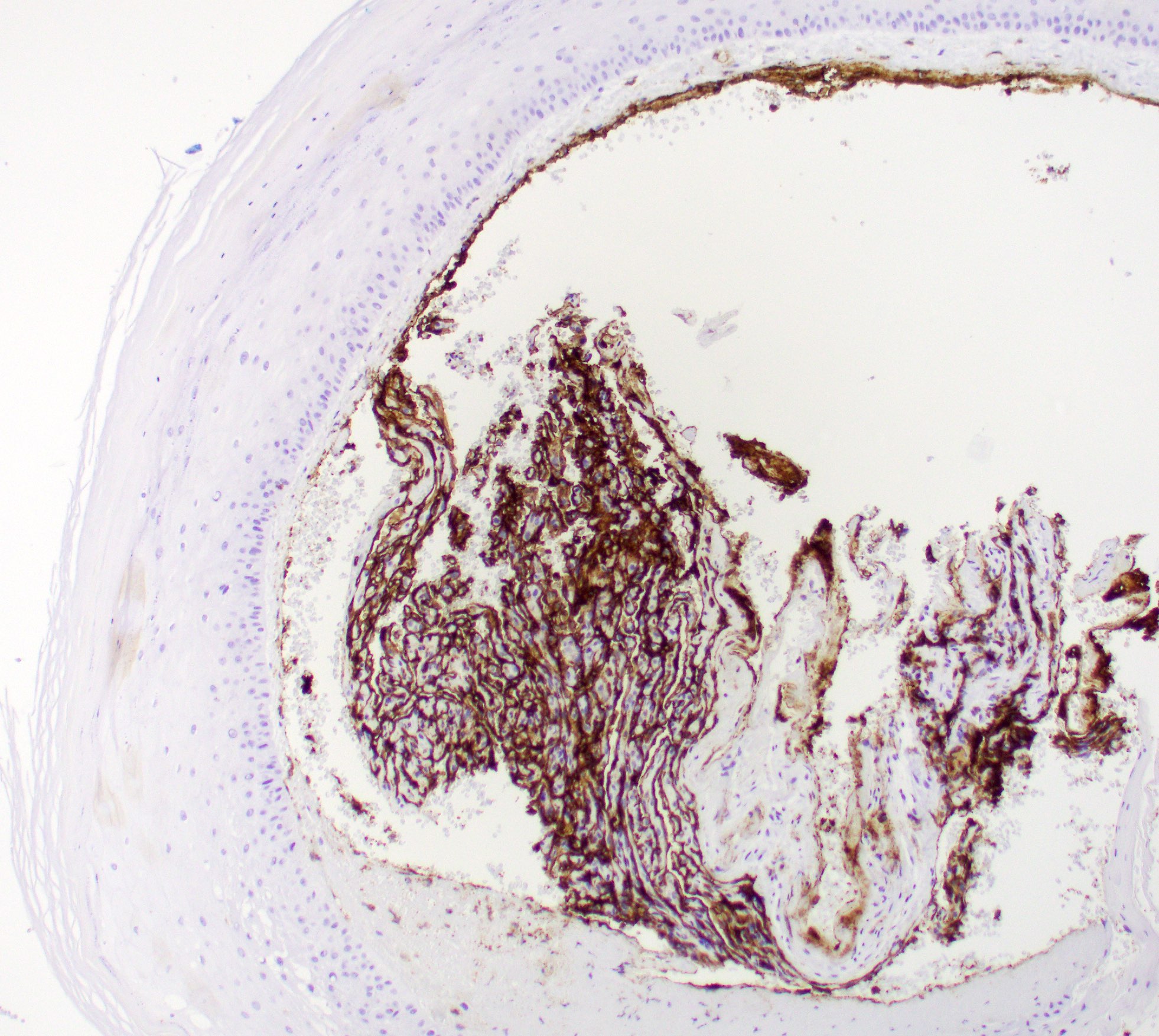
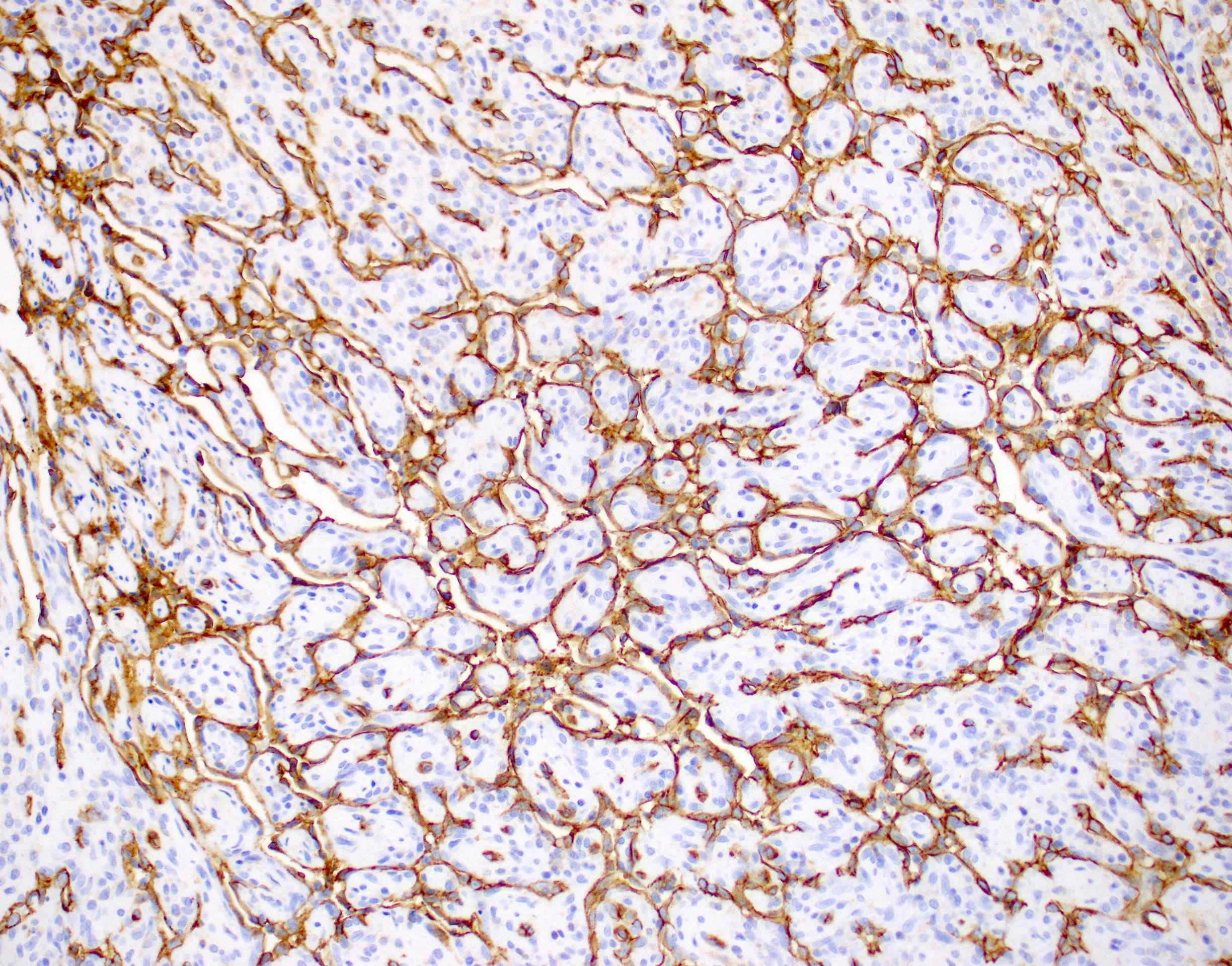
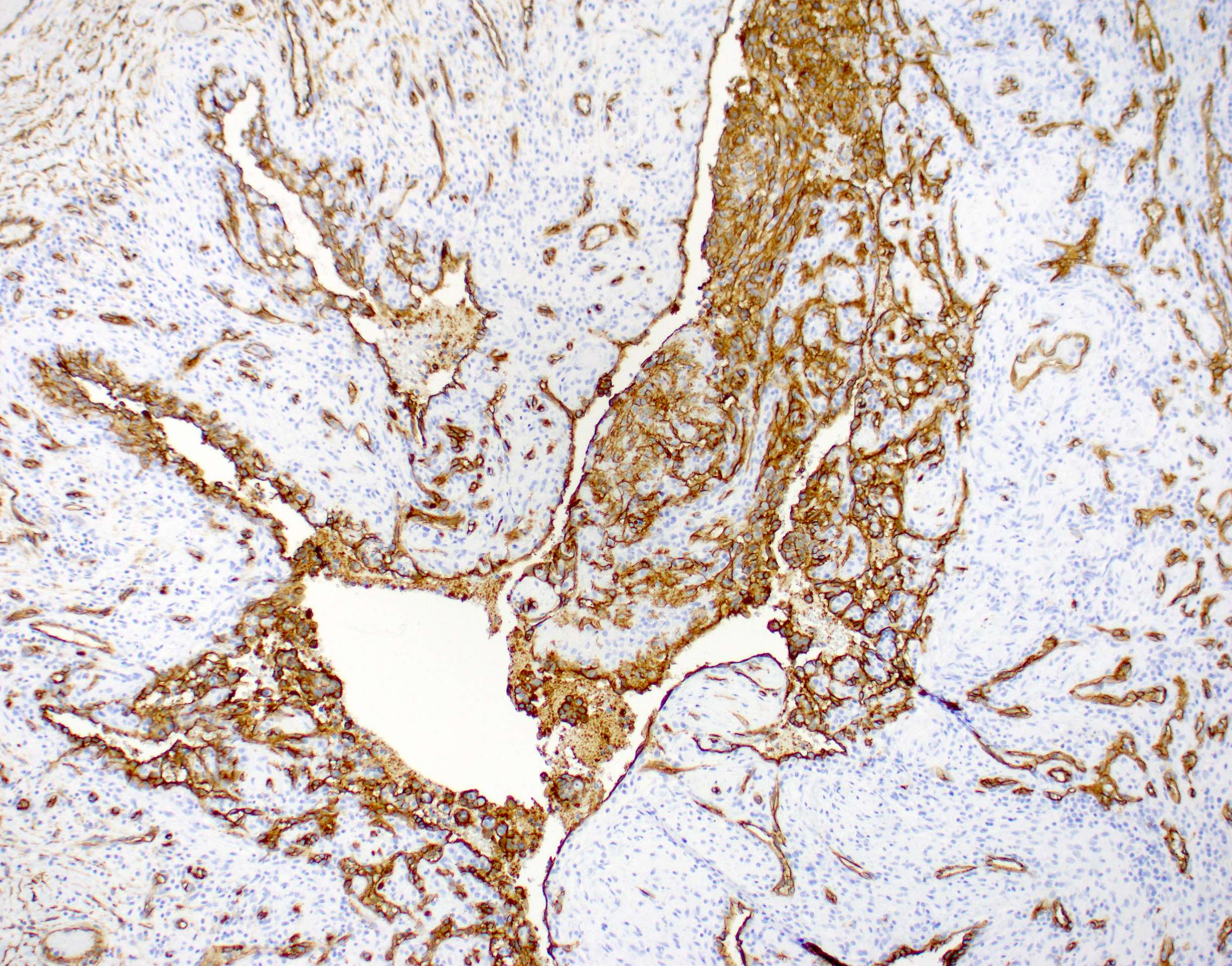
Positive stains
Negative stains
Electron microscopy description
- Papillae lined by nonstratified layer of plump endothelial cells
- Fibroblasts and pericytes in underlying stroma
- Ultrastructure and organization closely resembles granulation tissue (Cancer 1978;42:2304)
Videos
Masson "tumor"
Sample pathology report
- Skin and subcutaneous tissue, left index finger, mass, excision:
- Intravascular papillary endothelial hyperplasia (see comment)
- Comment: Sections show a dilated vessel centered in the superficial subcutaneous tissue with an associated intravascular proliferation of reactive endothelial cells, forming numerous papillary structures lined by a single layer of plump endothelial cells. The lesion is well circumscribed with a fibrous pseudocapsule and completely excised. No necrosis, no areas of infiltrative growth, no mitotic figures and no marked cytologic atypia is identified. Immunohistochemical stains for CD31 and ERG highlight the reactive endothelial cells, while CK cocktail is negative. These results support the diagnosis above. All control slides stained appropriately.
Differential diagnosis
- Pyogenic granuloma (lobular capillary hemangioma):
- Often arises in oral mucosa
- May be associated with pregnancy
- Proliferation of granulation tissue
- Inflammatory infiltrate, often composed of neutrophils, is present
- Arteriovenous malformation:
- Admixture of different vessels, including capillaries, veins and arteries
- Usually forms a larger mass involving deeper soft tissue
- Often have associated benign adipose tissue
- Extends beyond the confines of a single vessel (not intravascular)
- Thrombus:
- Composed of layers of platelets and fibrin
- Alternating layers of red blood cells can form lines of Zahn
- No papillary structures within vascular space
- Angiosarcoma:
- Solid areas of tumor growth
- Tumor necrosis common
- Stacking or piling up of endothelial cells
- Marked cellular pleomorphism
- Infiltrative growth pattern
- Irregular, anastomosing vascular channels
- Mitotic figures common, including atypical forms
Additional references
Board review style question #1
Board review style answer #1
C. Masson tumor.
Masson tumor is another name for intravascular papillary endothelial hyperplasia, which is currently favored to represent a reactive process as opposed to a true neoplasm. Hemangioma and arteriovenous malformation represent a true neoplasm or malformation respectively. Most cases of Masson tumor are associated with an organizing thrombus.
Comment Here
Reference: Papillary endothelial hyperplasia
Comment Here
Reference: Papillary endothelial hyperplasia
Board review style question #2
Board review style answer #2
D. Subcutaneous tissue of fingers.
The most common anatomic location for papillary endothelial hyperplasia is the subcutaneous tissue of the fingers. The heart, deep soft tissue and bone are all unusual locations for this entity.
Comment Here
Reference: Papillary endothelial hyperplasia
Comment Here
Reference: Papillary endothelial hyperplasia