Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Wang C, Longacre TA. Adenomas. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachadenomas.html. Accessed July 28th, 2025.
Definition / general
- Intestinal type adenoma: polypoid lesion with dysplastic intestinalized epithelium
- Foveolar type adenoma: polypoid lesion with dysplastic foveolar epithelium
Essential features
- Endoscopically visible polypoid lesion
- If flat lesion, refer to gastric dysplasia
- Classified into low grade or high grade dysplasia
- No lamina propria invasion
- Foveolar type adenoma maintains apical mucin cap
Terminology
- Foveolar type adenoma; gastric adenoma, foveolar type
- Intestinal type adenoma; gastric adenoma, intestinal type
ICD coding
- ICD-O: 8210/0 - adenomatous polyp, NOS
- ICD-10: D13.1 - benign neoplasm of stomach
- ICD-11: 2E92.1 & XH3DV3 - benign neoplasm of stomach & adenoma, NOS
Epidemiology
- Prevalence of gastric adenomas (Microorganisms 2021;9:108)
- Intestinal type adenoma is the most frequent adenoma (89.1%)
- Foveolar type adenoma (4.3%)
- Pyloric gland adenoma (3.4%)
- Adenomas associated with hereditary tumor syndromes (2.8%)
- Oxyntic gland adenoma (0.4%)
Sites
- Intestinal type adenoma: commonly occurs in stomach compartment where intestinal metaplasia commonly occurs (i.e., antrum and angularis incisura)
- Foveolar type adenoma: commonly occur in oxyntic mucosa (i.e., body and fundus)
Pathophysiology
- Genetic or epigenetic factors that promote intestinal metaplasia
Etiology
- Sporadic and syndromic
- Intestinal type adenoma
- Associated with intestinal metaplasia
- H. pylori infection
- Autoimmune gastritis
- Syndromes with APC gene mutations (i.e., familial adenomatous polyposis [FAP])
- Associated with intestinal metaplasia
- Foveolar type adenoma
- Commonly associated with polyposis syndromes
- Familial adenomatous polyposis
- Gastric adenocarcinoma and proximal polyposis of the stomach (GAPPS)
- Sporadic is rare
- Commonly associated with polyposis syndromes
Clinical features
- Predominantly asymptomatic
- Large adenomas may cause recurrent bleeding and anemia
- Associated with metachronous gastric adenocarcinoma
Diagnosis
- Diagnosed by upper endoscopy with biopsy / polypectomy
Prognostic factors
- Intestinal type gastric adenoma is more likely (but still with low probability) to progress to gastric cancer as compared to foveolar type gastric adenoma
- Foveolar type gastric adenoma with hybrid phenotype (both intestinal and gastric differentiation) carries higher cancer risk than only intestinal type adenoma
- Adenomas with low grade dysplasia have an annual malignant transformation rate of 0.6% and those with high grade dysplasia have annual malignant transformation rate of 6% (Histopathology 2021;78:106)
Case reports
- 62 year old woman with anemia (BMJ Case Rep 2021;14:e242836)
- 66 year old man with upper abdominal pain (World J Clin Cases 2020;8:5744)
- 79 year old woman with cholangitis (Gastrointest Endosc 2021;93:1422)
Treatment
- Endoscopic mucosal resection or endoscopic mucosal dissection
Gross description
- Intestinal type adenomas are flatly elevated whitish polyps
- Foveolar type adenomas are elevated lesions with a smooth surface and contractions (Digestion 2021;102:878)
- Usually small singular polyps, < 2 cm in largest dimension
- In FAP patients, usually coexist with multiple fundic gland polyps
Microscopic (histologic) description
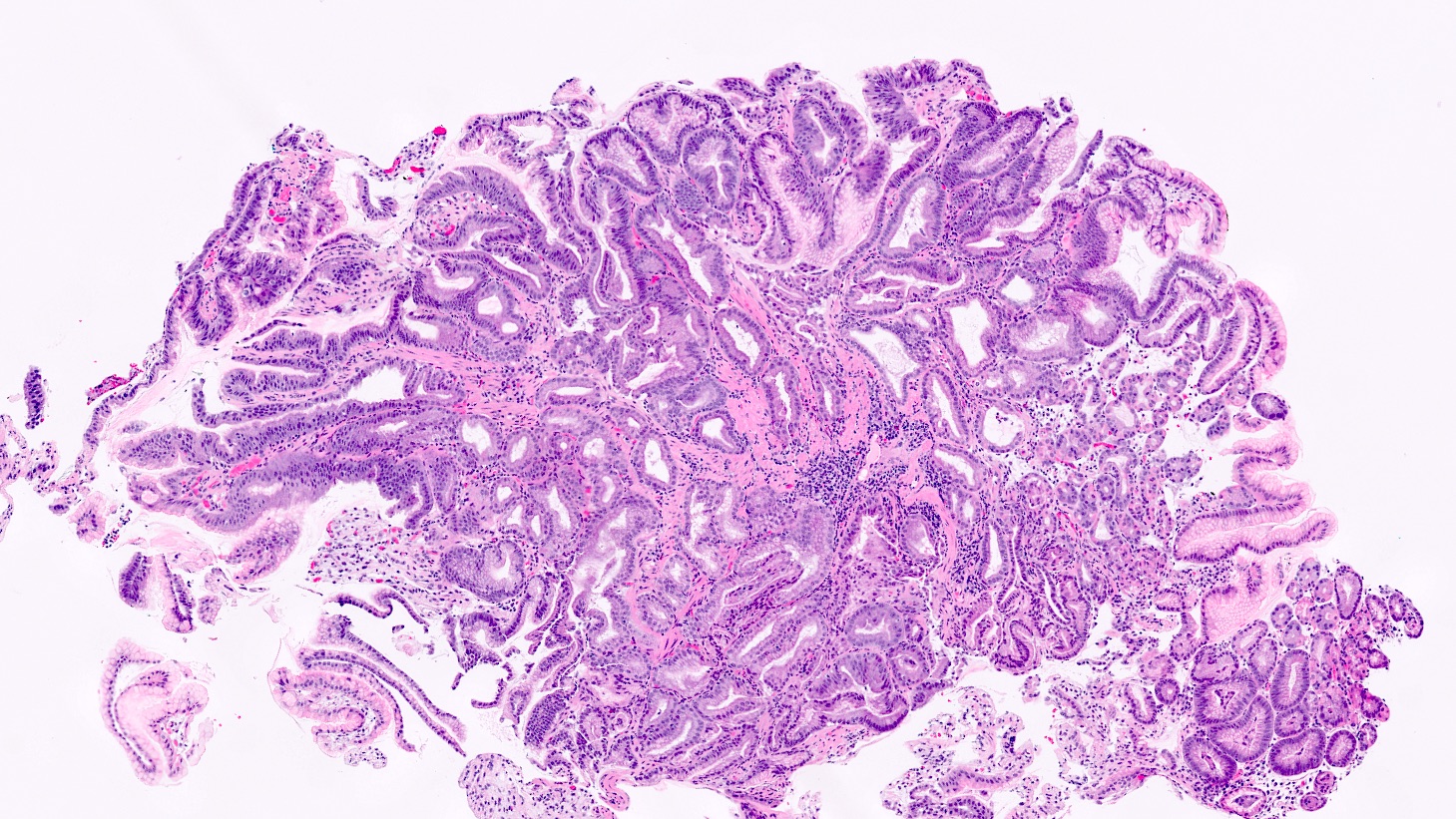
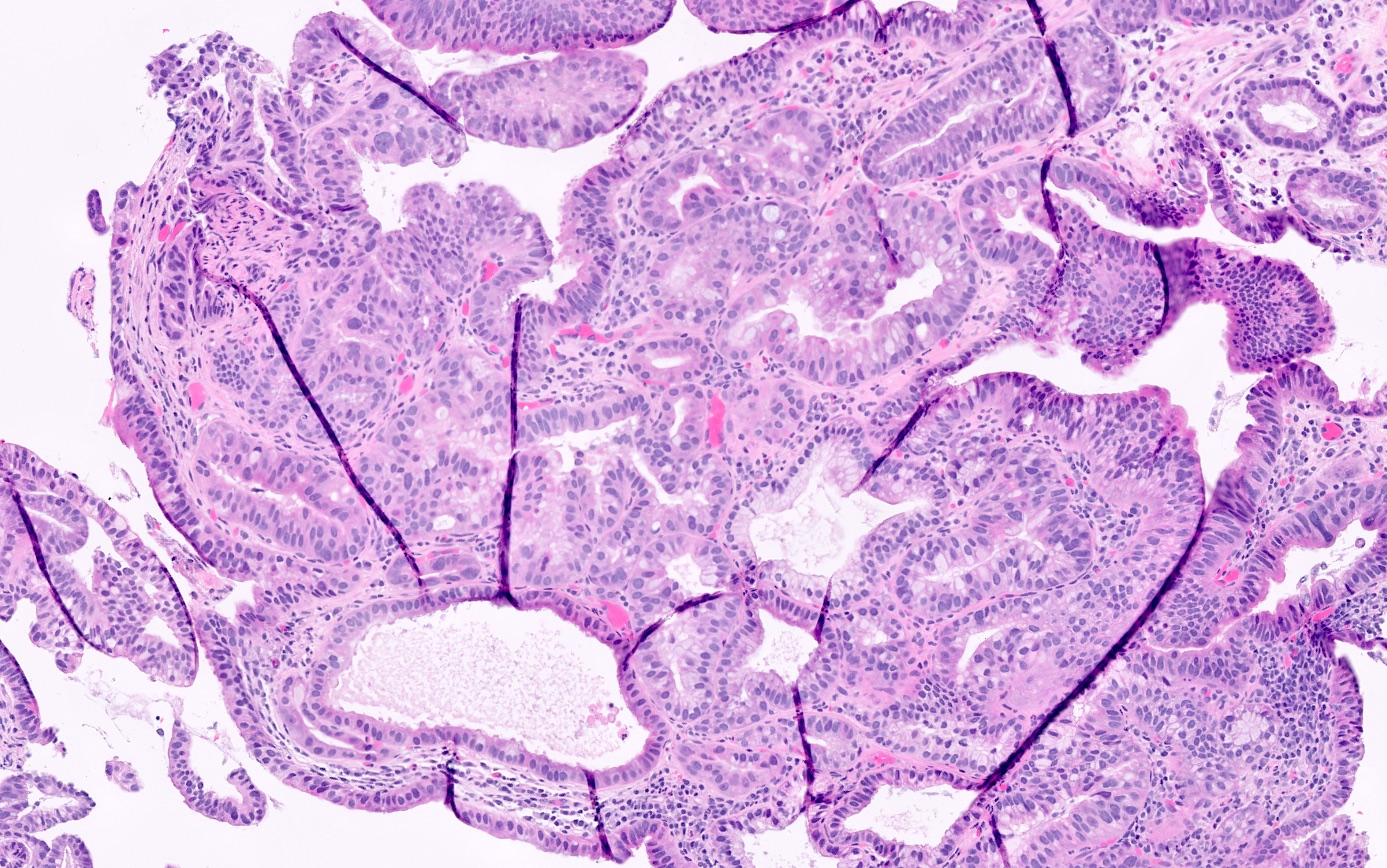
- Intestinal type adenoma
- Polypoid dysplastic columnar epithelium and tubules with varying degrees of Paneth and goblet cells (intestinal differentiation)
- Hyperchromatic elongated nuclei, similar to those seen in a colon tubular adenoma
- Background mucosa may exhibit chronic gastritis with intestinal metaplasia
- Lacks apical mucin caps
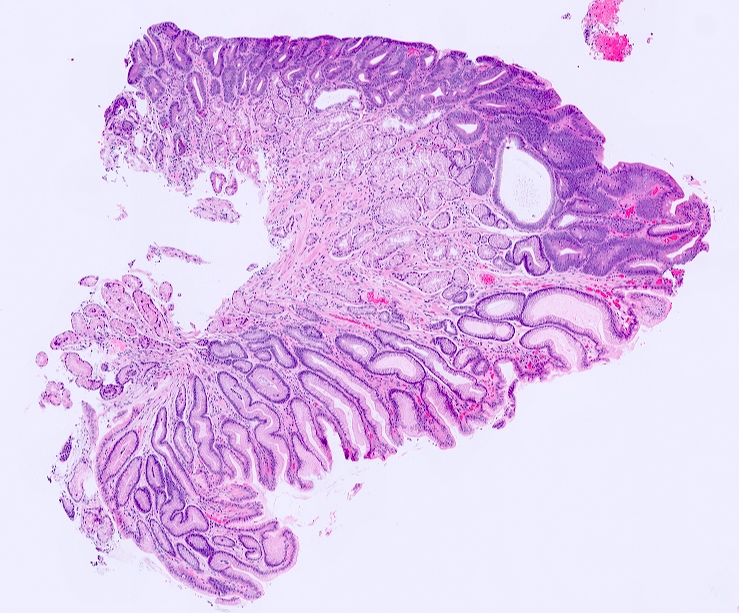
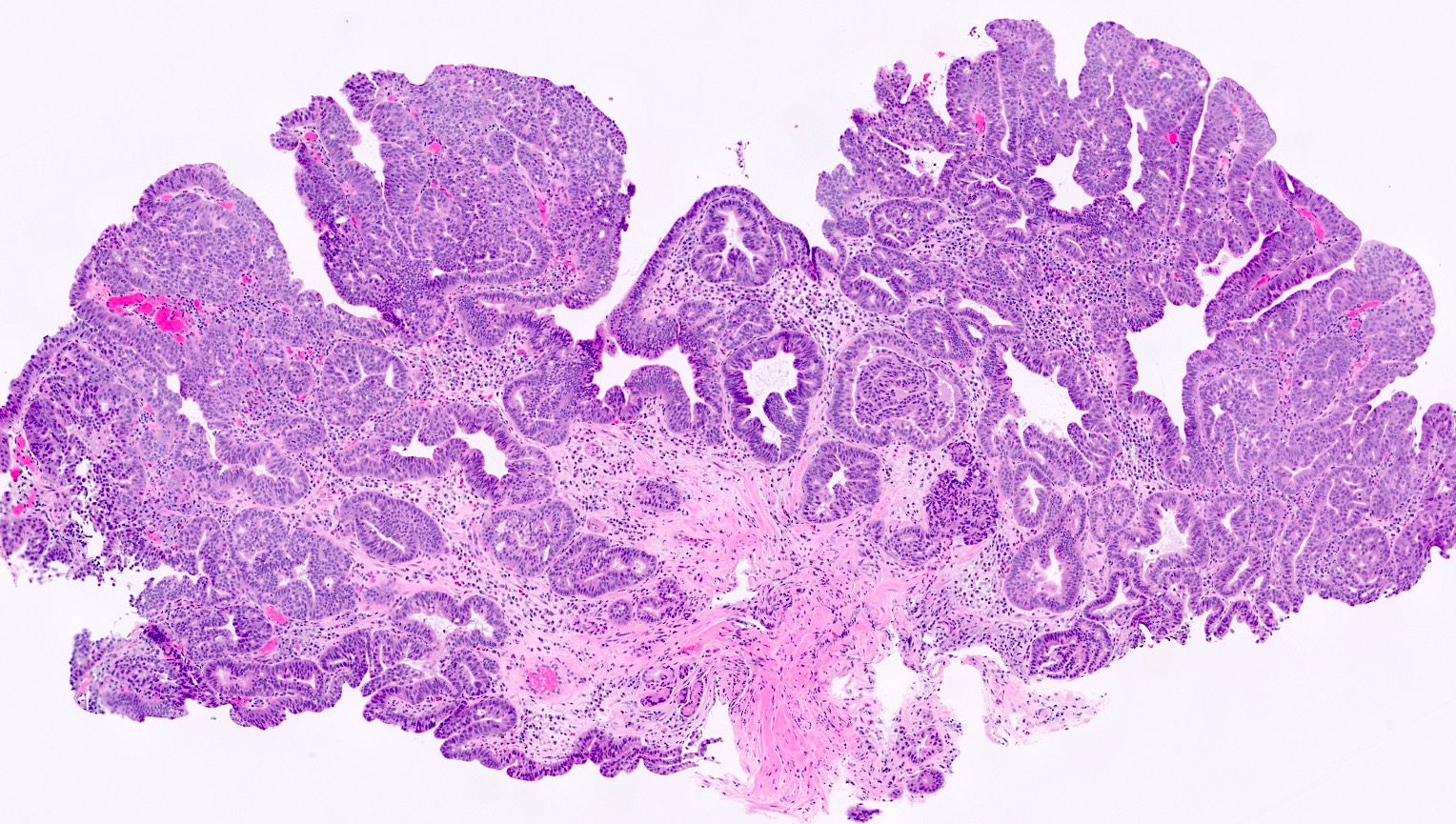
- Foveolar type adenoma
- Dysplastic columnar epithelium (foveolar type) with apical mucin caps
- Background gastric mucosa usually otherwise without abnormality (no inflammation, atrophy or metaplasia)
- May contain both intestinal and gastric differentiation in the same adenoma (hybrid phenotype)
- Dysplasia graded as low grade or high grade
- If high grade dysplasia, staged as pTis
Microscopic (histologic) images
Positive stains
- Foveolar type adenoma: MUC5AC and MUC6 (variable) (Histopathology 2021;78:106)
- Intestinal type adenoma: MUC2 and CDX2 (Histopathology 2021;78:106)
- PASD positive mucin
Sample pathology report
- Stomach, fundus polyp, biopsy:
- Fragments of gastric adenoma, foveolar type (see comment)
- Comment: There is no evidence of high grade dysplasia. Clinical and endoscopic correlation recommended to ensure adequacy of excision.
- Stomach, antral polyp, endoscopic mucosal resection:
- Gastric adenoma, intestinal type, with focal high grade dysplasia, 1.3 cm, excised (see comment)
- Comment: There is no evidence of lamina propria or muscularis mucosae invasion. There is no adenomatous epithelium at resection margins. The background gastric mucosa shows intestinal metaplasia. No Helicobacter organisms are present.
Differential diagnosis
- Reactive atypia:
- Uniform nuclear enlargement with visible nucleoli without crowding
- Cellular maturation at mucosal surface
- Surrounding inflammation, intestinal metaplasia or foveolar hyperplasia
- Other types of adenomas:
- Oxyntic adenoma:
- Irregular glands lined by columnar cells with a predominant chief cell component, mimicking oxyntic glands
- Pyloric gland adenoma:
- Closely packed glands lined by cuboidal to low columnar epithelium with ground glass cytoplasm, bland nuclei and without apical mucin
- Oxyntic adenoma:
- Gastric polyps with dysplasia:
- Fundic gland polyp with dysplasia:
- Background gastric mucosa shows dilated parietal cell lined glands with low or high grade epithelial dysplasia
- Hyperplastic polyp with dysplasia:
- Background gastric mucosa with cystically dilated, branching crypts and edematous lamia propria with mixed inflammatory infiltrate and low or high grade epithelial dysplasia
- Fundic gland polyp with dysplasia:
- Intramucosal adenocarcinoma:
- Complex architecture and significant atypia with invasion into lamina propria
- Variable desmoplastic stromal change
Additional references
Practice question #1
A polyp is identified in the gastric antrum. The background nonlesional gastric mucosa shows extensive Helicobacter organisms and moderate amounts of intestinal metaplasia. What is the most likely diagnosis of this lesion?
- Foveolar type adenoma
- Fundic gland polyp
- Intestinal type adenoma
- Pyloric gland adenoma
Practice answer #1
C. Intestinal type adenoma is commonly found in the antrum with association to background intestinal metaplasia. Longstanding H. pylori infection is a common cause of intestinal metaplasia. Intestinal type adenomas are far more common than foveolar type adenoma and pyloric gland adenomas. Fundic gland polyps are found in oxyntic mucosa (i.e., gastric body or fundus).
Comment Here
Reference: Adenomas
Comment Here
Reference: Adenomas
Practice question #2
Practice answer #2
C. Intramucosal adenocarcinoma. Section shows complex glandular architecture with back to back and cribriforming glands. The nuclei show significant atypia. Focally, there is glandular budding. The nuclei show significant atypia with nuclear rounding and loss of polarity. All features are consistent with intramucosal adenocarcinoma.
Comment Here
Reference: Adenomas
Comment Here
Reference: Adenomas