Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Srivastava S. Pyloric gland adenoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachpyloricglandadenoma.html. Accessed September 3rd, 2025.
Definition / general
- Grossly visible neoplastic lesion in the stomach, wherein the native glands are replaced by closely packed pyloric glands lined by cuboidal to low columnar epithelium
- 40 - 50% associated with high grade dysplasia
Essential features
- Closely packed tubular glands lined by cuboidal to low columnar epithelium with ground glass cytoplasm, bland nuclei and no well formed apical mucin cap
- 60% observed in corpus of the stomach, followed by cardia and antrum
- Associated with autoimmune gastritis, familial adenomatosis polyposis and Lynch syndrome
- Commonly associated with dysplasia
Terminology
- Pyloric gland tubular adenoma; gastric differentiated adenoma (German); pyloric gland intracystic papillary neoplasm (J Clin Pathol 2014;67:883)
ICD coding
- ICD-O: 8210/0 - adenomatous polyp
- ICD-10: K31.7 - polyp of stomach and duodenum
- ICD-11: 2E92.1&XH3DV3 - benign neoplasm of stomach and adenoma NOS
Epidemiology
- Accounts for 3% of all gastric epithelial polyps (Virchows Archive 2003;442:317)
- Slightly more common in females as compared with males (Am J Surg Pathol 2009;33:186)
- Mean age: 70 years
- No predilection for a specific geographic location
- Strongly associated with autoimmune gastritis; some association with familial adenomatosis polyposis
Sites
- In stomach, most commonly seen in fundus / corpus, followed by cardia and antrum
- Other sites: reported frequencies are variable in different studies; however, one of the largest series of 373 cases of pyloric gland adenoma (PGA) reports the following frequencies - duodenum including duodenal bulb (11%), gallbladder (4.3%), pancreas, bile duct (1.4%), pancreatic duct (0.3%), rectum (1.1%), esophagus (2.4%), cervix (rare) (J Clin Pathol 2014;67:883)
Pathophysiology
- Pyloric gland metaplasia (in the stomach) / gastric heterotopia (elsewhere) is the precursor lesion of pyloric gland adenoma (J Clin Pathol 2014;67:883)
Etiology
- Associated with autoimmune gastritis
- It is also seen in association with familial polyposis syndrome, Lynch syndrome, juvenile polyposis syndrome, McCune-Albright syndrome (Am J Surg Pathol 2014;38:784, Am J Surg Pathol 2014;38:1618, Virchows Arch 2017;470:391)
Clinical features
- Usually asymptomatic but may present with gastric distention, epigastric pain or heartburn
- Background mucosa is that of autoimmune gastritis or Helicobacter pylori gastritis
- Its predominance in females reflects its association with autoimmune gastritis
- Sporadic PGA tends to occur in younger patients and without any inflammatory background, sometimes in association with fundic gland polyp
Diagnosis
- Diagnosis is made by endoscopy and histology
Prognostic factors
- Since it is associated with high grade dysplasia and gastric adenocarcinoma, all PGAs should be resected
- Prognosis depends on the associated dysplasia and adenocarcinoma
- The neoplastic risk increases with the associated autoimmune gastritis, larger mean polyp size and tubulovillous architecture; however, after a complete endoscopic resection, the rate of local recurrence is low (< 10%) (Histopathology 2018;72:1007)
Case reports
- 60 year old man presenting with epigastric pain and polyp in corpus of stomach (Case Rep Gastroenterol 2013;7:392)
- 69 year old man with a submucosal tumor-like lesion in stomach body (World J Clin Cases 2020;8:2380)
- 75 year old man with STK11 germline mutation and multiple gastrointestinal tumors (Case Rep Gastroenterol 2020;14:547)
- 80 year old woman with a polypoid tumor in cardia (Am J Gastroenterol 2018;113:2645)
- 81 year old man with a flat lesion 20 mm in diameter (J Gastrointestin Liver Dis 2018;27:361)
Treatment
- Endoscopic mucosal resection, surgical resection
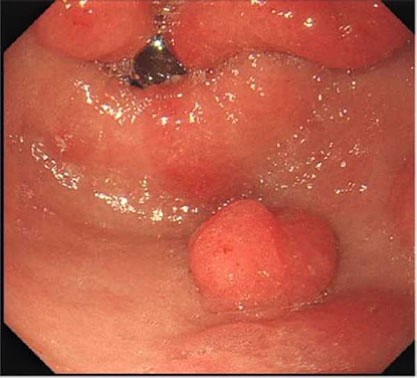
Clinical images
Gross description
- Polyp, sessile or pedunculated or masses ranging from 1 - 10 cm in size
- Usually single
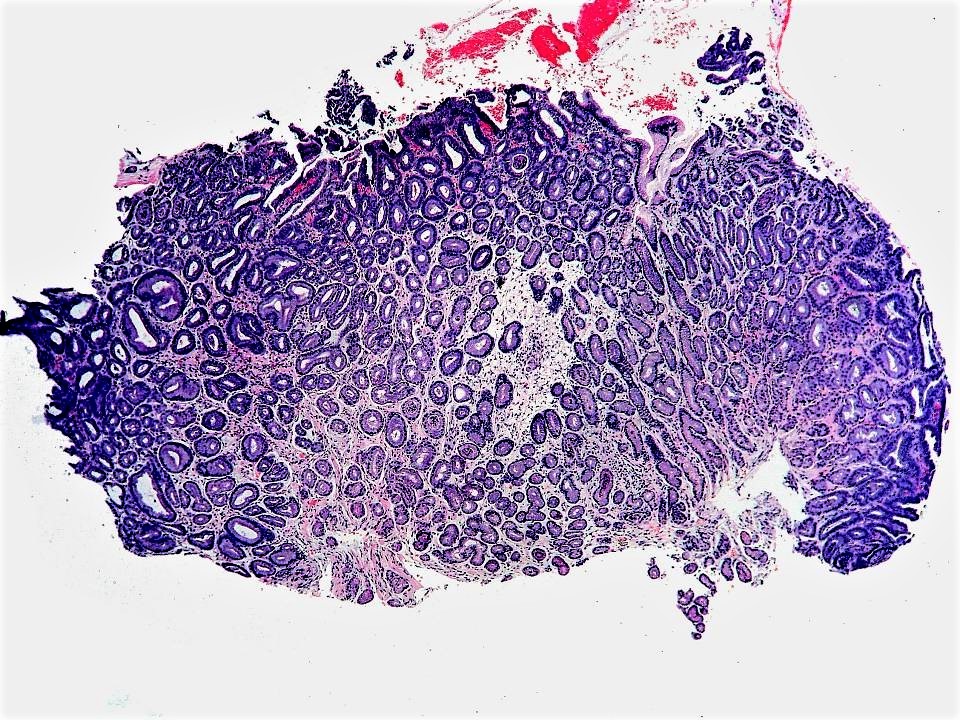
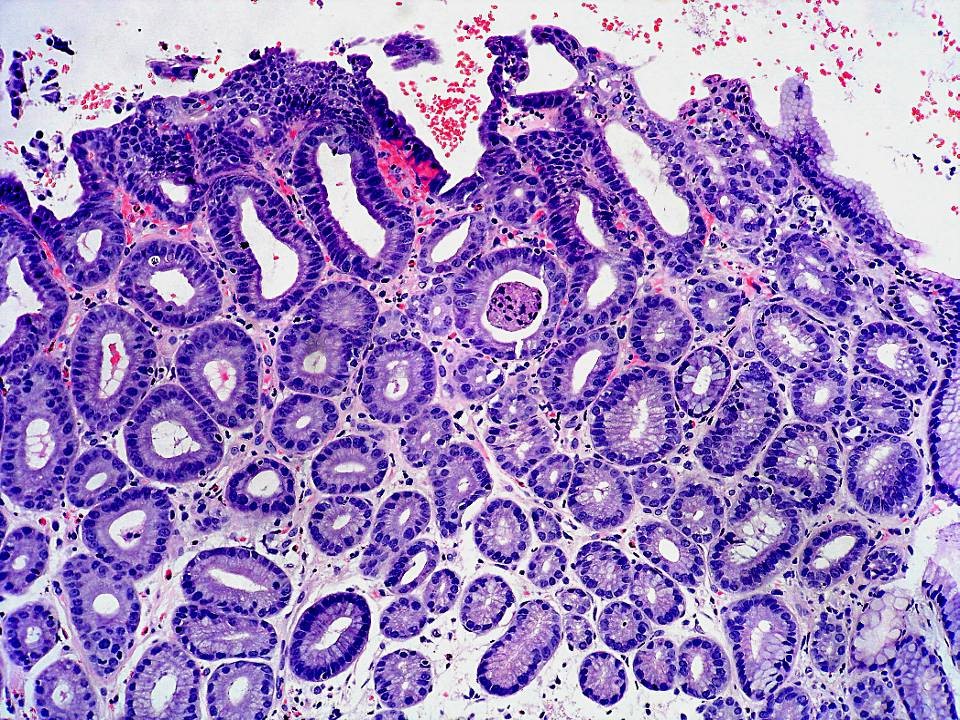
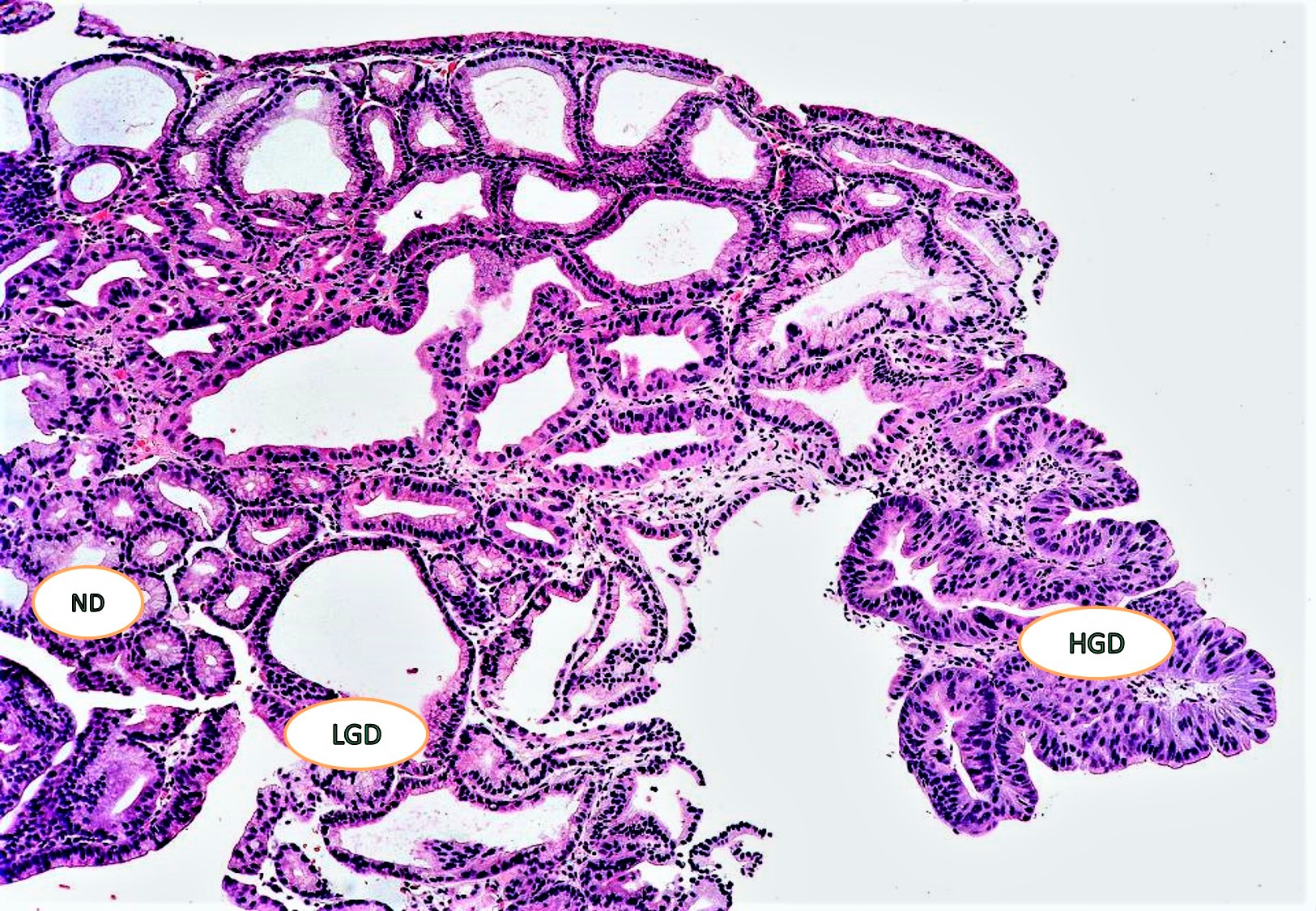
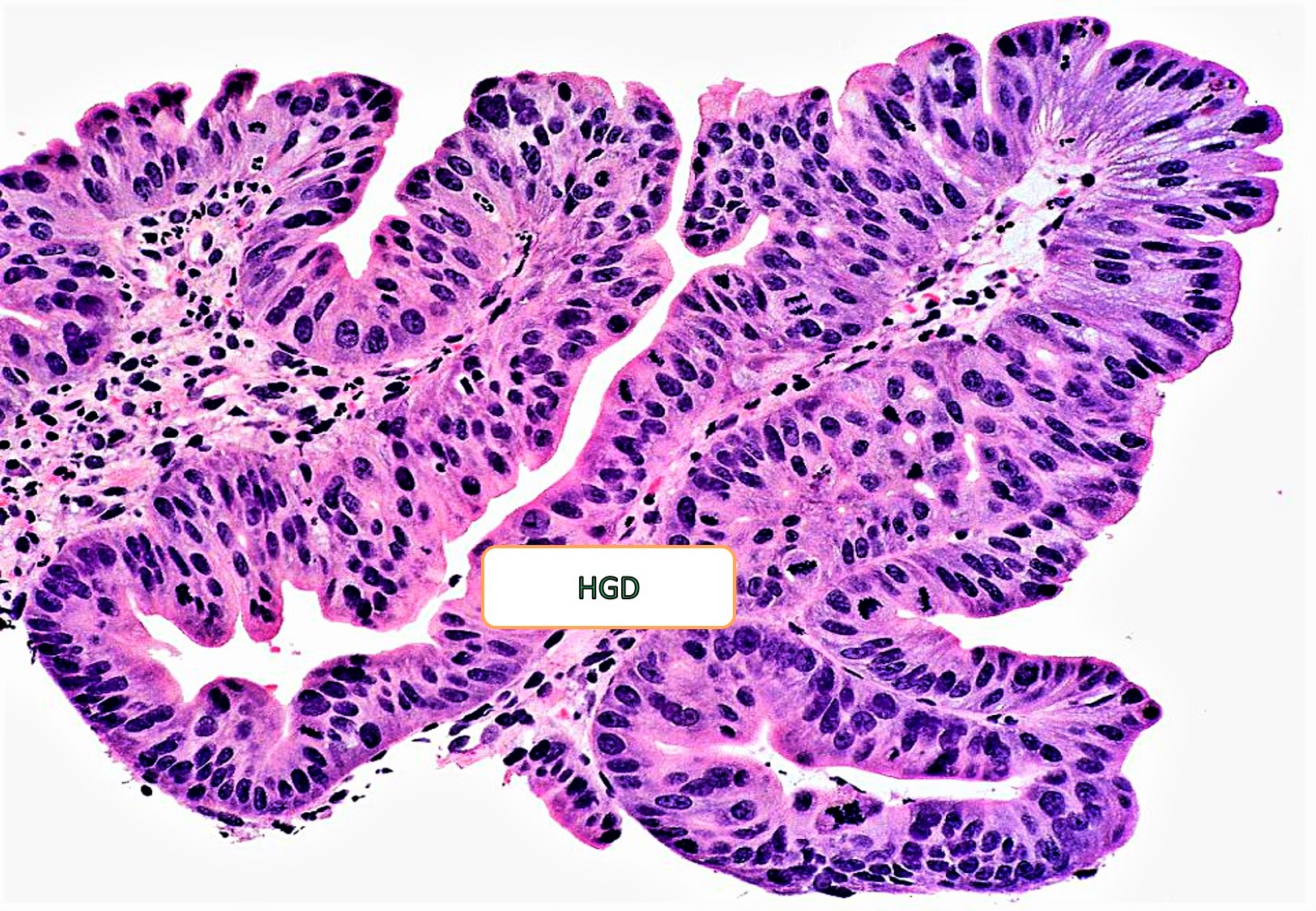
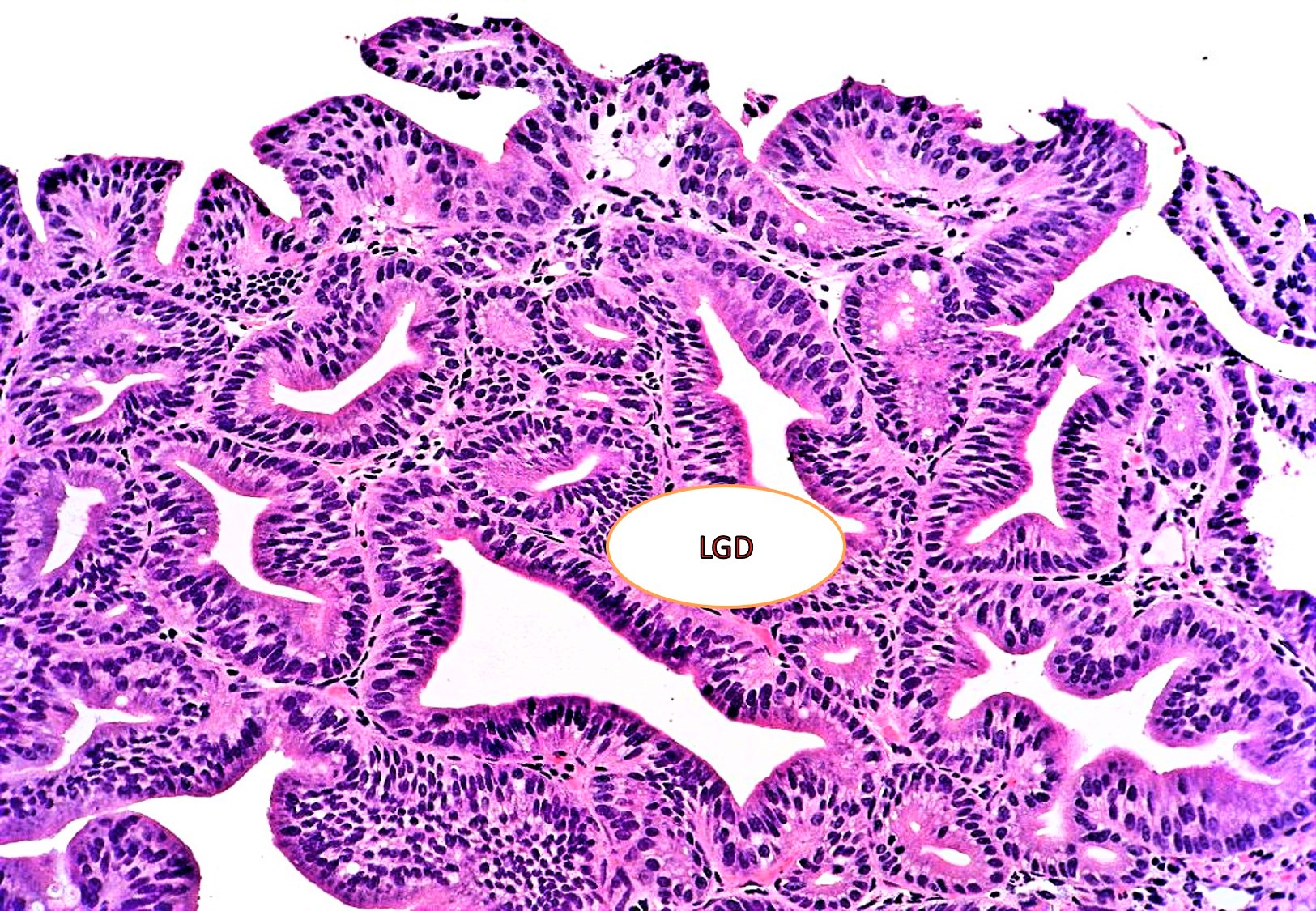
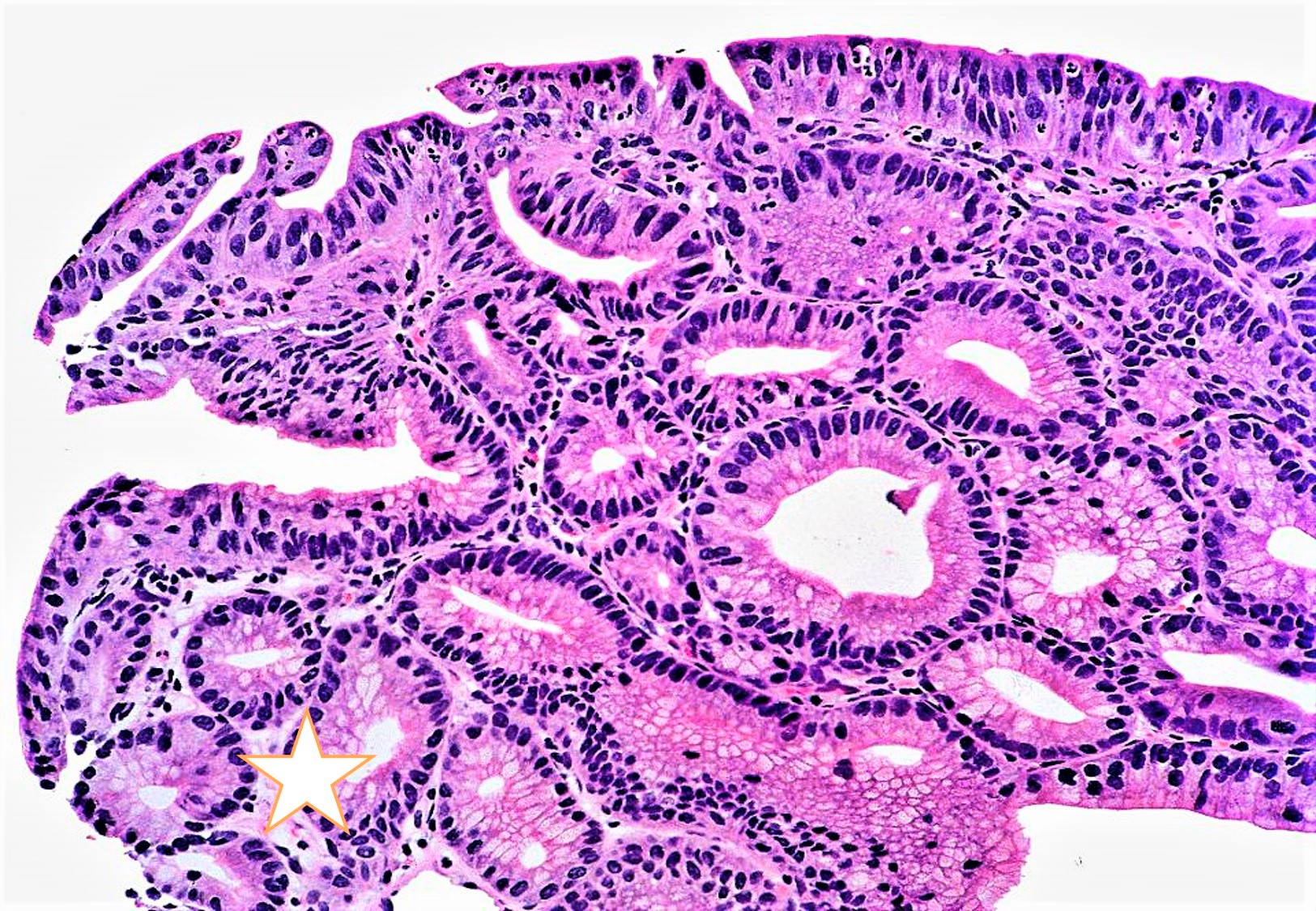
Microscopic (histologic) description
- Closely packed tubular glands (pyloric glands / pseudopyloric glands) with low cuboidal to columnar epithelium; cytoplasm is eosinophilic with ground glass appearance; round nuclei, basally located without any prominent nucleoli
- PGA can occur without dysplasia, with low grade dysplasia and with high grade dysplasia; PGA may also be associated with adenocarcinoma (12 - 47%) but submucosal invasion is observed in fewer than 10% of cases
- PGA without dysplasia: small tubular glands, closely packed, lined by bland cuboidal to columnar epithelium with basally arranged round nuclei with inconspicuous nucleoli
- PGA with low grade dysplasia: slightly irregularly arranged tubular glands with slightly elongated nuclei with mild hyperchromasia with some stratification
- PGA with high grade dysplasia: architectural distortion such as irregularly arranged occasional cribriform glands with nuclear crowding, loss of polarity, vesicular nuclei and prominent nucleoli and few mitoses
- PGA associated with adenocarcinoma: invasive irregular complex glands, loss of nuclear polarity, high nuclear:cytoplasmic ratio, vesicular nuclei with irregular nuclear membranes and numerous mitoses
Microscopic (histologic) images
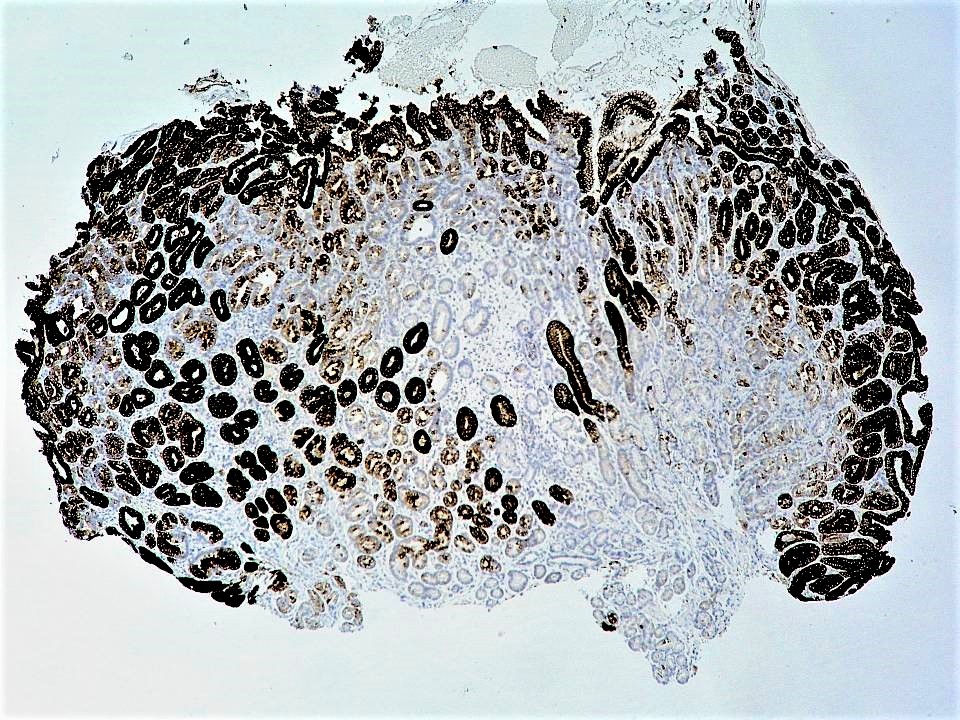
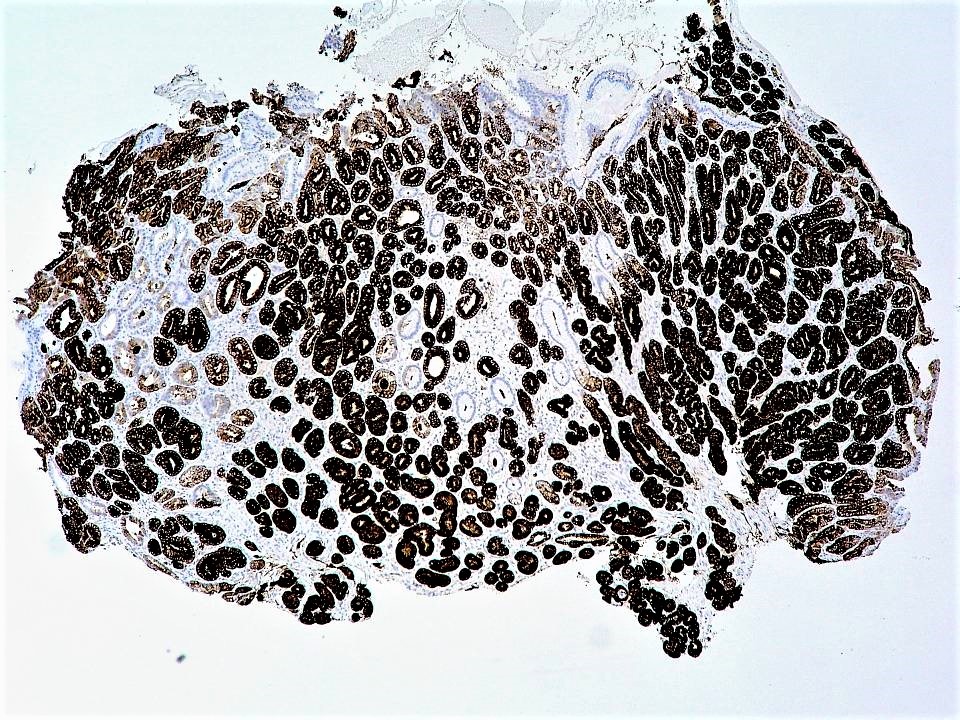
Positive stains
- Diffuse MUC6 in the deeper pyloric glands and MUC5AC in the superficial gastric glands (not limited to the surface foveolar epithelium generally)
- Concanavalin and MUC3 show similar expression as MUC6 (J Clin Pathol 2014;67:883)
- Nuclear beta catenin is also observed (Histopathology 2017;70:549)
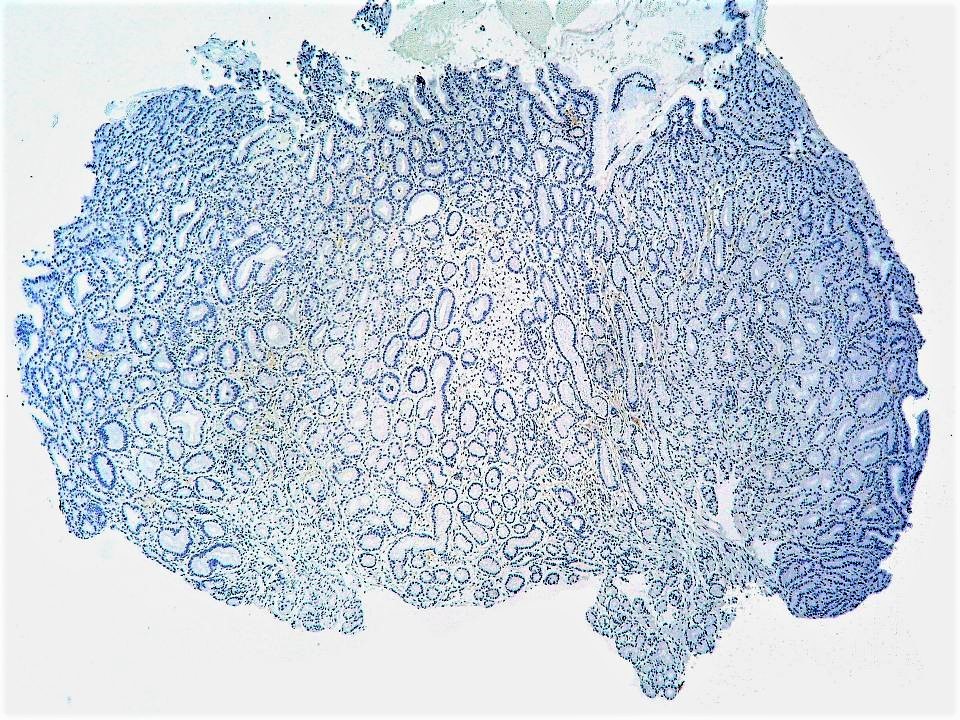
Negative stains
- MUC2 and CDX2 (generally negative but could be occasionally focally positive)
- PASD and Alcian blue negative
Molecular / cytogenetics description
- GNAS and KRAS mutations often occur in PGAs of both stomach and duodenum (J Pathol 2013;229:579)
- GNAS, KRAS and APC mutations have also been reported in sporadic and familial cases of PGA (Histopathology 2015;67:689)
- KRAS, APC, TP53 and CTNNB1 mutations may also occur in PGA without or with cytological dysplasia (Mod Pathol 2020;33:2075)
Sample pathology report
- Stomach, polypectomy:
- Pyloric gland adenoma (see comment)
- Comment: Histology shows tightly packed pyloric glands lined by cuboidal or low columnar epithelium with ground glass eosinophilic cytoplasm, basally located nuclei and absent apical mucin.
Differential diagnosis
- Hyperplastic polyp:
- Tall columnar epithelium, paler cytoplasm, apical mucin seen, irregular branching pits and edematous inflamed stroma
- Reactive foveolar hyperplasia:
- Proliferation of foveolar epithelium rather than deep pyloric glands
- Gastric foveolar type adenoma:
- Oxyntic gland adenoma:
- Arising from the oxyntic mucosa; proliferating glands show chief cell differentiation
- Pepsinogen I and II positive
Additional references
Practice question #1
A polypoid lesion of the stomach was resected in a 75 year old man. Based on the histological feature provided in the photomicrograph above, which of the following statements is correct?
- Cells have an apical mucin cap
- GNAS mutation is commonly observed
- MUC2 expression is frequent in this lesion
- TP53 mutations are commonly seen
Practice answer #1
B. KRAS and GNAS mutations are commonly seen in pyloric gland adenoma
Comment Here
Reference: Pyloric gland adenoma
Comment Here
Reference: Pyloric gland adenoma
Practice question #2
Which of the following statements is true about pyloric gland adenoma?
- It is most commonly observed in antrum of the stomach
- It is commonly observed in a background of autoimmune gastritis
- It is rarely associated with dysplasia
- PASD is extensively positive in the neoplastic glands
Practice answer #2
B. Pyloric gland adenoma is commonly observed in a background of autoimmune gastritis
Comment Here
Reference: Pyloric gland adenoma
Comment Here
Reference: Pyloric gland adenoma