22 March 2024 - Case of the Month #537
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Drs. Sherif Shabaan and Julie Jorns, Medical College of Wisconsin, Milwaukee, Wisconsin, USA for contributing this case and discussion and to Dr. Kristen Muller, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, USA for reviewing the discussion.

Case of the Month #537
Clinical history:
A 26 year old woman presented with modified Bloom Richardson grade 2 invasive ductal carcinoma and ipsilateral axillary lymph node metastasis at diagnosis. Her cancer was hormone receptor positive, HER2 equivocal (2+) on IHC but FISH non amplified and was clinically staged as cT2N1.
The patient showed partial clinical response following a neoadjuvant therapy regimen including
The patient received three doses of a granulocyte colony stimulating factor, with her last dose 40 days prior to surgery.
Sentinel lymph node excision images are shown below.
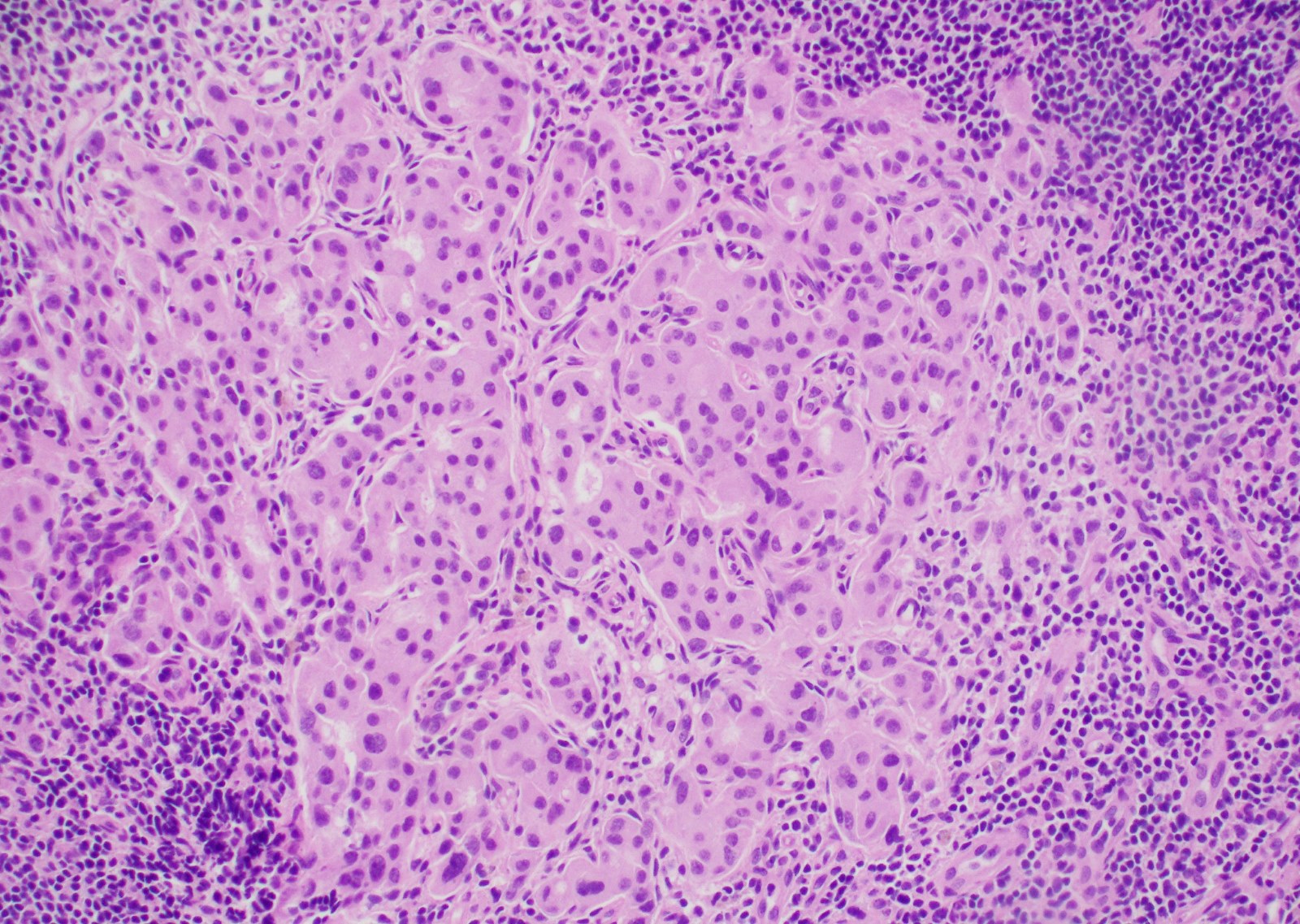
Microscopic images:
What is your diagnosis?
Diagnosis: Metastatic carcinoma and extramedullary hematopoiesis
Test question (answer at the end):
Which biomarker profile is most predictive of residual carcinoma following therapy among patients with breast cancer and ipsilateral axillary lymph node involvement prior to neoadjuvant chemotherapy?
Stains:
Discussion:
Around two thirds of all breast cancer is hormonally subtyped as hormone receptor positive (ER+ / PR+), HER2 negative. The response of this group to chemotherapy is highly variable but generally lower than in patients with other biomarker profiles, owing to their low proliferative activity (Breast Cancer Res Treat 2012;131:827).
First described by Hoda et al., sentinel lymph node extramedullary hematopoiesis may be challenging to diagnose following mastectomy and axillary nodal sampling without prior neoadjuvant chemotherapy (Microsc Res Tech 2002;59:85). Multinucleated megakaryocytes, erythroid and myeloid progenitors could potentially be mistaken for metastatic carcinoma (Pathobiology 2019;86:167) but are negative for cytokeratin immunohistochemistry.
The mechanism behind nodal extramedullary hematopoiesis in breast cancer remains unknown. However, there are many hypotheses in the literature. The differentiation of lymph node stem cells into hematopoietic cells is thought to be a response to a change in microenvironment (Arch Pathol Lab Med 1994;118:1014). This change is partly related to the use of pharmacologic drugs with some evidence for cyclophosphamide, doxorubicin and granulocyte colony stimulating factor. Moreover, doxorubicin was linked to the pathogenesis of extramedullary hematopoiesis in animal models (Toxicol Pathol 1994;22:473). Local injury, in the form of biopsy or surgery, has also been suggested to cause the production of growth factors / cytokines by inflammatory cells which may lead to extramedullary hematopoiesis (Pathobiology 2019;86:167).
Test question answer:
B. ER+/PR+/HER2-. Patients with HER2 positive breast cancer who undergo neoadjuvant chemotherapy with dual targeted anti HER2 therapy have better response (ER-/PR-/HER2+ > ER+/PR+/HER2+), followed by triple negative (ER-/PR-/HER2-) breast cancer, with luminal breast cancers (ER+/PR+/HER2-) having less chemotherapy response owing to their low proliferative activity.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Drs. Sherif Shabaan and Julie Jorns, Medical College of Wisconsin, Milwaukee, Wisconsin, USA for contributing this case and discussion and to Dr. Kristen Muller, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, USA for reviewing the discussion.

Website news:
(1) Make sure to come visit our booth at USCAP 2024 in Baltimore! We’ll be at booth #632 from March 25 - 27, 2024.
(2) New Appointment: Dr. Frido Bruehl was recently appointed to our new Board of Reviewers for Hematopathology / Hematology. Dr. Bruehl is a staff pathologist at OhioHealth in Columbus, Ohio.
(3) Read the February 2024 Curing Cancer Network newsletter in its entirety here. To sign up for this newsletter that comes out every 1 - 2 months, visit lp.constantcontactpages.com/su/onz6IND.
Visit and follow our Blog to see recent updates to the website.
(1) Make sure to come visit our booth at USCAP 2024 in Baltimore! We’ll be at booth #632 from March 25 - 27, 2024.
(2) New Appointment: Dr. Frido Bruehl was recently appointed to our new Board of Reviewers for Hematopathology / Hematology. Dr. Bruehl is a staff pathologist at OhioHealth in Columbus, Ohio.
(3) Read the February 2024 Curing Cancer Network newsletter in its entirety here. To sign up for this newsletter that comes out every 1 - 2 months, visit lp.constantcontactpages.com/su/onz6IND.
Visit and follow our Blog to see recent updates to the website.
Case of the Month #537
Clinical history:
A 26 year old woman presented with modified Bloom Richardson grade 2 invasive ductal carcinoma and ipsilateral axillary lymph node metastasis at diagnosis. Her cancer was hormone receptor positive, HER2 equivocal (2+) on IHC but FISH non amplified and was clinically staged as cT2N1.
The patient showed partial clinical response following a neoadjuvant therapy regimen including
- Anti PD1 therapy (as part of a clinical trial)
- Taxane (microtubule inhibitor)
- Adriamycin / Doxorubicin & Cyclophosphamide (AC regimen)
The patient received three doses of a granulocyte colony stimulating factor, with her last dose 40 days prior to surgery.
Sentinel lymph node excision images are shown below.
Microscopic images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Metastatic carcinoma and extramedullary hematopoiesis
Test question (answer at the end):
Which biomarker profile is most predictive of residual carcinoma following therapy among patients with breast cancer and ipsilateral axillary lymph node involvement prior to neoadjuvant chemotherapy?
- ER+/PR+/HER2+
- ER+/PR+/HER2-
- ER-/PR-/HER2+
- ER-/PR-/HER2-
Stains:
Discussion:
Around two thirds of all breast cancer is hormonally subtyped as hormone receptor positive (ER+ / PR+), HER2 negative. The response of this group to chemotherapy is highly variable but generally lower than in patients with other biomarker profiles, owing to their low proliferative activity (Breast Cancer Res Treat 2012;131:827).
First described by Hoda et al., sentinel lymph node extramedullary hematopoiesis may be challenging to diagnose following mastectomy and axillary nodal sampling without prior neoadjuvant chemotherapy (Microsc Res Tech 2002;59:85). Multinucleated megakaryocytes, erythroid and myeloid progenitors could potentially be mistaken for metastatic carcinoma (Pathobiology 2019;86:167) but are negative for cytokeratin immunohistochemistry.
The mechanism behind nodal extramedullary hematopoiesis in breast cancer remains unknown. However, there are many hypotheses in the literature. The differentiation of lymph node stem cells into hematopoietic cells is thought to be a response to a change in microenvironment (Arch Pathol Lab Med 1994;118:1014). This change is partly related to the use of pharmacologic drugs with some evidence for cyclophosphamide, doxorubicin and granulocyte colony stimulating factor. Moreover, doxorubicin was linked to the pathogenesis of extramedullary hematopoiesis in animal models (Toxicol Pathol 1994;22:473). Local injury, in the form of biopsy or surgery, has also been suggested to cause the production of growth factors / cytokines by inflammatory cells which may lead to extramedullary hematopoiesis (Pathobiology 2019;86:167).
Test question answer:
B. ER+/PR+/HER2-. Patients with HER2 positive breast cancer who undergo neoadjuvant chemotherapy with dual targeted anti HER2 therapy have better response (ER-/PR-/HER2+ > ER+/PR+/HER2+), followed by triple negative (ER-/PR-/HER2-) breast cancer, with luminal breast cancers (ER+/PR+/HER2-) having less chemotherapy response owing to their low proliferative activity.