Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Alexiev BA. Giant cell tumor of bone, NOS. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonegiantcelltumor.html. Accessed September 5th, 2025.
Definition / general
- Giant cell tumor of bone (GCTB) is a locally aggressive and rarely metastasizing neoplasm composed of neoplastic mononuclear stromal cells admixed with macrophages and osteoclast-like giant cells
- A small subset of cases are malignant
Essential features
- Bone tumor with compatible imaging
- Osteolytic circumscribed tumor involving the epiphysis and metaphysis, generally in skeletally mature individual
- Mononuclear cell neoplastic component without atypia together with numerous osteoclasts
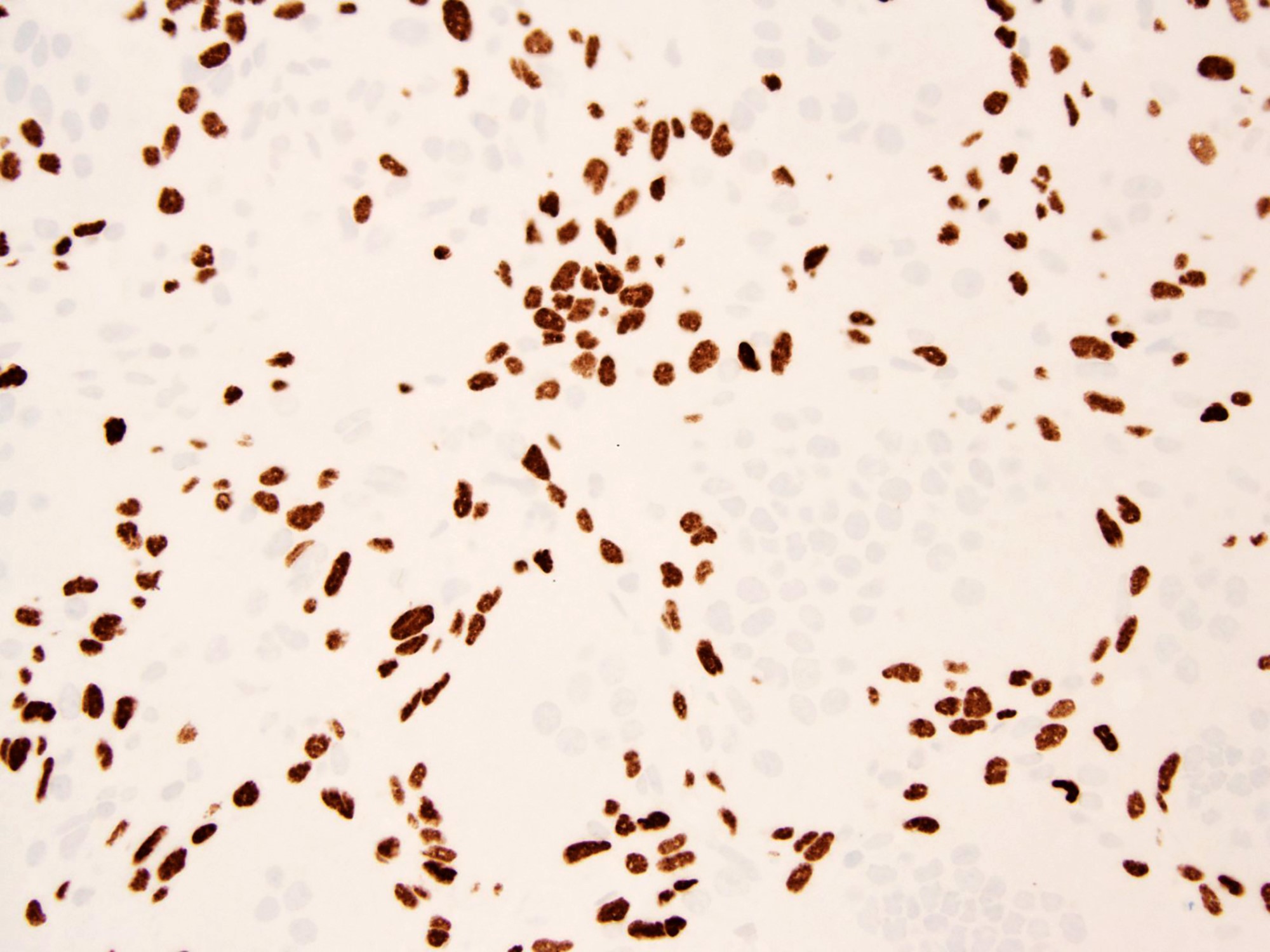
- Detection of H3.3 pGly34 mutated cells / H3.3 pGly34Trp (G34W) immunoreactivity
Terminology
- Not recommended: osteoclastoma
ICD coding
- ICD-10: 9250/1 - giant cell tumor of bone NOS
- ICD-11: 2F7B & XH4TC2 - neoplasms of uncertain behavior of bone or articular cartilage & giant cell tumor of bone NOS
Epidemiology
- GCTBs constitute 5% of all primary bone tumors (World Neurosurg 2020;144:e296)
- Annual incidence in the United States: 1.6 per 10,000,000 persons per year (Rare Tumors 2009;1:e52)
- Male to female ratio of 1:1.38 (Acta Orthop 2018;89:570)
- Median age of 35 years (Acta Orthop 2018;89:570)
- GCTB arising in the pediatric population is rare (Am J Surg Pathol 2016;40:1702)
- No differences in localization according to age and sex were found (Acta Orthop 2018;89:570)
Sites
- Tumor typically involves the metaphysis and the epiphysis of long bones (J Bone Joint Surg Am 1987;69:106)
- Distal femur and proximal tibia are the most common sites but the distal radius and proximal humerus are not uncommonly affected (Am J Surg Pathol 2017;41:1059, Acta Orthop 2018;89:570)
- In the axial skeleton, the proximal sacrum is the most common location but GCTB can occur in almost any bone, including the small bones of the hands and feet and sesamoid bones, such as the patella (Am J Surg Pathol 2017;41:1059)
Pathophysiology
- GCTB related clonal aberrations occur in a background of epigenetic histone modifications (especially the G34W mutation of H3F3A gene) (Hum Pathol 2018;81:1)
- Neoplastic mononuclear stromal cells in GCTB express receptor activator of NFκβ ligands (RANKLs) and various chemokines and cytokines associated with monocyte recruitment and reactive multinucleated giant cells (osteoclastogenesis) (Hum Pathol 2018;81:1)
- Activation of Wnt / beta catenin pathway in GCTB tumorigenesis (Pathol Res Pract 2009;205:626)
- Clonal telomeric associations (tas) were found in GCTB (Genes Chromosomes Cancer 2009;48:583)
- Transformation to malignancy may occur after therapeutic irradiation (Indian J Pathol Microbiol 2002;45:273)
- TP53 and HRAS mutations have been identified in malignant GCTB not associated with prior radiation (Histopathology 2001;39:629)
Etiology
- Etiology of sporadic GCTB is not known
- Pheochromocytoma paraganglioma and GCTB syndrome is caused by postzygotic G34W mutation of the histone 3.3 gene, H3F3A (Endocrinol Metab Clin North Am 2017;46:459)
- Patients with Paget bone disease have an increased risk of developing multifocal GCTB (J Bone Miner Res 2015;30:257)
- Gorlin-Goltz syndrome has occasionally been associated with GCTB (Pediatr Dev Pathol 2013;16:308, Genet Couns 2014;25:445)
Clinical features
- GCTB present with pain, swelling and occasionally restricted joint movement
- Pathological fracture occurs in 5 - 12% of patients (J Bone Joint Surg Am 1987;69:106, Orthop Clin North Am 2006;37:35)
- Vertebral and sacral tumors present with lower back pain, frequent radiation to the legs and sometimes with bladder, rectal or sexual dysfunction (Orthop Clin North Am 2006;37:35, Eur Spine J 2014;23:1949)
Diagnosis
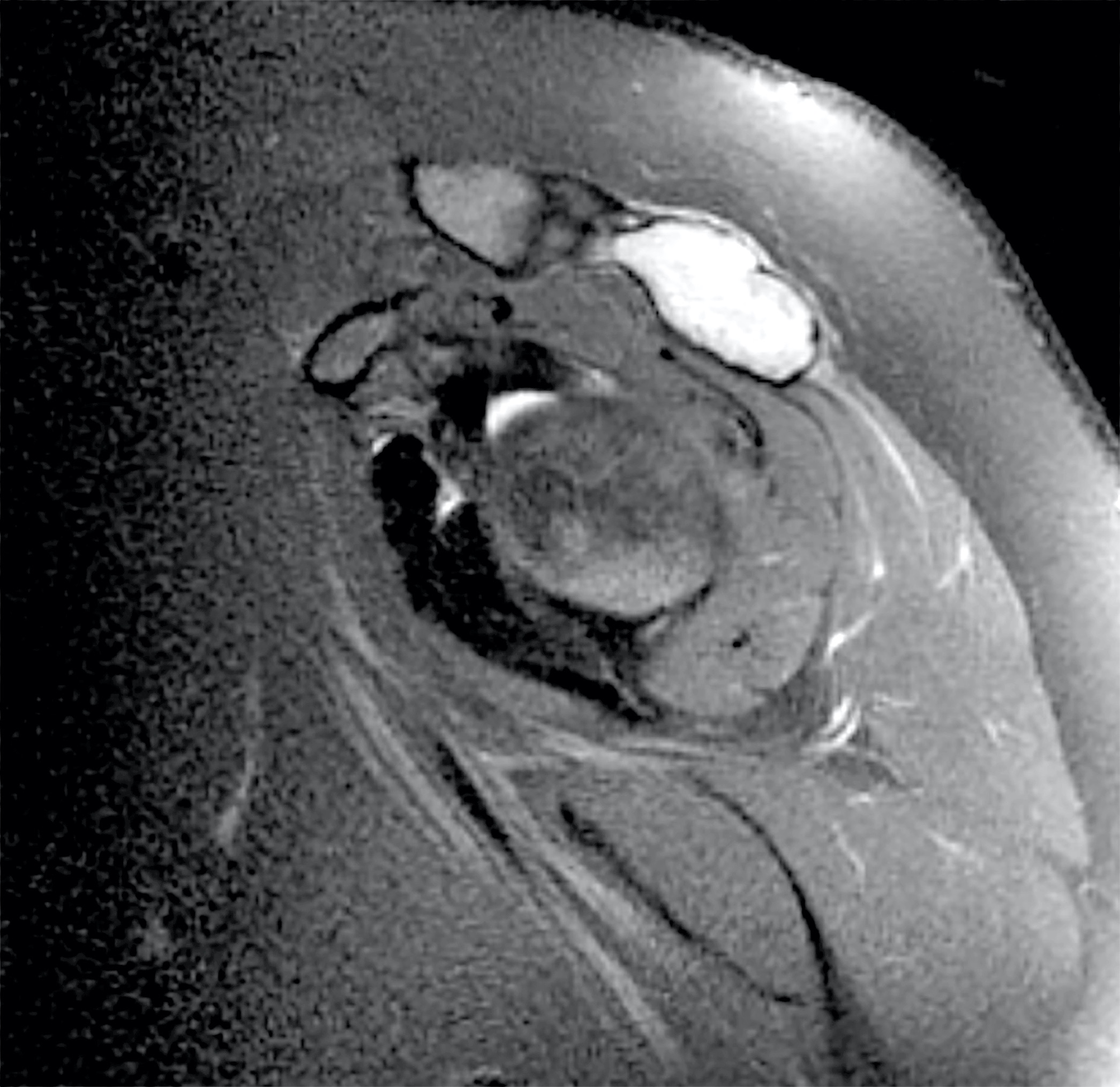
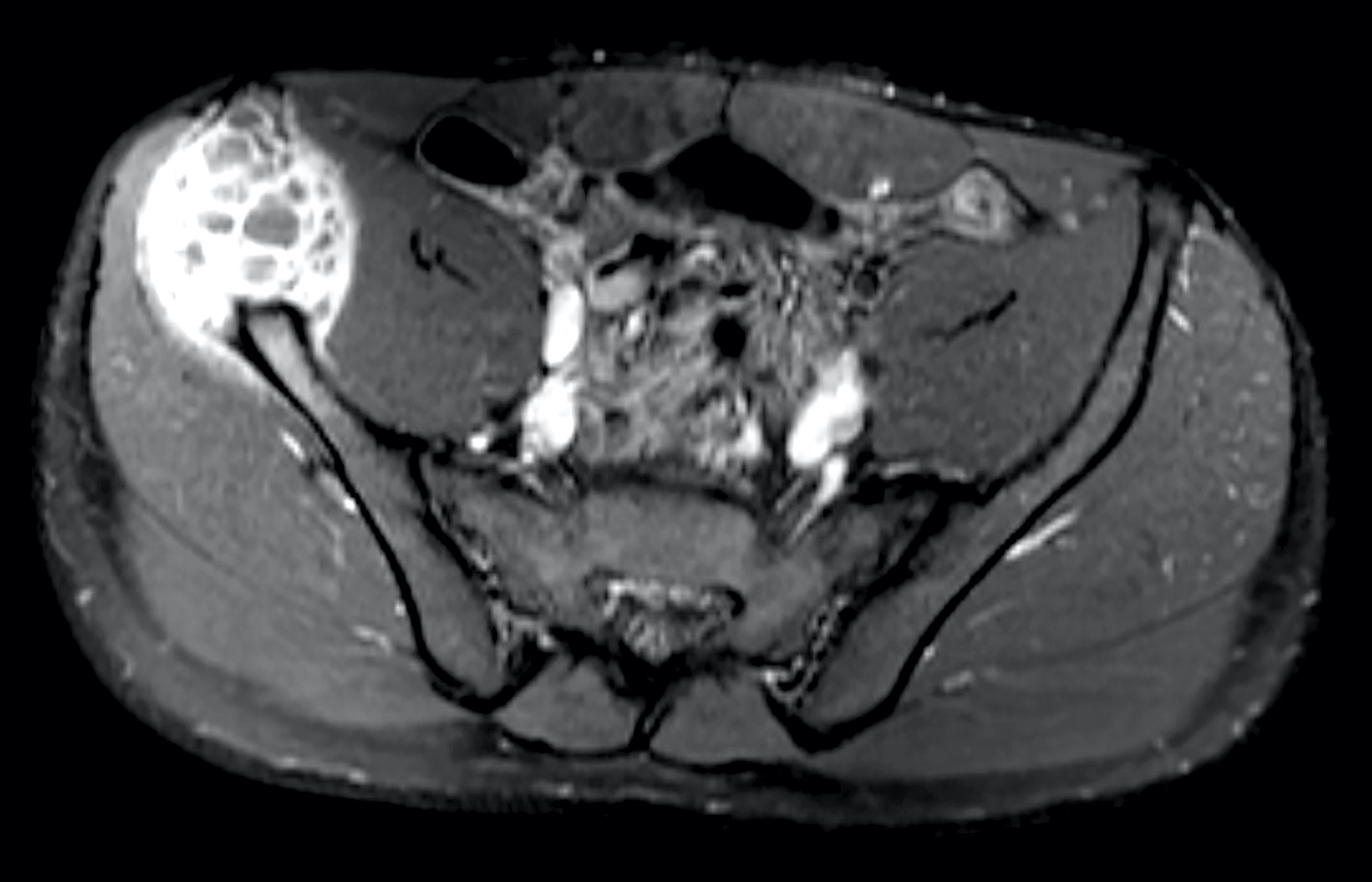
- In many cases, the diagnosis of GCTB is suggested by the tumor location and appearance on Xray, computed tomography and magnetic resonance scans
- A definitive diagnosis usually requires a biopsy
Radiology description
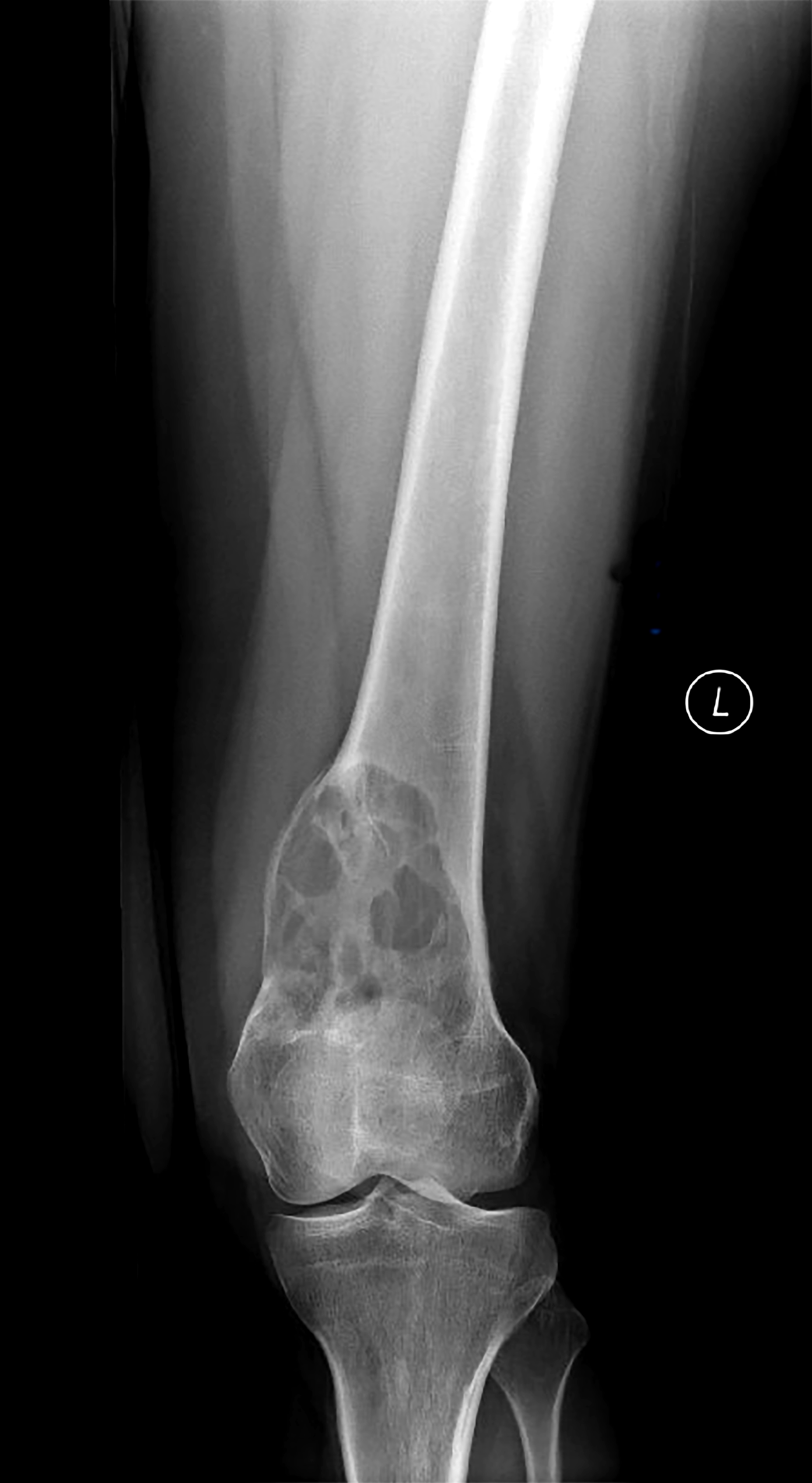
- Typical appearance of GCTB is best demonstrated on conventional radiographs, which show a lytic lesion that has a well defined but nonsclerotic margin, is eccentric in location, extends to the subchondral bone and occurs in patients with closed physes (Radiographics 2013;33:197)
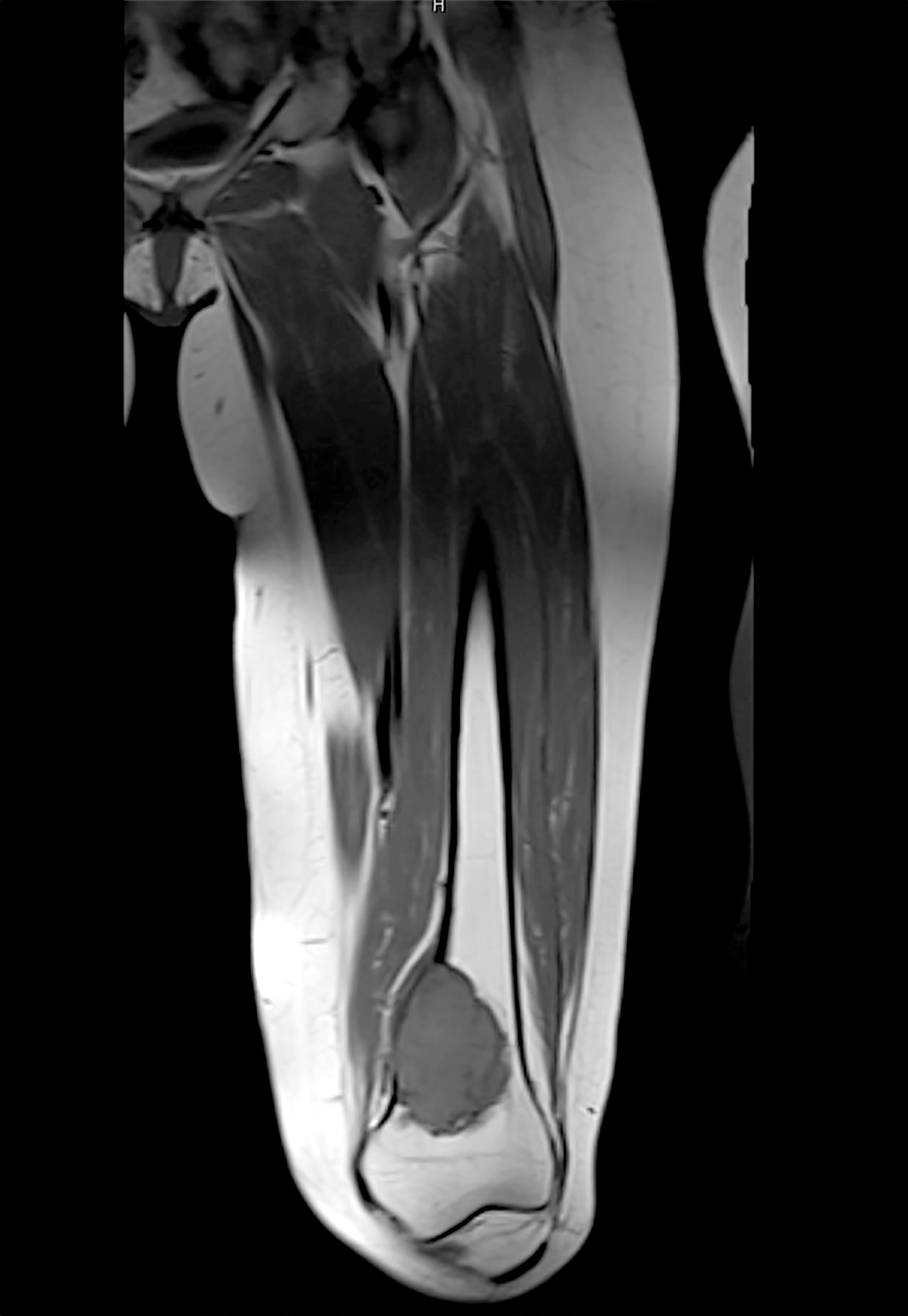
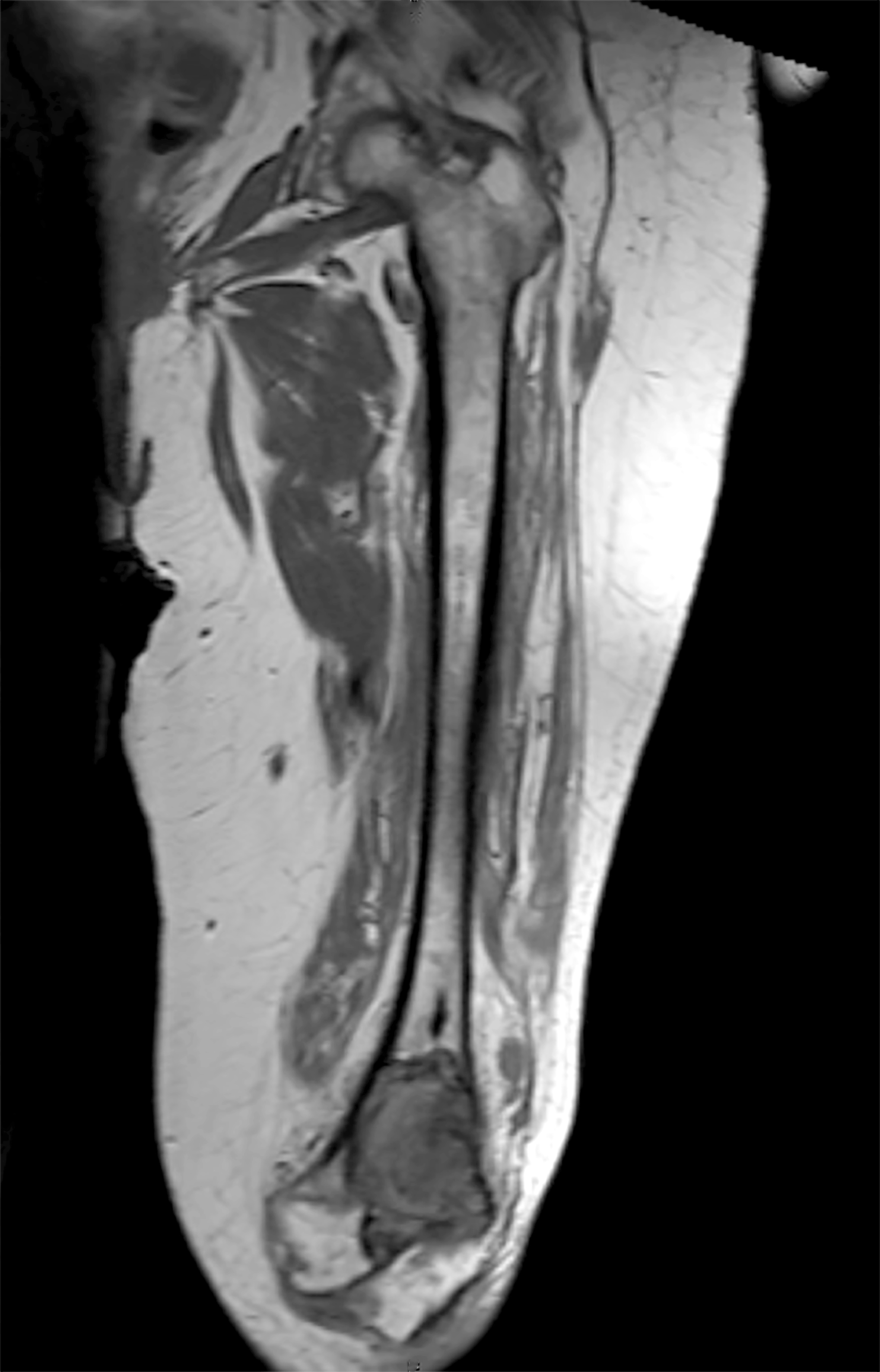
- CT and MR imaging allow superior delineation of GCTB
- Cortical thinning of bone is invariably apparent at radiography performed at clinical presentation (Radiographics 2001;21:1283)
- Expansile remodeling of bone is also frequently seen (47 - 60% of cases)
- Cortical penetration is seen in 33 - 50% of cases, often with an associated soft tissue mass (Radiographics 2001;21:1283)
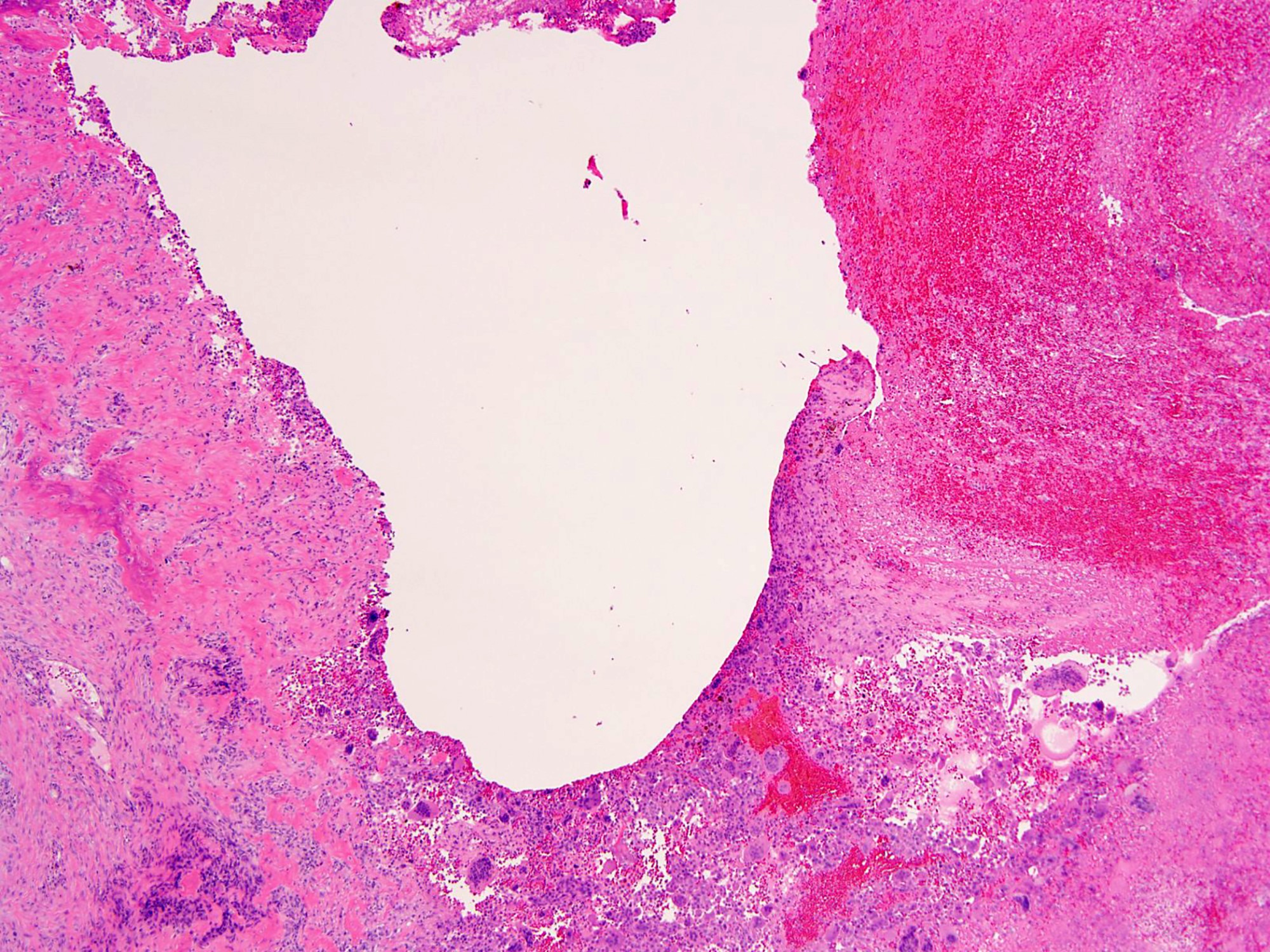
- Aneurysmal bone cyst components in GCTB are relatively common (14% of lesions)
- Campanacci et al classified the GCTB into 3 grades, depending on their radiographic appearance:
- Grade 1 lesion (latent) has a well defined margin and an intact cortex (J Bone Joint Surg Am 1987;69:106)
- Grade 2 lesion (active) has a relatively well defined margin but no radiopaque rim and the cortex is thinned and moderately expanded
- Grade 3 lesion (aggressive) has indistinct borders and cortical destruction
- It has been suggested that the Campanacci classification scheme may more easily guide treatment; however, it is doubtful whether this classification accurately predicts the aggressiveness of GCTB (SICOT J 2017;3:54)
- No correlation exists between the grading system and incidence of local recurrence and metastases (SICOT J 2017;3:54, Int Orthop 2012;36:2521)
Radiology images
Prognostic factors
- Pulmonary metastasis in ~2% of cases; they are very slow growing (nonaggressive) and may spontaneously regress; metastases have same morphology as the bone lesion (Pathol Int 1998;48:723)
- Local recurrence, a high Campanacci grade and curettage are possible high risk factors for pulmonary metastasis (J Bone Oncol 2017;7:23)
- Secondary malignancy in giant cell tumor of bone (arising after treatment of a benign giant cell tumor) has a poor prognosis, akin to other high grade sarcomas and much worse than primary malignancy in giant cell tumor of bone (Cancer 2003;97:2520)
Case reports
- 19 year old woman with tumor of T7 vertebral body (Surg Neurol 2009;71:228)
- 36 year old man with mass involving the twelfth thoracic spine (Orthopedics 2012;35:e453)
- 37 year old man with femoral neck tumor (Trauma Case Rep 2019;22:100216)
- 43 year old man with C5 tumor (Asian Spine J 2016;10:553)
- 47 year old woman with a tumor at the T5 level (J Neurosurg Spine 2007;6:600)
Treatment
- Preferential treatment is curettage and high speed drilling with local adjuvants (Curr Opin Oncol 2020;32:332, Eur J Cancer 2017;77:75)
- In more advanced cases, when joint salvage is regarded impossible, en bloc resection and endoprosthetic joint replacement is often considered
- Denosumab, a human monoclonal antibody directed against the receptor activator of nuclear factor kappa B ligand (RANK), is a highly effective treatment option for patients with advanced GCTB (Curr Opin Oncol 2020;32:332, Histopathology 2018;72:914)
- Bisphosphonates are the only systemic adjuvant directly affecting neoplastic cells (Curr Opin Oncol 2020;32:332)
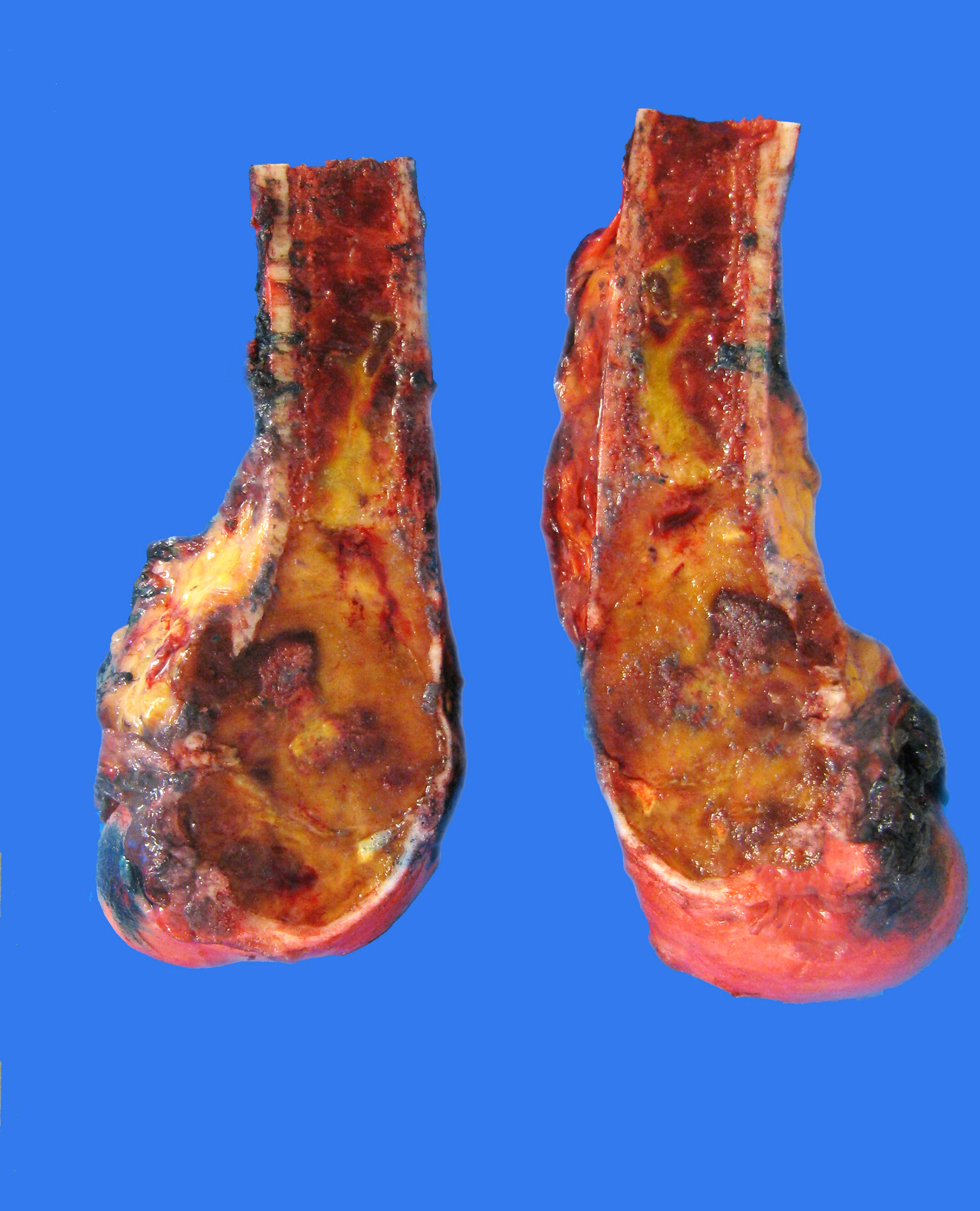
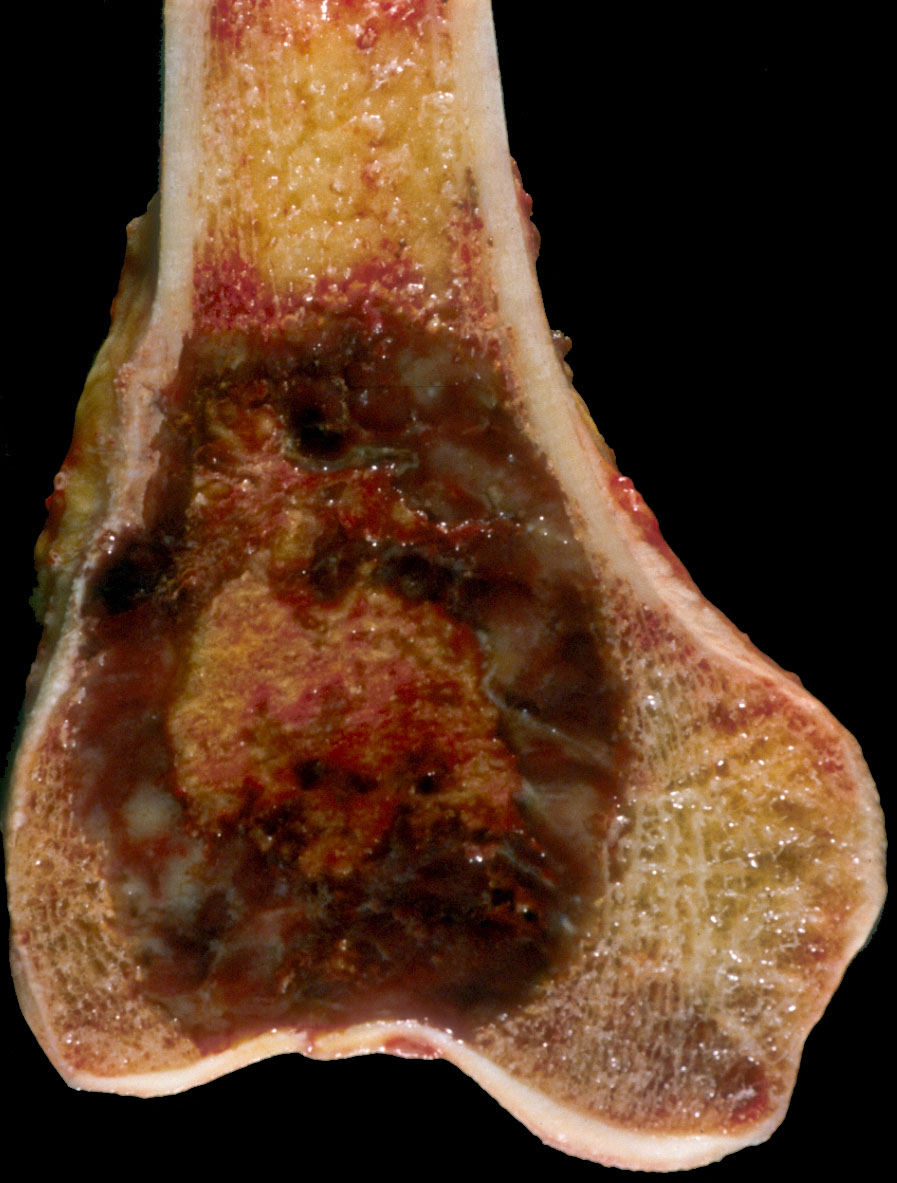
Gross description
- Typical gross lesion is a soft, friable, slightly brownish or red-tan, somewhat poorly defined neoplasm in the end of a long bone (AJR Am J Roentgenol 1985;144:955, Arch Bone Jt Surg 2016;4:2, Diagn Pathol 2014;9:111)
- Yellow and firm white areas corresponding to xanthomatous change and fibrous tissue are common
- Surrounding cortex is often thinned and may be destroyed completely
- Destructive tumors may extend into soft tissue
- Subchondral bone plate can be focally involved
- Extensive cystic hemorrhagic areas corresponding to aneurysmal bone cyst-like changes may be seen
- Cut surface of malignant GCTB is typically firm and fleshy
Gross images
Frozen section description
- Highly cellular lesion composed of large number of osteoclast-like giant cells, between which mononuclear cells are embedded (Int Orthop 2006;30:484, Diagn Pathol 2014;9:111)
- Due to the complex histological composition of GCTB, differential diagnosis is required to exclude the diagnosis of other lesions also containing giant cells, such as aneurysmal bone cyst, nonossifying fibroma, chondroblastoma, brown tumor of hyperparathyroidism and giant cell rich osteosarcoma (Int Orthop 2006;30:484)
- In addition to the histological findings, precise details regarding age, localization and radiology findings within the framework of GCTB differential diagnosis is vital (Int Orthop 2006;30:484)
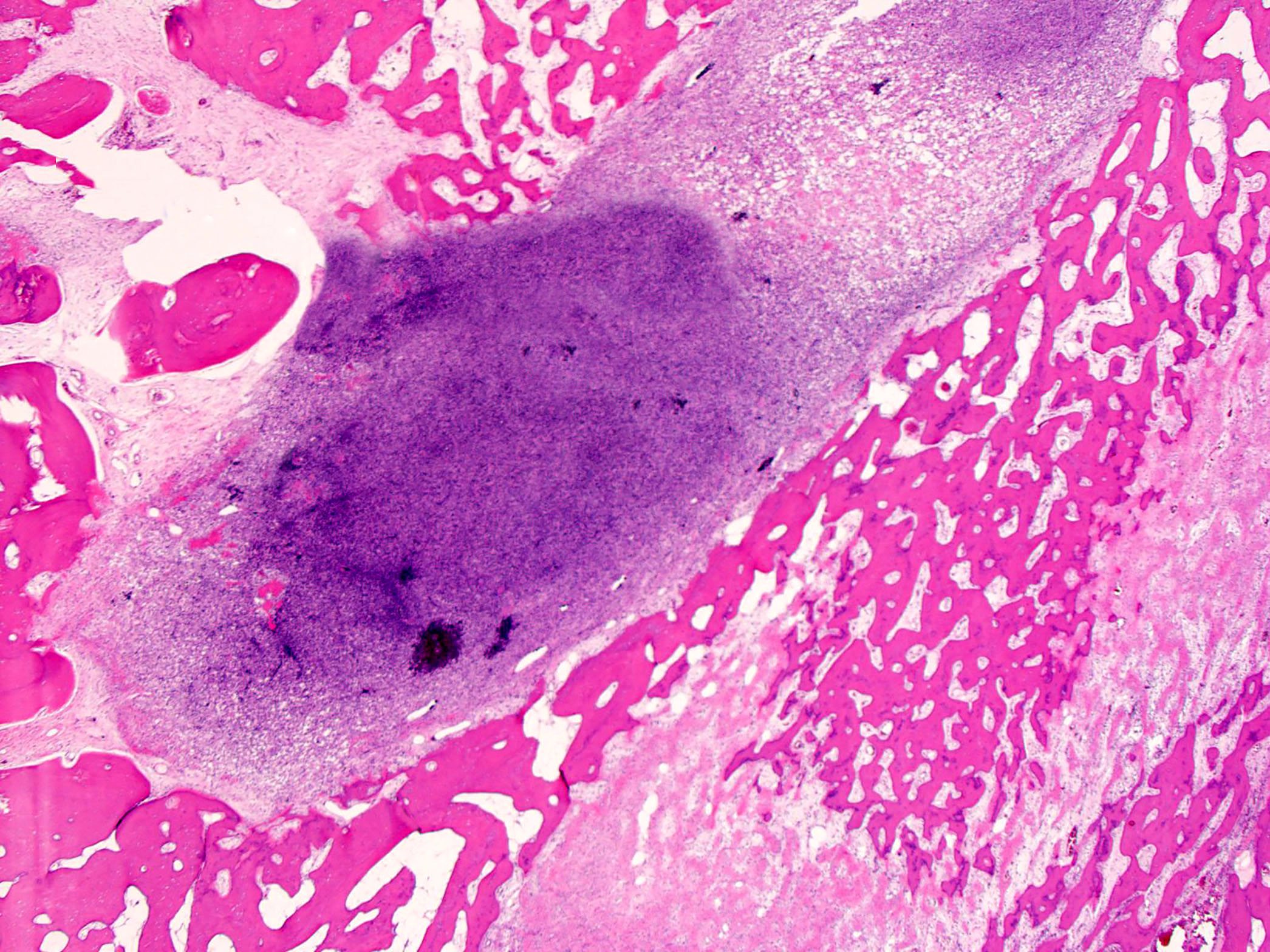
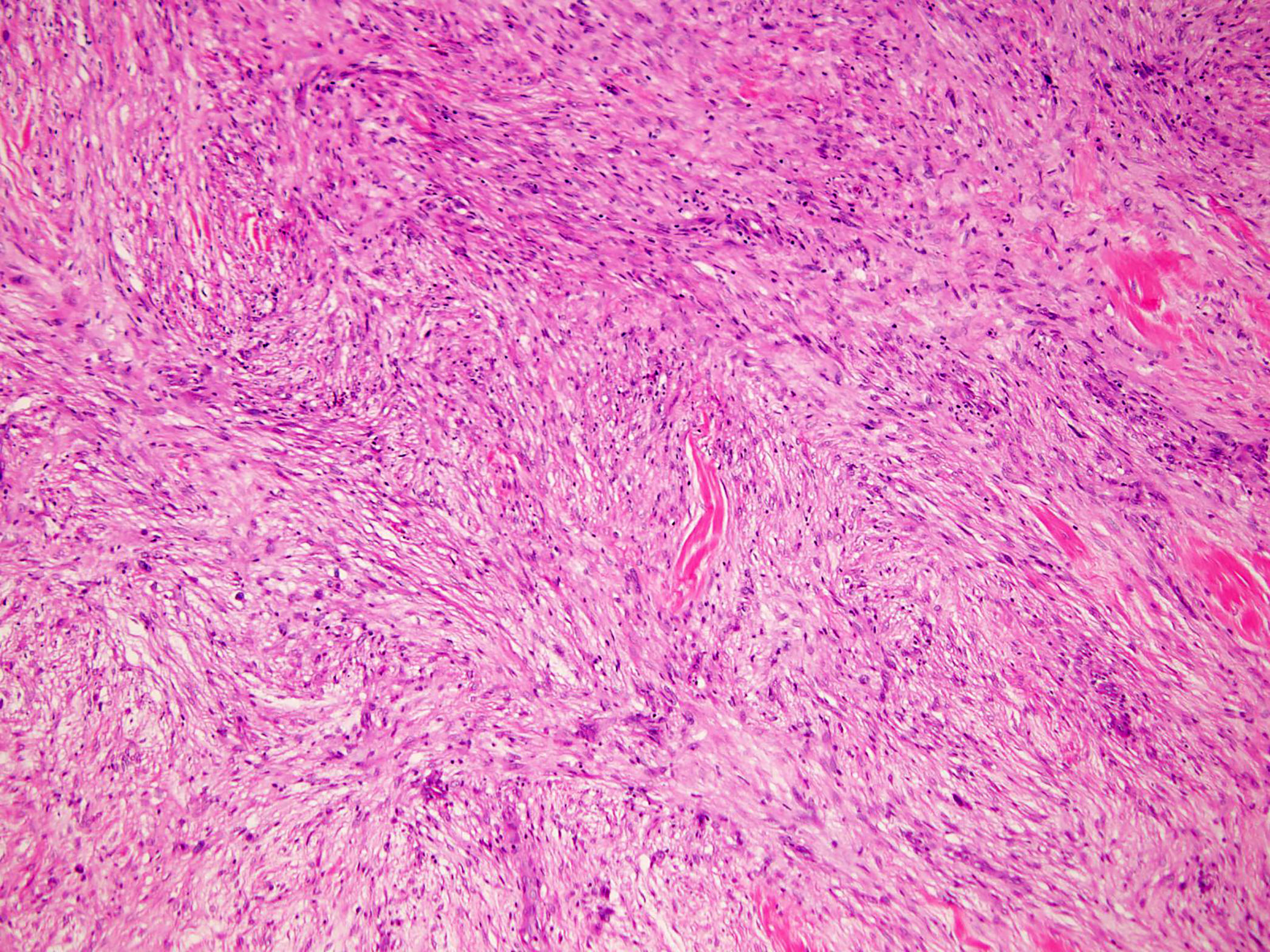
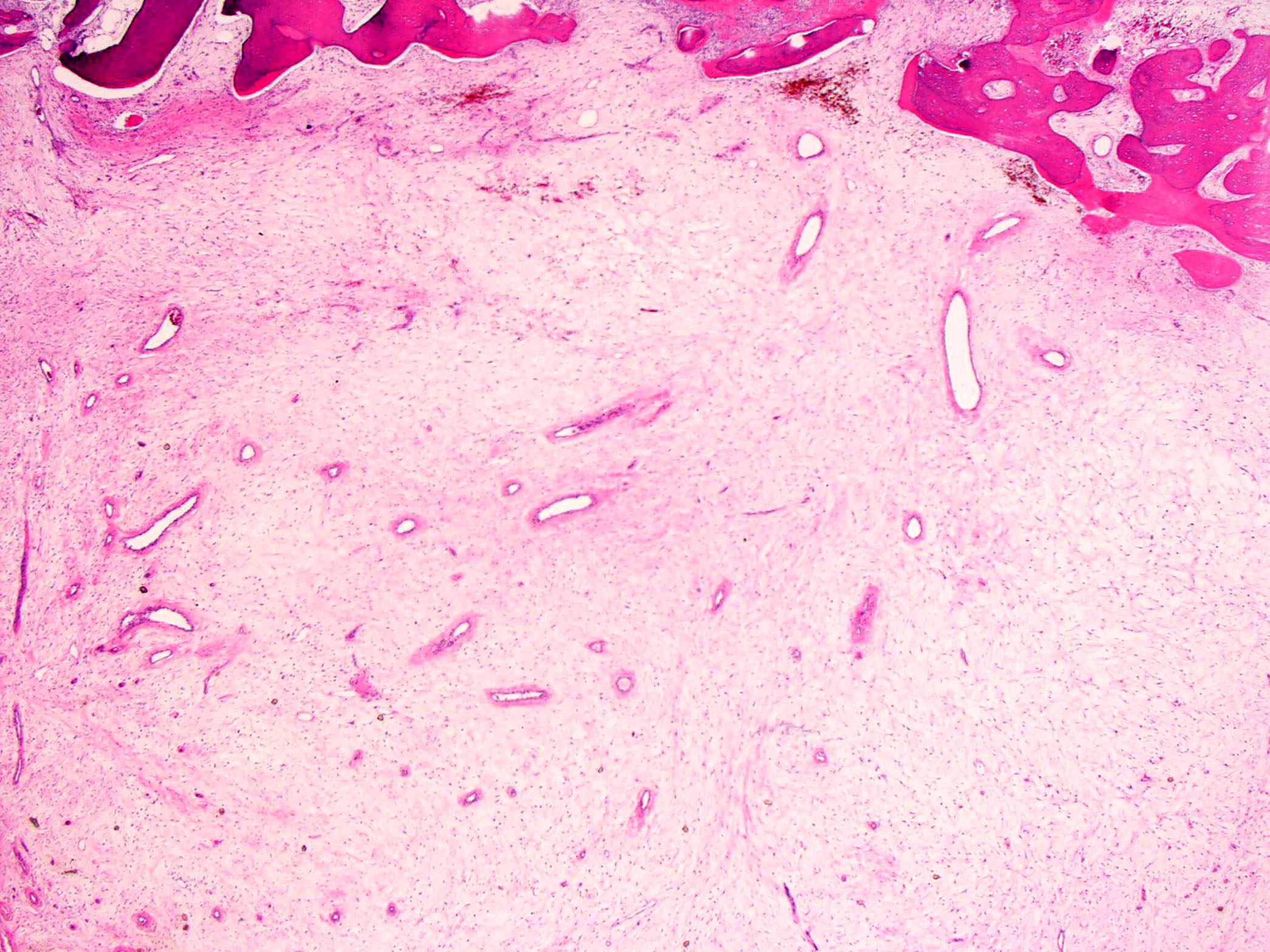
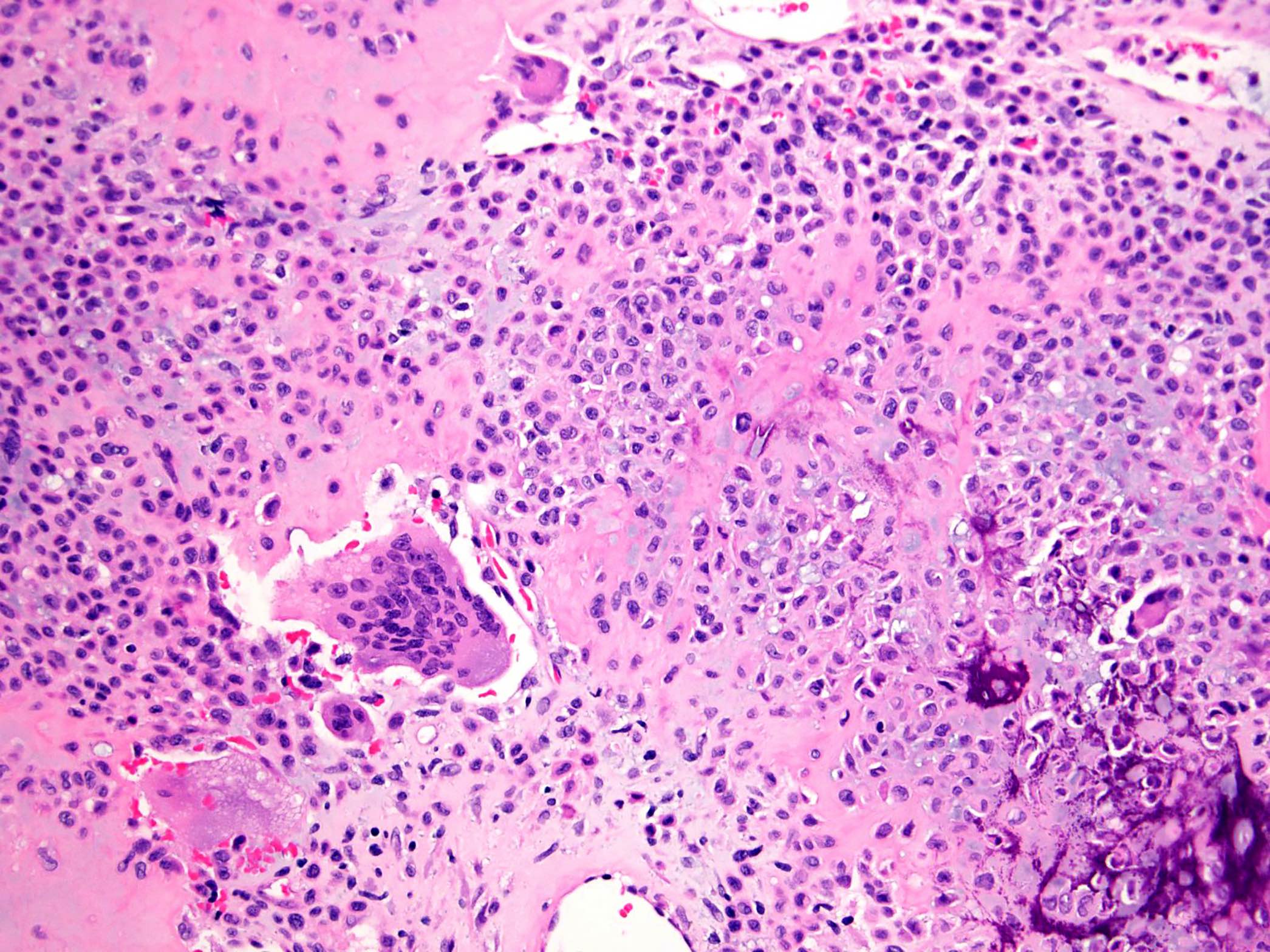
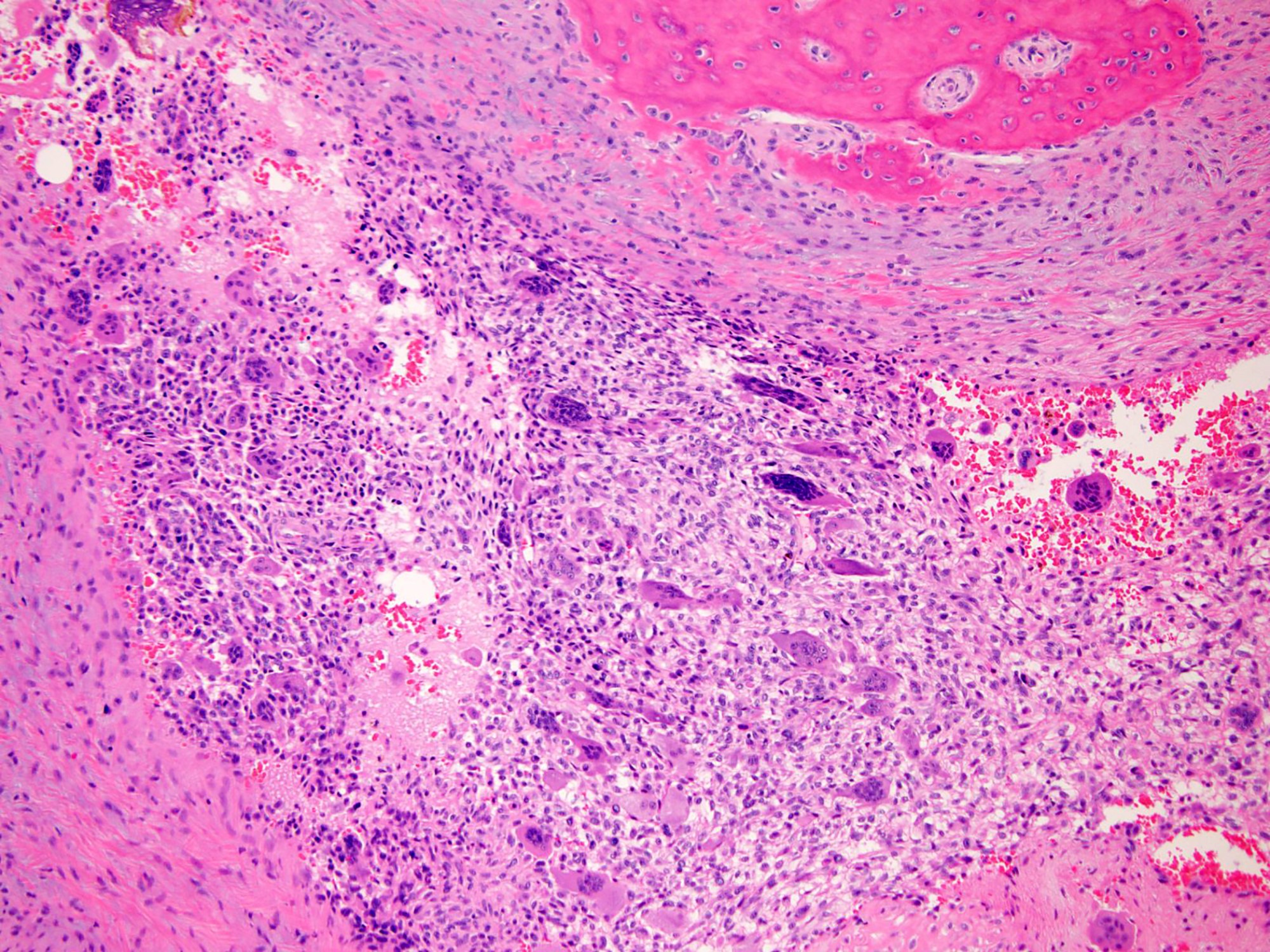
Microscopic (histologic) description
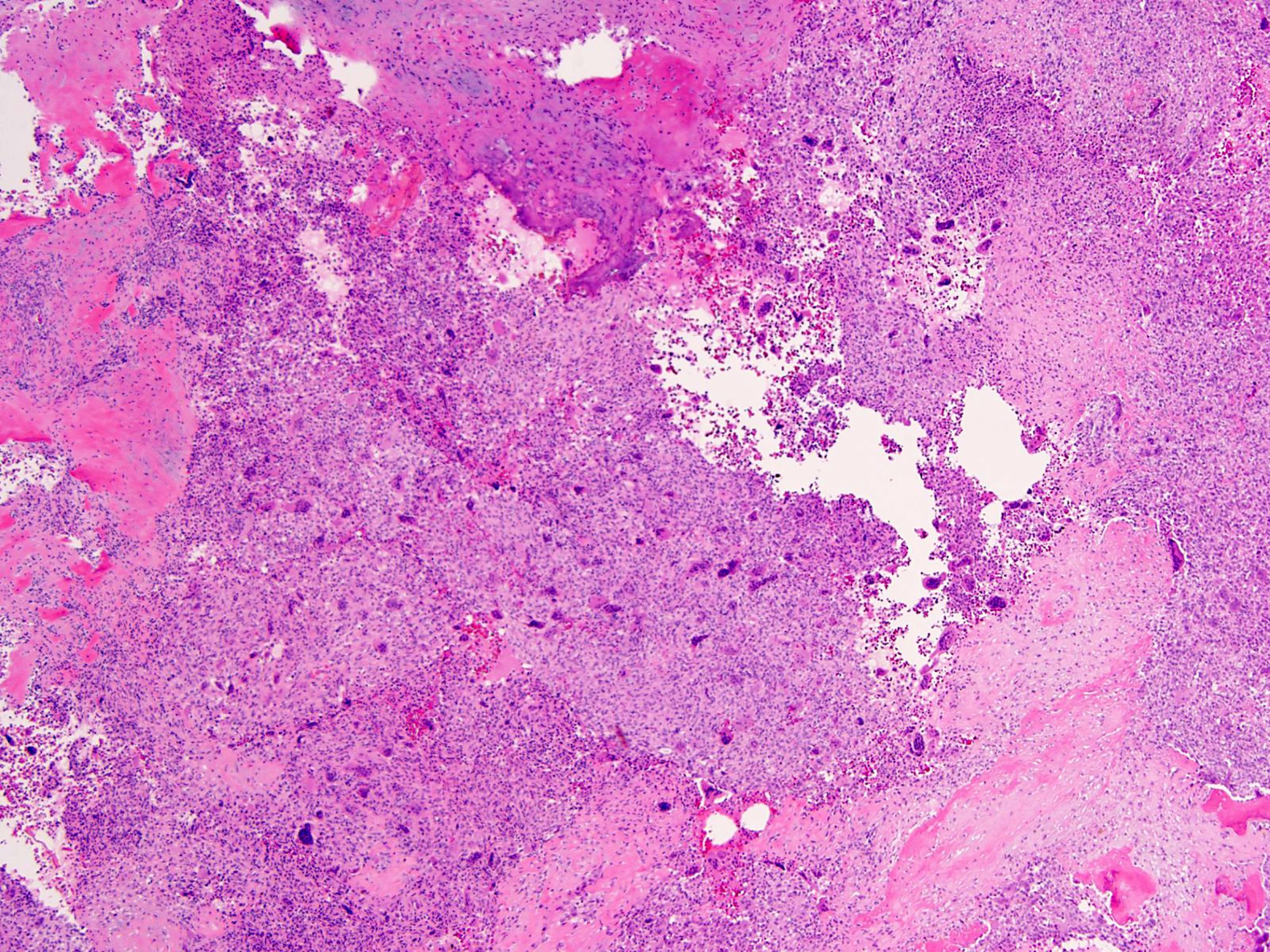
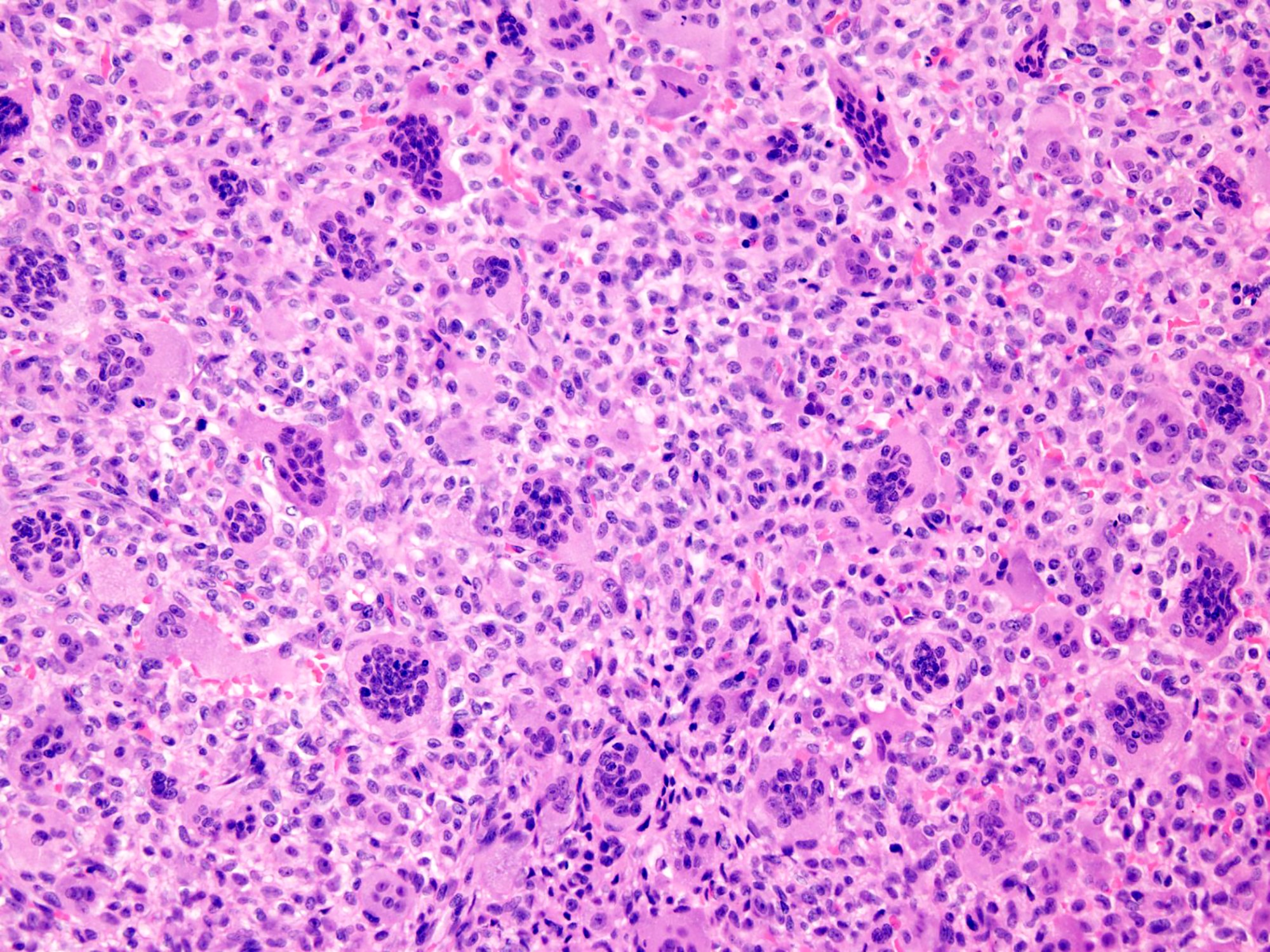
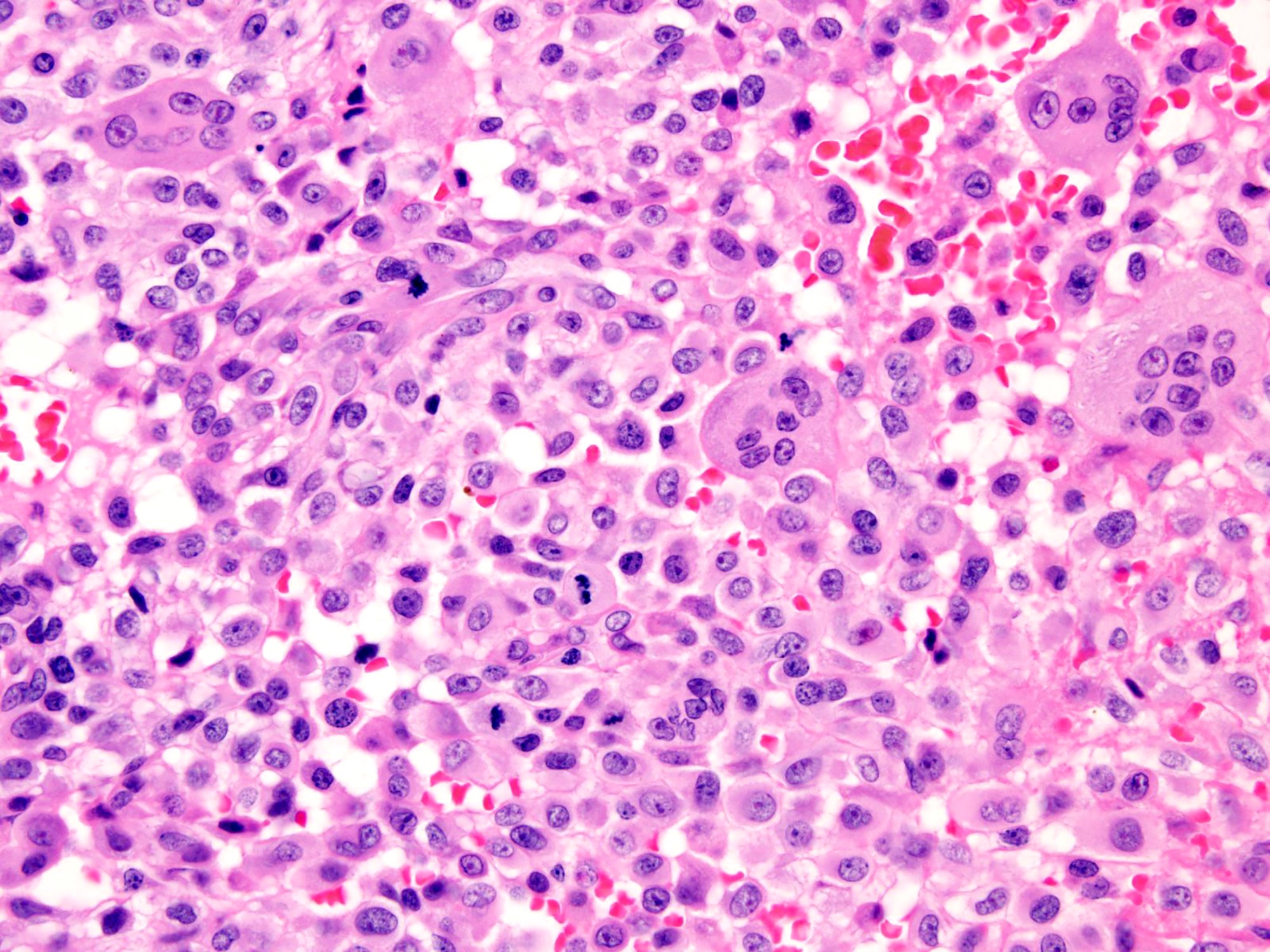
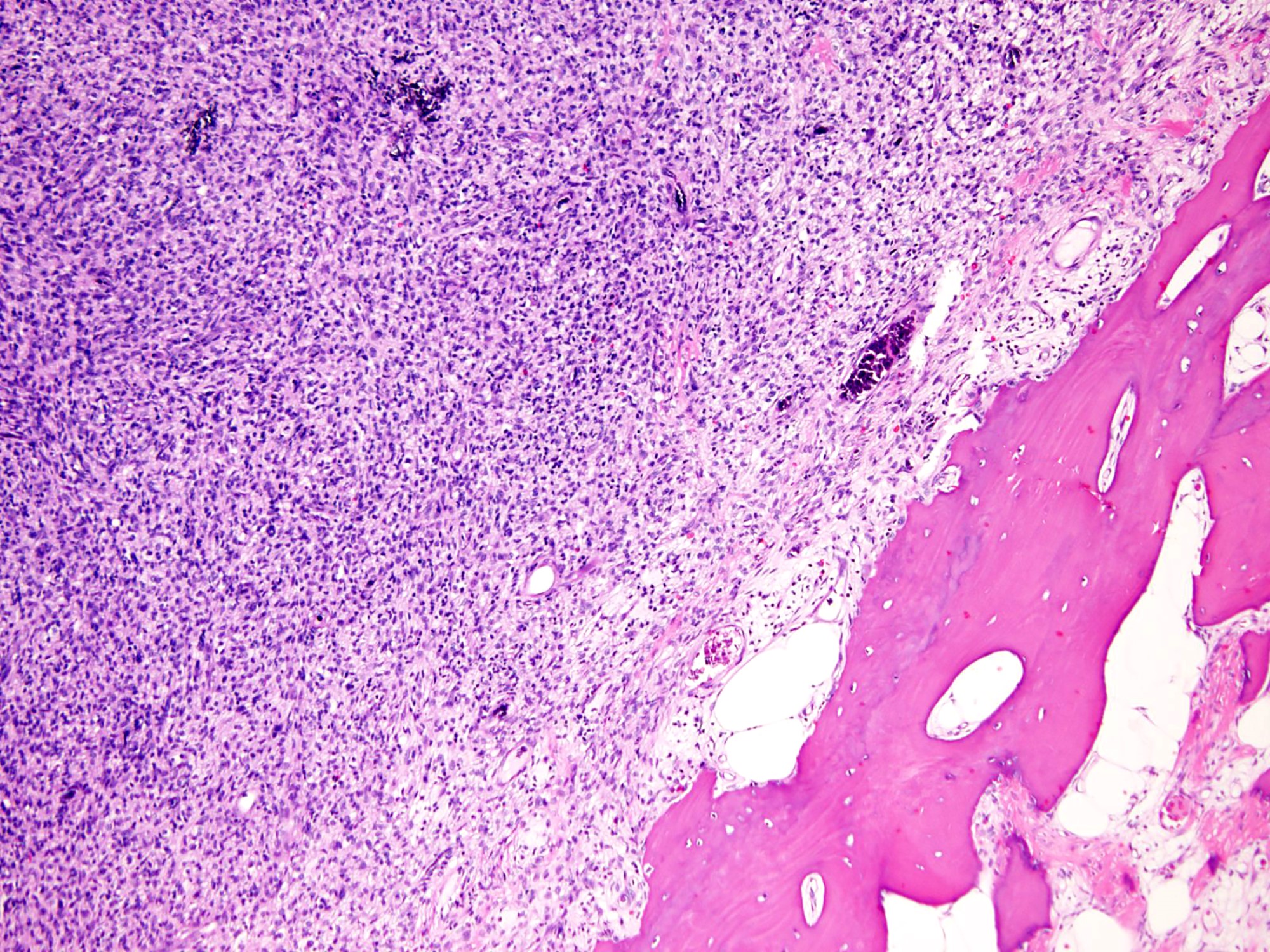
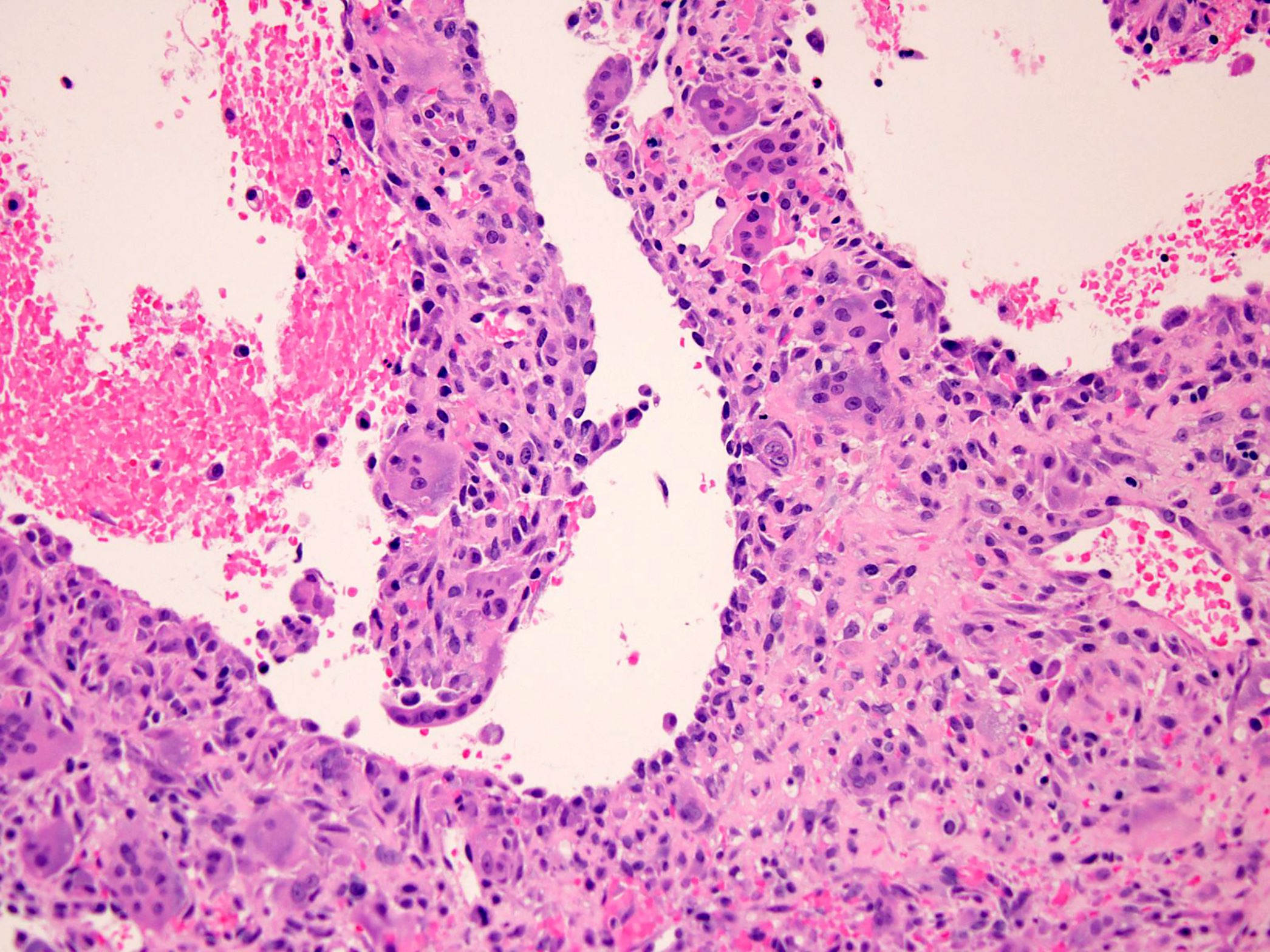
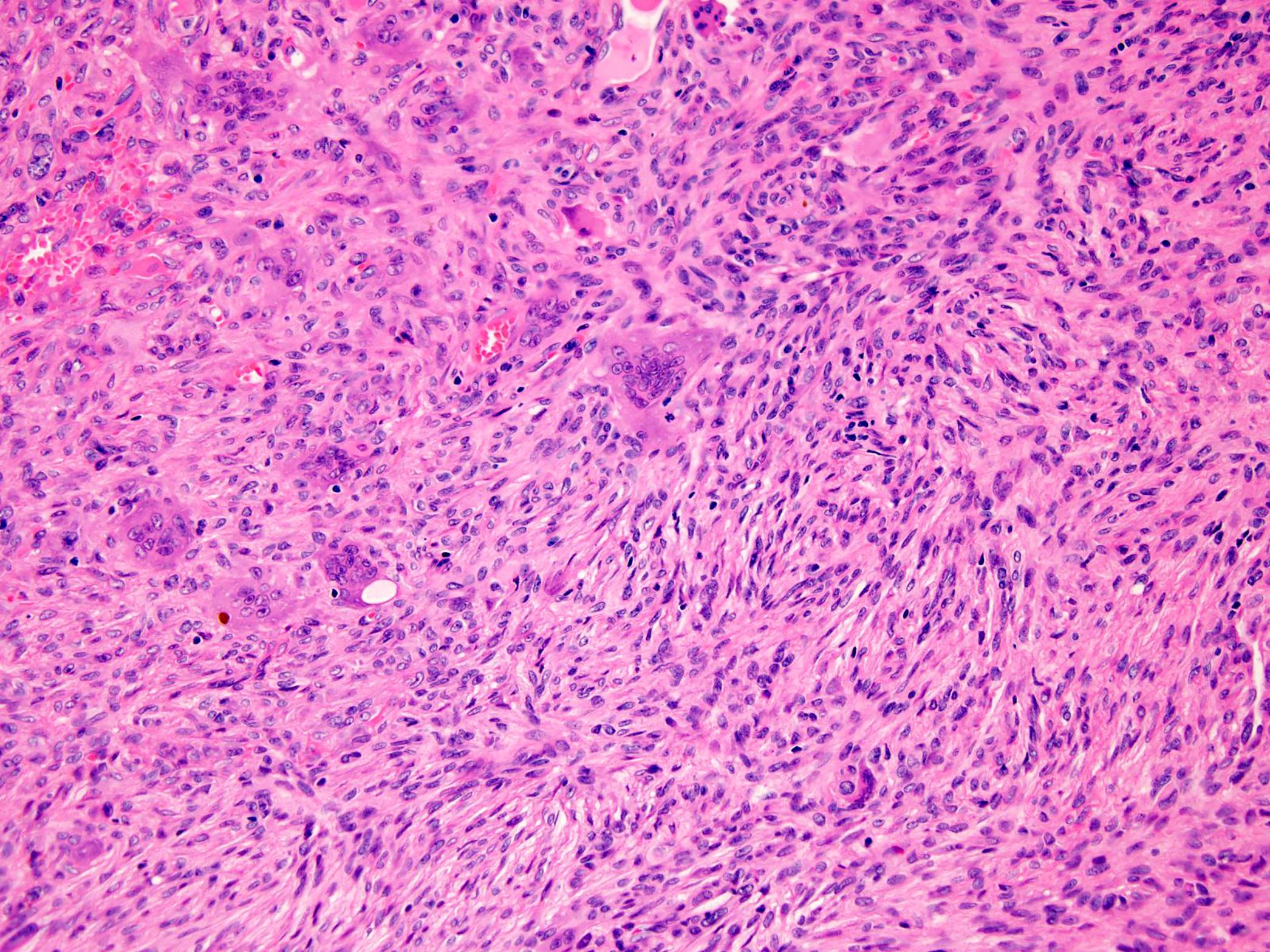
- Conventional giant cell tumor of bone:
- Highly cellular lesion composed of large number nonneoplastic osteoclast-like giant cells, between which mononuclear neoplastic cells are embedded (Histopathology 2021 May 15 [Epub ahead of print], Lancet Oncol 2010;11:275)
- Mononuclear neoplastic cells exhibit a variety of morphological appearances, including round to oval cells and spindled cells with pale eosinophilic cytoplasm and nuclei with dispersed chromatin and small nucleoli
- Mitoses are commonly present and can be numerous
- Presence of atypical mitoses should raise suspicion for malignancy
- Necrosis is usually seen in the setting of pathological fracture
- Hemorrhage, aneurysmal change, hemosiderin deposition, foamy microphages and fibrosis are common
- Tumor may contain woven bone and foci of cartilage matrix (Am J Surg Pathol 2020;44:748)
- Vascular invasion may be present
- Scattered mononuclear neoplastic cells with enlarged hyperchromatic nuclei, irregular nuclear contours, smudged chromatin and nuclear pseudoinclusions may be present and probably represent degenerative change (Skeletal Radiol 2004;33:641, Skeletal Radiol 2016;45:929)
- Cortical bone is often eroded or completely destroyed and replaced by a reactive rim of woven bone at the tumor periphery
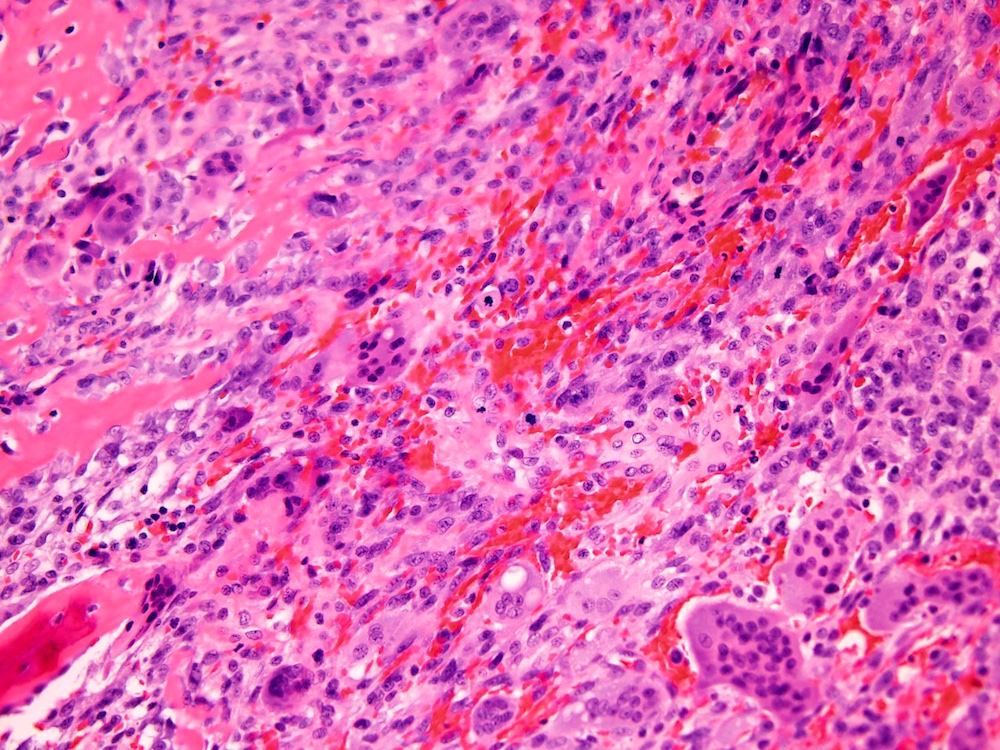
- Malignant giant cell tumor of bone:
- GCTB can undergo malignant transformation; malignancy in GCTB can be primary (nodule of highly pleomorphic mononuclear cells present within an otherwise conventional GCTB at first diagnosis) and secondary (after treatment of GCTB) (Technol Cancer Res Treat 2019;18:1533033819840000, Virchows Arch 2012;460:327)
- Malignant component of a GCTB does not have specific morphological features and may be an undifferentiated sarcoma, fibrosarcoma, chondrosarcoma or osteosarcoma (Am J Surg Pathol 2017;41:1059, J Bone Joint Surg Am 1986;68:1073, Mod Pathol 1989;2:541)
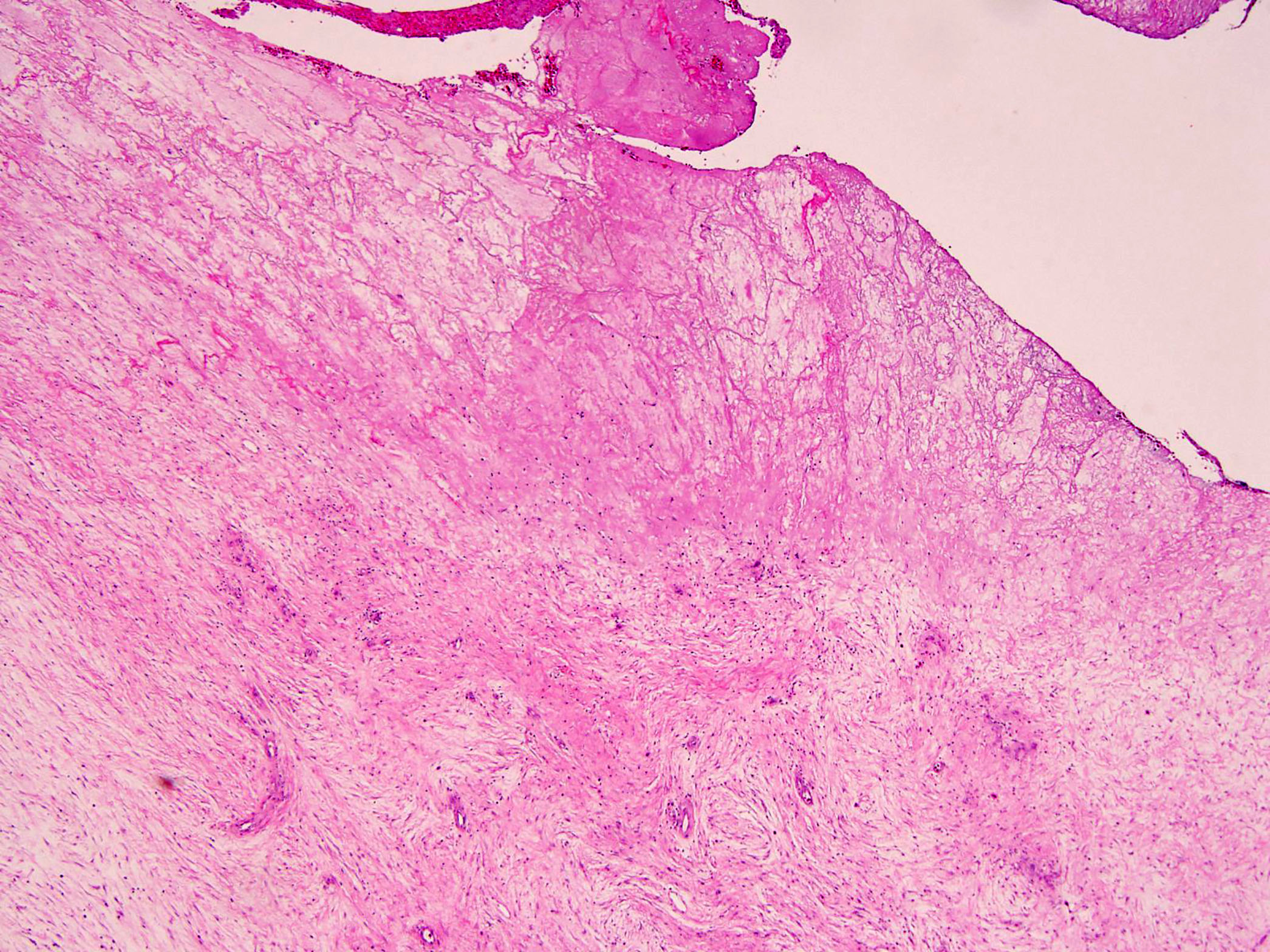
- Denosumab treated giant cell tumor of bone:
- histologic changes of GCTB after denosumab treatment are variable and consist of striking depletion of osteoclast-like giant cells and reduction of neoplastic stromal cells (Clin Cancer Res 2012;18:4415, Lancet Oncol 2010;11:275)
- Hemorrhage and incremental fibro-osseous tissue or new woven bone replace the lesions in various proportions (Clin Cancer Res 2012;18:4415, Front Oncol 2020;10:580605, Histopathology 2018;72:914)
- Cases of malignant transformation of GCTB during denosumab treatment have been reportedly growing (Ann Surg Oncol 2015;22:2860, Case Rep Med 2015;2015:767198)
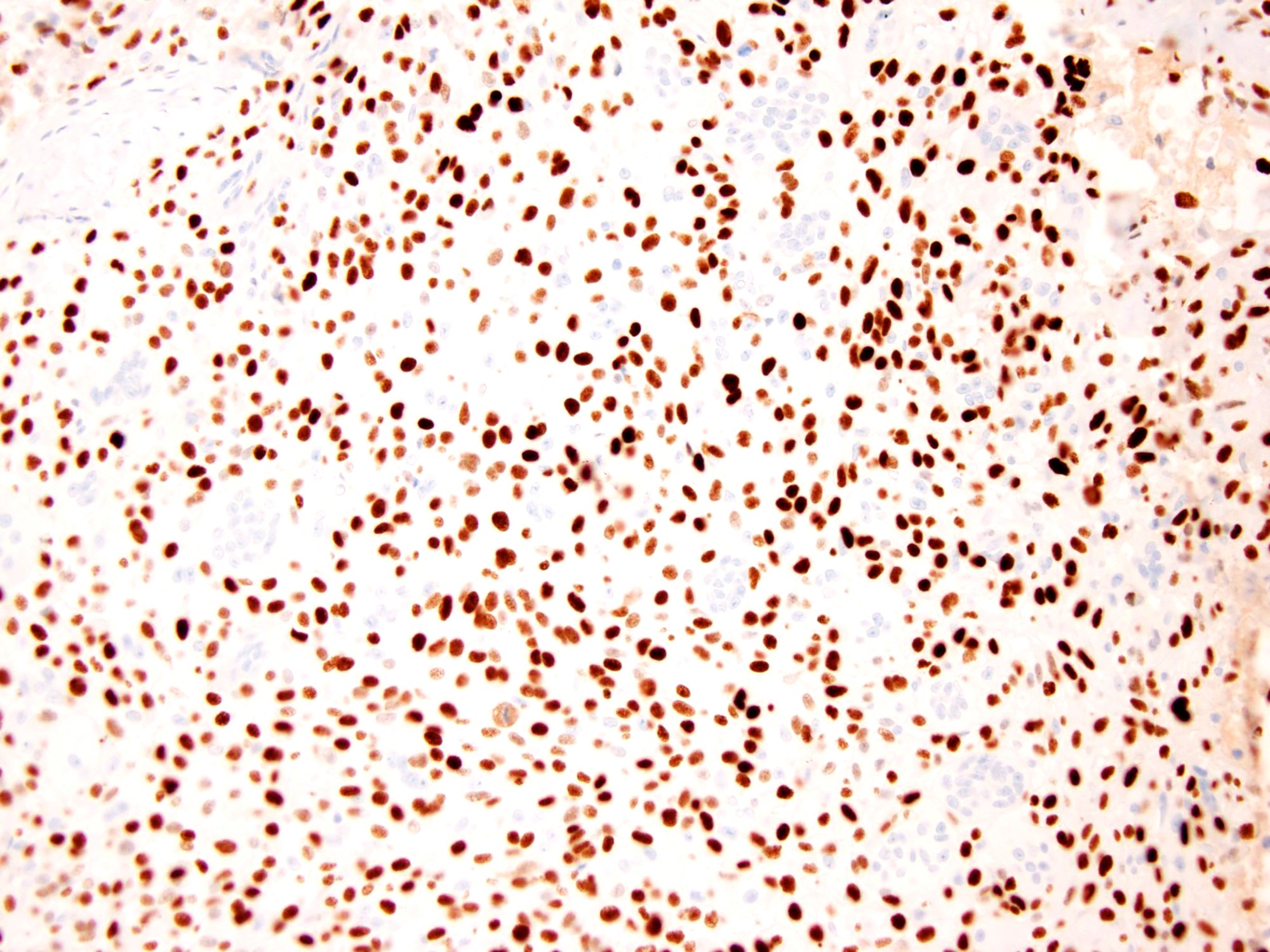
Microscopic (histologic) images
Contributed by Borislav A. Alexiev, M.D.
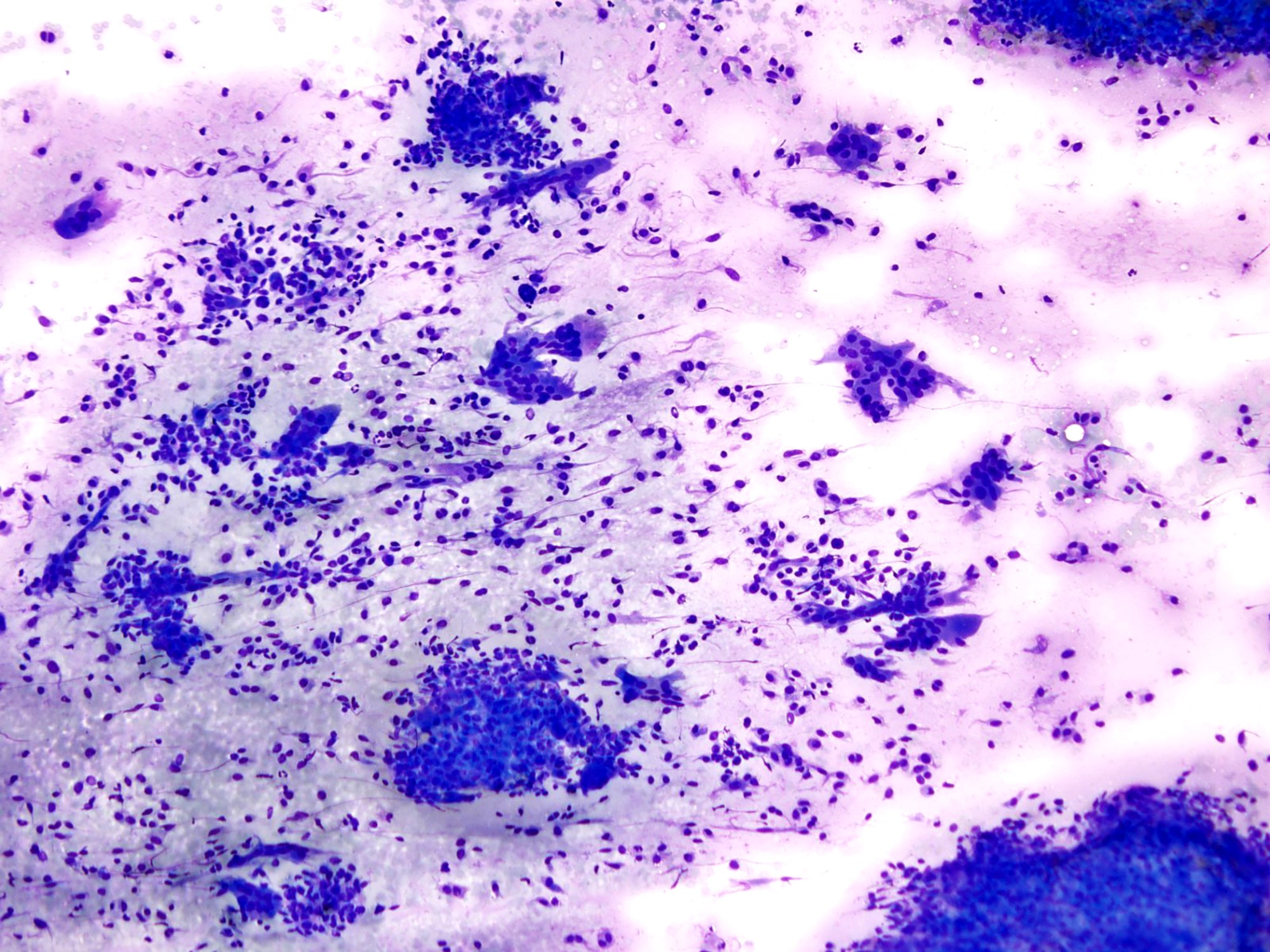
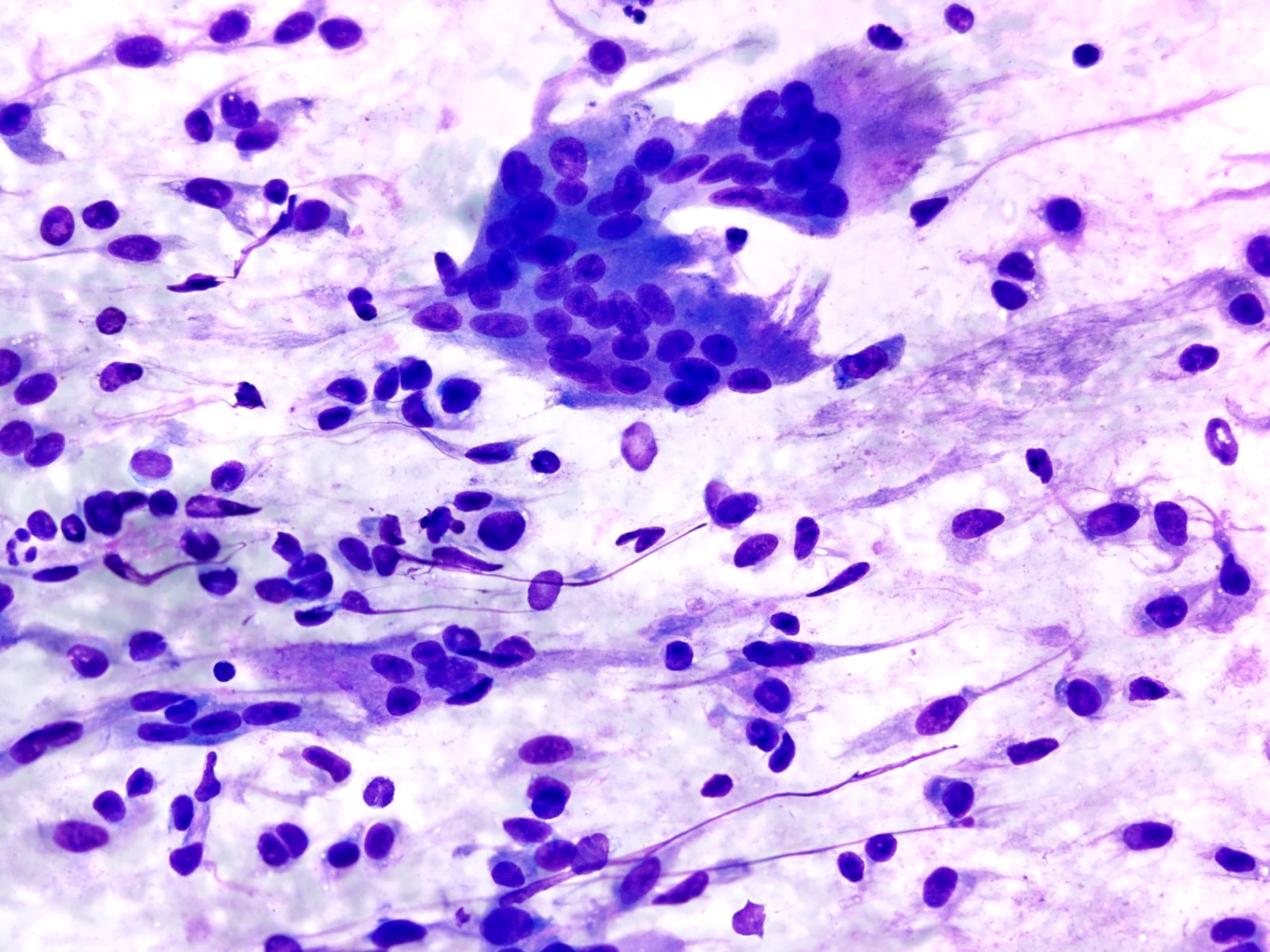
Cytology description
- Smear preparations demonstrate oval to spindled mononuclear cells in cohesive clusters bordered by multiple multinucleated giant cells (Cancer Cytopathol 2018;126:552, Diagn Cytopathol 2004;30:14)
- Mononuclear cells have spindled or plump cell bodies with moderate amounts of cytoplasm and well defined cytoplasmic membranes; oval nuclei demonstrate fine, evenly distributed chromatin and small nucleoli
- Multinucleated cells are osteoclast-like and are associated with clusters of mononucleated cells or lying freely
- They have a well demarcated cytoplasm and contain from a few to several dozen monomorphic nuclei (Diagn Cytopathol 1985;1:111)
Positive stains
Negative stains
Electron microscopy description
- Giant cells contain a great number of mitochondria, autophagic vacuoles and lysosomal bodies (Pathol Eur 1976;11:117)
- Stromal cells exhibit nuclear pseudoinclusions and prominent endoplasmic reticulum and Golgi complex (Virchows Arch A Pathol Anat Histol 1979;381:159)
Molecular / cytogenetics description
- GCTBs harbor H3F3A (G34W/V) mutations (Mod Pathol 2017;30:393, Am J Surg Pathol 2015;39:1576)
Sample pathology report
- Left distal femur, curettage:
- Giant cell tumor of bone (see comment)
- Comment: Radiology images of the left femur demonstrates a 5.2 x 5.9 x 5.2 cm expansile heterogeneous mass centered in the lateral femoral condyle. There is cortical breakthrough and an extraosseous component along the posterosuperior margin. Histologically, the neoplasm is cellular and composed of a large number of osteoclast-like giant cells, between which mononuclear round to oval cells and spindled cells with pale eosinophilic cytoplasm and nuclei with dispersed chromatin and small nucleoli are embedded. Scattered mitotic figures and no necrosis are seen (11 mitoses / 10 high power fields). There are aneurysmal change, clusters of hemosiderophages and fibrosis. The cortical bone is focally destroyed and replaced by a reactive rim of woven bone at the tumor periphery. Immunohistochemical stains for H3.3 G34W and p63 are positive in mononuclear cells. Overall, the appearance on computed tomography and magnetic resonance scans, morphological features and immunohistochemical profile support the diagnosis of giant cell tumor of bone.
- Giant cell tumor of bone can be locally aggressive and it has a propensity to recur locally after curettage alone. Furthermore, in approximately 3 - 7% of cases, distant metastases occur, most often to the lungs.
Differential diagnosis
- Chondroblastoma:
- Predilection for epiphyseal (subchondral) region of long bones (Skeletal Radiol 1985;14:1, Hum Pathol 1989;20:965)
- Sheets of polygonal cells with small grooved nuclei and eosinophilic cytoplasm, interspersed osteoclast-like giant cells and islands of chondroid matrix (Cancer 1972;30:401, J Bone Joint Surg Am 1951;33-A:997)
- Chicken wire pattern of calcification
- Positive for H3K36M expression (Orthop Surg 2021;13:616)
- Aneurysmal bone cyst:
- ABC can occur in any bone and secondary ABC changes are a common finding in giant cell tumor of bone, chondroblastoma and NOF, i.e. the radiology is not specific (see reference below and WHO Classification of Tumours Editorial Board: Soft Tissue and Bone Tumours, 5th Edition, 2020)
- In addition, primary aneurysmal bone cyst can show solid growth (Cancer 1993;71:729, Cancer 1983;51:2278)
- Secondary ABC with fibrous dysplasia and nonossifying fibroma typically occurs in the diaphysis of long bones in adolescents, whereas secondary ABC with chondroblastoma usually occurs in the metaphysis of the long bones in adolescents; secondary ABC with giant cell tumors occur in the metaphysis and epiphysis of the long bones in adults > 30 years of age (Oncol Lett 2017;13:2290)
- Negative for HG34W expression (Histopathology 2021 May 15 [Epub ahead of print])
- USP6 rearrangement (Head Neck Pathol 2019;13:281, Histopathology 2021;78:676)
- Nonossifying fibroma:
- Metaphyseal location in long bones in skeletally immature patients (Cureus 2021;13:e14102)
- Storiform proliferation of plump spindle cells, intermingled osteoclast-like giant cells, hemosiderophages and clusters of foamy histiocytes (J Pathol 2019;248:127)
- Negative for HG34W expression (Histopathology 2021 May 15 [Epub ahead of print])
- Mutations activating the RAS-MAPK pathway (KRAS, FGFR1 and NF1) in 80% of the tumors (J Pathol 2019;248:127)
- Giant cell rich osteosarcoma:
- Neoplastic osteoblasts with marked nuclear pleomorphism, prominent nucleoli and atypical mitoses (J Oral Maxillofac Pathol 2020;24:S67)
- Abundant spindle cells with marked atypia arranged in a streaming or storiform pattern (Int J Clin Exp Pathol 2015;8:9718)
- Infiltration of pre-existing lamellar bone structures
- Negative for HG34W expression
Practice question #1
A 31 year old man presented with a left distal femur metadiaphyseal expansile, predominantly solid, enhancing lesion measuring 6.6 cm in greatest dimension. There is medial distal femur diffuse cortical thinning overlying the lesion and periosteal edema and enhancement. No convincing extraosseous component is seen.
Hematoxylin eosin stains demonstrate a cellular lesion composed of a large number osteoclast-like giant cells, between which mononuclear cells are embedded. The mononuclear cells exhibit a variety of morphological appearances, including round to oval cells and spindled cells with pale eosinophilic cytoplasm and nuclei with dispersed chromatin and small nucleoli. Scattered mitotic figures and no necrosis are seen (7 mitoses / 10 high power fields). There is reactive woven bone formation, aneurysmal changes with hemosiderin deposition and fibrosis. The cortical bone is eroded; however, there is no complete cortical bone destruction. Immunohistochemical stains for H3.3 G34W and p63 are positive in mononuclear cells. P53 expression is wild type (no mutation).
Which of the following is most likely the correct diagnosis?
- Aneurysmal bone cyst
- Chondroblastoma
- Giant cell tumor of bone
- Osteoblastoma
- Osteosarcoma
Practice answer #1
Practice question #2
Which of the following is true about giant cell tumor of bone (GCTB)?
- GCTB is composed of neoplastic osteoclast-like giant cells and nonneoplastic mononuclear stromal cells
- GCTB is positive for HG34W
- GCTB is positive for HK36M
- GCTB treated with denosumab shows a striking increase of osteoclast-like giant cells
- GCTB typically affects the diaphysis of long bones
Practice answer #2