Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1Cite this page: Al Dallal H, Salih ZT. LSIL / CIN I. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixlsil.html. Accessed September 15th, 2025.
Definition / general
- Usually transient / self limited infection by human papillomavirus (low risk or high risk HPV)
- This category includes:
- Flat low grade squamous intraepithelial lesion (LSIL) / cervical intraepithelial neoplasia (CIN) I
- Exophytic / papillary LSIL (can be immature or mature)
Essential features
- Low grade squamous lesion caused by low or high risk HPV
- Koilocytes in the upper layers are characteristic
- Majority of LSIL regress spontaneously
Terminology
- Bethesda terminology: low grade squamous intraepithelial lesion (LSIL), use for cytology or cervical biopsies; recommended by LAST project and adopted by the World Health Classification of Female Genital Tumours (IARC 2020) (Arch Pathol Lab Med 2012;136:1266)
- Alternative terminology (no longer recommended): mild squamous dysplasia, cervical intraepithelial neoplasia I (CIN I)
- Exophytic forms: immature condyloma, mature condyloma / giant condyloma) (Am J Surg Pathol 2013;37:300, Hum Pathol 1998;29:641)
ICD coding
- ICD-10: N87.0 - mild cervical dysplasia
Epidemiology
- Young women < 40 years old but can occur in any age group
- LSIL cells are found in about 2% of all Pap smears (Obstet Gynecol Clin North Am 2008;35:599)
Sites
- HPV associated LSIL can involve:
- Cervix
- Vagina
- Vulva
- Anus
- Penis
- Scrotum
Pathophysiology
- LSIL is a heterogenous group caused by
- Low risk HPV: 6, 11, 42 and 44
- High risk HPV: 16, 18, 31, 33, 35, 45, 52 and 58
- HPV is a member of the papovavirus family and consists of a virion containing double stranded, circular DNA surrounded by a protein capsid
- HPV has 6 E (early) genes (E1, E2, E4, E5, E6, E7) and 2 L (late) genes
- Called E and L genes depending on when they are expressed during the cycle
- HPV needs a human host cell to replicate
- HPV infects squamous cells (a population of reserve / metaplastic cells in the transformation zone of the cervix) (Proc Natl Acad Sci U S A 2012;109:10516)
- HPV infection begins in the basal layers of the epithelium with expression of the E genes
- E4 protein of HPV interact with filaggrin (a cytokeratin binding protein), which leads to loss of specific cytokeratin from the cell and collapse of matrix
- As the cells mature and move toward the surface, L1 and L2 genes are expressed, which are necessary for the viral capsid proteins' transcription
- In LSIL, the HPV DNA does not integrate into the host DNA and remains in free episomal form; this allows for replication of the virus
- Koilocytes are filled with complete virions, ready to be discharged
Etiology
- Low risk HPV in most cases
- Exophytic LSIL, both immature and mature, is caused by HPV types 6 and 11 (Am J Surg Pathol 2013;37:300, Hum Pathol 1998;29:641)
- High risk HPV: 25 - 30% of the LSIL cases (Mod Pathol 2016;29:1501)
Clinical features
- Asymptomatic
- Found incidentally on Pap smear screening, cervical biopsy or hysterectomy
Diagnosis
- Pap smear (cervical cytology screening)
- Cervical biopsy
Prognostic factors
- 85.3% of LSILs regress, 7.3% persist, 7.3% progress to HSIL and 0.15% progress to invasive cancer (Mod Pathol 2016;29:1501)
- p16+ LSIL has a higher risk of progression to HSIL (Cancer Cytopathol 2016;124:58, Am J Obstet Gynecol 2009;201:488.e1)
Treatment
- Women 30 years of age and older
- Pap+ and no HPV test or HPV+ → colposcopy
- Pap+ and HPV- → repeat Pap or cotesting in 1 year → if Pap+ or HPV+ → colposcopy; if both negative, repeat cotesting in 3 years
- Women aged 21 - 24 years
- Colposcopy is not recommended; follow up in 1 year
- Pregnant women
- Deferring colposcopy until 6 weeks postpartum is acceptable
- Postmenopausal women
- HPV testing, repeat cytologic testing at 6 months and 12 months or colposcopy
- Types of available vaccines
- HPV bivalent vaccine (Cervarix) will only protect against HPV 16 and 18
- HPV quadrivalent vaccine (Gardasil) will protect against HPV types 6, 11, 16 and 18
- HPV 9 valent vaccine, recombinant (Gardasil 9) can protect against HPV types 6, 11, 16, 18, 31, 33, 45, 52 and 58
- Reference: Obstet Gynecol 2013;121:829, National Comprehensive Cancer Network: NCCN Guidelines [Accessed 2 June 2021]
Gross description
- Flat lesions usually do not produce a grossly identifiable lesion
- Appears white after application of 3% acetic acid (acetowhite) on colposcopy examination
- Exophytic lesions can occasionally be seen grossly as small and friable frond-like lesions
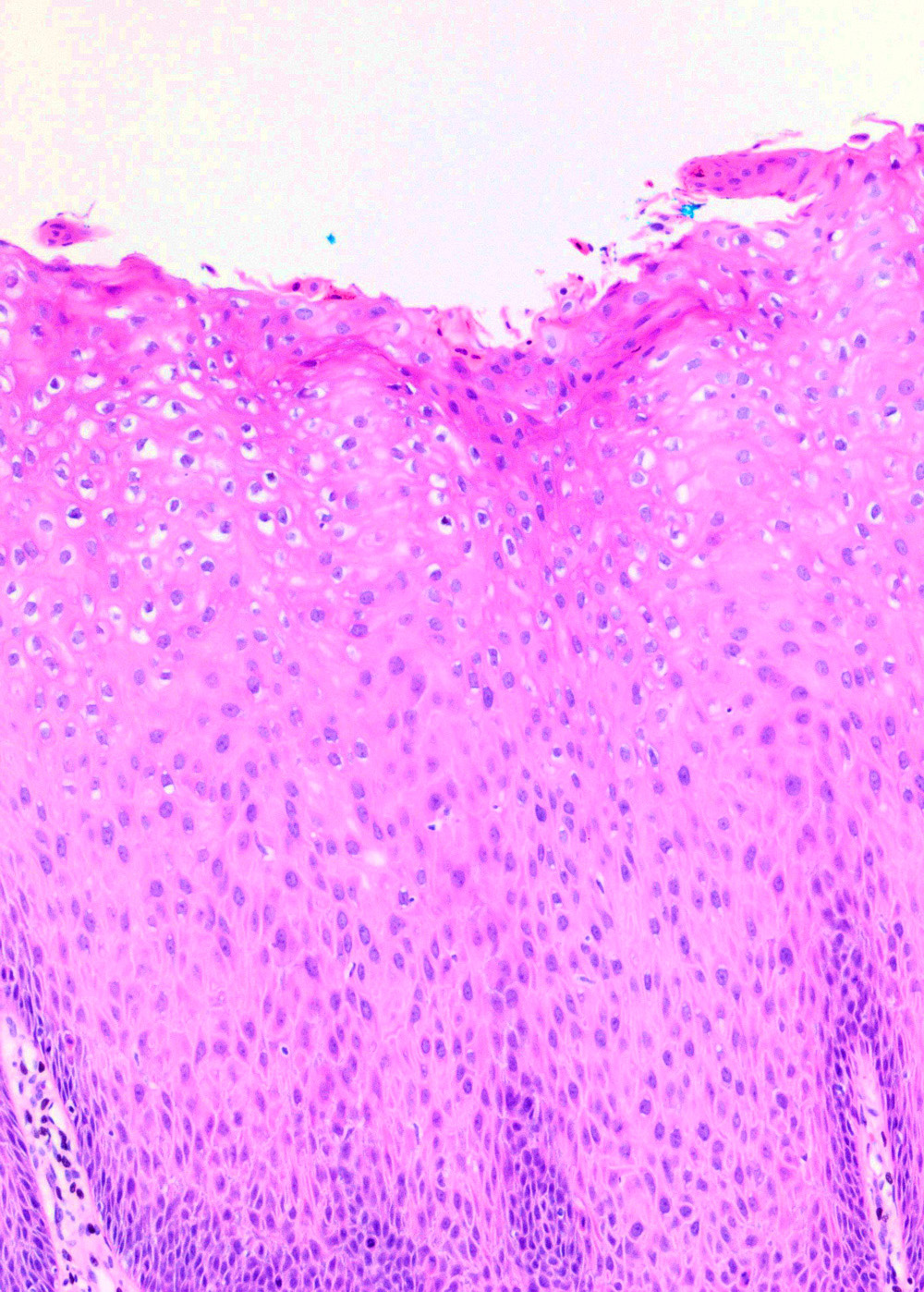
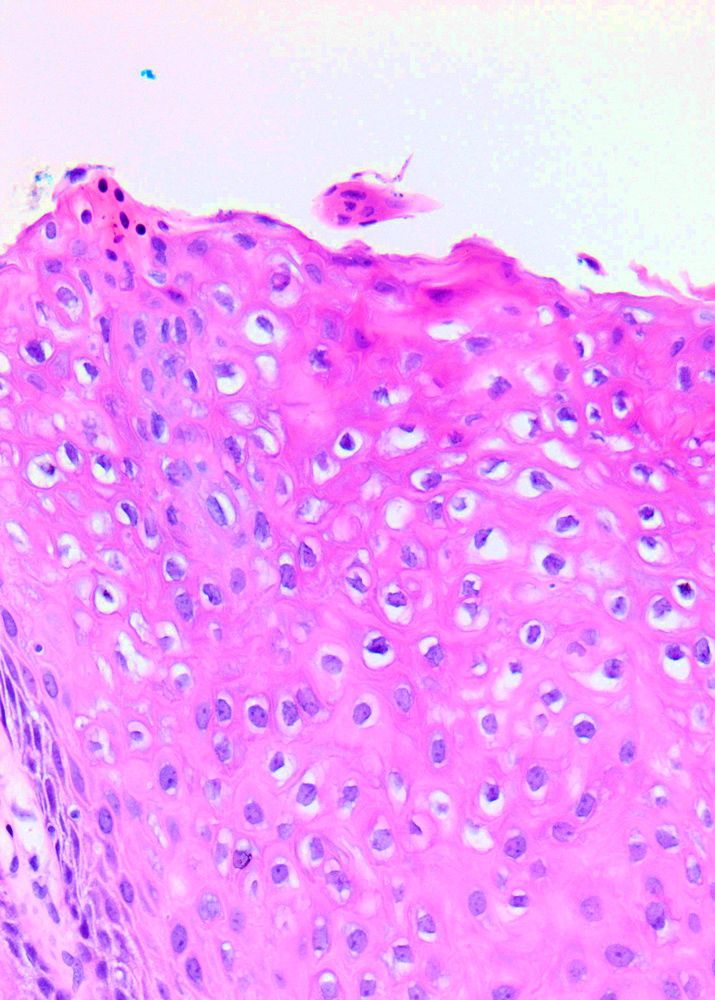
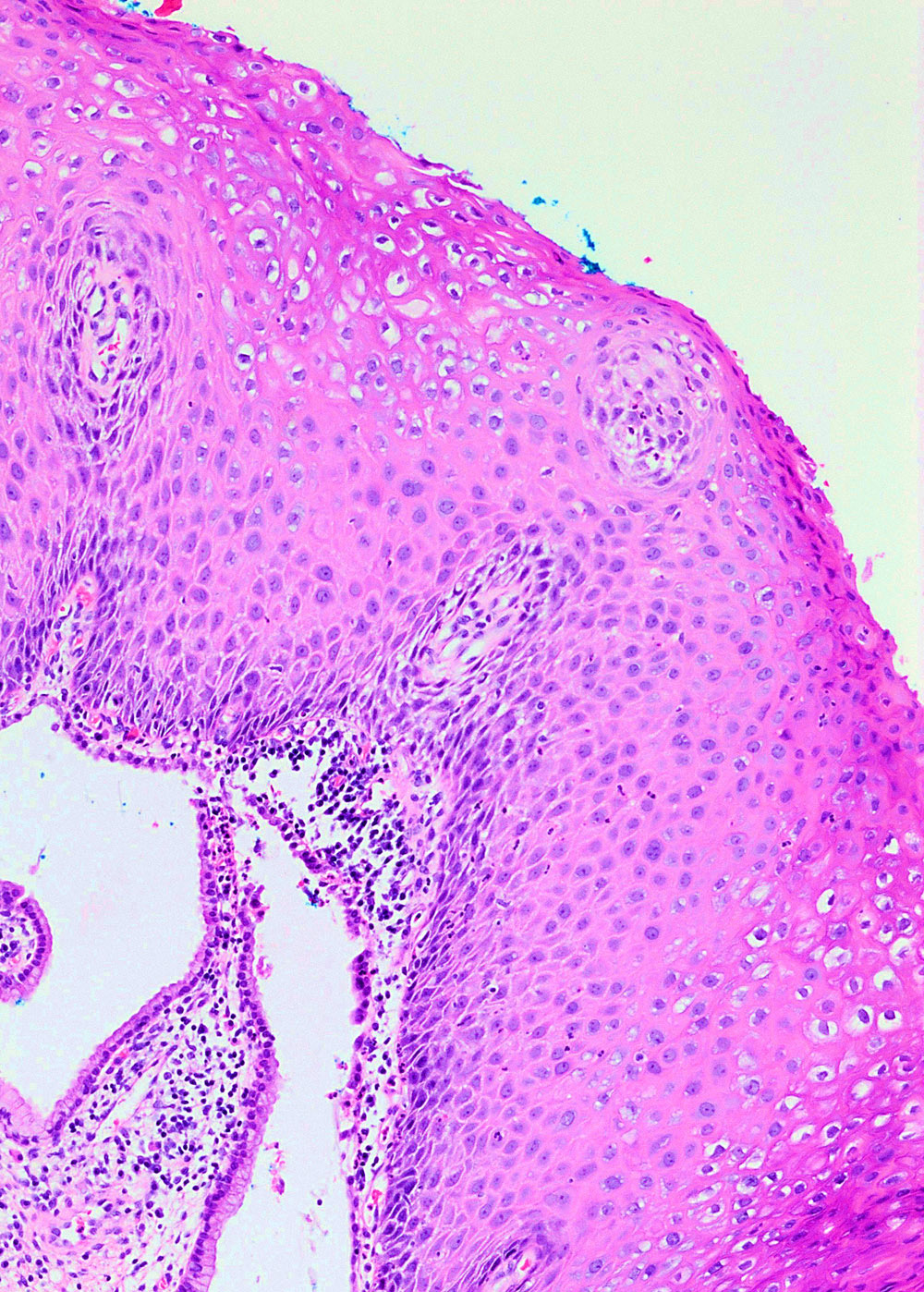
Microscopic (histologic) description
- Flat LSIL
- Preserved maturation
- Basal layer preserves polarity while intermediate to superficial cells lose polarity
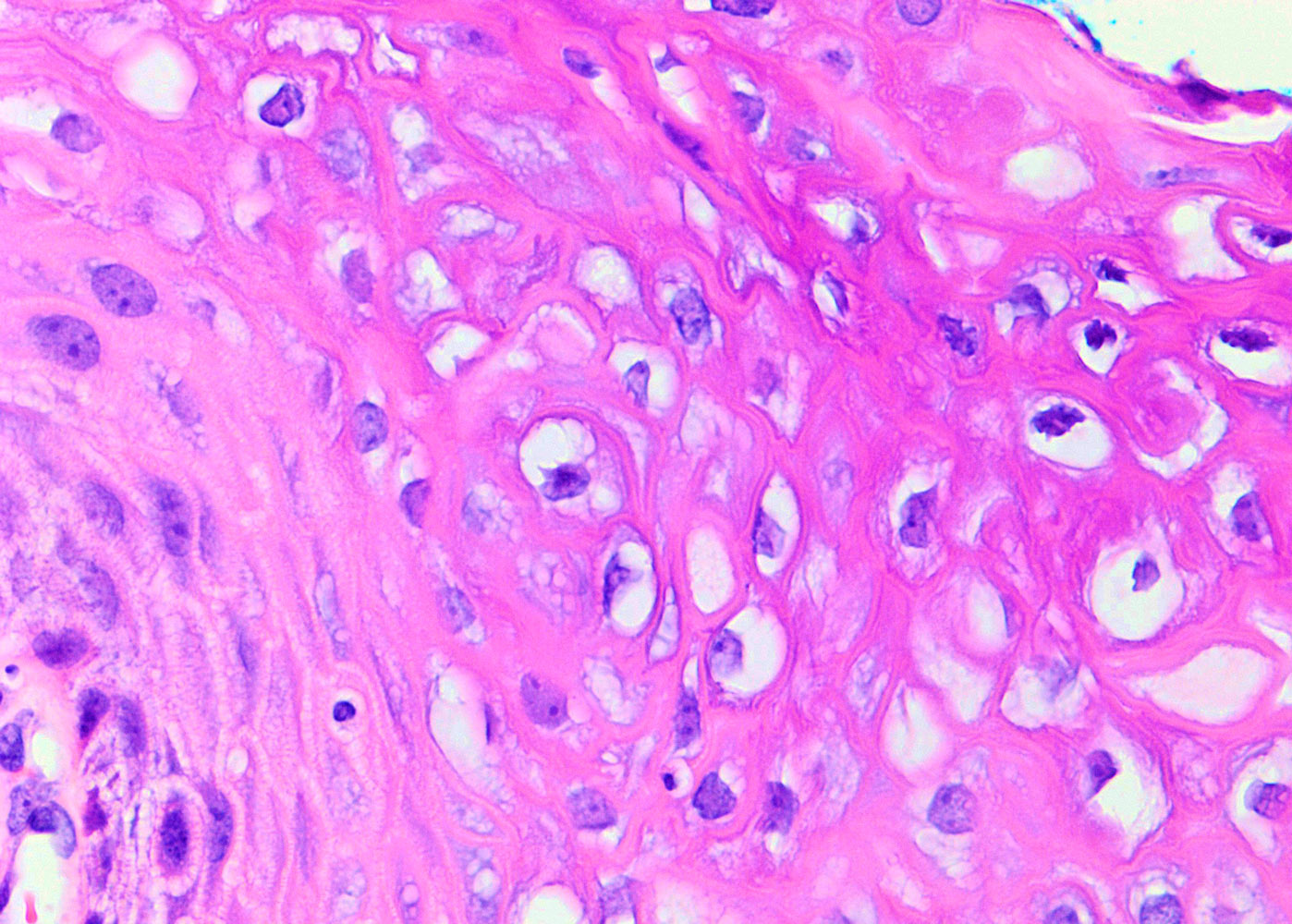
- Nuclei in the superficial layer are large, hyperchromatic and irregular with perinuclear halos (koilocytosis / koilocytotic atypia)
- May show mitotic activity
- Exophytic LSIL
- Mature: papillomatosis with preserved maturation and koilocytic atypia
- Immature: slender papillae with metaplastic immature squamous epithelium and mild koilocytic atypia
Microscopic (histologic) images
Virtual slides
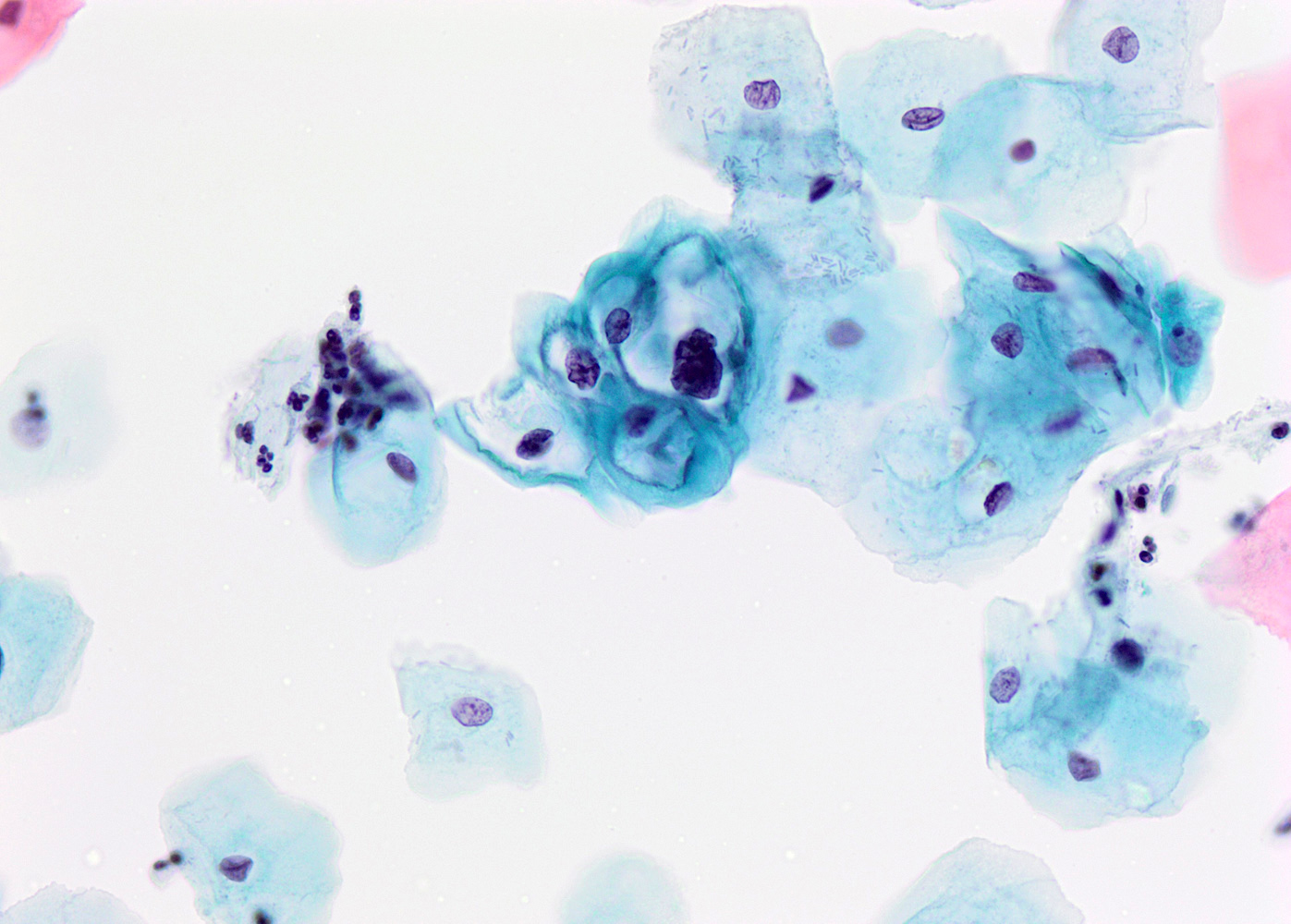
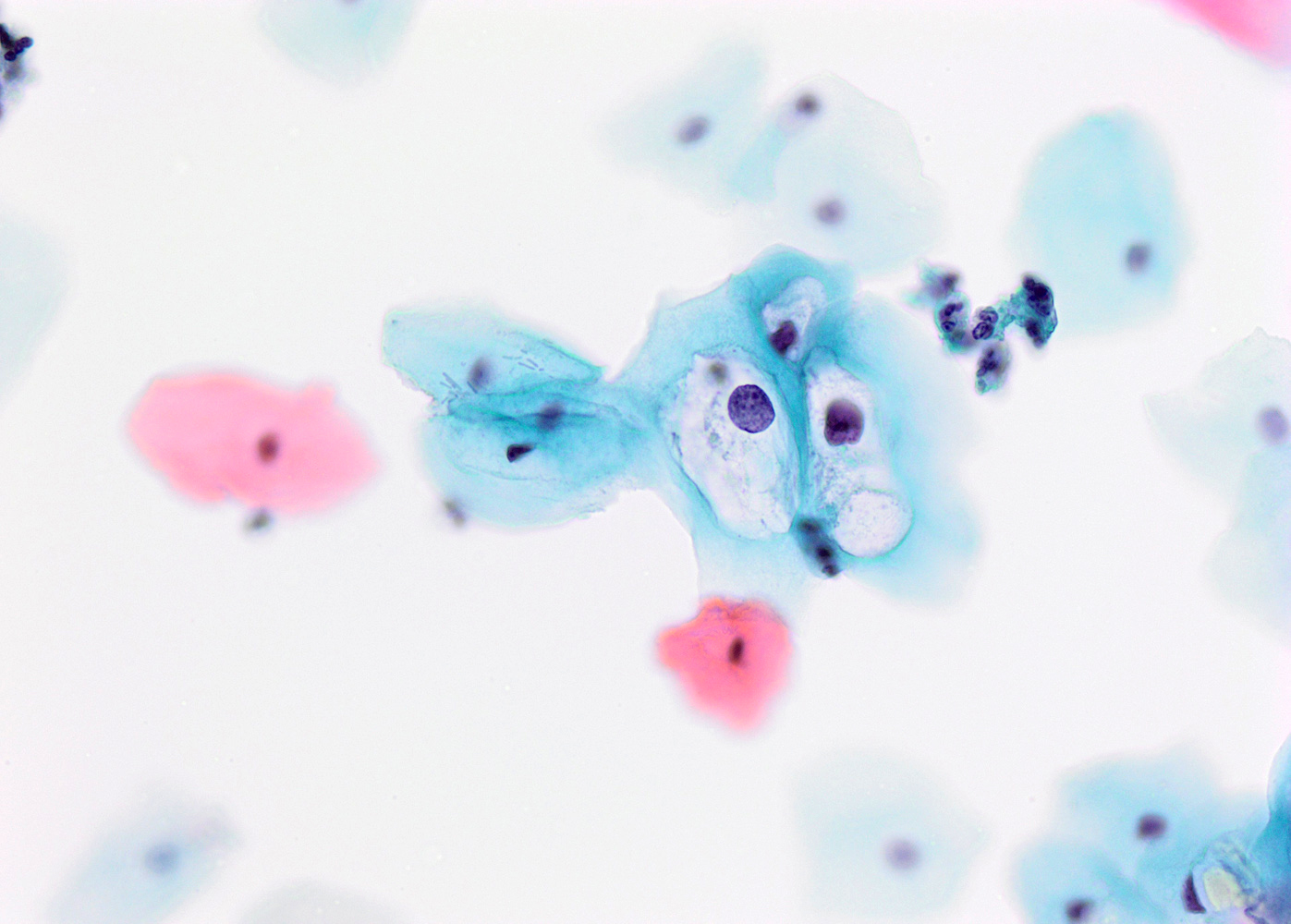
Cytology description
- Presence of koilocytes: intermediate squamous cell with enlarged hyperchromatic nuclei (1 or multiple nuclei) surrounded by perinuclear halo
- Nuclear features:
- Nuclear enlargement comparted to intermediate squamous cell (increased N/C ratio)
- Dense hyperchromatic chromatin
- Irregular nuclear membranes
- Perinuclear clear halo with a well defined, thick cytoplasmic rim
- See LSIL / CIN I cytology
Negative stains
- p16 is usually negative or weak and patchy, although lesions caused by high risk HPV will show overexpression (~33% of cases), limiting its use as a biomarker (Int J Surg Pathol 2012;20:146)
Molecular / cytogenetics description
- Molecular assays available based on RNA ISH include:
- HPV E6 / E7 mRNA in situ hybridization (ISH) assay covering 18 common high risk types (HR-RISH, aka HR-HPV RNA18 ISH)
- HR-RISH was also positive in 78% of anogenital low grade squamous intraepithelial lesion, including 81% of CIN1 (Am J Surg Pathol 2017;41:607)
- Molecular assays based on the detection of HPV DNA include:
- Nonamplified hybridization assays, such as Southern transfer hybridization (STH), dot blot hybridization (DB) and in situ hybridization (ISH)
- Signal amplified hybridization assays, such as hybrid capture assays (HC2)
- Target amplification assays, such as polymerase chain reaction (PCR) and in situ PCR (Int J Biol Markers 2009;24:215)
Videos
Squamous lesions of the cervix and their differential diagnosis
by Carlos Parra-Herran, M.D.
Sample pathology report
- Cervix, biopsy:
- Low grade squamous intraepithelial lesion (LSIL) / CIN I (see comment)
Differential diagnosis
- Inflammatory changes / repair:
- Nuclei are round, uniform and lack hyperchromasia
- Squamous metaplasia:
- Cells with mucin vacuoles, nuclei lack hyperchromasia
- Radiation and chemotherapy effects:
- Previous history, low N/C ratio
- High grade squamous intraepithelial lesion (HSIL):
- Shows hyperchromatic crowded squamous cells with high N/C ratio, present throughout the epithelium
- Mitotic figures are seen above the basal layer
- p16 shows block type staining in most HSILs; however, about 33% of LSILs also show p16 overexpression; therefore, p16 helps only if it is negative or patchy (not overexpressed), as it excludes HSIL and would be supportive of LSIL in the right diagnostic context
Additional references
Practice question #1
Practice answer #1