Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Van Treeck BJ, Hagen CE. Collagenous colitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/coloncollagenous.html. Accessed October 2nd, 2025.
Definition / general
- Form of microscopic colitis clinically associated with chronic watery diarrhea and histologically characterized by colonic intraepithelial lymphocytosis, surface mucosal damage, lamina propria inflammation and a subepithelial collagen band
Essential features
- Subtype of microscopic colitis in which patients present with chronic watery diarrhea and normal or nearly normal endoscopic findings
- Pathophysiology and etiology are unclear but thought to be multifactorial with a possible luminal antigen triggering inflammation and mucosal damage in a genetically predisposed individual
- Histology is characterized by a subepithelial collagen band, intraepithelial lymphocytosis, mixed inflammation in the lamina propria and surface mucosal damage with preserved crypt architecture
ICD coding
- ICD-10: K52.831 - Collagenous colitis
Epidemiology
- Wide age range including children but typically affects adults 50 - 70 years old (Am J Gastroenterol 2017;112:78)
- Strong female predominance (F:M = 9:1) (Am J Gastroenterol 2015;110:265, Am J Gastroenterol 2017;112:78)
- Incidence is 4.14 per 100,000 person years (Am J Gastroenterol 2015;110:265)
- Possible increased prevalence in Caucasians (Am J Gastroenterol 2017;112:78)
Sites
- Colon (right > left / rectum) (Clin Gastroenterol Hepatol 2020;18:2003, Neth J Med 2005;63:137)
Pathophysiology
- Poorly understood
- Presumed mechanism includes a dysregulated immune reaction to an unknown luminal antigen (medication, dietary factor, infectious agent, other) in a genetically predisposed individual (Lancet Gastroenterol Hepatol 2019;4:305)
- Watery diarrhea is a result of inhibited sodium channel upregulation, downregulation of tight junctions and colonocyte aquaporins and bile acid malabsorption (Lancet Gastroenterol Hepatol 2019;4:305)
Etiology
- Strong association with certain medications
- NSAIDs, aspirin, proton pump inhibitors, H2 receptor antagonists, selective serotonin reuptake inhibitors, among others (Am J Gastroenterol 2017;112:78)
- Other specific etiologies are unknown
Clinical features
- Symptoms include chronic or intermittent watery diarrhea, abdominal pain, weight loss, arthralgias, myalgias, fecal urgency, incontinence and fatigue (Am J Gastroenterol 2017;112:78, Frontline Gastroenterol 2019;10:388)
- Colonoscopy is normal or has mild nonspecific findings such as erythema or edema
- Rarely, mucosal tears or perforation can occur during endoscopy, likely as a result of decreased colonic wall compliance (Dig Liver Dis 2017;49:1073)
- Association with other autoimmune diseases (Lancet Gastroenterol Hepatol 2019;4:305, Am J Gastroenterol 2017;112:78, Frontline Gastroenterol 2019;10:388):
- 4.3% of patients with celiac disease also have microscopic colitis
- Also associated with type 1 diabetes, psoriasis and autoimmune thyroiditis
- Smoking is a risk factor (Scand J Gastroenterol 2011;46:1334, Frontline Gastroenterol 2019;10:388)
Diagnosis
- Colonoscopy with colon biopsies are required for diagnosis
- At least 2 biopsies from the ascending, transverse, descending and sigmoid colon are recommended due to patchy involvement of the colon (Am J Gastroenterol 2009;104:774, Am J Gastroenterol 2017;112:78)
Prognostic factors
- Symptomatic remission ranges from 2 - 92% (Am J Gastroenterol 2017;112:78)
- Spontaneous remission may occur in up to 15% of patients (Am J Gastroenterol 1997;92:57)
- If remission is achieved, repeat colonoscopy with biopsy not usually necessary (Frontline Gastroenterol 2019;10:388)
- No increased risk of colorectal adenocarcinoma (J Clin Med 2019;8:1942)
Case reports
- 49 and 61 year old women with collagenous colitis occurring in the setting of inflammatory bowel disease (Gastroenterol Rep (Oxf) 2019;7:218)
- 68 year old woman with melanoma and anti-PD1 induced collagenous colitis (Melanoma Res 2016;26:308)
- 72 year old man with pseudomembranous collagenous colitis (ACG Case Rep J 2016;3:e187)
- 80 year old woman presenting with spontaneous colon perforation in the setting of collagenous colitis (BMC Gastroenterol 2016;16:124)
Treatment
- Discontinuation of any offending medications (Am J Gastroenterol 2017;112:78)
- Antidiarrheals such as loperamide, diphenoxylate or bismuth subsalicylate
- For more severe symptoms, corticosteroids such as budesonide can be used
- Surgical intervention is a last resort
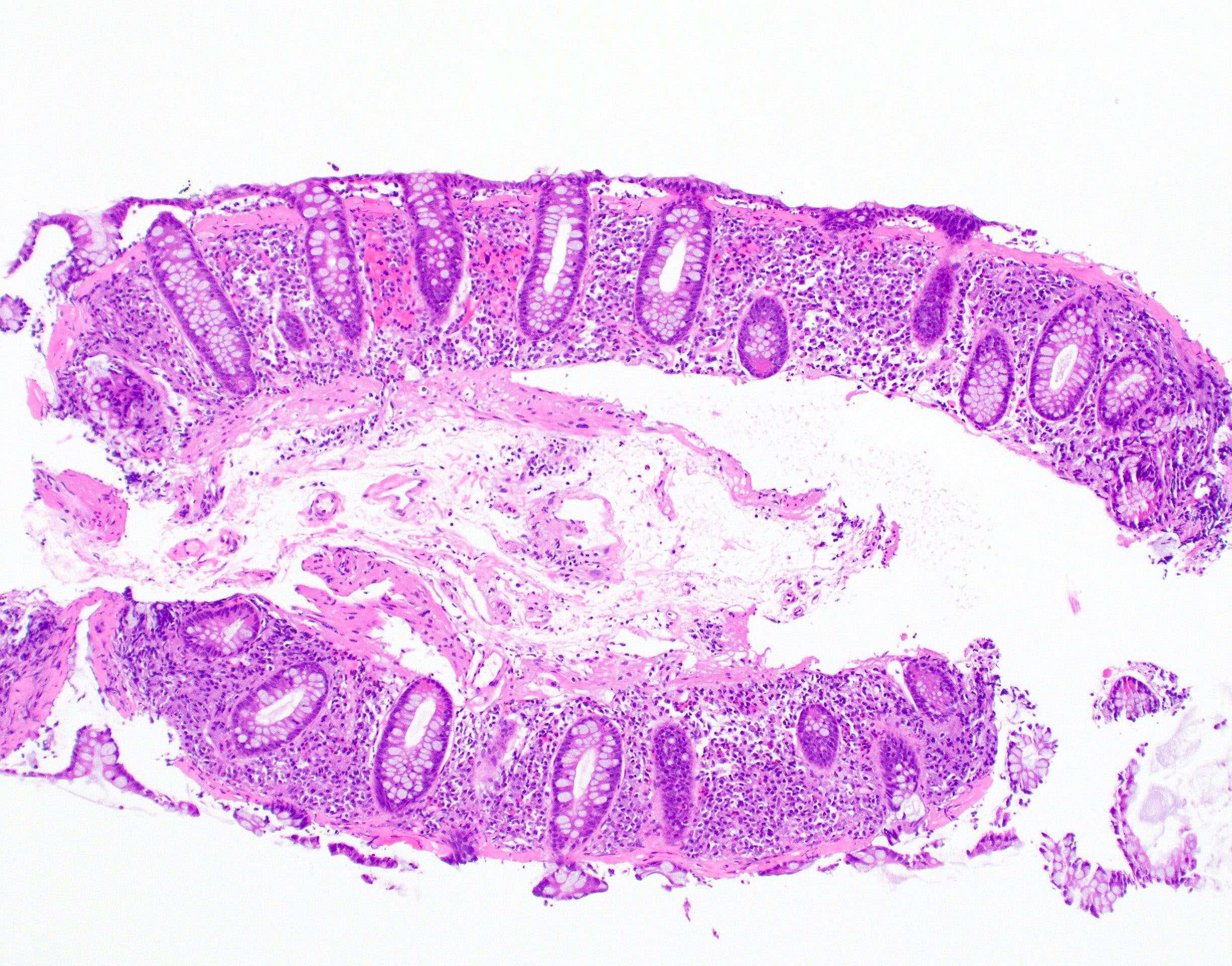
Microscopic (histologic) description
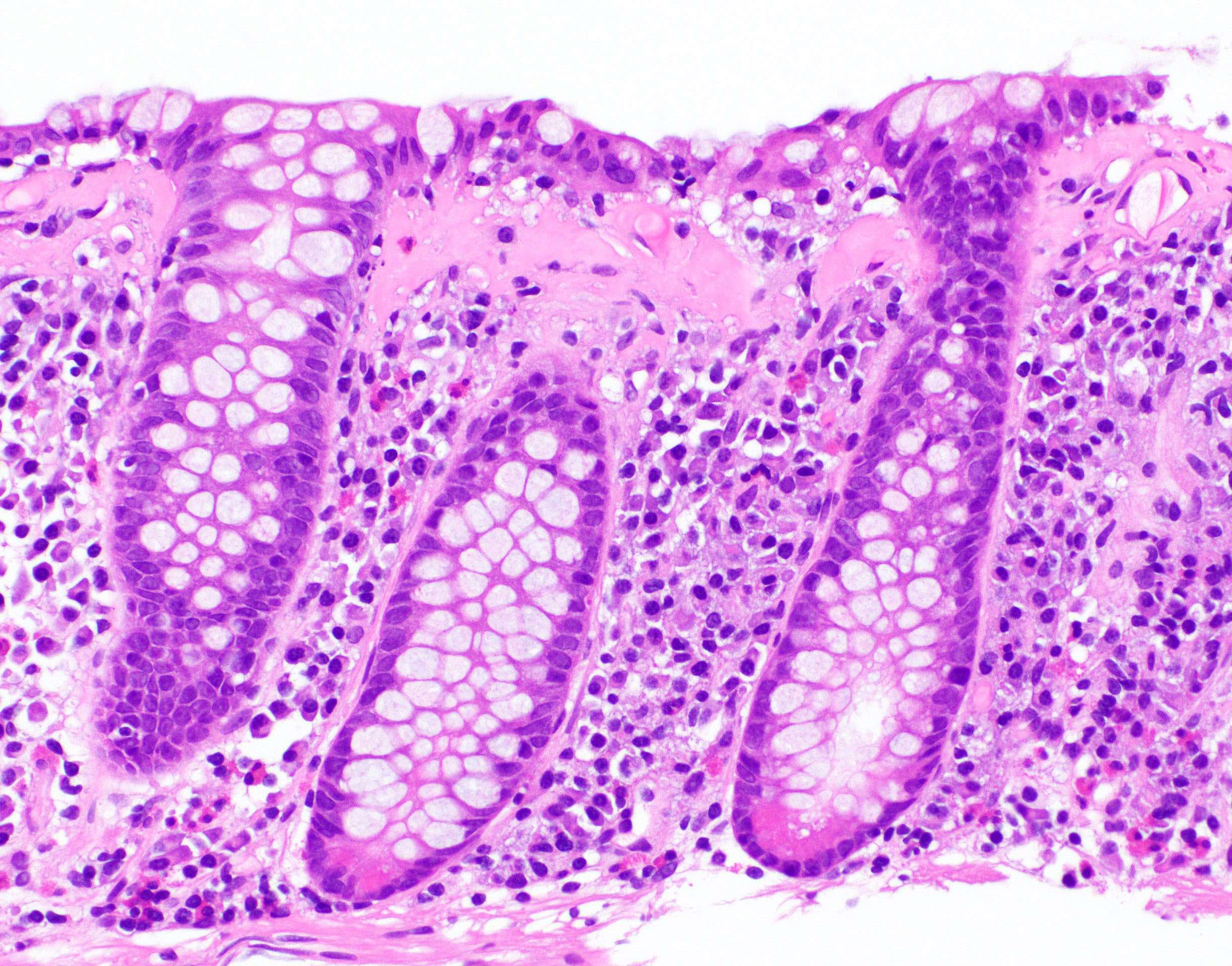
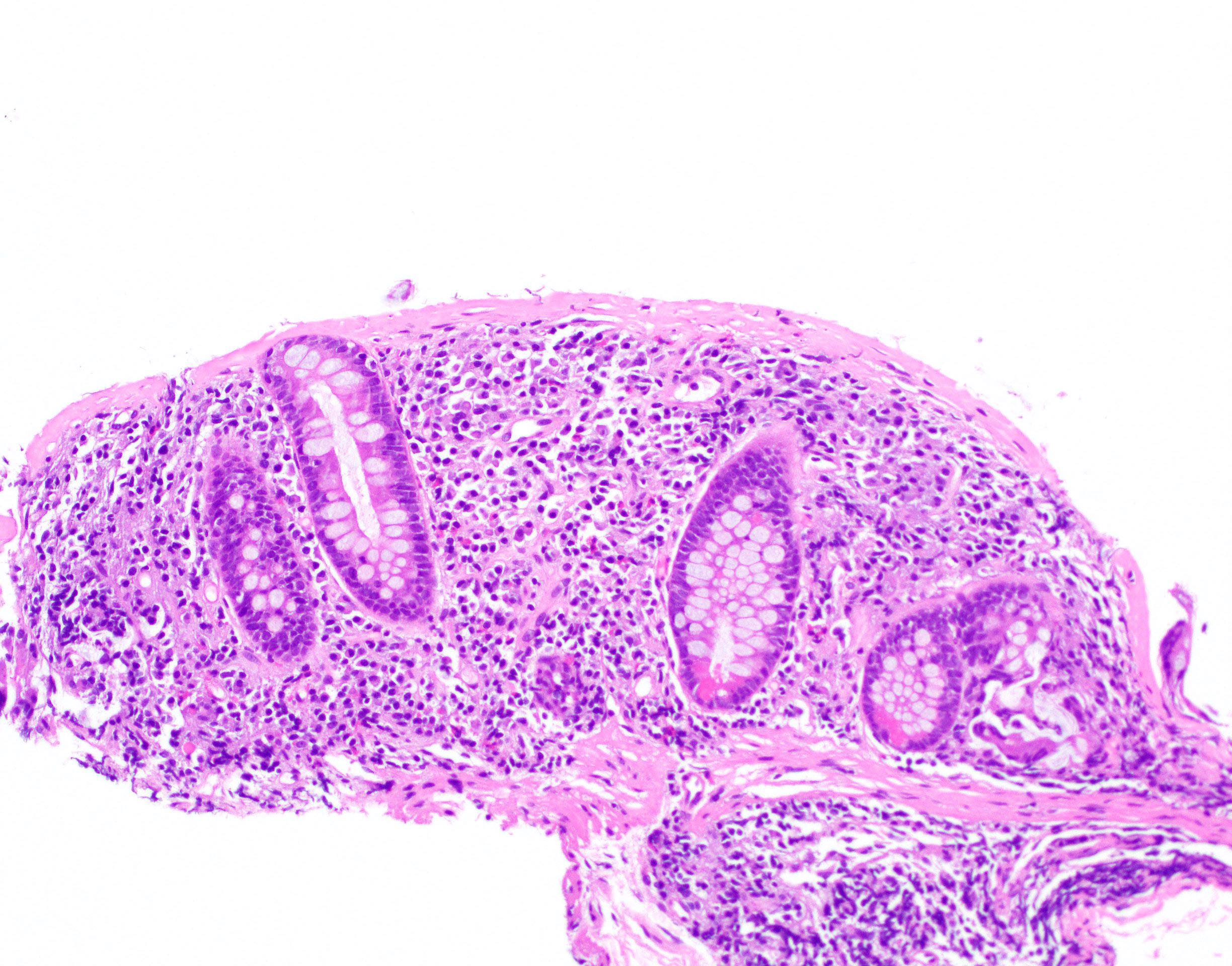
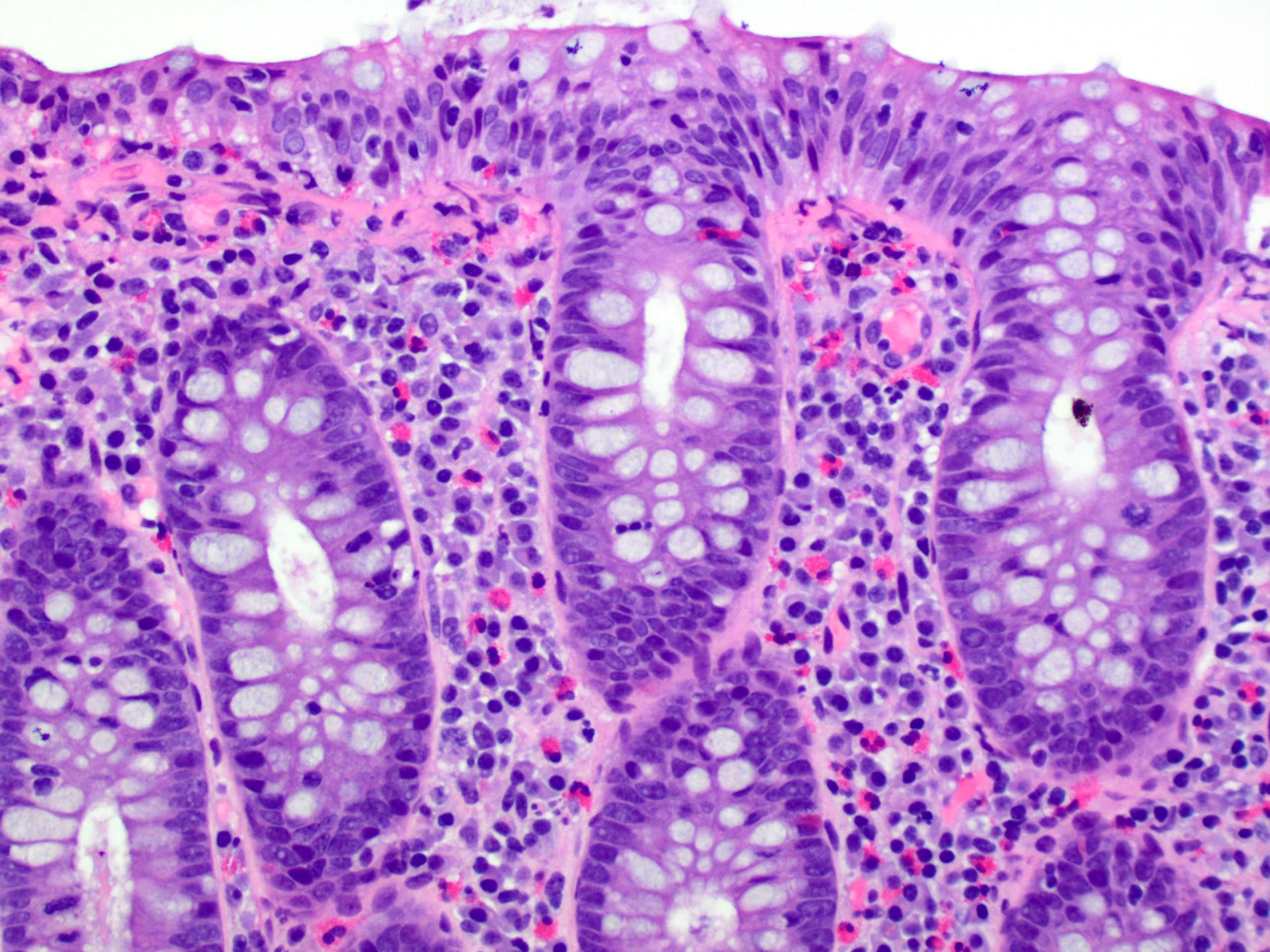
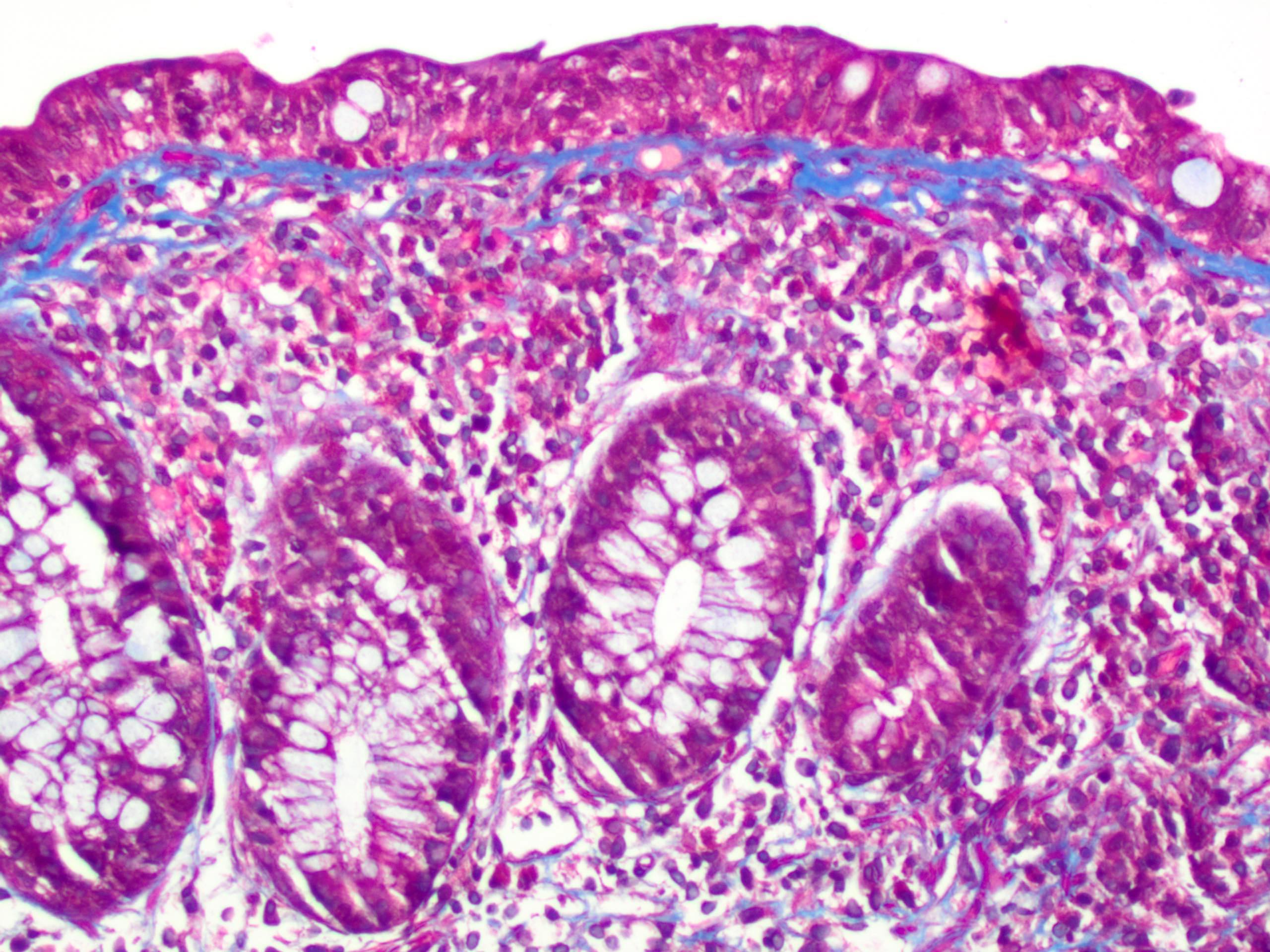
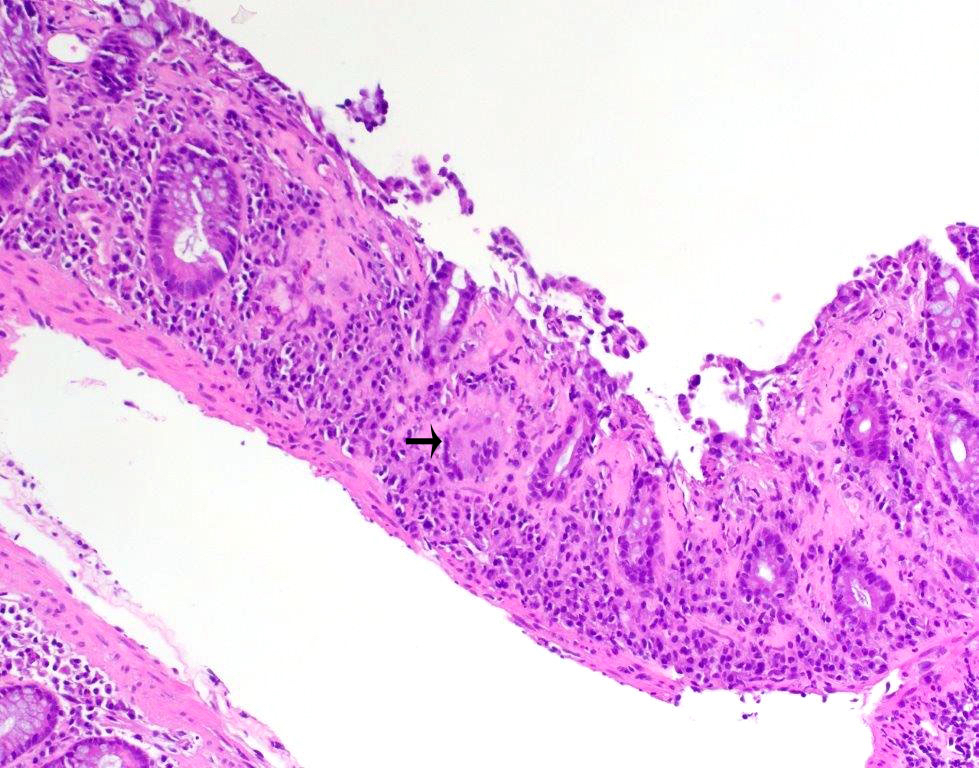
- Thickened subepithelial collagen band, usually with capillary, red blood cell and inflammatory cell entrapment (Histopathology 2015;66:613)
- Collagen band typically > 10 microns
- Occasional cases can have an irregular collagen band that is < 10 microns; some have labeled such cases as "incomplete collagenous colitis"
- Trichrome stain can be useful in equivocal cases
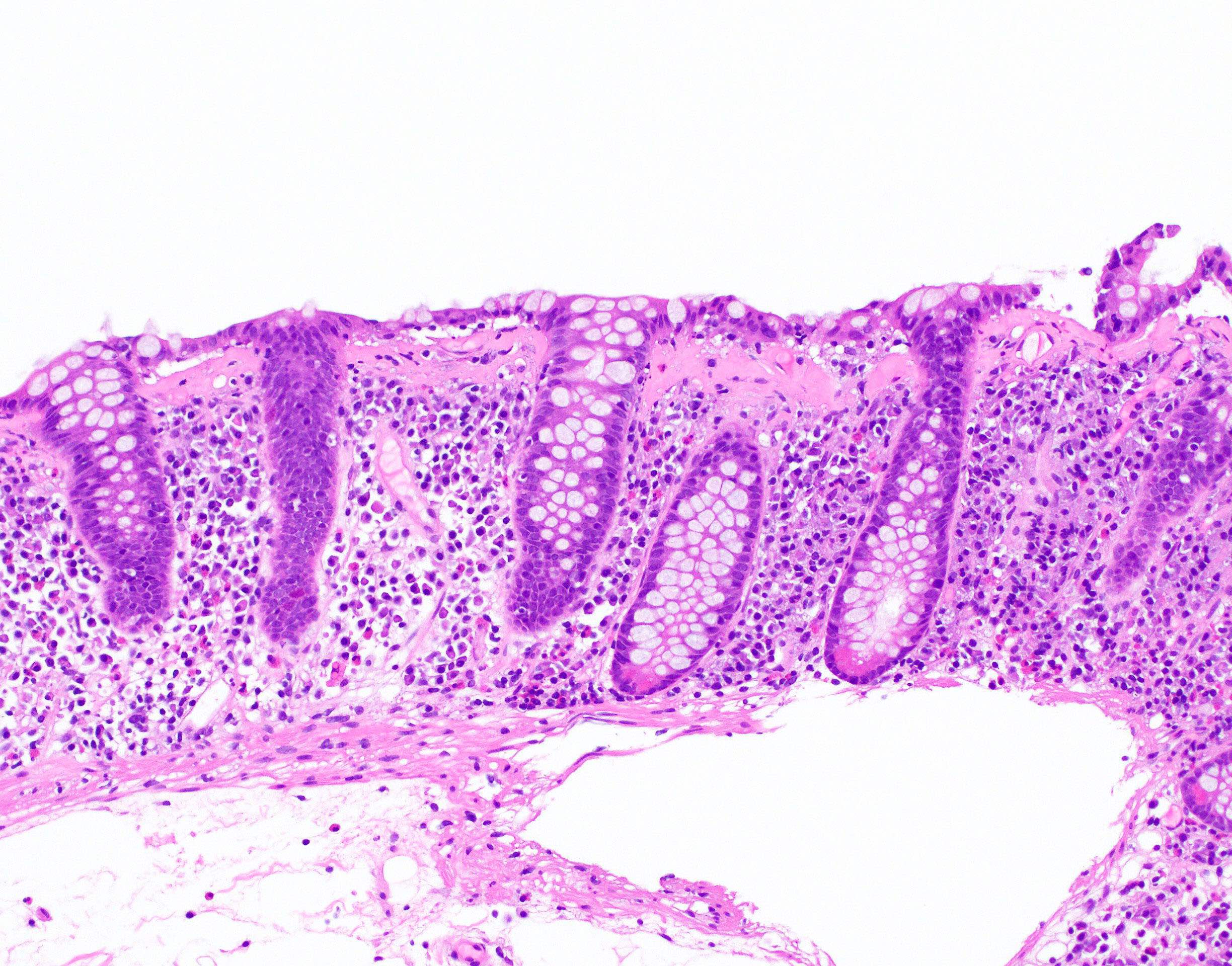
- Surface mucosal damage with loss of mucin, flattening and detachment
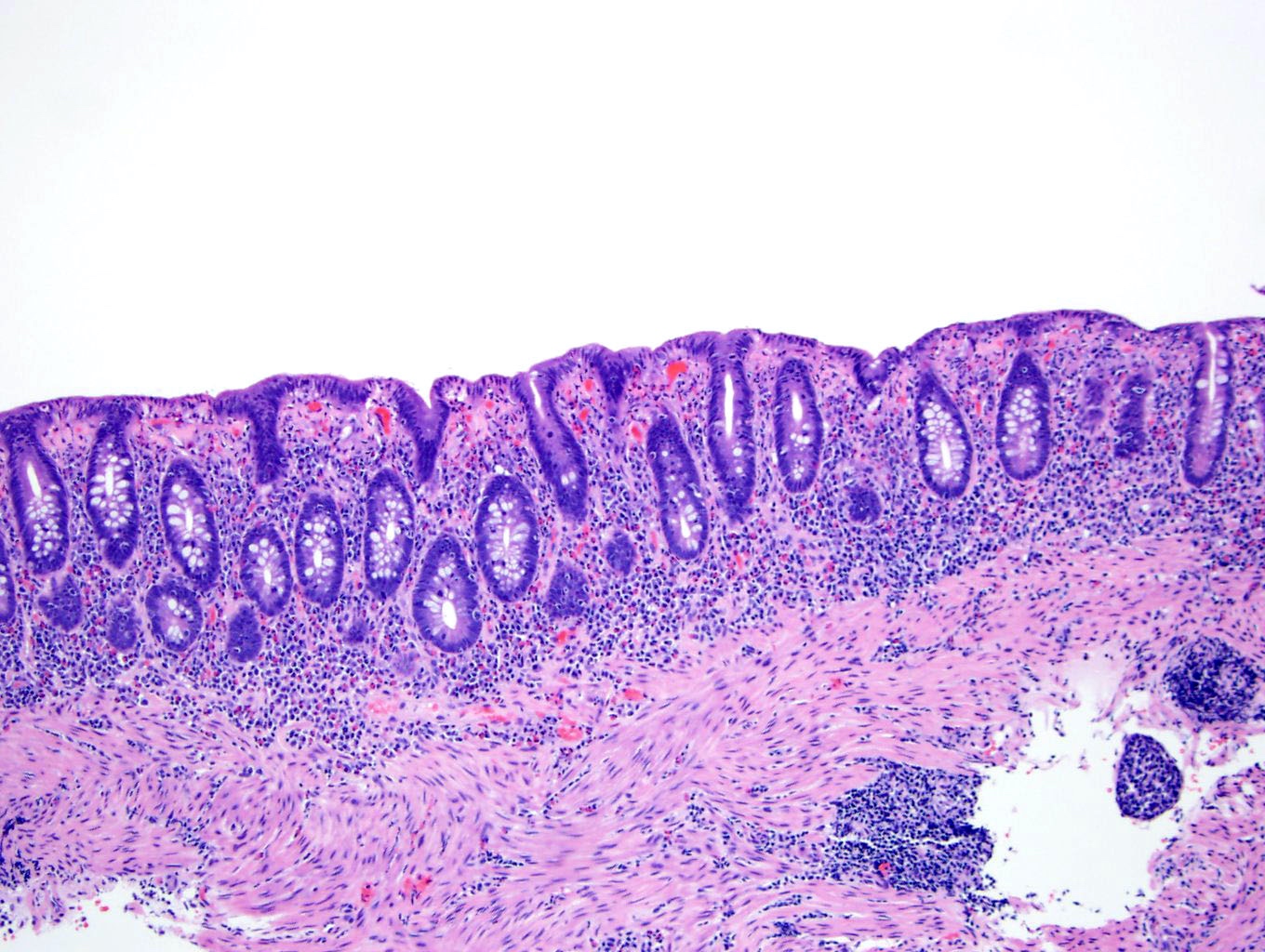
- Increased lamina propria inflammation composed of lymphocytes, plasma cells and eosinophils
- Neutrophilic inflammation can be seen but is typically not prominent
- Increased intraepithelial lymphocytes; may be mild (< 20 per 100 epithelial cells)
- Crypt architecture is preserved or minimally distorted
- Paneth cell metaplasia can be seen
- Up to 8% of cases can have crypt atrophy or irregularity (Am J Surg Pathol 2002;26:1414)
- Subepithelial multinucleated giant cells can be seen but have no clinical significance (Pathology 2008;40:671)
- Pseudomembranous collagenous colitis has been described; unclear whether truly a variant of collagenous colitis or due to superimposed infection or medication injury (Dig Dis Sci 2004;49:1763, Pathol Res Pract 2013;209:735)
Microscopic (histologic) images
Positive stains
- Masson trichrome stain highlights the subepithelial collagen band
- CD3 highlights intraepithelial lymphocytes
- Tenascin immunohistochemical stain also highlights the collagen band (Histopathology 2015;66:613)
Negative stains
- Congo red stain
Sample pathology report
- Colon, random, biopsies:
- Colonic mucosa with a thickened subepithelial collagen band, increased intraepithelial lymphocytes and surface epithelial injury, consistent with collagenous colitis
Differential diagnosis
- Lymphocytic colitis:
- Lack of subepithelial collagen band and greater number of intraepithelial lymphocytes
- Inflammatory bowel disease:
- Lack of subepithelial collagen band
- Architectural distortion and prominent neutrophilic inflammation
- Endoscopic evidence of inflammation and clinical history of bloody diarrhea
- Chronic ischemic colitis:
- Diffuse lamina propria hyalinization as opposed to a discrete subepithelial collagen band
- Withered, injured crypts
- Amyloidosis:
- Usually surrounds blood vessels, though rarely may create a subepithelial layer mimicking collagenous colitis
- Congo red stain is positive
- Lack of surface epithelial injury and inflammation
Practice question #1
A 55 year old female with a 1 year history of chronic watery diarrhea presents for evaluation. Stool ova / parasites and culture are negative for infectious organisms. Colonoscopy is performed and reveals a grossly normal appearing colon. The biopsy histology is shown. Which of the following diagnoses is correct?
- Collagenous colitis
- Crohn's colitis
- Irritable bowel syndrome
- Lymphocytic colitis
Practice answer #1
Practice question #2
A 57 year old female was recently diagnosed with collagenous colitis. Which of the following is a characteristic histologic feature of collagenous colitis?
- Architectural distortion
- Cryptitis and crypt abscess
- Granulomas
- Mixed lamina propria inflammation
Practice answer #2