Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Genetics | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3Cite this page: Mikhailov A. Systemic lupus erythematosus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneysle.html. Accessed September 15th, 2025.
Definition / general
- Lupus nephritis (LN) is an immune complex mediated renal injury encountered in systemic lupus erythematosus (SLE)
- Associated with activation of the classical complement pathway and presents as glomerular, tubulointerstitial and vascular disease, significantly increasing the risk of death in systemic lupus erythematosus patients
Essential features
- Diagnosis is made in patients with a clinical diagnosis of systemic lupus erythematosus
- Light, immunofluorescence and electron microscopy are required for the correct classification of lupus nephritis
- Lupus nephritis class is determined by the histological type of glomerular changes (mesangial, endocapillary / extracapillary, membranous or global sclerosing) and the localization and abundance of the immune complexes
- Full house immunofluorescence staining, significant C1q positivity, extraglomerular immunostaining and the finding of tubuloreticular inclusions by electron microscopy establish the lupus etiology of nephritis
Terminology
- Mesangial hypercellularity: > 3 nuclei fully surrounded by matrix in ≥ 1 mesangial areas, not including perihilar region, on a 3 um section (Kidney Int 2020;98:1120)
- Crescent: a lesion consisting of extracapillary hypercellularity forming more than 2 cell layers, composed of a variable mixture of cells
- Fibrin and fibrous matrix may be present
- 10% or more of Bowman capsule should be involved (Kidney Int 2018;93:789)
- Cellular crescent: > 75% cells and fibrin and < 25% fibrous matrix (Kidney Int 2018;93:789)
- Fibrous crescent: > 75% fibrous matrix and < 25% cells and fibrin (Kidney Int 2018;93:789)
- Fibrocellular crescent: 25 - 75% cells and fibrin and the remainder fibrous matrix (Kidney Int 2018;93:789)
- Fibrinoid necrosis: fibrin associated with glomerular basement membrane disruption or lysis of the mesangial matrix (Kidney Int 2018;93:789)
- Karyorrhexis: presence of apoptotic, pyknotic and fragmented nuclei (Kidney Int 2020;98:1120)
ICD coding
Epidemiology
- Commonly seen in women in the third decade
- More common in African, Asian and Hispanic populations than in Europeans
- Lupus nephritis most often occurs during the first 3 years after the diagnosis of systemic lupus erythematosus
- Males, patients < 33 years of age at the time of the diagnosis and non-White patients show a higher risk of developing lupus nephritis earlier in the course of systemic lupus erythematosus
- Reference: UpToDate: Lupus Nephritis - Diagnosis and Classification [Accessed 21 April 2023]
Sites
- Kidney glomeruli, tubulointerstitial compartment and less frequently, renal arteries
Pathophysiology
- Anti-double stranded DNA (dsDNA) antibody binds to dsDNA, forming an immune complex
- Immune complexes deposit in the glomerular compartments according to their charge
- Inflammatory response with activation of the classical complement pathway leads to an influx of inflammatory cells
- Complement activation damages the glomerular endothelium and dying neutrophils release nuclear antigens, enhancing the inflammatory response (Kidney Int 2016;90:493)
Etiology
- Lupus nephritis is primarily caused by type 3 (immune complex) hypersensitivity reaction
- Hydralazine can unmask and aggravate incipient lupus; other most common medications implicated in drug induced lupus are procainamide, isoniazid, minocycline and TNF inhibitors (Cureus 2019;11:e4996)
Diagrams / tables
Clinical features
- Lupus nephritis is typically detected by an abnormal urinalysis (see Laboratory)
- Classification of LN, International Society of Nephrology (ISN) / Renal Pathology Society (RPS), 2004 (J Am Soc Nephrol 2004;15:241)
- Class I, minimal mesangial LN: glomeruli are normal by light microscopy (LM), mesangial immune deposits by immunofluorescence (IF) or electron microscopy (EM)
- Class II, mesangial proliferative LN: pure mesangial hypercellularity of any degree or mesangial expansion by light microscopy, mesangial immune deposits with none or rare isolated subepithelial or subendothelial deposits by immunofluorescence or electron microscopy
- Class III, focal LN (involving < 50% of glomeruli): active or inactive focal, segmental or global endocapillary or extracapillary glomerulonephritis with focal subendothelial immune deposits by immunofluorescence / electron microscopy; mesangial alterations may or may not be present
- Class III (A), purely active lesions: focal proliferative LN
- Class III (A / C), active and chronic lesions: focal proliferative and sclerosing LN
- Class III (C), chronic inactive with glomerular scars: focal sclerosing LN
- Class IV, diffuse LN (involving > 50% of glomeruli): active or inactive diffuse endocapillary or extracapillary glomerulonephritis with diffuse subendothelial immune deposits; mesangial alterations may or may not be present
- Class IV-S: segmental lesions
- Class IV-G: global lesions
- Class IV-S (A) or IV-G (A), purely active lesions: diffuse segmental or global proliferative LN
- Class IV-S (A / C) or IV-G (A / C), active and chronic lesions: diffuse segmental or global proliferative and sclerosing LN
- Class IV-S (C) or IV-G (A / C), chronic inactive with glomerular scars: diffuse segmental or global sclerosing LN
- Class V, membranous LN: global or segmental subepithelial immune deposits at any stage () by light microscopy or immunofluorescence / electron microscopy, with or without mesangial alterations
- Class VI, advanced sclerosing LN: no activity, 90% or more of glomeruli globally sclerosed
- Combined class III / IV and V (focal or diffuse and membranous LN) may be diagnosed if the subepithelial immune deposits involve at least 50% of the glomerular capillary surface area in at least 50% of glomeruli in the presence of class III / IV lesions
- Lupus nephritis can transform from one class to another
- 2017 proposal for revision of the ISN / RPS Classification includes the elimination of the S and G subdivisions in class IV, elimination of the term endocapillary proliferation and modified activity / chronicity indices that should be applied to all classes (see Microscopic description) (Kidney Int 2018;93:789)
Diagnosis
- Patients with known lupus who develop persistent hematuria, proteinuria, active urinary sediment, elevated serum creatinine / glomerular filtration rate decrease, low complement, elevated anti-dsDNA
- Kidney biopsy establishes the diagnosis and guides treatment
Laboratory
- Class I LN: normal urinalysis, no or minimal proteinuria, normal serum creatinine
- Class II LN: microhematuria or mild proteinuria
- Class III LN: hematuria and proteinuria, which may be accompanied by nephrotic syndrome, active urinary sediment, decreased glomerular filtration rate, less frequently hypertension, rarely renal insufficiency; reduced complements and positive anti-dsDNA antibody
- Class IV LN: hematuria, proteinuria with nephrotic syndrome, red blood cell casts, hypertension, decreased glomerular filtration rate and renal failure are frequent; low complements, elevated anti-dsDNA antibody levels
- Class V LN: nephrotic range proteinuria, reduced complements, positive anti-dsDNA antibody
- Silent LN: kidney biopsy with class III, IV or V without any clinical evidence of kidney disease (UpToDate: Lupus Nephritis - Diagnosis and Classification [Accessed 21 April 2023])
Radiology description
- Ultrasound, CT, MRI and nuclear medicine have only a minor role in the diagnosis of lupus nephritis (F1000Res 2015;4:153)
- Iodine contract dyes are not indicated in patients with lupus nephritis
- MRI can detect interstitial edema in patients with lupus nephritis
Prognostic factors
- LN classes I and II: excellent renal prognosis
- LN class III: favorable prognosis with no histological progression and renal function deterioration; a small percent progressing to class IV and severe renal damage
- LN class IV: worst renal prognosis, with class IV-S possibly faring worse than IV-G (controversial)
- LN class V: predisposed to thrombotic complications, such as renal vein thrombosis and pulmonary emboli
- Serological markers of worse renal outcome are low complement levels, high titer of anti-C1q and anti-dsDNA antibodies (Lupus 2021;30:2256)
- Histological markers of worse renal outcome are significant interstitial fibrosis and tubular atrophy, vascular involvement and thrombotic microangiopathy
- African American patients, Hispanic patients and those living in poverty have a worse prognosis (UpToDate: Lupus Nephritis - Diagnosis and Classification [Accessed 21 April 2023])
- 10 - 30% of patients with lupus nephritis progress to end stage renal disease (Adv Chronic Kidney Dis 2019;26:313)
Case reports
- 24 year old woman with lupus podocytopathy superimposed on diabetic glomerulosclerosis (Medicine (Baltimore) 2021;100:e27077)
- 34 year old woman with membranous glomerulopathy diagnosed as lupus nephritis 11 years after onset (CEN Case Rep 2019;8:301)
- 51 year old woman with lupus vasculopathy presenting with favorable renal outcome (CEN Case Rep 2020;9:74)
Treatment
- Treatment is guided by the LN class, activity and chronicity indices
- LN classes I and II require blockade of the renin-angiotensin-aldosterone system (RAAS) in all patients with hypertension or proteinuria
- LN class III, class IV and class V require immunosuppressive therapy
- Goal of immunosuppressive therapy is a complete response (a substantial reduction in protein excretion, improvement or stabilization of the serum creatinine, improvement of the urinary sediment) (Ann Rheum Dis 2020;79:713)
- Immunosuppressive therapy consists of initial and subsequent phases
- Initial (induction) therapy typically consists of cyclophosphamide or mycophenolate (MMF) and glucocorticoid
- Subsequent (maintenance) therapy consists of MMF or azathioprine
- Outcomes of kidney transplantation in systemic lupus erythematosus are comparable to nonlupus patients (Adv Chronic Kidney Dis 2019;26:313)
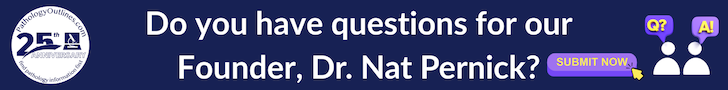
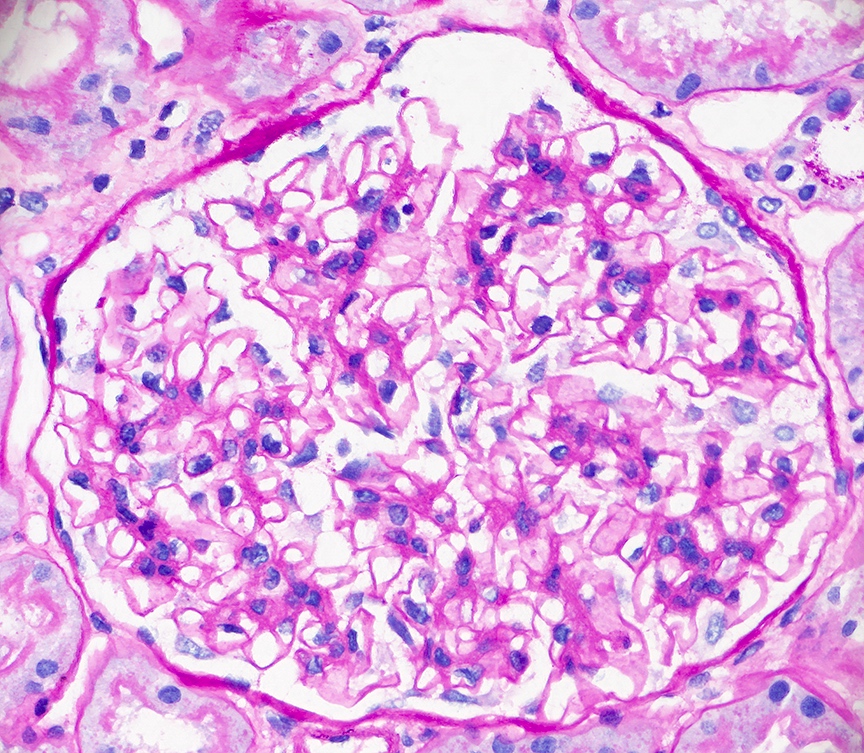
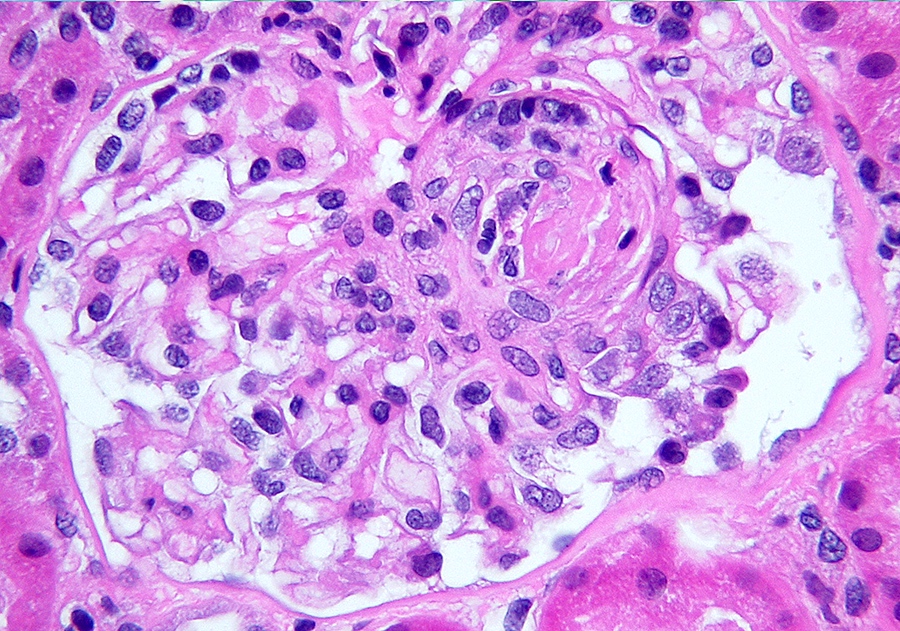
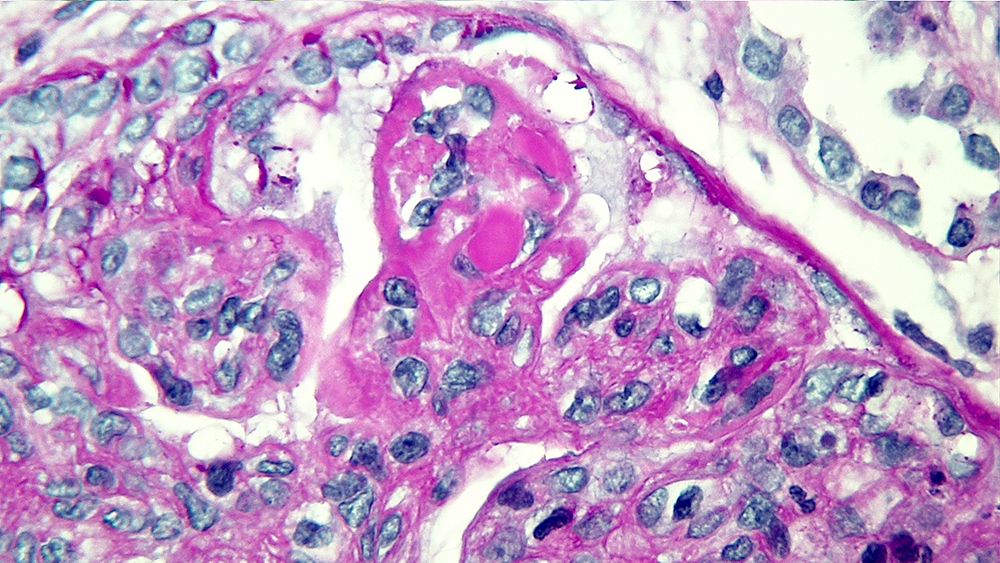
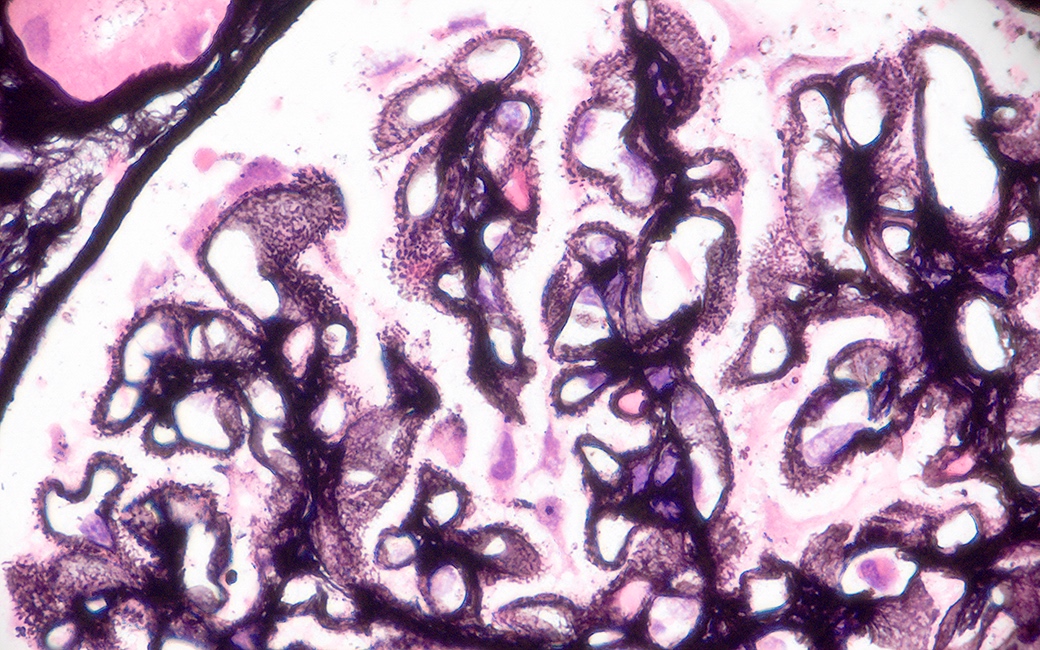
Microscopic (histologic) description
- LN class I: normal glomeruli by light microscopy
- LN class II: mesangial hypercellularity or mesangial matrix expansion
- LN classes III - IV: lesions may be active (endocapillary or extracapillary proliferation) or chronic (sclerosing)
- Wire loop deposits, hyaline microthrombi, membranoproliferative lesions
- Fibrinoid necrosis and karyorrhexis may be present
- LN class V: thickening of the glomerular capillary walls, microspikes and domes may be associated with any mesangial alterations
- LN class VI: extensive glomerular sclerosis
- Lupus podocytopathy: diffuse and severe foot process effacement in the absence of subendothelial or subepithelial immune deposits
- Tubulointerstitial disease: observed in all LN classes, active in LN classes III and IV consisting of lymphocytic interstitial inflammation with plasma cells, monocytes / macrophages and edema
- Vascular lesions: uncomplicated vascular immune deposits, noninflammatory necrotizing vasculopathy, vasculitis, thrombotic microangiopathy, vascular thrombi with recanalization in lupus anticoagulant syndrome
- LN activity and chronicity scoring system modified in 2018 and is based on scoring of 1 (< 25% of glomeruli), 2 (25 - 50% of glomeruli) and 3 (> 50% of glomeruli) (Kidney Int 2018;93:789)
- LN activity index
- Endocapillary proliferation
- Neutrophils / karyorrhexis
- Fibrinoid necrosis (score x 2)
- Hyaline deposits
- Cellular / fibrocellular crescents (score x 2)
- Interstitial inflammation (total score 0 - 24)
- LN chronicity index
- Total glomerulosclerosis score (global or segmental sclerosis; exclude sclerosis due to hypertension and normal aging)
- Fibrous crescents
- Tubular atrophy
- Interstitial fibrosis (total score 0 - 12)
- Reference: Clin Rev Allergy Immunol 2011;40:170
Microscopic (histologic) images
Contributed by Alexei Mikhailov, M.D., Ph.D.
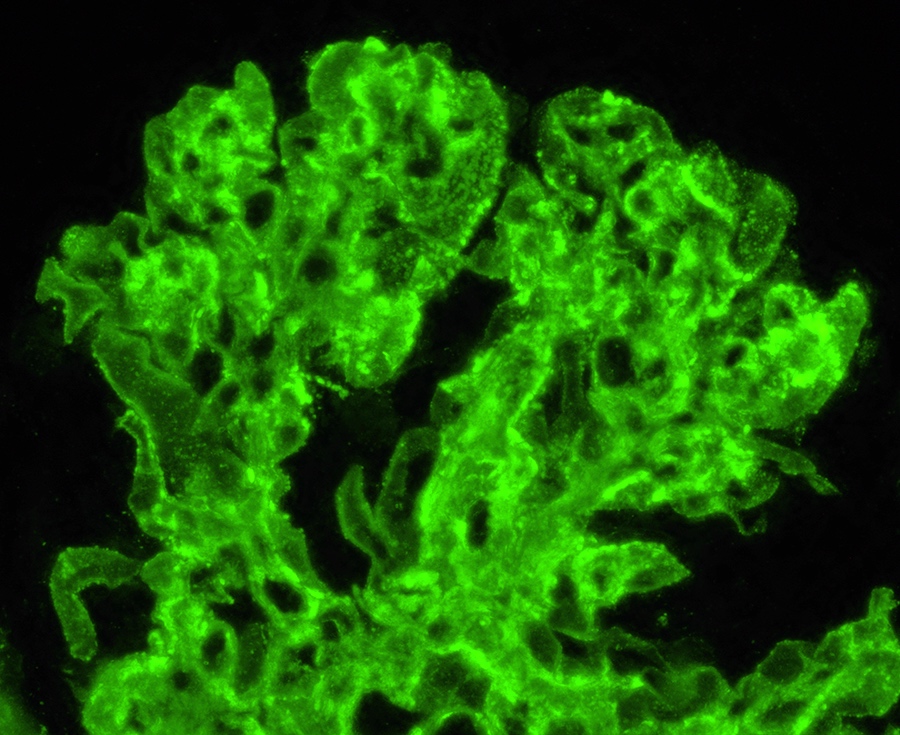
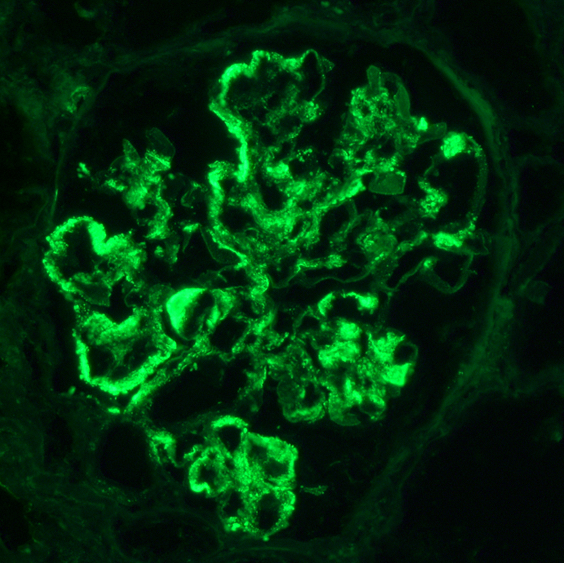
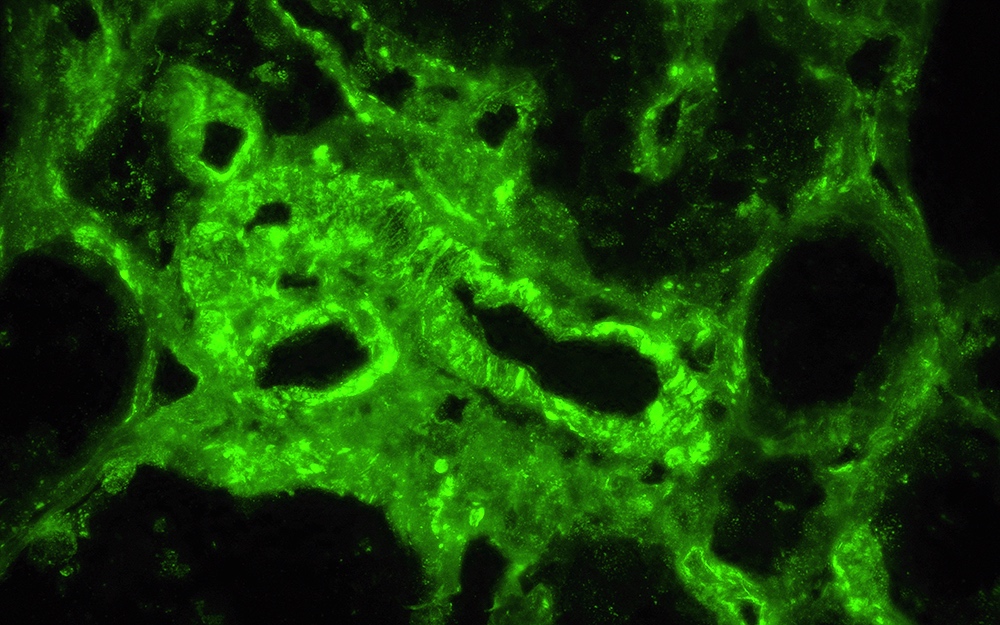
Immunofluorescence description
- Diagnostic criteria: IgG dominant full house immunofluorescence (positive IgG, IgA, IgM, C3, C1q, kappa and lambda light chains)
- Especially important are C1q positivity and extraglomerular immunostaining on the Bowman capsules, arteries, tubular basement membranes and in the interstitium
- Immunofluorescence staining is granular and may be subepithelial, intramembranous, subendothelial or mesangial
- In some cases, antinuclear antibody (ANA) test is seen with antibodies to IgG and the light chains
- Reference: Clin J Am Soc Nephrol 2019;14:1605
Immunofluorescence images
Positive stains
- PAS special stain is the most useful staining method in every LN class to evaluate mesangial and endocapillary changes
- Masson trichrome special stain is most useful in LN classes III and IV and helps to detect foci of fibrinoid necrosis, glomerular and interstitial sclerosing changes
- PAMS (Jones Silver) special stain is most useful in LN class V and emphasizes capillary wall thickening and neomembrane formation (microspikes and domes)
- IgG1, IgG2 and IgG3 subclasses are highly expressed in lupus nephritis (Intern Med 2002;41:936)
- CD68 immunostaining identifies cells of macrophage lineage, especially useful in evaluating hypercellular glomeruli (Kidney Int Rep 2022;7:841)
Negative stains
- PLA2R
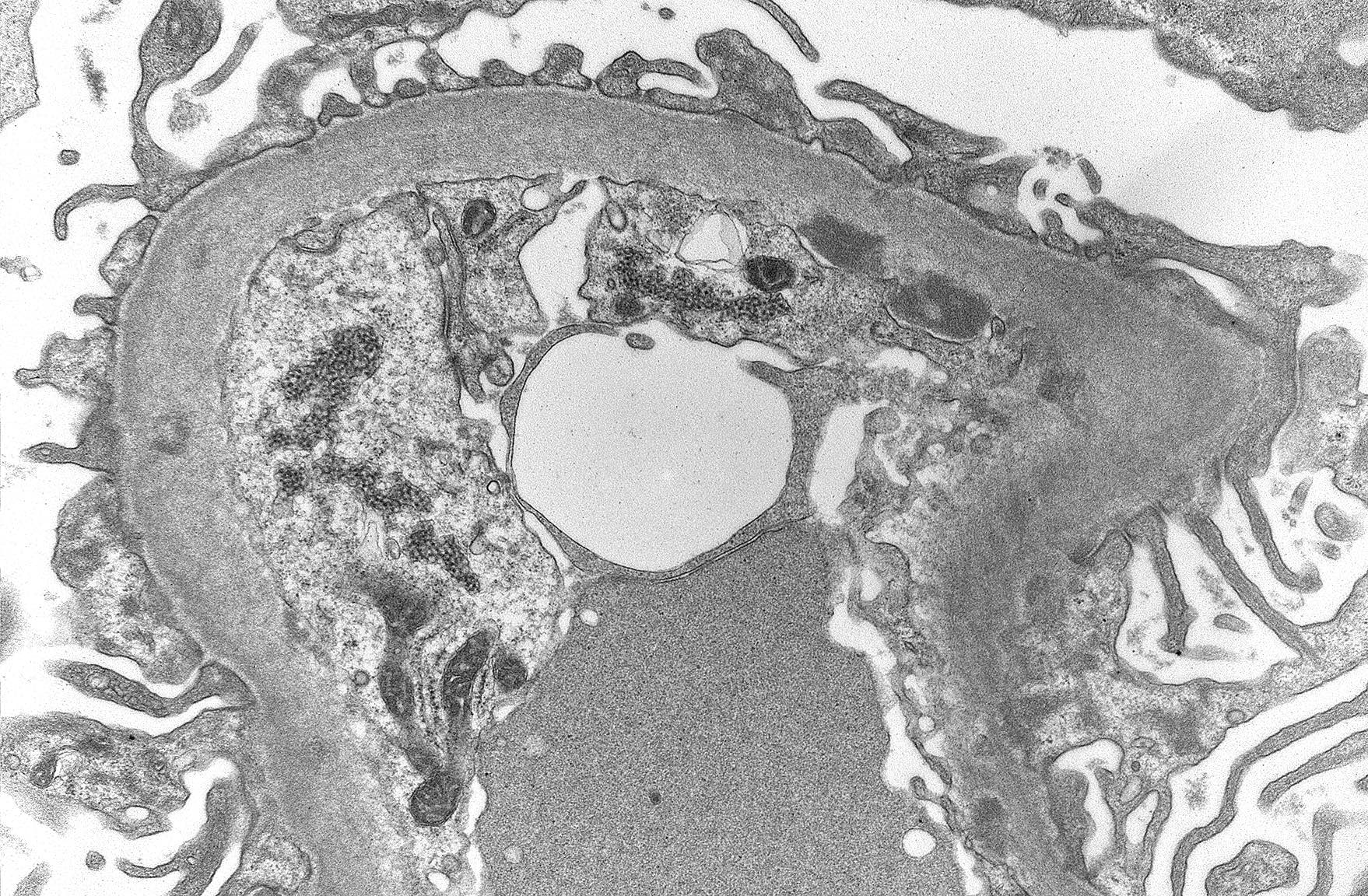
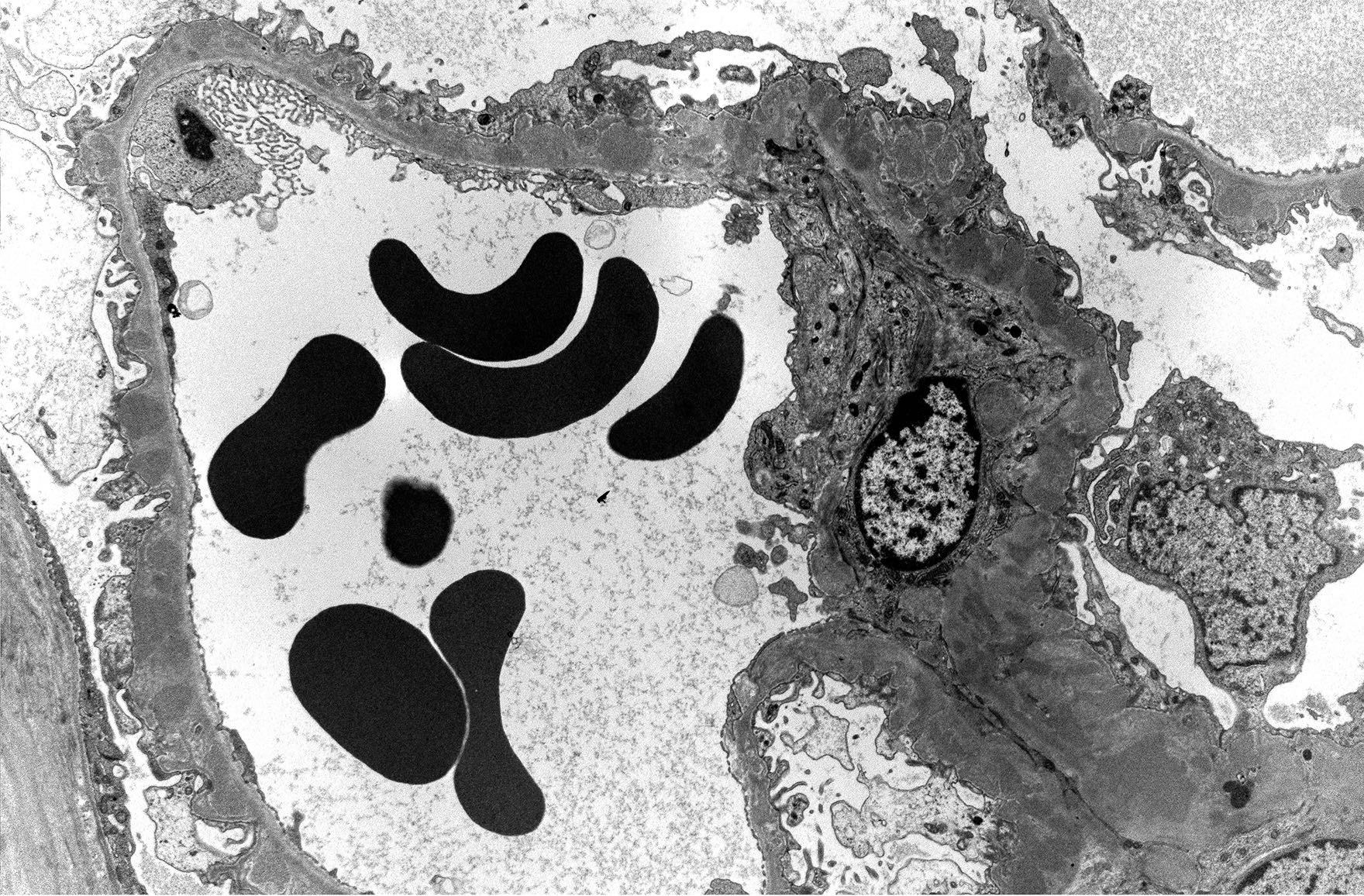
Electron microscopy description
- Finalizes the classification of lupus nephritis for a given case
- Granular electron dense deposits (smaller in LN classes I - II and larger in classes III - IV) are seen in subepithelial, intramembranous, subendothelial and mesangial locations; locations are important in determining the LN class
- Subepithelial immune deposits show adjacent neomembrane formation
- Immune deposit substructure may be present
- Tubuloreticular inclusions: reticular aggregates of branching membranous tubule within the cisternae of endoplasmic reticulum found within the endothelial cells are useful in establishing the diagnosis of lupus erythematosus; are also found in other conditions with elevated levels of interferon (Pathology 2019;51:727)
Electron microscopy images
Genetics
- HLA-DR3, HLA-DR15 and HLA-DR3 are risk alleles for lupus nephritis (Clin Immunol 2017;185:32)
- Variants in ITGAM (CD11b integrin), FCGR (Fc gamma receptor), IRF5 (interferon regulatory factor 5), TNIP1 (inhibitor of NFκB 1), TNFSF4 (TNF super family 4), APOL1 (apolipoprotein L1), PDGFRA (platelet derived growth factor receptor alpha) are associated with lupus nephritis (Clin Immunol 2017;185:32)
Sample pathology report
- Kidney, biopsy:
- Diffuse glomerulonephritis with 20% cellular crescents (4/20) and fibrinoid necrosis and focal and segmental glomerular scarring, consistent with lupus nephritis ISN / RPS class IV-G (A / C) (see comment)
- 10% focal global glomerulosclerosis (2/20)
- Mild arteriosclerosis
- Mild interstitial fibrosis and tubular atrophy
- Comment: activity - 8/24, chronicity - 3/12
- Clinical information: The patient is a 47 year old woman with a history of systemic lupus erythematosus and hypertension. Recent lupus flare, proteinuria and acute kidney injury.
- Laboratory data
- Serum creatinine: 1.5 mg/dL
- UPC: 1800 mg/g creatinine
- C3: 47 mg/dL
- C4: 48 mg/dL
- Urinalysis: 150 RBC/HPF, 40 WBC/HPF
- Light microscopy: The biopsy consists of tissue from the renal cortex. The tissue is sampled at 10 levels of section with H&E, PAS, trichrome and PAMS stains. Per level of section up to 20 glomeruli are available, of which 2 are globally sclerosed and a few are segmentally sclerosed. 4 glomeruli display cellular crescents, fibrinoid necrosis and karyorrhexis in the capillary tuft and in the crescent. The nonsclerosed glomeruli display marked endocapillary hypercellularity. Tubules show focally flattened epithelium and absent brush borders; small foci of interstitial lymphocytic infiltration are seen. There is mild interstitial fibrosis and tubular atrophy. Arteries of the medium caliber are present and show mild intimal fibroelastosis; there is no significant arteriolar hyalinosis.
- Immunofluorescence microscopy: Up to 5 nonsclerosed glomeruli are available for evaluation. Mild to high intensity granular immunofluorescence staining was detected in the mesangial areas and less in the capillary walls with antibodies to IgG (4+), IgA (3+), IgM (2+), C3 (4+), C1q (3+), kappa light chains (4+) and lambda light chains (4+). Extraglomerular staining is seen on the arterial walls with antibodies to IgG.
- Semithin sections: 4 nonsclerosed glomeruli are available and 1 of them shows a fibrocellular crescent. All glomeruli show endocapillary hypercellularity. Foci of mild lymphocytic infiltration are seen in the interstitium.
- Electron microscopy: Glomerular basement membranes are of normal thickness. Numerous subendothelial electron dense (immune complex) deposits are seen. There is mild segmental podocyte foot process effacement. Capillary lumens are patent. The mesangium shows a moderately expanded mesangial matrix and contains large electron dense deposits.
Differential diagnosis
- IgA nephropathy:
- IgA dominant
- Postinfectious glomerulonephritis:
- Hump-like subepithelial immune deposits do not show adjacent microspikes
- C1q nephropathy:
- No clinical or serological evidence of lupus
- Primary (idiopathic) membranous glomerulopathy:
- Membranoproliferative glomerulonephritis:
- No C1q positivity
- Fibrillary glomerulonephritis:
- DNAJB9 positive
- Drug induced lupus nephritis:
- No dsDNA antibodies
Additional references
Practice question #1
A 40 year old patient with a history of systemic lupus erythematosus is presenting with acute kidney injury and a new onset nephrotic syndrome. dsDNA is positive, C3 is 50 mg/dL, serum creatinine is 1.5 mg/dL and the urinary protein to creatinine ratio is 3,500 mg/g. Which of the following histological manifestations is most characteristic of the lupus nephritis class he is most likely presenting with?
- Acute tubular injury
- ANA reaction
- Mesangial electron dense deposits
- Microspikes and domes (neomembrane formation) seen with the Jones stain
Practice answer #1
D. Microspikes and domes (neomembrane formation) seen with the Jones stain. Neomembrane formation is most characteristic for lupus nephritis (LN) class V, even though it may sometimes be seen if subepithelial deposits are present in LN class IV. Answers A, B and C are incorrect because acute tubular injury, ANA reaction and mesangial electron dense deposits may be seen in any LN class.
Comment Here
Reference: Systemic lupus erythematosus
Comment Here
Reference: Systemic lupus erythematosus
Practice question #2
Which of the following is most specific to lupus nephritis and helpful in differentiating between lupus nephritis and other etiologies?
- Hyaline microthrombi
- Mesangial proliferation
- Positive immunostaining on the arterioles and tubular basement membranes with antibodies to IgG
- Subendothelial electron dense deposits
Practice answer #2
C. Positive immunostaining on the arterioles and tubular basement membranes with antibodies to IgG. Extraglomerular immunostaining is very specific to lupus nephritis. Answer A is incorrect because hyaline microthrombi in the glomerular capillaries may also be seen in other conditions; for example, cryoglobulinemia (cryoglobulin plugs) and microthrombi consisting of monoclonal immunoglobulins in immunotactoid glomerulopathy.
Answer B is incorrect because mesangial proliferation may be seen in a very wide range of etiologies, including minimal change disease, IgA nephropathy, focal segmental glomerulosclerosis (FSGS), Alport syndrome, etc. Answer D is incorrect because subendothelial electron dense deposits may be seen in any renal disease where immune complexes are formed (e.g., IgA nephropathy and postinfectious glomerulonephritis).
Comment Here
Reference: Systemic lupus erythematosus
Comment Here
Reference: Systemic lupus erythematosus
Practice question #3
Biopsy is done on a patient with a history of systemic lupus erythematosus and nephrotic syndrome. Electron microscopy reveals the findings shown above. Which complication is the patient predisposed to?
- Fibromuscular dysplasia of the renal artery
- Oxalate nephropathy
- Papillary necrosis
- Renal vein thrombosis
Practice answer #3
D. Renal vein thrombosis. The risk of deep vein thrombosis, especially renal vein thrombosis, is increased in patients with lupus nephritis classes III, IV and V but especially in patients with membranous lupus nephritis (class V). Answer A is incorrect because fibromuscular dysplasia of the renal artery is a noninflammatory process leading to arterial stenosis. Answer B is incorrect because oxalate nephropathy is associated with deposition of calcium oxalate crystals in kidney tubules. The etiology includes primary hyperoxaluria, enteric hyperoxaluria (fat malabsorption) and ingestions (e.g., ethylene glycol poisoning). Answer C is incorrect because papillary necrosis is a complication of NSAID nephropathy.
Comment Here
Reference: Systemic lupus erythematosus
Comment Here
Reference: Systemic lupus erythematosus