Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Chan AWH. Cirrhosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livercirrhosis.html. Accessed September 9th, 2025.
Definition / general
- Diffuse nodulation of liver due to fibrous bands subdividing liver into regenerative nodules
Essential features
- Diffuse nodulation of liver due to fibrous bands subdividing liver into regenerative nodules
- Viral hepatitis B / C, alcoholic liver disease, nonalcoholic (metabolic associated) fatty liver disease are most common causes
ICD coding
Epidemiology
- Major cause of global health burden, accounting for 1.2% of disability adjusted life years (DALYs) and 2% of deaths worldwide in 2010 (Lancet 2012;380:2197, Lancet 2012;380:2095)
Sites
- Liver
Pathophysiology
- Combination of processes (J Hepatol 2017;66:778)
- Fibrosis: excessive production of collagen type I / III by hepatic stellate cells with or without portal fibroblasts through chronic inflammation (tumor necrosis factor [TNF] alpha), transforming growth factor [TGF] beta, IL1), cytokines from Kupffer cells, endothelial cells, bile duct cells, hepatocytes and disruption of extracellular matrix and toxins
- Regeneration of hepatocytes through proliferation of progenitor cells of the ductular reaction
- Parenchymal extinction due to vascular disruption
- Regression (J Hepatol 2015;63:1038)
- Cirrhosis is potentially reversible after successful treatment of chronic liver disease, e.g. viral hepatitis
- Cessation of chronic damage allows hepatocyte recovery and modulates the microenvironment
- Shifting balance from inflammation to resolution results in phenotypic adjustments of immune cells
- Myofibroblasts are deactivated by senescence, apoptosis and inactivation
- Matrix degradation also occurs
Etiology
- Prevalence of causes varies by geographic location
- Common causes include:
- Chronic viral hepatitis B (with or without D) and C
- Fatty liver disease: alcoholic and nonalcoholic (metabolic associated)
- Metabolic: hereditary hemochromatosis, alpha-1 antitrypsin deficiency, Wilson disease
- Immune mediated: autoimmune hepatitis, primary biliary cholangitis, primary sclerosing cholangitis
- Chronic biliary obstruction
- Drug induced liver injury
- Cryptogenic (idiopathic) cirrhosis: accounts for 8 - 9% of liver transplants in the U.S.; burnt out nonalcoholic fatty liver disease (NAFLD) / nonalcoholic steatohepatitis (NASH) is a common cause of cryptogenic cirrhosis (Hepatology 2000;32:689)
Clinical features
- General (nonspecific): malaise, fatigue, anorexia, weight loss
- Specific (due to impaired liver function):
- Impaired protein synthesis (leukonychia [white nails], ascites, bruising)
- Impaired biliary excretion (jaundice, pruritus)
- Impaired nitrogen metabolism (hepatic encephalopathy)
- Impaired estrogen metabolism (palmar erythema, spider nevus, testicular atrophy, gynecomastia)
- Complications:
- Decompensation: development of jaundice, ascites, variceal hemorrhage or hepatic encephalopathy
- Portal hypertension: ascites (with or without spontaneous bacterial peritonitis), splenomegaly, esophageal / gastric varices
- Liver failure: coagulopathy, hepatic encephalopathy, hepatorenal syndrome, hepatopulmonary syndrome, portopulmonary hypertension
- Hepatocellular carcinoma: cirrhosis is a key risk factor and the annual incidence of HCC among cirrhotic patients is 2 - 8% (Lancet 2014;384:2053, Hepatology 2010;51:1972)
Diagnosis
- Ultrasound, CT or MRI radiologically
- Elastography
- Liver biopsy
Laboratory
- Clinical subclassification of cirrhosis uses blood with or without clinical parameters
- Child-Pugh score / grade (J Hepatol 2005;42:S100)
- 5 parameters: albumin, bilirubin, international normalized ratio (INR) / prothrombin time, ascites and hepatic encephalopathy
- Each parameter is assigned from 1 - 3
- Total score ranges from 5 - 15 and is categorized as grade A (5, 6), B (7 - 9) and C (10 - 15)
- Model for end stage liver disease (MELD) score (J Hepatol 2005;42:S100)
- 3 parameters: bilirubin, creatinine and INR
- Used to prioritize need for liver transplantation
- Albumin bilirubin (ALBI) score / grade (J Clin Oncol 2015;33:550)
- 2 parameters: albumin, bilirubin
- Simple, objective and evidence based alternative of Child-Pugh score / grade
Radiology description
- There are multiple nodular isodense lesions deforming the liver margin on the arterial phase CT
Case reports
- 28 year old woman with cirrhosis secondary to autoimmune hepatitis and alpha-1 antitrypsin ZZ phenotype (Cureus 2021;13:e12606)
- 44 year old man with Wilson disease presenting with muscle stiffness, gait instability and liver cirrhosis (Lancet 2020;396:990)
- 62 year old man with cirrhosis took daily probiotics and developed Lactobacillus associated spontaneous bacterial peritonitis (Cureus 2020;12:e11896)
Treatment
- Treating the underlying cause of cirrhosis
- Treating and preventing complications (ascites, hepatic encephalopathy, variceal hemorrhage, and portal hypertension)
- Avoid additional liver injury (e.g. alcohol)
- Patients with MELD ≥ 15 or decompensation should be referred to a transplant center (Hepatology 2014;59:1144)
- Regular ultrasound surveillance of HCC (Hepatology 2018;68:723)
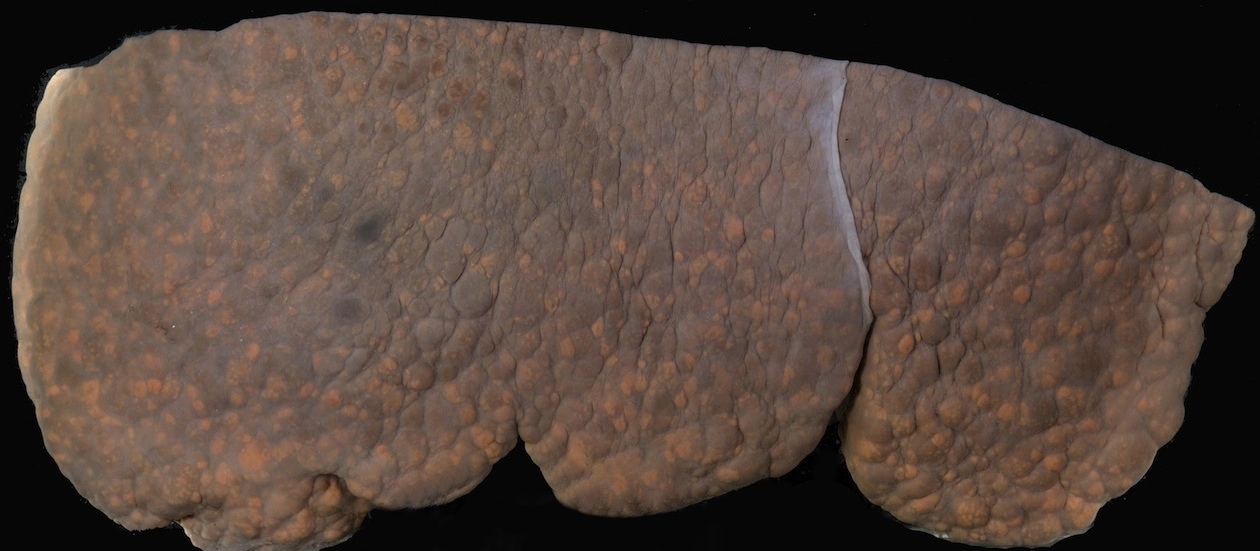
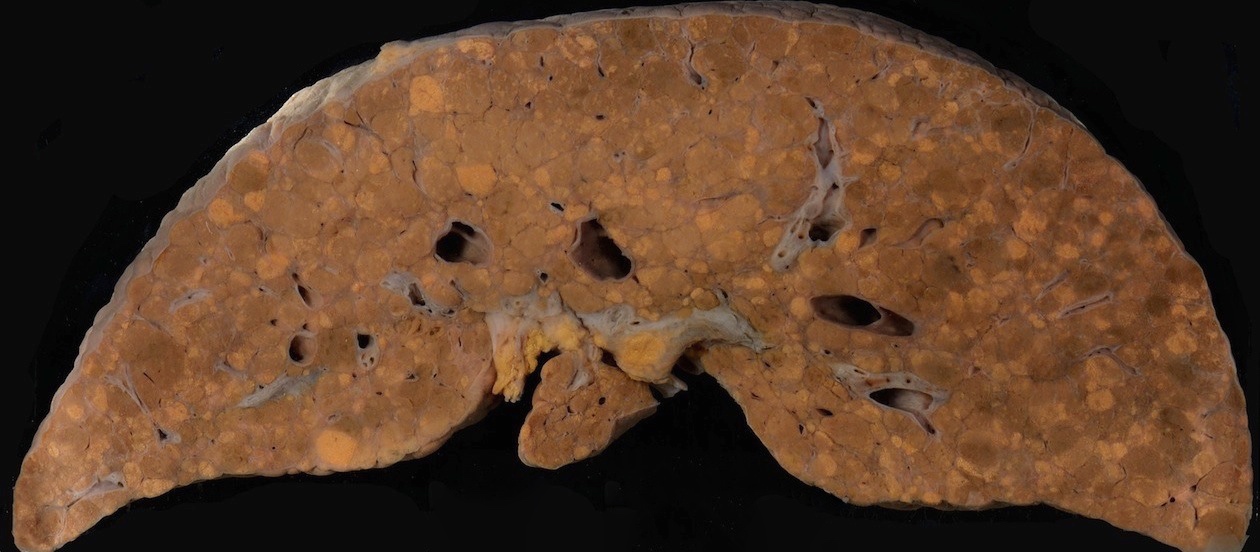
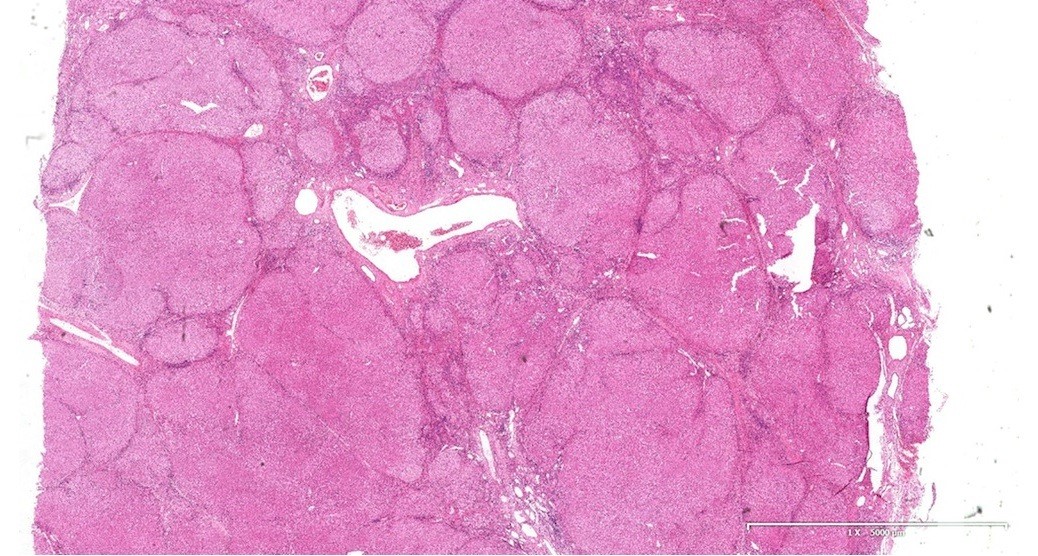
Gross description
- Multiple regenerative nodules throughout the entire liver, separated by bridging fibrosis
Gross images
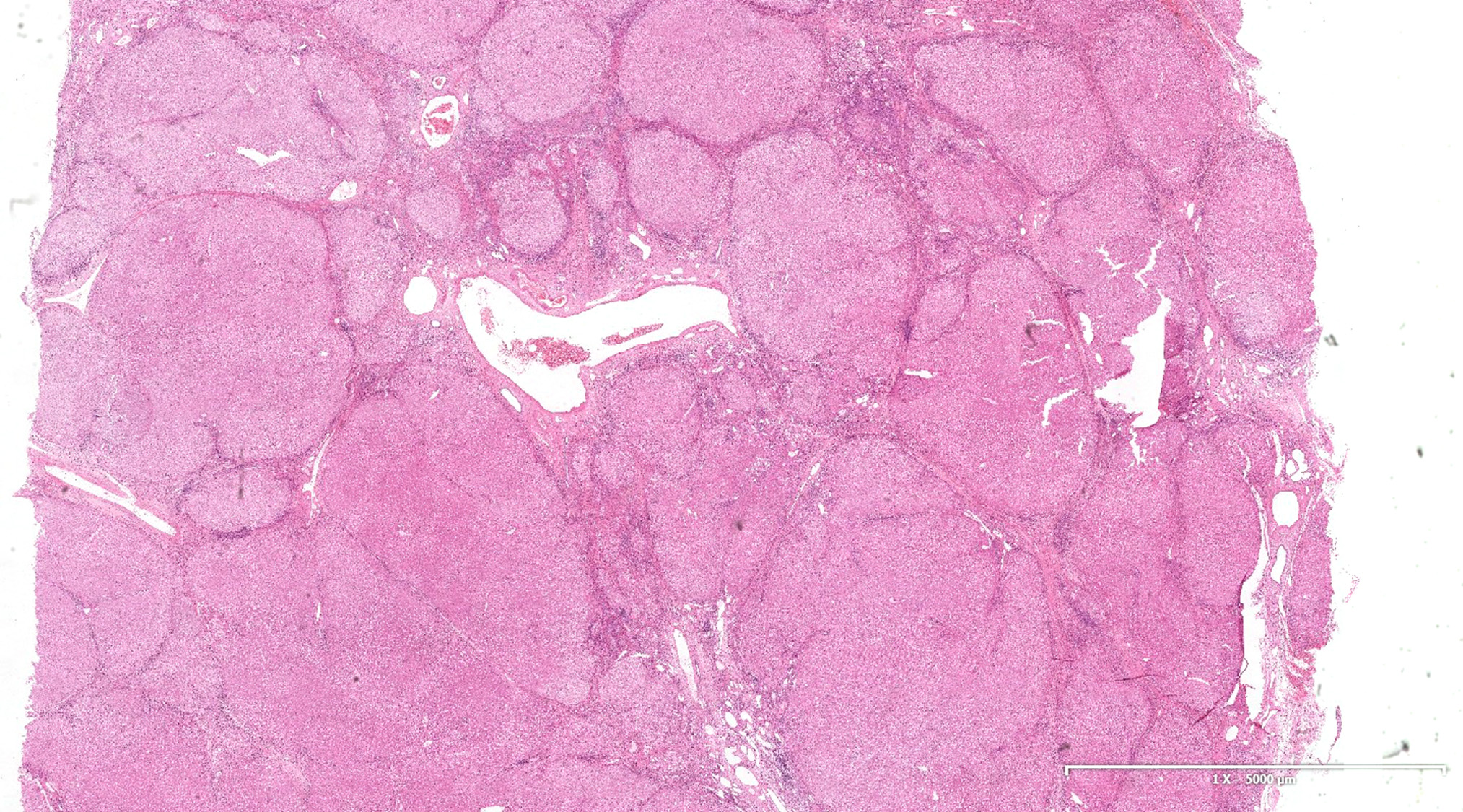
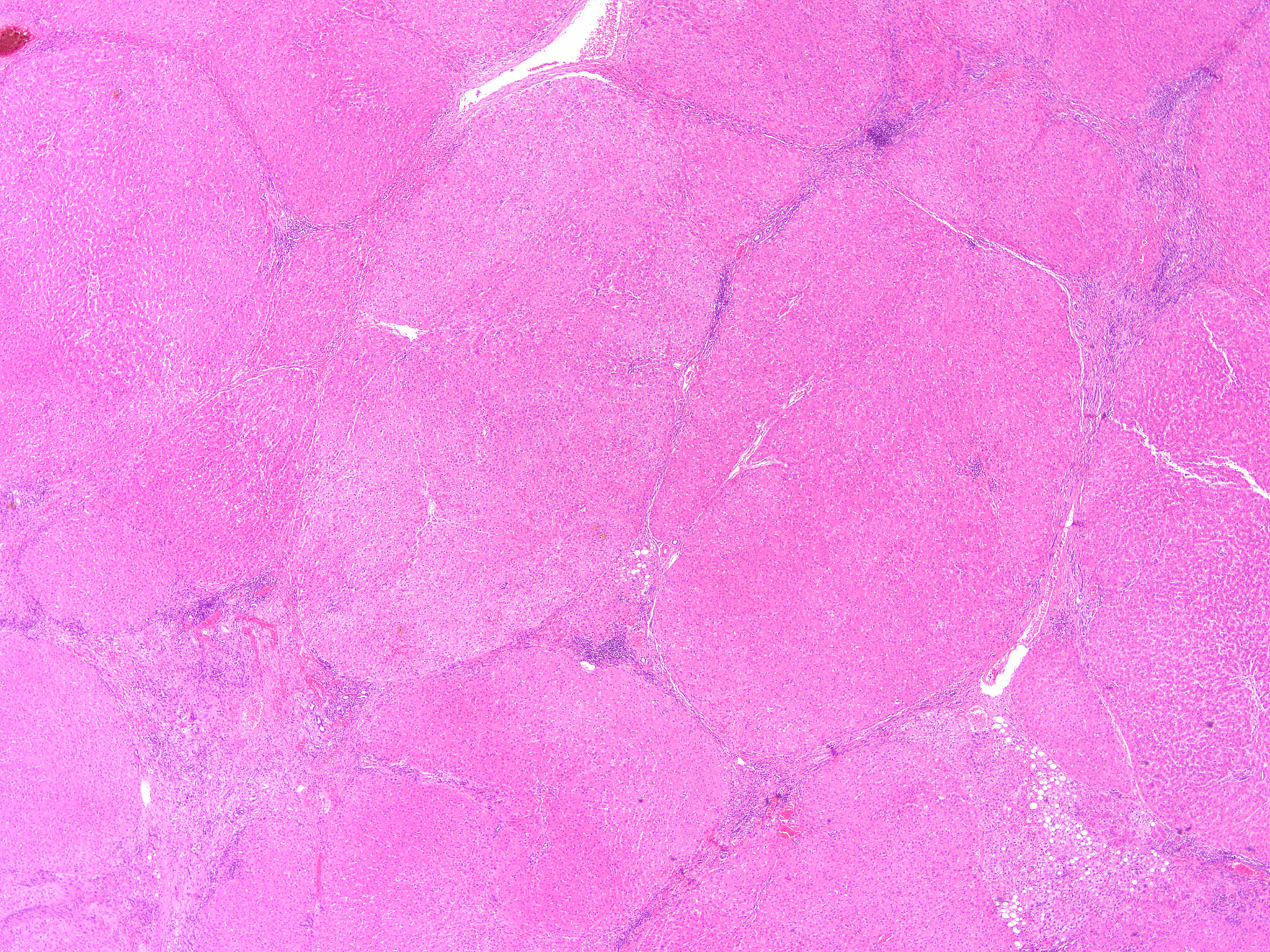
Microscopic (histologic) description
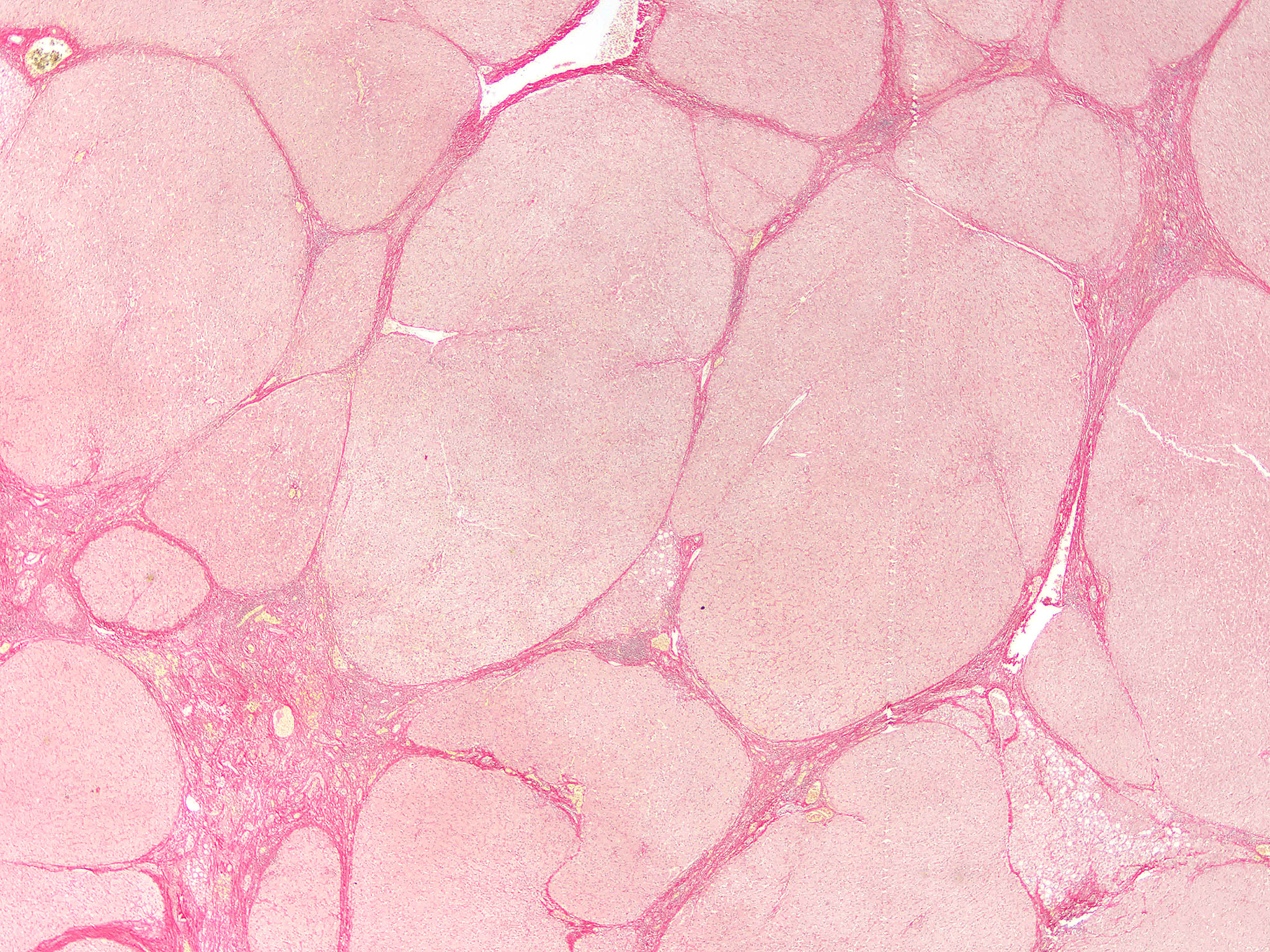
- Nonbiliary type cirrhosis:
- Diffuse disruption in architecture of the entire liver (loss of normal central - portal relationship)
- Bridging fibrous septa
- Rounded parenchymal nodules of regenerating hepatocytes
- Biliary type cirrhosis:
- Diffuse disruption in architecture of the entire liver (loss of normal central - portal relationship)
- Bridging fibrous septa
- Irregular, jigsaw puzzle shaped parenchymal nodules of regenerating hepatocytes with peripheral pale halo (peripheral septal edema, loose packed fibrous tissue and chronic cholestasis of periseptal hepatocytes leading to feathery degeneration)
- Alcoholic type cirrhosis:
- Micronodular cirrhosis, Mallory bodies, fatty change
- Perivenular and pericellular fibrosis (highlighted with trichrome stain) with partial / complete obliteration of central vein (identifiable as central vein due to lack of arterioles)
- More prominent bridging from central zone to central zone and central zone to portal zone than in other causes of cirrhosis
- Usually few inflammatory cells, unless superimposed viral or alcoholic hepatitis
- Subclassification: micronodular (< 3 mm) versus macronodular (≥ 3 mm)
- Typically not very clinically significant
- Former is more commonly associated with alcoholic liver disease, genetic hemochromatosis and Wilson disease, whereas the latter is more frequently associated with viral hepatitis
- Micronodular cirrhosis and macronodular cirrhosis may be transformed into each other in either direction, depending on disease activity (Arch Pathol Lab Med 2000;124:1599)
- Difficult to assess in liver biopsy specimen
- Subclassification: Laennec fibrosis scoring system (J Hepatol 2011;55:1004)
- 4A: mild cirrhosis; marked septation with rounded contours or visible nodules; most septa are thin (1 broad septum allowed)
- 4B: moderate cirrhosis with at least 2 broad septa
- 4C: severe cirrhosis with at least 1 very broad septum or many minute nodules
- Excellent interobserver agreement (kappa 0.83)
- Correlate with severity of portal hypertension and Child-Pugh and MELD scores
Microscopic (histologic) images
Positive stains
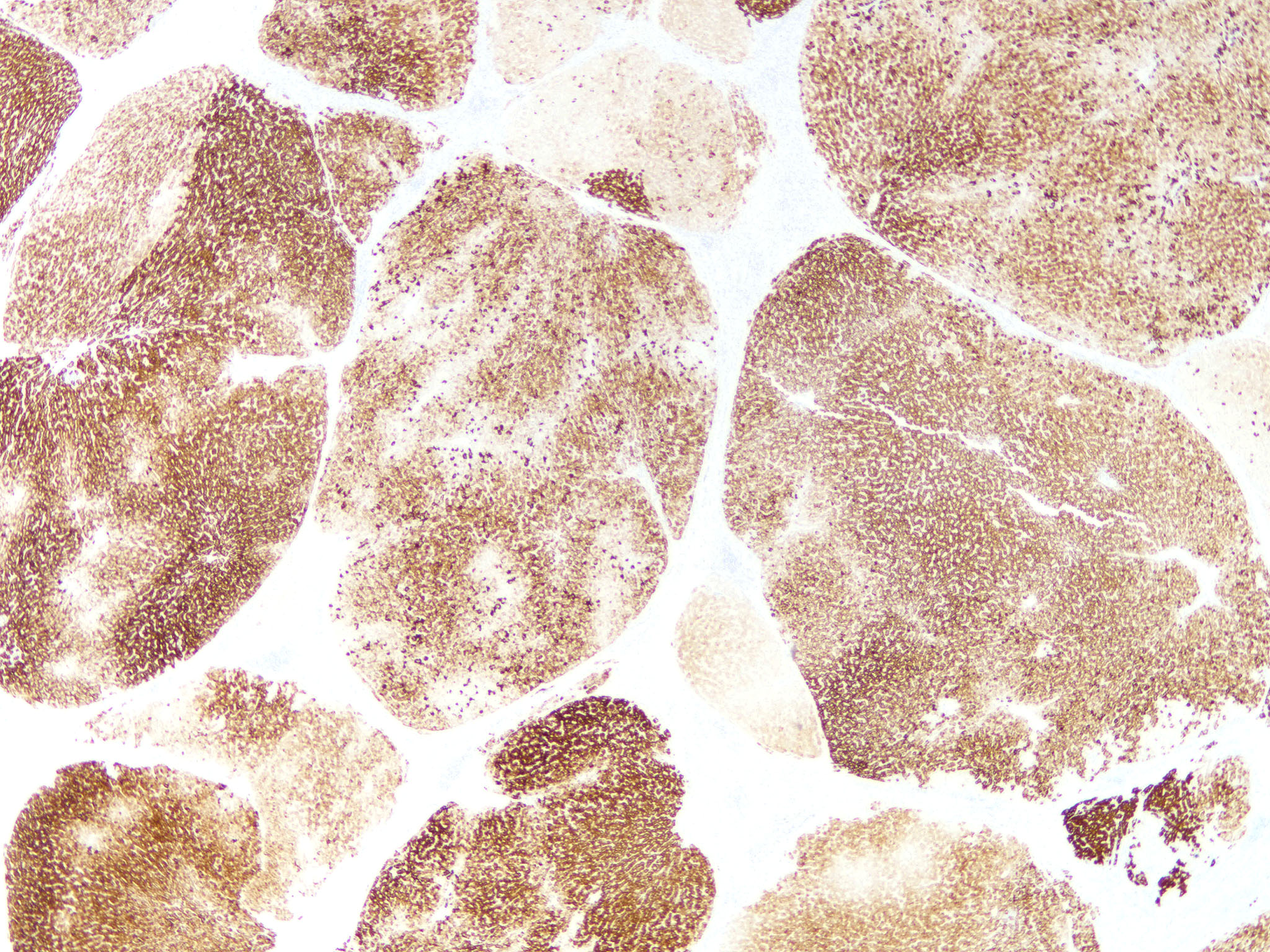
- Trichrome: highlights fibrous septa
- Sirius red: highlights fibrous septa
- Reticulin: highlights fibrous septa
Sample pathology report
- Liver, biopsy:
- Steatohepatitis with cirrhosis (see comment)
- Comment: In clinical history of diabetes mellitus and hypertension without significant alcoholic consumption, the overall features are consistent with metabolic associated fatty liver disease with cirrhosis.
Differential diagnosis
- Congenital hepatic fibrosis:
- Absence of regenerative nodules
- Dilated irregular ducts embedded in broad fibrous septa
- Focal nodular hyperplasia:
- Localized lesion with absence of diffuse nodulation
- Nodular regenerative hyperplasia:
- Absence of fibrous septa
- Alternating hepatocyte atrophy and hypertrophy highlighted on reticulin stain
Practice question #1
Practice answer #1
C. Feathery degeneration
Ballooning degeneration is a hallmark pathological change of steatohepatitis, which is not associated with biliary type cirrhosis (answer A). Bilirubinostasis may be present in late biliary type cirrhosis but is not associated with periseptal halo (answer B). Feathery degeneration is one of the features of chronic cholestasis contributing to the periseptal halo in biliary type cirrhosis (answer C). Florid duct lesion is one of the characteristic features of primary biliary cholangitis, which is not associated with periseptal halo (answer D). Periductal fibrosis is one of the characteristic features of primary sclerosing cholangitis, which is not associated with periseptal halo (answer E).
Comment Here
Reference: Cirrhosis
Ballooning degeneration is a hallmark pathological change of steatohepatitis, which is not associated with biliary type cirrhosis (answer A). Bilirubinostasis may be present in late biliary type cirrhosis but is not associated with periseptal halo (answer B). Feathery degeneration is one of the features of chronic cholestasis contributing to the periseptal halo in biliary type cirrhosis (answer C). Florid duct lesion is one of the characteristic features of primary biliary cholangitis, which is not associated with periseptal halo (answer D). Periductal fibrosis is one of the characteristic features of primary sclerosing cholangitis, which is not associated with periseptal halo (answer E).
Comment Here
Reference: Cirrhosis
Practice question #2
A 60 year old man was admitted with massive hematemesis and hypovolemic shock. He failed to respond to resuscitation. Postmortem examination revealed a liver shown as above. What is the most likely cause of his massive gastrointestinal bleeding?
- Acute gastritis
- Aortoesophageal fistula
- Esophageal varices
- Hepatocellular carcinoma
- Peptic ulcer
Practice answer #2