Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Ikura Y. Metabolic dysfunction associated steatotic liver disease (MASLD) / Metabolic dysfunction associated steatohepatitis (MASH). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livernash.html. Accessed September 14th, 2025.
Definition / general
- Metabolic dysfunction associated steatotic liver disease (MASLD) is hepatic steatosis generated in association with overweight / obesity, type 2 diabetes mellitus or other metabolic dysregulations (see Diagrams / tables) (Hepatology 2023;78:1966)
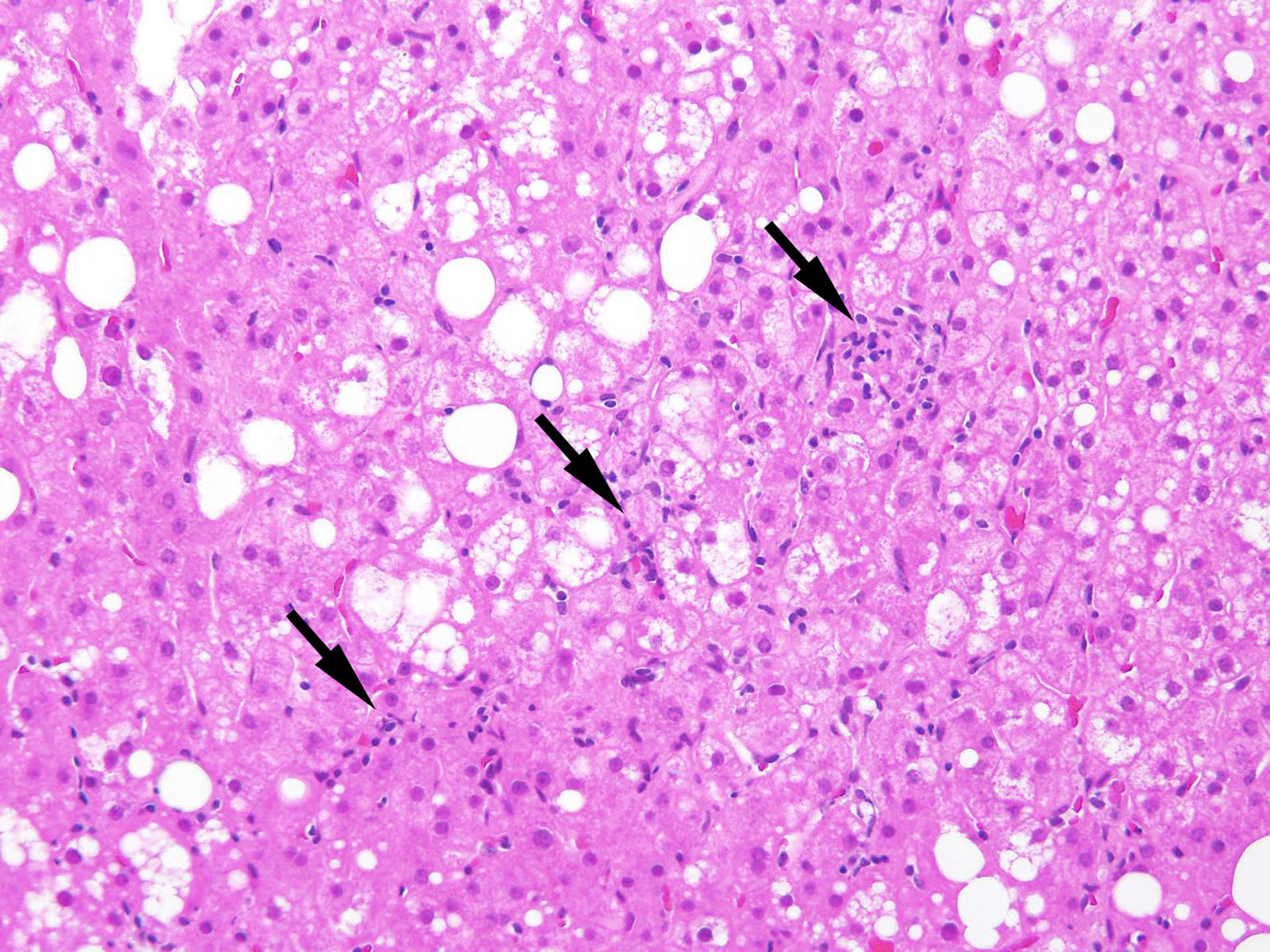
- Metabolic dysfunction associated steatohepatitis (MASH) is an aggressive form of MASLD characterized by marked inflammatory damage and hepatocyte ballooning
Essential features
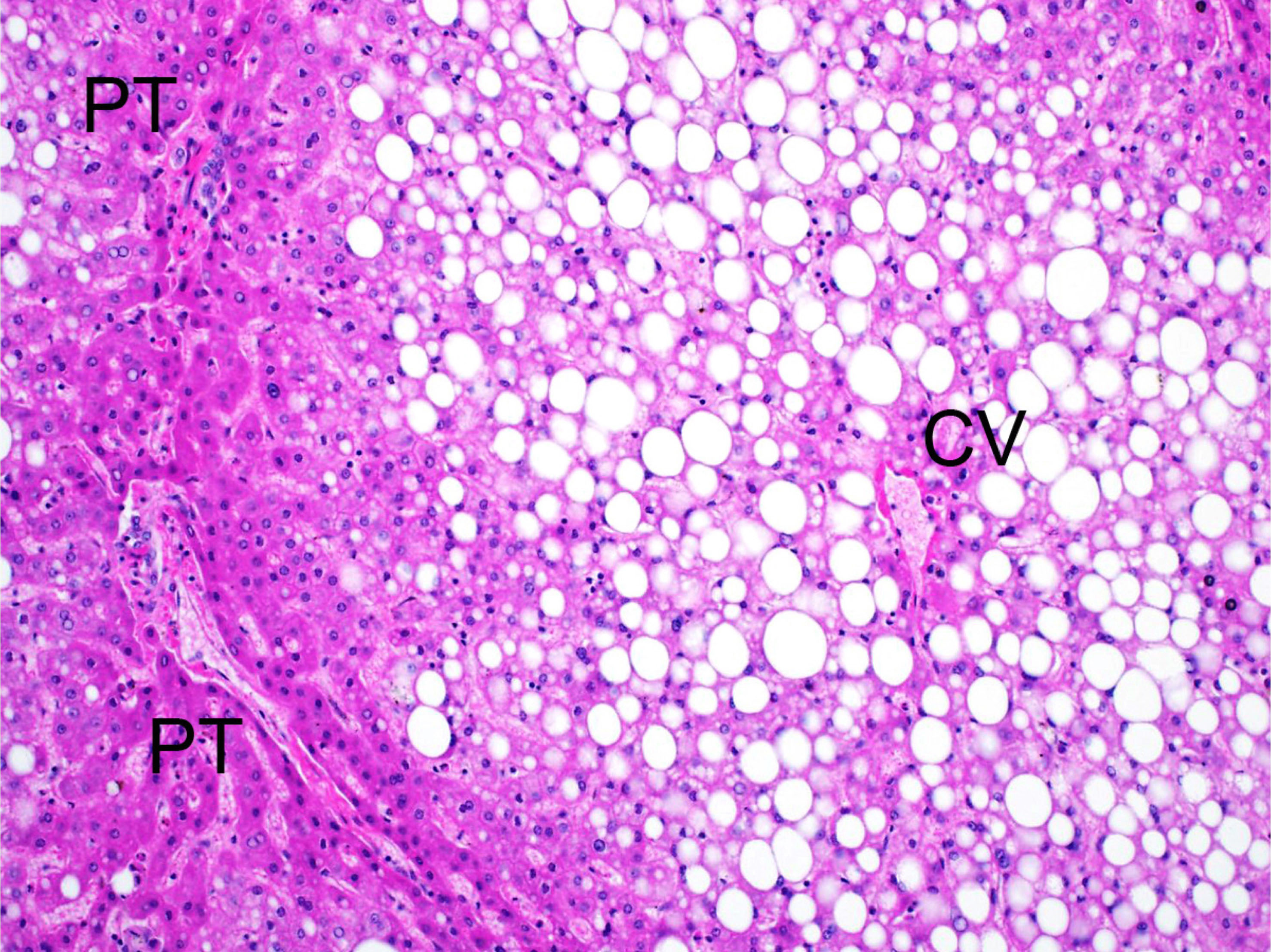
- Macrovesicular hepatosteatosis accentuated on zone 3, potentially accompanying fibroinflammatory changes in metabolic patients
- Morphologically, MASLD covers all forms of hepatic steatosis with or without inflammation / fibrosis
- Histologic grade is assessed using a scoring system including steatosis, lobular inflammation and ballooning degeneration (Hepatology 2005;41:1313)
- MASH is not the sole progressive form of MASLD (J Hepatol 2015;62:1148)
- Patients are at risk for fibrosis, cirrhosis and hepatocellular carcinoma
- Other liver diseases, such as autoimmune liver diseases, may be a complication (see Diagrams / tables) (Hepatology 2023;78:1966, World J Gastroenterol 2024;30:1949)
Terminology
- As described above, metabolic dysfunction associated steatotic liver disease (MASLD) refers to any fatty liver disease caused by metabolic dysregulation and metabolic dysfunction associated steatohepatitis (MASH) refers to an aggressive form of the disease characterized by inflammation and ballooning in addition to steatosis (see Diagrams / tables)
- Steatotic liver disease in moderate habitual drinkers with metabolic dysfunction is now classified as MASLD, while cases involving increased alcohol intake are referred to as metabolic dysfunction and alcohol related liver disease (MetALD) (see Diagrams / tables)
- Nonalcoholic fatty liver disease (NAFLD) and metabolic dysfunction associated fatty liver disease (MAFLD) have been used as former nomenclatures of MASLD (J Hepatol 2020;73:202)
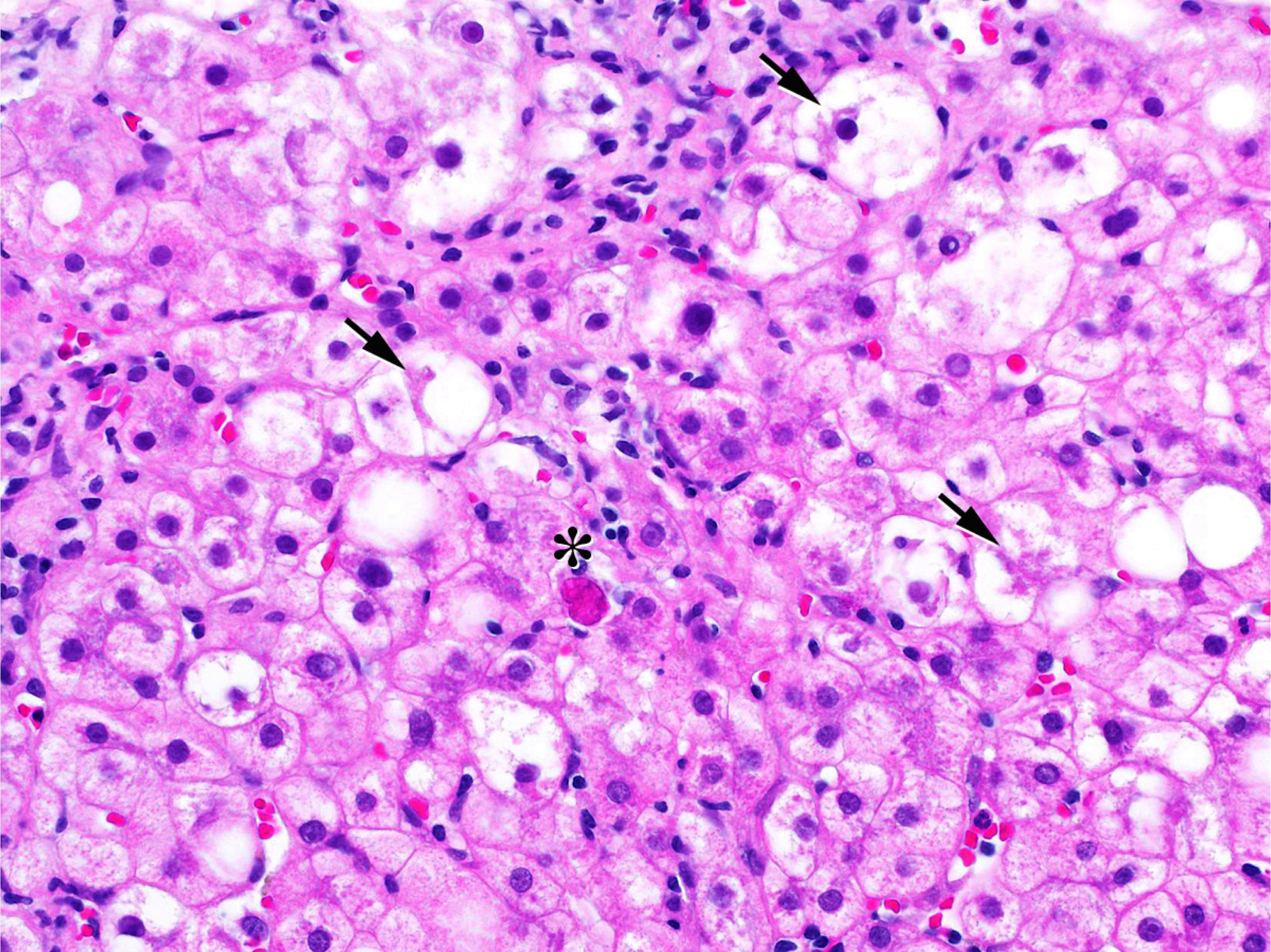
- Cytoplasmic inclusions known as Mallory-Denk bodies (see Microscopic images) are also termed Mallory hyaline and intracytoplasmic hyaline
ICD coding
- ICD-10: K76.0 - fatty (change of) liver, not elsewhere classified
Epidemiology
- One of the most important causes of liver disease worldwide in adults and children (Nat Rev Gastroenterol Hepatol 2018;15:11)
- Global prevalence is ~24% (Nat Rev Gastroenterol Hepatol 2018;15:11)
- It largely affects patients with unhealthy metabolic conditions but can occur even in lean individuals (Medicine (Baltimore) 2012;91:319)
Pathophysiology
- Hepatic manifestation of metabolic disorders
- Oxidative stress and lipotoxicity are considered key factors in disease progression (Hepatology 2006;43:506, J Atheroscler Thromb 2009;16:893)
- Genetic variants in patatin-like phospholipase domain containing protein 3 (PNPLA3), transmembrane 6 superfamily 2 (TM6SF2), membrane bound O-acyltransferase domain containing 7 (MBOA7) and hydroxysteroid 17-beta dehydrogenase 13 (HSD17B13) are known modifiers of MASLD (Clin Med (Lond) 2018;18:s54, J Hepatol 2018;68:268)
Etiology
- Overweight / obesity, hyperglycemia / type 2 diabetes mellitus and other metabolic disorders (dyslipidemia, insulin resistance, hypertension, etc.) (Hepatology 2023;78:1966, J Hepatol 2020;73:202)
Diagrams / tables
Clinical features
- Most patients with MASLD are asymptomatic and diagnosed incidentally (Clin Liver Dis 2016;20:277)
- Prevalence of MASLD is high in people of Asian and Hispanic origin (Clin Liver Dis 2018;22:39)
- Fatty livers induced by alternative causes (medications, starvation, inherited disorders of lipid metabolism, etc.) are not MASLD (Hepatology 2023;78:1966)
Diagnosis
- Clinically or histologically detected hepatic steatosis in patients with metabolic disorders (see Diagrams / tables)
- Disease severity is evaluated semiquantitatively with the NASH Clinical Research Network criteria (Hepatology 2005;41:1313)
- The need to distinguish between simple steatosis and steatohepatitis is still controversial (J Hepatol 2020;73:202)
- Distinction from alcohol related liver disease (ALD) is made into 3 categories (MASLD / MetALD / ALD), depending on the amount of alcohol the patient drinks (see Diagrams / tables) (Hepatology 2023;78:1966)
- Fatty livers induced by alternative causes (medications, starvation, inherited disorders of lipid metabolism, etc.) are not considered MASLD (Hepatology 2023;78:1966)
- Other liver diseases, such as autoimmune liver diseases, may be a complication (see Diagrams / tables) (Hepatology 2023;78:1966, World J Gastroenterol 2024;30:1949)
Radiology description
- Bright liver and increased hepatorenal contrast on ultrasound (US) (Tohoku J Exp Med 1983;139:43)
- Liver / spleen attenuation ratio < 1.1 on computed tomography (CT) (Hepatol Commun 2019;3:1347)
- High signal intensity on T1 weighted magnetic resonance images (MRI)
- Whole hepatic lipid volume is quantifiable by using a special MRI technique (Hepatol Res 2019;49:1374)
Radiology images
Prognostic factors
- Presence of fibrosis is a sole prognostic factor in MASLD (Gastroenterology 2015;149:389, Hepatology 2015;61:1547)
Case reports
- 7 and 10 year old siblings with MASLD and 2,4-dienoyl-CoA reductase 1 deficiency (Int J Obes (Lond) 2024;48:1818)
- 16 year old transgender girl with signs of hepatocellular injury and fibrosis due to MASH (JPGN Rep 2024;5:223)
- 62 year old obese, diabetic woman with both MASLD and ALD (Dig Med Res 2024;7:16)
- 68 year old man with oral lichen planus and MASLD (Cureus 2024;16:e65054)
Treatment
- Mainstay of therapy for MASLD is to treat the underlying metabolic abnormalities
- While numerous clinical trials have been conducted, practical applications have been slow to emerge; however, in 2024, resmetirom received accelerated approval from the FDA for clinical use in MASLD (Drugs 2024;84:729)
Gross description
- Swollen soft liver with yellowish-brown color
- Surface of the affected liver becomes irregular with progression of fibrosis
- Some cases show cirrhosis or hepatocellular carcinoma
Frozen section description
- Lipid stain methods (oil red O, Sudan black B, filipin, etc.) to detect liver fat can be performed on frozen sections
Microscopic (histologic) description
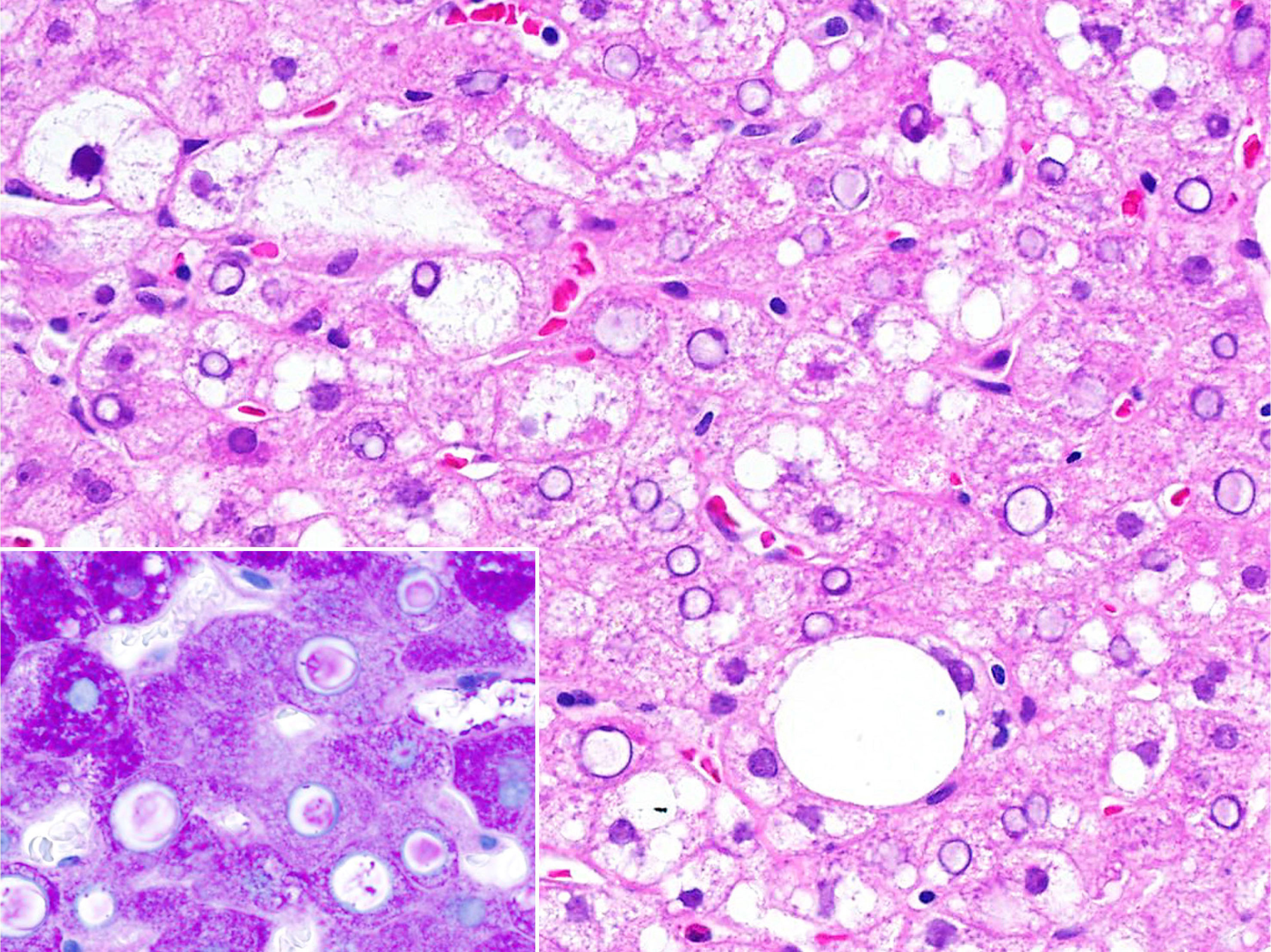
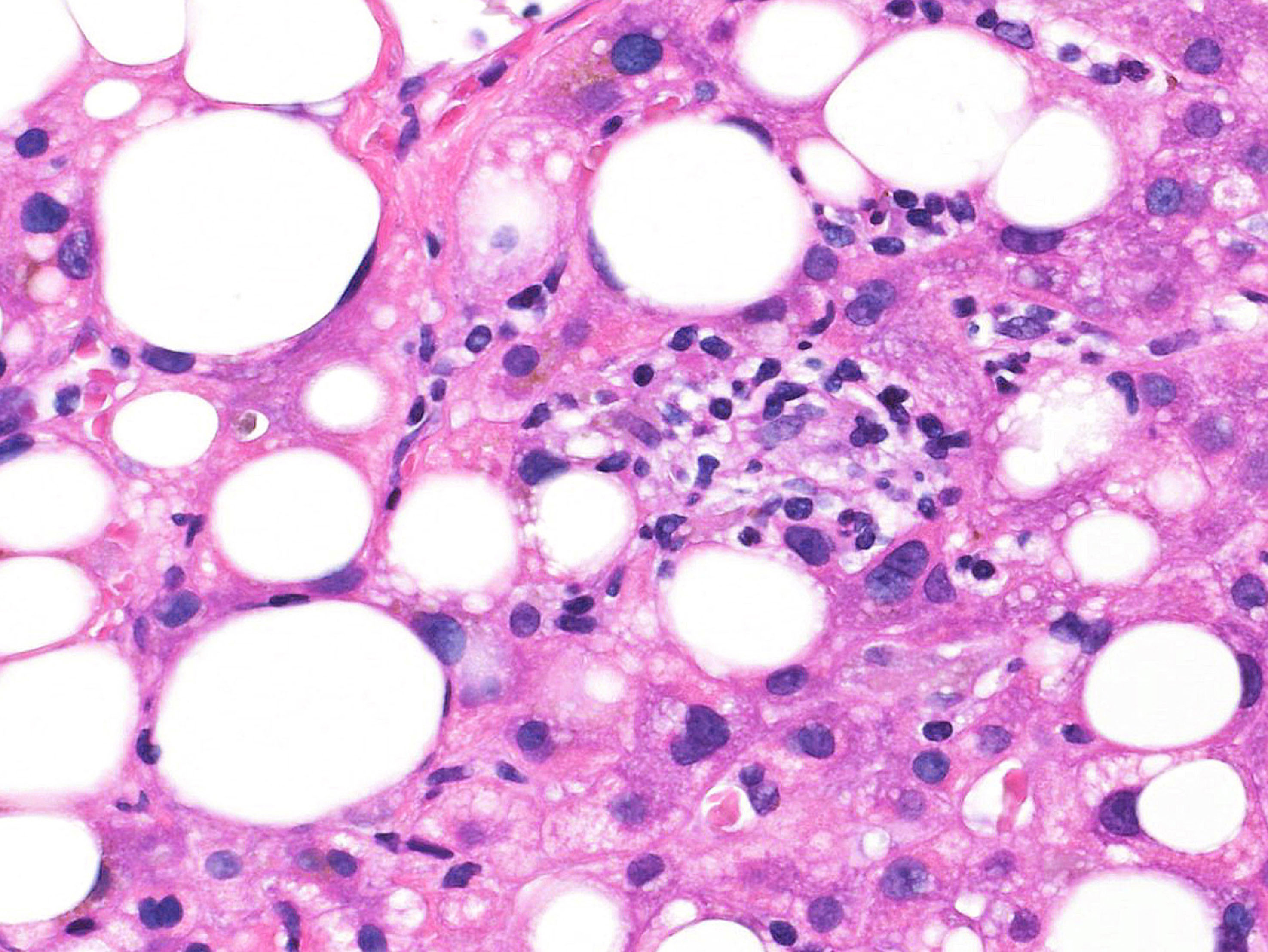
- Predominantly macrovesicular steatosis in ≥ 5% hepatocytes under low magnification (4x or lower) is a sole histologic requirement for diagnosis of MASLD
- Disease severity is evaluated separately by grade of activity and stage of fibrosis
- Activity grade is assessed according to nonalcoholic fatty liver disease activity score (NAS) using the sum of 3 components (total 0 - 8 points) (Hepatology 2005;41:1313)
- Steatosis
- 0: < 5%
- 1: 5 - 33%
- 2: 34 - 66%
- 3: > 66%
- Lobular inflammation
- 0: none
- 1: < 2 foci/20x field
- 2: 2 - 4 foci/20x field
- 3: > 4 foci/20x field
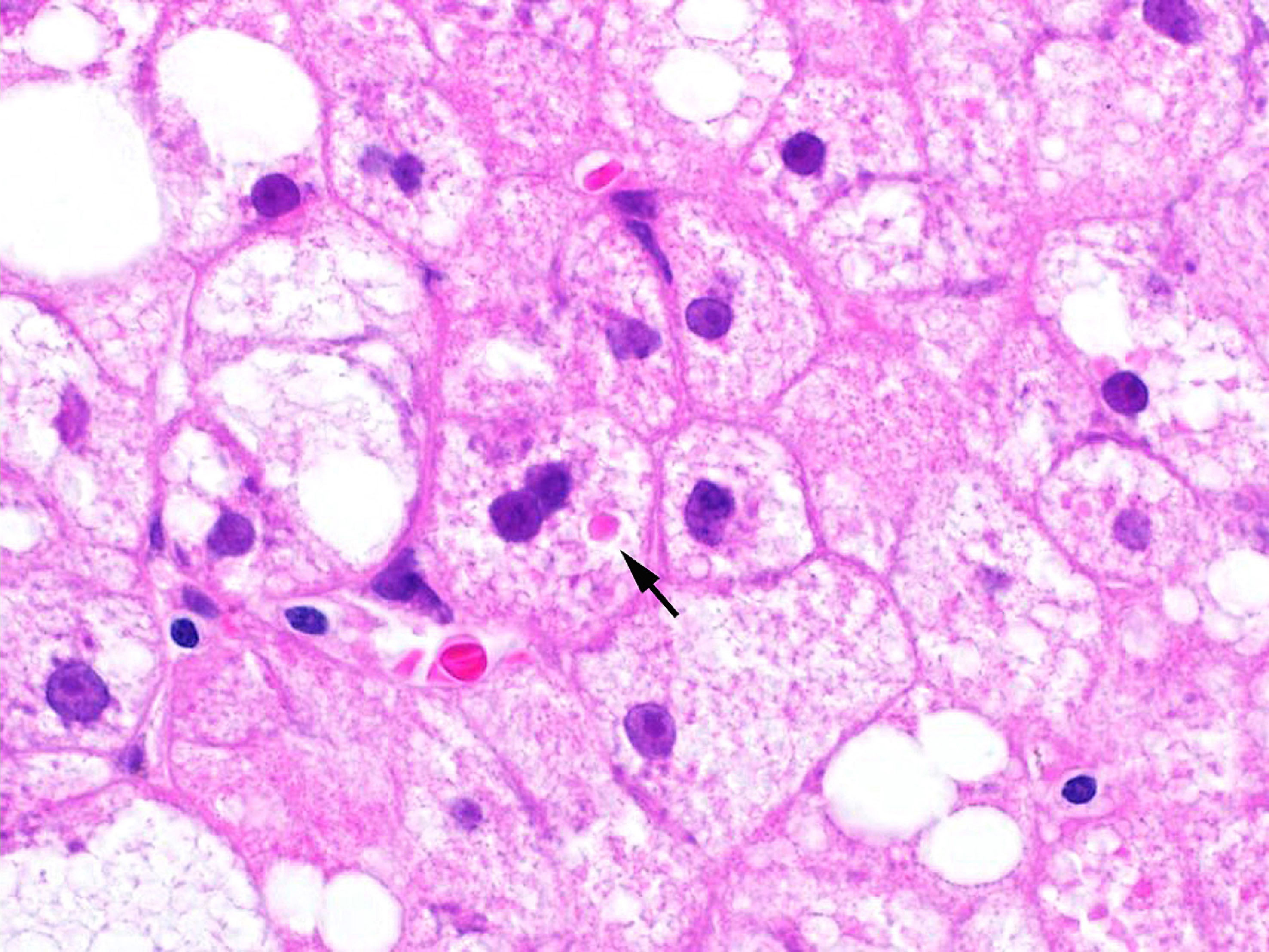
- Ballooning degeneration
- 0: none
- 1: few
- 2: many
- Steatosis
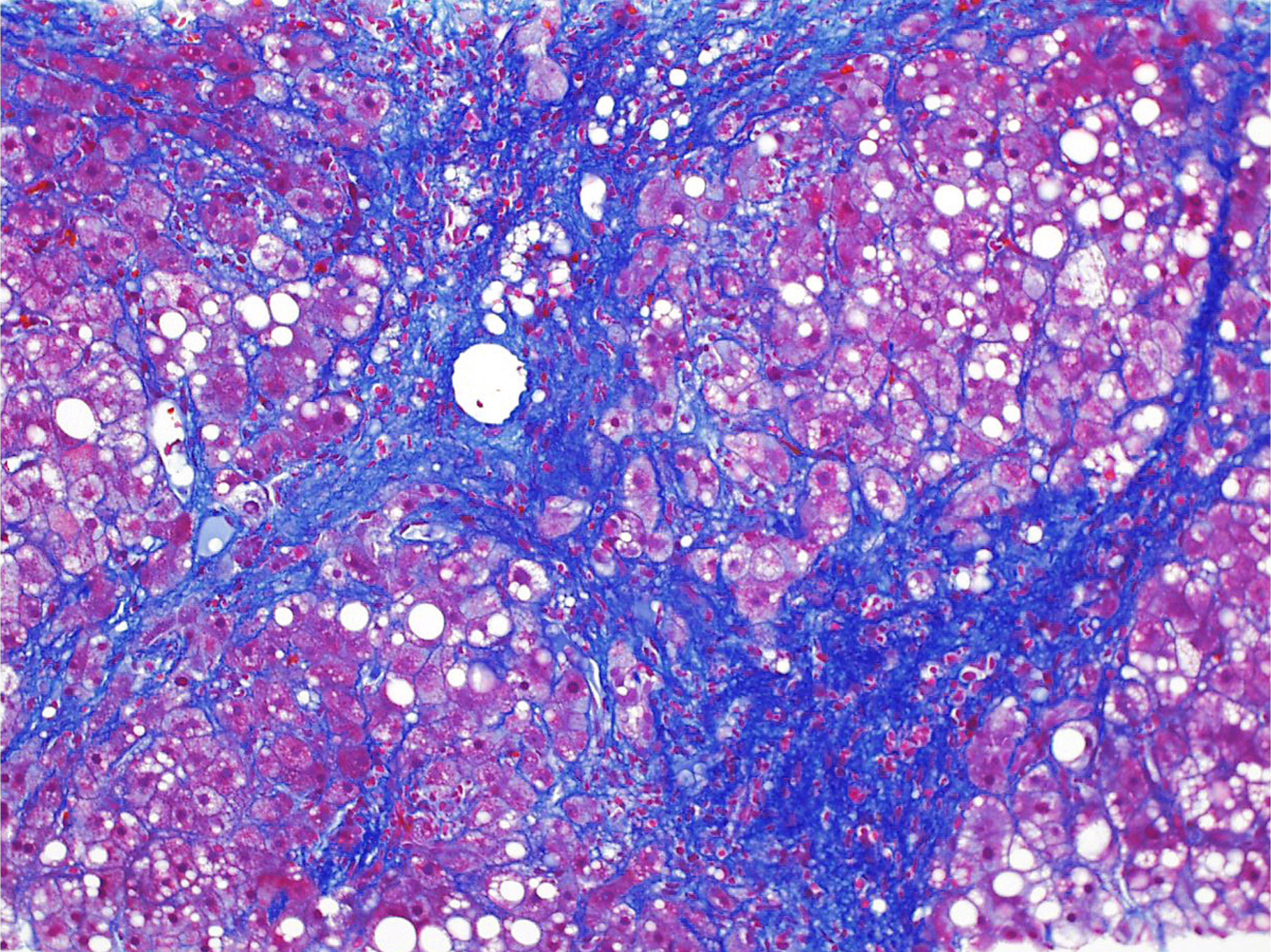
- Fibrosis stage is assessed into 5 levels (Hepatology 2005;41:1313)
- Stage 0: none
- Stage 1: perivenular (zone 3) fibrosis
- Stage 2: perivenular + portal fibrosis
- Stage 3: bridging fibrosis
- Stage 4: cirrhosis
- Other characteristic findings are Mallory-Denk bodies, glycogenated nuclei, giant mitochondria (megamitochondria) and lipogranuloma
- Histologic changes of concomitant liver conditions may be seen (Hepatology 2023;78:1966, World J Gastroenterol 2024;30:1949)
- In MASLD associated cirrhosis, steatotic hepatocytes may become depleted, resulting in a loss of visible steatosis; however, the term cryptogenic cirrhosis should not be used for this condition (J Hepatol 2020;73:202)
Positive stains
- Special stains for collagen (Masson trichrome, Sirius red, Azan-Mallory, etc.) mandatory; faint fibrosis cannot be detected on H&E tissue slides
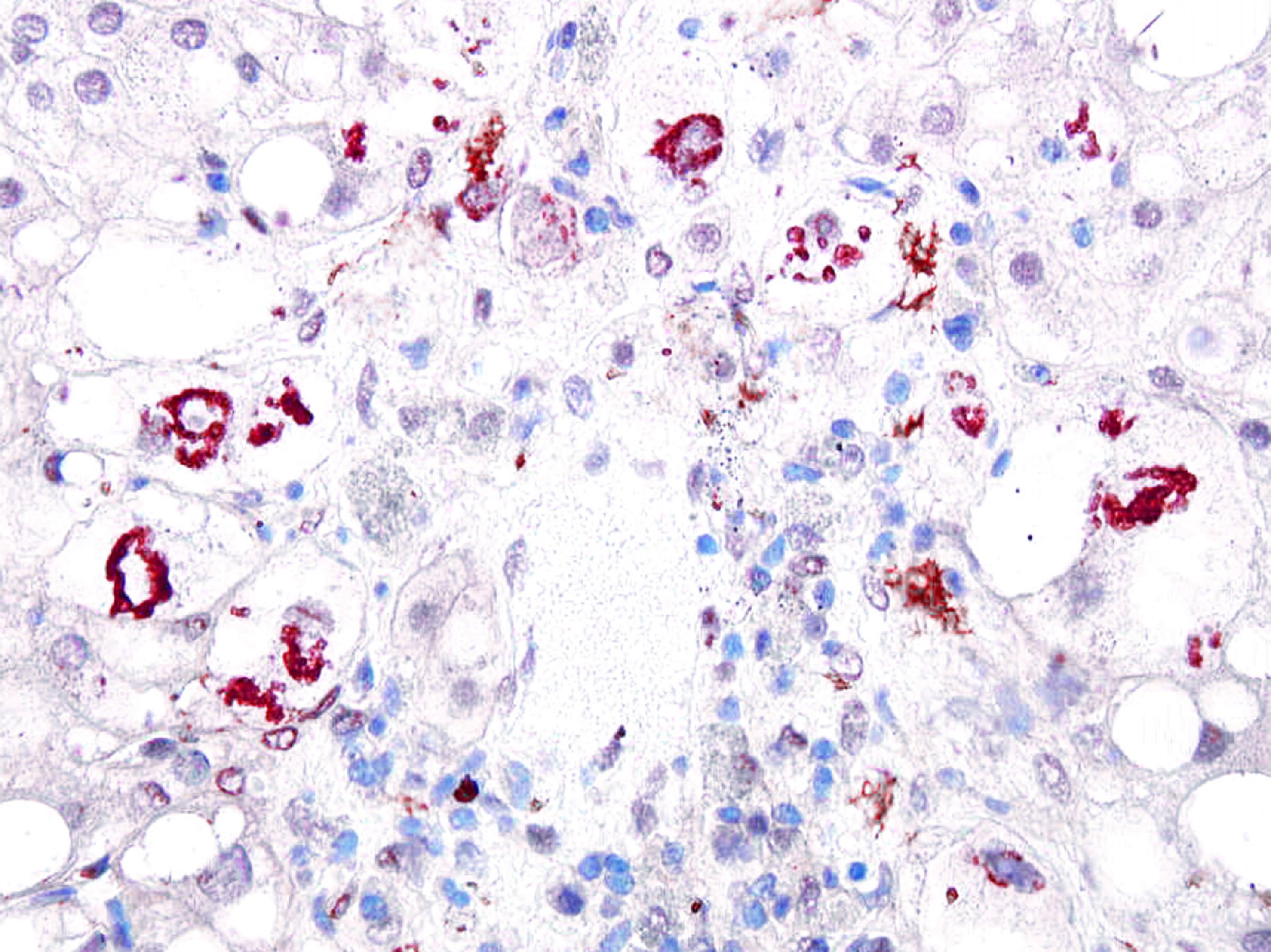
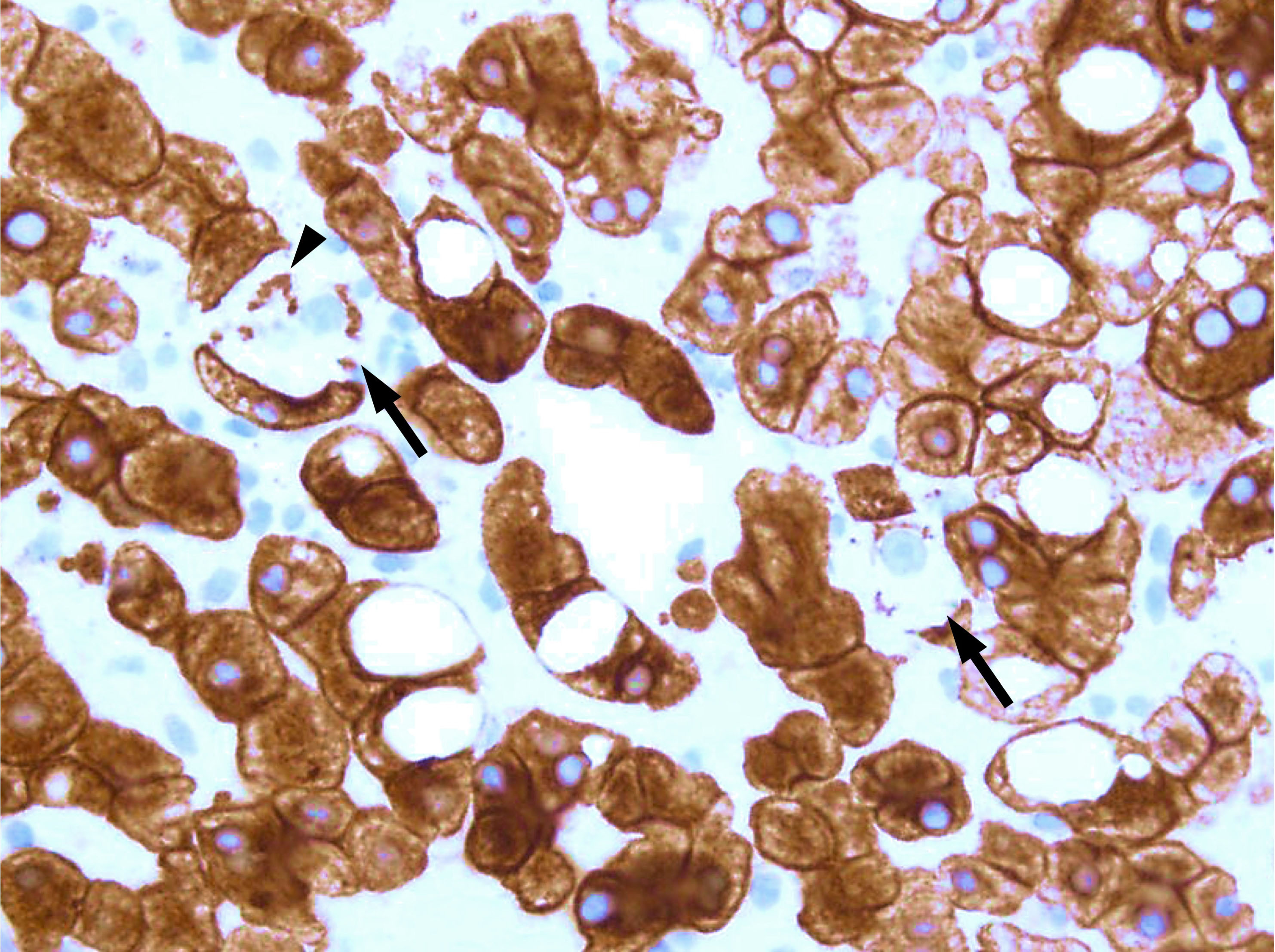
- Ubiquitin, p62, CK18: Mallory-Denk bodies are stained
- References: Histochem Cell Biol 2008;129:735, Exp Mol Pathol 2011;90:252
Negative stains
- CK18: ballooned hepatocytes are characteristically negative (J Hepatol 2010;53:719)
Sample pathology report
- Liver, needle biopsy:
- Moderate steatosis, consistent with metabolic dysfunction associated steatotic liver disease
- NAS 6 points = steatosis 2 + inflammation 2 + ballooning 2
- Stage 2 (perivenular + portal fibrosis), Kleiner-Brunt methodology
Differential diagnosis
- Alcohol related liver disease (ALD):
- Can be diagnosed according amount of alcohol intake (Hepatology 2023;78:1966)
- Can coexist with MASLD (Dig Med Res 2024;7:16, J Hepatol 2020;73:202)
- Genetic disorders (Wilson disease, lysosomal acid lipase deficiency, etc.):
- Should be suggested by the specific clinical background
- Drug induced SLD:
- Cortisol is a representative cause of drug induced SLD (Intern Med 2024;63:3165)
- Methotrexate may exacerbate MASLD (>Nat Rev Rheumatol 2023;19:96)
- Viral hepatitis:
- Hepatitis C is still an important condition that needs to be differentiated from MASLD (Clin Pract 2024;14:2542, Clin Gastroenterol Hepatol 2024;22:2137)
- Differential diagnosis of SLDs should be made in collaboration with clinicians
Practice question #1
A 71 year old woman (nondrinker) presented with possible diagnosis of hepatocellular carcinoma and SLD with abdominal ultrasound. Percutaneous liver biopsy was performed for definitive diagnosis. The photomicrograph above shows nontumorous liver tissue (background). What information has the lowest priority for accurate pathologic diagnosis?
- Autoantibodies
- Genetic test results
- Medications
- Metabolic factors
- Virus markers
Practice answer #1
B. Genetic test results. Liver histology shows inflammatory damage associated with lymphoid follicle formation and steatosis. These morphological features are common findings in both autoimmune hepatitis and chronic hepatitis C. Indeed, this case was positive for hepatitis C virus genotype 3. ALD, MASLD and drug induced SLD should always be investigated as possible comorbid pathological mechanisms (Clin Pract 2024;14:2542). Some genetic disorders cause SLD but the incidence is very low. Answer A is incorrect because autoimmune diseases should be ruled out. Answer C is incorrect because steatosis is relatively common in drug induced liver injury. Answer E is incorrect because chronic hepatitis C is most likely in cases with such histology. Answer D is incorrect because MASLD is the most common type of SLD.
Comment Here
Reference: Metabolic dysfunction associated steatotic liver disease (MASLD) / Metabolic dysfunction associated steatohepatitis (MASH)
Comment Here
Reference: Metabolic dysfunction associated steatotic liver disease (MASLD) / Metabolic dysfunction associated steatohepatitis (MASH)
Practice question #2
Practice answer #2
E. Ubiquitin positive. The inclusion shown is a Mallory-Denk body. It is a ubiquitinated aggregate of keratin filament that occurs in ballooned hepatocytes. Answer A is incorrect because the intracellular inclusion is negative for actin. Answer B is incorrect because the intracellular inclusion is positive for CK18. Answer C is incorrect because the intracellular inclusion is not related to viral infection. Answer D is incorrect because the intracellular inclusion is not restricted to alcohol related liver injury.
Comment Here
Reference: Metabolic dysfunction associated steatotic liver disease (MASLD) / Metabolic dysfunction associated steatohepatitis (MASH)
Comment Here
Reference: Metabolic dysfunction associated steatotic liver disease (MASLD) / Metabolic dysfunction associated steatohepatitis (MASH)