Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Electron microscopy images | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Yoshikawa A, Bychkov A, Sathirareuangchai S. Emphysema. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungnontumoremphysema.html. Accessed September 24th, 2025.
Definition / general
- Abnormal enlargement of air spaces distal to the terminal bronchioles characterized by destruction of the alveolar septa with little or no fibrosis
Essential features
- Destruction of acinar structure and airspace enlargement
- Affects multiple pulmonary functions and causes chronic respiratory symptoms
Terminology
- By the Global Initiative for Chronic Obstructive Lung Disease (GOLD), an international organization launched by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. and the World Health Organization (WHO)
- Chronic obstructive pulmonary disease (COPD) (Global Initiative for Chronic Obstructive Lung Disease: 2021 GOLD Reports [Accessed 20 December 2021])
- Common progressive disease that is characterized by persistent respiratory symptoms and usually associated with the prolonged exposure to noxious particles or gases, especially smoking
- Airflow limitation is caused by a combination of airways disease (chronic bronchitis) and lung parenchymal destruction (emphysema)
- Major types of emphysema (Lancet 2004;364:709, Int J Chron Obstruct Pulmon Dis 2008;3:193):
- Centriacinar, centrilobular or proximal acinar emphysema (mostly associated with smoking and COPD)
- Panacinar or panlobular emphysema
- Paraseptal or distal acinar emphysema
- Minor types of emphysema:
- Combined pulmonary fibrosis and emphysema (CPFE)
- Interstitial emphysema
- Bullous emphysema
- Senile emphysema
- Irregular emphysema
- Congenital lobar emphysema
ICD coding
- ICD-10:
- ICD-11:
Epidemiology
- Globally, COPD is the third leading cause of death (Lancet 2012;380:2095)
- Affects 1.4% of adults in the U.S. (CDC: Chronic Obstructive Pulmonary Disease (COPD) Includes - Chronic Bronchitis and Emphysema [Accessed 20 December 2021], American Lung Association: Trends in COPD (Chronic Bronchitis and Emphysema) - Morbidity and Mortality [Accessed 13 January 2022])
- M:F = 1:0.9
- Usually older than 45 years old
Sites
- Centriacinar emphysema
- Upper lobe predominant
- Respiratory bronchioles and surrounding lung parenchyma
- Panacinar emphysema
- Lower lobe predominant
- Entire acinus
- Paraseptal emphysema
- Upper lung
- Distal part of acinus in subpleural area
Pathophysiology
- Destruction of lung parenchymal tissue due to chronic inflammation
- Protease mediated destruction of elastin is an important feature (Thorax 2016;71:105)
- Morphological progression (Int J Chron Obstruct Pulmon Dis 2016;11:2287, Clin Anat 2015;28:227)
- Increase in size and number of small fenestrae in alveolar walls (pores of Kohn), which leads to loss of elastic recoil
- Breakdown and merging of fibrovascular trabeculae (framework)
- Remodeling of acini results in airspace enlargement
Etiology
- Inhalation
- Cigarette smoking and environmental pollutants, especially for centriacinar emphysema
- However, there is individual susceptibility (Annu Rev Physiol 2014;76:493)
- Infections
- Genetic factors
- Alpha-1 antitrypsin deficiency is well known risk factor, especially for panacinar emphysema (Eur Respir J 2017;49:1600154, Lancet 2004;364:709)
- Telomerase mutations, especially for CPFE (J Clin Invest 2015;125:563)
- Polymorphism of serpin family genes (BMC Med Genet 2010;11:159)
Diagrams / tables
Clinical features
- Dyspnea; chronic, progressive and usually irreversible
- Chest inflation
- Combined pulmonary fibrosis and emphysema (CPFE) (Chest 2012;141:222, Eur Respir J 2005;26:586)
- Coexistence of interstitial fibrosis and emphysema of unknown causes
- Patients with CPFE have different pulmonary function tests and outcomes compared to patients with pure emphysema or pure fibrosis
- Interstitial emphysema (Am J Surg Pathol 2014;38:339)
- Air gains access to the pulmonary interstitium to cause air leak and pneumothorax
- Common in premature infants
- Adults: commonly in usual interstitial pneumonia but can occur in any interstitial lung diseases
- Bullous emphysema
- Formation of multiple bullae > 1 cm with thin wall
- Can cause bullae inflation and pneumothorax
- Senile emphysema
- Due to age related alteration of acini
- Irregular emphysema
- Occurs in relation to scars
- Congenital lobar emphysema (Pediatr Clin North Am 1994;41:453)
- Hyperinflation of one or more lobes due to malformation of bronchioles
- Causes respiratory distress
- Can be sporadic or caused by autosomal dominant inheritance
Diagnosis
- Primarily diagnosed by imaging studies with compatible clinical manifestation
- Rarely diagnosed solely in biopsy specimens
- More commonly diagnosed in autopsy specimens or as a background finding in resection specimens
Laboratory
- Screening for alpha-1 antitrypsin deficiency (AATD) is recommended by some experts in all patients with COPD (Chronic Obstr Pulm Dis 2016;3:668)
- Alpha-1 antitrypsin (AAT) serum level and genotype
Radiology description
- Xray: overinflation of the lung but it may not be seen in early stages
- Chest CT: emphysematous regions are represented by low attenuation areas (Eur Respir J 2016;48:216)
Radiology images
Prognostic factors
- Based on exacerbation risk of COPD (Global Initiative for Chronic Obstructive Lung Disease: About GOLD [Accessed 27 December 2021])
- GOLD score 3 or 4 (severe or very severe airflow limitation)
- Previous history of exacerbation and hospitalization
- Faster loss of forced expiratory volume in 1 sec
- COPD assessment test score ≥ 10 (CAT: COPD Assessment Test [Accessed 27 December 2021], Eur Respir J 2009;34:648)
Case reports
- 31 year old woman with congenital lobar emphysema (Surg Today 2013;43:539)
- 32 year old woman with severe bullous emphysema (Asian Cardiovasc Thorac Ann 2016;24:597)
- 38 year old man with COVID-19, complicated by mediastinal emphysema and pneumothorax (Korean J Radiol 2020;21:541)
- 52 year old man with emphysema from diffuse parenchymal pulmonary amyloidosis (Thorax 2021;76:421)
- 61 year old man with metastatic carcinoma mimicking emphysema (Medicine (Baltimore) 2017;96:e8927)
- 63 year old man with CPFE and severe pulmonary hypertension (Autops Case Rep 2017;7:15)
- 65 year old woman with severe emphysema (Clin Respir J 2017;11:1091)
- 83 year old man died of CPFE (Int J Chron Obstruct Pulmon Dis 2015;10:1299)
Treatment
- Based on treatment of COPD (Global Initiative for Chronic Obstructive Lung Disease: About GOLD [Accessed 27 December 2021])
- Smoking cessation
- Medications: bronchodilators, antimuscarinic drugs, steroids, etc.
- Ventilatory support
- Surgical interventions: lung volume reduction surgery, bullectomy, lung transplant
- Augmentation therapy for alpha-1 antitrypsin deficiency (Eur Respir Rev 2015;24:46)
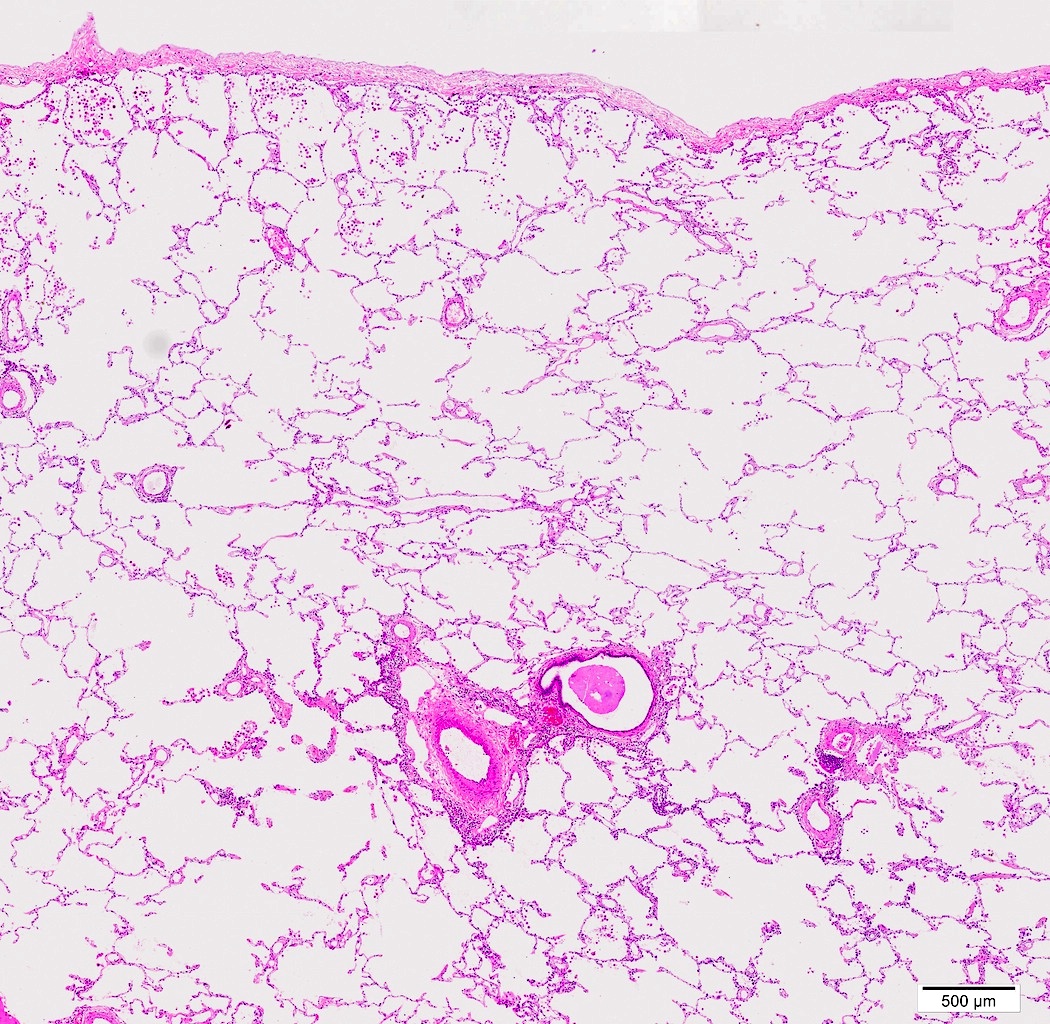
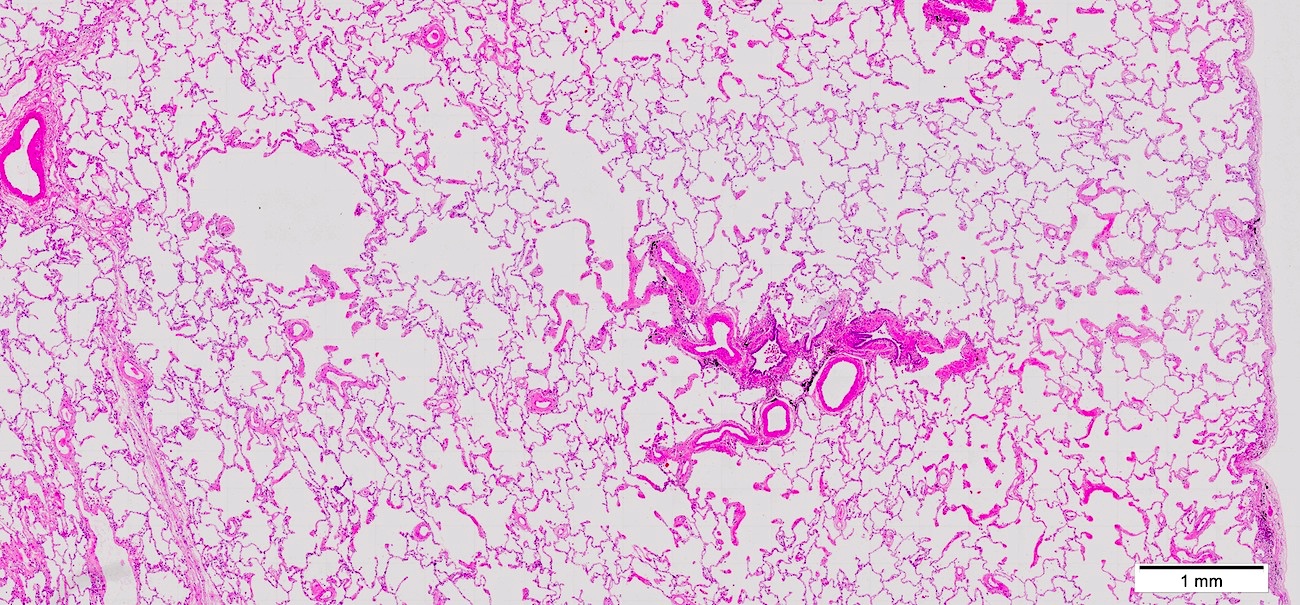
Gross description
- Hyperinflation or ballooning due to entrapment of the air from airway obstruction
- Lungs may be overlapping the heart
- Upper lobes are more involved
- Centriacinar: sparse empty spaces with pigmentation (anthracosis) corresponding enlarged airspaces
- Panacinar: airspaces are more or less evenly inflated throughout the secondary lobules
- Paraseptal: inflated subpleural airspaces with thin walls
- Bullous emphysema
- Descriptive term regarding emphysematous lung with visible bullae upon gross examination
- Bulla: an air filled space of 1 cm in diameter within the lung which has developed because of emphysematous destruction of the lung parenchyma (StatPearls: Bullous Emphysema [Accessed 5 January 2022])
Gross images
Images hosted on other servers:
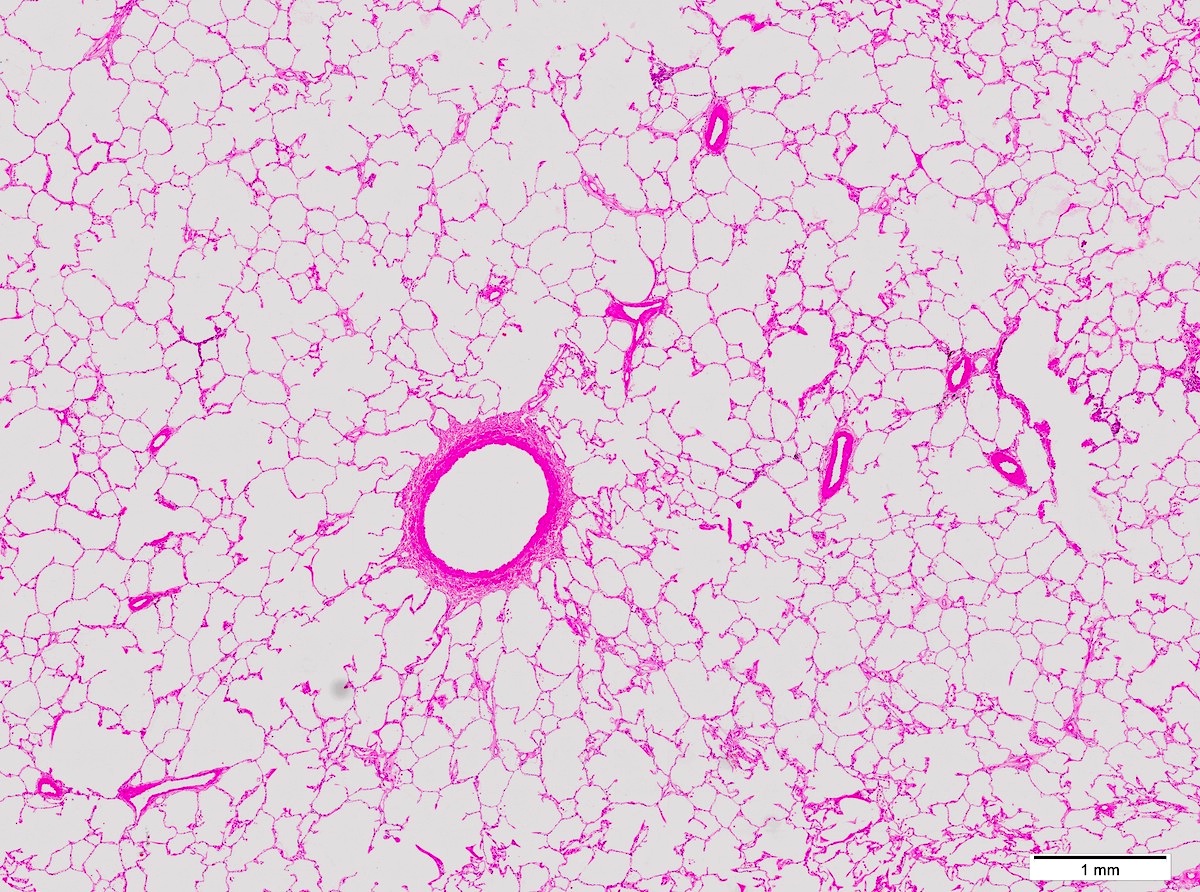
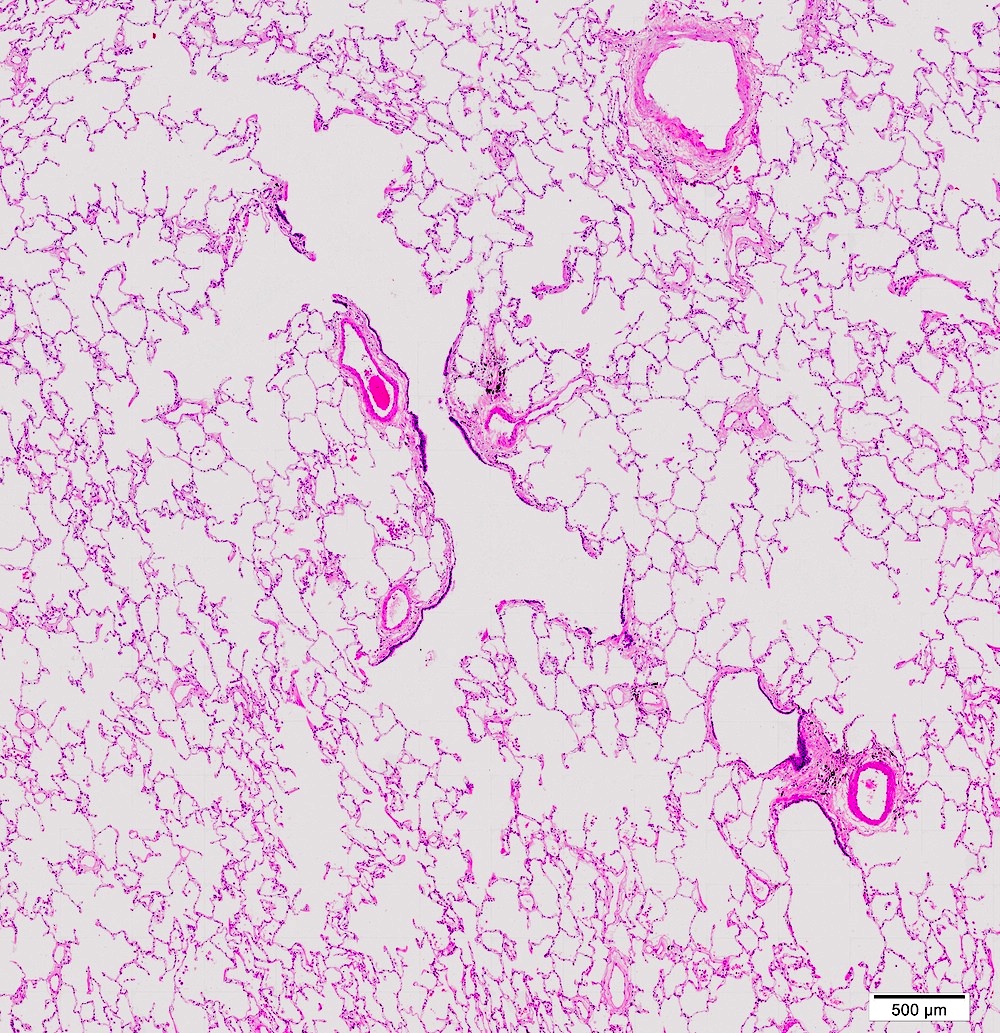
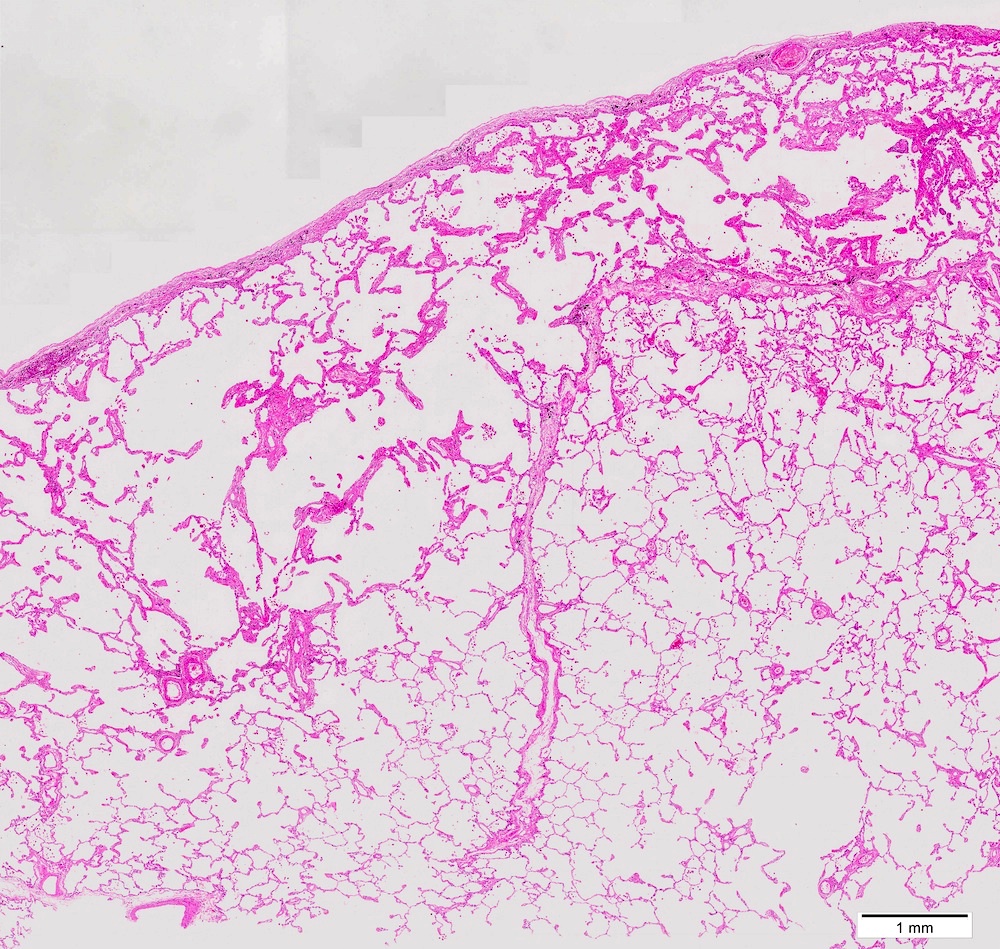
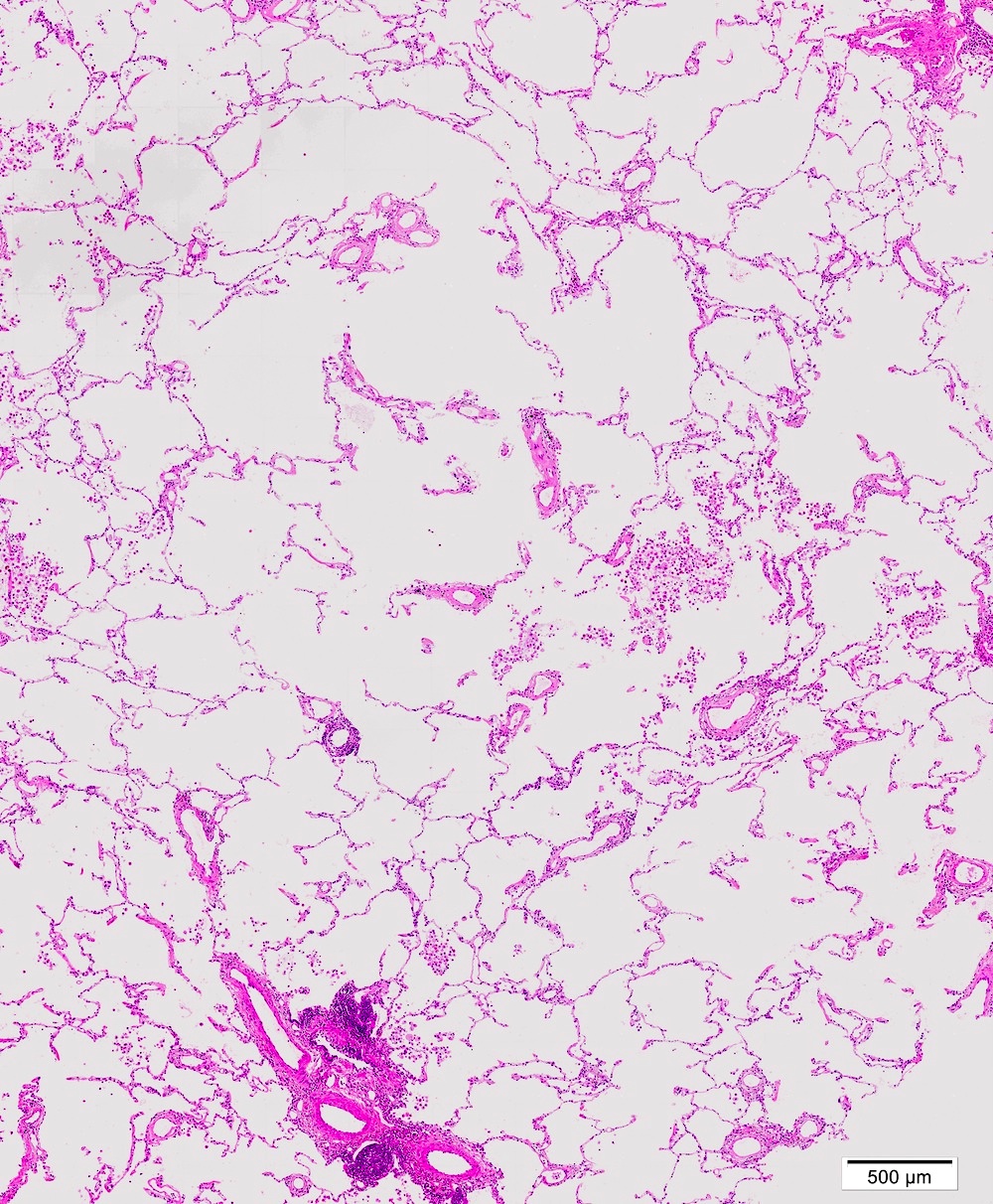
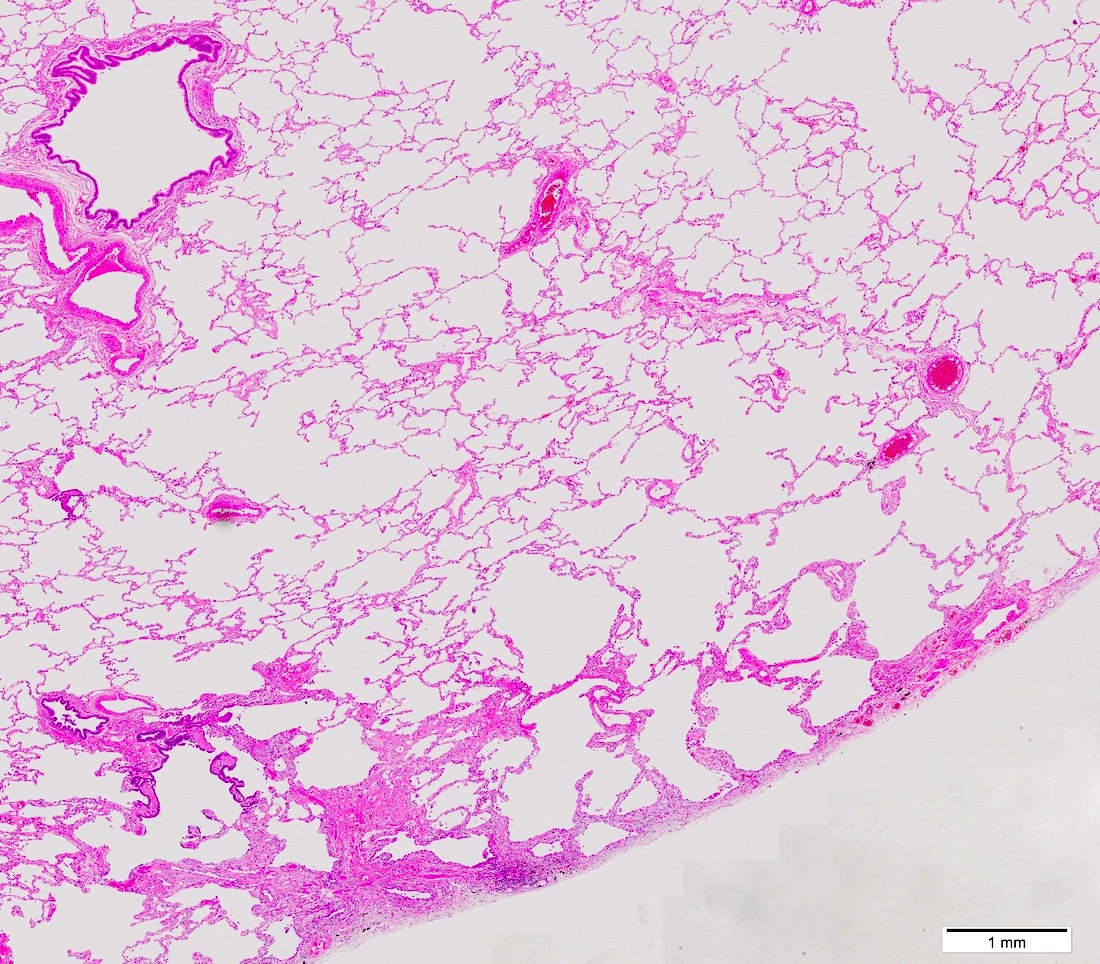
Microscopic (histologic) description
- General findings
- Airspace enlargement; the size of airspace in the background parenchyma serves as a reference; although exact microscopic criteria have not been established
- Fragmented alveolar walls
- If the acinar arrangement is maintained, it is representing pores of Kohn
- If not, it is representing acinar destruction
- Mild fibrotic change can be seen
- Any degrees of inflammation can accompany
- Subtype is determined with histological landmarks, although exact classification is better appreciated at gross exam:
- Bronchovascular bundle of terminal bronchiole and arteriole is in the center of acinus
- Connective tissue septa (secondary lobule of Miller) are the periphery of acinus, which is often ambiguous in less inflamed lung
- Note: similar appearance can be seen due to inadequate inflation or fixation of specimen
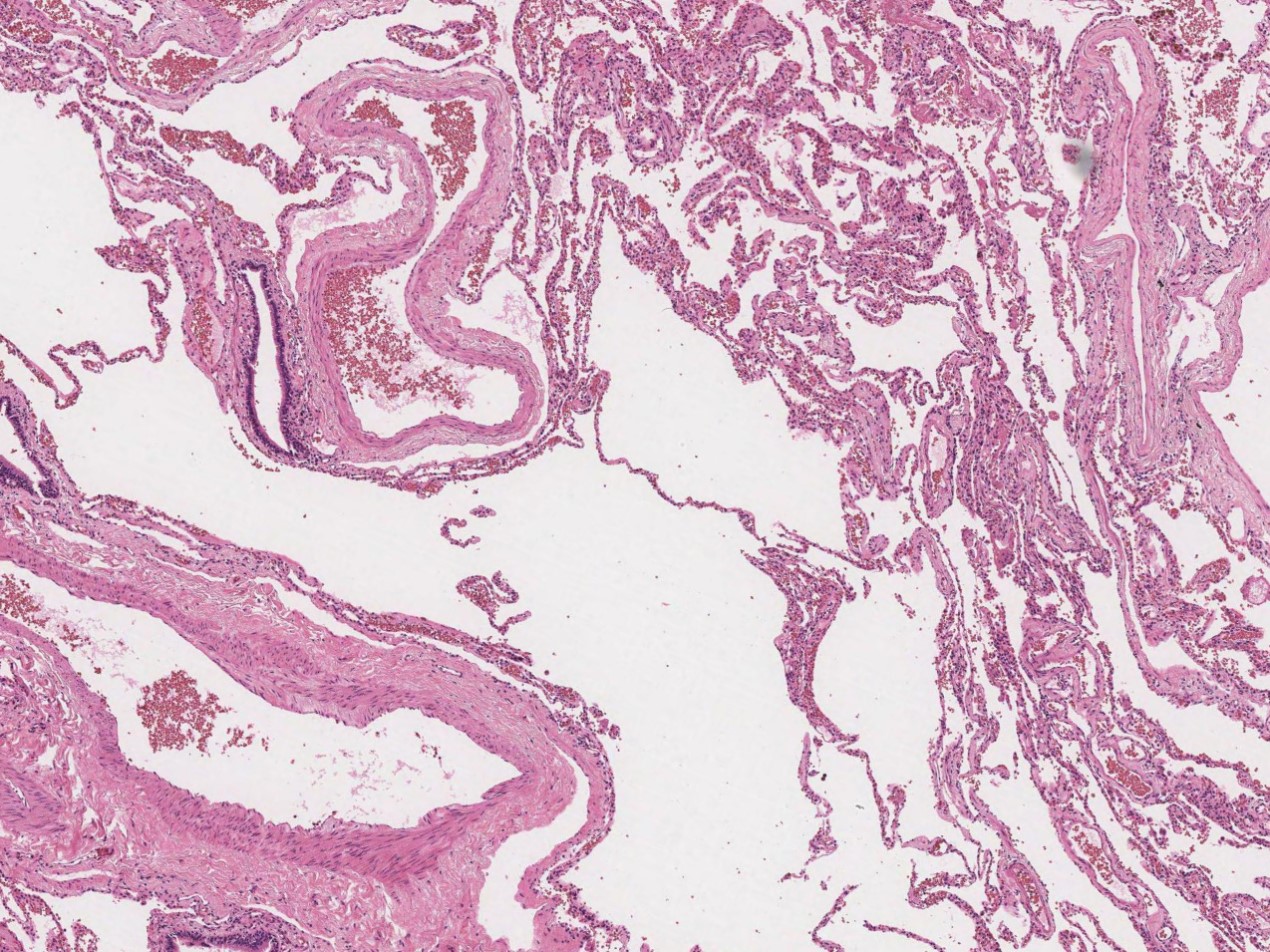
- Combined pulmonary fibrosis and emphysema (CPFE)
- Centrilobular emphysema in upper lobes
- Usual interstitial pneumonia in lower lobes
- Interstitial emphysema
- Elongated or angulated spaces in fibrotic interstitium
- Surrounded by dense fibrosis and lining of multiple giant cells but not epithelium
- Most commonly around bronchovascular bundles
Microscopic (histologic) images
Positive stains
- Elastic stains, such as elastic van Gieson and elastica Masson
- Elastic fibers are less organized and appear unraveled and loose in emphysematous lung (Eur Respir J 2008;31:998)
- Not required for diagnosis
Videos
Emphysema histology
Emphysema classification
Sample pathology report
- Lung, right upper lobe, wedge resection:
- Squamous cell carcinoma (see comment)
- Comment: Background lung parenchyma with emphysema, respiratory bronchiolitis and smoking related interstitial fibrosis.
Differential diagnosis
- Usual interstitial pneumonia:
- Interstitial emphysema versus honeycomb change: honeycomb is the air space surrounded by bronchiolar epithelium on fibrotic wall
- Lymphangiomyomatosis:
- Cystic air spaces, proliferation of spindle to epithelioid cells (HMB45+)
- Pulmonary Langerhans cell histiocytosis:
- Stellate nodules with fibrosis and Langerhans cells (CD1a+)
Additional references
Practice question #1
Practice answer #1
B. Cigarette smoking has a strong association with emphysema, particularly centriacinar
Comment Here
Reference: Emphysema
Comment Here
Reference: Emphysema
Practice question #2
Which one of the following lung pathologies can be found in individual with alpha-1 antitrypsin deficiency (AATD)?
- Bronchiolitis
- Centriacinar emphysema
- Interstitial emphysema
- Panacinar emphysema
- Usual interstitial pneumonia
Practice answer #2
D. Lung pathologies in AATD patient include panacinar emphysema and bronchiectasis
Comment Here
Reference: Emphysema
Comment Here
Reference: Emphysema