Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Electron microscopy description | Electron microscopy images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Chunyu C. Antisynthetase syndrome associated myositis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/muscleantisynthetase.html. Accessed May 13th, 2024.
Definition / general
- Defined by the presence of 1 of the antisynthetase syndrome autoantibodies and at least 1 of the following 3 clinical features: interstitial lung disease, inflammatory myopathy or inflammatory polyarthritis
- Other common symptoms include Raynaud phenomenon, mechanic hands, skin rashes, sicca syndrome and constitutional symptoms, such as fever
- To date, 8 antisynthetase autoantibodies have been identified (Jo1, PL12, PL7, EJ, OJ, KS, Zo and Ha), all of which are directed against aminoacyl tRNA synthetases (ARS: enzymes that attach amino acid onto its corresponding tRNA)
- Reference: Autoimmun Rev 2014;13:367
Essential features
- Jo1 is the first identified and the most common anti-aminoacyl tRNA synthetase (ARS) autoantibody, affecting 18% of European patients with idiopathic immune myopathies, other anti-aminoacyl tRNA synthetase autoantibodies collectively accounted for 3% (Ann Rheum Dis 2001;60:116)
- Majority of patients with anti-aminoacyl tRNA synthetase autoantibodies also have the anti-Ro52 / SSA autoantibody that is commonly associated with Sjögren disease (Autoimmun Rev 2009;8:632)
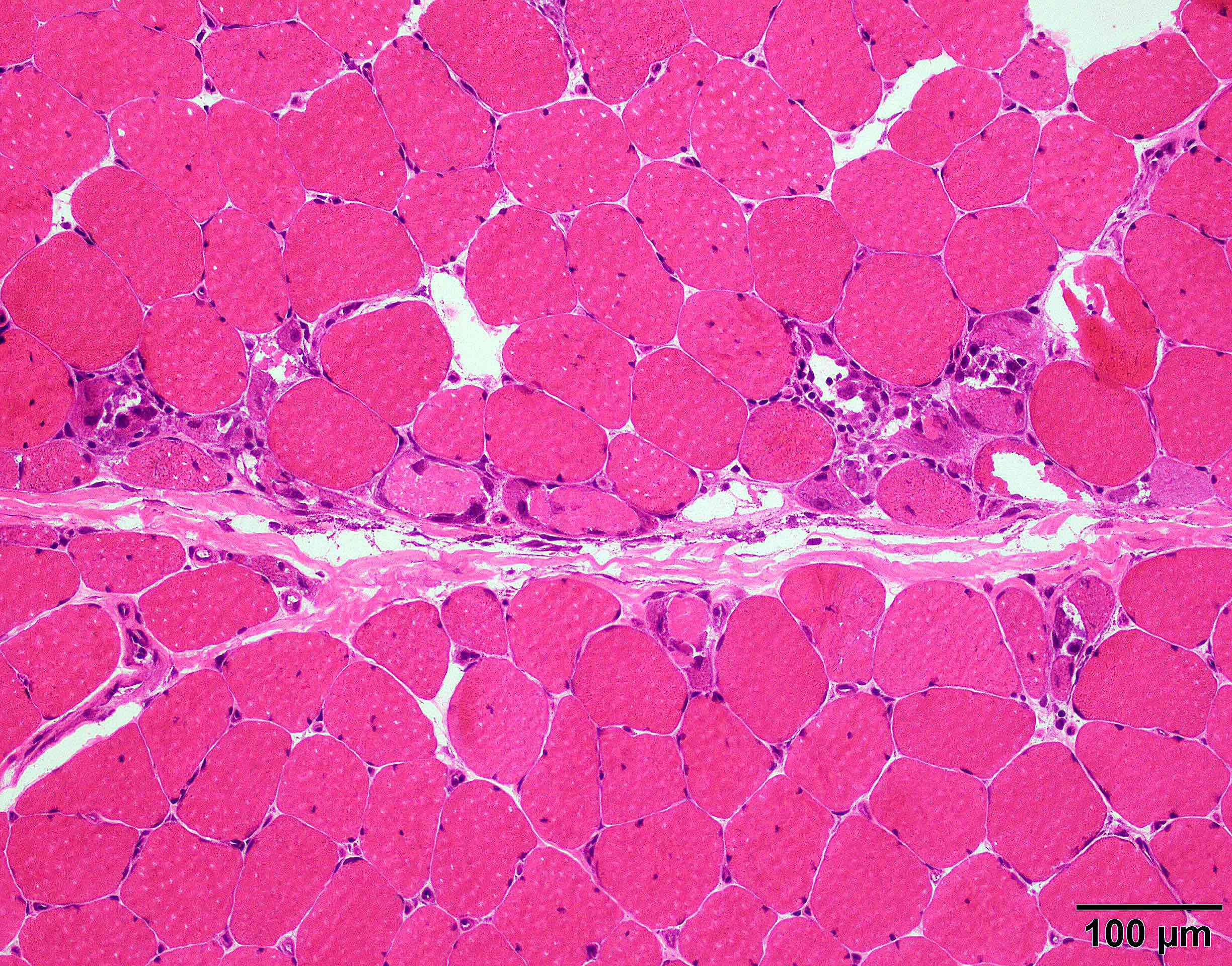
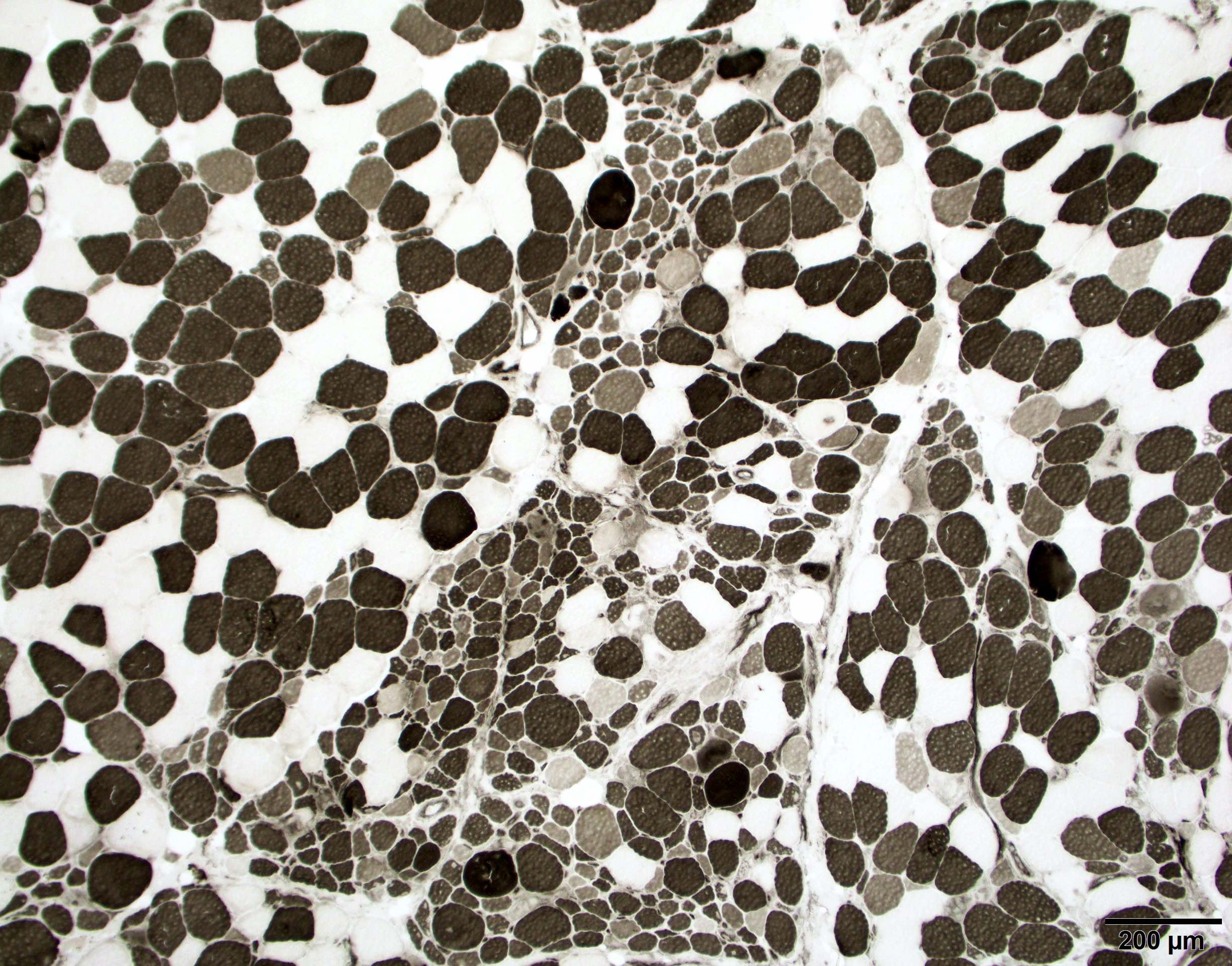
- Histopathologically, Jo1 antibody positive patients show a characteristic necrotizing perifascicular myositis (Brain 2015;138:2485)
- This injury pattern has also been referred to as immune myopathies with perimysial pathology (Curr Opin Rheumatol 2011;23:595)
- Myositis associated with PL7, EJ, OJ or KS autoantibodies demonstrates similar perifascicular necrotizing myopathy as Jo1 myositis (Brain 2016;139:e50)
- Patients with PL12 autoantibody may demonstrate severe interstitial lung disease but much milder muscle disease (Brain 2016;139:e50)
- When myositis is present, it demonstrates pathologically as immune mediated necrotizing myopathy: pauci-inflammation and randomly distributed necrotic fibers (Muscle Nerve 2012;46:282)
- Patients with anti-Jo1 are more likely to have cancer than patients with anti-PL7 / PL12 (13% versus 5%), while anti-PL7 / PL12 positive patients are far more likely to exhibit interstitial lung disease than Jo1 (90% versus 68%) (Autoimmun Rev 2012;11:739)
- Coexistence of Jo1 and anti-Ro52 seems to be associated with increased risk of malignancy (19%) (Semin Arthritis Rheum 2012;41:890)
- Small series of patients with OJ, KS, Zo and Ha antibodies indicate they have a similar clinical profile as other antisynthetase syndrome (Best Pract Res Clin Rheumatol 2020;34:101503)
Terminology
- Antisynthetase syndrome
- Aminoacyl tRNA synthetases (ARS)
- Necrotizing perifascicular myositis
- Immune myopathies with perimysial pathology
ICD coding
- ICD-10: M35.8 - other specified systemic involvement of connective tissue
Epidemiology
- ~25% of all immune and inflammatory myopathies patients may have antisynthetase syndrome, providing a prevalence estimate of 1/25,000 - 33,000 worldwide
- F:M = 2:1
- Mean age at presentation is 40 - 59
- Reference: Autoimmun Rev 2014;13:883
Sites
- Muscle, joints and lung (Autoimmun Rev 2014;13:367)
Pathophysiology
- Unknown
Etiology
- Unknown; genetic predisposition, viral infections and medication use may play a role (Curr Med Chem 2015;22:1963)
Clinical features
- Hallmark clinical features of antisynthetase syndrome are myositis, polyarthritis (62%) and interstitial lung disease (70%)
- Other common symptoms include Raynaud phenomenon (47%), fever (43%), skin rashes (32%), mechanic hands (28%), sclerodactyly (12%) and cancer (9%)
- Patients with non anti-Jo1 anti-aminoacyl tRNA synthetase autoantibodies are more likely to present with interstitial lung disease, while those with anti-Jo1 autoantibodies are more likely to present with myositis and arthralgia
- Reference: Autoimmun Rev 2014;13:883
Diagnosis
- Based on the clinical features and confirmed in the presence of positive serologic testing for anti-aminoacyl tRNA synthetase antibodies (anti-Jo1, anti-PL12, anti-PL7, anti-OJ, anti-KS, anti-Ha, anti-Zo) (Autoimmun Rev 2014;13:367)
- Interstitial lung disease is diagnosed by high resolution computed tomography of the lungs (see radiology description)
- Absence of myositis or interstitial lung disease does not exclude the diagnosis of antisynthetase syndrome
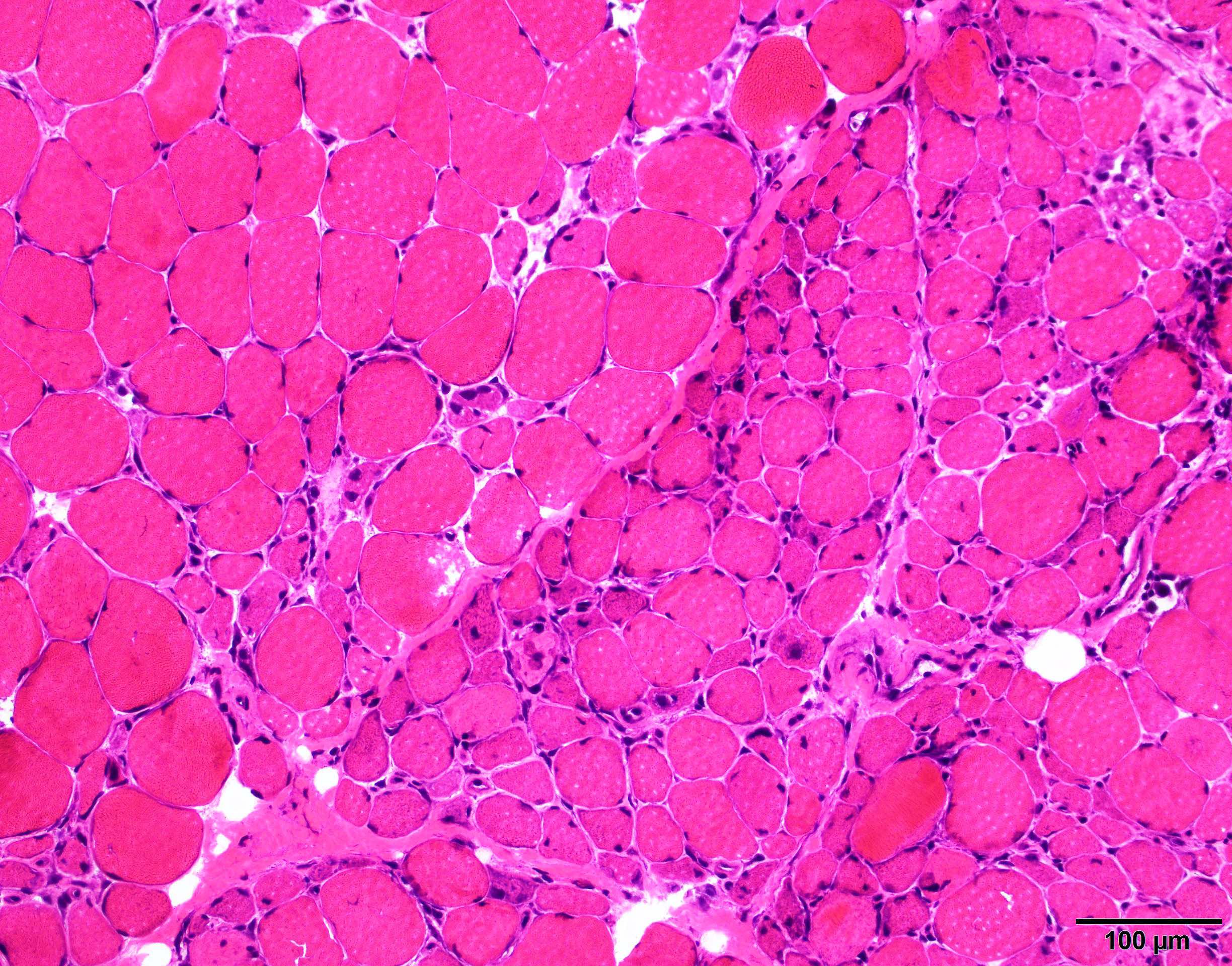
- Features on the muscle biopsy include necrotizing perifascicular myositis and perimysial connective tissue damage or necrotizing myopathy (Brain 2015;138:2485, J Neurol Neurosurg Psychiatry 2000;68:472, Muscle Nerve 2012;46:282)
Laboratory
- Presence of positive anti-aminoacyl tRNA synthetase antibodies (anti-Jo1, anti-PL12, anti-PL7, anti-OJ, anti-KS, anti- Ha, anti-Zo)
- Creatine kinase levels are often significantly elevated
- Majority of patients with anti-aminoacyl tRNA synthetase autoantibodies also have the anti-Ro52 / SSA autoantibody that is commonly associated with Sjögren disease (Autoimmun Rev 2009;8:632)
Radiology description
- Most frequent patterns are nonspecific interstitial pneumonia (70% of the patients) and organizing pneumonia (20% of the patients)
- Nonspecific interstitial pneumonia pattern characterized by patchy or diffuse ground glass opacities with associated reticular opacities
- Organizing pneumonia pattern characterized by peribronchial or subpleural consolidation or ground glass opacities without fibrosis
- Muscle MRI finding is not specific
- Reference: Eur Radiol 2019;29:5349
Prognostic factors
- Chronic, requiring long term treatment
- Most common causes of death were pulmonary fibrosis (49%) and pulmonary hypertension (11%)
- Patients with non-Jo1 anti-aminoacyl tRNA synthetase autoantibodies have worse survival than Jo1 positive patients
- 5 and 10 year unadjusted cumulative survivals were 90% and 70% for Jo1 patients and 75% and 47% for non-Jo1 patients (p < 0.005)
- References: Ann Rheum Dis 2014;73:227, Autoimmun Rev 2012;12:210
Case reports
- 21 year old man with fever, arthralgia and pulmonary infiltrates (N Engl J Med 2012;367:2134)
- 36 year old woman with fatigue, weight loss, progressive weakness in a scapuloperoneal distribution and dysphagia (J Clin Neuromuscul Dis 2017;18:223)
- 52 year old man with asymmetric polyarthralgia, myalgia, weight loss, dyspnea and progressive muscle weakness (Clin Rheumatol 2013;32:715)
- 68 year old woman with eosinophilic pleural effusion (Intern Med 2018;57:2227)
Treatment
- No FDA approved medication for antisynthetase syndrome
- Treatment of antisynthetase syndrome should target the most severe or life threatening disease manifestation, often interstitial lung disease
- Treatment of antisynthetase syndrome associated myositis is not significantly different from other idiopathic inflammatory myopathies
- Reference: Best Pract Res Clin Rheumatol 2020;34:101503
Microscopic (histologic) description
- See diagnosis
Microscopic (histologic) images
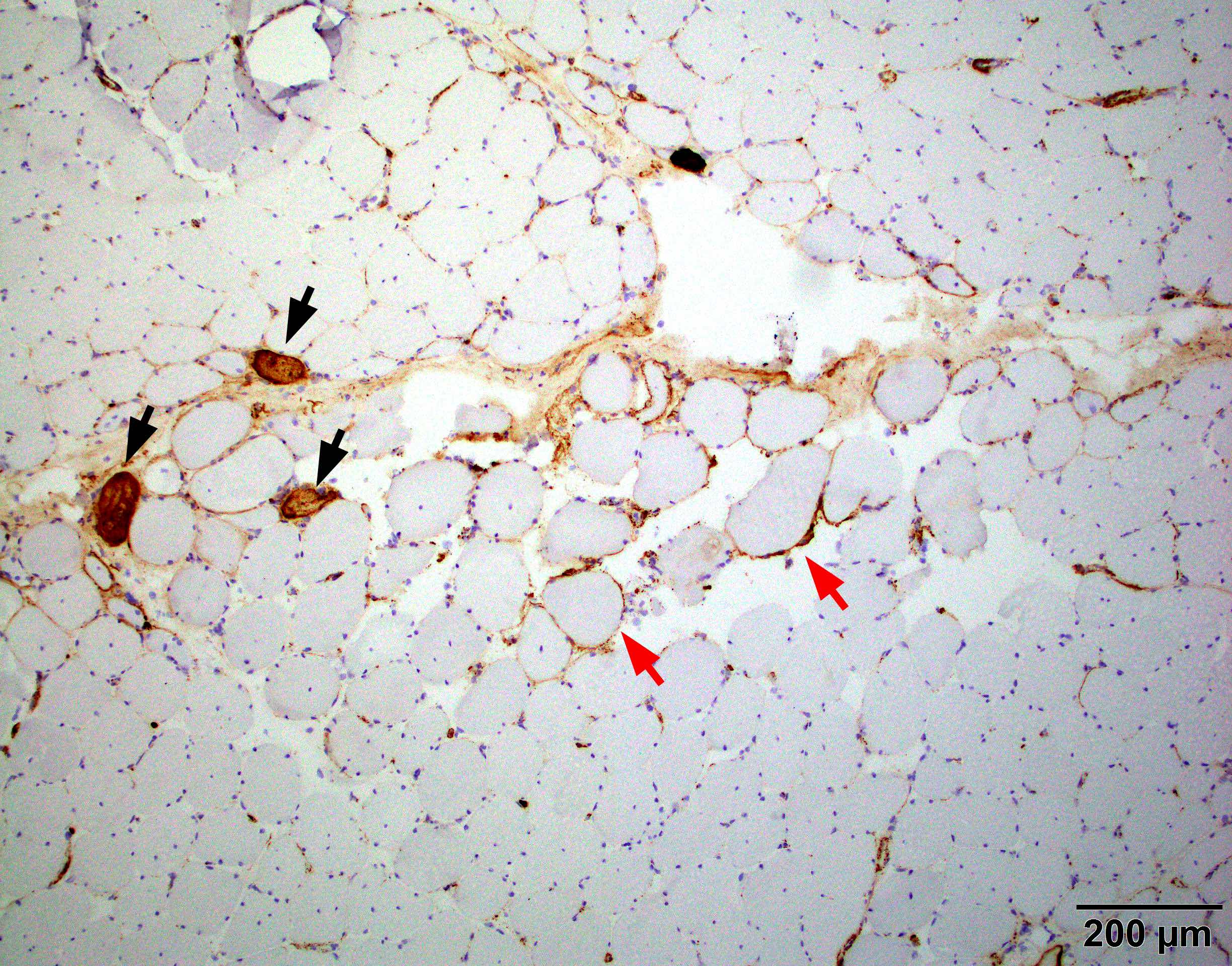
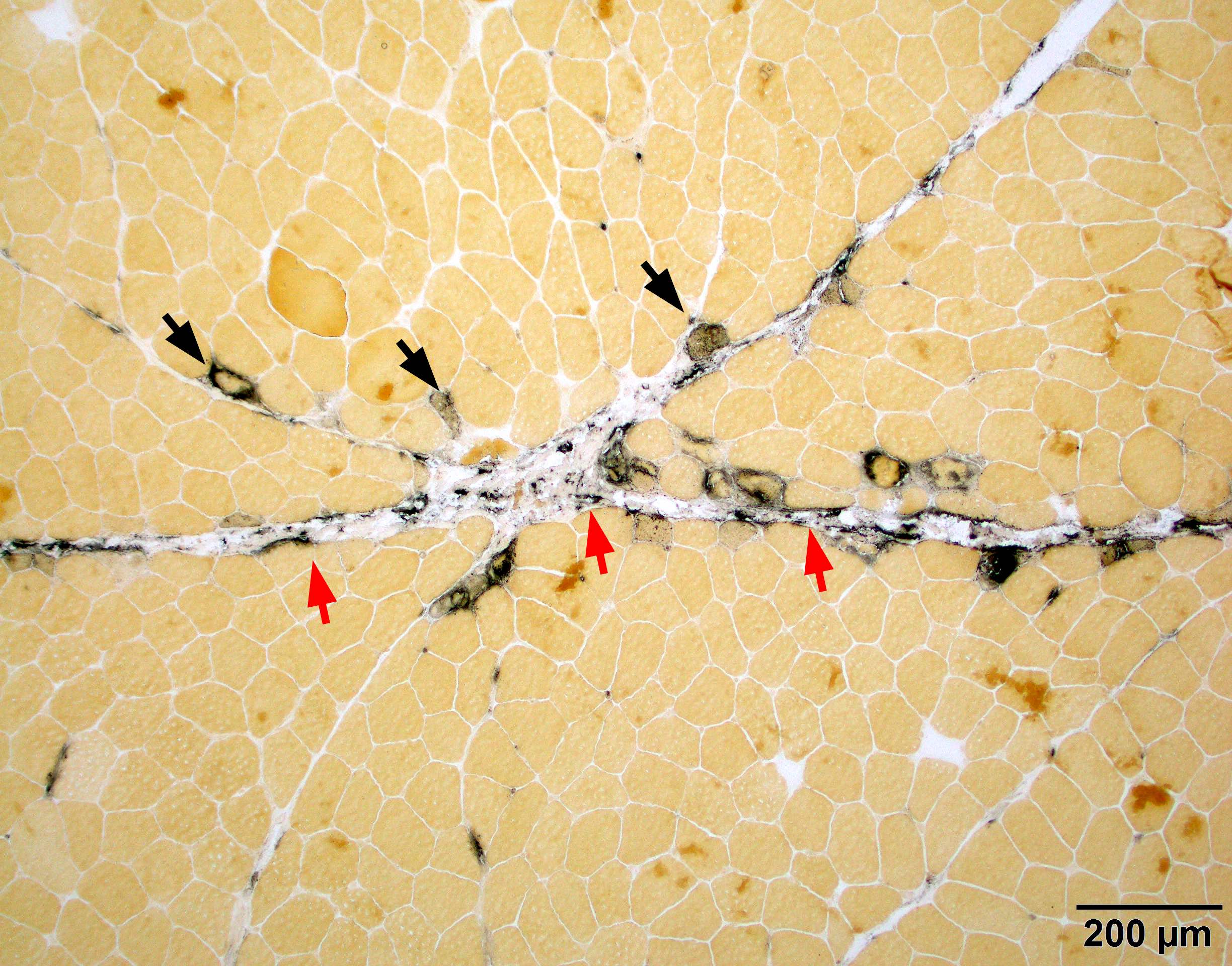
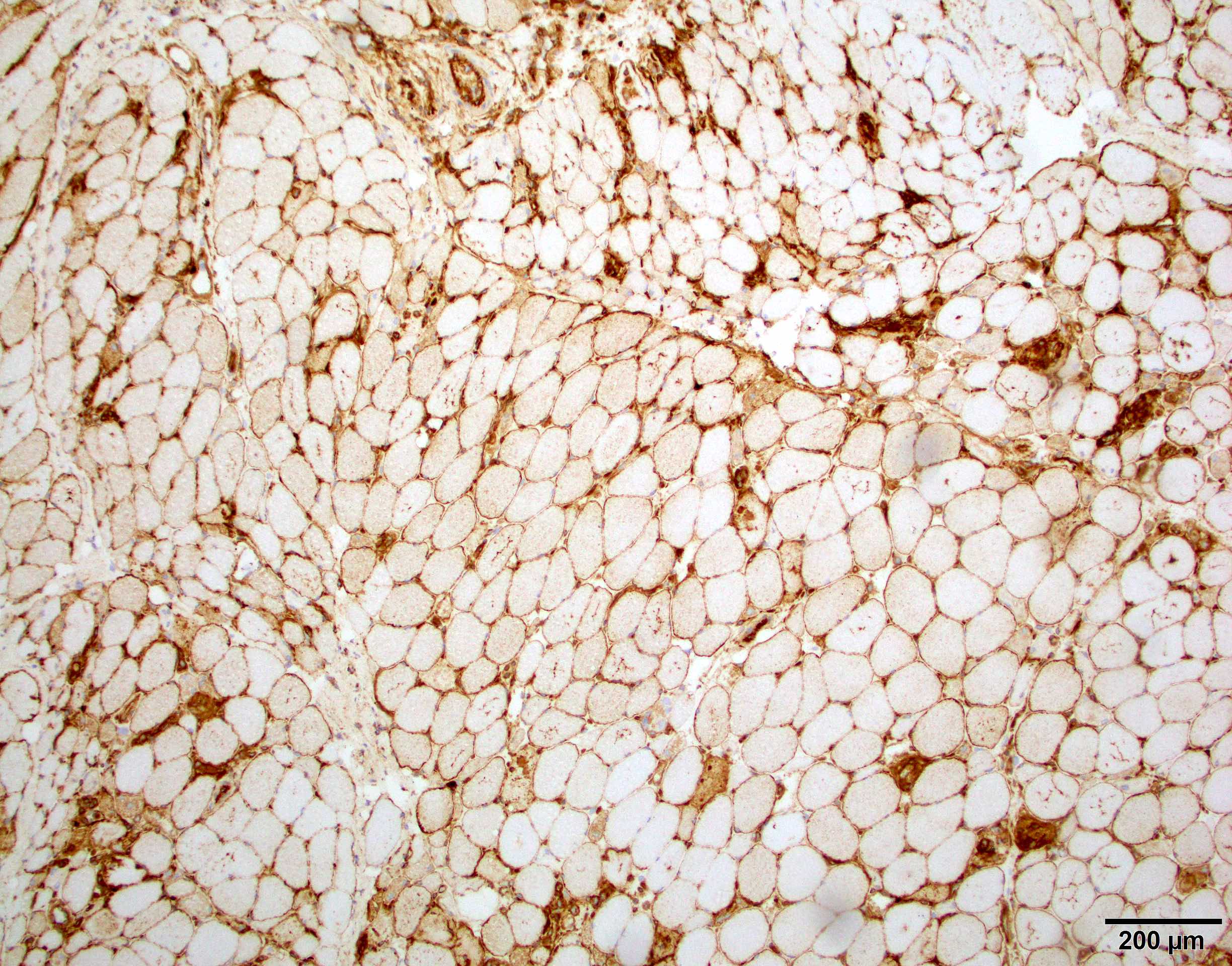
Positive stains
- Strong sarcoplasmic C5b9 expression is seen in acutely necrotic fibers
- Sarcolemmal C5b9 expression in a subset of viable myofibers, mostly perifascicular fibers
- Capillary C5b9 expression can be seen but usually less frequent than dermatomyositis
- MHC1 is diffusely positive or patchy and accentuated in perifascular fibers
- Alkaline phosphatase shows prominent perimysial connective tissue damage
- CD8+ T cells are found in both perimysium and endomysium
- CD4+ T cells are mainly found in perimysium and around vessels
- CD20+ B cells are either absent or restricted to perimysium
- References: Brain 2015;138:2485, J Neurol Neurosurg Psychiatry 2000;68:472
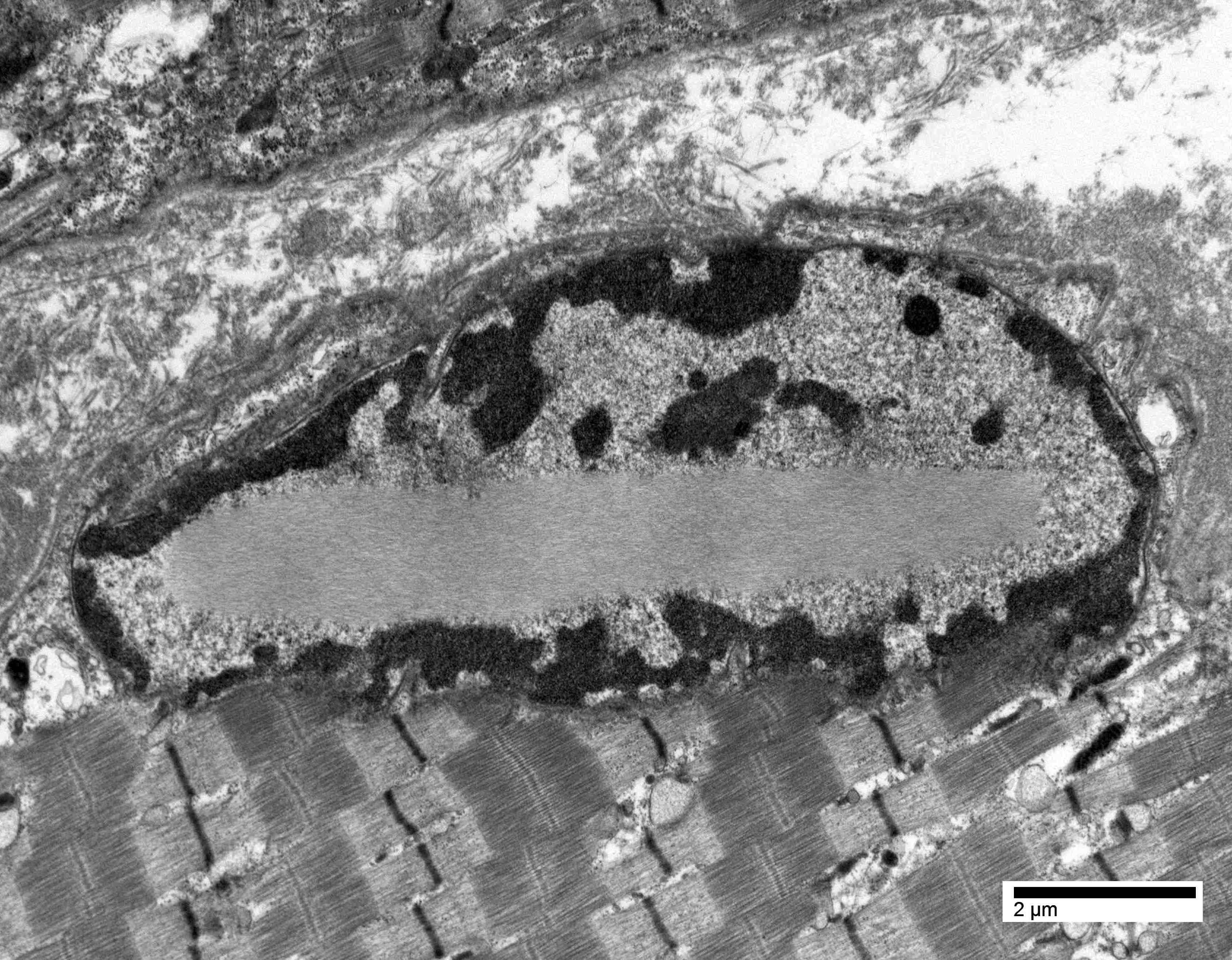
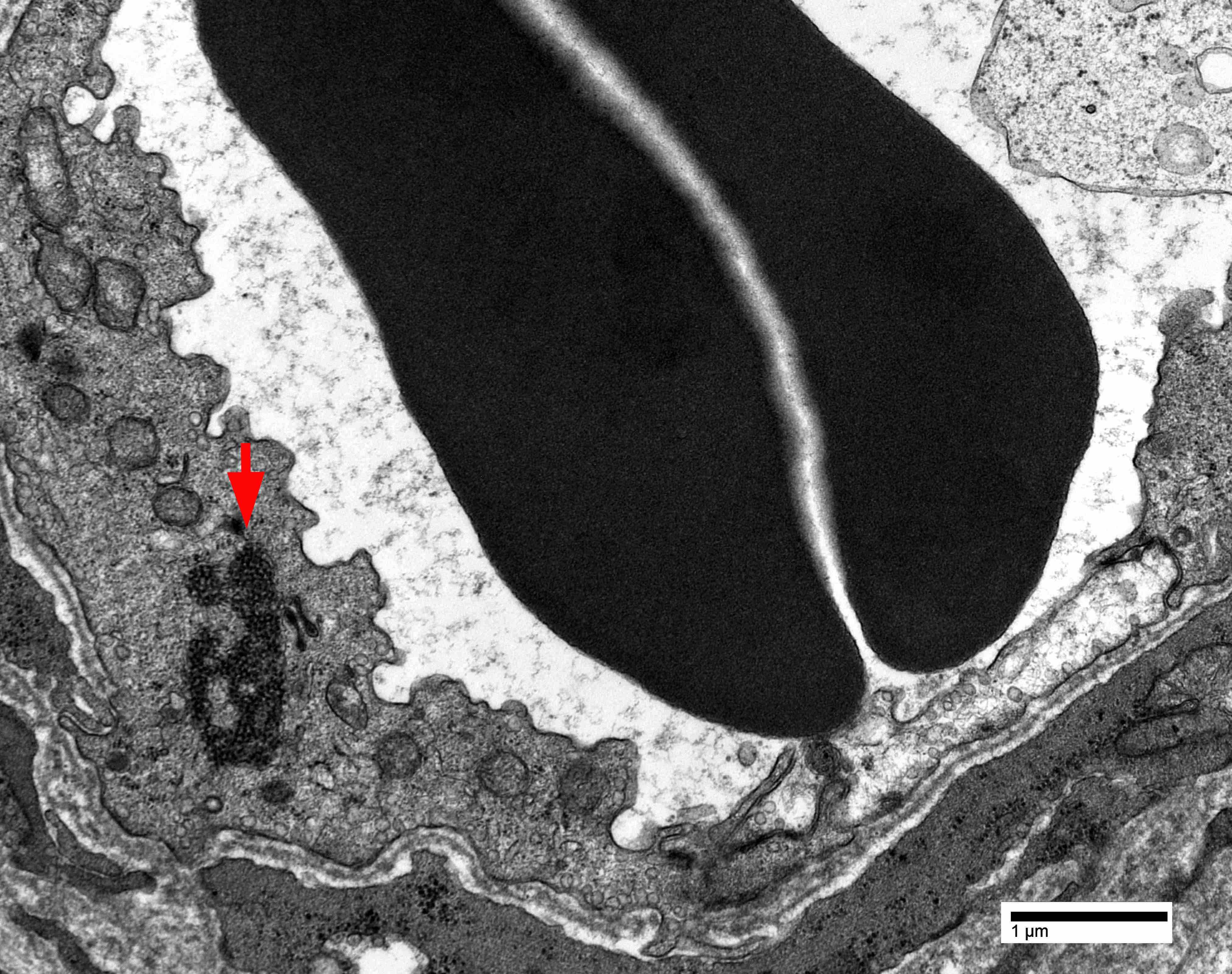
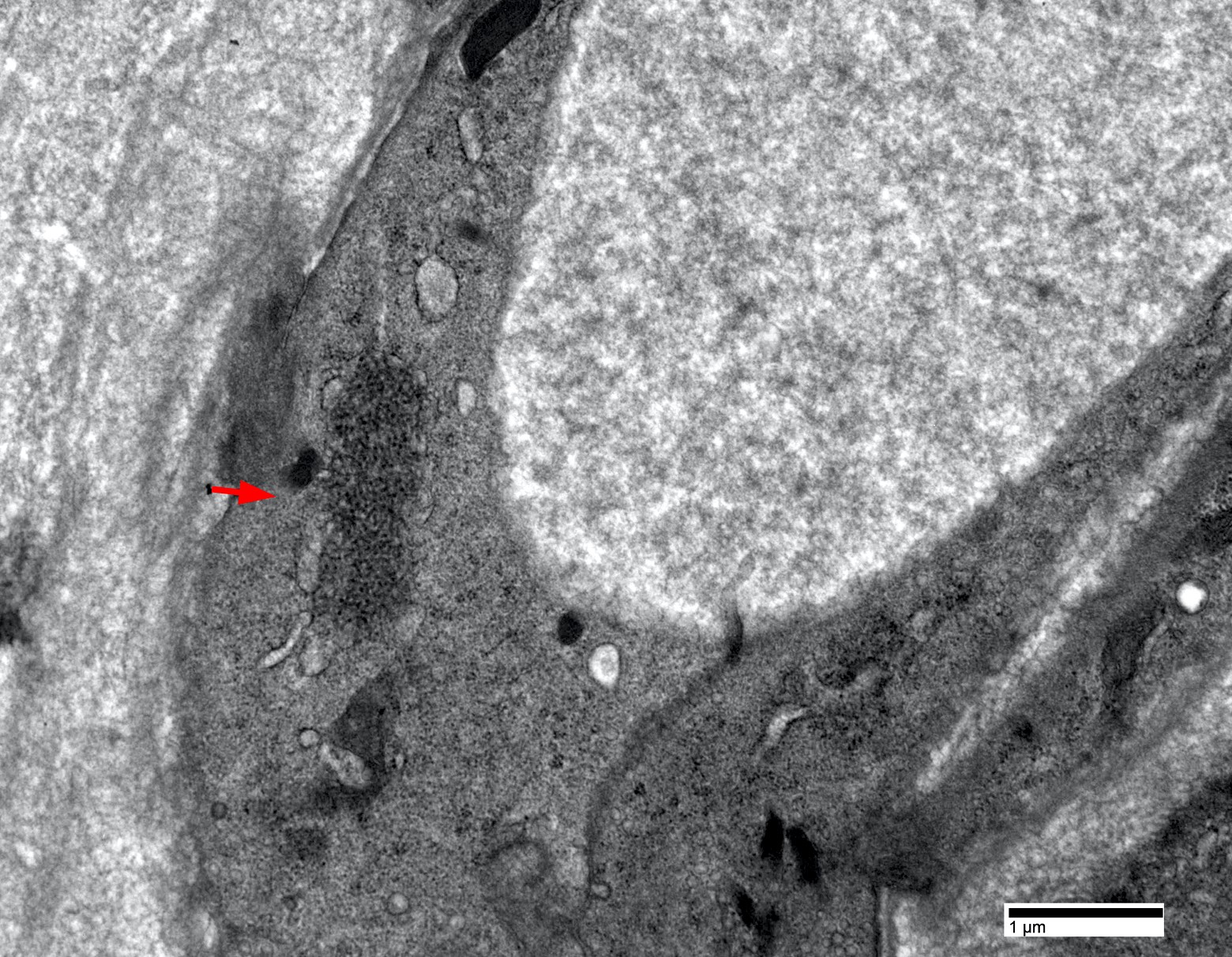
Electron microscopy description
- Endothelial tubuloreticular inclusions can be present but much less frequent than dermatomyositis (Brain 2015;138:2485)
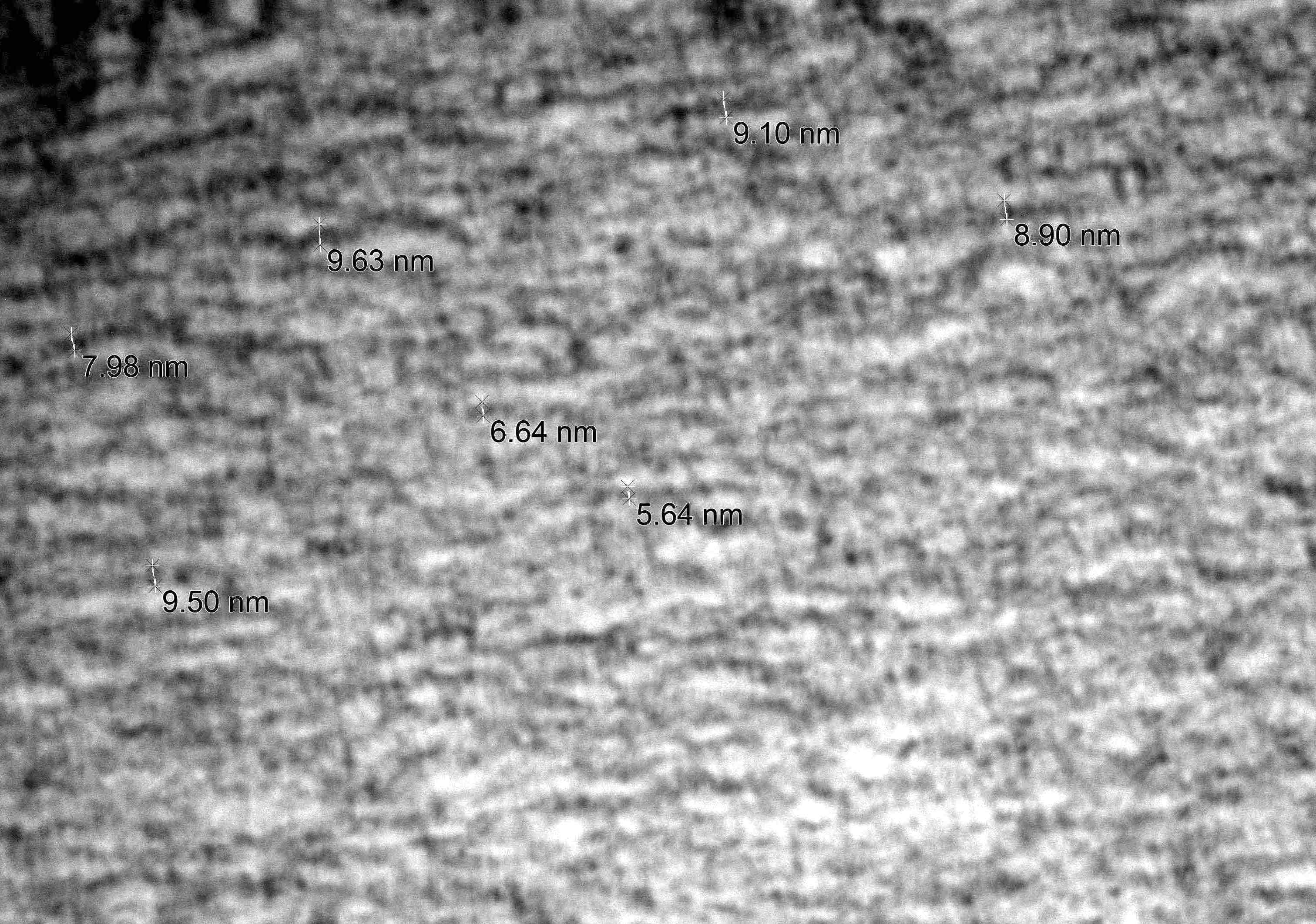
- Intranuclear actin aggregation is an electron microscopy hallmark for antisynthetase syndrome (Neurology 2015;84:1346)
Electron microscopy images
Sample pathology report
- Skeletal muscle, left quadriceps (biopsy):
- Inflammatory myopathy with abundant necrotic fibers, perifascicular atrophy and perimysial connective tissue damage (see comment)
- Comment: The quadriceps muscle biopsy shows multifocal perimysial lymphohistiocytic inflammation, abundant necrotic fibers, perifascicular atrophy and perimysial connective tissue damage. Immunostaining shows patchy myofiber MHC1 upregulation with perifascicular accentuation. Ultrastructural examination demonstrates rare but unequivocal endothelial tubuloreticular inclusions in capillary. The main diagnostic considerations include dermatomyositis and necrotizing perifascicular myositis, which may show overlapping features exemplified by this case (Brain 2015;138:2485). The latter is highly associated with serum anti-Jo1 antibody and interstitial lung disease. Correlation with serology and chest imaging is recommended.
Differential diagnosis
- Dermatomyositis:
- Significant overlap between the histology of dermatomyositis and antisynthetase syndrome associated myositis
- Differentiation is not always possible solely based on histology, correlation with serology is highly recommended
- Generally shows more perifascicular atrophy and less perifascicular necrosis than Jo1 myositis (Brain 2015;138:2485)
- However, dermatomyositis with Mi2 autoantibody may show a perifascicular necrotizing myopathy pattern identical to Jo1 myositis (Acta Neuropathol Commun 2020;8:125)
- Immune mediated necrotizing myopathy:
- Typically lacks visible lymphocytic inflammation or significant MHC1 upregulation
- Necrotic fibers are randomly scattered (Curr Rheumatol Rep 2018;20:21, J Neurol Neurosurg Psychiatry 2016;87:1038)
- Other overlap myositis, such as systemic sclerosis / myositis with anti-PM / Scl antibodies, Sjögren syndrome, lupus:
- Differentiation relies on correlations of muscle pathology, clinical symptoms and serum autoantibodies (Autoimmun Rev 2014;13:883)
- Polymyositis:
- Due to the rapid discovery of serum autoantibodies, diagnosis has been drastically reduced or entirely abandoned (Neuromuscul Disord 2015;25:268, JAMA Neurol 2018;75:1528)
- Most patients with the traditional polymyositis diagnosis now fall in the immune mediated necrotizing myopathy or antisynthetase syndrome categories (JAMA Neurol 2018;75:1528)
Additional references
Board review style question #1
A 57 year old man presents with shortness of breath, weakness and elevated creatine kinase levels. Chest CT shows bilateral lung ground glass opacities. Muscle biopsy shows necrotic fibers and myophagocytosis predominantly involving perifascicular fibers. The perimyisial connective tissue appears edematous and fragmented. Which of the following is the most likely diagnosis?
- Antisynthetase syndrome
- Dermatomyositis
- Immune mediated necrotizing myopathy
- Inclusion body myositis
- Polymyositis
Board review style answer #1
Board review style question #2
Which of the following is a distinctive pathological feature between antisynthetase syndrome myositis and dermatomyositis?
- Endothelial tubuloreticular inclusions
- Intranuclear actin aggregate
- Myofiber sarcolemma C5b9 deposition
- Perifascicular atrophy
- Perifascicular myofiber necrosis
Board review style answer #2
B. Intranuclear actin aggregate. In inflammatory myopathies, so far, intranuclear actin aggregate has only been reported in antisynthetase syndrome myositis. All other answer choices can be seen in both antisynthetase syndrome myositis and dermatomyositis.
Comment Here
Reference: Antisynthetase syndrome associated myositis
Comment Here
Reference: Antisynthetase syndrome associated myositis