Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Immunofluorescence description | Negative stains | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Huang C, Elsensohn AN. Atopic dermatitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumoracuteeczematousdermatitis.html. Accessed October 2nd, 2025.
Definition / general
- Eczema (or atopic dermatitis) is a general term that refers to a group of chronic and relapsing skin conditions that cause inflamed skin
- Signs and symptoms of atopic dermatitis include rash, pruritus and xerosis
Essential features
- Essential (required features) (J Am Acad Dermatol 2014;70:338)
- Pruritus and xerosis
- Age specific patterns with chronic or relapsing history
- Microscopic features are variable depending on the chronicity of the lesion (acute, subacute and chronic)
- Acute lesions show more marked spongiosis
- Subacute lesions show irregular acanthosis along with spongiosis
- Chronic lesions show hyperkeratosis, moderate to marked psoriasiform hyperplasia and variably mild spongiosis (Patterson: Weedon's Skin Pathology, 5th Edition, 2020)
Terminology
- Eczema: atopic dermatitis
- Dyshidrotic eczema: pompholyx, dyshidrosis
Epidemiology
- ~90% of patients develop eczema by 5 years of age
- ~60% of patients have an onset during the first year of life
- Initial onset is most common between 3 and 6 months of age
- Prevalence of onset peaks during early childhood
- Prevalence of eczema in American adults is ~7.2%; this includes adults with continuation of childhood disease and de novo eczema (J Investig Allergol Clin Immunol 2017;27:78, J Am Acad Dermatol 2014;70:338)
- Genetic predisposition is strongly and consistently associated with atopic dermatitis (Am Fam Physician 2012;86:35, Allergy Asthma Proc 2019;40:84, Int J Mol Sci 2020;21:6484)
- Family history of atopic disease is seen in 70% of patients
Sites
- Typical sites according to age group
- Infants (birth to 6 months): face, scalp, trunk and extensor aspects of extremities; sparing of diaper area
- Children (6 months to 12 years): flexural areas, including antecubital fossa, popliteal fossa, wrists, ankles and the nape of neck; dorsum of feet, hands and periorbital folds
- Adolescents and adults (12 years and beyond): flexural areas, hands, upper trunk and forehead
- Adults: head and neck, hands and feet (dyshidrotic eczema)
- References: J Investig Allergol Clin Immunol 2017;27:78, Pediatr Dermatol 2022;39:345, JAAD Int 2022:11:1
Pathophysiology
- Complex interactions of genetic predispositions, environmental triggers and immune dysregulation resulting in subsequent compromised skin barrier
- Mutation in filaggrin gene, a vital gene for skin cell maturity; causes a haphazard organization of the skin cells resulting in a disrupted epidermal barrier, which leads to increased water loss and decreased protection from harmful substances
- Reference: Br J Dermatol 2019;180:464
Etiology
- Exact cause is unknown
- Atopic dermatitis results from compromise of the skin barrier and inflammation
- Reference: J Allergy Clin Immunol Pract 2014;2:361
Clinical features
- Universal features include pruritus and xerosis
- Clinical presentation is variable according to the phase of disease, age of patient and changes during the disease course
- Atopic dermatitis may be categorized depending on the phase of the disease
- Acute: ill defined, oozing, crusted, eroded papules or vesicles on erythematous plaques
- Lesions on dark skinned individuals may appear as hypopigmentation or have follicular accentuation
- Subacute: thickened, scaly or excoriated plaques
- Chronic: thickened, hyperpigmented plaques, fibrotic papules or hypopigmentation resulting from extensive irritation and rubbing; lichenified skin from scratching results in accentuated skin fold lines
- Acute: ill defined, oozing, crusted, eroded papules or vesicles on erythematous plaques
- Reference: J Am Acad Dermatol 2014;70:338
Diagnosis
- Diagnosis can be established clinically from history and physical examination alone with adequate childhood and family history of allergies, asthma and skin disease (J Am Acad Dermatol 2014;70:338)
- Pruritus and xerosis with typical inflammatory skin lesions and excoriation in an age specific distribution
- Diagnosis is often straightforward in infants, children and adults with a childhood onset
- Adults with new onset dermatitis without childhood history of eczema must exclude other conditions with inflamed scaly rashes (J Investig Allergol Clin Immunol 2017;27:78)
- Skin biopsy may be required in adults with a de novo onset of pruritus rash
- Skin biopsy may also be performed in adult patients presenting with recalcitrant, eczematous dermatitis to rule out secondary causes
- Skin biopsy will not help in differentiating atopic dermatitis from allergic contact dermatitis or id reaction
Laboratory
- Elevated serum immunoglobulin E (IgE) level is seen in 80% of patients (J Am Acad Dermatol 2014;70:338)
- Serum IgE is not routinely obtained; can be helpful for uncertain diagnosis
- Skin patch testing is gold standard for identifying allergens (J Investig Allergol Clin Immunol 2017;27:78)
- Mainly helpful in adults with de novo atopic dermatitis with a history of possible allergen exposure to determine if the patient has allergic contact dermatitis rather than eczema
- Helpful in cases of refractory chronic atopic dermatitis unresponsive to treatment, rash with atypical pattern according to age and rash with a changing pattern
Prognostic factors
- ~70 - 90% of childhood eczema resolves by adulthood (J Am Acad Dermatol 2014;70:338)
- ~12% of childhood cases have a relapsing disease course with resolution in adolescence and recurrence in adulthood (J Investig Allergol Clin Immunol 2017;27:78)
- Factors associated with increased severity of persistent or recurring dermatitis and poor healing include family history, associated allergic rhinitis or asthma, early age at onset, female (adults) and severe atopic dermatitis (Acta Derm Venereol 1985;65:206)
Case reports
- 9 month old boy with refractory atopic dermatitis (Ann Allergy Asthma Immunol 2018;120:23)
- 12 year old boy with eczematous skin lesion (J Plast Surg Case Stud 2023;4:001)
- 56 year old man with dyshidrotic eczema (Cureus 2020;12:e10839)
Treatment
- Restore and maintain epidermal barrier: emollient, oil baths, topical moisturizers
- Identification and avoidance of potential allergens and triggers
- Anti-inflammatory treatment: topical steroids (to include wet wraps), calcineurin inhibitors, oral steroids, oral antihistamines and cyclosporine (rapid onset); more recent targeted and effective therapies include subcutaneous IL4R inhibitors, subcutaneous IL13R inhibitors and oral JAK inhibitors
- Ultraviolet (UV) therapy has been proven to be helpful in patients
- Treatment of secondary skin infections
- Reference: Postepy Dermatol Alergol 2020;37:1
Clinical images
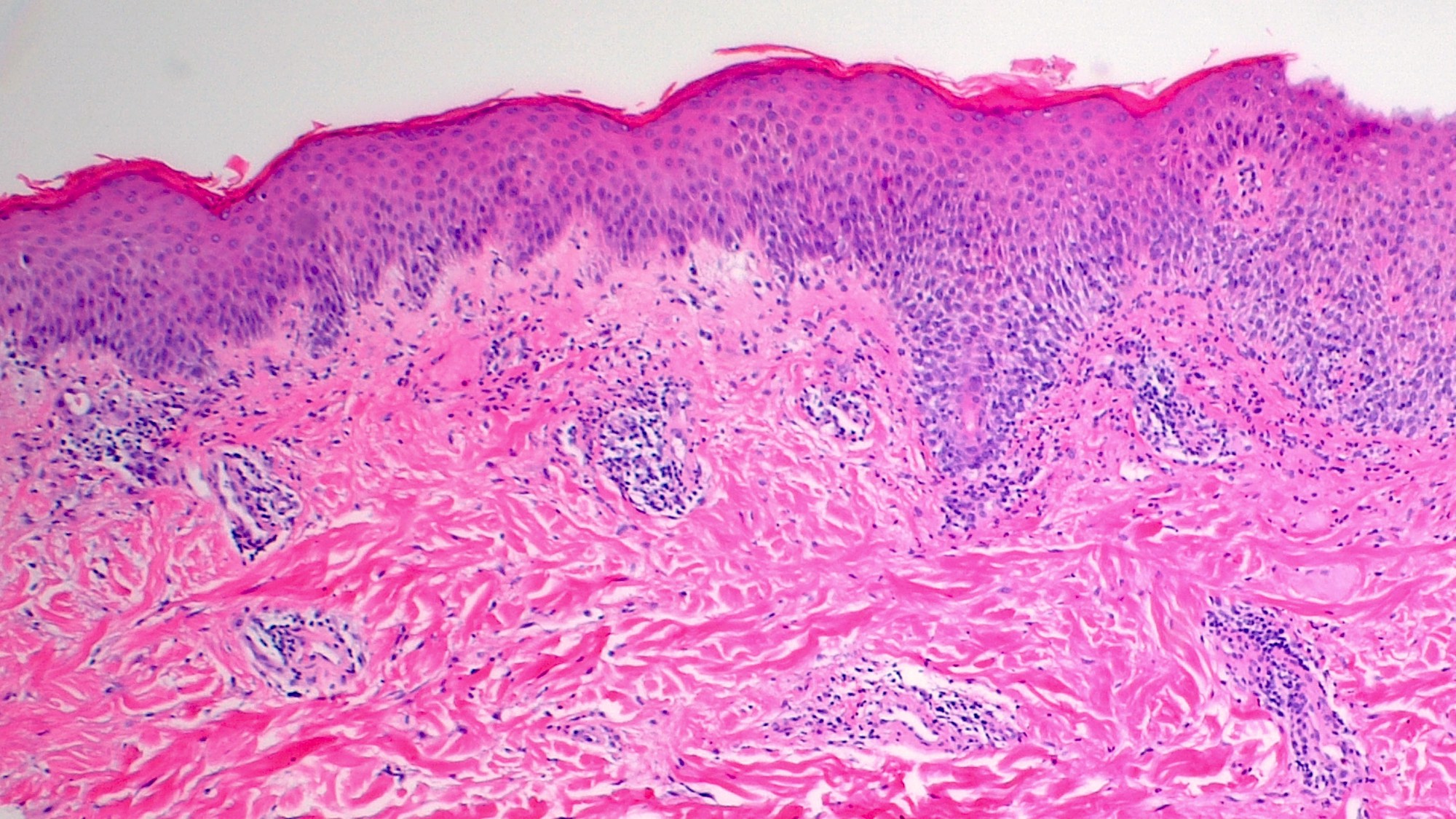
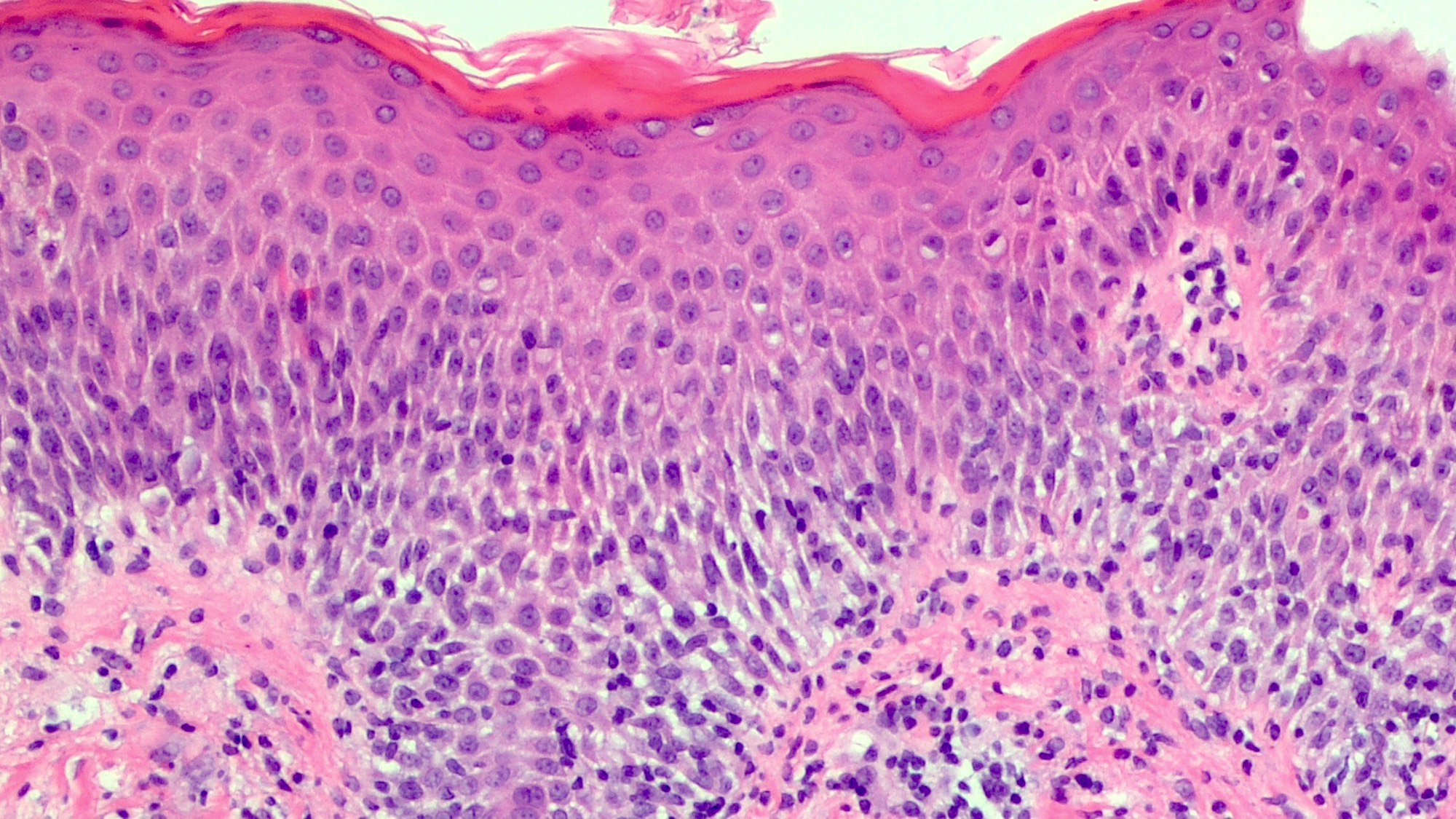
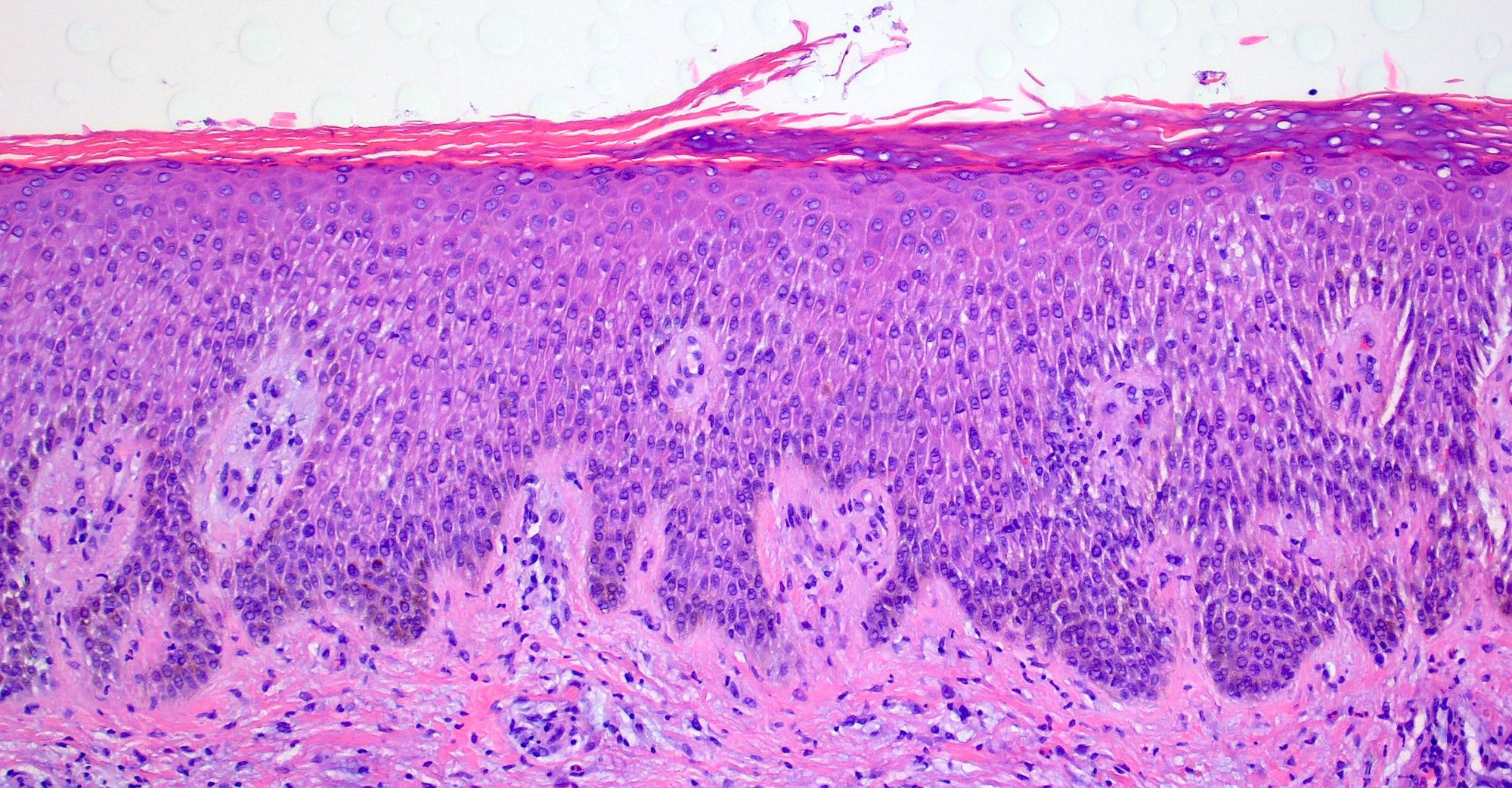
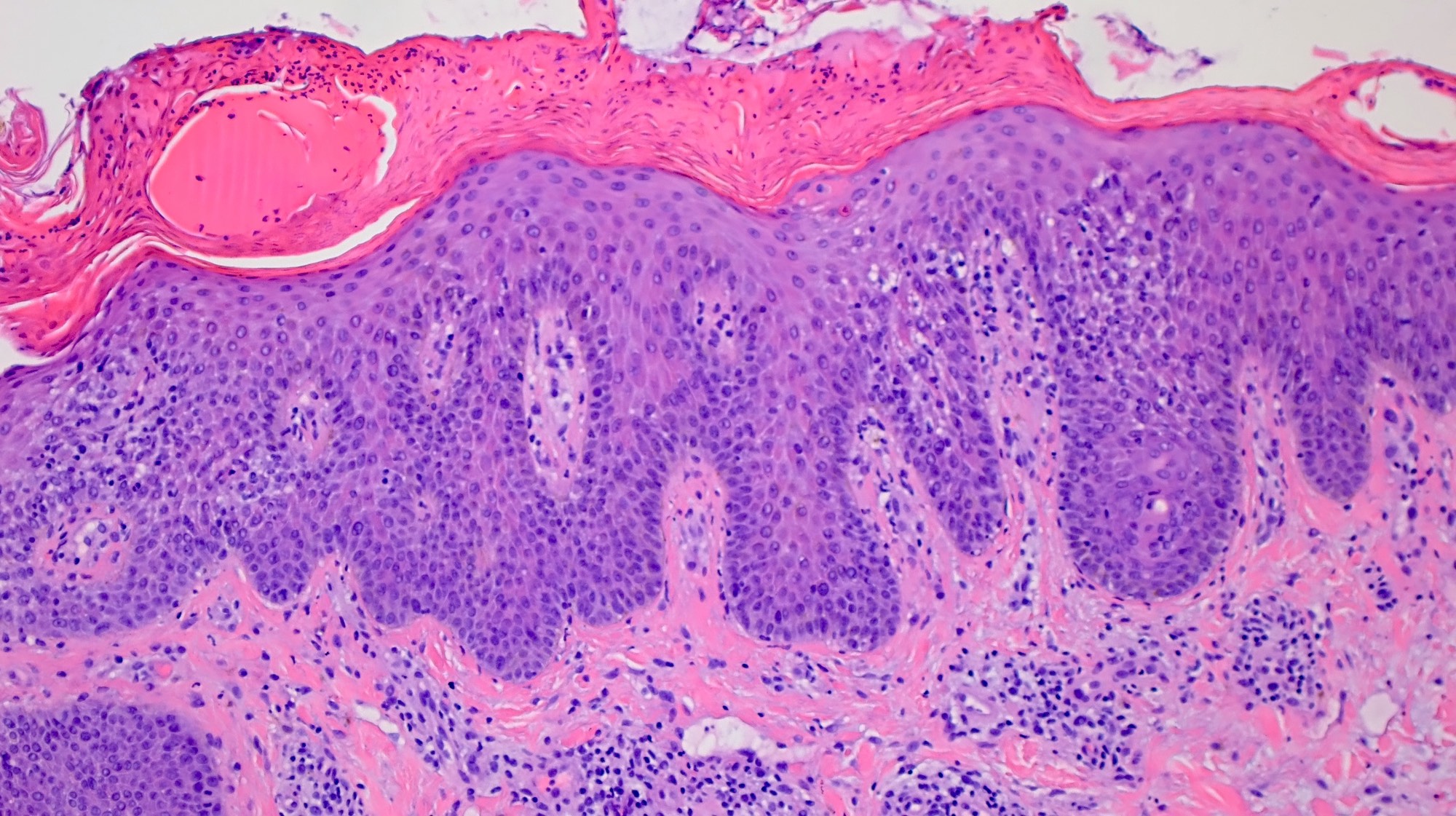
Microscopic (histologic) description
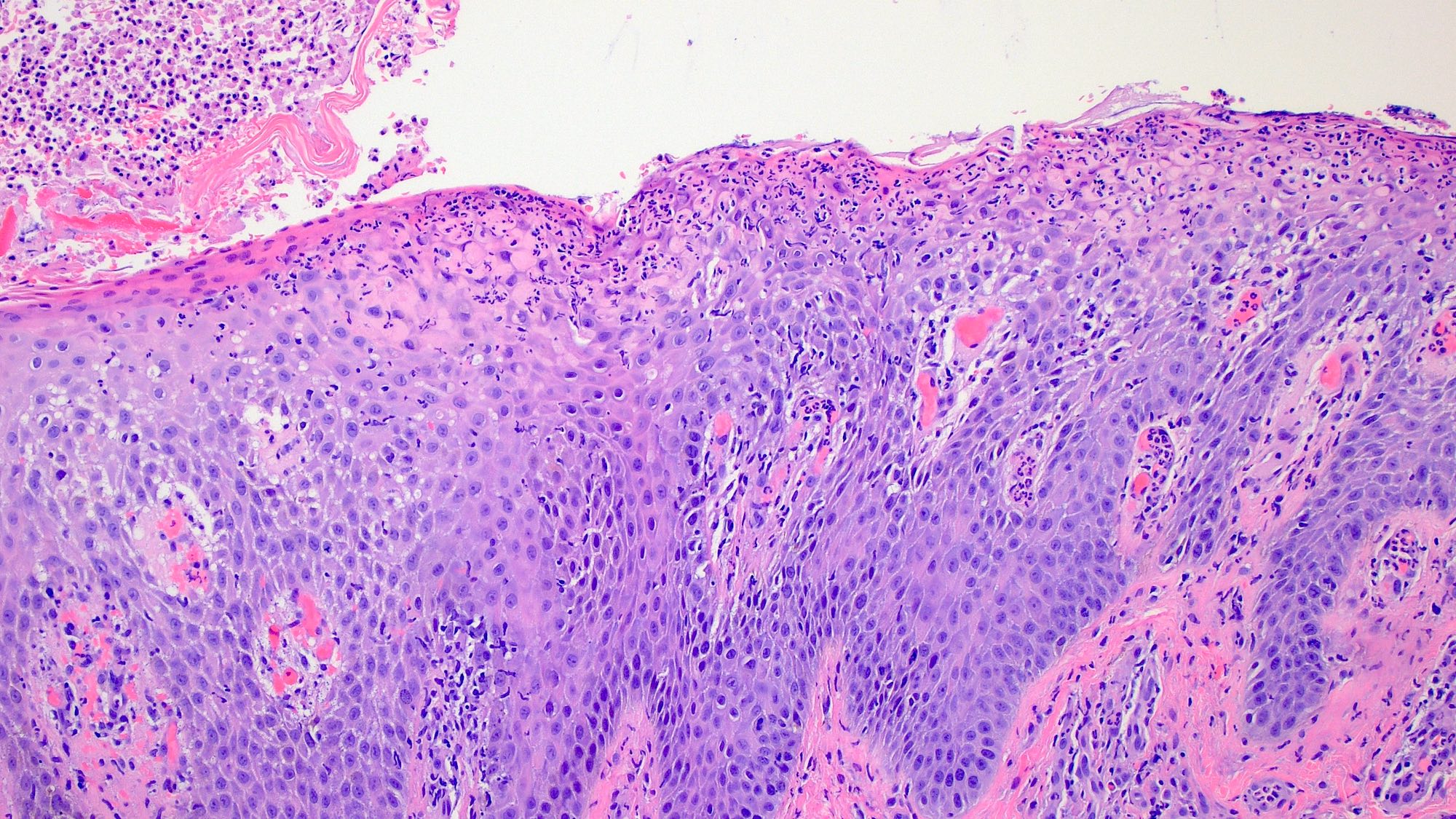
- Atopic dermatitis falls under the spongiotic dermatosis pattern histologically; spongiotic dermatitis is a microscopic terminology while atopic dermatitis (eczema) is a clinical diagnosis
- Microscopically, atopic dermatitis is broken down into 3 stages
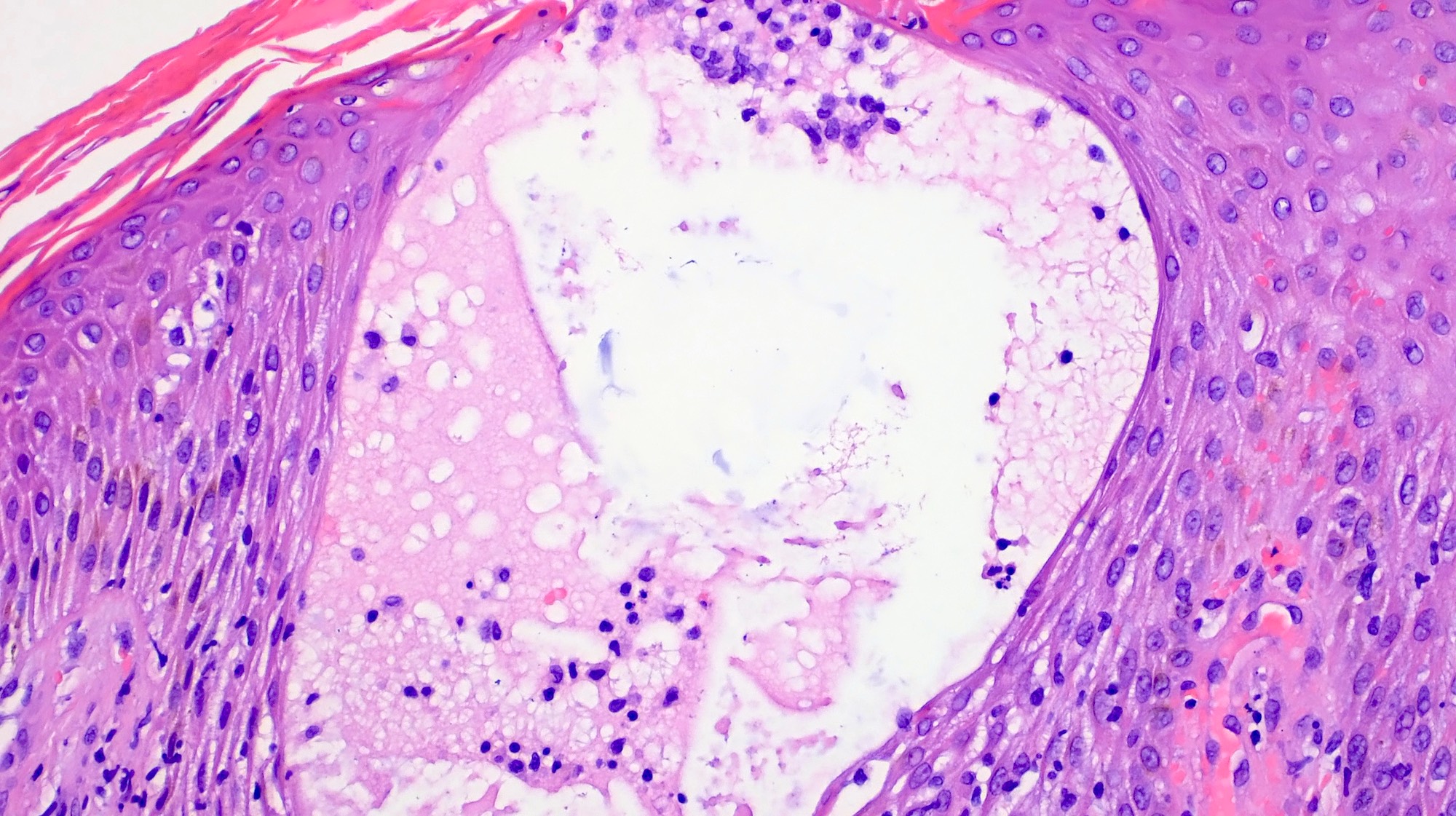
- Acute eczema
- Retained basket weave orthokeratosis
- Spongiosis featuring intercellular edema with widening of the intercellular spaces showing accentuation of intercellular bridges of the squamous epithelium
- Intradermal microvesicles or less commonly, subepidermal microvesicles
- Vesicles filled with proteinaceous fluid containing lymphocytes, histiocytes and occasional eosinophils
- Variable dermal edema with highly variable mixed inflammatory cell infiltrates composed of lymphocytes, histiocytes and occasionally eosinophils or neutrophils
- Subacute eczema (most frequently encountered type of eczema for pathologists)
- Irregular acanthosis and parakeratosis
- Mild to moderate spongiosis with focal spongiotic vesiculation
- Exocytosis of inflammatory cells
- Associated superficial dermal perivascular lymphohistiocytic inflammatory infiltrate
- Swelling of endothelial cells
- Papillary dermal edema
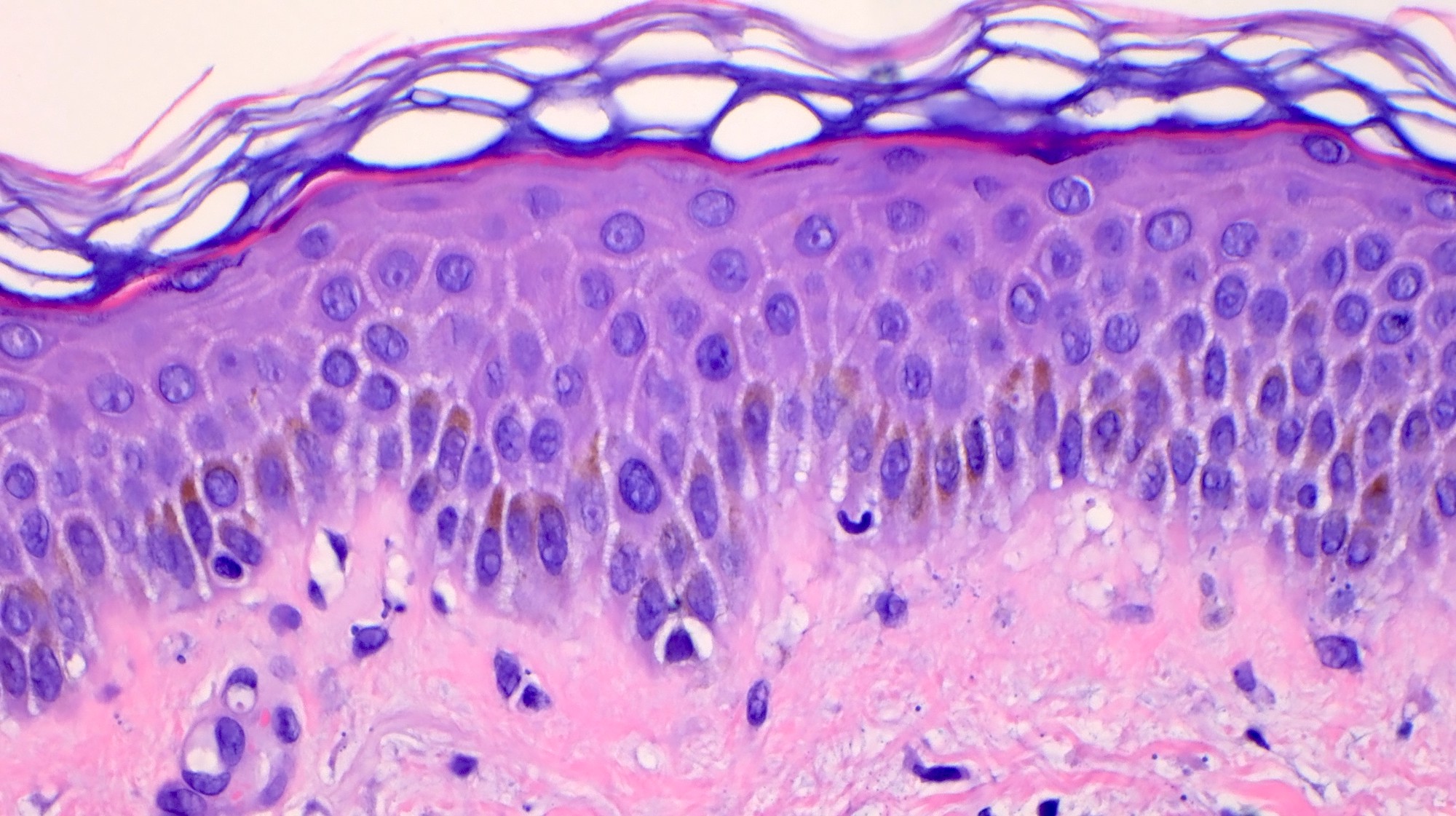
- Chronic eczema
- Significant epidermal acanthosis
- May show a psoriasiform pattern with hyperkeratosis, hypergranulosis and minimal parakeratosis
- Fibrosis of the papillary dermis is another feature of chronicity
- Mild to no spongiosis
- Acute eczema
- References: Adv Anat Pathol 2008;15:76, Clin Lab Med 2017;37:673
Microscopic (histologic) images
Virtual slides
Immunofluorescence description
- Direct and indirect immunofluorescence are negative
Videos
Eczema / atopic contact dermatitis, etc.: spongiotic dermatitis pattern
Spongiotic dermatitis
Sample pathology report
- Skin, left upper back, punch biopsy:
- Subacute spongiotic dermatitis with secondary excoriation (see comment)
- PAS negative for fungal elements (controls adequate)
- Comment: The patient's clinical history and photos were reviewed and multiple levels were examined. Sections show mild to moderate epidermal acanthosis with spongiosis and serum scale crust. There is a superficial perivascular lymphohistiocytic infiltrate with scattered neutrophils and rare eosinophils. Moderate papillary dermal edema is also noted. The histologic differential diagnosis includes atopic dermatitis, allergic / irritant contact dermatitis and id reaction. Clinical correlation is recommended.
Differential diagnosis
- Contact dermatitis (irritant or contact):
- Variable spongiosis
- Langerhans cell microabscesses and eosinophils in the epidermis (eosinophilic spongiosis) may be clues to favor allergic contact dermatitis over other spongiotic processes
- Perivascular infiltrate and exocytosis of neutrophils and lymphocytes
- Vasodilatation and edema in dermis
- Eczematous drug eruption:
- Variable spongiosis
- Eosinophils in dermis
- Marked vascular wall thickening
- Vacuolar interface changes
- Often lymphocytic exocytosis, dyskeratotic keratinocytes, parakeratosis
- Id reaction:
- Variable spongiosis
- Superficial perivascular infiltrate with exocytosis of neutrophils and lymphocytes
- Tinea:
- Scabies:
- Variable spongiosis
- Eosinophilic spongiosis
- Stratum corneum with mite, scybala or eggs
- Reference: Am J Clin Dermatol 2021;22:349
Practice question #1
Practice answer #1
A. Atopic dermatitis. Atopic dermatitis demonstrates variable spongiosis. Acute lesions show retained basket weave orthokeratosis with more marked spongiosis. As lesions become more chronic, they begin to show less spongiosis and more acanthosis. Answer C is incorrect because although guttate psoriasis may show some spongiosis, it is characterized by a mound of parakeratosis with associated neutrophilic abscess (so called open faced jelly sandwich). Guttate psoriasis also shows mild acanthosis, papillary dermal edema, capillary dilatation and a sparse lymphocyte predominant dermal infiltrate. Answer D is incorrect because due to the acute nature of erythema multiforme (EM), it can retain basket weave orthokeratosis in the stratum corneum; however, EM would show other features such as dyskeratotic keratinocytes in all layers of the epidermis with confluent epidermal necrosis and associated basal layer vacuolar interface pattern, rather than a spongiotic reaction pattern. The dermis can show sparse lymphocytic infiltrate. Answer B is incorrect because dermatitis herpetiformis may feature subepidermal blistering with dense neutrophilic infiltrate and associated eosinophils. In early lesions, the presence of dermal papillary neutrophilic microabscesses is a characteristic feature.
Comment Here
Reference: Atopic dermatitis
Comment Here
Reference: Atopic dermatitis
Practice question #2
Which of the following choices is in the histologic differential diagnosis for spongiotic dermatitis?
- Allergic contact dermatitis, id reaction
- Darier disease, Grover disease
- Psoriasis, pityriasis rubra pilaris
- Subacute lupus erythematosus, erythema multiforme
Practice answer #2
A. Allergic contact dermatitis, id reaction. Spongiotic dermatitis can be seen in irritant dermatitis, allergic contact dermatitis, eczematous dermatitis, id reaction and arthropod reaction. Answer D is incorrect because subacute lupus erythematosus and erythema multiforme show a vacuolar interface pattern. Answer C is incorrect because psoriasis and pityriasis rubra pilaris show a psoriasiform pattern. Answer B is incorrect because Darier disease and Grover disease show a pattern of focal acantholytic dyskeratosis.
Comment Here
Reference: Atopic dermatitis
Comment Here
Reference: Atopic dermatitis