Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Rosa G. Allergic contact dermatitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorallergiccontact.html. Accessed October 3rd, 2025.
Definition / general
- T cell mediated, delayed (type IV) hypersensitivity reaction to allergens from skin contact
- Most common occupational skin disease
- Healthcare workers, hairdressers / beauticians, machinists, chemical industry
- Most common allergen: nickel
- Other common allergens: latex, fragrances, cosmetic products, soaps, topical antibiotics, poison ivy
- Reference: Contact Dermatitis 2019;80:77
Essential features
- Spongiotic dermatitis from a skin allergen
ICD coding
- ICD-10: L25.9 - contact dermatitis (occupational) NOS
Epidemiology
- Any age / gender
Sites
- Any
Pathophysiology
- Hapten binding phase (initial step)
- Contact allergen (hapten) penetrates skin barrier
- Hapten is bound to a skin protein carrier
- Sensitization (afferent) phase
- Antigen presenting cells (including Langerhans cells) present the hapten protein complex to priming T cells
- Generates hapten specific memory / effector T cells
- Elicitation (efferent phase) (Allergy 2009;64:1699)
- Repeat exposure to hapten elicits hapten specific memory / effector T cells
- Elicits an inflammatory / cytokine response
- Leads to tissue damage - clinical manifestation of allergic contact dermatitis (ACD), 48 - 72 hours after repeat exposure
- Repeat exposure to hapten elicits hapten specific memory / effector T cells
Etiology
- Common culprits include nickel, poison ivy, dyes / fragrances
Clinical features
- Eczematous scaly lesions
- Severe cases can be vesicular / bullous
- Chronic / repeated exposure can lead to lichenification
- Mostly confined to site of direct contact with allergen
- Transfer of allergen from primary contact site to other areas can occur
- Reference: J Cutan Pathol 2016;43:498
Diagnosis
- Can be established on clinical history and presentation alone
- Histologic features are nonspecific
- Gold standard for definitive diagnosis: patch testing
- Reference: J Clin Aesthet Dermatol 2010;3:36
Case reports
- 11 year old girl with allergic contact dermatitis due to homemade "slime" (Pediatr Dermatol 2019;36:335)
- 28 year old woman with allergic contact dermatitis from a cell phone (Dermatol Online J 2010;16:9)
- 50 year old man with allergic contact dermatitis due to electronic cigarettes (Dermatitis 2018;29:94)
Treatment
- Allergen avoidance and symptomatic treatment
Clinical images
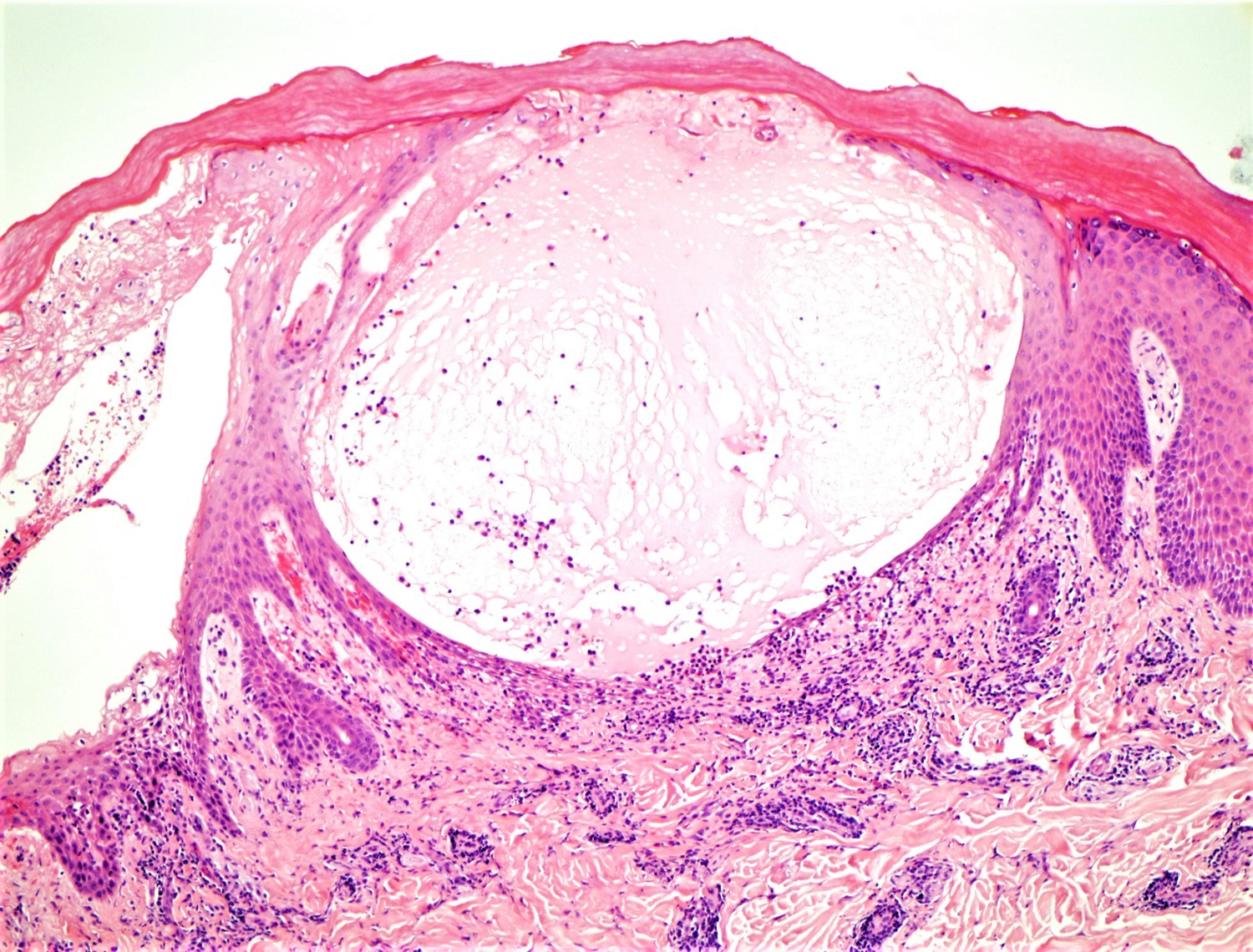
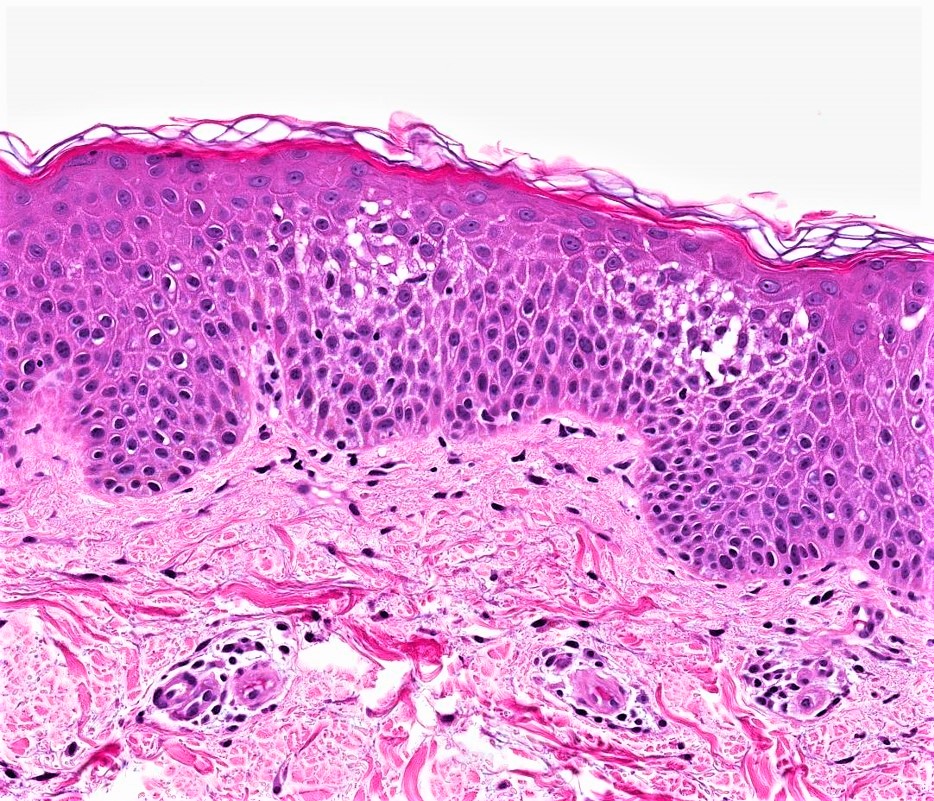
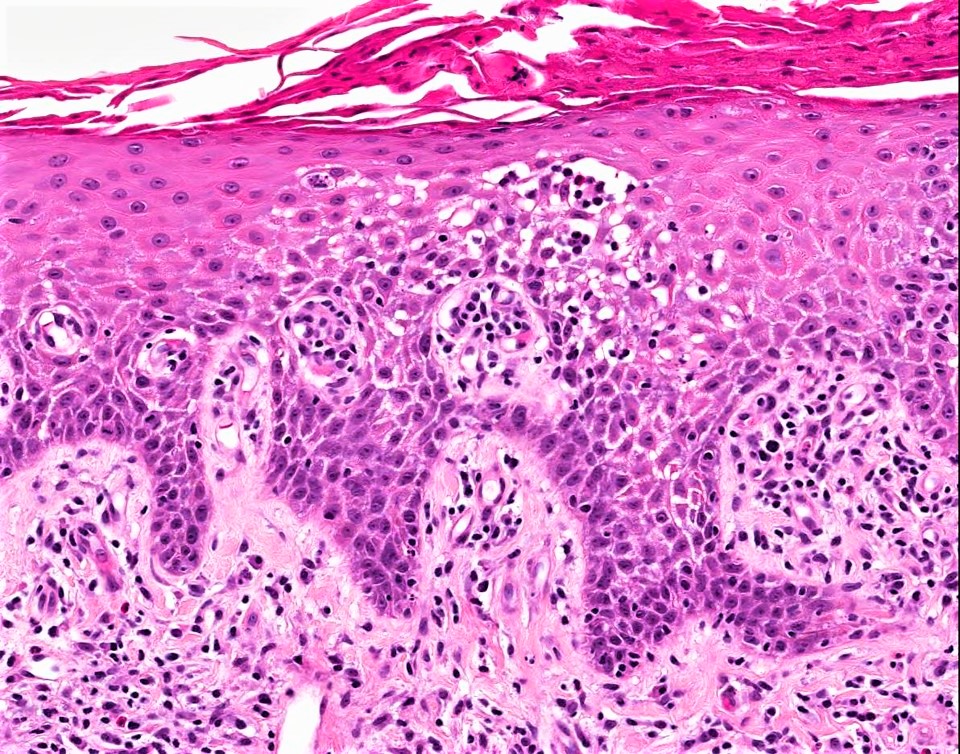
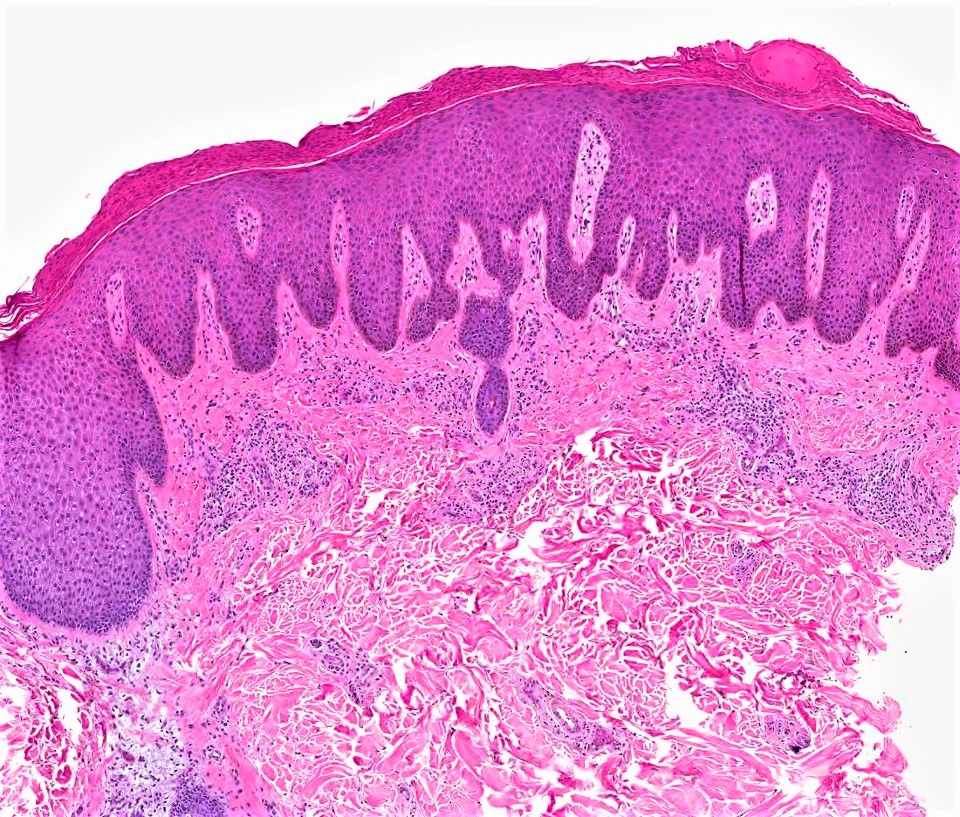
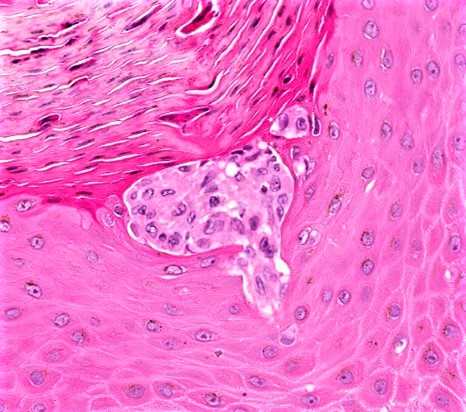
Microscopic (histologic) description
- Spongiotic dermatitis in various stages (acute, subacute and chronic)
- Acute:
- Epidermal edema
- With or without prominent intercellular bridges or vesiculation
- Normal basket weave orthorkeratosis
- Subacute:
- Acanthosis and epidermal edema
- With or without hyperkeratosis or parakeratosis
- Chronic:
- Marked acanthosis
- Hyperkeratosis with or without parakeratosis
- Minimal epidermal edema
- Langerhans cell microabscesses can be associated with ACD but are a nonspecific finding
- Langerhans cells have abundant cytoplasm and horseshoe shaped nuclei
- Reference: J Cutan Pathol 2016;43:498
- Acute:
Microscopic (histologic) images
Immunofluorescence description
- IHC not necessary for diagnosis
Sample pathology report
- Skin, arm, punch biopsy:
- Acute spongiotic dermatitis (see comment)
- Comment: Possibilities could include an eczematous dermatitis, such as allergic contact dermatitis, given the presence of a Langerhans cell microabscess. There is literature regarding Langerhans cell microabscesses in association with allergic contact dermatisis, although this association is nonspecific.
Differential diagnosis
- Atopic dermatitis:
- Spongiotic changes similar to ACD
- Clinical presentation and patch testing will help differentiate from ACD
- Dermatophytosis:
- Spongiotic changes similar to ACD
- Changes to the stratum corneum can be a clue to a dermatophyte infection
- Neutrophils in the stratum corneum
- Sandwich sign - orthokeratosis between parakeratosis and hyphae
- Clinical presentation, potassium hydroxide (KOH) prep or fungal stains (PAS, GMS) will help differentiate from ACD
- Irritant contact dermatitis:
- Dermatitis from direct contact with irritant chemical or substance (nonimmune mechanism)
- Spongiotic changes similar to ACD, with or without keratinocyte necrosis
- With or without neutrophils in the epidermis (neutrophilic spongiosis)
- Mycosis fungoides (MF):
- Early patch stage mycosis fungoides can show spongiotic changes similar to ACD
- To differentiate from ACD (the following favors MF)
- Degree of lymphocyte exocytosis
- Lymphocyte tagging basement membrane
- Pautrier microabscess (lymphocyte collections in epidermis)
- Unusual to have numerous eosinophils
- Unusual to have severe spongiotic changes
- Clinical presentation and disease course will help differentiate from ACD
- T cell receptor gene rearrangement analysis can help differentiate MF from other entities
- Early / urticarial phase of bullous pemphigoid:
- Can show spongiotic changes
- Eosinophils tagging basement membrane with or without eosinophilic spongiosis can be a clue to bullous pemphigoid
- Clinical presentation and direct immunofluorescence will help differentiate from ACD
Practice question #1
What is the gold standard for establishing a diagnosis of allergic contact dermatitis?
- Endoscopy
- Patch testing
- Serum histamine levels
- Skin biopsy
Practice answer #1
B. Patch testing. Commercial patch testing involves applying a set of the most common allergens to the skin and assessing for reactions at 48 and 72- 96 hours respectively (as determined by the North American Contact Dermatitis Group criteria). Skin biopsy could be helpful in establishing the injury pattern of a rash and could raise suspicion for allergic contact dermatitis but a skin biopsy by itself would not be diagnostic. Serum histamine levels and endoscopy play no role in the diagnosis of allergic contact dermatitis.
Comment Here
Reference: Allergic contact dermatitis
Comment Here
Reference: Allergic contact dermatitis
Practice question #2
Practice answer #2
D. Spongiotic dermatitis. The classic histologic features of allergic contact dermatitis are those of a spongiotic dermatitis. In chronic longstanding allergic contact dermatitis, there can also be psoriasiform changes with marked acanthosis and lesser degrees of spongiosis. Sclerosing dermatitis is a dermal process that would be seen in lichen sclerosus, morphea / scleroderma and other sclerosing lesions but not typically in ACD. Interface dermatitis is seen in autoimmune connective tissue disease, drug reactions, erythema multiforme and other interface processes. Irritant contact dermatitis can show a combination of both spongiotic and interface changes. Granulomatous dermatitis is seen in granuloma annulare, granulomatous drug reactions, sarcoidosis and infections, among other entities.
Comment Here
Reference: Allergic contact dermatitis
Comment Here
Reference: Allergic contact dermatitis