Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Duran J, Plaza JA. Morphea and systemic sclerosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorscleroderma.html. Accessed April 28th, 2024.
Definition / general
- Rare autoimmune fibrosing entity subtyped based on clinical presentation (Clin Dermatol 2013;31:432, Annu Rev Pathol 2011;6:509)
Essential features
- Dysregulation of collagen synthesis and degradation (Annu Rev Pathol 2011;6:509)
- Vascular and immune dysfunction causes organ damaging fibrosis
- Divided into subsets (J Eur Acad Dermatol Venereol 2017;31:1401, Clin Dermatol 2013;31:432, Lancet 2017;390:1685)
- Localized scleroderma (morphea: limited / circumscribed, generalized, linear, deep and mixed types)
- Systemic sclerosis:
- Limited cutaneous systemic sclerosis
- Diffuse cutaneous systemic sclerosis
- Systemic sclerosis sine scleroderma
Terminology
- Systemic sclerosis
- Localized scleroderma / morphea
ICD coding
- ICD-10:
- L94.0 - localized scleroderma (morphea)
- M34 - systemic sclerosis (scleroderma)
- M34.0 - progressive systemic sclerosis
- M34.1 - CREST syndrome
- M34.2 - systemic sclerosis induced by drug and chemical
- M34.8 - other forms of systemic sclerosis
- M34.81 - systemic sclerosis with lung involvement
- M34.82 - systemic sclerosis with myopathy
- M34.83 - systemic sclerosis with polyneuropathy
- M34.89 - other systemic sclerosis
- M34.9 - systemic sclerosis, unspecified
- ICD-11:
Epidemiology
- Localized scleroderma
- Incidence 0.4 - 2.7 cases per 100,000 persons (J Rheumatol 1997;24:73, Rheum Dis Clin North Am 2002;28:603)
- F:M = 2.6 - 6:1, except in linear morphea (no sex predominance) (Br J Rheumatol 1988;27:286)
- Systemic sclerosis
- Incidence: 0.3 - 2.8 per 100,000 per year (J Eur Acad Dermatol Venereol 2017;31:1401)
- African Americans > Caucasians (G Ital Dermatol Venereol 2018;153:208)
- F:M = 3:1 (J Eur Acad Dermatol Venereol 2017;31:1401)
- Positive family history increases the relative risk twelvefold (J Eur Acad Dermatol Venereol 2017;31:1401)
- Higher severity has been suggested in African American women (G Ital Dermatol Venereol 2018;153:208)
- Older age and male gender are associated with poor outcomes (Semin Arthritis Rheum 2014;44:208)
- Scleroderma affects children and adolescents (Pediatr Clin North Am 2018;65:757)
- ~33% of cases of localized scleroderma begin in childhood, in contrast with < 10% of systemic sclerosis cases (Pediatr Clin North Am 2018;65:757, J Rheumatol 1997;24:73, J Rheumatol 2006;33:1004, Clin Rheumatol 2007;26:1259)
Sites
- Localized scleroderma
- Skin, subcutaneous tissue, underlying muscle and bone
- When present on the face, head and underlying central nervous system may rarely be involved (J Am Acad Dermatol 2011;64:217)
- Systemic sclerosis
- Skin and internal organs (heterogeneous presentation) (J Eur Acad Dermatol Venereol 2017;31:1401)
- Limited cutaneous systemic sclerosis
- Face and distal to elbows and knees
- Internal organ involvement in later stages
- Diffuse cutaneous systemic sclerosis
- Face, trunk, proximal and distal extremities
- Limited cutaneous systemic sclerosis
- Skin and internal organs (heterogeneous presentation) (J Eur Acad Dermatol Venereol 2017;31:1401)
Pathophysiology
- Not completely understood (Clin Dermatol 2013;31:432)
- Hypothesis: genetic predisposition followed by exogenous stimulus triggering an inflammatory cascade and fibrosis (Clin Dermatol 2013;31:432)
- Pathogenesis involves abnormalities in vascular and immune systems, leading to organ fibrosis (Annu Rev Pathol 2011;6:509)
Etiology
- Postulated etiologic stimuli (J Am Acad Dermatol 2011;64:217):
- Lyme disease
- Trauma
- Radiation (most frequently described)
- Medications (bisoprolol, D-penicillamine, bromocriptine and bleomycin)
- Infections (borrelia has been implied; cytomegalovirus)
- Postulated environmental factors in systemic sclerosis (Clin Dermatol 2013;31:432, Neth J Med 2010;68:348, J Dtsch Dermatol Ges 2012;10:705)
- Occupational and industrial exposures (vinyl chloride, silica dust and organic solvents)
- Chemotherapy drugs (taxanes and gemcitabine) (Lancet 2017;390:1685)
- Virus (parvovirus, cytomegalovirus)
Clinical features
- Localized scleroderma: see Diagrams / tables (J Eur Acad Dermatol Venereol 2017;31:1401)
- Systemic sclerosis
- Skin (J Eur Acad Dermatol Venereol 2017;31:1401)
- Raynaud phenomenon: > 90% of patients
- Typically affects hands, less commonly feet; it may also involve ears, nose and tongue
- Onset: edema of fingers and hands
- Sclerotic changes cause dermatogenic contractures, sclerodactyly, perioral plications, microstomia and mask-like facial stiffness
- With or without hair loss, decreased sweating, hyperpigmentation / hypopigmentation / depigmentation and pruritus
- Digital ulcers
- Calcinosis cutis
- Late stage: diminished skin fibrosis of trunk and proximal extremities
- Raynaud phenomenon: > 90% of patients
- Musculoskeletal (J Eur Acad Dermatol Venereol 2017;31:1401)
- Arthralgia
- Musculoskeletal pain
- Muscle weakness
- Overlap syndromes (myositis and rheumatoid arthritis)
- Pulmonary (J Eur Acad Dermatol Venereol 2017;31:1401)
- Interstitial lung disease (65%)
- Pulmonary arterial hypertension (15%)
- Gastrointestinal manifestations
- Involvement of esophagus (80%), stomach (40 - 70%) and small and large intestine
- Upper gastrointestinal involvement in nearly all patients in longstanding disease
- Cardiovascular (J Eur Acad Dermatol Venereol 2017;31:1401)
- Myocardial fibrosis, manifestations depend on severity and extension
- Renal (J Eur Acad Dermatol Venereol 2017;31:1401)
- Slowly progressive obliterative vasculopathy
- Scleroderma renal crisis (malignant hypertension and oligo / anuric acute renal failure) - rare but severe
- Skin (J Eur Acad Dermatol Venereol 2017;31:1401)
Diagnosis
- Localized scleroderma
- Routine systemic workup is not recommended
- Clinical presentation
- Physical examination
- Localized scleroderma cutaneous assessment tool (LoSCAT) (Rheumatology (Oxford) 2010;49:373)
- Histopathology - not possible to differentiate between localized scleroderma and systemic sclerosis nor to differentiate among different localized scleroderma subtypes
- Biopsy should be sufficiently deep
- Only if the clinical presentation is inconclusive
- Laboratory
- Blood differential and chemistry
- Creatine kinase (suspected myositis)
- Autoantibodies may be present but their routine screening is not recommended
- Imaging
- Brain MRI and head CT (i.e. en coup de sabre or progressive facial hemiatrophy):
- Detect muscle, joint or bone involvement
- Detect potential subcortical calcifications or brain atrophy
- Surgical planning
- Brain MRI and head CT (i.e. en coup de sabre or progressive facial hemiatrophy):
- Systemic sclerosis
- Clinical presentation
- Physical examination
- Capillaroscopy
- Modified Rodnan skin score (mRSS)
- Histopathology - not possible to differentiate between localized scleroderma and systemic sclerosis nor to differentiate among different localized scleroderma subtypes
- Biopsy should be sufficiently deep
- Laboratory
- Blood differential and chemistry
- Creatine kinase (suspected myositis)
- Blood differential and chemistry
- Autoantibodies
- Antinuclear antibody (ANA) (95%)
- Systemic sclerosis associated antibodies (Lancet 2017;390:1685, J Eur Acad Dermatol Venereol 2017;31:1401)
- Centromere
- Topoisomerase 1
- RNA polymerase III
- Exosomal ribonucleoprotein (PM / Scl)
- Uridine rich small nuclear ribonucleoprotein (U1-snRNP)
- Systemic sclerosis overlap syndromes (features of other connective tissue disorders combined with systemic sclerosis)
- Anti Ro / La, anti centromere - Sjögren overlap syndrome
- Cyclic citrullinated peptide (CCP) - rheumatoid arthritis overlap syndrome
- Rheumatoid factor (Fc portion of IgG) - rheumatoid arthritis overlap syndrome
- Mitochondrial Ag M2 - primary biliary cirrhosis
- Organ oriented diagnostic workup
- Laboratory
- Imaging
- Clinical presentation
Radiology images
Prognostic factors
- Localized scleroderma
- 25% of patients experience reactivation of disease after resolution (Br J Dermatol 2015;172:722)
- Factors associated with reactivation:
- Early age of onset of disease (Br J Dermatol 2015;172:722)
- Subtype of localized scleroderma
- Skin and soft tissue atrophy, contractures (may affect functionality)
- Factors associated with reactivation:
- 25% of patients experience reactivation of disease after resolution (Br J Dermatol 2015;172:722)
- Systemic sclerosis
- Chronic and unpredictable course
- Factors related to poor outcome (Semin Arthritis Rheum 2014;44:208):
- Male gender
- Older age
- Lung, kidney and heart involvement
- Skin extension
- High erythrocyte sedimentation rate
- Quality of life and psychosocial well being are often affected
- Multidisciplinary care is required due to involvement of several organs
- Leading cause of mortality in last 2 decades is cardiopulmonary involvement (73% of all systemic sclerosis related deaths) (Semin Arthritis Rheum 2014;44:208)
Case reports
- 22 year old woman, gravida 1 para 0, at 7 months gestation complaining of skin thickening on the breasts (Dermatol Online J 2017;23:13030)
- 28 year old woman with myasthenia gravis who developed linear scleroderma 7 years after diagnosis (J Dermatol 2000;27:31)
- 44 year old woman status post lumpectomy and chemoradiation with skin erythema, sclerosis and contracture of her right breast 15 months after completion of treatment (Histopathology 2018;72:342)
Treatment
- Localized scleroderma
- Topical therapy
- Corticosteroids
- Calcipotriol
- Tacrolimus
- Systemic therapy
- Systemic corticosteroids
- Methotrexate
- Mycophenolate mofetil
- Others systemic medications
- Phototherapy
- Physical therapy
- Surgical interventions
- Topical therapy
- Systemic sclerosis
- Organ based approach (determine organ involvement and disease activity)
- Reference: J Eur Acad Dermatol Venereol 2017;31:1401
Clinical images
Microscopic (histologic) description
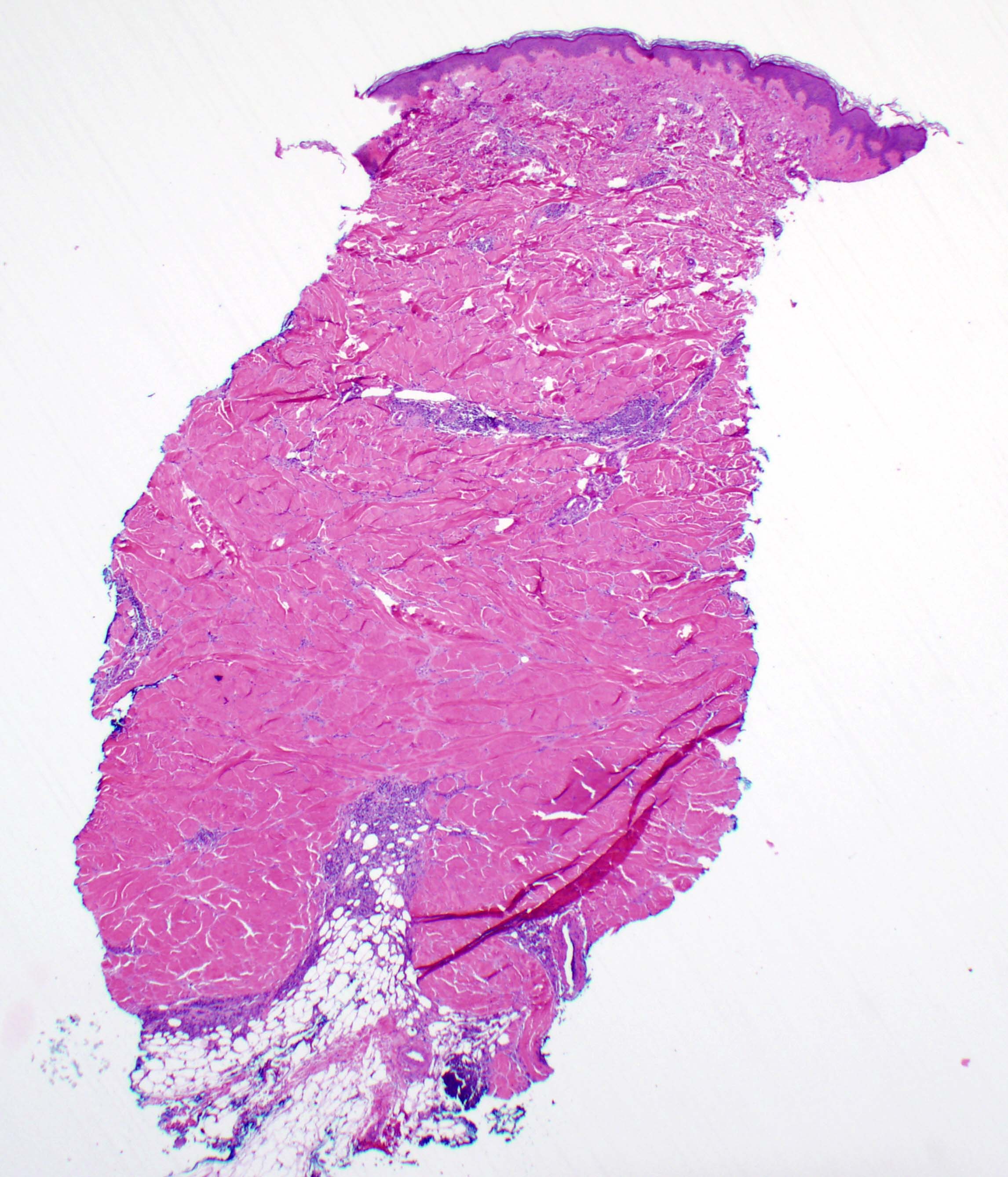
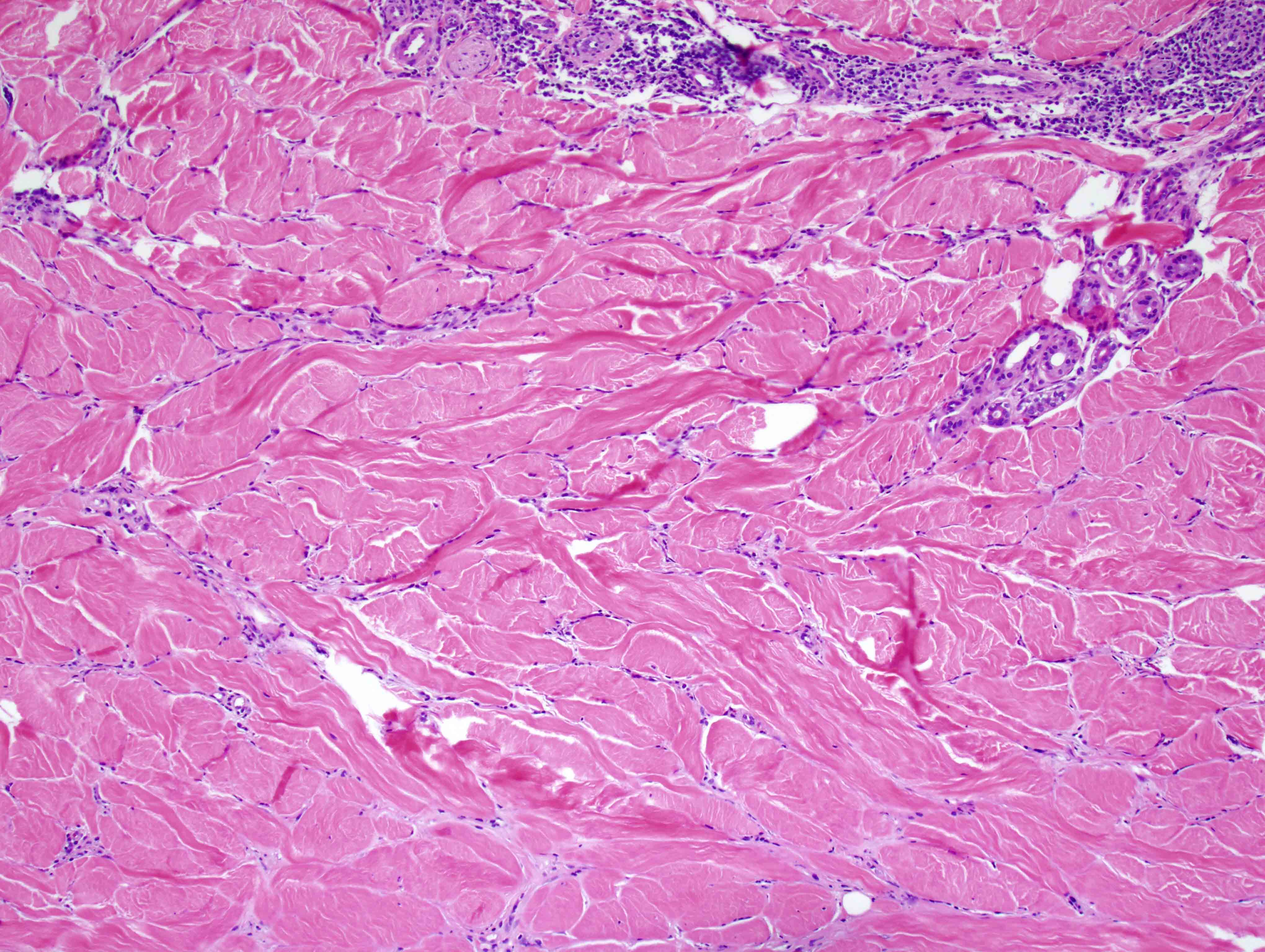
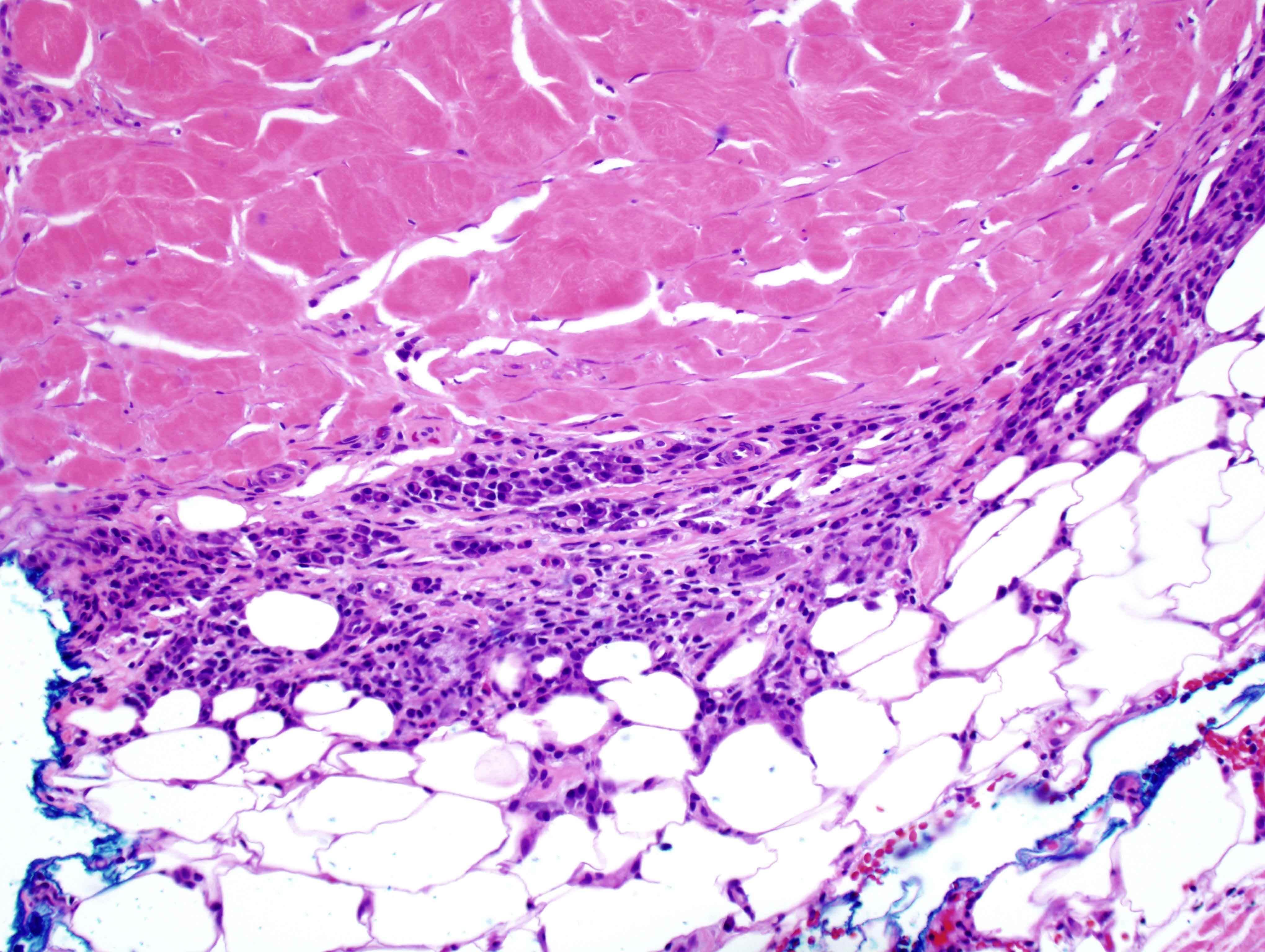
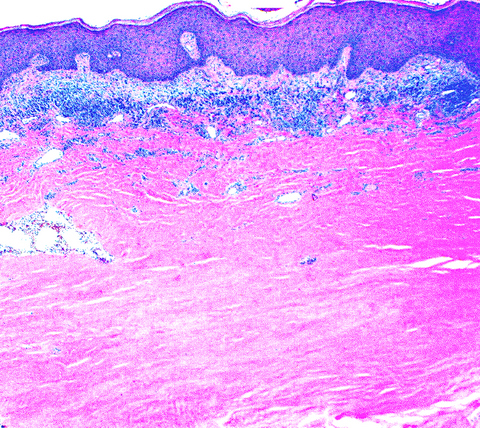
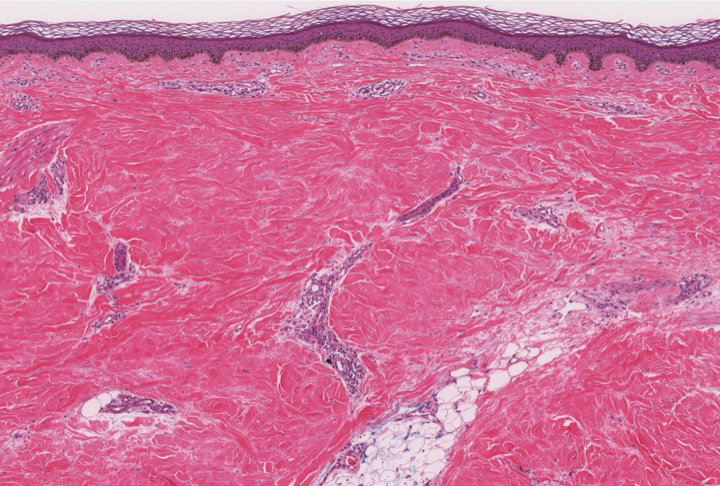
- Localized scleroderma and systemic sclerosis have mostly indistinct histologic features (J Eur Acad Dermatol Venereol 2017;31:1401)
- Some authors have suggested histopathological differences (Am J Dermatopathol 1998;20:242):
- Density and distribution of inflammatory infiltrate (systemic sclerosis may be less inflammatory on biopsy)
- Thickness of collagenized tissue, found to be mostly lower reticular dermis and subcutis in systemic sclerosis compared to involvement of all levels of dermis in localized scleroderma
- Some authors have suggested histopathological differences (Am J Dermatopathol 1998;20:242):
- Biopsy is performed when clinical features are inconclusive
- Spectrum of changes over time leading to thickened, collagenized dermis
- Preservation of elastic fibers by elastic van Gieson stain with variable changes:
- Areas with thickened collagen show wider, compressed and parallel straightened fibers (rather than the wavy, branching distribution of normal skin) (J Cutan Pathol 2009;36:952)
- Preservation of elastic fibers by elastic van Gieson stain with variable changes:
- Punch biopsy shows rigid, squared silhouette at low power
- Early disease (J Eur Acad Dermatol Venereol 2017;31:1401)
- Thickened collagen bundles within papillary and reticular dermis
- Dense perivascular and periadnexal inflammatory infiltrate, as well as between collagen bundles and at the limit of the dermis and subcutis
- Inflammatory infiltrate: predominantly lymphocytes; plasma cells, histiocytes and eosinophils are also seen
- Overlying epidermis may be unaffected or atrophic
- Blood vessel wall edema may be seen
- Late / fibrotic stage (J Eur Acad Dermatol Venereol 2017;31:1401)
- Relatively avascular skin
- Adnexal structures are atrophic or absent
- Entrapped atrophic adnexal structures may show loss of surrounding adipose tissue
- Minimal inflammation
- Highly packed, eosinophilic collagen bundles
- Blood vessel wall sclerosis
- Can affect subcutaneous fat
- Morphea profunda, morphea of childhood, generalized morphea, linear morphea
- Panniculitis is predominantly septal, resulting in widening and thickening
- Some subtypes are restricted to the superficial dermis
- Superficial morphea
- Rare variants
- Bullous morphea:
- Bullae arise on indurated plaques (subepidermal)
- Marked papillary dermal edema
- Ectatic lymphatic vessels
- Keloidal / nodular morphea:
- Keloidal lesions in association with morphea plaques
- Guttate morphea:
- Localized and superficial
- Usually associated with larger plaques
- Bullous morphea:
Microscopic (histologic) images
Sample pathology report
- Skin, trunk, biopsy:
- Scleroderma (see comment)
- Comment: Sections show a punch biopsy with squared silhouette and thickened dermal collagen. Adnexal structures are atrophic and entrapped within the collagenous stroma. There is dense perivascular and periadnexal lymphoplasmacytic infiltrate, as well as between collagen bundles and at the dermal subcutis junction. Altogether, these findings are consistent with scleroderma. Clinical correlation is advised for subclassification.
Differential diagnosis
- Scleredema:
- Hypertrophied collagen bundles with intervening mucin
- No inflammatory infiltrate
- Edematous lesions may be difficult to distinguish
- Chronic radiation dermatitis:
- Variable epidermal atrophy, acanthosis, hyperkeratosis
- Radiation induced changes (atypia, elastosis and superficial capillary ectasia)
- Loss of adnexal structures
- Lichen sclerosus et atrophicus:
- Sclerosis limited to papillary dermis
- Vacuolar change in basal cells
- Edema of superficial dermis
- Band-like or lichenoid inflammatory cell infiltrate in active lesions
- Keloid:
- Raised lesion
- Dense and thickened dermal collagen bundles
- Markedly eosinophilic, hyalinized (bubble gum) collagen bundles
- Decreased dermal vascularity, with occasional ectatic vessels
- Keloidal / nodular morphea shows associated morphea plaques
- Hypertrophic scar:
- Raised lesion
- Dense and thickened dermal collagen bundles
- Lacks hyalinized collagen bundles
- Perpendicularly oriented vessels
- Active lesions show a cellular appearing dermis with numerous myofibroblasts arranged in fascicles and nodules
- Scleromyxedema:
- Mucin deposition in upper and mid dermis
- Increased disorganized fibroblastic proliferation and collagen deposition
- Nephrogenic systemic fibrosis:
- Clinical history remarkable for renal insufficiency and gadolinium exposure
- Disorganized collagen bundles in deep dermis and adipose septae
- Spindle cells in between collagen bundles
- Increased mucin deposition
- Osseous sclerotic bodies and multinucleated giant cells may be seen
Board review style question #1
Board review style answer #1
C. Histological features are mostly indistinct. Localized scleroderma and systemic sclerosis have indistinct histologic findings and require clinical correlation for their classification and subclassification.
Comment Here
Reference: Scleroderma
Comment Here
Reference: Scleroderma
Board review style question #2
Which of the following histopathological findings are most consistent with a diagnosis of morphea?
- Edema and hypertrophied collagen bundles with intervening mucin
- Sclerosis limited to papillary dermis, vacuolar change in basal cells and edema of superficial dermis
- Thick and dense collagenized dermis, entrapped atrophic adnexal structures with loss of surrounding adipose tissue
- Variable epidermal atrophy, acanthosis, atypia and loss of adnexal structures
Board review style answer #2
C. Thick and dense collagenized dermis, entrapped atrophic adnexal structures with loss of surrounding adipose tissue. Some of the most characteristic findings in localized scleroderma and systemic sclerosis include a spectrum of changes over time leading to a thickened, collagenized dermis. The early phases of disease may present with perivascular and periadnexal inflammatory infiltrate as well as between collagen bundles and at the limit of the dermis and subcutis. The late / fibrotic stages are usually less inflammatory. The adnexal structures are atrophic or absent and may show loss of surrounding adipose tissue.
Comment Here
Reference: Scleroderma
Comment Here
Reference: Scleroderma