Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3Cite this page: Fernández-Figueras MT, Pérez Muñoz N. Actinic keratosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticactinickeratosis.html. Accessed October 5th, 2025.
Definition / general
- Intraepidermal keratinocytic lesion secondary to solar damage
- Most common precursor of cutaneous squamous cell carcinoma (SCC)
Essential features
- Most common precursor of cutaneous squamous cell carcinoma
- Secondary to solar damage
- Epidermal dysplasia that is not full thickness
- Parakeratosis, dermal solar elastosis and mild dermal lymphocytic infiltrate
Terminology
- Solar keratosis, senile keratosis, keratinocytic intraepithelial neoplasia
ICD coding
Epidemiology
- Advancing age, usually > 40 years old
- Pale skin (Curr Probl Dermatol 2015;46:1)
- Sun exposure (Curr Probl Dermatol 2015;46:1)
- Prolonged immunosuppression (Curr Probl Dermatol 2015;46:1)
- M > F (Curr Probl Dermatol 2015;46:1)
Sites
- Sun exposed sites: face, scalp, upper chest and distal arm (Curr Probl Dermatol 2015;46:1)
Pathophysiology
- Cumulative solar damage causes a high mutation burden in the germinative (basal) layer of keratinocytes
Etiology
- Chronic sun damage (ultraviolet UVB radiation and UVA to a lesser extent)
- Chronic immunosuppression
- Arsenic exposure
- PUVA therapy
- Chronic cutaneous inflammation
- βHPV (Viruses 2017;9:187)
- High prevalence rates and viral loads in actinic keratoses
- Virus, when combined with UV exposure, may play a role in progression to SCC
Diagrams / tables
Clinical features
- Single or multiple erythematous and hyperkeratotic macules or papules
- Usually < 1 cm in diameter
- Sometimes pigmented or ulcerated
- Chronic sun damage of background skin
- Reference: J Drugs Dermatol 2010;9:1125
Diagnosis
- Usually by clinical examination
- Dermoscopy shows erythematous to brown networks, irregular hyperpigmented follicular openings, grey dots and lineal or circular structures; surface scales are common (Curr Probl Dermatol 2015;46:70)
- In vivo reflectance confocal microscopy shows a disarranged or mildly atypical honeycomb pattern (Eur J Dermatol 2016;26:549)
Prognostic factors
- Can remain stable for long periods or regress
- Rate of transformation to SCC: closer to 1/100 (from 1/10 to 1/1000 in different studies)
- Proliferative variant has higher risk of invasion
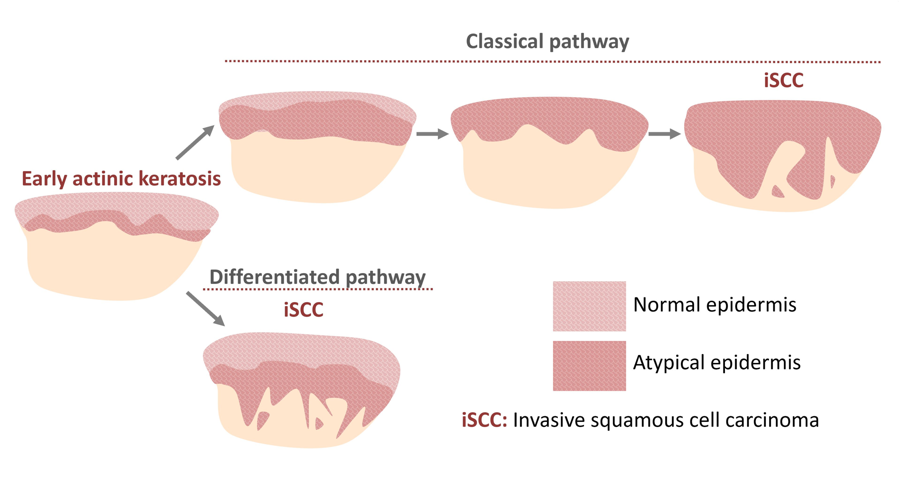
- 2 main pathways for progression to SCC (J Eur Acad Dermatol Venereol 2018;32:581):
- Classical: atypical basal keratinocytes in an actinic keratosis invade the mid to upper epidermis and transform to invasive SCC
- Differentiated: invasive SCC develops directly from actinic keratosis with dysplasia limited to the basal layer
Case reports
- 54 year old man with a dark lesion on his nasal tip; biopsy revealed pigmented actinic keratosis (Cureus 2019;11:e4721)
- 68 year old woman with non small cell lung adenocarcinoma with eruptive inflamed actinic keratosis consequent to systemic chemotherapy (Dermatol Online J 2017;23:13030/qt77s2r0p9)
- 72 year old woman developed an acute inflammation of her actinic keratosis while on oral capecitabine chemotherapy for rectal adenocarcinoma (J Cutan Med Surg 2012;16:298)
- 77 year old woman with seborrheic keratosis that transformed into bowenoid actinic keratosis (Case Rep Dermatol 2020;12:19)
Treatment
- Excision
- Cryosurgery
- Topical drugs: 5-fluorouracil, ingenol mebutate, diclofenac or imiquimod
- 5-fluorouracil is the most effective and most cost effective treatment
- Photodynamic therapy
- Above methods often combined
- References: J Eur Acad Dermatol Venereol 2017;31:13, Australas J Dermatol 2020 Aug 25 [Epub ahead of print]
Clinical images
Gross description
Gross images
- See Clinical images
Frozen section description
- Frozen section not performed as lesion is precancerous
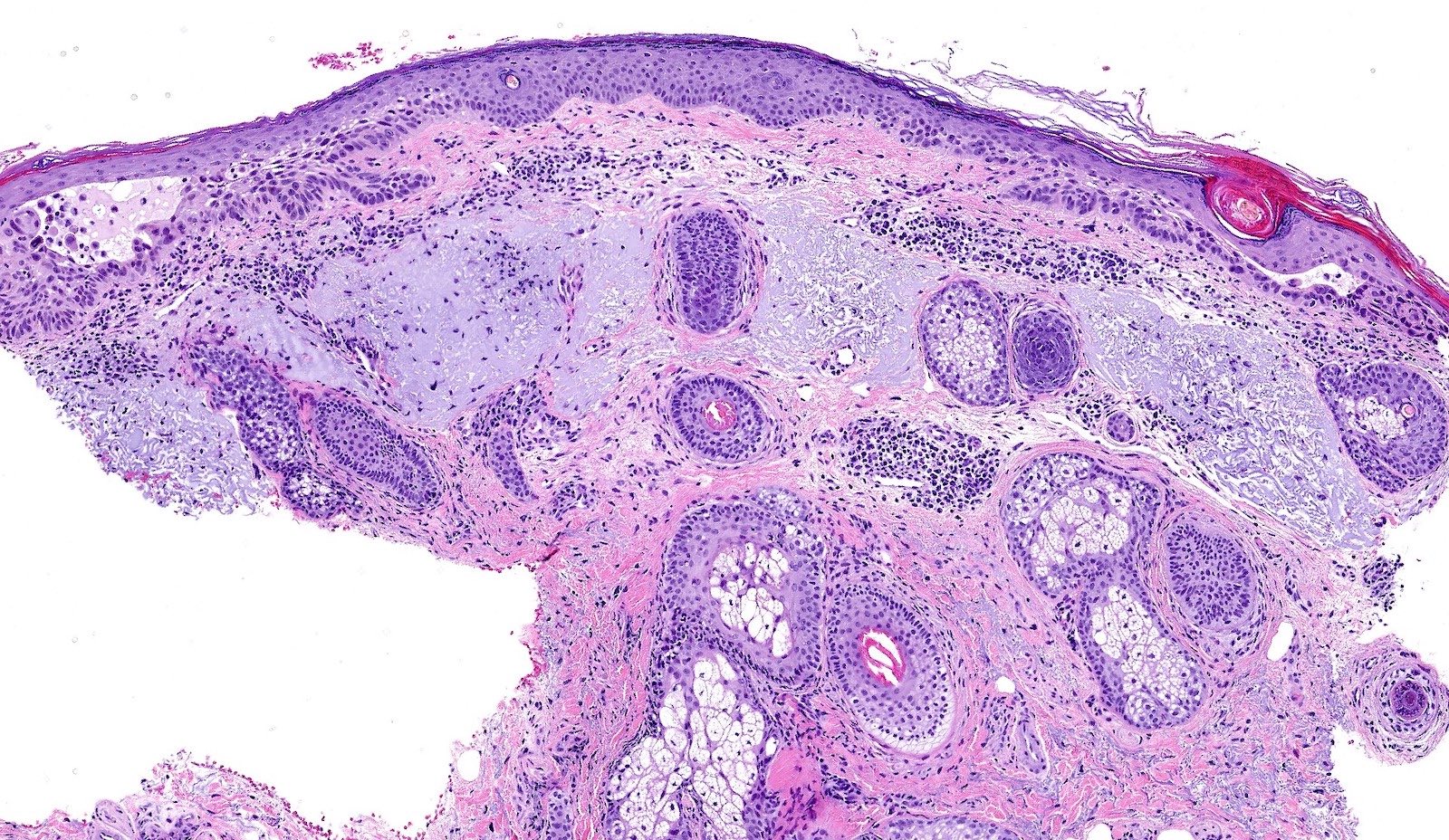
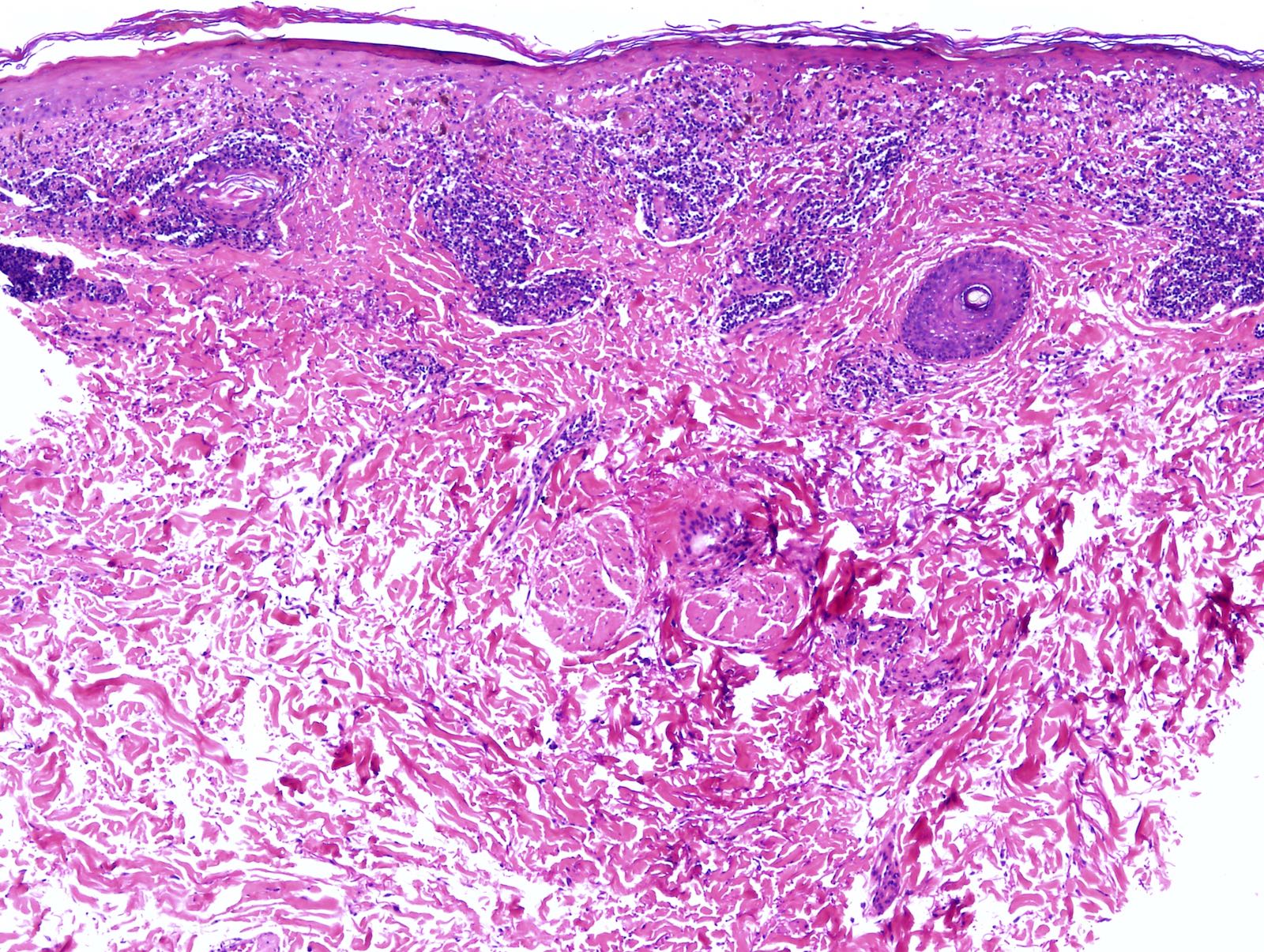
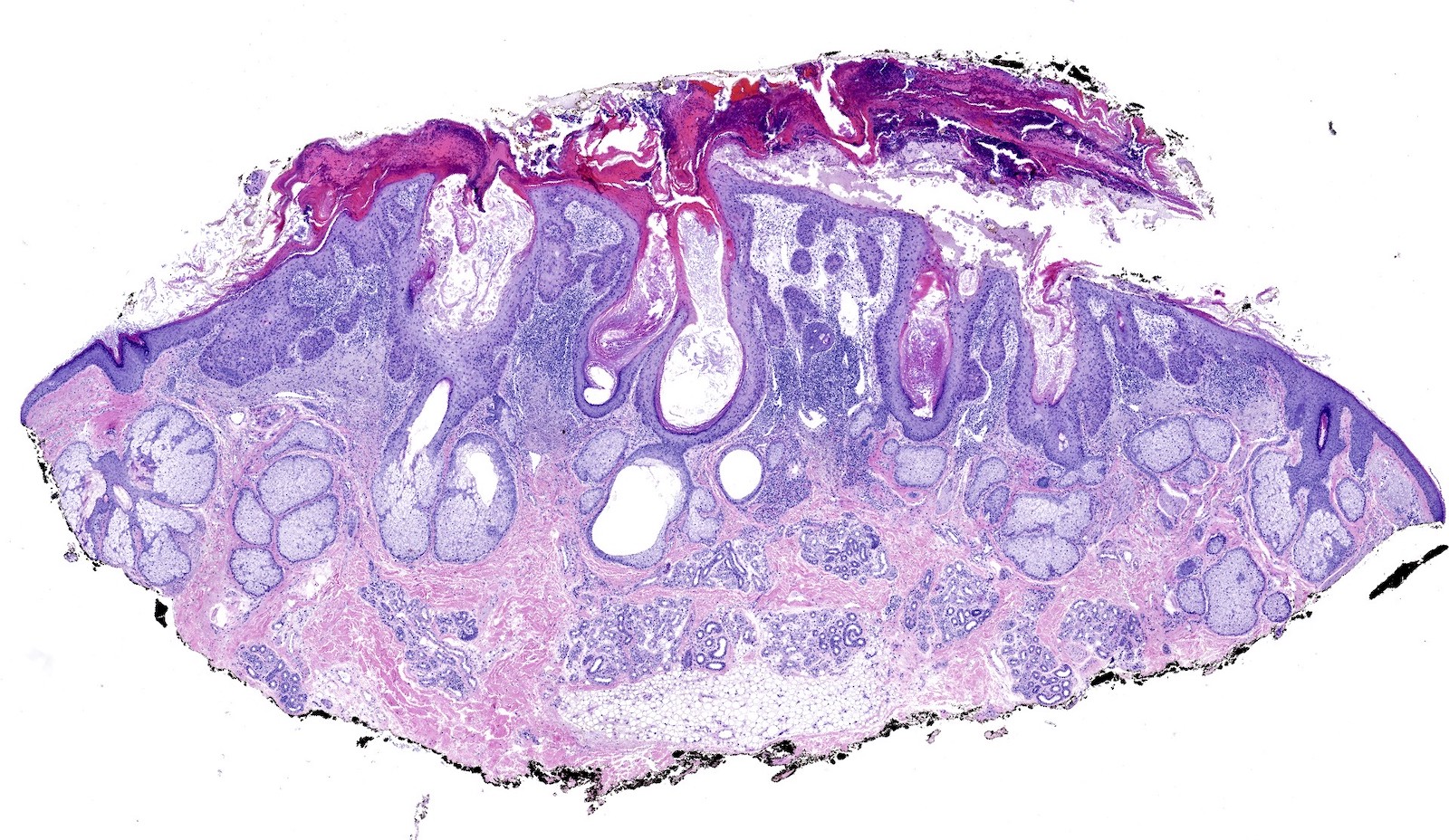
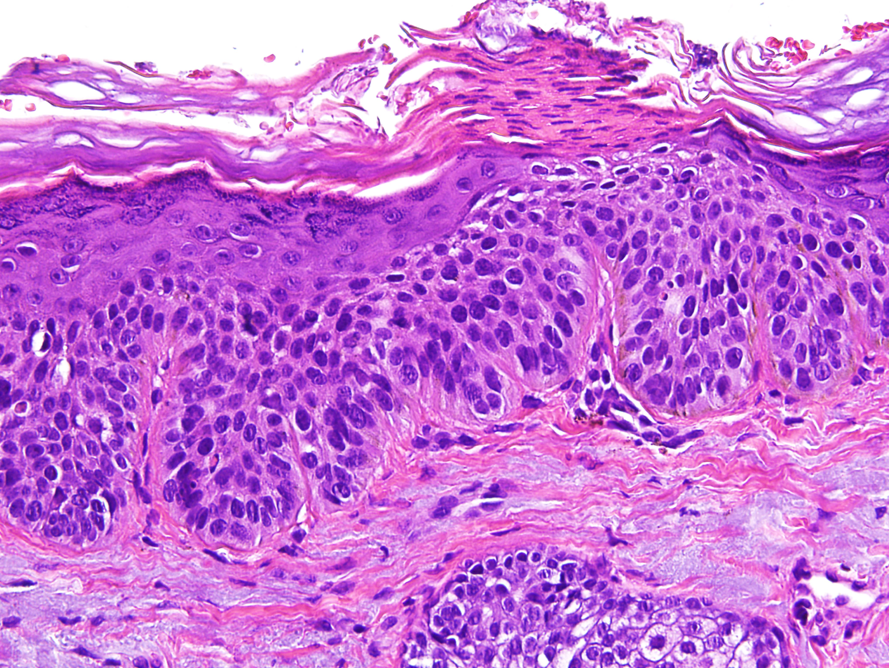
Microscopic (histologic) description
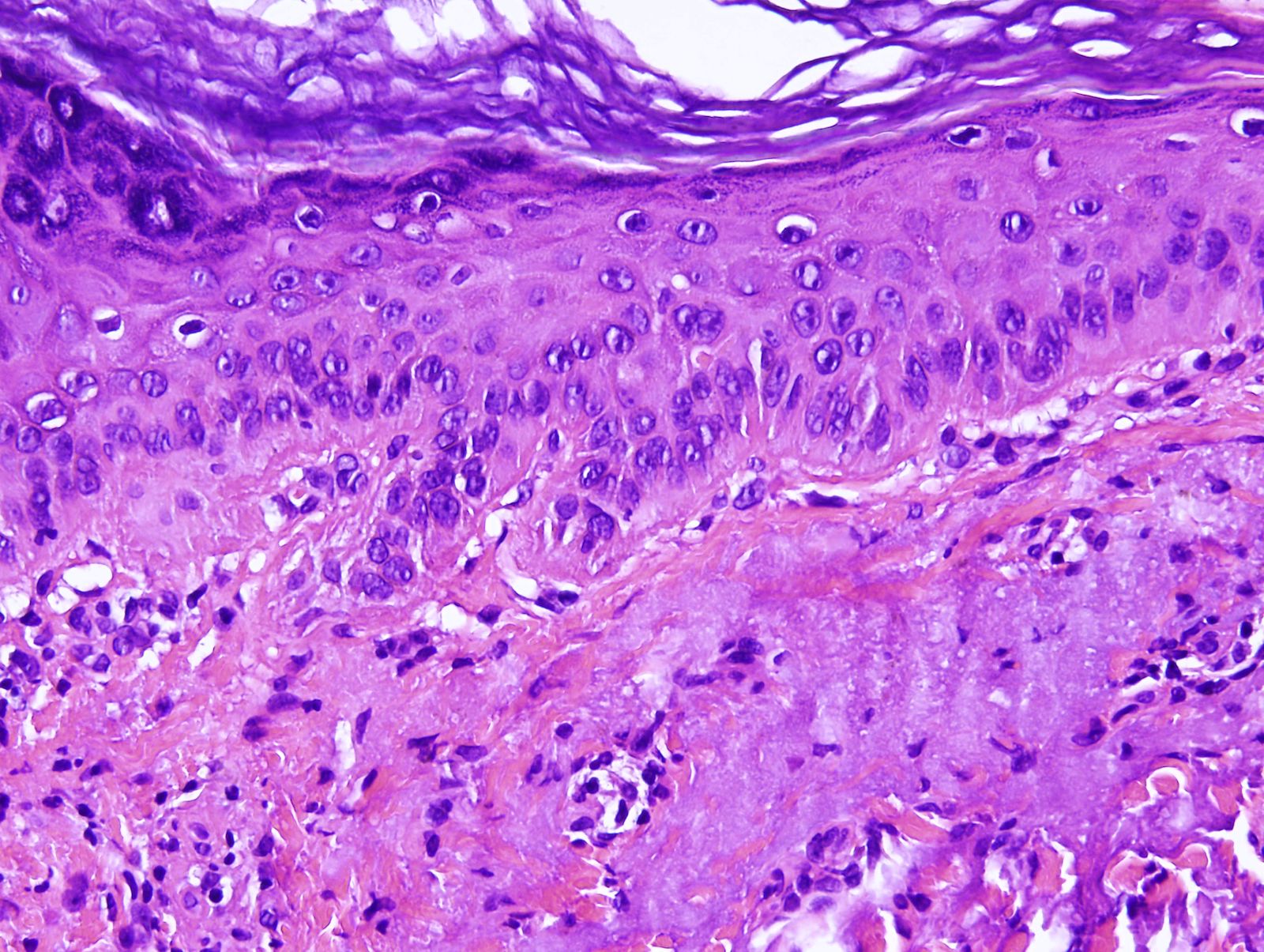
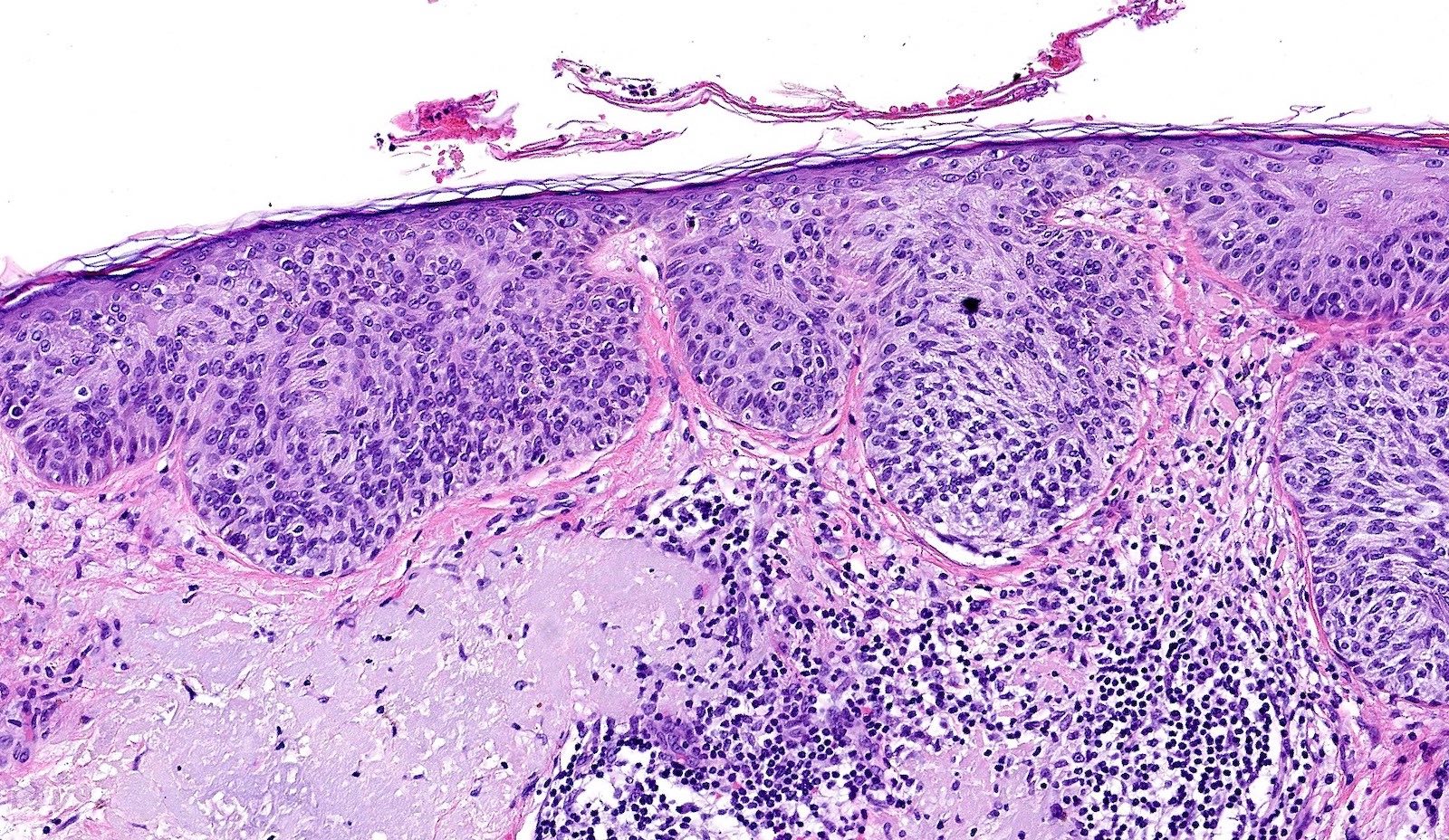
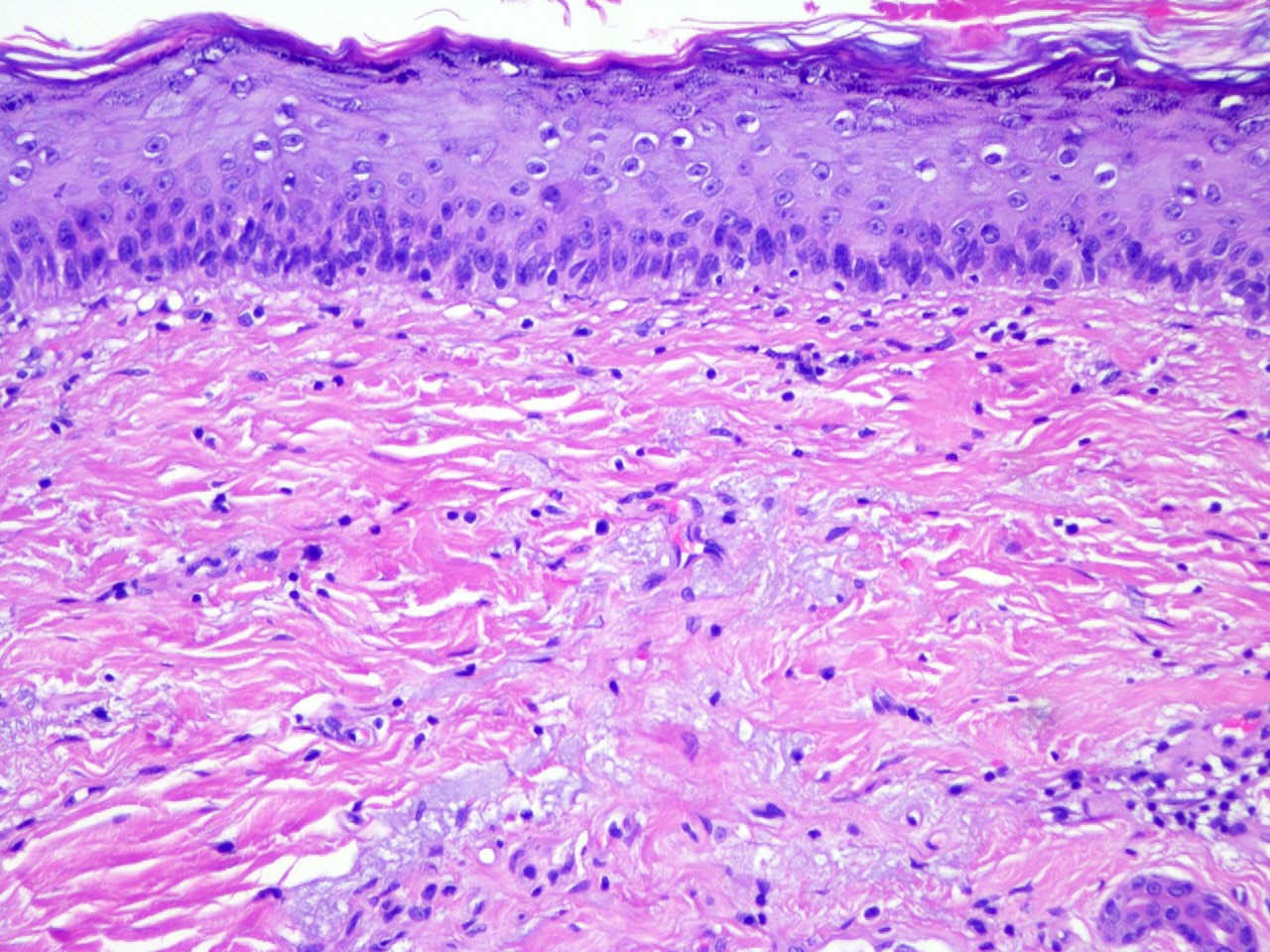
- Atypia of basal keratinocytes with loss of polarization, crowding and overlapping
- Can progress to involve the mid to upper epidermal layers
- Can extend along adnexal structures; typically limited to infundibular extension
- Never full thickness
- Typically, mild acanthosis with occasional downward buds; tangential sectioning of these buds can prompt overdiagnosis of superficially invasive SCC but these do not represent actual squamous pearls
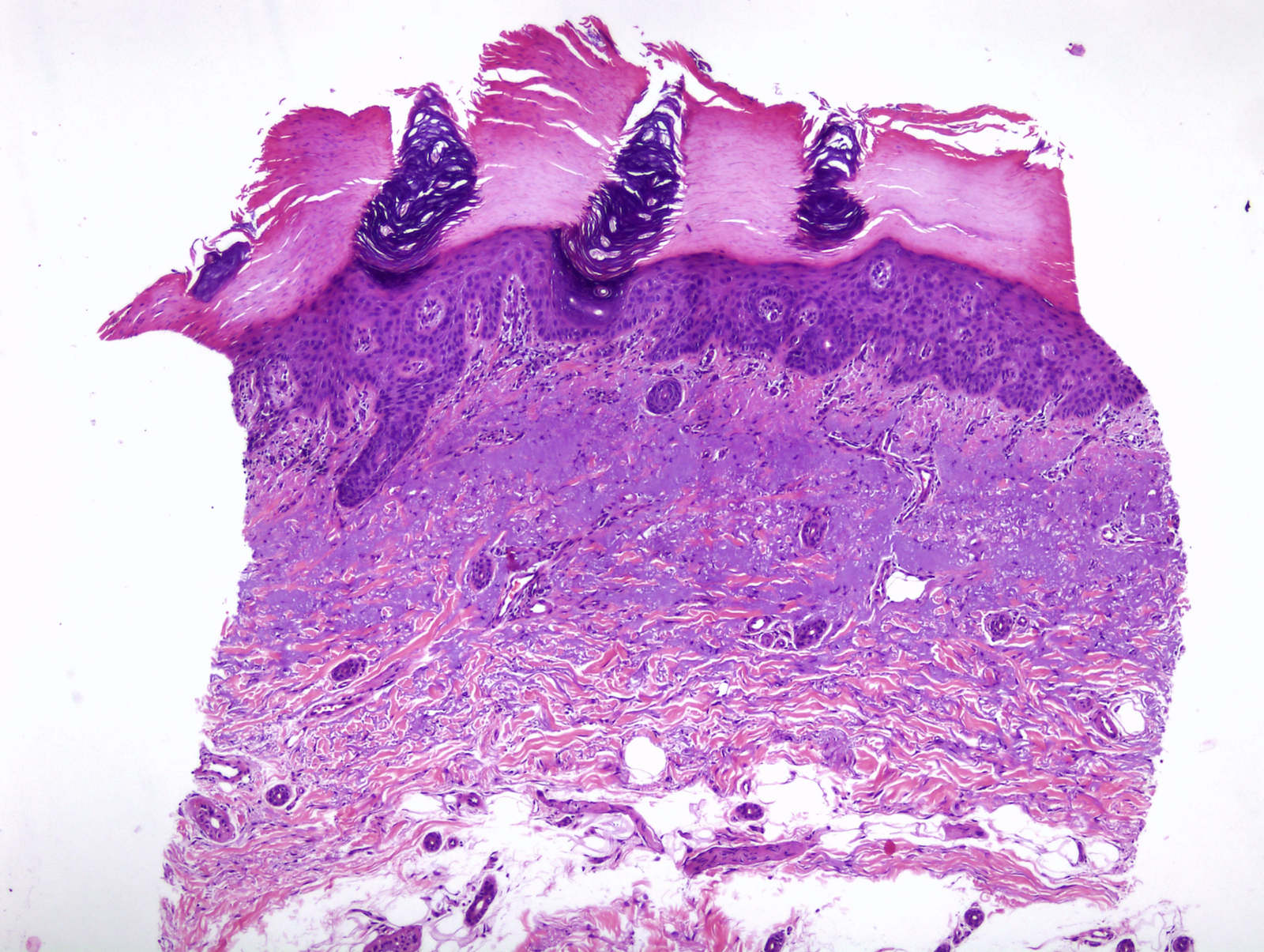
- Focal parakeratosis
- Flag sign: occasional columns of grey loose keratin above preserved acrosyringiums (known as Freudenthal funnels) alternate vertically with eosinophilic compact hyperkeratosis
- Lost / attenuated granular layer
- Dermal changes: solar elastosis, mild inflammatory infiltrate (usually lymphocytes; plasma cells present in longstanding lesions)
- Variants:
- Hypertrophic / hyperplastic: prominent irregular acanthosis, parakeratosis and orthokeratosis
- Atrophic: thin epidermis
- Lichenoid: band-like lymphocytic infiltrate of papillary dermis, basal keratinocytes with scattered apoptosis and vacuolar change
- Acantholytic: suprabasal clefting between atypical keratinocytes
- Pigmented: increased melanin in the basal keratinocytes and melanocytes; melanophages in the papillary dermis
- Proliferative: dermal projections of nested atypical keratinocytes; dense dermal inflammation
- Bowenoid: near full thickness atypia, usually focal
- Pagetoid: pale cells
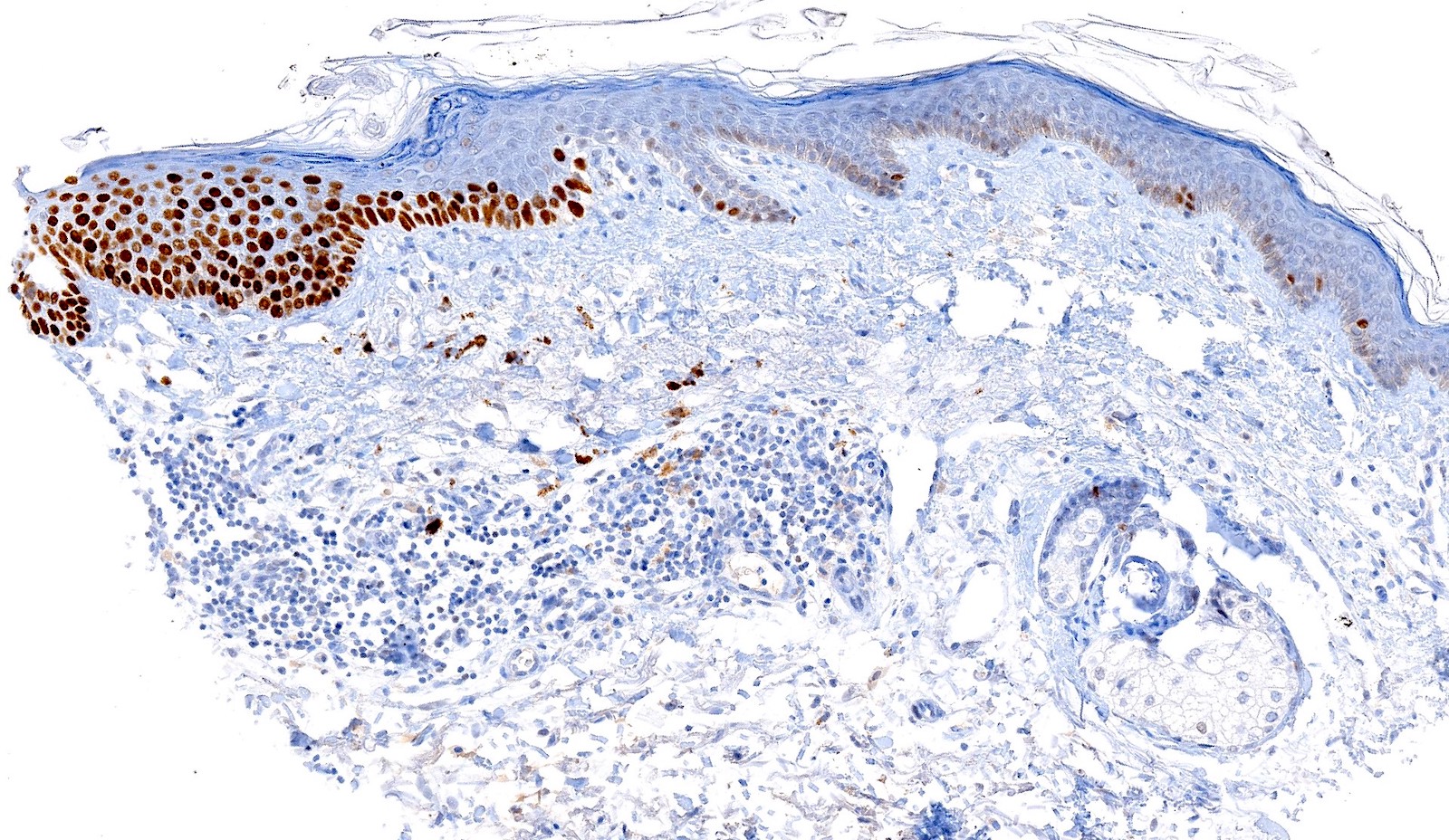
Microscopic (histologic) images
Contributed by María-Teresa Fernández-Figueras, Ph.D.
Positive stains
- p53 (50%)
- Cyclin D1 (50%)
- Increased Ki67 expression
- MelanA can be positive in pigmented lesions (Am J Dermatopathol 2009;31:305)
Molecular / cytogenetics description
- Main driver mutations present in cutaneous invasive squamous cell carcinoma such as TP53, NOTCH1 and NOTCH2 are already present in actinic keratosis
- MAPK pathway seems to play a leading role in invasion
- References: Nat Commun 2018;9:3667, Clin Cancer Res 2019;25:2379, Br J Cancer 2014;110:520
Videos
Tutorial on actinic keratosis histopathology
Sample pathology report
- Skin, forehead, curettage:
- Fragments of hypertrophic actinic keratosis (see comment)
- Comment: Due to fragmentation, small areas of in situ or invasive squamous cell carcinoma cannot be ruled out.
Differential diagnosis
- Actinic cheilitis:
- Similar histologically but in case of invasion the risk of metastasis is 11% (StatPearls: Actinic Cheilitis [Accessed 22 March 2021])
- Squamous cell carcinoma:
- In situ: full thickness epidermal dysplasia
- Invasive:
- Isolated dermal squamous cells or pearls
- Dermal desmoplasia
- Pseudomaturation with large keratinized cells close to the dermal collagen
- Finger-like projections of proliferative actinic keratosis are challenging to differentiate from invasion, especially when tangentially sectioned
- Bowen disease (classical):
- Involves non sun exposed areas
- Full thickness atypia of keratinocytes
- Sharply delineated
- Gives rise to nonactinic related invasive tumors with higher metastatic risk (J Eur Acad Dermatol Venereol 2019;33:11, J Cutan Pathol 2006;33:261)
- Benign lichenoid keratosis:
- Also known as lichen planus-like keratosis: resembles a lichen planus and often shows hypergranulosis (Dermatol Reports 2011;3:e25)
- Sharply demarcated
- Mild reactive keratinocyte atypia
- Dysmaturatative drug eruptions:
- In patients receiving chemotherapeutic drugs (J Eur Acad Dermatol Venereol 2016;30:638)
- Atypical starburst-like or ring-like mitoses are common
- Dyskeratosis of basal and suprabasal layers of the epidermis
- Occasional squamous syringometaplasia
- Grover disease (transient acantholytic dermatosis):
- Lesions show dismaturation and lentiginous silhouette (Am J Dermatopathol 2010;32:541)
- Areas of acantholysis or dyskeratosis can be present in actinic keratosis but the phenomenon of acantholytic dyskeratosis favors the diagnosis of Grover disease
Practice question #1
Which of the following is true about the entity shown in the photo above?
- Clinically ranges from small papules to pustulous plaques or erythroderma
- It is frequently located in the genital area
- It is the most common precursor of cutaneous invasive squamous cell carcinoma
- Nodular growth pattern is considered a low risk variant
- p16 is positive in high risk cases
Practice answer #1
C. The image depicts actinic keratosis, which is the most common precursor of cutaneous invasive squamous cell carcinoma. Answer C is an essential feature of actinic keratosis as it has well established its link in the development of squamous cell carcinoma either in the classical or differentiated pathways. Erythroderma is not a clinical feature of actinic keratosis. The genital area, which is not typically sun exposed, is not a frequent location. Actinic keratosis does not typically occur in a nodular growth pattern. p16 positivity is seen in high risk HPV related lesions, whereas βHPV associated with actinic keratosis is not considered one of these strains.
Comment Here
Reference: Actinic keratosis
Comment Here
Reference: Actinic keratosis
Practice question #2
Positivity of which of the following these immunohistochemical stains may be helpful in the diagnosis of actinic keratosis?
- BerEP4
- EMA
- MelanA
- p16
- p53
Practice answer #2
E. p53. p53 protein is overexpressed in the basal layers of the epithelium in 50% of actinic keratosis, which may aid in the diagnosis of difficult cases. BerEP4 is positive in basal cell carcinoma but negative in actinic keratosis. EMA is widely expressed on epithelial cells and has no use in solar damaged skin. MelanA might show a slight melanocytic hyperplasia but is not specific for actinic keratosis. Finally, strong p16 positivity is seen in lesions caused by high risk HPV, whereas βHPV associated with actinic keratosis is not considered one of these strains.
Comment Here
Reference: Actinic keratosis
Comment Here
Reference: Actinic keratosis
Practice question #3
Which immunohistochemical positive staining in actinic keratosis can be the cause of a diagnostic error?
- CD20
- HMB45
- MelanA
- Sox10
- Vimentin
Practice answer #3
C. MelanA. The presence of MelanA positive cells and pseudomelanocytic nests is a well known pitfall in the histological and immunohistochemical diagnosis of actinic keratosis. These cells are typically negative for other melanocytic markers, such as SOX10 or HMB45. CD20 is a marker of B lymphocytes and vimentin is negative in squamous epithelium.
Comment Here
Reference: Actinic keratosis
Comment Here
Reference: Actinic keratosis