Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Gonzalez RS, Graham RP. HCC - fibrolamellar variant. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/livertumorfibrolamellar.html. Accessed May 14th, 2024.
Definition / general
- Uncommon yet distinctive primary hepatocellular malignancy
- Typically affects young individuals from teens to 40 years
- Large oncocytic neoplastic cells forming tumor tongues separated by collagen bundles
- Characteristically no underlying chronic liver disease
- > 95% of cases harbor the oncogenic DNAJB1-PRKACA fusion gene formed by intrachromosomal deletion on chromosome 19 (Mod Pathol 2018;31:141)
- Rare cases related to biallelic PRKAR1A loss (Hepatology 2018;68:1441)
- Likely a distinct entity due to unique distinctive clinical, histologic and molecular biologic features
Essential features
- Primary hepatocellular neoplasm
- Eosinophilic tumor cells characterized by ample granular cytoplasm
- Intratumoral fibrosis
- Recurrent protein kinase A oncogenic driver abnormalities
Terminology
- Fibrolamellar carcinoma
ICD coding
- ICD-10: C22.0 - liver cell carcinoma
Epidemiology
- Predilection for teenage to 40 years old
- ~99% of cases diagnosed under the age of 50 years at presentation (Mod Pathol 2018;31:141)
- Propensity for late recurrence
Sites
- Liver
Etiology
- Almost all are characterized by DNAJB1-PRKACA oncogenic driver fusion gene (for other mutations, refer to Molecular / cytogenetics description below) (Science 2014;343:1010)
- No chronic liver disease
Clinical features
- Rare over 50 years old
- No gender preference
- Symptoms related to hepatic mass (Semin Diagn Pathol 2017;34:146)
- Rarely associated with gynecomastia or other paraneoplastic phenomena (Lancet 1984;1:538)
- Not associated with viral hepatitis, inborn errors of metabolism or cirrhosis
- Metastasizes to abdominal lymph nodes and peritoneum with greater propensity than conventional hepatocellular carcinoma (Eur J Pediatr Surg 2014;24:461)
Diagnosis
- Combination of
- Compatible histomorphology
- Appropriate immunophenotype (CK7, CD68 positive) or detection of key genomic events (DNAJB1-PRKACA, PRKACA rearrangement, PRKACA amplification, PRKAR1A loss)
Laboratory
- Serum alpha fetoprotein is classically not elevated
- No other routinely used serum or plasma markers
- Circulating tumor DNA assay has yet to be made commercially available
Radiology description
- CT scan and MRI: nonspecific findings; central scar (similar to focal nodular hyperplasia) may be identified; often calcified
Prognostic factors
- Perhaps the most controversial aspect of fibrolamellar carcinoma - not adequately stratified by current AJCC staging scheme
- Features associated with adverse outcome: vascular invasion, number of tumors, surgical resectability (Cancer 2006;106:1331, J Gastrointest Surg 2016;20:1725, Oncology 2013;85:197)
Case reports
- Carney complex
- 9 year old boy (J Pediatr Endocrinol Metab 2007;20:247)
- 14 year old girl 5 years after hepatocellular adenoma (Arch Pathol Lab Med 2004;128:222)
- 53 year old woman with synchronous auricular myxoma (Case Rep Pathol 2015;2015:241708)
- Peritoneal spread
- 23 year old woman with ovarian metastasis (Rom J Morphol Embryol 2017;58:187)
- 26 year old woman (Eur J Radiol 1999;32:119)
Treatment
- Surgery is the only curative option (Am J Gastroenterol 2009;104:2617)
- Early detection of relapse with multimodality therapy improves survival (Eur J Surg Oncol 2009;35:617)
Gross description
- Single (75%), large (frequently > 10 cm), hard, well circumscribed, bulging, tan tumor with fibrous bands
- Central stellate scar is noted in approximately 70%
- Variable bile staining, hemorrhage and necrosis
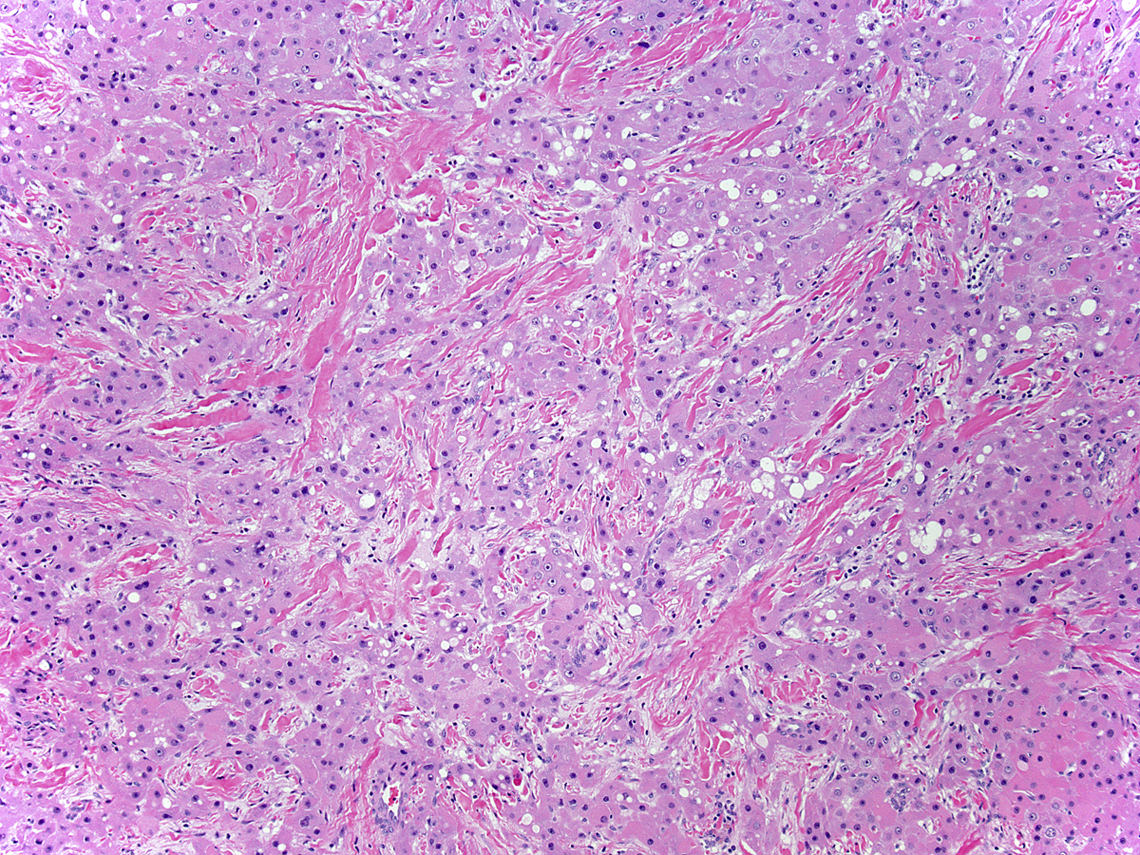
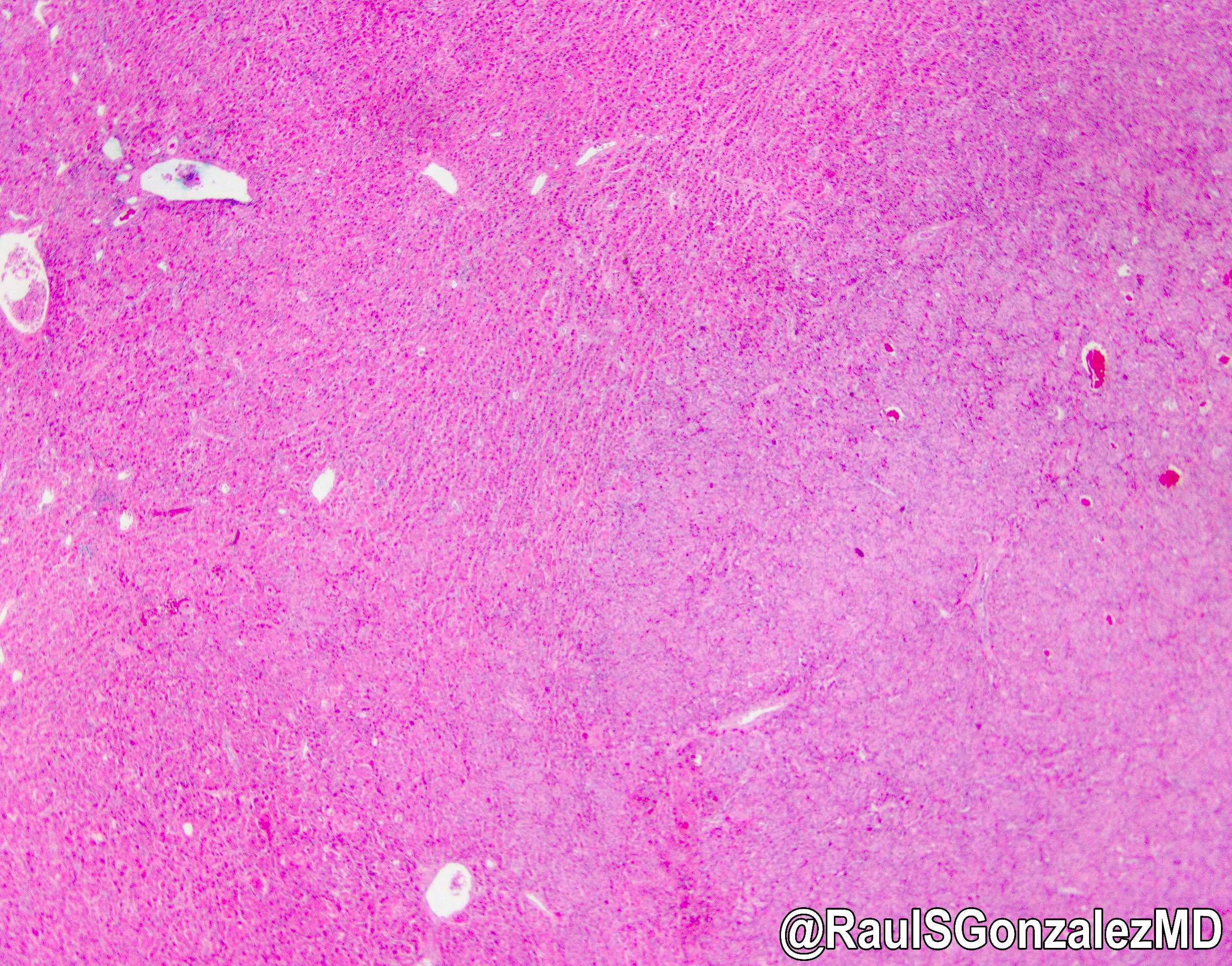
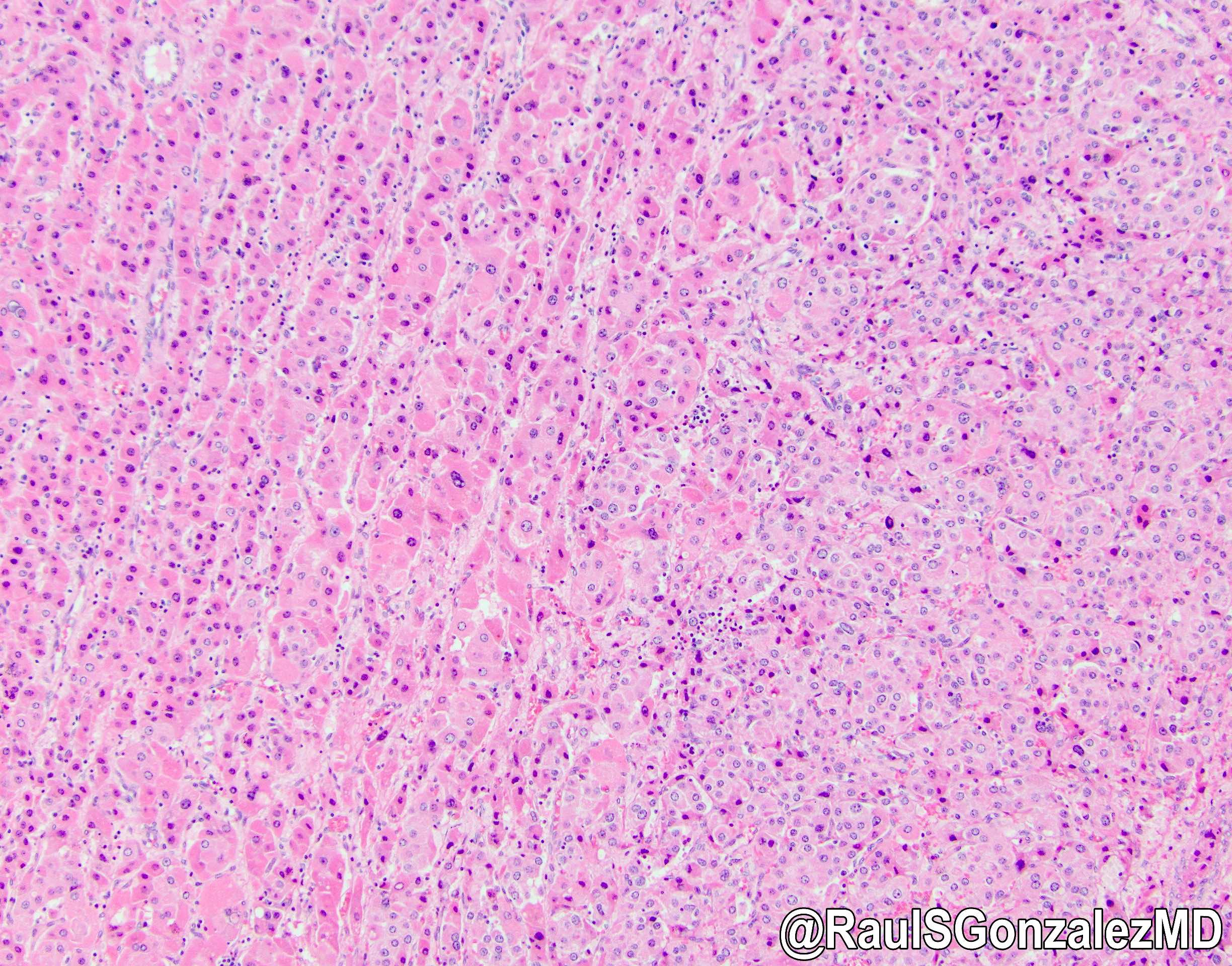
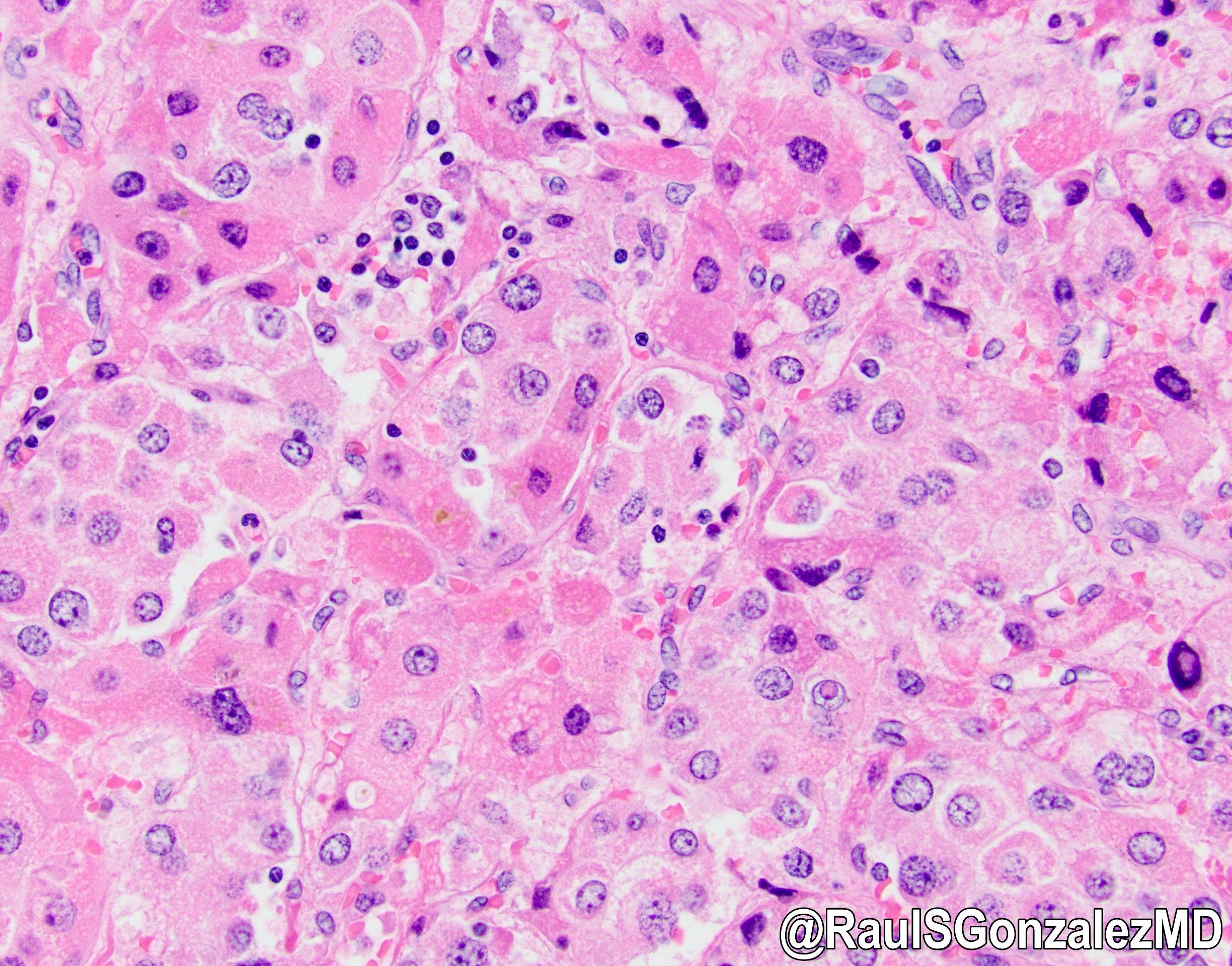
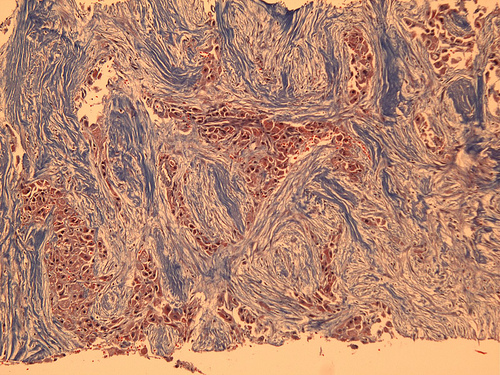
Microscopic (histologic) description
- Trabecula, sheets or cords of neoplastic cells with abundant oncocytic cytoplasm cells in background of dense collagen bundles frequently arranged in parallel lamellae
- Cells are large and polygonal with well defined cell borders
- Abundant granular and eosinophilic cytoplasm due to abundant mitochondria
- Pale or pink bodies are frequently noted but not necessary for diagnosis
- Typical nuclear features include open chromatin and prominent macronucleoli (Adv Anat Pathol 2007;14:217)
- Vascular invasion may be seen
- Histologically, fibrous bands coalesce into central scar
- Nonneoplastic liver is within normal histologic limits
- Radiologic calcification corresponds to stromal calcification
- Calcified individual cells may be identified as well
- Variable: focal nuclear anisonucleosis, sheet-like growth without intervening fibrous bands, pseudoglandular or pelioid patterns
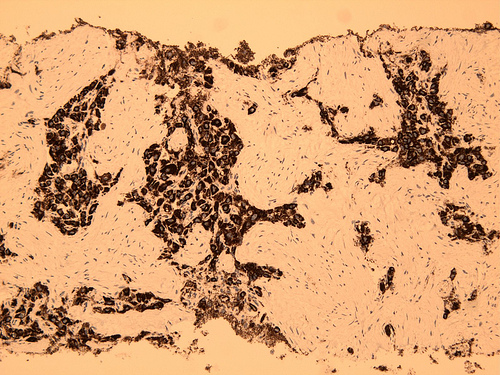
Microscopic (histologic) images
Contributed by Rondell P. Graham, M.B.B.S. and @RaulSGonzalezMD on Twitter
Case #161
Images hosted on other servers:
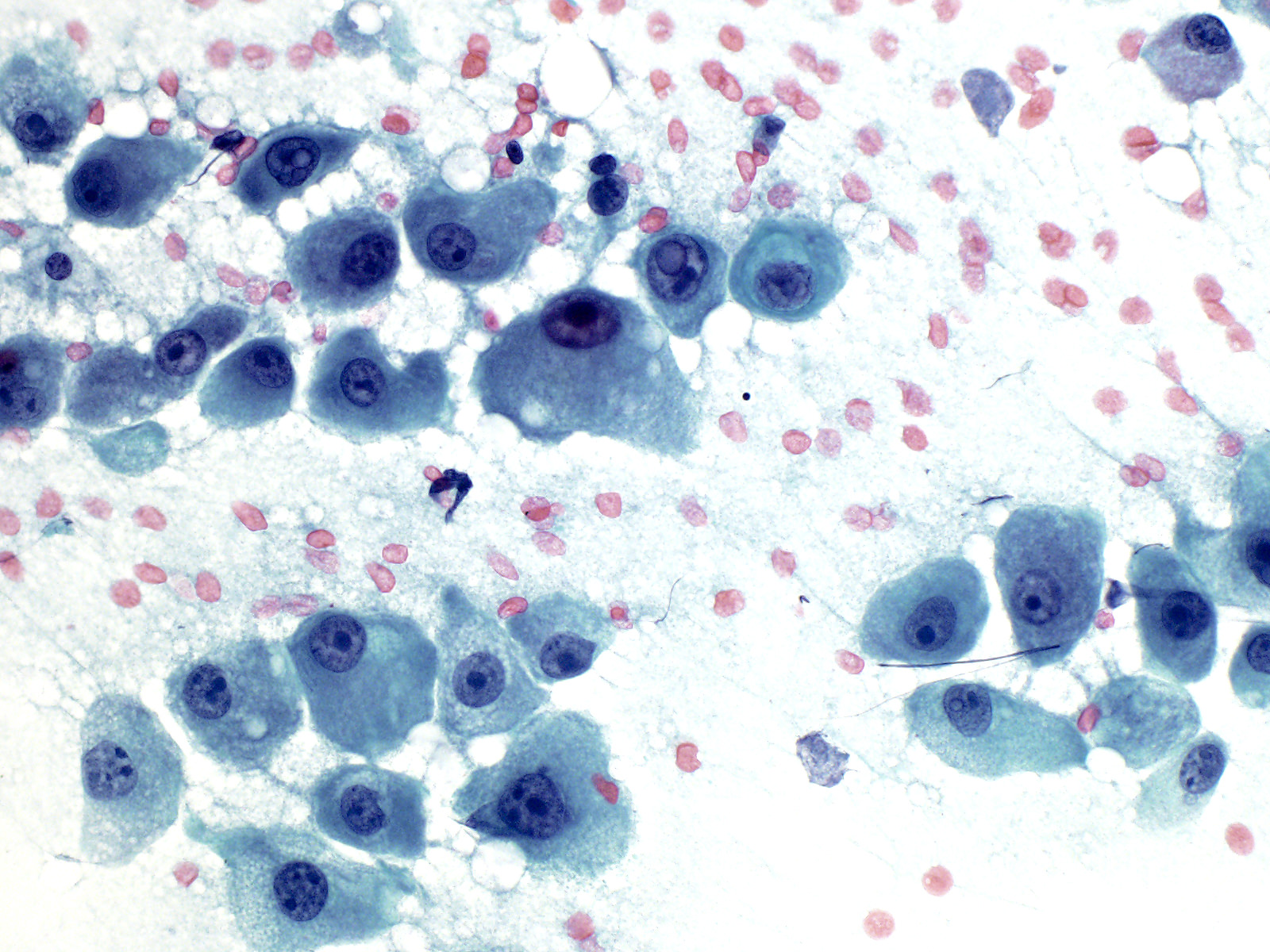
Cytology description
- Individual cells with ample cytoplasm, open nuclear chromatin and prominent nucleoli; may contain bile
Cytology images
Positive stains
- HepPar1 and CK7 (Mod Pathol 2010;23:1180, Histopathology 1990;17:101)
- CD68 (Mod Pathol 2011;24:390)
- CK19
- Also fibrinogen (pale bodies), alpha-1 antitrypsin, polyclonal CEA and CAM 5.2 (CK8 / 18)
Negative stains
- Liver fatty acid binding protein (LFABP)
- In rare cases PRKAR1A; often individuals with the Carney complex
Electron microscopy description
- Numerous mitochondria
- Abundant endoplasmic reticulum membranes with concentric whorls
- Internalized canaliculi lined by microvilli (Mod Pathol 2017;30:892)
Molecular / cytogenetics description
- > 95% of cases are characterized by DNAJB1-PRKACA fusion gene; diagnostic tests exist
- Rare cases characterized by biallelic PRKAR1A loss (mostly in patients with the Carney complex) instead of the above fusion gene (Hepatology 2018;68:1441)
- Single case characterized by PRKACA amplification without the above genomic changes has been identified (Surg Pathol Clin 2018;11:377)
- Transcriptome has been published and revealed multiple insights (Proc Natl Acad Sci U S A 2015;112:E5916)
- Overall fewer chromosomal abnormalities than classic hepatocellular carcinoma (Mod Pathol 2009;22:134)
Sample pathology report
- Liver, segment 3, resection:
- Fibrolamellar hepatocellular carcinoma (see synoptic report and comment)
- Comment: A trichrome stain shows no significant fibrosis. An iron stain is unremarkable.
Differential diagnosis
- Cholangiocarcinoma:
- Truly glandular, often conspicuous pleomorphism
- Focal nodular hyperplasia:
- Ductular reaction around central scar
- Lesional cells are not characteristically oncocytic
- Does not have the nuclear features of fibrolamellar carcinoma
- Hepatocellular carcinoma, sclerosing variant:
- No oncocytes, smaller tumor cells, pseudoglandular pattern common
- Metastatic carcinoma with sclerotic stroma:
- Conspicuous pleomorphism
- Neuroendocrine tumors:
- Only oncocytic examples
- Nuclear features are often not typical of fibrolamellar carcinoma
- Positive for neuroendocrine markers
- Paraganglioma:
- May have abundant oncocytic cytoplasm
- Round nuclei without the typical features of fibrolamellar carcinoma, vascular stroma without dense fibrosis
- Positive for neuroendocrine markers and negative for cytokeratins (Am J Surg Pathol 2002;26:945)
Board review style question #1
What is the characteristic status of the nonneoplastic liver in patients with fibrolamellar carcinoma?
- Chronic viral hepatitis C without advanced fibrosis
- Cirrhosis due to chronic viral hepatitis B
- Glycogen storage disease
- Normal
- Steatohepatitis
Board review style answer #1