Table of Contents
Definition / general | Epidemiology | Diagrams / tables | Clinical features | Radiology images | Prognostic factors | Case reports | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Differential diagnosis | Board review style question #1 | Board review style answer #1Cite this page: Gulwani H. Thymic squamous cell carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mediastinumthymiccarcinoma.html. Accessed May 13th, 2024.
Definition / general
- By definition, has overt cellular anaplasia
Epidemiology
- Ages ≥ 50 years; occasionally children
Diagrams / tables
Clinical features
- Associated with hypercalcemia, elevated parathyroid hormone levels, pulmonary sarcoidosis
- Not associated with paraneoplastic syndromes such as myasthenia gravis or pure red cell aplasia
- Patients usually present with mass related symptoms
- Aggressive clinical course
- Must exclude other primaries, which are much more common (lung, trachea, bronchi, esophagus)
- Usually squamous cell carcinoma and variants (lymphoepithelioma-like, basaloid)
- Proposed staging system (Am J Clin Pathol 2012;138:115)
Radiology images
Prognostic factors
- May be less aggressive than commonly believed; important prognostic factors are lymph node status and tumor size (Am J Clin Pathol 2012;138:103)
- Keratinizing: good prognosis with few fatalities if well differentiated
Case reports
- 42 year old man with multiple lung, bone and brain metastases (Acta Neurol Taiwan 2010;19:41)
- 47 year old Asian woman with malaise, weight loss, chest pain and shortness of breath (Case of the Month #479)
- 52 year old man with complaints of left anterior chest pain (Kyobu Geka 2003;56:509)
Gross description
- Unencapsulated, no internal fibrous septation, firm / hard / gritty with gray-white cut surface, necrosis and hemorrhage
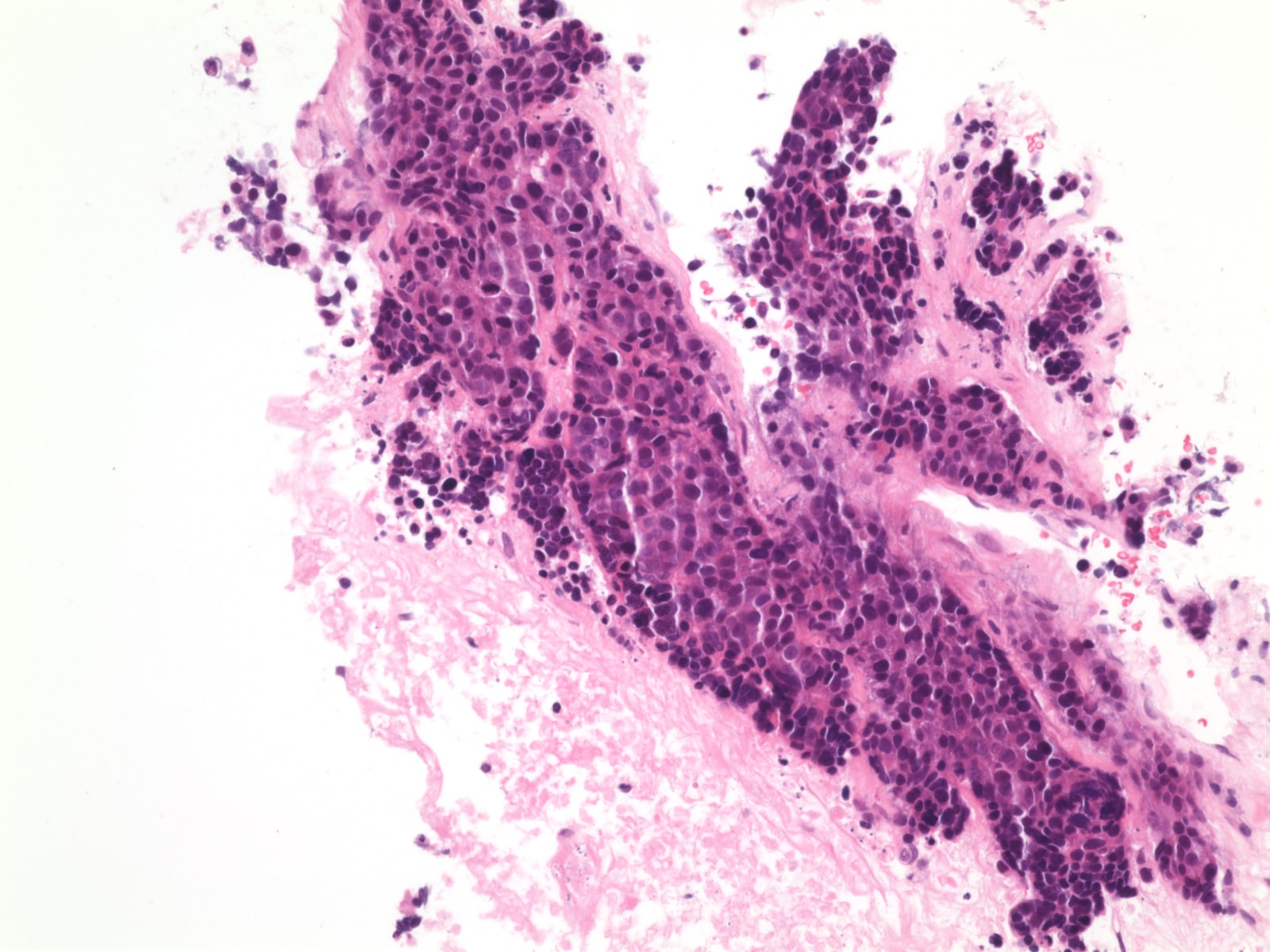
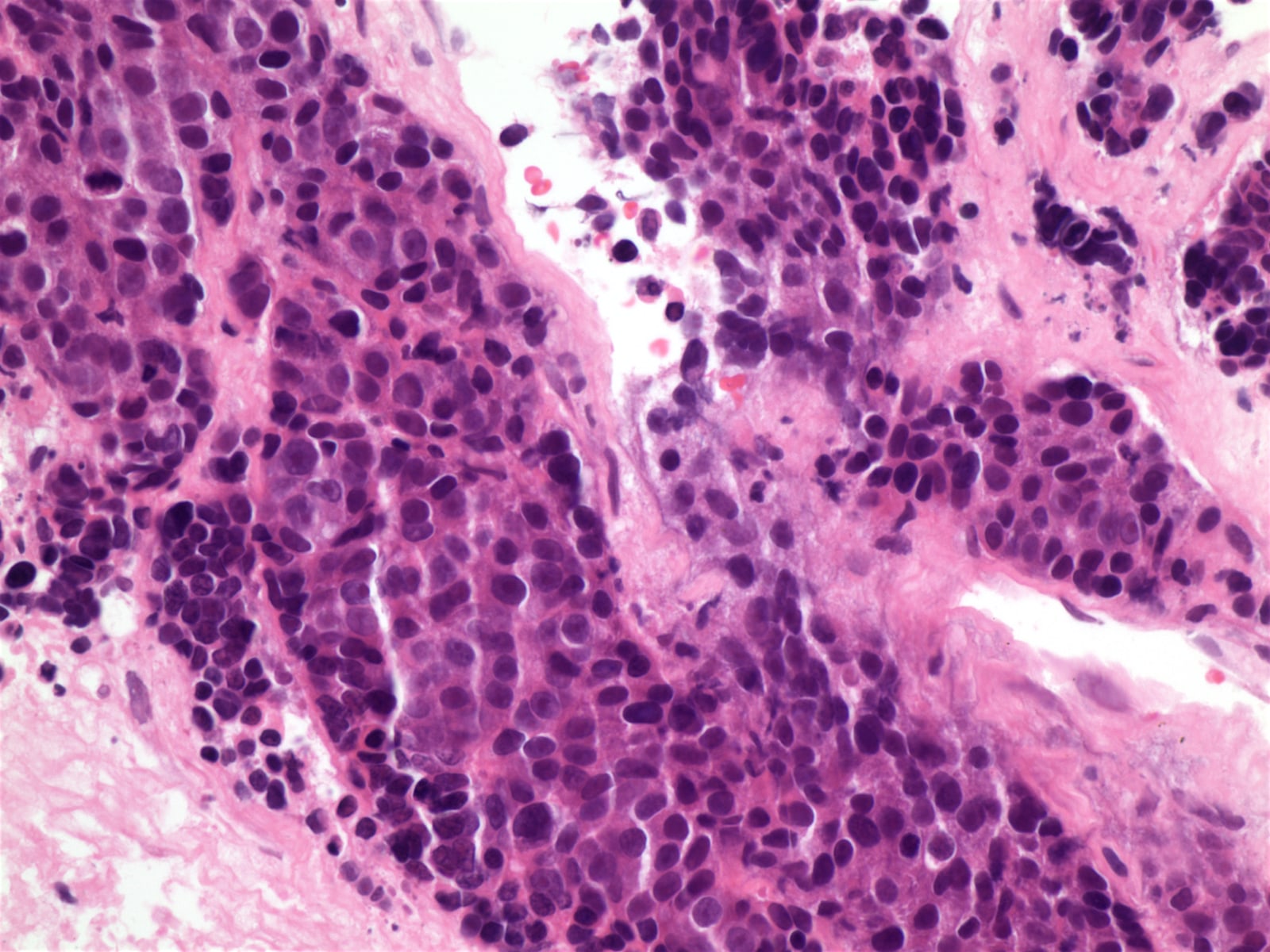
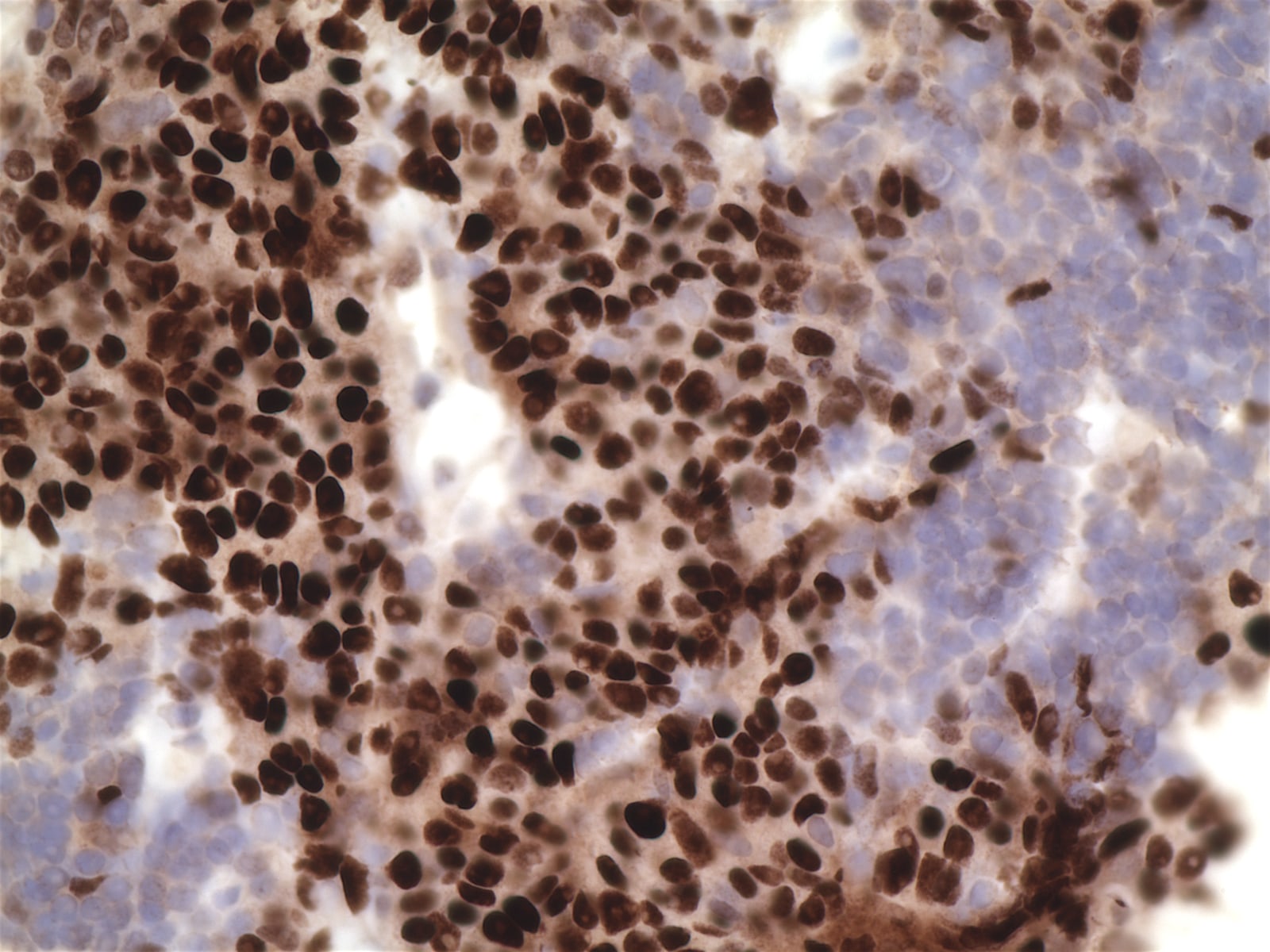
Microscopic (histologic) description
- Usually cohesive cellular growth, regularly round / oval nuclear outlines, eosinophilic nucleoli, geographic necrosis
- Usually foci of medullary differentiation, abortive Hassall corpuscles, rosettes, gland-like spaces, T lymphocytes; no perivascular spaces
- Keratinizing:
- Similar to tumor in skin, lung, other sites
- Lobular growth with fibrous bands
- Nests and cords of large polyhedral cells with intercellular bridges
- Vesicular or hyperchromatic nuclei, prominent nucleoli, eosinophilic or glassy cytoplasm, keratin pearls
- Also angiolymphatic invasion, necrosis
- Rarely coexists with thymoma
- Non-keratinizing
- Angular nests of malignant squamous cells in desmoplastic stroma
- No intercellular bridges, no eosinophilic cytoplasm, no keratin pearls
Microscopic (histologic) images
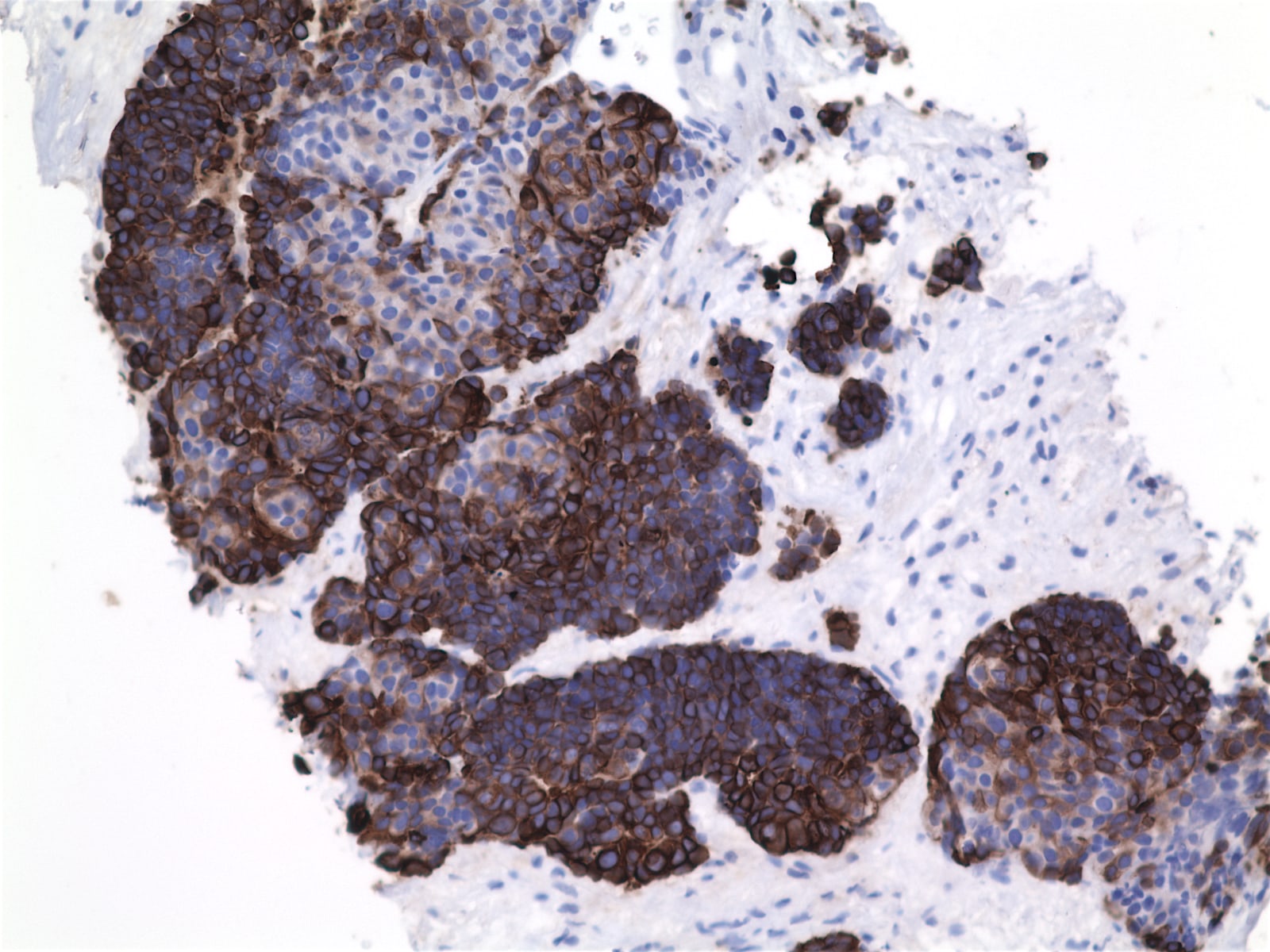
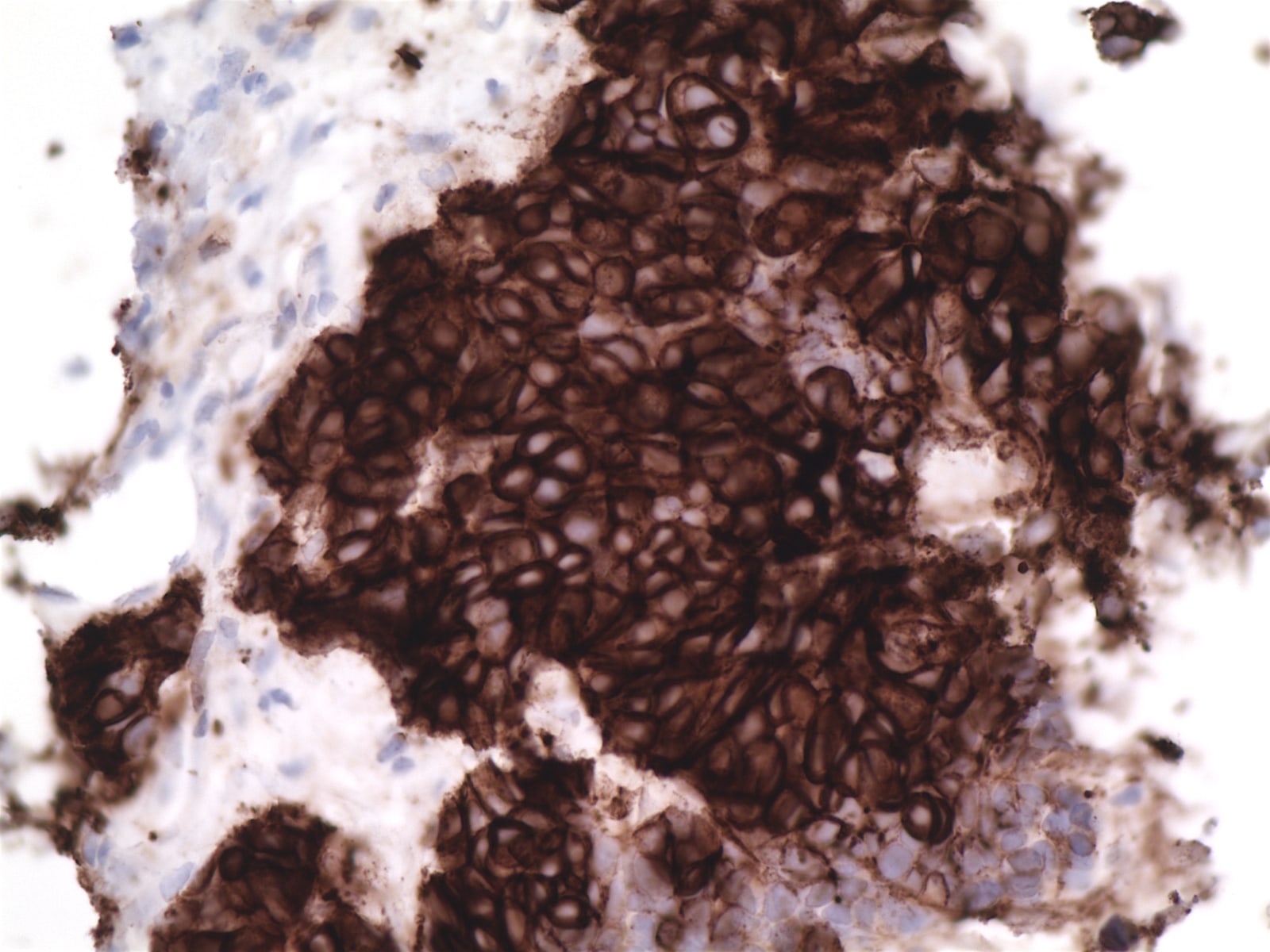
Positive stains
- Keratin, CD5, CD70, often EMA, variable CEA (if overt glandular differentiation), c-kit, GLUT1 (Am J Surg Pathol 2000;24:742, Am J Surg Pathol 2011;35:1296, Virchows Arch 2011;458:615)
Negative stains
- Vimentin, proteasome beta subunit (Am J Surg Pathol 2011;35:1296)
Electron microscopy description
- Well formed desmosome-like intercellular junctions, cytoplasmic tonofilaments that may insert into junctional complexes
Differential diagnosis
- Metastatic carcinoma
- Thymoma type B3:
- GLUT1 usually negative (Mod Pathol 2009;22:1341)
Board review style question #1
Which 2 antibodies are most helpful in diagnosing thymic carcinoma?
A. CK5/6, 34bE12
B. CD5, p63
C. CEA, synaptophysin
D. p63, p40
E. KIT / CD117, INSM1
A. CK5/6, 34bE12
B. CD5, p63
C. CEA, synaptophysin
D. p63, p40
E. KIT / CD117, INSM1
Board review style answer #1
B. CD5 combined with p63 are helpful thymic markers.
Comment Here
Reference: Thymic squamous cell carcinoma
Comment Here
Reference: Thymic squamous cell carcinoma