26 July 2006 - Case #54
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Sarah Webb, Harris Methodist HEB, Bedford, Texas, USA.

Case #54
Clinical history:
The patient is a 59 year old woman with a slow growing tumor of the parotid gland present for several years. Upon excision, it was 3 cm, mottled and tan-yellow with scalloped borders.
There was also peripheral soft tissue invasion and necrosis.
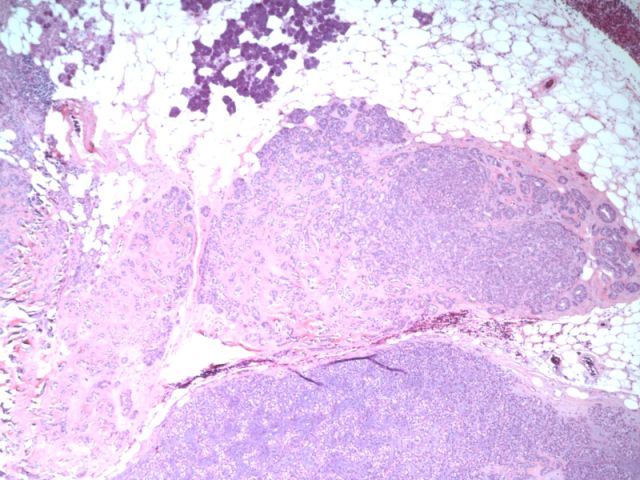
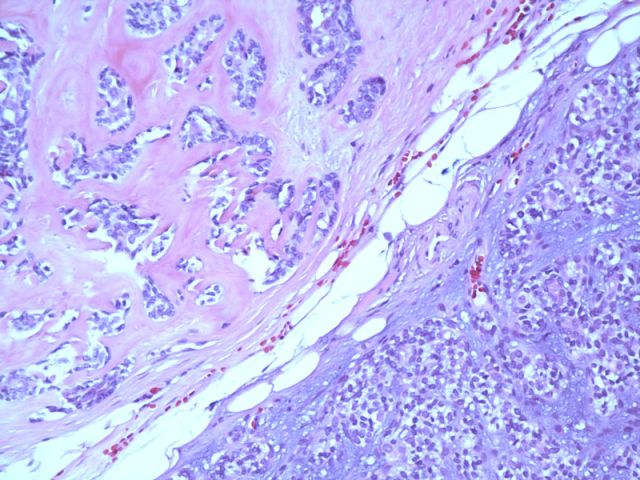
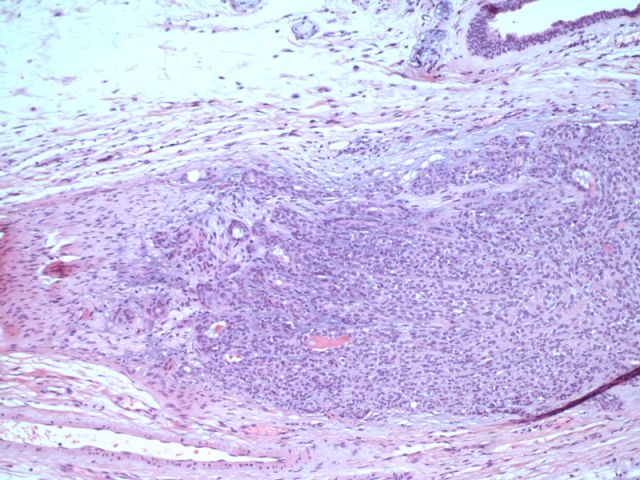
Microscopic images:
What is your diagnosis?
Diagnosis: Epithelial myoepithelial carcinoma of the salivary gland
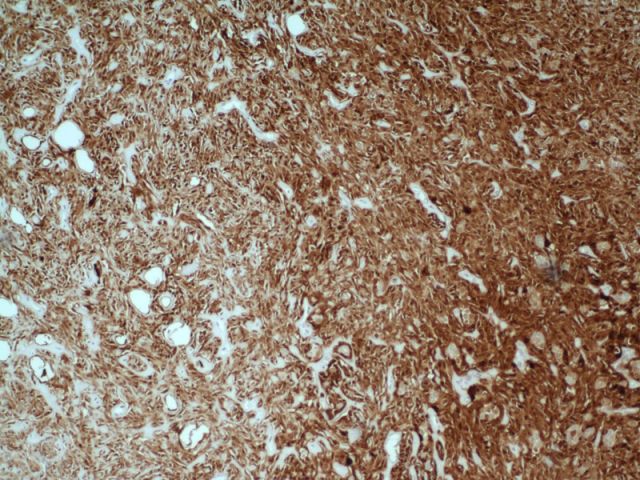
Stain images:
Discussion:
Epithelial myoepithelial carcinoma is a rare salivary gland tumor, representing less than 0.5% of tumors at this site. Most (80%) cases arise in the parotid gland and occur in women (60%), with a mean patient age of 60 years or older.
Grossly, these tumors are well circumscribed, up to 3 cm, and infiltrate into adjacent tissue. Microscopically, they are a low grade malignancy with epithelial and myoepithelial components. They are often multinodular with a thick fibrous capsule. Most tumor cells have myoepithelial features, with clear cytoplasm or naked nuclei. Focally, there are ducts or tubules with an outer rim of myoepithelial cells and inner, dark ductal cells. The ductal cells have scant eosinophilic cytoplasm and round, bland nuclei. These tumors may also have spindled or plasmacytoid cells.
The myoepithelial component is PAS+, diastase sensitive due to cytoplasmic glycogen. The myoepithelial component is also immunoreactive for S100, p63 and smooth muscle actin, with variable keratin staining (Cancer 2005;105:240). The epithelial component is strongly immunoreactive for keratin and EMA, with occasional S100 staining.
Cytologic smears are usually cellular, with single cells and naked nuclei. A biphasic pattern may not be evident since the clear cells have fragile cytoplasm and often appear as naked nuclei (Diagn Cytopathol 2003;28:163).
These tumors are low grade malignancies with frequent local recurrences. They were previously often considered to be benign. However, with sufficient follow up, there are rare regional nodal metastases and distant metastases to the lung and kidney.
The differential diagnosis may be broad. It includes myoepithelial carcinoma, which many authors define as lacking any epithelial component (Am J Surg Pathol 2000;24:761). Pleomorphic adenomas are also biphasic tumors but have a prominent myxochondroid stroma and the myoepithelial cells usually lack cytoplasmic clearing. Other biphasic tumors include adenoid cystic carcinoma (prominent cribriform pattern) and polymorphous low grade adenocarcinoma (affects intraoral salivary glands, clear cells do not predominate and are not associated with ductal cells). Clear cell carcinomas usually affect the minor salivary glands, are unencapsulated, lack epithelial cells and are negative for myoepithelial markers. Finally, metastatic renal cell carcinoma should be considered.
References: Arch Pathol Lab Med 2002;126:676
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Sarah Webb, Harris Methodist HEB, Bedford, Texas, USA.

Website news:
(1) This case is sponsored by Sakura Finetek, USA. Leading the revolution in Pathology, the Tissue-Tek Xpress Rapid Tissue Processor is helping laboratories achieve new levels of productivity. Enabling a continuous flow of up to 40 cassettes every 15 minutes, this system can process up to 120 specimens per hour. The Xpress allows for a balanced distribution of work throughout the day, eliminating bottlenecks and batches common with overnight processing. Improved turnaround times, reduced waste, and increased productivity are just a few benefits this technology can offer your lab. Results are the same or better than overnight processing. Help your lab reach its full potential with the Tissue-Tek Xpress Rapid Tissue Processor. For more information, contact Ms. Elise Green, Marketing Manager at 1-800-725-8723 extension 7873 or at egreen@sakuraus.com.
Visit and follow our Blog to see recent updates to the website.
(1) This case is sponsored by Sakura Finetek, USA. Leading the revolution in Pathology, the Tissue-Tek Xpress Rapid Tissue Processor is helping laboratories achieve new levels of productivity. Enabling a continuous flow of up to 40 cassettes every 15 minutes, this system can process up to 120 specimens per hour. The Xpress allows for a balanced distribution of work throughout the day, eliminating bottlenecks and batches common with overnight processing. Improved turnaround times, reduced waste, and increased productivity are just a few benefits this technology can offer your lab. Results are the same or better than overnight processing. Help your lab reach its full potential with the Tissue-Tek Xpress Rapid Tissue Processor. For more information, contact Ms. Elise Green, Marketing Manager at 1-800-725-8723 extension 7873 or at egreen@sakuraus.com.
Visit and follow our Blog to see recent updates to the website.
Case #54
Clinical history:
The patient is a 59 year old woman with a slow growing tumor of the parotid gland present for several years. Upon excision, it was 3 cm, mottled and tan-yellow with scalloped borders.
There was also peripheral soft tissue invasion and necrosis.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Epithelial myoepithelial carcinoma of the salivary gland
Stain images:
Discussion:
Epithelial myoepithelial carcinoma is a rare salivary gland tumor, representing less than 0.5% of tumors at this site. Most (80%) cases arise in the parotid gland and occur in women (60%), with a mean patient age of 60 years or older.
Grossly, these tumors are well circumscribed, up to 3 cm, and infiltrate into adjacent tissue. Microscopically, they are a low grade malignancy with epithelial and myoepithelial components. They are often multinodular with a thick fibrous capsule. Most tumor cells have myoepithelial features, with clear cytoplasm or naked nuclei. Focally, there are ducts or tubules with an outer rim of myoepithelial cells and inner, dark ductal cells. The ductal cells have scant eosinophilic cytoplasm and round, bland nuclei. These tumors may also have spindled or plasmacytoid cells.
The myoepithelial component is PAS+, diastase sensitive due to cytoplasmic glycogen. The myoepithelial component is also immunoreactive for S100, p63 and smooth muscle actin, with variable keratin staining (Cancer 2005;105:240). The epithelial component is strongly immunoreactive for keratin and EMA, with occasional S100 staining.
Cytologic smears are usually cellular, with single cells and naked nuclei. A biphasic pattern may not be evident since the clear cells have fragile cytoplasm and often appear as naked nuclei (Diagn Cytopathol 2003;28:163).
These tumors are low grade malignancies with frequent local recurrences. They were previously often considered to be benign. However, with sufficient follow up, there are rare regional nodal metastases and distant metastases to the lung and kidney.
The differential diagnosis may be broad. It includes myoepithelial carcinoma, which many authors define as lacking any epithelial component (Am J Surg Pathol 2000;24:761). Pleomorphic adenomas are also biphasic tumors but have a prominent myxochondroid stroma and the myoepithelial cells usually lack cytoplasmic clearing. Other biphasic tumors include adenoid cystic carcinoma (prominent cribriform pattern) and polymorphous low grade adenocarcinoma (affects intraoral salivary glands, clear cells do not predominate and are not associated with ductal cells). Clear cell carcinomas usually affect the minor salivary glands, are unencapsulated, lack epithelial cells and are negative for myoepithelial markers. Finally, metastatic renal cell carcinoma should be considered.
References: Arch Pathol Lab Med 2002;126:676