Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Salama A, Xu B. Myoepithelial carcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsmyoepithelialcarcinoma.html. Accessed August 25th, 2025.
Definition / general
- Myoepithelial carcinoma of the salivary gland is a carcinoma that is composed exclusively or near exclusively of myoepithelial cells
- May arise de novo or ex pleomorphic adenoma
Essential features
- Carcinoma composed entirely of myoepithelial cells showing invasive growth
- Subclassified as de novo or ex pleomorphic adenoma (ex PA)
- Over 50% shows PLAG1 fusion
Terminology
- Malignant myoepithelioma (not recommended)
ICD coding
Epidemiology
- May affect patients of a wide age range: the reported median age of presentation is 59 years (range: 14 - 90) (Am J Surg Pathol 2015;39:931, Arch Otolaryngol Head Neck Surg 2010;136:702)
- No obvious gender predilection
- May occur in pediatric population (Hum Pathol 2017;67:37)
- Accounts for approximately 4% of salivary gland neoplasms (Arch Otolaryngol Head Neck Surg 2010;136:702)
- Frequency may be underestimated, as myoepithelial carcinoma is generally underrecognized (Surg Pathol Clin 2021;14:67, Am J Surg Pathol 2019;43:601)
Sites
- Parotid gland is the most common site of involvement, accounting for 24 - 73% of cases (J Oral Maxillofac Surg 2015;73:1938, Am J Surg Pathol 2015;39:931, Arch Otolaryngol Head Neck Surg 2010;136:702)
- Sites of involvement in a descending frequency are the parotid gland, minor salivary glands (especially those from the palate) and the submandibular gland (J Oral Maxillofac Surg 2015;73:1938, Am J Surg Pathol 2015;39:931, Arch Otolaryngol Head Neck Surg 2010;136:702)
Clinical features
- Nonspecific; the most commonly presentation is a painless mass (Arch Otolaryngol Head Neck Surg 2010;136:702)
Diagnosis
- Definite diagnosis can only be rendered in resection specimen by demonstrating invasiveness and (near) pure myoepithelial population within the tumor
Radiology description
- CT shows a solitary, lobulated or multinodular, heterogeneously enhancing mass with a partial ill defined border (Oral Surg Oral Med Oral Pathol Oral Radiol 2017;123:e182)
Prognostic factors
- Relatively aggressive clinically: 15 - 27% develops distant metastasis and over 33% have local recurrence (Arch Otolaryngol Head Neck Surg 2010;136:702, J Oral Maxillofac Surg 2015;73:1938, Am J Surg Pathol 2015;39:931, Am J Surg Pathol 2000;24:761, Arch Biochem Biophys 1989;269:272)
- Higher propensity for distant rather than regional metastasis
- Reported adverse prognostic factors include myoepithelial carcinoma ex pleomorphic adenoma, necrosis, high mitotic index (> 4 per 10 high power fields) and positive margin status (Am J Surg Pathol 2015;39:931, Arch Otolaryngol Head Neck Surg 2010;136:702)
Case reports
- 28 year old woman with a 4.0 cm parotid mass (Case Rep Otolaryngol 2020;2020:8325374)
- 64 year old patient present with a large mass in the maxillary sinus (Head Neck Pathol 2021 Jan 4 [Epub ahead of print])
- 65 year old African American man with a painless hard palate mass metastasizing to lung and spine (Case Rep Pathol 2019;2019:3863270)
Treatment
- Surgical resection with negative margin is considered the standard of care
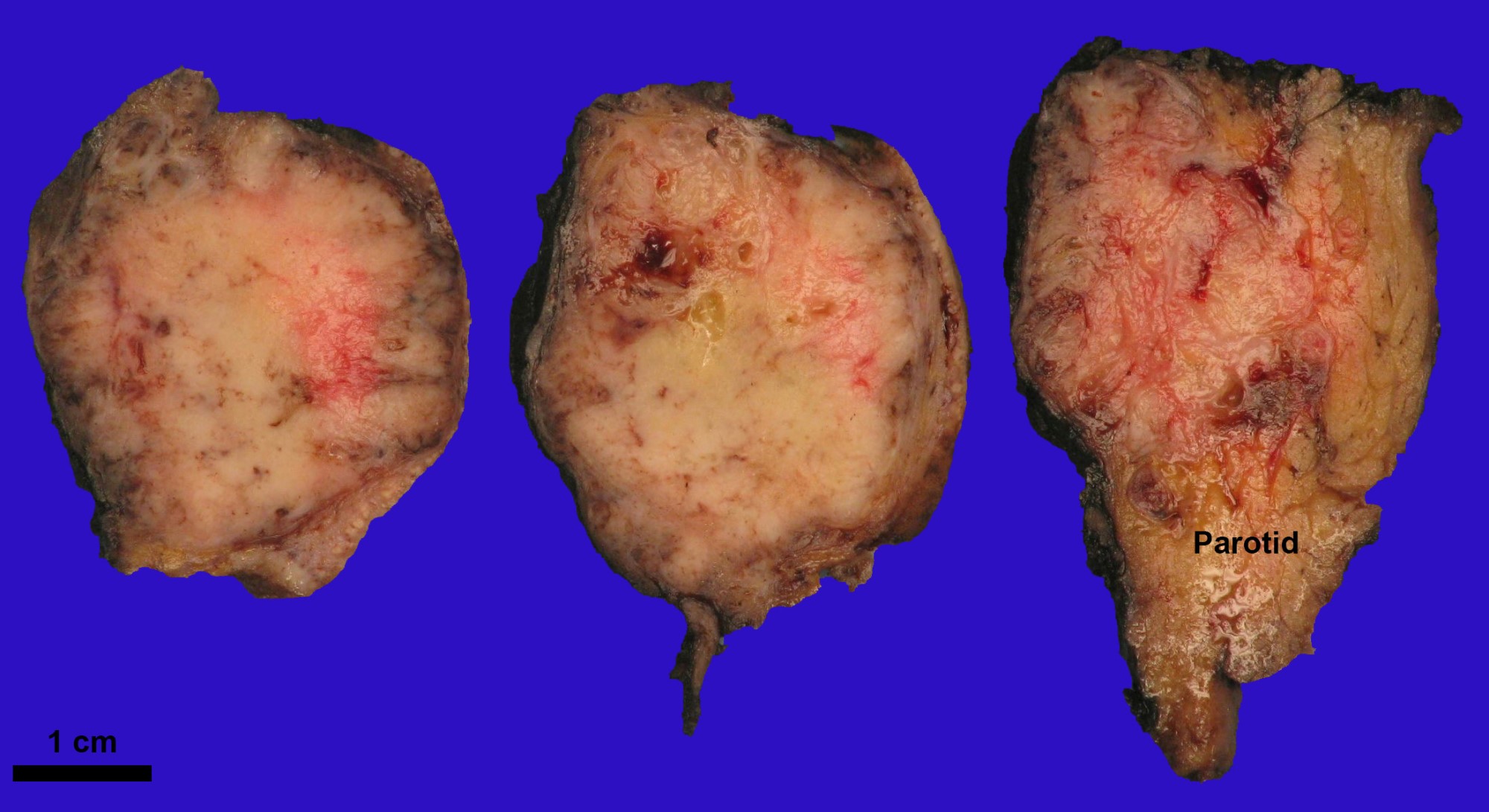
Gross description
- Gross appearance is nonspecific
- Tumor is often present as an expansile, lobulated to multinodular, beige to white mass, sometimes with ill defined / infiltrative border
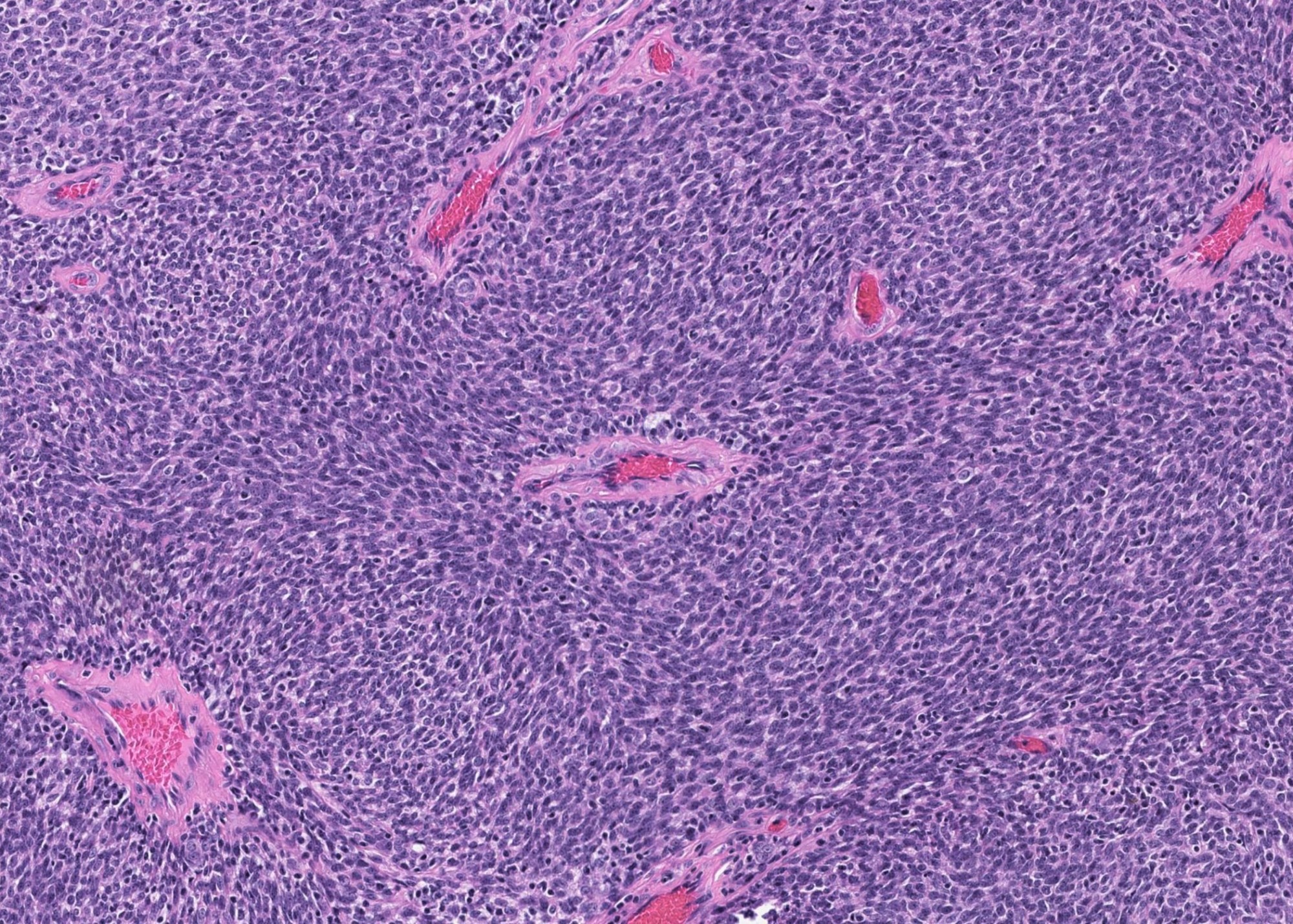
Microscopic (histologic) description
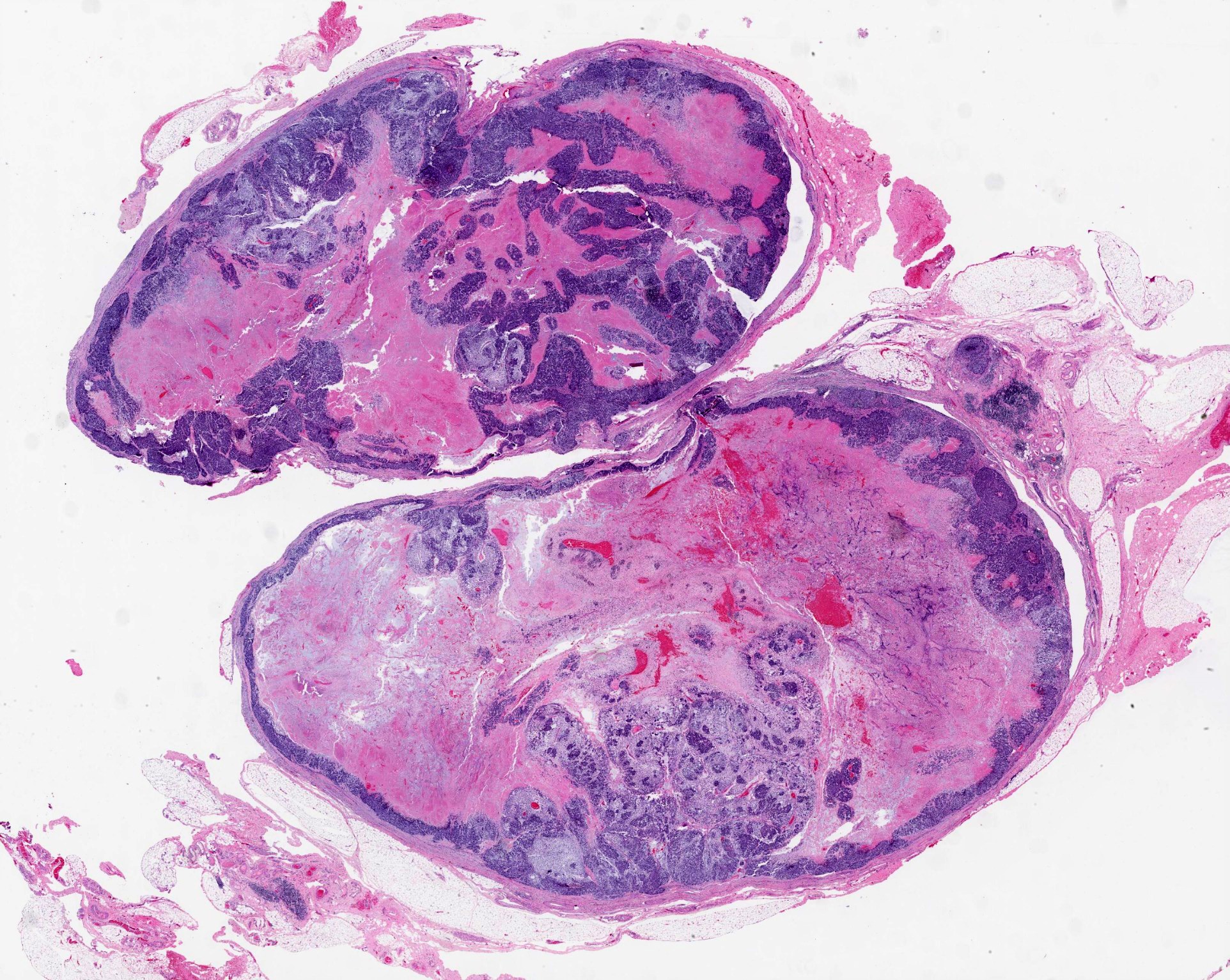
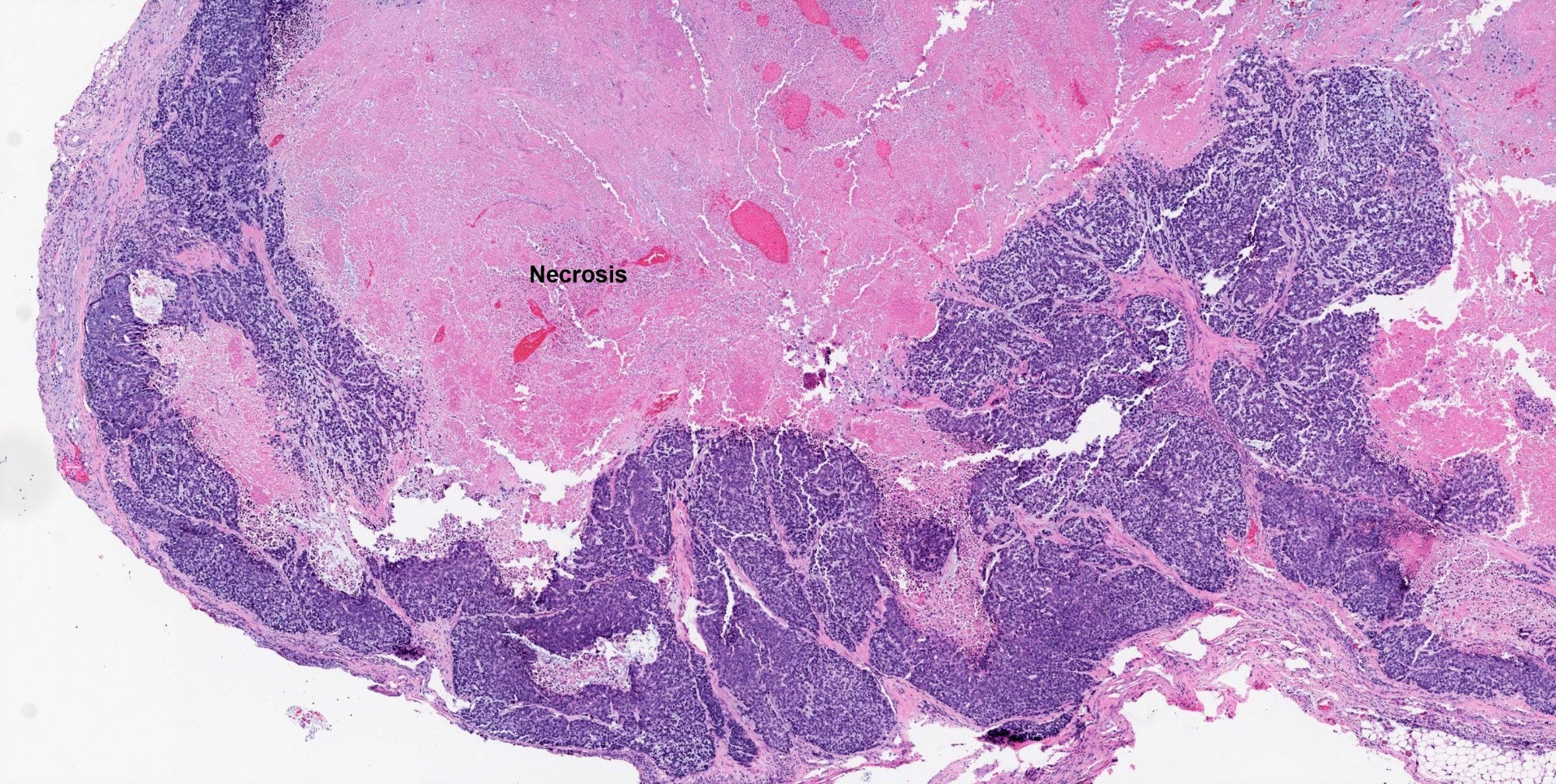
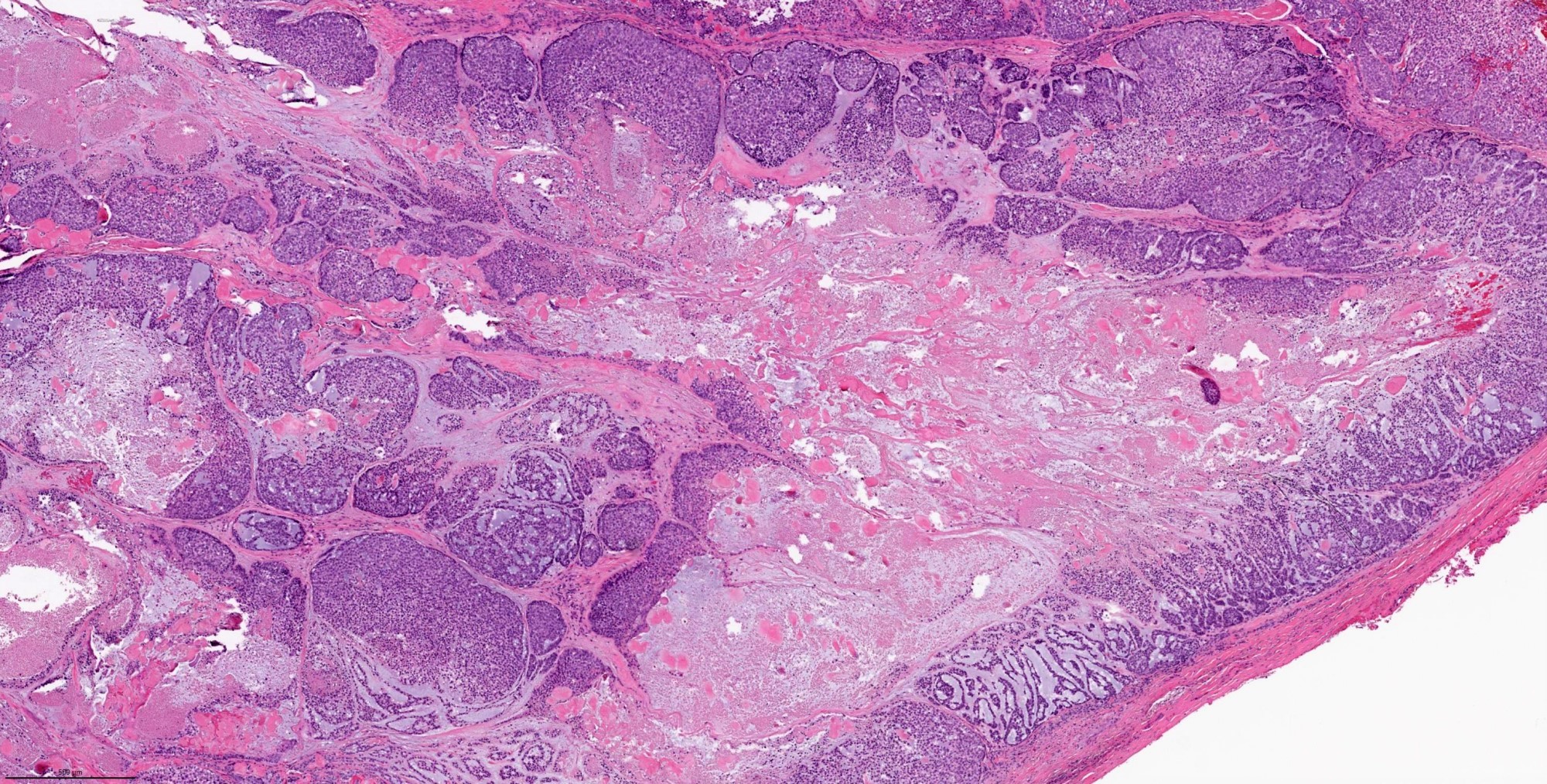
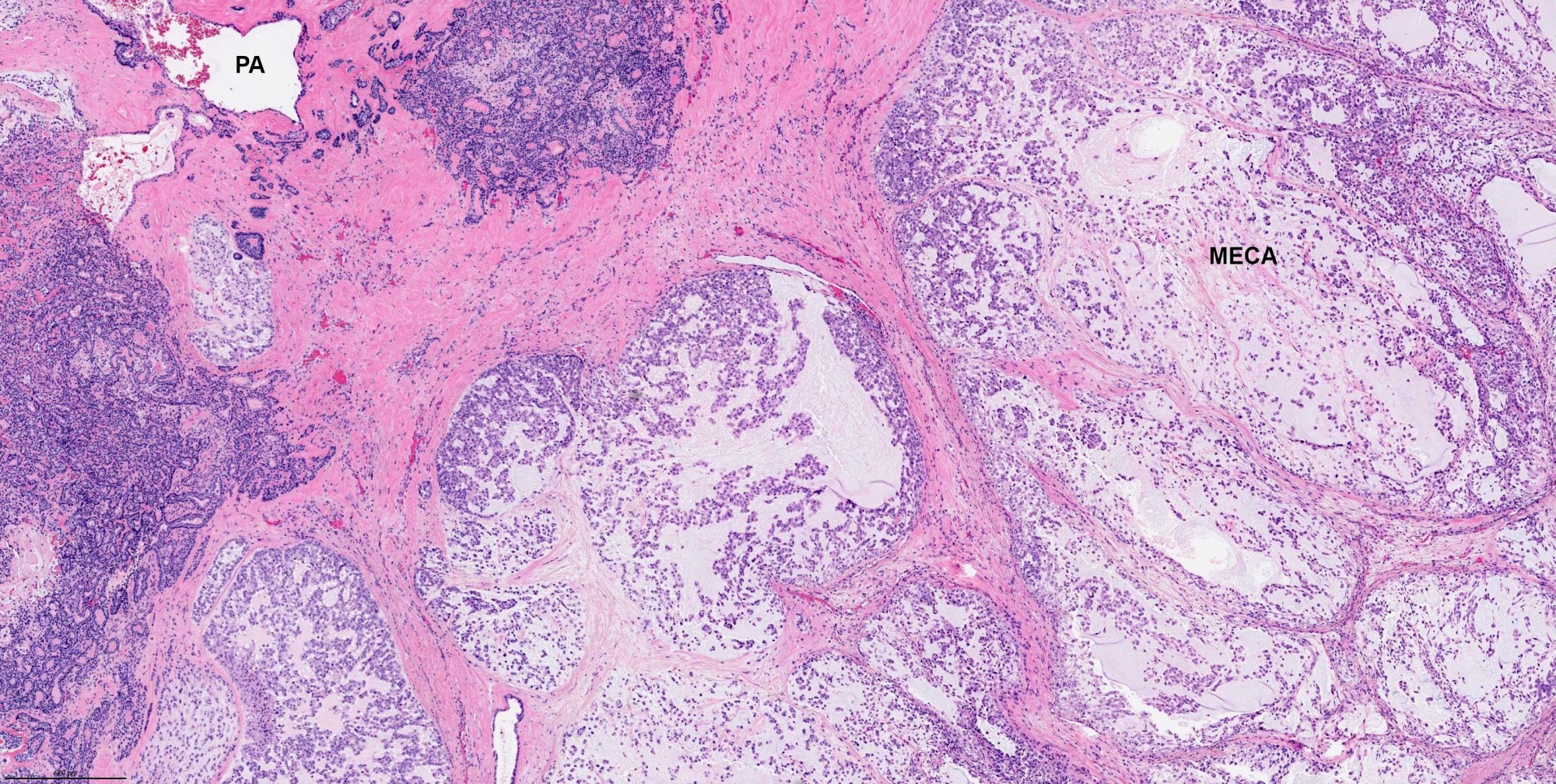
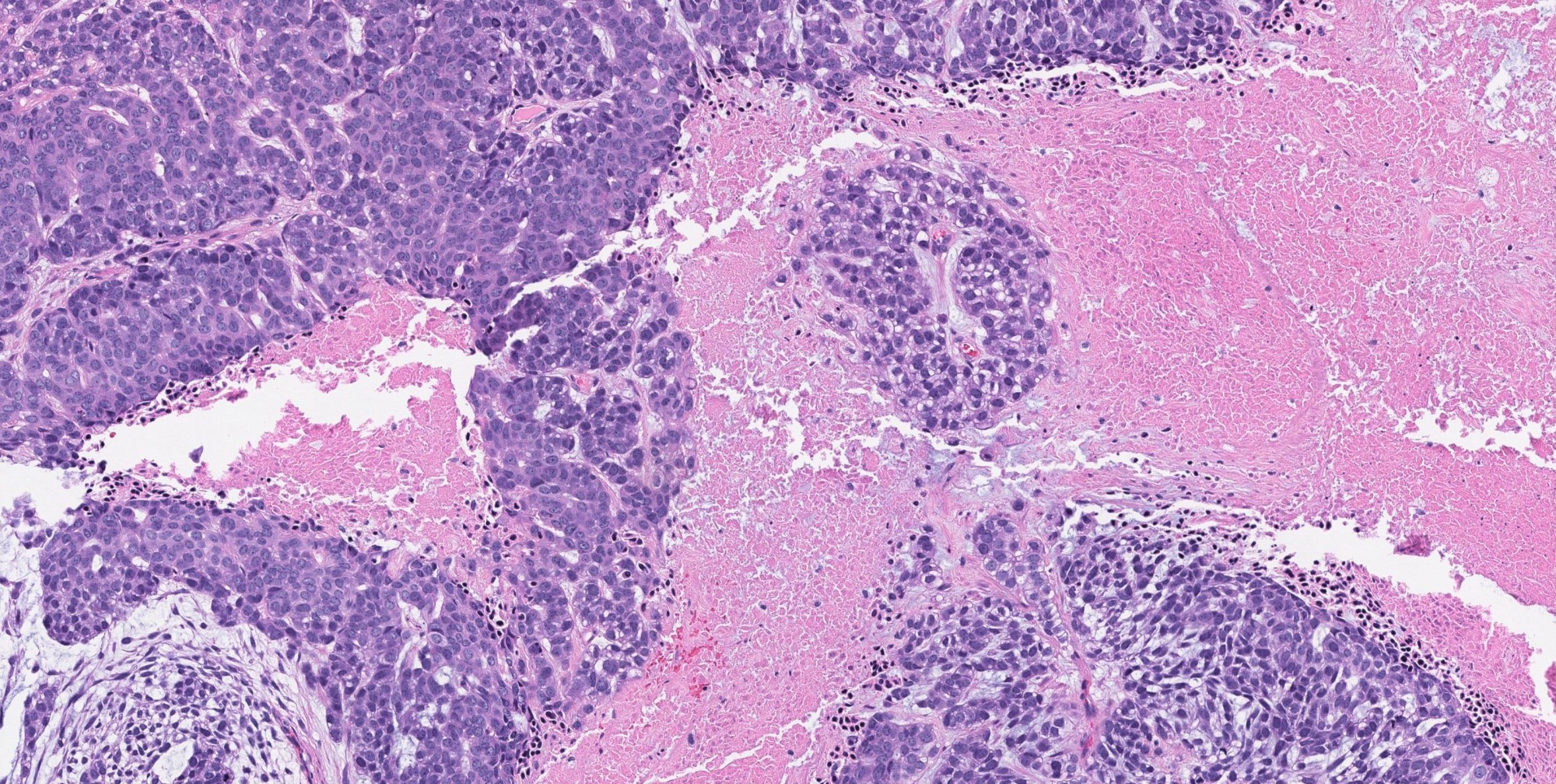
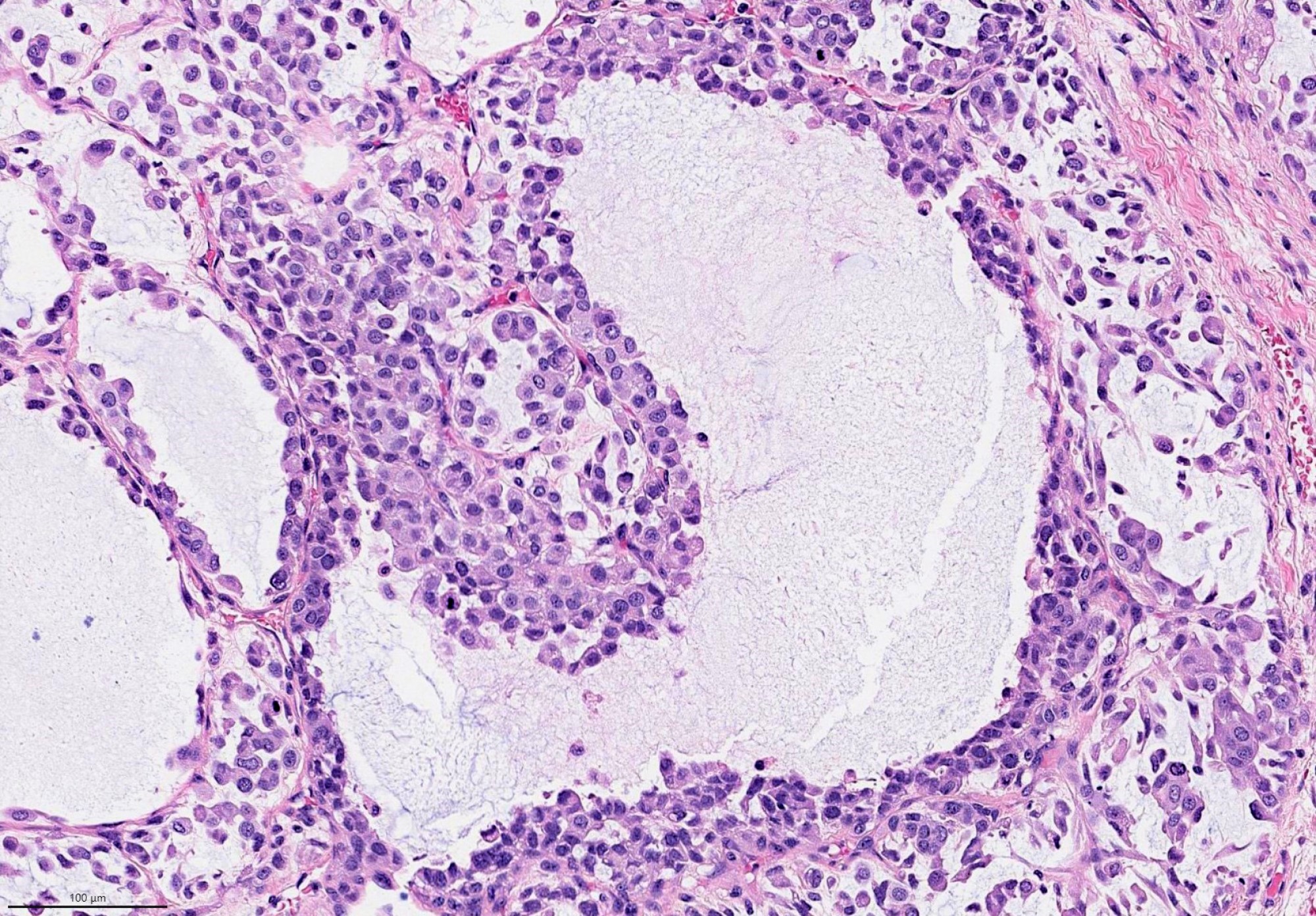
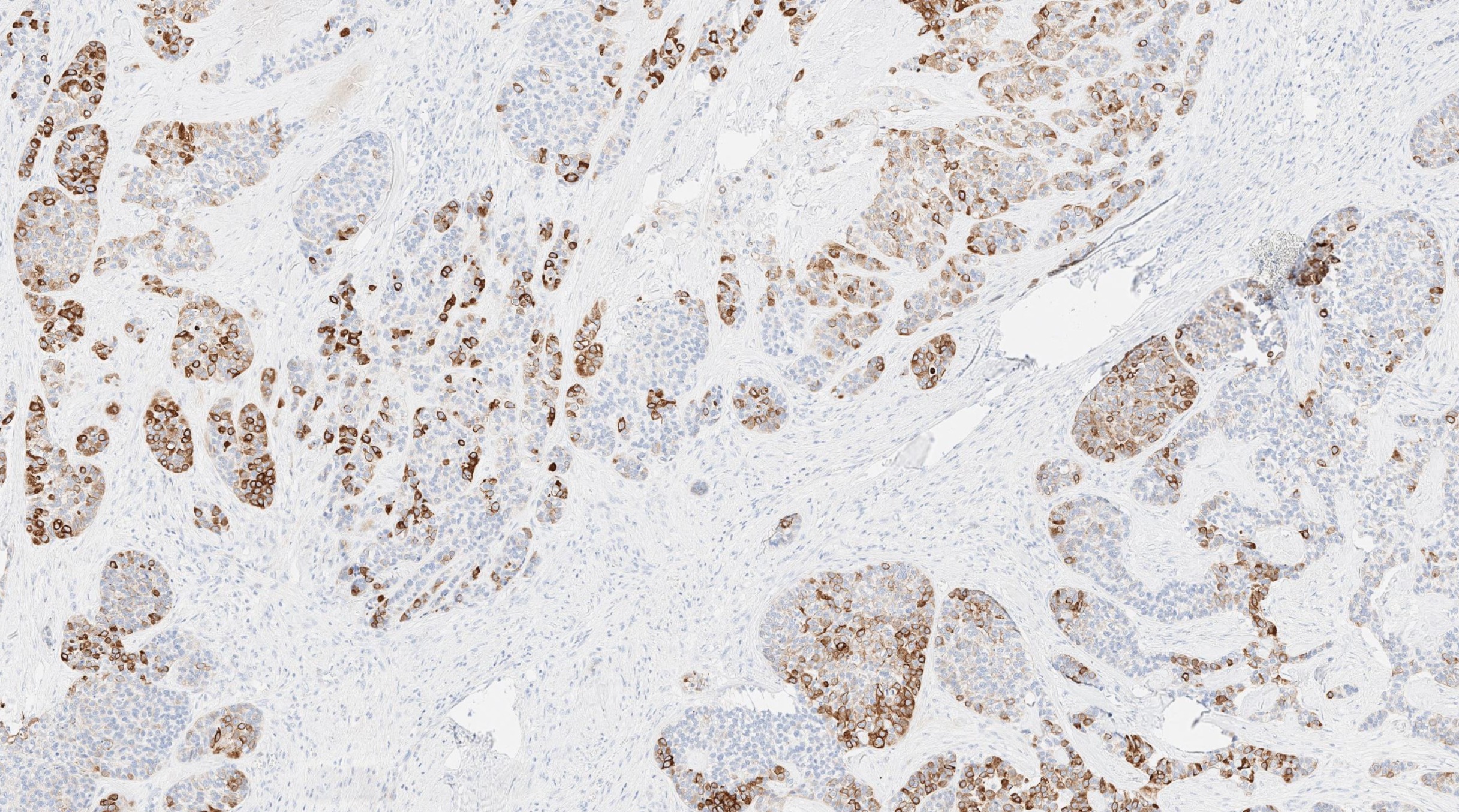
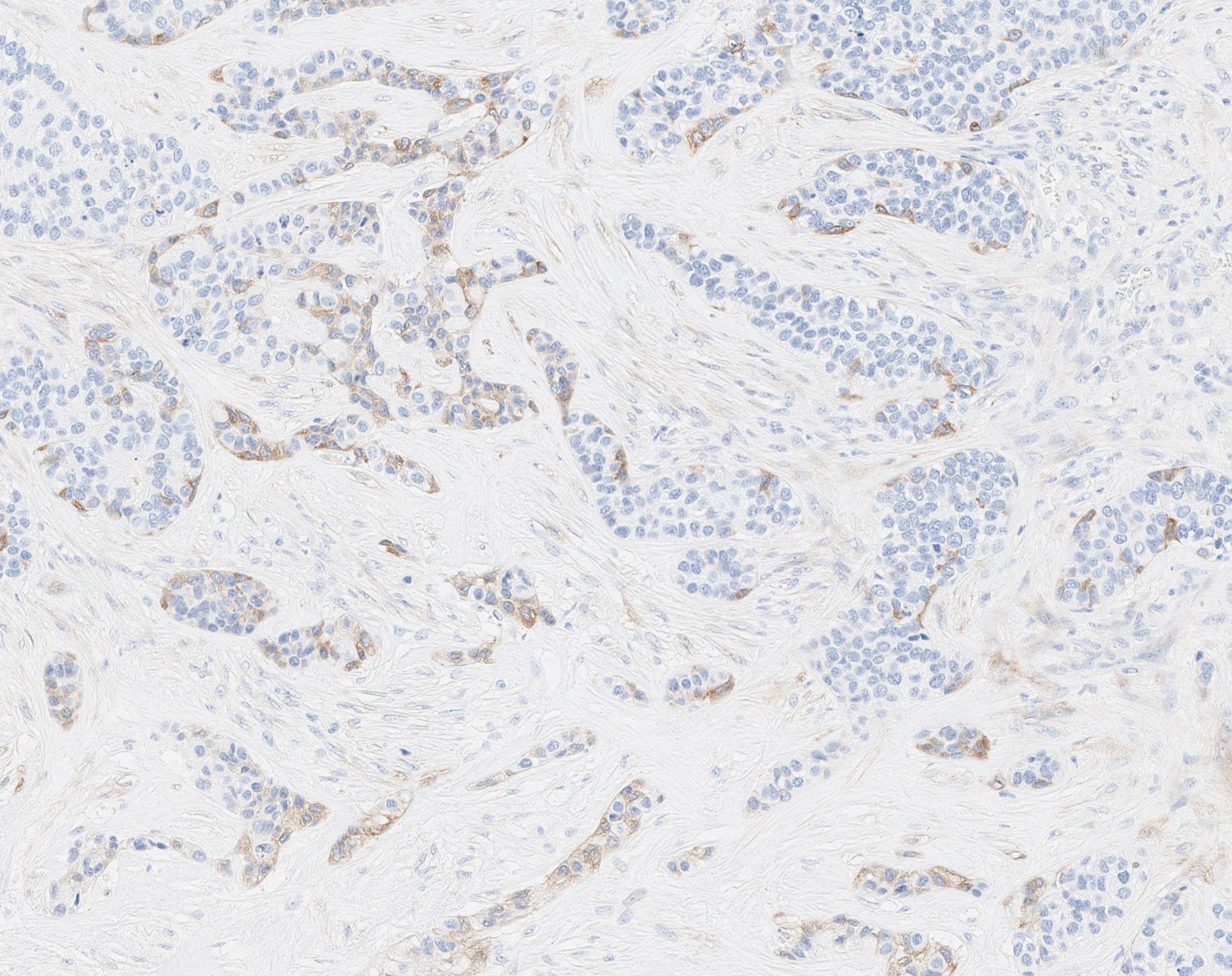
- Invasiveness is typically demonstrated as expansile invasive multinodular growth: myoepithelial carcinoma rarely shows infiltration of single cells / small clusters or desmoplastic reaction
- Nodules often have a hypocellular center with hyalinized stroma or bland necrosis surrounded by a hypercellular peripheral zone
- Tumor necrosis can be seen within the hypercellular central zone of a tumor nodule
- Currently, there is no well defined, widely accepted grading system: presence of tumor necrosis is considered by some as a feature of high grade myoepithelial carcinoma (Am J Surg Pathol 2015;39:931)
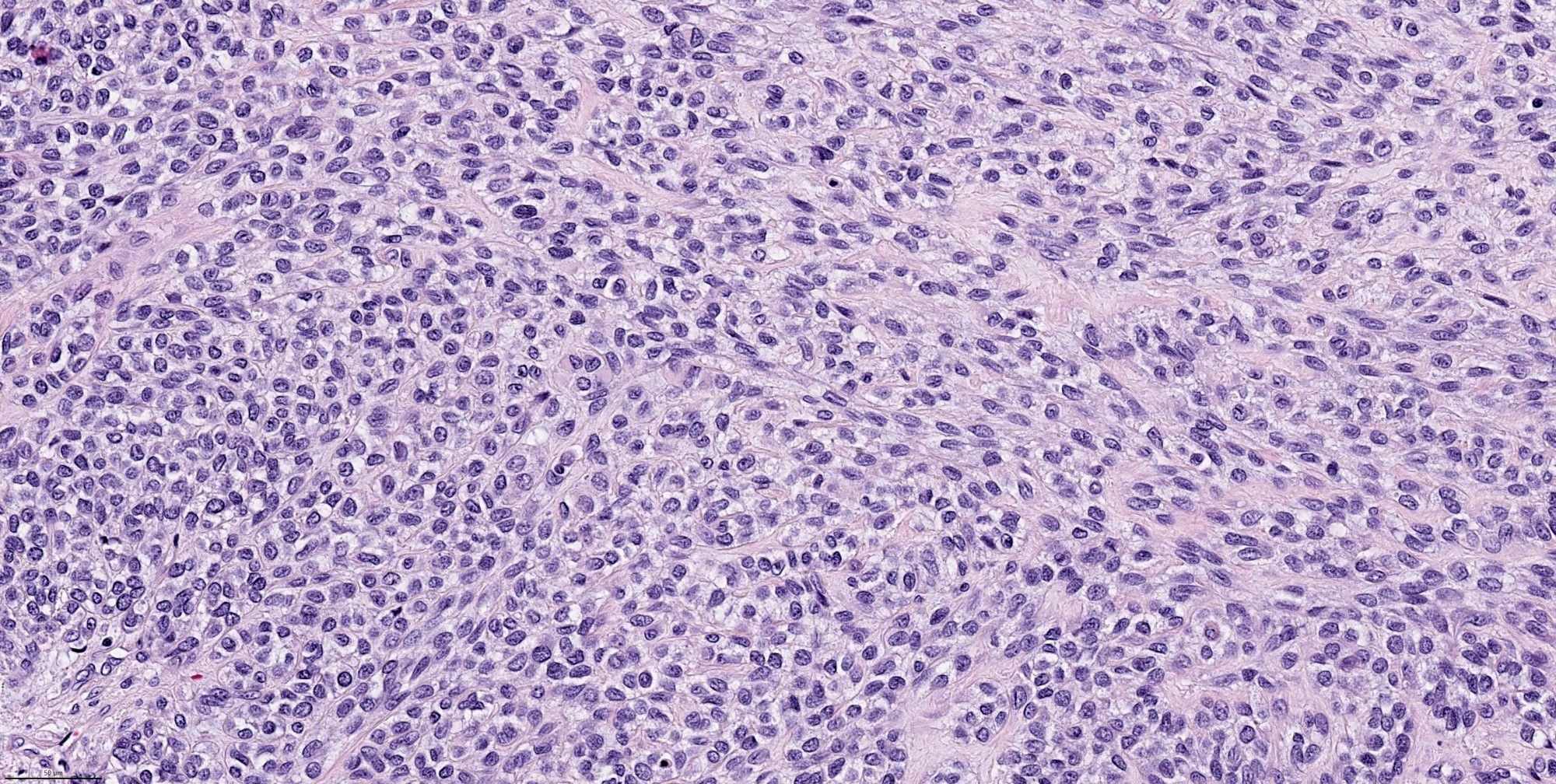
- Composed (near) entirely of myoepithelial cells showing various cytologic features, including clear cell, epithelioid, plasmacytoid or spindle cell morphology
- Hyalinized, myxoid or myxochondroid stroma may be seen in myoepithelial carcinoma de novo and ex PA
- Common architectural patterns include solid, trabeculae, cords, nests and single cells
- Presence of pre-existing / residual pleomorphic adenoma component can be seen in myoepithelial carcinoma ex PA
Microscopic (histologic) images
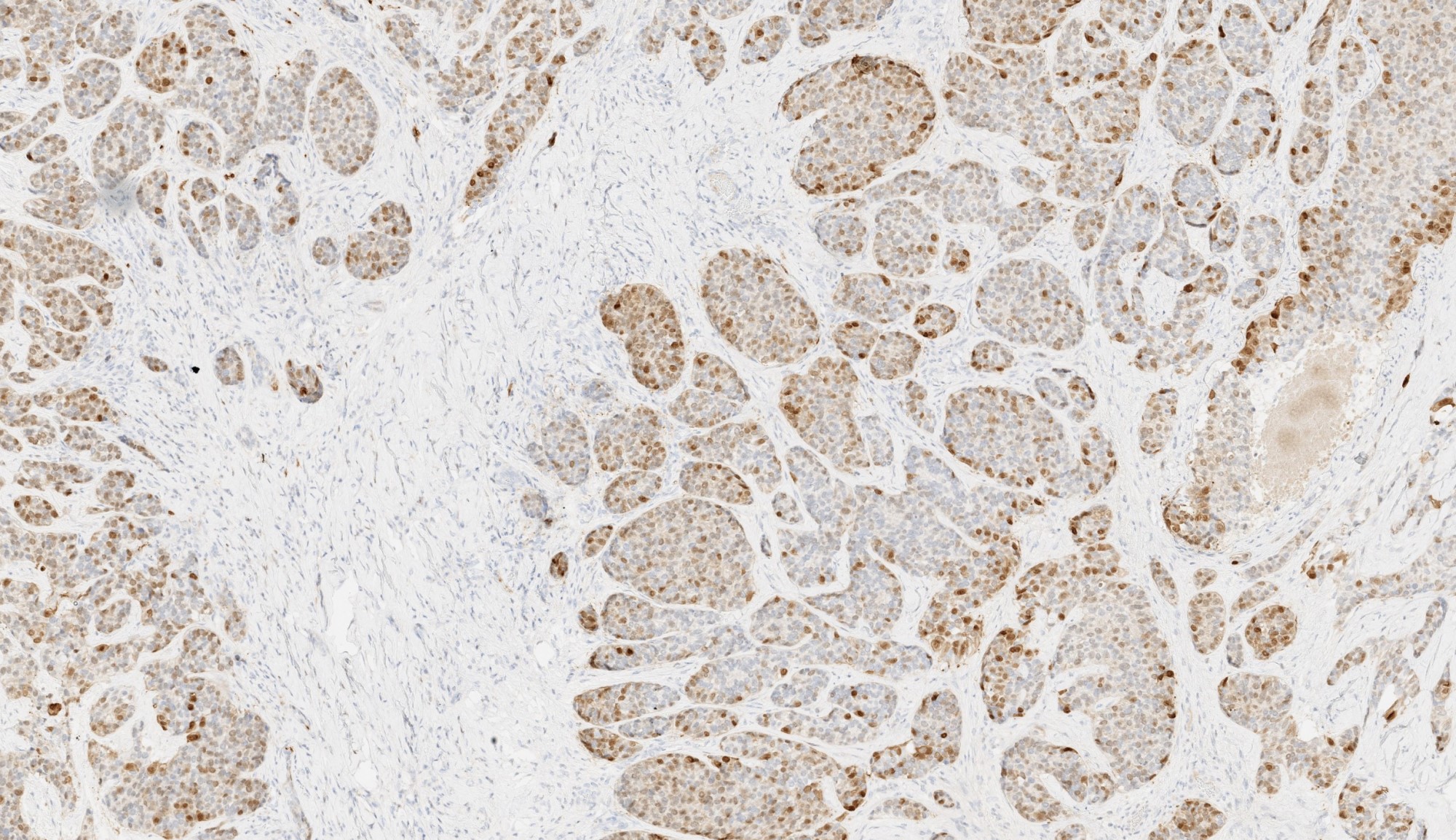
Contributed by Abeer Salama, M.D. and Bin Xu, M.D., Ph.D.
Cytology description
- Hypercellular specimen composed entirely of myoepithelial cells
- Myoepithelial cells shows a mixture of plasmacytoid, epithelioid or spindle morphology arranges as small groups or single cells (Cancer 2002;96:32, Kokyu To Junkan 1985;33:533)
- Scant amount of metachromatic stroma, mitotic figures and nuclear pleomorphism may be present
Positive stains
Negative stains
- Melanocytic markers, such as HMB45 and MelanA (Surg Pathol Clin 2021;14:67)
Molecular / cytogenetics description
- PLAG1 fusion is the most common molecular event, being detected in approximately 50% of myoepithelial carcinoma de novo and ex PA (Nat Commun 2017;8:1197, Am J Surg Pathol 2021;45:1)
- Fusion partners include FGFR1, TGFBR3, ND4 and others
- Clear cell myoepithelial carcinoma may additionally show EWSR1 fusion (Am J Surg Pathol 2015;39:338, Am J Surg Pathol 2021;45:1, Nat Commun 2017;8:1197)
- Despite EWSR1 rearrangements by FISH, corresponding fusion transcripts have not been identified in most cases and the significance is unclear
- Small proportion has HMGA2 fusion (Nat Commun 2017;8:1197)
Sample pathology report
- Parotid gland, left; superficial parotidectomy:
- Myoepithelial carcinoma, high grade, 3.5 cm (see comment and synoptic report)
- Comment: The tumor shows a mitotic index of 8 per 10 high power fields. Tumor necrosis is noted. Immunohistochemistry studies show that the tumor is positive for S100, calponin and CAM5.2, whereas negative for HMB45. The morphologic and immunohistochemical features are most consistent with myoepithelial carcinoma.
Differential diagnosis
- Myoepithelioma:
- Benign counterpart of myoepithelial carcinoma
- Encapsulated without evidence of invasion (being capsular, vascular and perineural)
- Pleomorphic adenoma:
- Similarity:
- Pleomorphic adenoma can be myoepithelial rich and may contain areas with pure myoepithelial cells
- Pleomorphic adenoma may have pseudopod(s) protruding outside of tumor capsule
- Difference:
- Pleomorphic adenoma lacks the multinodular / lobulated invasive growth of myoepithelial carcinoma and contains areas typical of pleomorphic adenoma with ductal, myoepithelial and stromal component
- Similarity:
- Polymorphous adenocarcinoma:
- Both tumors contained one cell type and are positive for S100
- Other myoepithelial markers, e.g. calponin and SMA, are typically negative or very focally positive in polymorphous adenocarcinoma
- Polymorphous adenocarcinoma shows architectural diversity with single filing, trabecular, cribriform, papillary and solid growth pattern, whereas myoepithelial carcinoma usually has cord and solid architecture
- Myxoid stromal component may be seen in polymorphous adenocarcinoma but is usually focal
- Polymorphous adenocarcinoma shows mutations or fusion involving PRKD 1 / PRKD 2 / PRKD 3 genes, whereas myoepithelial carcinoma has frequent PLAG1 fusion
- Myoepithelial tumor of the soft tissue:
- Myoepithelial tumors arising from salivary glands or soft tissue are indistinguishable on histology and immunohistochemistry level (Head Neck Pathol 2020;14:121)
- EWSR1 fusions with POU5F1, PBX1, ZNF444, KLF17 and PBX3 seem restricted to soft tissue myoepithelial tumors (Head Neck Pathol 2020;14:121)
- Radiological correlation is essential to determine the site of origin
Additional references
Practice question #1
Practice answer #1
B. The low power H&E clearly shows invasion, which supports a diagnosis of carcinoma and excludes benign entities, such as pleomorphic adenoma. At high power, the tumor contains one type of tumor cells, which exclude all carcinoma with biphasic patterns (e.g. adenoid cystic carcinoma). The immunohistochemical profile is consistent with myoepithelial phenotype. Therefore, the correct diagnosis is myoepithelial carcinoma.
Comment Here
Reference: Myoepithelial carcinoma
Comment Here
Reference: Myoepithelial carcinoma
Practice question #2
Which of the following statement about the myoepithelial carcinoma of the salivary gland is true?
- It harbors PRKD1 fusion
- It has negligible risk of distant metastasis
- It is biphasic, composed of epithelial (ductal) and myoepithelial elements
- It may arise de novo or ex pleomorphic adenoma
Practice answer #2
D. Myoepithelial carcinoma contains only one cell type (myoepithelial cells) and does not contain epithelial (ductal) cells. PRKD1 fusion is seen in polymorphous adenocarcinoma / cribriform adenocarcinoma. Myoepithelial carcinoma is relatively aggressive, with approximately 20% risk of distant metastasis. It may arise de novo or ex pleomorphic adenoma.
Comment Here
Reference: Myoepithelial carcinoma
Comment Here
Reference: Myoepithelial carcinoma