17 February 2022 - Case of the Month #512
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Drs. Andrii Puzyrenko and Julie Jorns, Medical College of Wisconsin, Milwaukee, Wisconsin, USA for contributing this case and discussion and to Dr. Kristen Muller, Dartmouth Geisel School of Medicine, Lebanon, New Hampshire, USA and Dr. Gary Tozbikian, Ohio State University, Columbus, Ohio, USA for reviewing the discussion.
Case of the Month #512
Clinical history:
A 61 year old woman with silicone breast implants presented with right breast fullness and a large fluid collection around the right breast implant on CT scan.
Radiology and histopathology images:
What is your diagnosis?
Diagnosis: Breast implant associated anaplastic large cell lymphoma (BIA-ALCL)
Test question (answer at the end):
What stains are typically positive in breast implant associated anaplastic large cell lymphoma (BIA-ALCL)?
A. ALK, CD3
B. CD20, EBER
C. CD4, CD30
D. CD43, TCR
Discussion:
Breast implant associated anaplastic large cell lymphoma (BIA-ALCL) is a rare primary breast lymphoma with an incidence of 0.1 to 0.3 per 100,000 women with breast implants (Semin Diagn Pathol 2020;37:57).
Overall, primary breast lymphomas account for less than 2% of all extranodal lymphomas, less than 1% of all non-Hodgkin lymphomas and less than 0.5% of all breast neoplasms. Most primary breast lymphomas are diffuse large B cell lymphomas, comprising approximately 60% of primary breast lymphomas. T cell lymphomas, including BIA-ALCL, represent less than 10% (Am J Surg Pathol 2008;32:1299).
The etiology of BIA-ALCL is unknown but can occur with textured saline and silicone filled breast implants and typically occurs in patients who have long standing implants. Development of BIA-ALCL is likely a complex process involving many factors including bacterial biofilm growth, textured implant surface, chronic inflammation, autoimmune mediated response and germline mutations in the JAK/STAT pathway (Haematologica 2016;101:e387, Mod Pathol 2008;21:455).
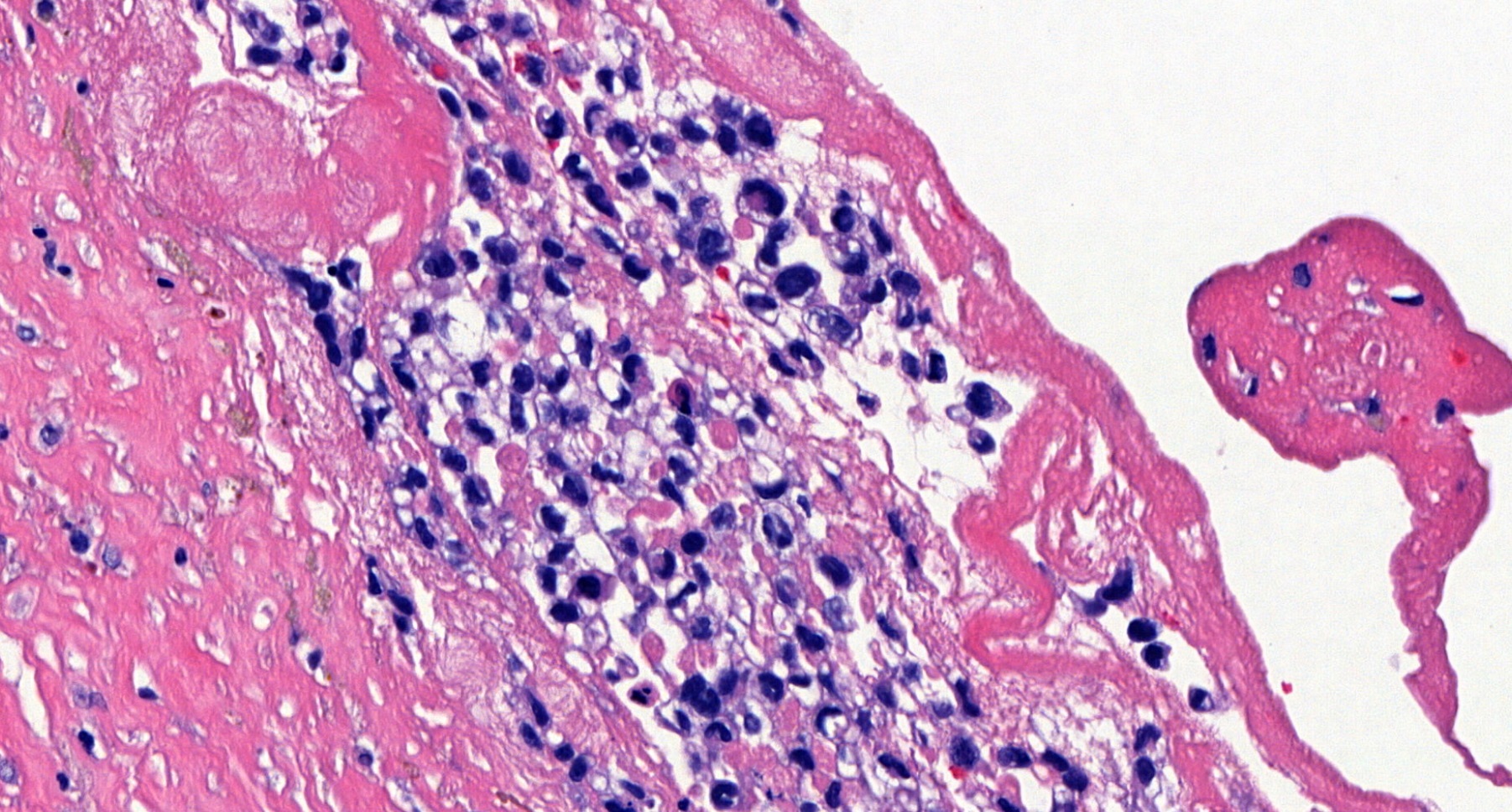
Grossly, BIA-ALCL shows a thickened membranous capsule covered by fibrinoid material and an effusion between the implant and the capsule (J Clin Oncol 2014;32:114).
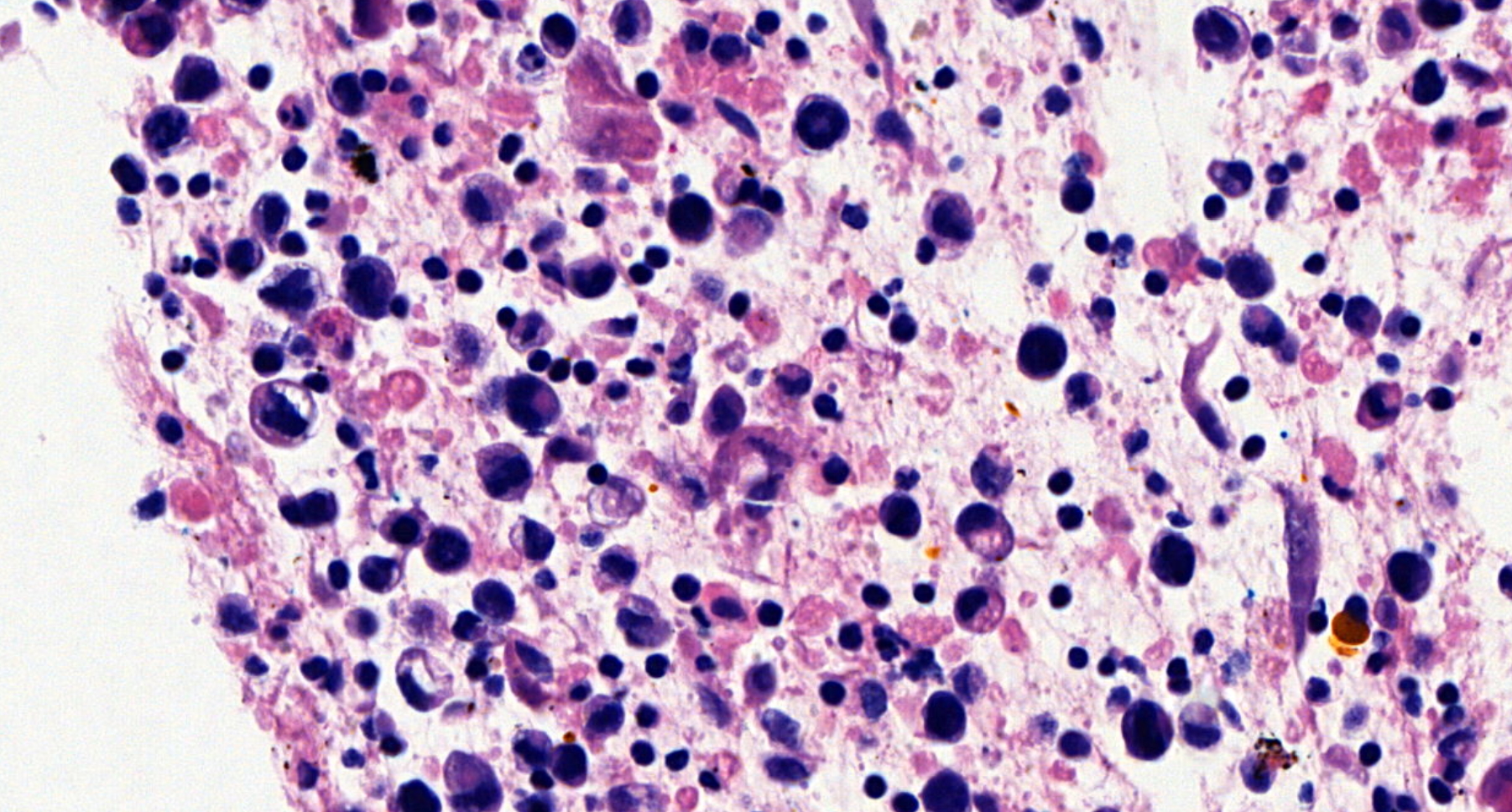
The histological hallmark of BIA-ALCL is large, discohesive lymphoma cells with hyperchromatic nuclei and abundant eosinophilic cytoplasm. The nuclei are large, oval, horseshoe shaped or multilobated, with prominent nucleoli and frequent mitoses. The malignant cells can appear as small clusters within the effusion or as floating clots on the lining of the fibrous capsule, often with extensive necrosis along the luminal side of the capsule (JAMA 2008;300:2030).
Immunohistochemically, BIA-ALCL frequently expresses CD30 (~99%), CD43 (~80%), CD4 (~80%), TIA-1 (~69%), granzyme B (~68%), epithelial membrane antigen (~60%), CD3 (~33%), CD8 (~10%). Most cases of BIA-ALCL are negative for T cell receptors (TCR), anaplastic lymphoma kinase (ALK) and Epstein-Barr virus encoded RNA (EBER) by in situ hybridization. In contrast, systemic ALCL is frequently ALK positive (Mod Pathol 2019;32:166).
Staging is based on spread into or beyond the implant capsule and lymph node involvement. Survival is generally excellent after complete resection of tumor and removal of implants and is much better than in patients with systemic ALCL. Removal of the contralateral implant is often performed due to the risk (up to 4%) of bilateral disease. In patients with positive margins, residual or unresectable disease, radiation is recommended, as is systemic chemotherapy in more advanced stage disease (Aesthet Surg J 2019;39:S3, J Clin Oncol 2016;34:160).
Test question answer:
C. CD4, CD30
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Drs. Andrii Puzyrenko and Julie Jorns, Medical College of Wisconsin, Milwaukee, Wisconsin, USA for contributing this case and discussion and to Dr. Kristen Muller, Dartmouth Geisel School of Medicine, Lebanon, New Hampshire, USA and Dr. Gary Tozbikian, Ohio State University, Columbus, Ohio, USA for reviewing the discussion.
Case of the Month #512
Clinical history:
A 61 year old woman with silicone breast implants presented with right breast fullness and a large fluid collection around the right breast implant on CT scan.
Radiology and histopathology images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Breast implant associated anaplastic large cell lymphoma (BIA-ALCL)
Test question (answer at the end):
What stains are typically positive in breast implant associated anaplastic large cell lymphoma (BIA-ALCL)?
A. ALK, CD3
B. CD20, EBER
C. CD4, CD30
D. CD43, TCR
Discussion:
Breast implant associated anaplastic large cell lymphoma (BIA-ALCL) is a rare primary breast lymphoma with an incidence of 0.1 to 0.3 per 100,000 women with breast implants (Semin Diagn Pathol 2020;37:57).
Overall, primary breast lymphomas account for less than 2% of all extranodal lymphomas, less than 1% of all non-Hodgkin lymphomas and less than 0.5% of all breast neoplasms. Most primary breast lymphomas are diffuse large B cell lymphomas, comprising approximately 60% of primary breast lymphomas. T cell lymphomas, including BIA-ALCL, represent less than 10% (Am J Surg Pathol 2008;32:1299).
The etiology of BIA-ALCL is unknown but can occur with textured saline and silicone filled breast implants and typically occurs in patients who have long standing implants. Development of BIA-ALCL is likely a complex process involving many factors including bacterial biofilm growth, textured implant surface, chronic inflammation, autoimmune mediated response and germline mutations in the JAK/STAT pathway (Haematologica 2016;101:e387, Mod Pathol 2008;21:455).
Grossly, BIA-ALCL shows a thickened membranous capsule covered by fibrinoid material and an effusion between the implant and the capsule (J Clin Oncol 2014;32:114).
The histological hallmark of BIA-ALCL is large, discohesive lymphoma cells with hyperchromatic nuclei and abundant eosinophilic cytoplasm. The nuclei are large, oval, horseshoe shaped or multilobated, with prominent nucleoli and frequent mitoses. The malignant cells can appear as small clusters within the effusion or as floating clots on the lining of the fibrous capsule, often with extensive necrosis along the luminal side of the capsule (JAMA 2008;300:2030).
Immunohistochemically, BIA-ALCL frequently expresses CD30 (~99%), CD43 (~80%), CD4 (~80%), TIA-1 (~69%), granzyme B (~68%), epithelial membrane antigen (~60%), CD3 (~33%), CD8 (~10%). Most cases of BIA-ALCL are negative for T cell receptors (TCR), anaplastic lymphoma kinase (ALK) and Epstein-Barr virus encoded RNA (EBER) by in situ hybridization. In contrast, systemic ALCL is frequently ALK positive (Mod Pathol 2019;32:166).
Staging is based on spread into or beyond the implant capsule and lymph node involvement. Survival is generally excellent after complete resection of tumor and removal of implants and is much better than in patients with systemic ALCL. Removal of the contralateral implant is often performed due to the risk (up to 4%) of bilateral disease. In patients with positive margins, residual or unresectable disease, radiation is recommended, as is systemic chemotherapy in more advanced stage disease (Aesthet Surg J 2019;39:S3, J Clin Oncol 2016;34:160).
Test question answer:
C. CD4, CD30