Table of Contents
Definition / general | Thelarche | Gross anatomy | Breast proper | Stroma | Nipple areolar complex | Diagrams / tables | Gross images | Microscopic (histologic) imagesCite this page: Lategan B. Anatomy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastnormalanatomy.html. Accessed May 6th, 2024.
Definition / general
- Specialized modified skin appendage and defining features of class Mammalia (Wikipedia: Mammal)
- Demonstrates morphologic alteration throughout the reproductive life cycle (menarche, pregnancy, lactation and menopause, in addition to maternal hormonal effects in utero)
- Reference: Mills: Histology for Pathologists, Fourth Edition, 2012
Thelarche
- Rapid growth of breasts at onset of puberty, usually age 10 - 11 in females (Wikipedia: Thelarche, Arch Dis Child 1976;51:170)
- Onset prior to age 8 in girls with normal BMI in general population
- Breast tissue resembles gynecomastia with epithelial hyperplasia in ductal system in a solid or micropapillary configuration (BMC Pediatr 2008;8:27)
- Excision of initial subareolar disc will lead to amastia after puberty
- Associated with increased BMI and non-Hispanic black and Mexican American ethnicity (Pediatrics 2009;123:84)
- May be isolated or part of precocious (central) puberty if other signs of puberty are present
- No tests currently predict risk of progression to precocious puberty in premature thelarche (J Pediatr 2010;156:466)
- Earlier onset of thelarche and longer interval between thelarche and menarche may be associated with increased breast cancer risk (Breast Cancer Res 2014;16:R18)
Tanner staging:
Gross anatomy
- Breast Proper:
- Suspended from anterior chest by ligaments of Cooper (Wikipedia: Cooper's Ligaments) attached to skin and fascia of major and minor pectoral muscles
- Covered by skin and subcutaneous tissue anteriorly
- Spans 2nd rib to 6th rib sacroiliac (SI), midaxillary line to medial border at edge of sternum midline, in addition to axillary tail of Spence (Wikipedia: Tail of Spence), which extends into axilla
- Posterior / deep margin is fascia of pectoralis major muscle
- Breast tissue may extend beyond these limits into adjacent subcutaneous tissue
- In some patients, mastectomy removes most but not all breast epithelial elements, raising possibility of breast disease at these sites
- Accessory breast tissue may be present along the milk line (axilla → anterior chest wall → pubis → upper thighs)
- Accessory / supernumerary nipples but also breast parenchyma
- Both malignant and benign breast disease may arise in these ectopic sites
- Glandular tissue is most abundant in upper outer quadrant of breast; as a result, half of all breast cancers occur here
- Nipple areolar complex:
- Located slightly medial and inferior on breast, level of 4th intercostal on nonpendulous breast
- Cone shaped protuberance, 10 - 12 mm in average height, mean nipple diameter 11 - 13 mm, mean areolar diameter 4 cm
- Montgomery tubercles - areolar protuberances (10 - 20), more prominent during pregnancy; composed of ducts and sebaceous apparatus
- Lymphatic drainage:
- Four major routes => cutaneous, axillary, internal thoracic, posterior intercostal
- Cutaneous
- Superficial plexus within dermis
- Most if not all lymphatics connect to areolar lymphatic plexus (plexus of Sappey)
- Significant for sentinel lymph node procedure, injection in area of nipple will likely identify sentinel nodes, as would injection in region of tumor
- Cutaneous lymphatic anastomoses account for rare cases of metastases to contralateral breast in absence of distant metastases
- Cutaneous lymphatics of inferior breast may drain to epigastric plexus → lymphatic channels of liver and intra-abdominal lymph nodes
- Axilla
- Majority (75%) of drainage
- Initially through 1 - 2 sentinel nodes, first to be involved in 90% of patients with lymph node metastases
- Three levels
- Level I - low axilla
- Level II - mid axilla
- Includes Rotter nodes (interpectoral)
- Level III
- Apical or infraclavicular nodes
- Metastases here portend a worse prognosis
- Intramammary nodes
- May be found anywhere in breast parenchyma
- Considered as axillary lymph nodes for staging purposes
- Only very rarely the sentinel node
- Internal thoracic
- < 10% of lymphatic flow from breast, may be more prominent if lymphatic drainage is obstructed / disrupted due to disease in axilla or previous treatment
- Terminates in internal mammary nodes
- Involvement does not alter treatment in most cases; as a result, rarely sampled when systemic therapy is planned
- Posterior intercostal
- Least important route of drainage
- Supraclavicular nodes
- Are deemed regional nodes for staging purposes
- Metastases to all other lymph nodes, including cervical and contralateral axillary nodes, are classified as distant metastases
- Cutaneous
- References (lymphatics): Ann Surg Oncol 2008;15:863, Hum Pathol 2001;32:178
- Four major routes => cutaneous, axillary, internal thoracic, posterior intercostal
Breast proper
- Epithelial and stromal components; specific lesions arise in each component or may have a dual morphology
- Epithelium
- Large ducts
- Three dimensional arborizing fan shaped system with apex towards the nipple
- Large ducts → segmental ducts → subsegmental ducts → lobules
- Lactiferous sinuses are likely artifactual (J Anat 2005;206:525); this study changed commonly held views of anatomy (Wikipedia: Breast)
- Duct systems are only rarely confined to a single quadrant and may overlap
- Anastomoses may exist between large duct regions
- Involvement of multiple duct systems by DCIS (a clonal proliferation) may be explained as follows
- DICS arising in single large duct system may be present in overlapping quadrants
- DCIS arising in single large duct system may involve adjacent systems through anastomotic connections
- Separate foci of DCIS may arise in different duct systems
- Terminal duct lobular units (TDLU)
- "Functional unit" of breast (lacation)
- Postulated as origin of most epithelial neoplasms (breast or myoepithelial)
- Two types of epithelia: luminal cells and myoeptihelium
Luminal cells ("epithelial cells"):- Innermost layer of bilayered ductolobular system
- Usually express luminal keratins LMWCK, CK7, CK8, CK18, CK19
- May express "basal keratins" HMWCK, CK5 / 6, CK14, CK17 (J Histochem Cytochem 1986;34:869)
- Most express ER-α and or PgR in a heterogeneous pattern at any given time
- Also expresses E-cadherin, mammaglobin and GCDFP-15
- Outer layer resting on basement membrane
- Contractile meshwork partially covering basement membrane, i.e. incomplete on cross section
- Usually expresses "basal" keratins HMWCK, CK5 / 6, CK14, CK17
- Also smooth muscle actin, calponin, smooth muscle myosin heavy chain, in addition to p63, S100, CD10, P-cadherin and mapsin
- Does NOT express ER or PgR
- Loss of myoepithelium usually considered hallmark of invasive process, with the exception of microglandular adenosis, encapsulated papillary carcinoma and solid papillary carcinoma
- Large ducts
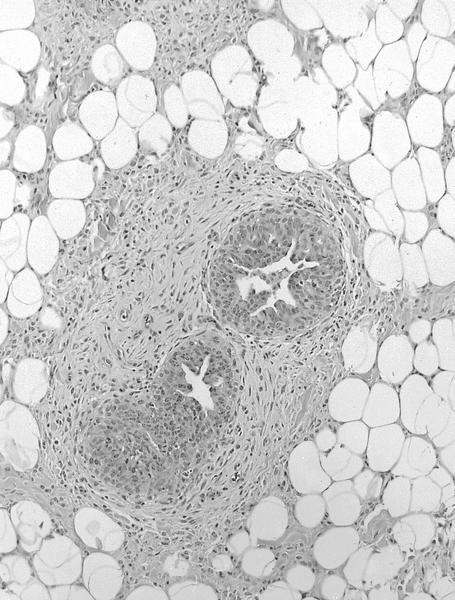
Stroma
- Interlobular
- Surrounds large ducts and TDLUs
- Mature adipose tissue (majority of breast volume), fibroconnective tissue (fibroblasts, myofibroblasts), blood vessels and lymphatics, nerves
- Stromal fat varies throughout reproductive life
- Stromal myofibroblasts
- May express ER and PgR
- Usually also CD34
- Stromal lesions not specific to breast may arise in interlobular stroma, including angiolipoma, angiosarcoma, desmoid fibromatosis, lipoma, myofibroblastoma
- PASH (pseudoangiomatous stromal hyperplasia) is specific to breast
- Intralobular
- Surrounds acini in TDLUs
- Compared to interlobular stroma, looser in appearance or even myxoid
- Often small numbers of inflammatory cells
- Lesions arising here are biphasic involving epithelial and stromal components, including fibroadenoma, phyllodes tumor
Nipple areolar complex
- Ramifying duct system terminating in 15 - 20 major ducts, which open onto areola
- Covered in pigmented skin
- Toker cells
- Cytologically benign cells with clear / pale cytoplasm
- Immunoprofile similar to luminal epithelial cells
- Are most abundant adjacent to duct orifices
- Must distinguish from mammary Paget disease (DCIS involving nipple)
- Keratin producing squamous cells extend into proximal 1 - 2 mm of large ducts
- Squamous metaplasia of lactiferous ducts (SMOLD) is extension of squamous epithelium beyond proximal 1 - 2 mm; associated with smoking
- Keratin entrapment may cause epidermal inclusions and abscess formation with marked inflammatory response
- Basement membrane of ducts and duct lobular system is contiguous with that of skin
- Tumor cells may extend onto skin from DCIS without crossing basement membrane (Paget disease)
- External shape / size of the breast is not predictive of internal anatomy or its lactation potential
- References (nipple): Breast Cancer Res Treat 2007;106:171, Eur Surg Res 2006;38:545, Cancer 2004;101:1947, Aesthetic Plast Surg 2009;33:295, Am J Surg 2007;194:433, Arch Pathol Lab Med 1982;106:60
Diagrams / tables