Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1Cite this page: Yoshikawa A. Hypersensitivity pneumonitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/lungnontumorextrinsicallergic.html. Accessed September 14th, 2025.
Definition / general
- Also known as extrinsic allergic alveolitis
- A complex health syndrome of varying intensity, clinical presentation and natural history
- Due to immunologically induced inflammation of lung parenchyma in response to inhalation of a large variety of antigens (Am J Respir Crit Care Med 2005;171:792)
Essential features
- An interstitial pneumonia with acute to chronic respiratory failure caused by inhalation exposure to a variety of natural or chemical antigens
- Histologically characterized by airway centered inflammation with fibrosis and poorly formed nonnecrotizing granulomas
Terminology
- Also called extrinsic allergic alveolitis
ICD coding
- J67.8
Epidemiology
- 4 - 15% of interstitial lung diseases (Eur Respir J Suppl 2001;32:114s)
- Prevalence and incidence vary by climate, geographical condition, living environment and agricultural practice
- UK incidence is 0.9 per 100,000 person per year (QJM 2007;100:233)
- Higher prevalence and mortality rate in farmers and agricultural industries (Am J Ind Med 2006;49:997)
- Mean age is 50 - 60 years old
- No sexual predominance
- Smoking is related to lower prevalence but worse prognosis (Intern Med 1995;34:966)
Sites
- Predominant in middle to upper lobes of the lung; usually bilateral
Pathophysiology
- Gene polymorphisms related to the acquired immune response may predispose to HP (Am J Respir Crit Care Med 2012;186:314):
- Major histocompatibility complex class 2 (MHC class II)
- Proteasome subunit beta type 8 (PSMB8)
- Transporter associated with Antigen Processing 1 (TAP1)
- Malfunction of regulatory T cells (Eur Respir J 2011;37:632)
- Antigen exposure results in early formation of type III immune complexes, followed by type IV delayed hypersensitivity
Etiology
- HP is developed through inhalation and exposure to a causative antigen
- Causative agents: spores of bacteria, fungi, mycobacteria, animal proteins and chemicals from hay, grain, sugar cane, bark, cheese, cork and animal feces (J Investig Allergol Clin Immunol 2015;25:237)
- According to the causative antigen, HP may have different names:
- Air conditioner lung: due to thermophilic bacteria
- Byssinosis: in textile workers due to fibers from cotton, linen and hemp
- Resembles asthma clinically
- Disease mechanism may not be immune mediated, endotoxin from bacterial contamination of cotton may play a role
- Farmer's lung: from moldy hay containing spores of thermophilic actinomycetes
- Maple bark stripper’s lung: fungal spores
- Pigeon breeder's lung: also called bird fancier's disease; proteins from serum, feathers excreta
- Hot tub lung: nontuberculous Mycobacterium
Clinical features
- HP is classified into acute, subacute and chronic, however there is a lack of consensus for the criteria
- Acute hypersensitivity pneumonitis
- Influenza-like syndrome a few hours after exposure to an antigen: fever, dyspnea, cough, crackles may be detected on chest auscultation
- Symptoms resolve several hours after antigen removal
- Repeated acute episodes of farmer’s lung leads to centriacinar emphysema (Eur Radiol 2003;13:2212)
- Subacute hypersensitivity pneumonitis
- Slowly progressive respiratory failure over weeks to months
- Fever, dyspnea, cough, fatigue, crackles may be detected on chest auscultation
- Pulmonary function may be normal
- Probably results from continuous low level exposure to the antigen
- Chronic hypersensitivity pneumonitis
- Slowly progressive and insidious respiratory failure; often without acute episodes
- Dyspnea, cough, fatigue, weight loss, fine crackles on chest auscultation
- Restrictive pattern on pulmonary function tests
- Decreased total lung capacity (TLC)
- Decreased forced vital capacity (FVC)
- Decreased diffusing capacity of the lung for carbon monoxide (DLCO)
- Often associated with bird antigen exposure
- Acute exacerbation followed by respiratory deterioration within 1 - 2 months can occur; usually without further antigen exposure (Chest 2008;134:844, Chest 2008;134:1265)
Diagnosis
- Diagnosis is based on clinical, radiological (high resolution computed tomography, HRCT) and pathological examination
- Surgical lung biopsy is often necessary to differentiate subacute and chronic hypersensitivity pneumonitis from other interstitial lung disease; however, it is rare for acute hypersensitivity pneumonitis to be biopsied
- Although several diagnostic criteria have been proposed, none are widely accepted
- A large cohort study by HP Study Group suggested clinical predictors for the diagnosis of HP (Am J Respir Crit Care Med 2003;168:952)
- Exposure to a known offending antigen
- Positive precipitating antibodies
- Recurrent episodes of symptoms
- Inspiratory crackles
- Symptoms 4 - 8 hours after exposure
- Weight loss
- Bronchoalveolar lavage is supportive in the diagnosis but lacks standardization (Chest 2012;142:208, Am J Respir Crit Care Med 2012;186:314)
- Increased total cell count
- Increased lymphocyte percentage ≥ 30% for nonsmokers or exsmokers or ≥ 20% for current smokers; a normal lavage rules out the presence of active HP (Am Rev Respir Dis 1990;141:S169, Br J Ind Med 1986;43:401)
- CD4 / CD8 ratiois usually decreased in HP but can be increased as high as in sarcoidosis; CD4 / CD8 ratio is now considered to vary by clinical conditions such as causative antigen and smoking status
- Inhalation challenge is supportive but lacks standardization (Chest 2012;142:208, Am J Respir Crit Care Med 2012;186:314, Eur Respir J 2014;44:1658)
- Antigen exposure at the workplace or home or direct inhalation of the specific antigen after a period of avoidance provokes symptoms of HP and decreases FVC in 8 - 12 hours
- The patient should be monitored at least for 24 hours after the inhalation in case of severe attack of HP
Laboratory
- Serum IgG antibody to causative antigens may be increased; however, serum antibody could be positive in 31% of non HP subjects (Am J Respir Crit Care Med 2003;168:952)
- Avian antigens: pigeon, parakeet, budgerigar, chicken
- Fungus: trichosporon, aspergillus
- Bacteria: actinomycete
- Mycobacteria: Mycobacterium avium-intracellulare
- Chemicals
- Increased serum KL-6, often over 1000 IU (normal limit is < 500 IU)
Radiology description
- Findings on the chest X-ray vary from nonspecific change, especially in acute and subacute hypersensitivity pneumonitis, to upper lobe predominant fibrosis of chronic HP
- Typically, HRCT shows ground glass opacity and centrilobular nodular opacity with / without emphysema and fibrosis
- It is often challenging to differential HP from other interstitial lung diseases on HRCT such as nonspecific interstitial pneumonia (NSIP) and usual interstitial pneumonia (UIP) (Am J Surg Pathol 1994;18:136, AJR Am J Roentgenol 1995;165:807)
- HRCT features to differentiate chronic HP from NSIP and UIP (Radiology 2008;246:288):
- Lobular areas with decreased attenuation and vascularity
- Centrilobular nodules
- Absence of lower zone predominance of abnormalities
Radiology images
Prognostic factors
- Many patients show favorable prognosis compared to other interstitial lung diseases and improve with appropriate treatment (QJM 2007;100:233, Respir Med 2014;108:793, Am J Ind Med 2006;49:997)
- Interstitial fibrosis and emphysema are associated with worse prognosis, and once developed, may remain or progress despite treatment (Am J Med 2004;116:662, Radiology 2007;244:591)
- Smoking is also associated with worse prognosis (Intern Med 1995;34:966)
Case reports
- 12 year old boy with HP due to feather duvet (BMJ Case Rep 2015 Jun 25;2015)
- 30 year old woman with HP (Chest 2014;145:856)
- 37 year old man with HP due to shiitake mushroom spores (Med Mycol 2012;50:654)
- 37 year old man who died of HP due to Fusarium vasinfectum (Int Arch Allergy Immunol 2015;166:150)
- 45 year old man with HP due to metalworking fluid (Occup Med (Lond) 2015;65:598)
- 45 year old man with pneumomediastinum as a primary manifestation of chronic HP (Med Sci Monit 2011;17:CS152)
- 72 year old woman with HP and combined pulmonary fibrosis and emphysema (BMJ Case Rep 2015 Dec 21;2015)
Treatment
- Avoidance of antigen is the key of HP management
- Oral or systemic corticosteroids are considered for severe case or when the antigen is not removable; however, steroids do not change long term outcome and are not standardized (Chest 2013;144:1644)
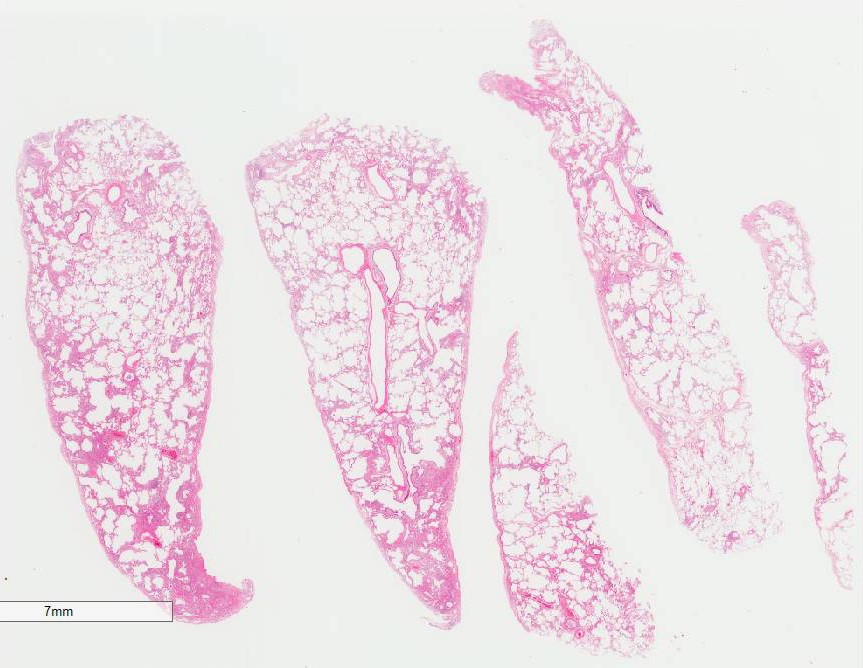
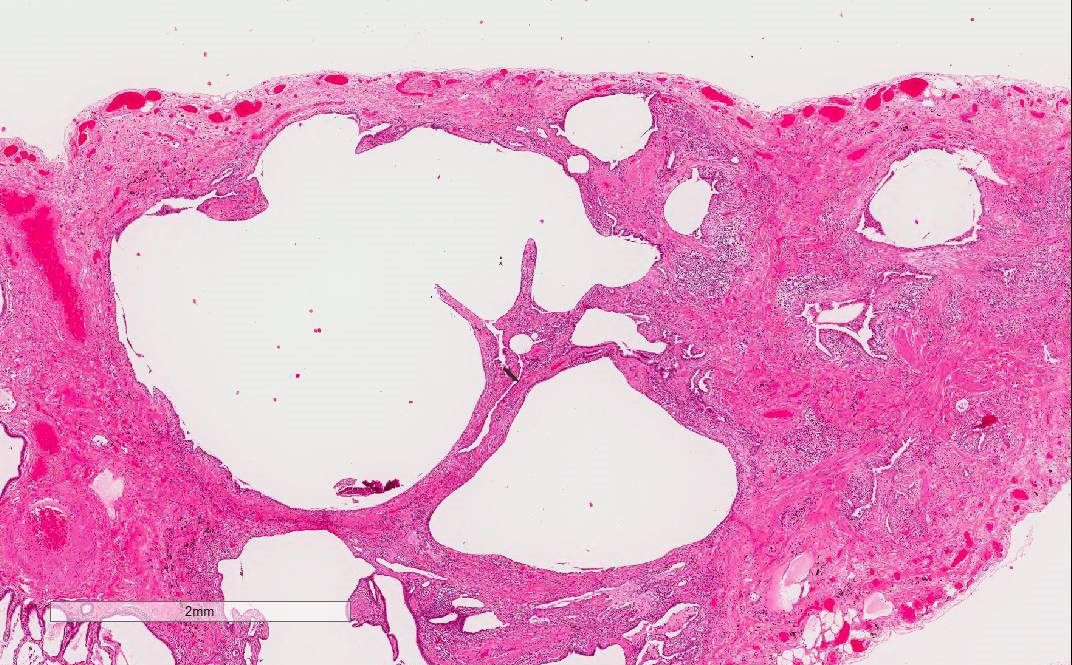
Gross description
- Diffuse involvement with mild to moderate increase in lung weight
- Bronchocentric fibrotic changes may be seen
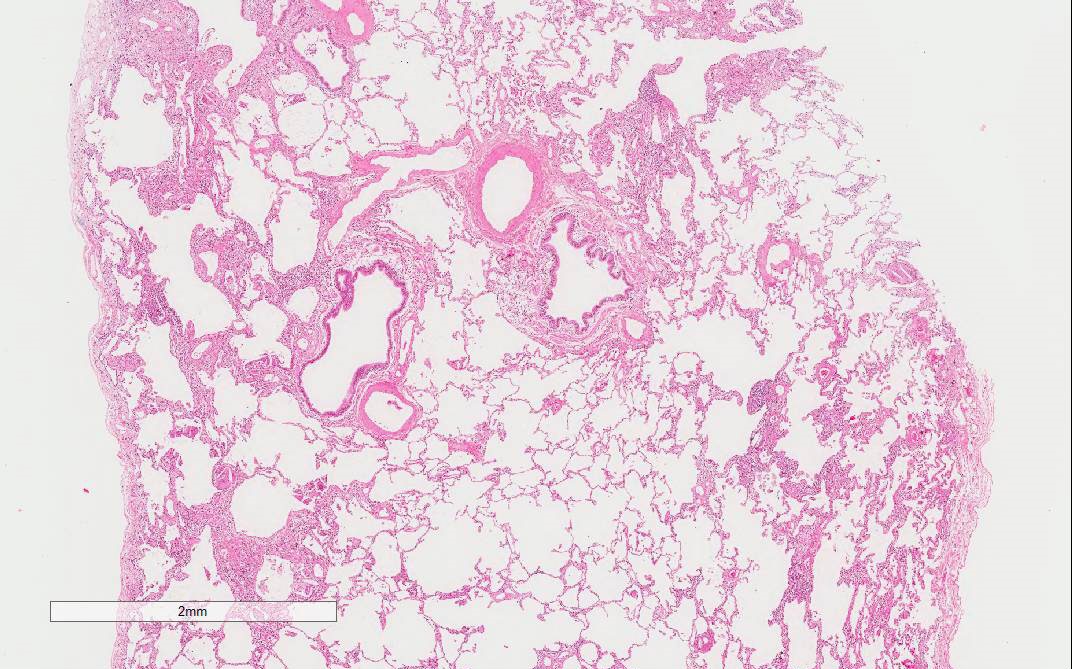
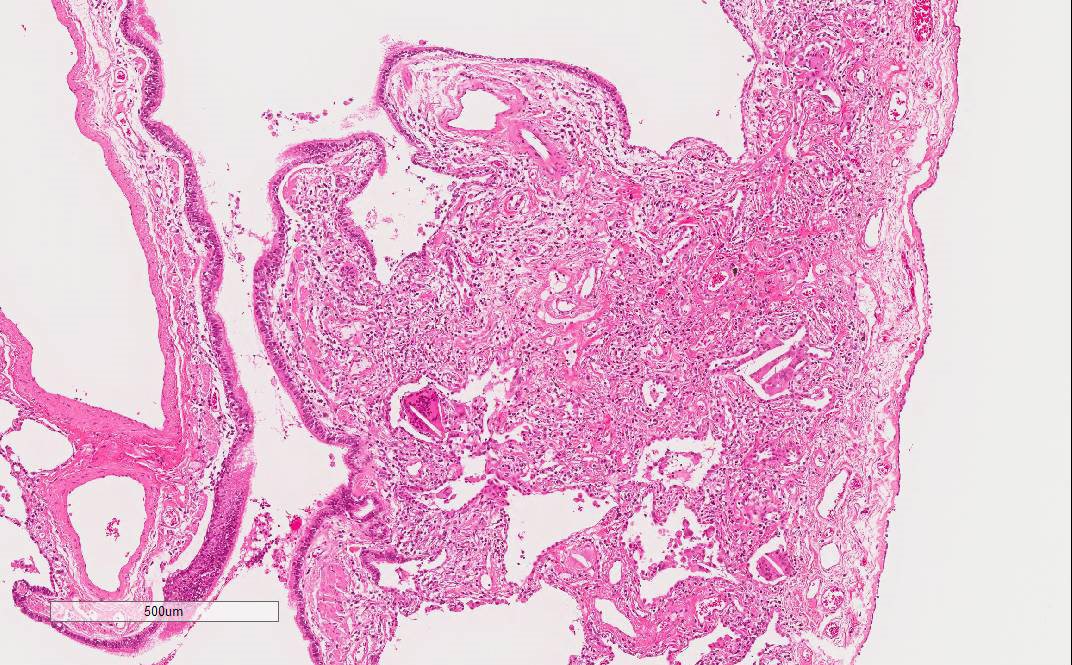
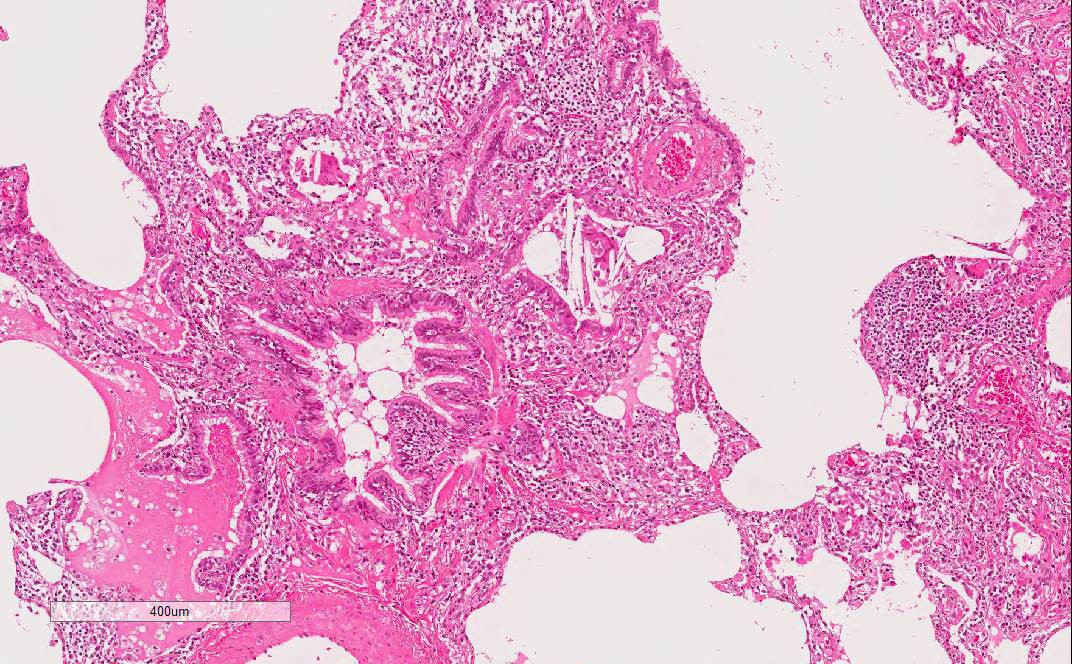
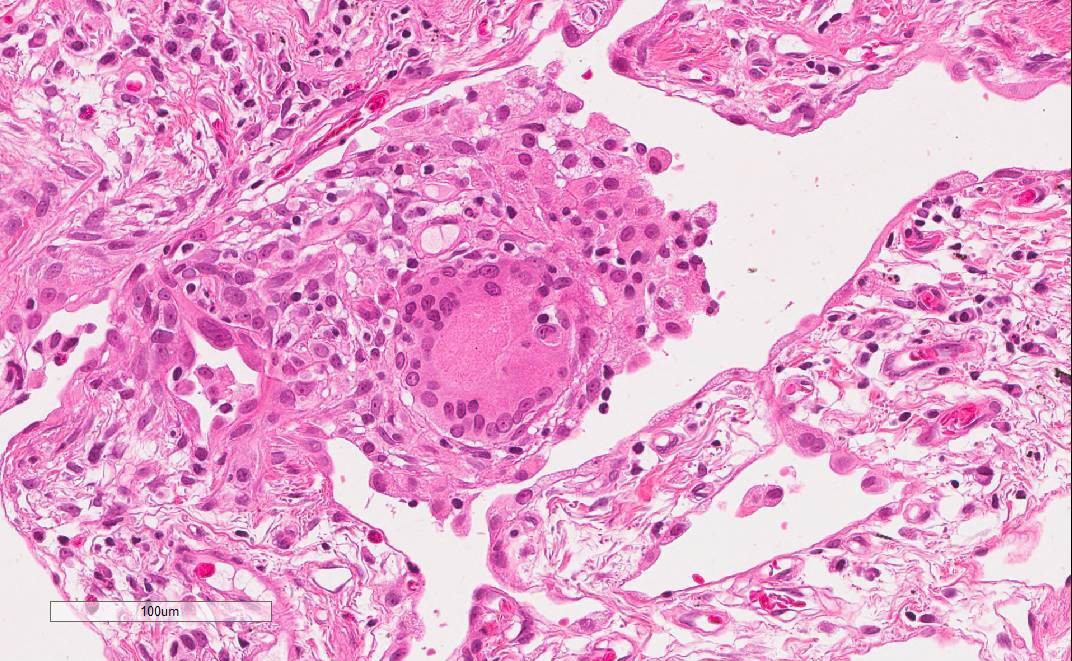
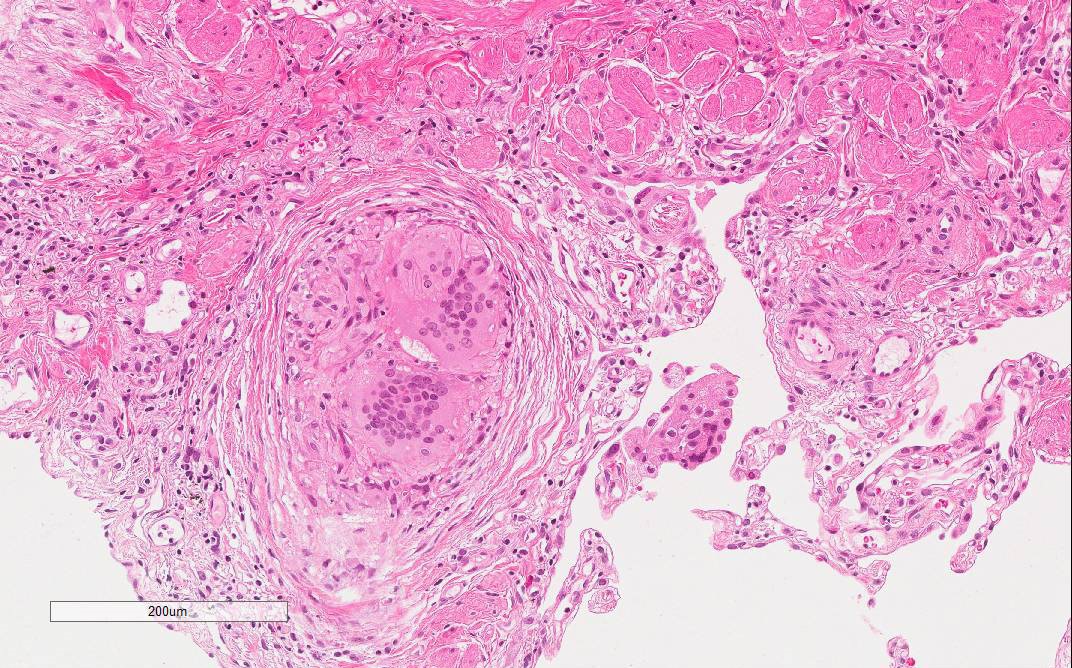
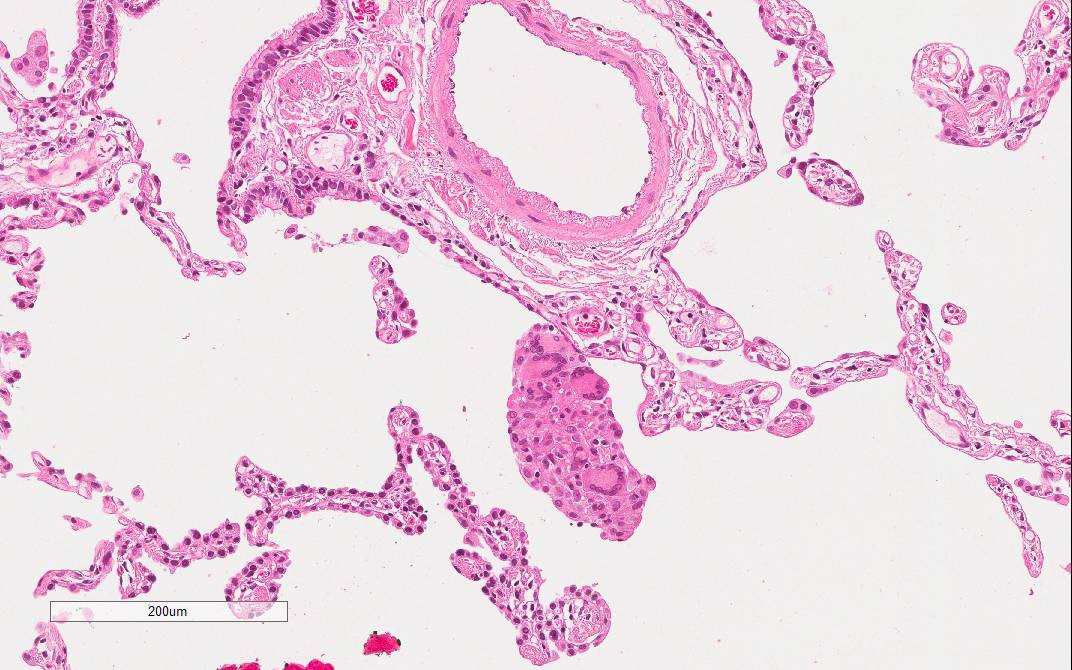
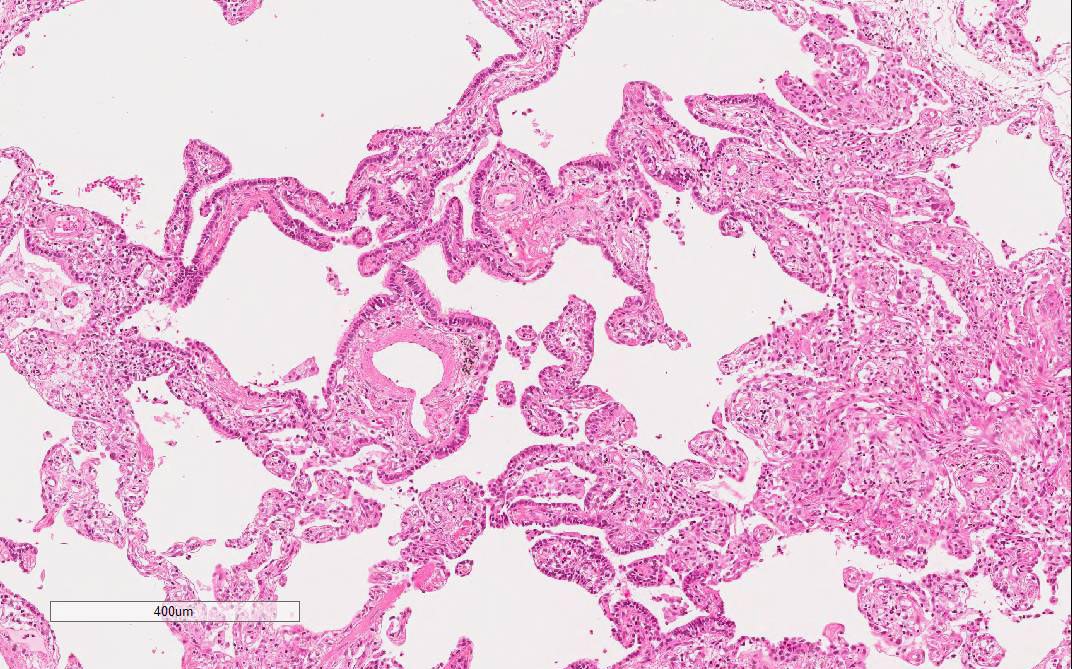
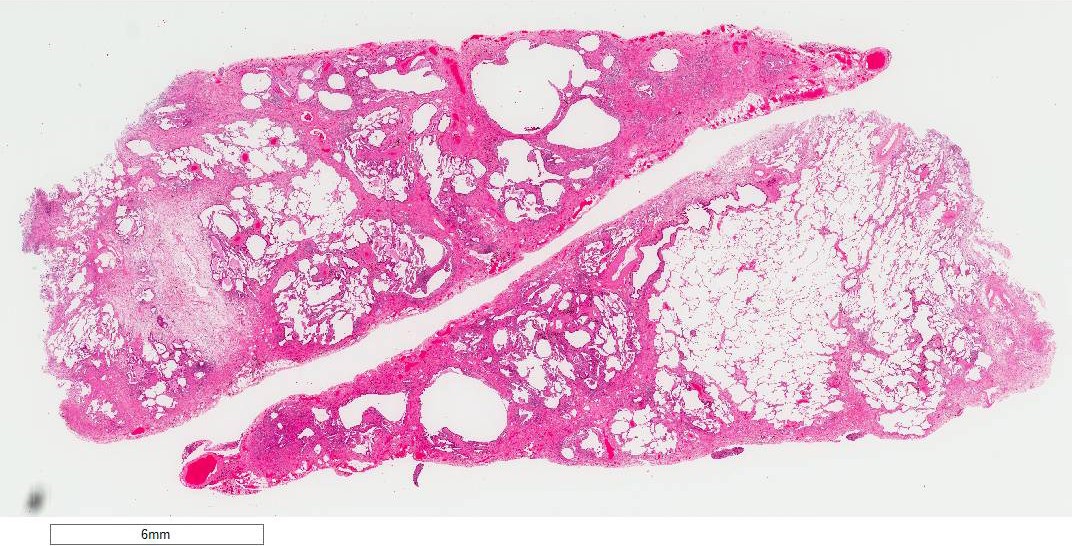
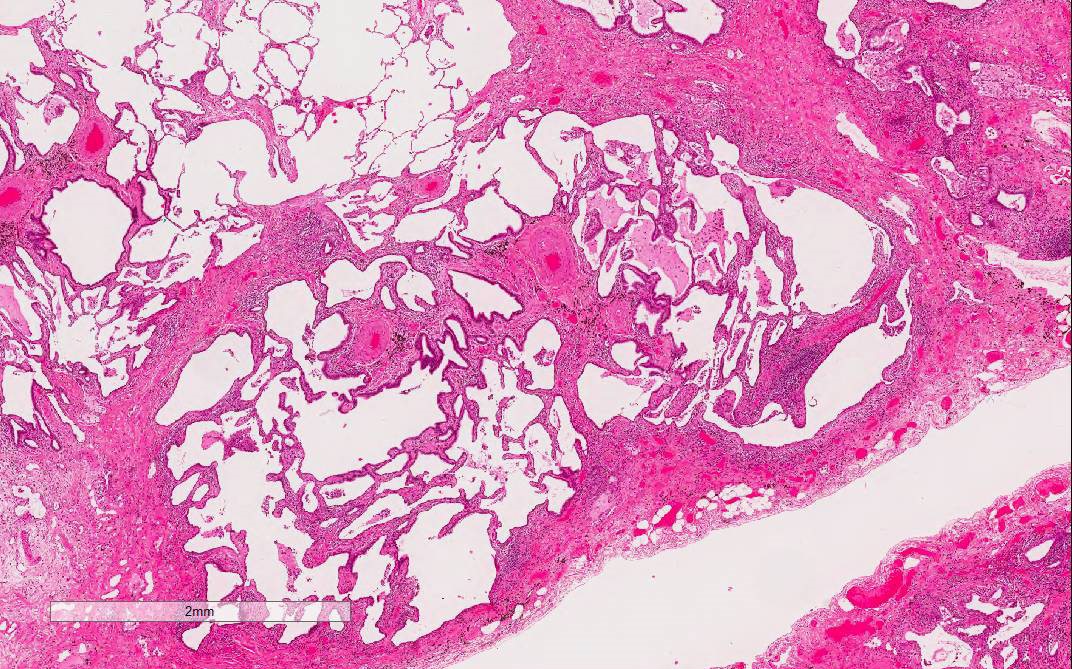
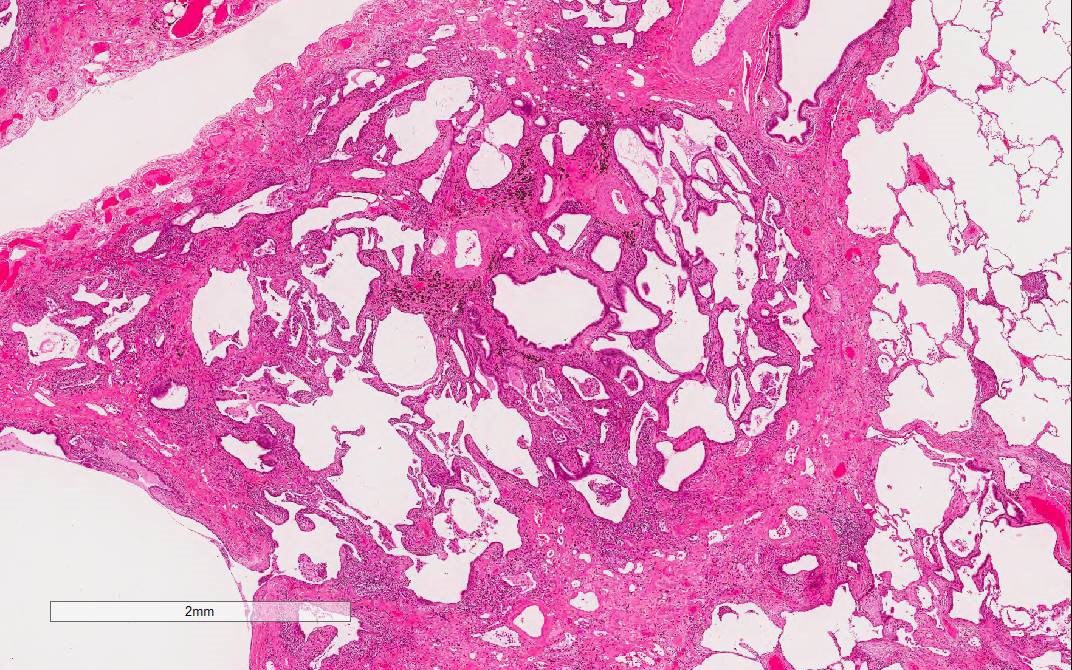
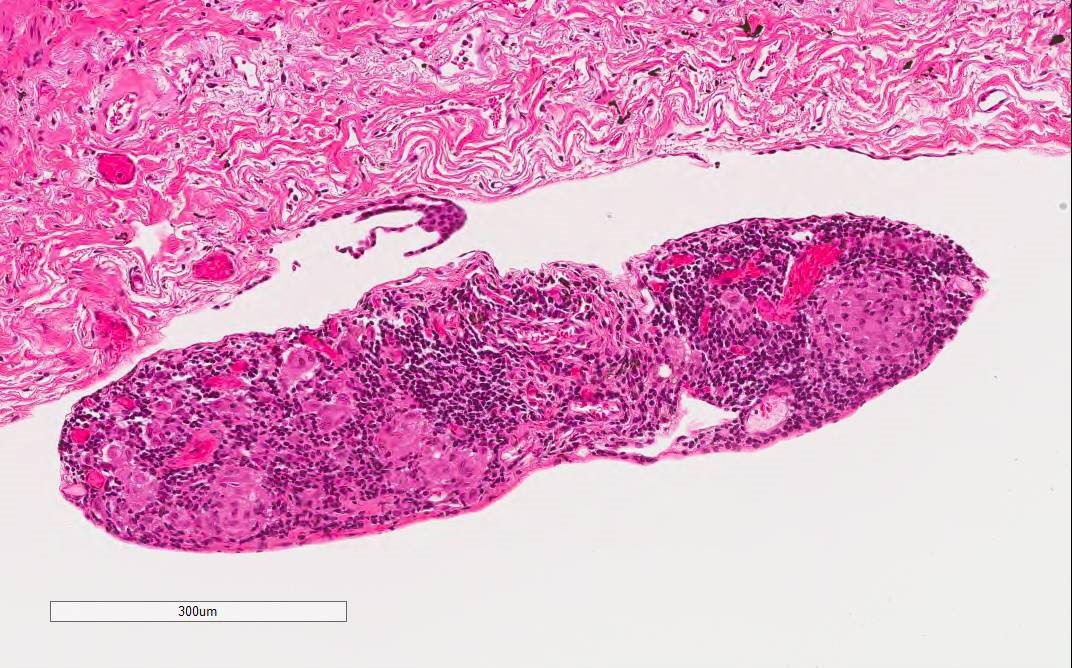
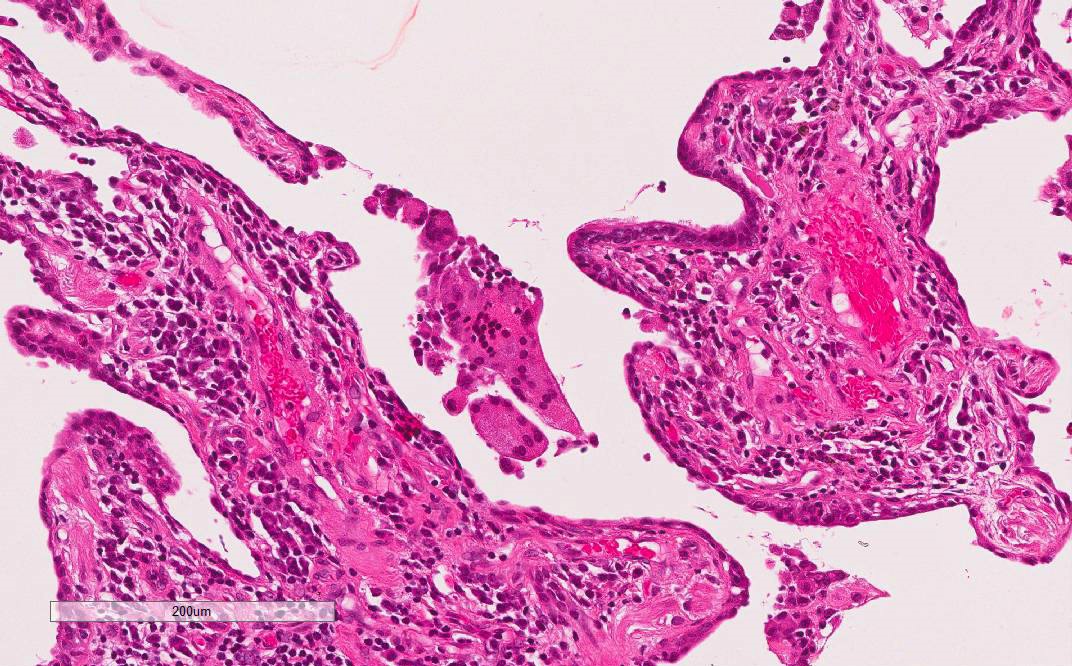
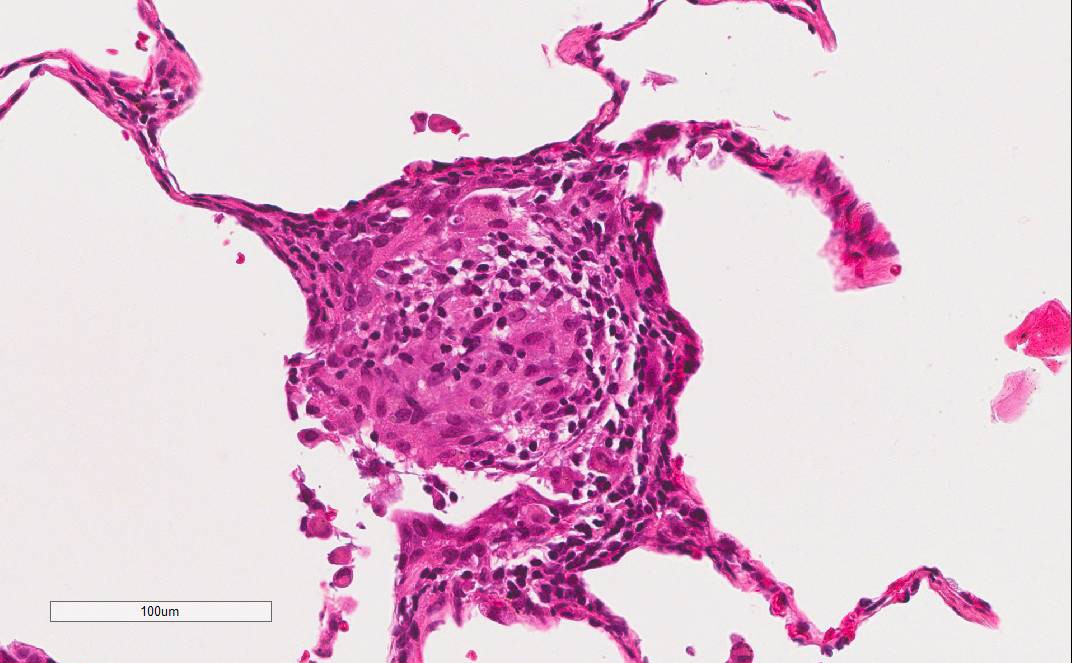
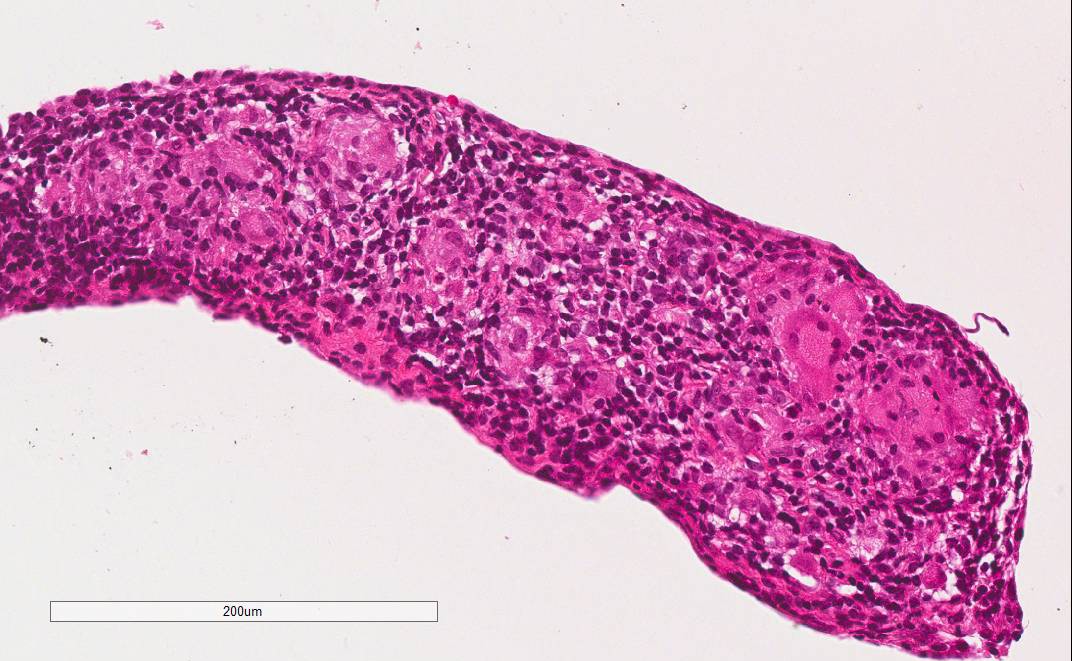
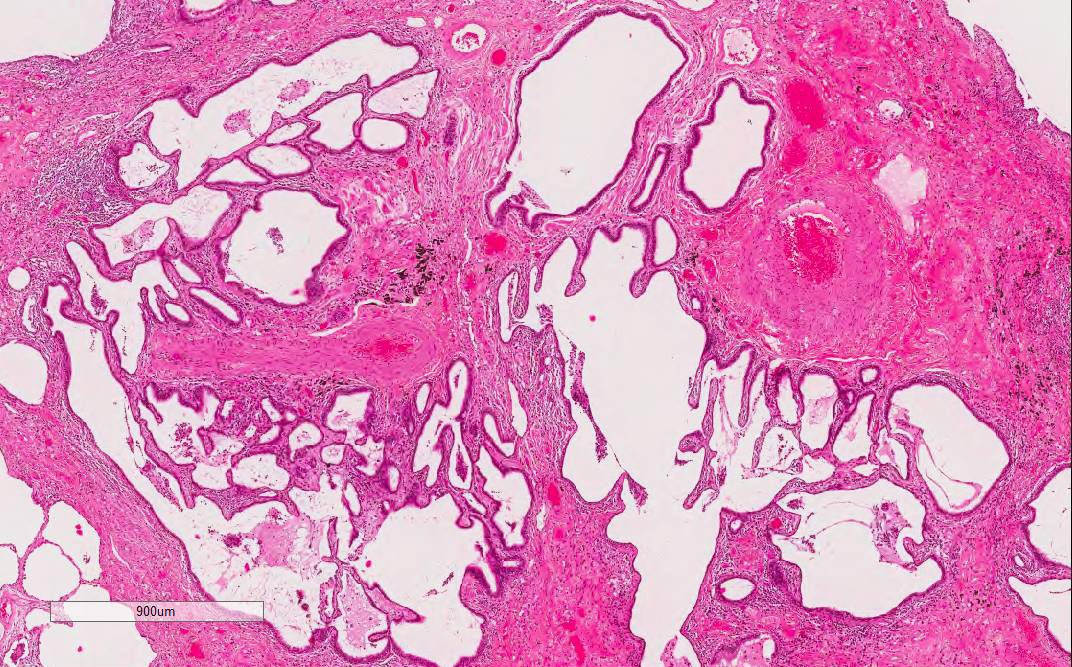
Microscopic (histologic) description
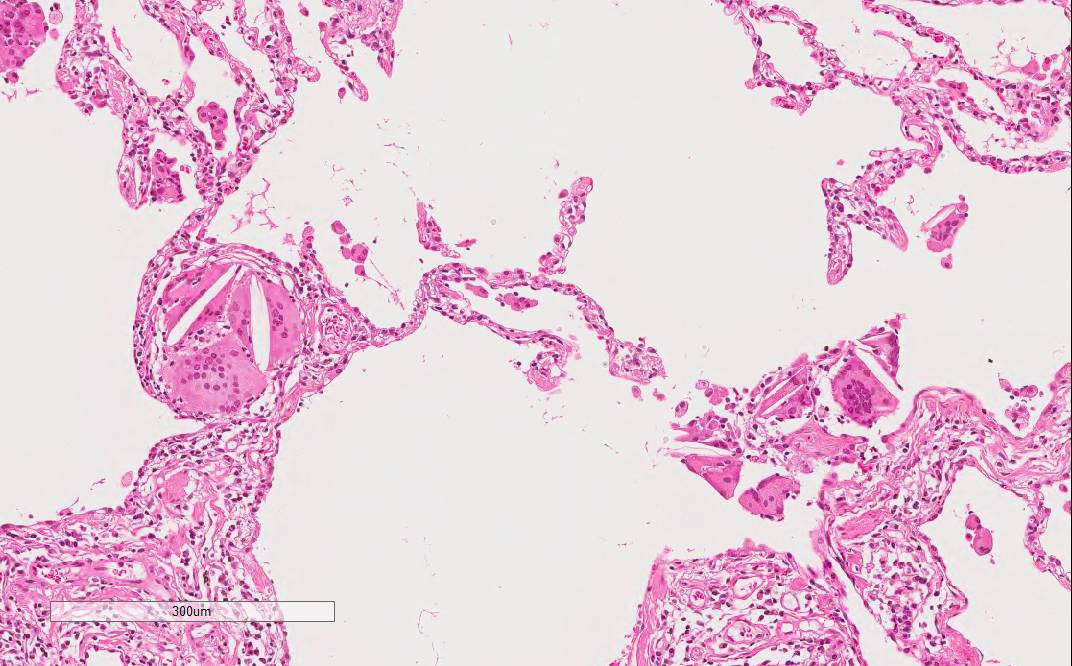
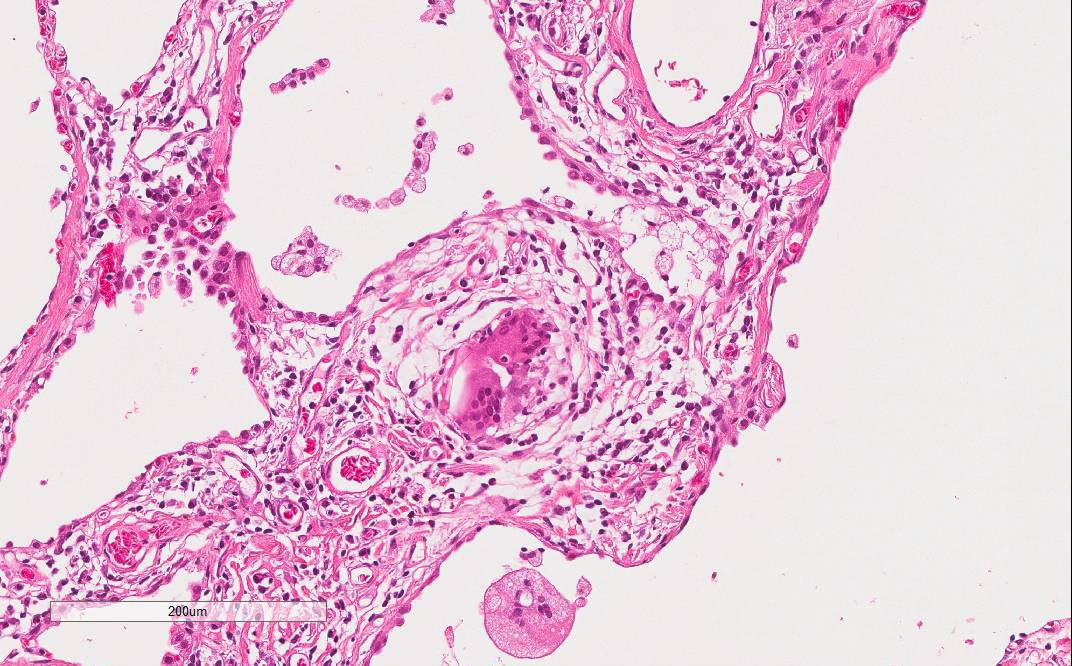
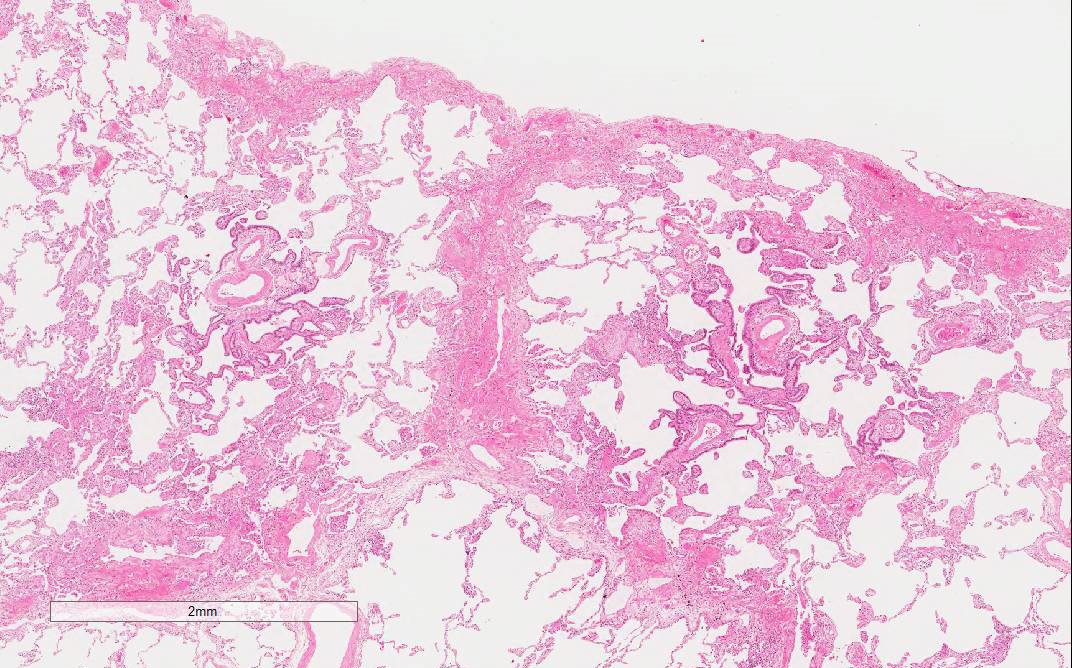
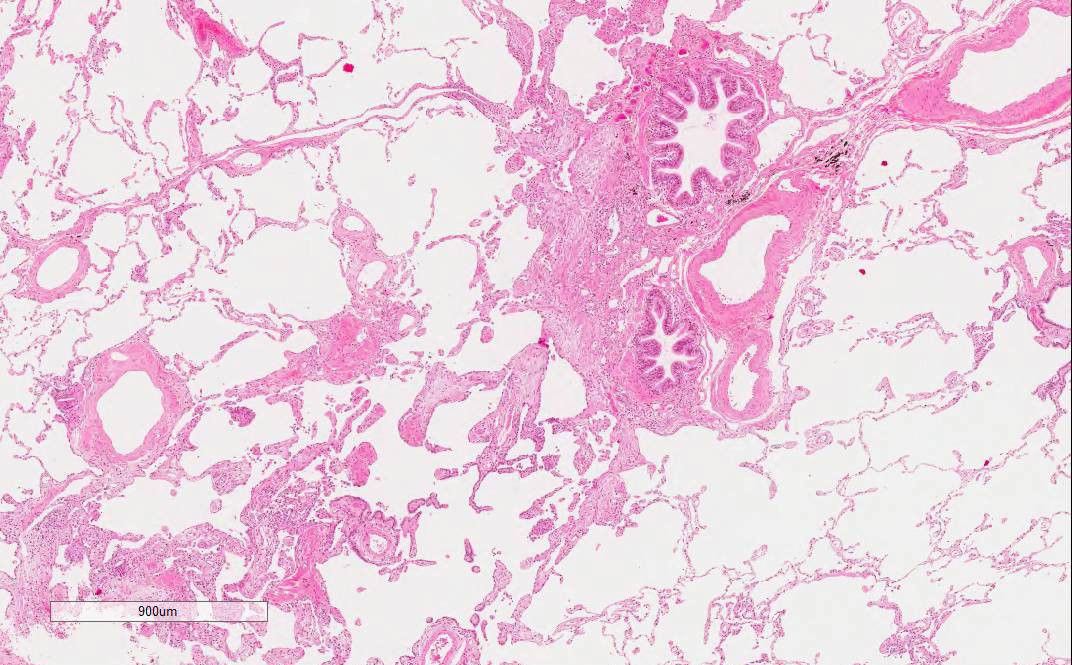
- Common findings(J Clin Pathol 2013;66:888, Am J Respir Crit Care Med 2012;186:314, J Investig Allergol Clin Immunol 2015;25:237, Arch Pathol Lab Med 2008;132:199):
- Airway centered (peribronchiolar) change
- Interstitial cellular infiltration
- Poorly formed nonnecrotizing granulomas or interstitial giant cells with cholesterol clefts
- Well formed granulomas can be found but may raise differential diagnosis with sarcoidosis if the granulomas are numerous and predominant
- Acute HP
- Airway centered inflammation with little fibrosis
- Neutrophilic infiltration with / without capillaritis
- Intra-alveolar fibrin deposition
- Subacute HP
- Airway centered infiltration with fibrosis
- Lymphocytic infiltration with granulomas or giant cells
- Chronic HP
- Predominantly airway centered inflammation with diffuse fibrotic change
- Lymphocytic infiltration with granulomas or giant cells
- Often overlaps with NSIP, UIP, organizing pneumonia and airway centered interstitial fibrosis
- Bridging fibrosis (fibrotic band connecting bronchioles with each other and with lobular septa) and peribronchiolar metaplasia can be a diagnostic clue to differentiate HP from IPF (J Clin Pathol 2013;66:888, Histopathology 2012;61:1026)
- Additional findings
- Byssinosis bodies (hemosiderin coated strands of fiber within fibrous tissue) can be found in byssinosis
- Foamy macrophages in alveolar spaces
- Organizing pneumonia
Microscopic (histologic) images
Scroll to see all images:
Contributed by Akira Yoshikawa, M.D.
Images hosted on other servers:
Images hosted on other servers:
Cytology description
- Bronchoalveolar lavage fluid shows lymphocytosis (see Diagnosis)
Positive stains
- Staining for cathepsin K and CD68 may be helpful to detect small granulomas
- Giemsa, Grocott and Ziehl-Neelsen stains rule out infectious diseases, if suspected
Differential diagnosis
- Airway centered interstitial fibrosis: absence of antigen exposure
- Connective tissue disease related interstitial pneumonia
- Idiopathic nonspecific interstitial pneumonia
- Organizing pneumonia
- Respiratory bronchiolitis related interstitial lung disease
- Sarcoidosis
- Smoking related interstitial fibrosis: smoking history, acellular fibrosis
- Usual interstitial pneumonia / idiopathic pulmonary fibrosis
Additional references
Practice question #1
Which two clinical and morphological findings are suggestive for HP?
- Intra-alveolar fibrin deposition
- Monocytosis in bronchoalveolar lavage
- Necrotizing granuloma
- Organizing pneumonia
- Weight loss
Practice answer #1
A. and E.
Comments:
Comment Here
Reference: Hypersensitivity pneumonitis
Comments:
- Intra-alveolar fibrin deposition is suggestive for acute HP, also for acute fibrinous and organizing pneumonia
- Typical bronchoalveolar lavage of HP shows lymphocytosis
- Necrotizing granuloma is more suggestive for tuberculosis
- Organizing pneumonia can be seen in HP but it is not specific
- Weight loss is suggestive for HP according to the large cohort study (see Diagnosis)
Comment Here
Reference: Hypersensitivity pneumonitis