Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Johnson E, Dioufa N. Chronic rhinosinusitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/nasalchronicrhinitis.html. Accessed September 24th, 2025.
Definition / general
- Nonspecific or specific chronic inflammation of the nasal cavity (rhinitis), paranasal sinuses (sinusitis) or both (rhinosinusitis)
- Sequel to acute rhinitis (symptoms lasting 6 weeks or less), with development of secondary bacterial infection
Essential features
- Submucosal mixed inflammatory infiltrate, including lymphocytes and variable amounts of plasma cells, eosinophils, histocytes and neutrophils
- Associated with deviated nasal septum or nasal polyps; ulceration and infection can extend into sinuses
- In longstanding / recurrent disease, epithelial hyperplasia with papillary appearance (hyperplastic papillary rhinosinusitis) can be seen
Terminology
- Rhinitis, sinusitis
Epidemiology
- Prevalence of chronic rhinosinusitis ranges from 4.8% to 12% in the United States (Thompson: Diagnostic Pathology - Head and Neck, 3rd Edition, 2022, J Allergy Clin Immunol Pract 2022;10:1395)
- Age: occurs over wide age range
- Sex: equal sex distribution
Sites
- Unilateral or bilateral, nasal cavity or paranasal sinus
Pathophysiology
- In a healthy epithelial barrier, intact tight junction proteins effectively protect against various external stimuli
- Environmental factors impair the integrity of the epithelial barrier, resulting in an imbalance of epithelium immune response, dysfunction of mucociliary clearance and excessive tissue remodeling in chronic rhinosinusitis (CRS) (Allergy 2024;79:1146)
- Frequently associated with deviated septum or nasal polyps
Etiology
- Developmental etiology
- Deviated nasal septum, primary ciliary dyskinesia
- Allergic rhinosinusitis is caused by environmental exposure to allergens in sensitive patients (Indian J Otolaryngol Head Neck Surg 2020;72:117, Med Mycol 2009;47:S324)
- Caused by exposure to allergen in sensitized immunocompetent people mediated by type I, IgE immune reaction
- More common allergens are pollen, animal dander, dust mites, mold
- Aspergillus species is the most common, followed by dematiaceous (brown pigmented) fungi found in soil, wood and decomposing plant material
- Allergic rhinosinusitis may predispose patients to recurrent or chronic sinusitis
- Infectious rhinosinusitis caused by microorganisms (Am J Rhinol 2005;19:153, J Allergy Clin Immunol Pract 2016;4:584)
- Variety of microorganisms, most commonly viruses and bacteria
- Symptoms include nasal congestion and watery nasal discharge, usually self limiting
- Viral rhinosinusitis results in common cold
- Most commonly due to rhinoviruses, influenza, parainfluenza, adenoviruses and respiratory syncytial virus
- Bacterial sinusitis
- Most commonly due to Streptococcus pneumoniae, Haemophilus influenzae, alpha hemolytic streptococci
- Variety of microorganisms, most commonly viruses and bacteria
- Other causes
- Atrophic rhinosinusitis (ozena, rhinitis sicca [stench]) (Am J Med 2009;122:747)
- Caused by various factors
- Nutritional deficiencies (e.g., vitamin A, iron)
- Chronic exposure to irritants
- Prior radiation or surgery
- Hypoestrogenemia
- Autoimmune disease
- Caused by various factors
- Aspirin intolerance or aspirin exacerbated respiratory disease (Allergy Asthma Immunol Res 2011;3:3)
- Samter triad or syndrome: includes aspirin intolerance, sinonasal polyps (usually bilateral), asthma
- Nonallergic rhinosinusitis with eosinophilia syndrome
- May be precursor to aspirin intolerance syndrome
- Idiopathic
- Occupational or environmental exposure
- Systemic diseases: cystic fibrosis, others
- Medication induced (rhinosinusitis medicamentosa)
- Topical or systemic medications (e.g., propranolol, oral contraceptives, reserpine), nasal sprays
- Pregnancy: hormone induced changes on sinonasal mucosa, increased blood volume and airway resistance
- Atrophic rhinosinusitis (ozena, rhinitis sicca [stench]) (Am J Med 2009;122:747)
Diagrams / tables
Clinical features
- Allergic rhinosinusitis (Otolaryngol Head Neck Surg 2015;152:S1)
- In sensitized patients, exposure results in allergic reaction with nasal congestion, rhinorrhea, sneezing and itching
- Reaction begins within minutes of exposure, peaking ~15 minutes later
- Noninfected nasal secretions appear clear
- Infected secretions appear purulent
- In sensitized patients, exposure results in allergic reaction with nasal congestion, rhinorrhea, sneezing and itching
- Infectious rhinosinusitis (Int Forum Allergy Rhinol 2021;11:213, Curr Allergy Asthma Rep 2020;20:28)
- Associated with pain localized over infected site; headaches are common
- Acute symptoms: > 7 days but < 3 weeks
- Subacute symptoms: 4 weeks to 3 months
- Chronic symptoms: lasting > 3 months
- Patients with resistant or refractory chronic sinusitis have increased incidence of Staphylococcus aureus, anaerobic bacteria and Gram negative organisms
- Pseudomonas aeruginosa commonly cultured in patients receiving multiple courses of antibiotics
- Atrophic rhinosinusitis (Am J Med 2009;122:747)
- Symptoms include nasal obstruction, headaches, nasal crusting, anosmia, epistaxis, halitosis and foul smelling nasal odor
Diagnosis
- Diagnostic criteria for chronic rhinosinusitis (symptoms present for ≥ 12 weeks) (Dtsch Arztebl Int 2024;121:643)
- 2 or more of the following symptoms
- Nasal obstruction
- Anterior or posterior rhinorrhea
- Facial pain / pressure
- Impaired sense of smell (hyposmia / anosmia)
- And at least 1 objective sign
- Evidence of inflammation on nasal endoscopy (edema, polyps, secretions in the middle nasal meatus)
- Evidence of inflammation of the paranasal sinuses on computed tomography (CT)
- 2 or more of the following symptoms
Laboratory
- Allergic rhinosinusitis: elevated total serum IgE, skin testing is gold standard for diagnosing allergies
- Infectious rhinosinusitis: microbiology cultures or respiratory viral panels
Radiology description
- Mucosal thickening or soft tissue opacification of nonexpanded sinus with thickening and sclerosis of sinus bony walls
Prognostic factors
- Prognosis for all types of rhinosinusitis is excellent, with a high likelihood of cure when appropriate therapy is administered
Case reports
- 26 year old man with chronic allergic rhinosinusitis with nasal polyps, which evolved into an invasive Aspergillus infection (IDCases 2023;32:e01772)
- 27 year old man complaining of recurrent episodes of epistaxis (Case Rep Otolaryngol 2019;2019:3725720)
- 47 year old man with anaphylactic reaction to a nonsteroidal anti-inflammatory drug (NSAID) and 6 months of persistent upper and lower airway complaints (Front Allergy 2024;5:1484931)
- 49 year old woman with a chief complaint of right sided facial pressure for > 3 years (Cureus 2023;15:e42246)
- Patient with 25 year history of chronic allergic rhinosinusitis, unsuccessfully treated with multiple drugs and surgeries (Cureus 2022;14:e21153)
Treatment
- Nasal saline irrigations, antihistamines and topical corticosteroids to suppress chronic inflammation (Aust J Gen Pract 2024;53:928)
- Avoidance of allergens (allergic fungal sinusitis) and aspirin (aspirin exacerbated respiratory disease)
- Immunotherapy for documented IgE mediated allergies
- Surgical approaches for relief of symptoms after failed conservative management
- Functional endoscopic sinus surgery (FESS)
Gross description
- Aggregate of tan-white to tan-brown, soft to hard, irregular morcellated portions of osteocartilaginous tissue
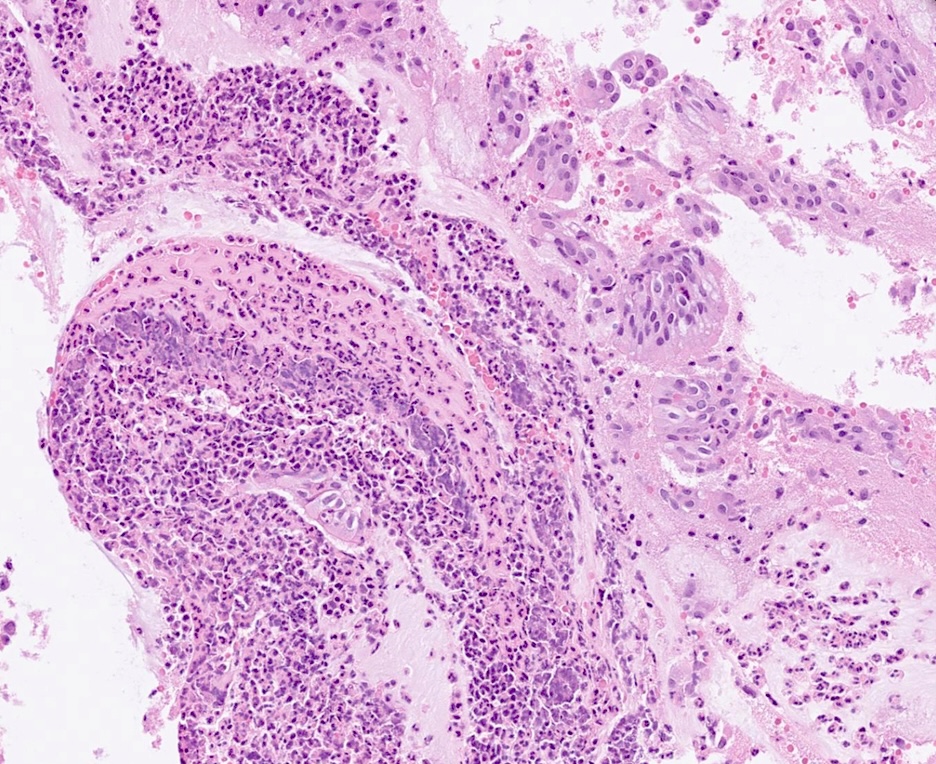
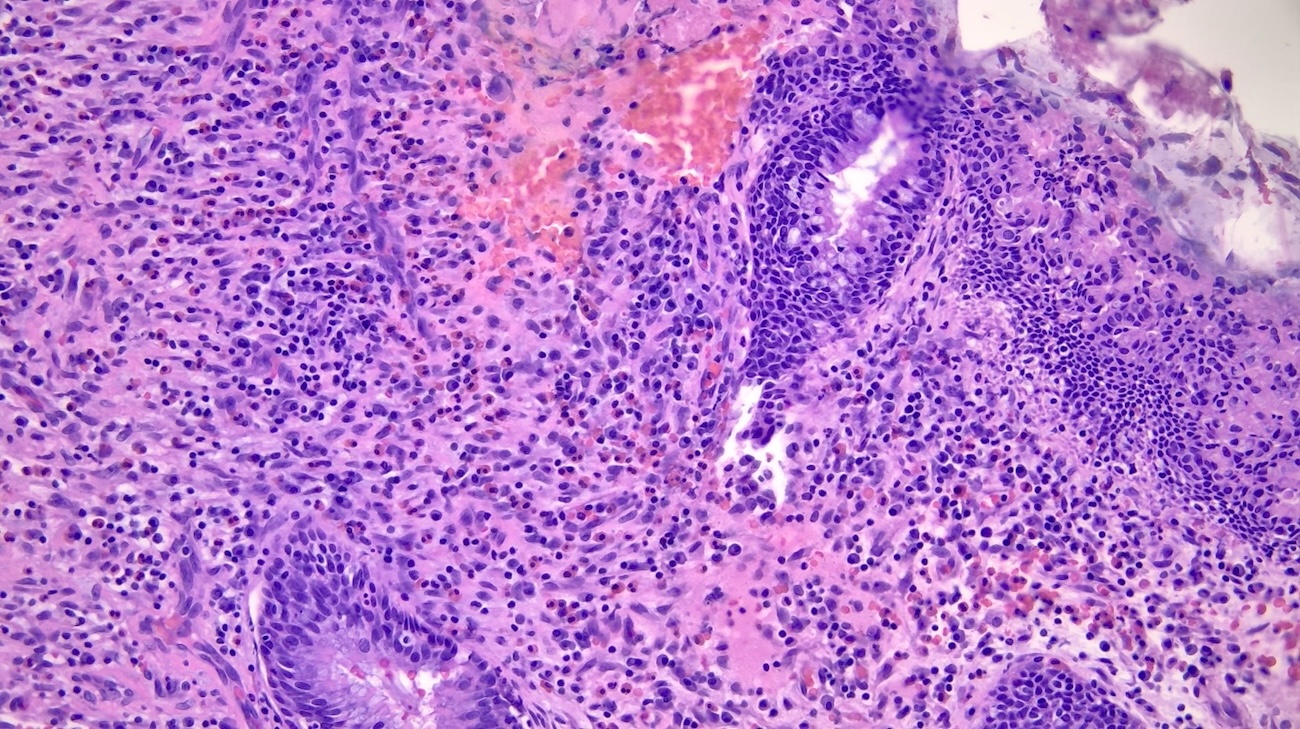
Microscopic (histologic) description
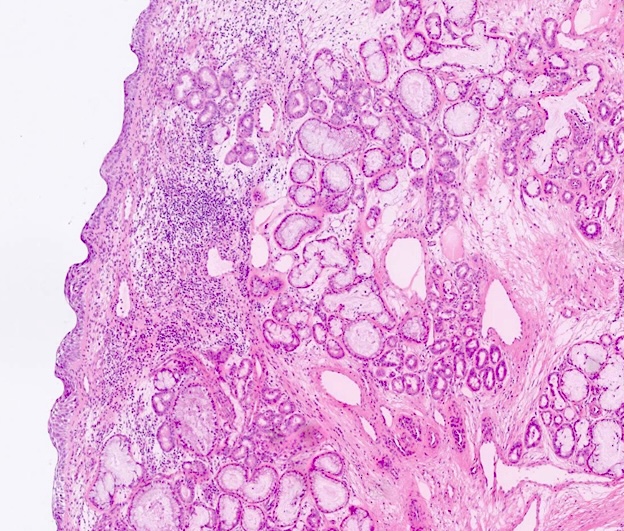
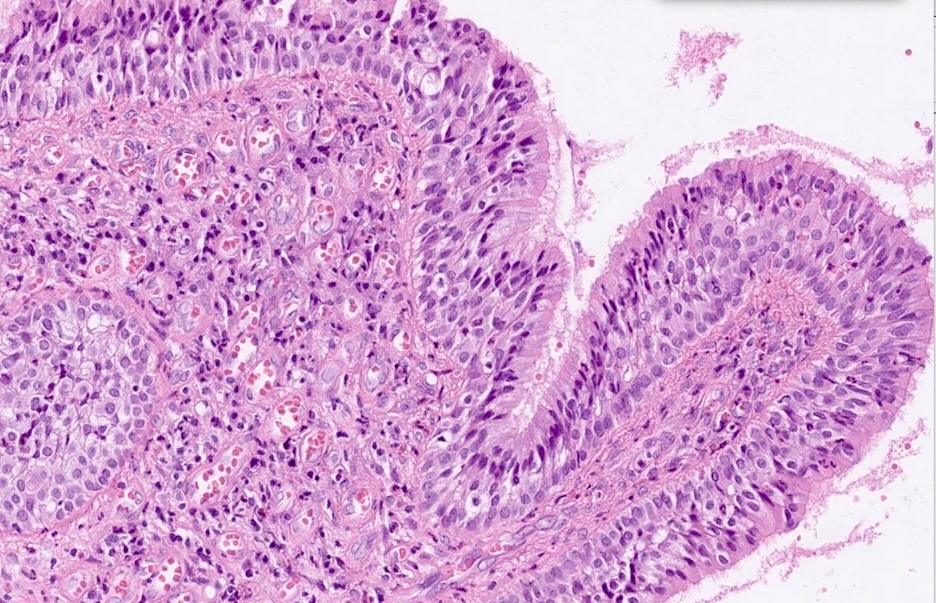
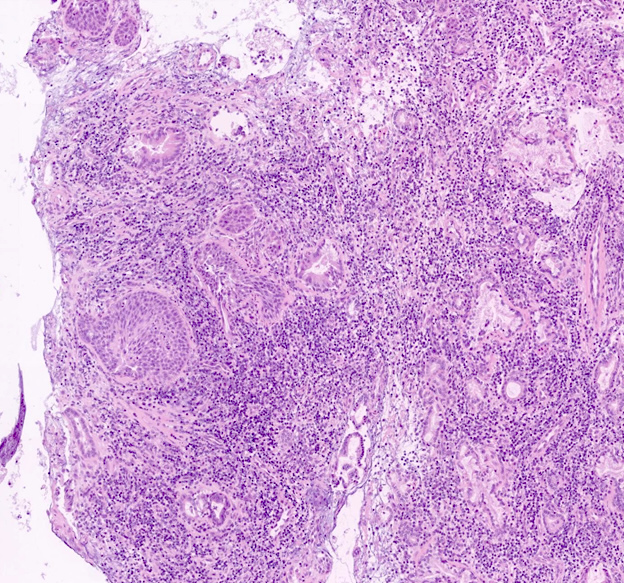
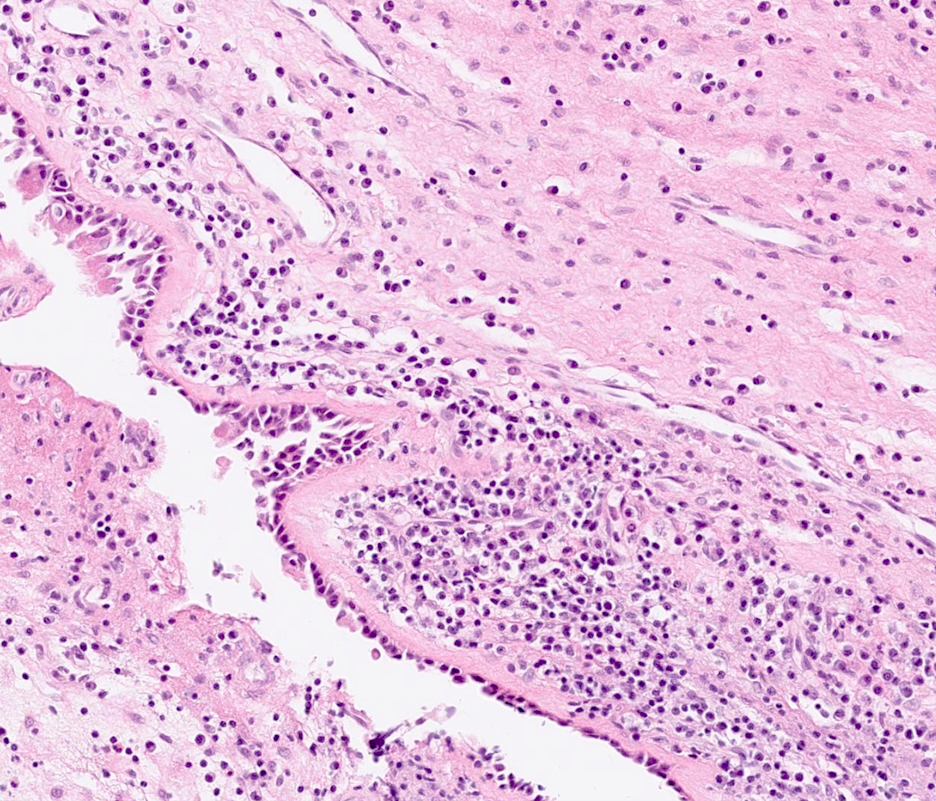
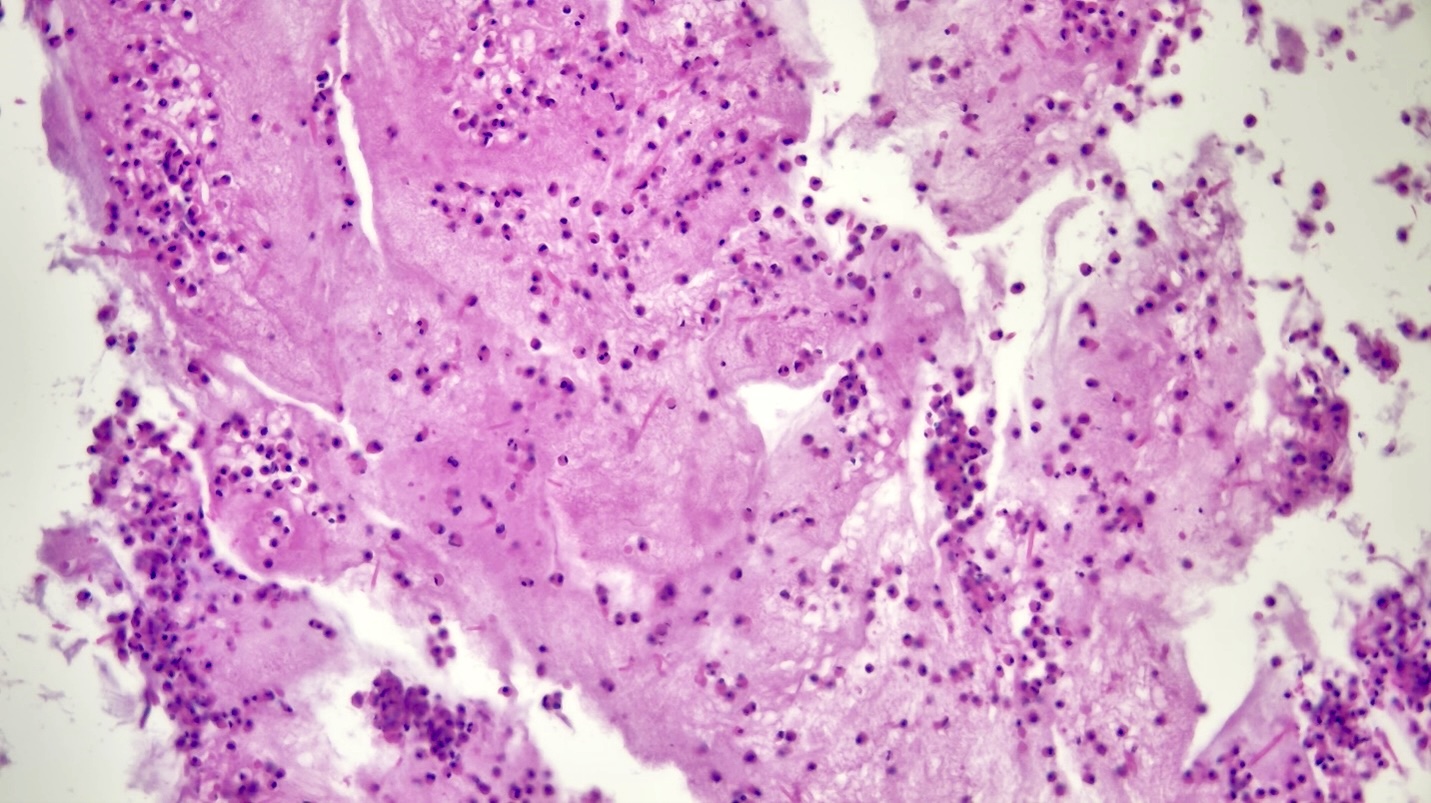
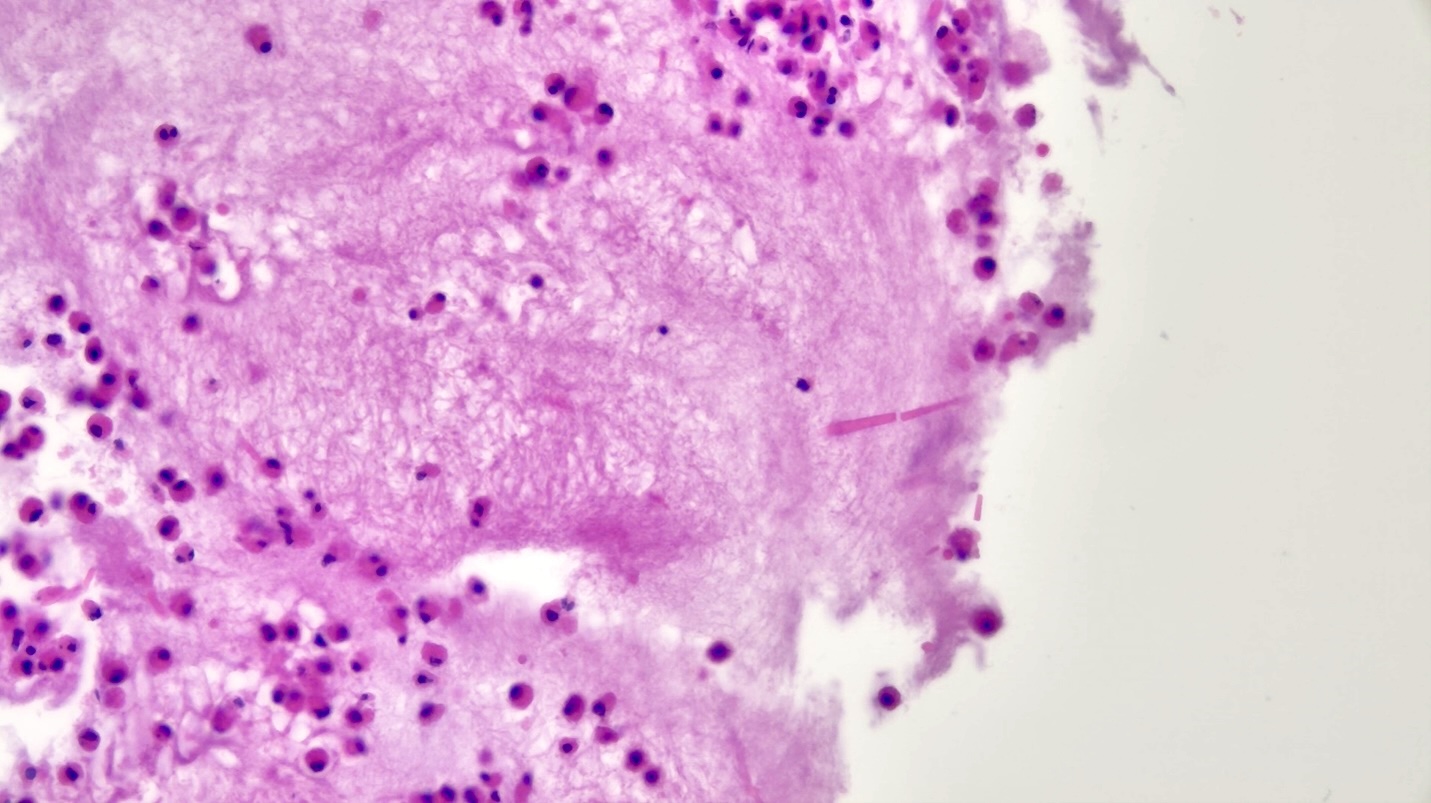
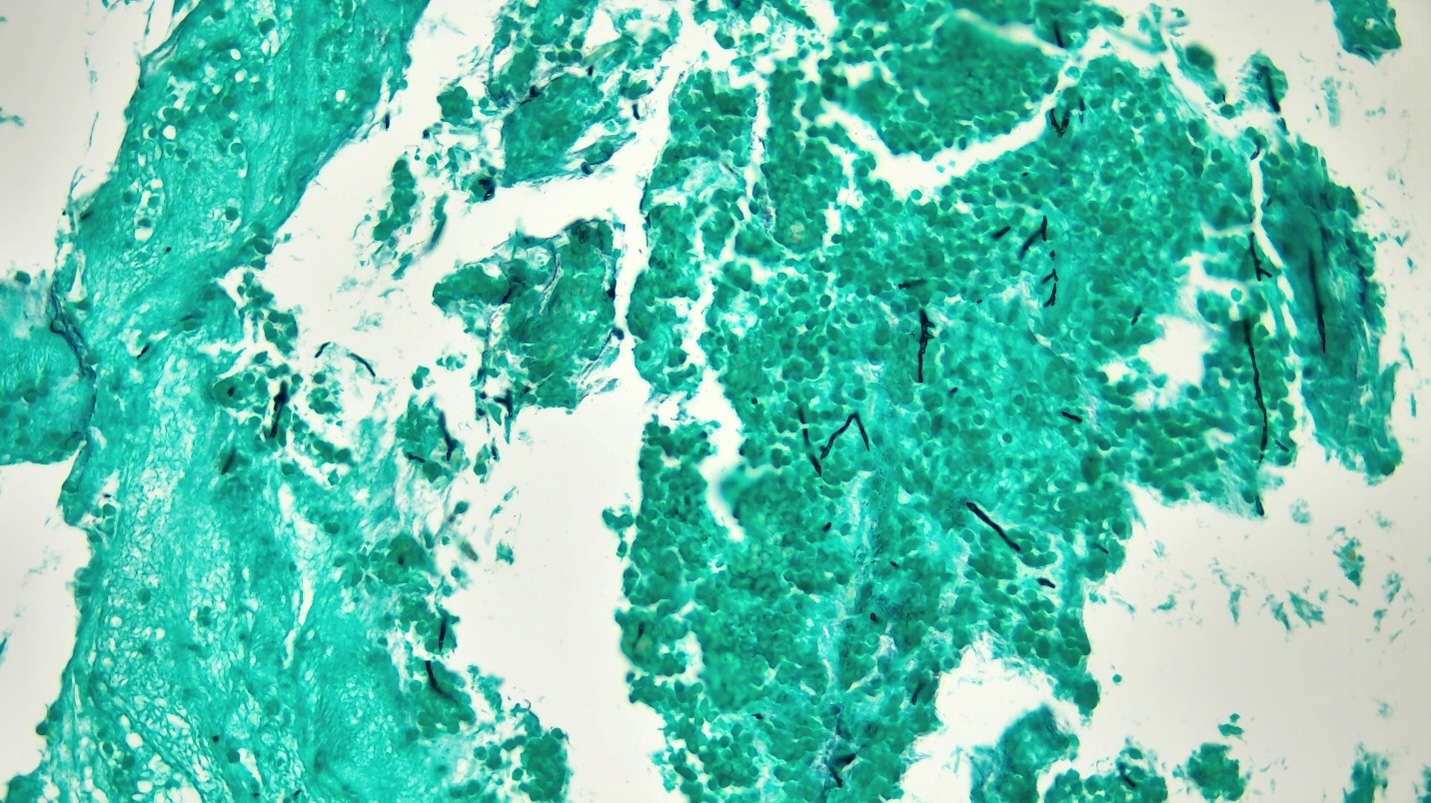
- Allergic rhinosinusitis
- Submucosal edema with mixed inflammatory infiltrate, predominantly eosinophils
- Abundant extracellular mucin material alternating with inflammatory debris
- Charcot-Leyden crystals (degenerated eosinophils) and fungal forms can be seen
- Squamous metaplasia of surface epithelium may be present
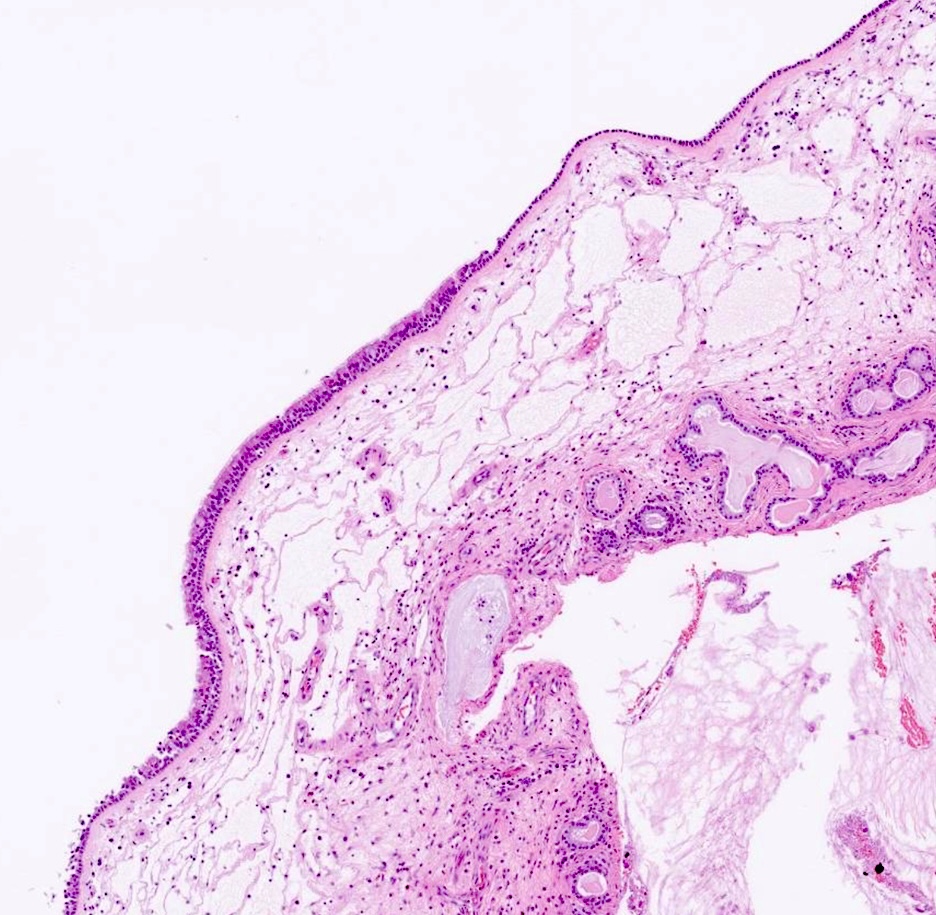
- Atrophic rhinosinusitis
- Squamous metaplasia of surface epithelium is very common
- Submucosal edema with nonspecific chronic inflammation, fibrosis and atrophy of the seromucous glands
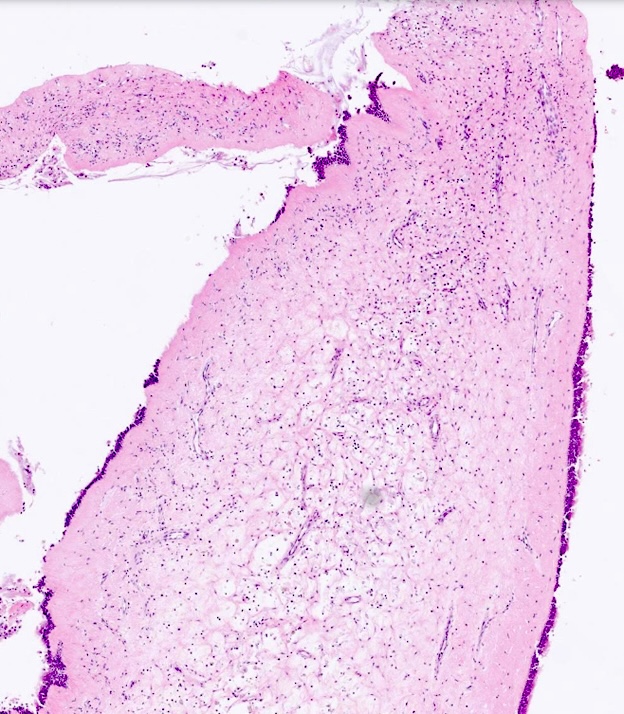
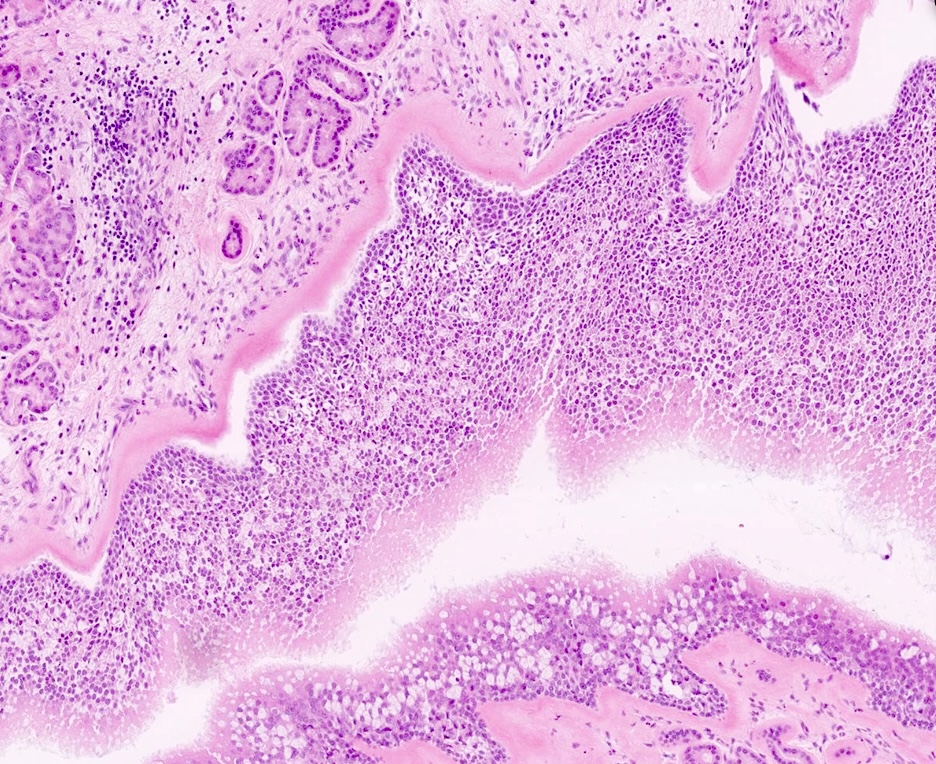
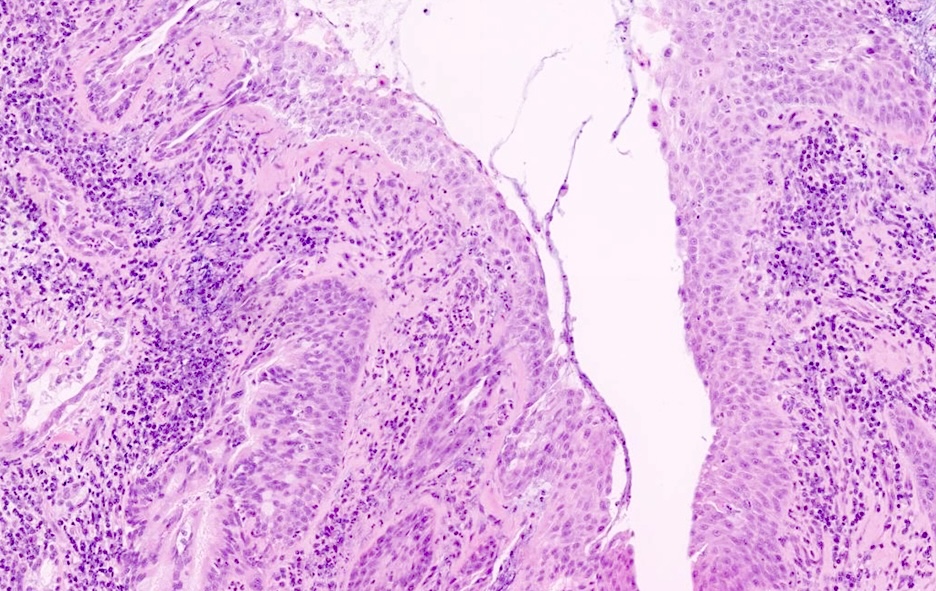
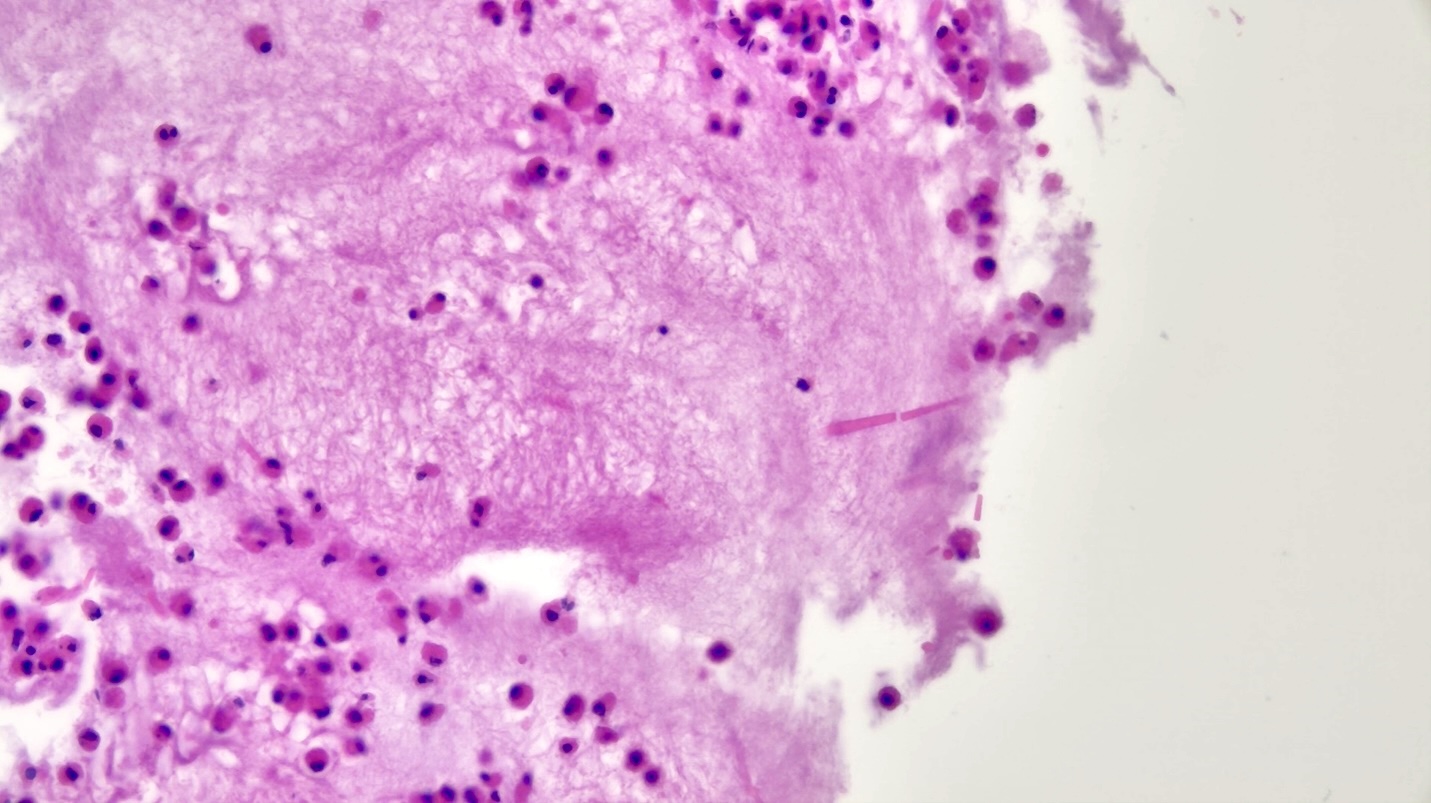
- Nonspecific chronic sinusitis
- Submucosal mixed inflammatory infiltrate, including lymphocytes, plasma cells, eosinophils, histiocytes and neutrophils
- Important to document the dominant inflammatory component and degree (mild, moderate, severe) to guide therapies
- Submucosal edema with seromucous gland hyperplasia
- Vascular proliferation may be seen
- In longstanding / recurrent / persistent disease, epithelial hyperplasia with papillary appearance (hyperplastic papillary rhinosinusitis) can be present
- Sinonasal inflammatory polyps (polypoid fragments of sinonasal mucosa with prominent stromal edema, lack of seromucinous glands and mixed inflammatory cells) can often be seen
- References: Curr Health Sci J 2020;46:66, Int Forum Allergy Rhinol 2014;4:463
Microscopic (histologic) images
Contributed by Erika Johnson, M.D. and Nikolina Dioufa, M.D.
Positive stains
Sample pathology report
- Sinus, left, contents, nasal / sinus endoscopy:
- Bone and sinonasal mucosa with moderate chronic inflammation (lymphoplasmacytic predominance), mild submucosal edema and focal squamous metaplasia
- Findings consistent with chronic sinusitis
Differential diagnosis
- Sinonasal adenocarcinoma:
- Complex architectural growth patterns, back to back glands composed of single cell type
- Usually low to intermediate grade tumors
- Perineural or lymphovascular invasion may be seen
- Stroma may be collagenized or myxoid, with areas of necrosis
- Diagnosis of exclusion
- Sinonasal papilloma:
- Presence of thickened transitional epithelium with endophytic or exophytic growth and associated mucocytes, microcysts and inflammatory cells
- Malignant transformation is rare
- Associated with human papillomavirus (HPV)
- EGFR somatic mutations for inverted type and KRAS for oncocytic type
- Sinonasal lymphoma:
- Typically older individuals (50 - 70 years of age)
- Most common type: diffuse large B cell lymphoma (DLBCL)
- Composed of centroblasts or less often, immunoblasts arranged in a diffuse pattern
- Mitotic figures are common; coagulative necrosis may be present
- Positive for pan-B cell markers by immunohistochemistry
- 50 - 75% of cases are of nongerminal center B cell type, usually positive for IRF4 (MUM1) and FOXP1
- 25 - 50% of cases are of germinal center B cell type, usually positive for CD10, BCL6, LMO2 or GCET1
- IgG4 related disease:
- Lymphoplasmacytic infiltrate with increased IgG4+ cells and an IgG4+:IgG+ ratio of > 40%, with storiform fibrosis
- Obliterative phlebitis can be seen
- Clinically compatible features (IgG4 RD in other body sites, elevated serum IgG4 and response to steroid / rituximab therapy)
Practice question #1
A 45 year old man presents with chronic nasal congestion, postnasal drainage and facial pressure. A biopsy of the sinonasal mucosa reveals thickened basement membrane, mixed inflammatory infiltrate including lymphocytes, goblet cell hyperplasia, plasma cells and eosinophils (see image above). Which of the following is the most likely underlying condition?
- Allergic fungal rhinosinusitis
- Granulomatosis with polyangiitis
- Nonspecific chronic rhinosinusitis
- Sarcoidosis
- Sinonasal undifferentiated carcinoma
Practice answer #1
C. Nonspecific chronic rhinosinusitis. Thickened basement membrane, hyperplastic changes and mixed inflammation are most commonly seen in chronic rhinosinusitis. This can be in the context of deviated nasal septum and sinonasal inflammatory polyps. Answer B is incorrect because granulomatosis with polyangiitis would present with granulomatous inflammation, vasculitis, necrosis and multinucleated giant cells. Answer A is incorrect because allergic fungal sinusitis is an allergic, hypersensitivity mediated condition associated with exposure to an allergen that presents with clinical symptoms soon after. Additionally, there would be predominance of eosinophils, unless there is superimposed infection. Answer E is incorrect because patients usually report unilateral symptoms of congestion and discharge. The lesion would be composed of small round blue and undifferentiated cells, not an inflammatory infiltrate. Answer D is incorrect because a case of sarcoidosis would have nonnecrotizing granulomas.
Comment Here
Reference: Chronic rhinosinusitis
Comment Here
Reference: Chronic rhinosinusitis
Practice question #2
A 50 year old woman with a history of asthma and recurrent sinus infections undergoes endoscopic sinus surgery. Histologic examination reveals abundant mucin, dense eosinophilic infiltrate and Charcot-Leyden crystals. Grocott stain highlights scattered septate fungal hyphae. What is the most likely diagnosis?
- Allergic fungal rhinosinusitis
- Chronic bacterial rhinosinusitis
- Invasive fungal sinusitis
- Sinonasal adenocarcinoma
Practice answer #2
A. Allergic fungal rhinosinusitis. This is a form of chronic rhinosinusitis caused by a hypersensitivity reaction to various antigens, namely Aspergillus. It is characterized by thick allergic type mucin, containing inflammatory debris, Charcot-Leyden crystals and fungal forms. It is often seen in patients with asthma. Answer C is incorrect because invasive fungal sinusitis is most commonly seen in immunocompromised patients, with inflammation seen in the tissue (not the mucin) and fungi seen in the vessel wall (angioinvasive) with extensive hemorrhagic type necrosis. Answer B is incorrect because chronic bacterial rhinosinusitis is bacterial in origin, not fungal; therefore, it would not show septate fungal hyphae upon staining. Answer D is incorrect because histology does not show atypical cells with an invasive growth pattern as typically found in a malignant epithelial tumor.
Comment Here
Reference: Chronic rhinosinusitis
Comment Here
Reference: Chronic rhinosinusitis