Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Tondi Resta I, Jalaly JB. Mucosal neuroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavityoralmucosalneuroma.html. Accessed August 26th, 2025.
Definition / general
- Uncommon, benign peripheral nerve sheath proliferations or tumors often identified incidentally or in association with certain genetic syndromes
- Includes traumatic neuroma, solitary circumscribed neuroma, genetic syndrome associated neuroma (including multiple endocrine neoplasia type 2B [MEN2B] and PIK3CA associated overgrowth spectrum [PROS]), pseudoperineurioma
Essential features
- Well circumscribed neural proliferation that may demonstrate haphazard growth
- Presentation in pediatric patients often occurs in the setting of MEN2B or other possible genetic syndrome (such as PTEN hamartoma tumor syndrome or PIK3CA associated overgrowth spectrum)
Terminology
- Neuroma, not otherwise specified
- Traumatic neuroma
- Solitary circumscribed neuroma (palisaded encapsulated neuroma)
- Neuroma in association with genetic syndrome
- Oral perineurioma
ICD coding
- ICD-O: 9570/0 - solitary circumscribed neuroma
- ICD-10
- ICD-11
Epidemiology
- Traumatic neuroma: more common in women, fourth to sixth decades of life
- Solitary circumscribed neuroma: more common in men in their fifth to seventh decades of life
- Genetic syndrome associated neuromas: more common in pediatric patients with no specific gender predilection
- Oral pseudoperineurioma: young female patients
Sites
- Majority occur on the tongue, lips, palate and gingiva
- Other sites include the hard palate, buccal mucosa, skin around the mouth
Pathophysiology
- Traumatic neuromas: injury to a nerve causes proliferation of nerve fascicles in an attempt to undergo regenerative changes
- Solitary circumscribed neuromas result from a proliferation of Schwann cells within the nerve
- In the setting of MEN2B, RET proto-oncogene mutations lead to overactivation of a tyrosine kinase receptor, which leads to oncogenesis (Endocr Relat Cancer 2018;25:T29)
- In the setting of PROS, PIK3CA mutations lead to proliferation (Pediatr Res 2017;82:850)
- Oral pseudoperineuriomas develop after nerve injury or enlargement as in the setting of PROS
Etiology
- Traumatic neuromas result from iatrogenic nerve injury
- May develop in patients with MEN2B, PTEN hamartoma tumor syndromes or PROS (Arch Dermatol 2006;142:625, Pediatr Res 2017;82:850)
Clinical features
- Incidental lesions often present as a soft papule in the oral cavity
- Patients with genetic syndromes (MEN2B, PROS) may present with multiple small soft papules
- In the setting of MEN2B syndrome, these are often the first identified lesion of the syndrome presenting with bilateral nodules in the commissure or as multiple nodules on the anterior third of the tongue (Ann Dermatol 2010;22:452)
Diagnosis
- Physical examination of the nodule(s)
- Careful history
- Biopsy
Prognostic factors
- Mucosal neuromas themselves have excellent prognosis
- Close clinical follow up is required in patients with genetic syndromes to follow for the development of other neoplasms
Case reports
- 9 year old boy with numerous papules and nodules on his lips and tongue and enlarged face and bones (Ann Dermatol 2010;22:452)
- 24 year old man with a soft left sided tongue nodule (Indian J Pathol Microbiol 2020;63:604)
- 28 year old woman with multiple conjunctival and mucosal nodules (Am J Ophthalmol Case Rep 2023;30:101828)
- 30 year old man with painful swelling of the left palate (J Med Case Rep 2016;10:116)
- 43 year old man with multiple conjunctival nodules, diffusely enlarged lips and numerous nodules on the lateral borders of the tongue, buccal and labial mucosa (J Oral Maxillofac Pathol 2020;24:339)
Treatment
- No treatment required for an incidental mucosal neuroma
- In the setting of MEN2B, prophylactic thyroidectomy followed by sequential serum calcitonin and CEA levels; additional imaging as needed to evaluate for new tumors (including abdominal imaging to monitor for pheochromocytomas) (Endocr Relat Cancer 2018;25:T29)
Clinical images
Microscopic (histologic) description
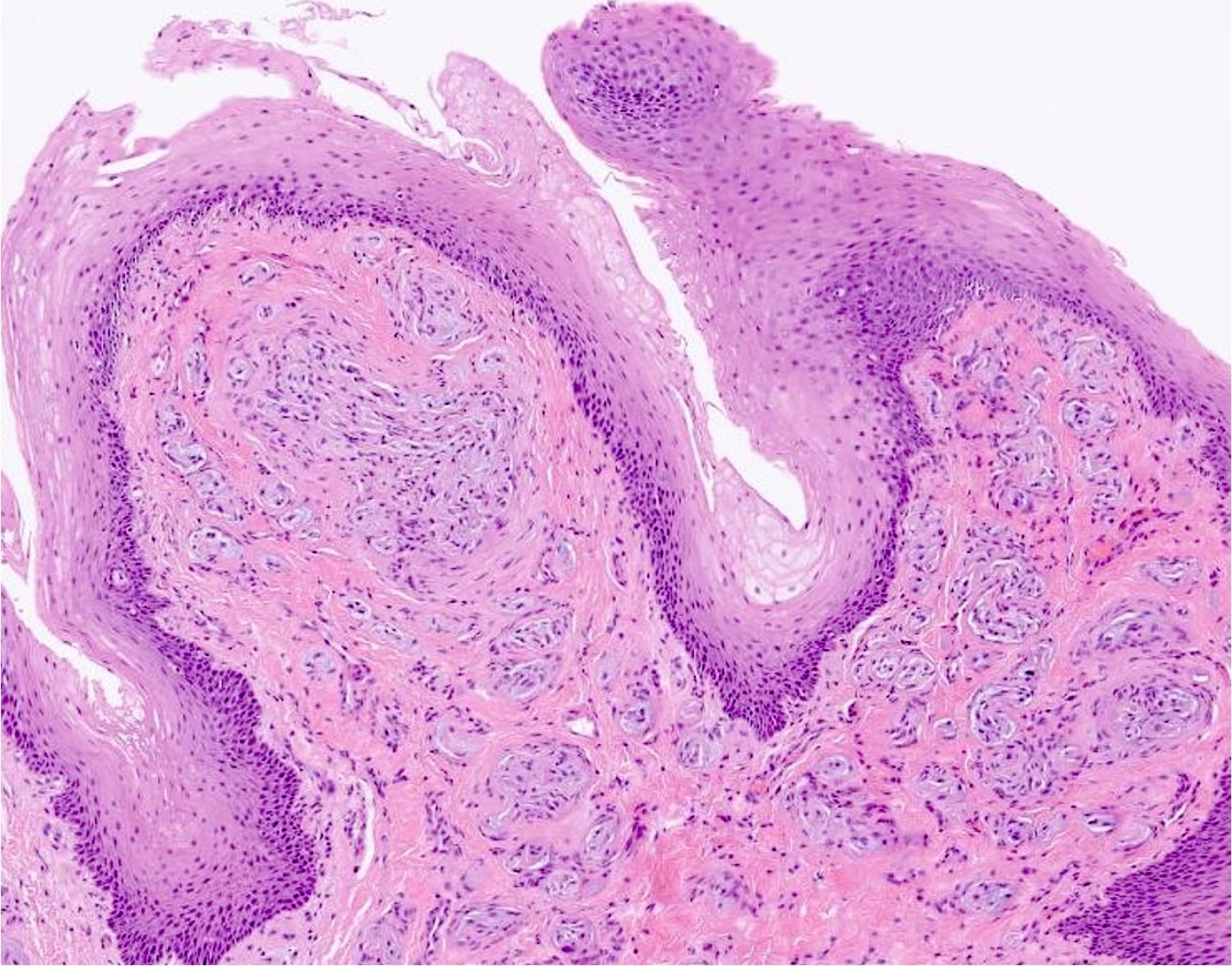
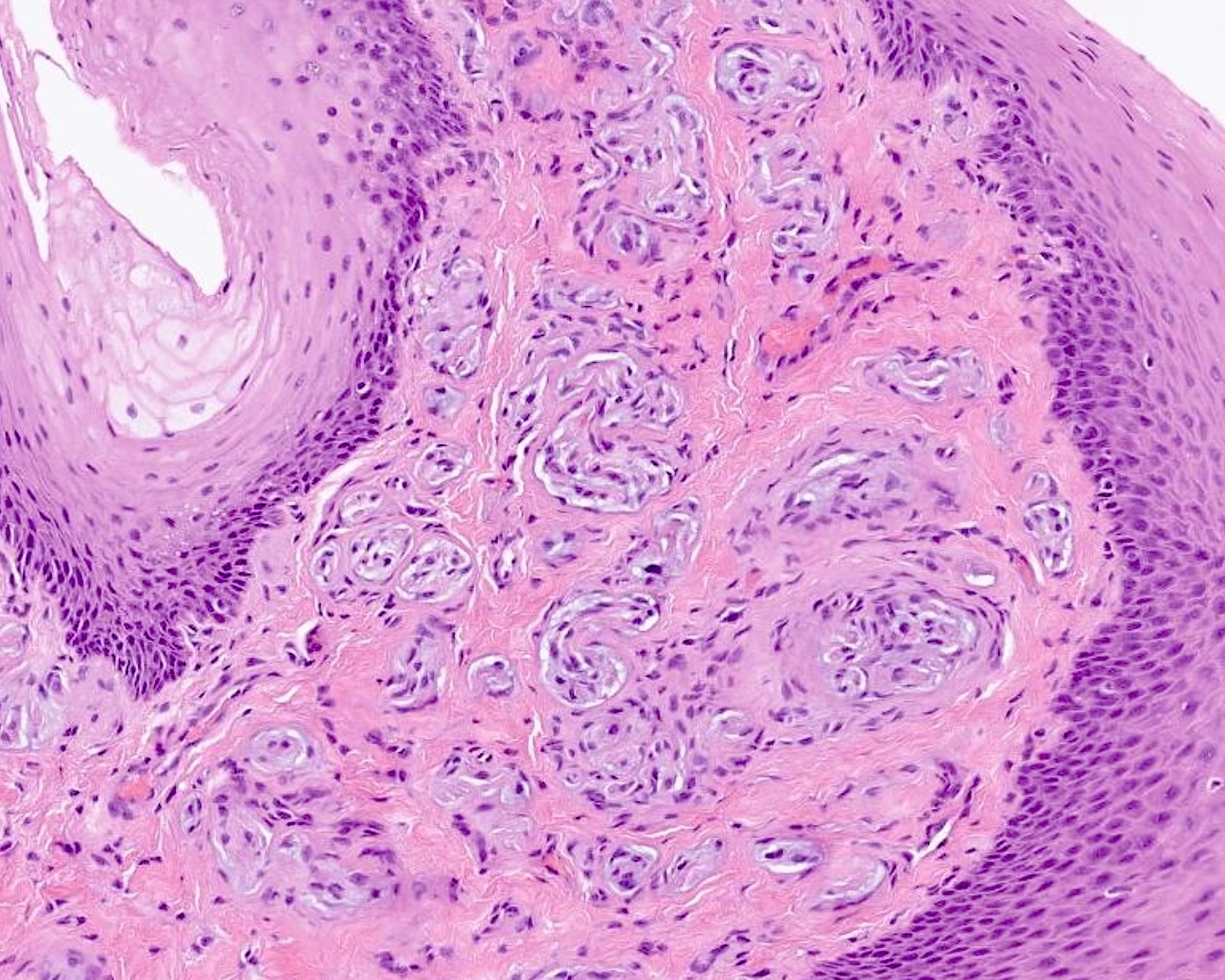
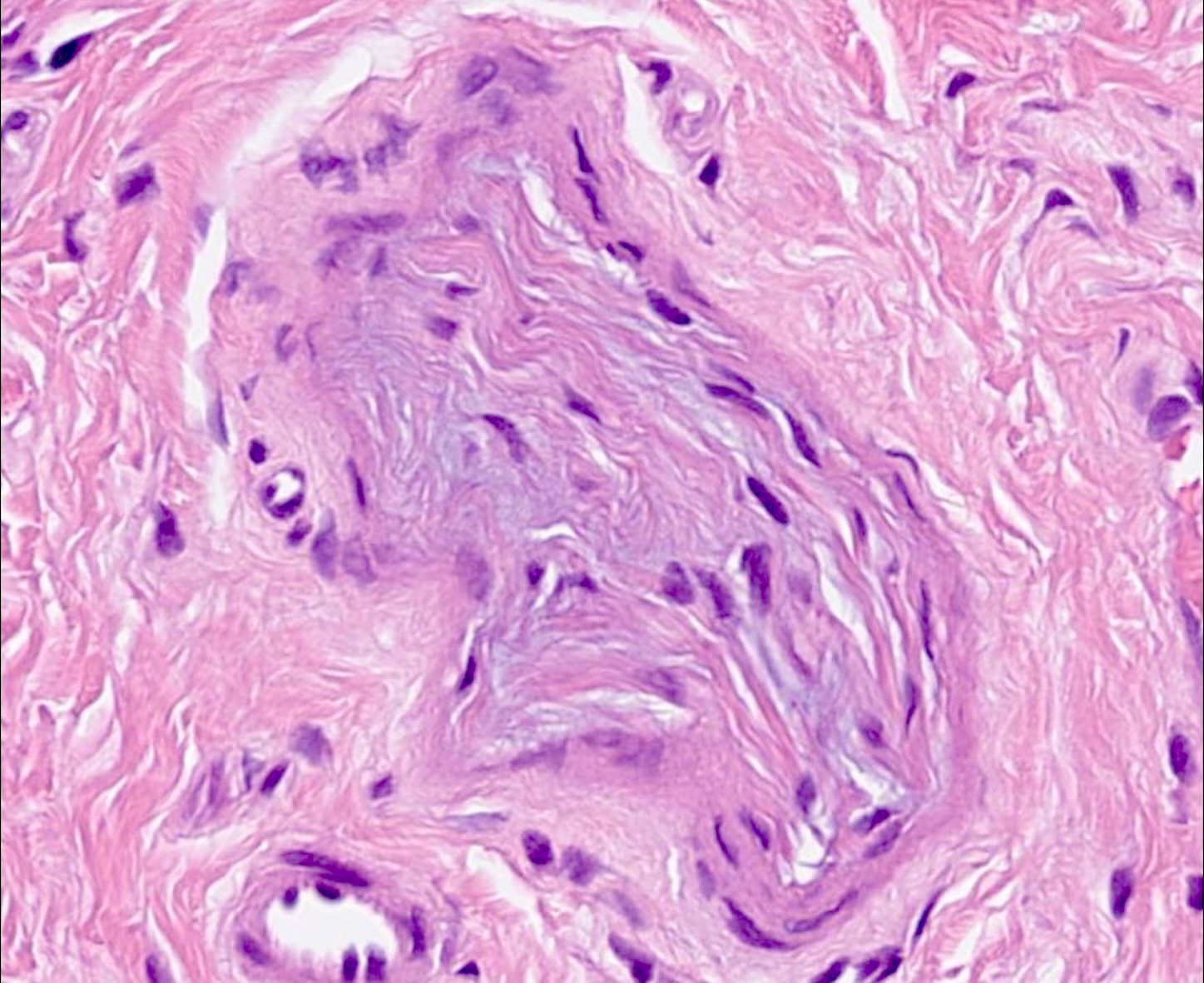
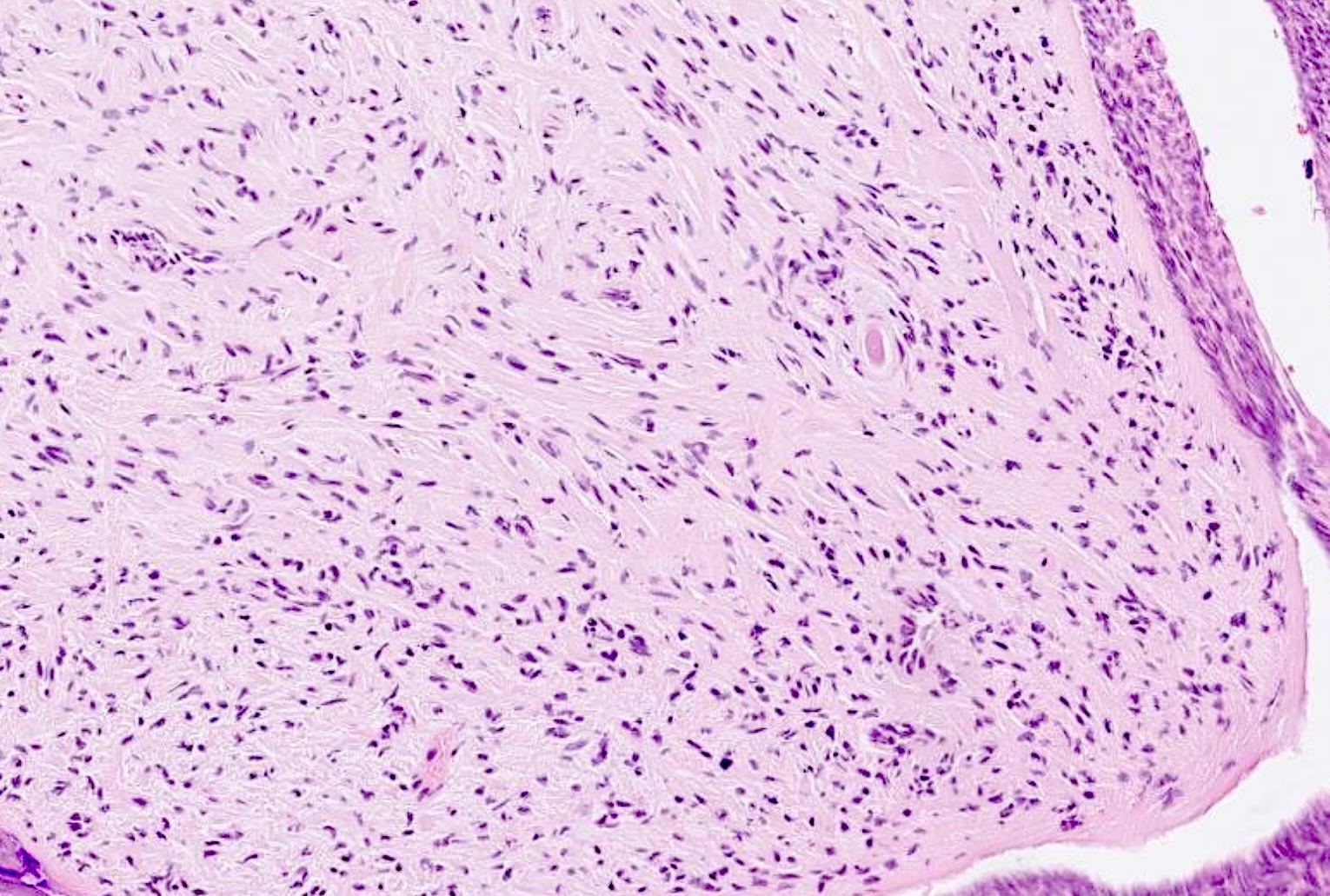
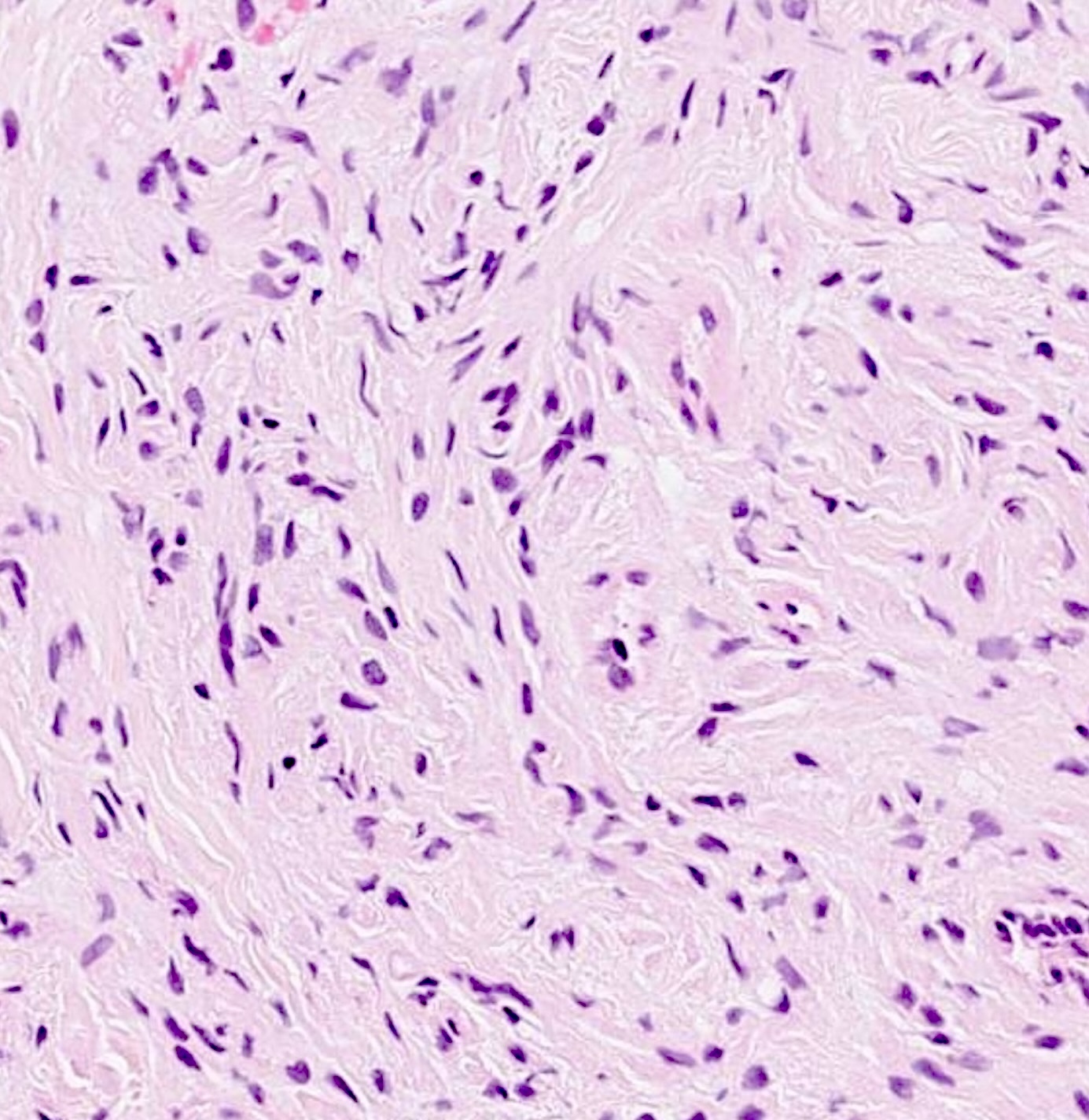
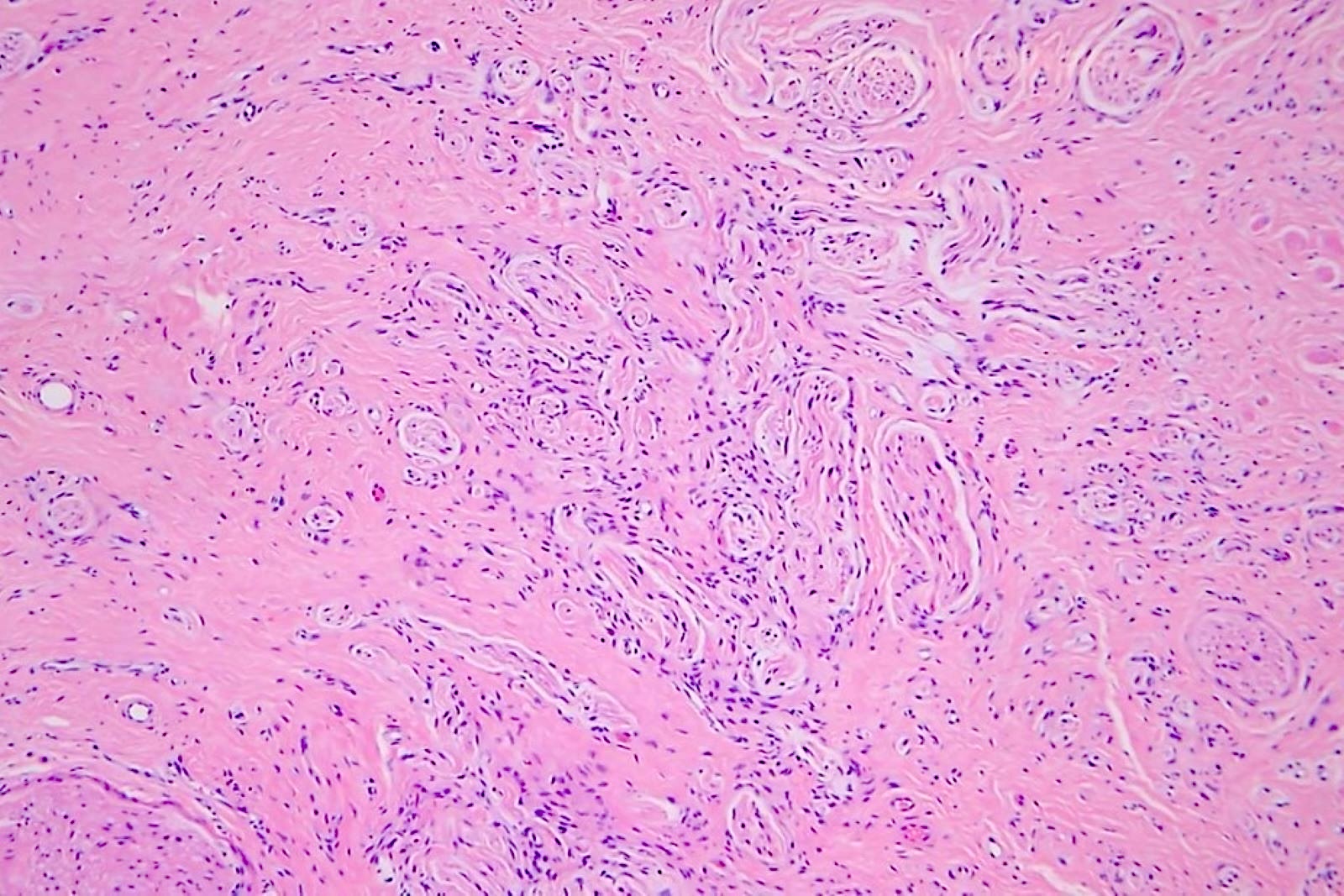
- Traumatic neuroma: unencapsulated, hyperplastic and disorganized neural proliferation composed of cytologically bland Schwann cells (Arch Dermatol 2006;142:625)
- Solitary circumscribed neuroma: numerous intersecting Schwann cells growing in a multinodular or fungating pattern (Head Neck Pathol 2010;4:15)
- Genetic syndrome associated neuromas (MEN2B and PROS): unencapsulated and hyperplastic Schwann cell proliferation with a prominent thickened perineurium (Pediatr Dermatol 2020;37:1128)
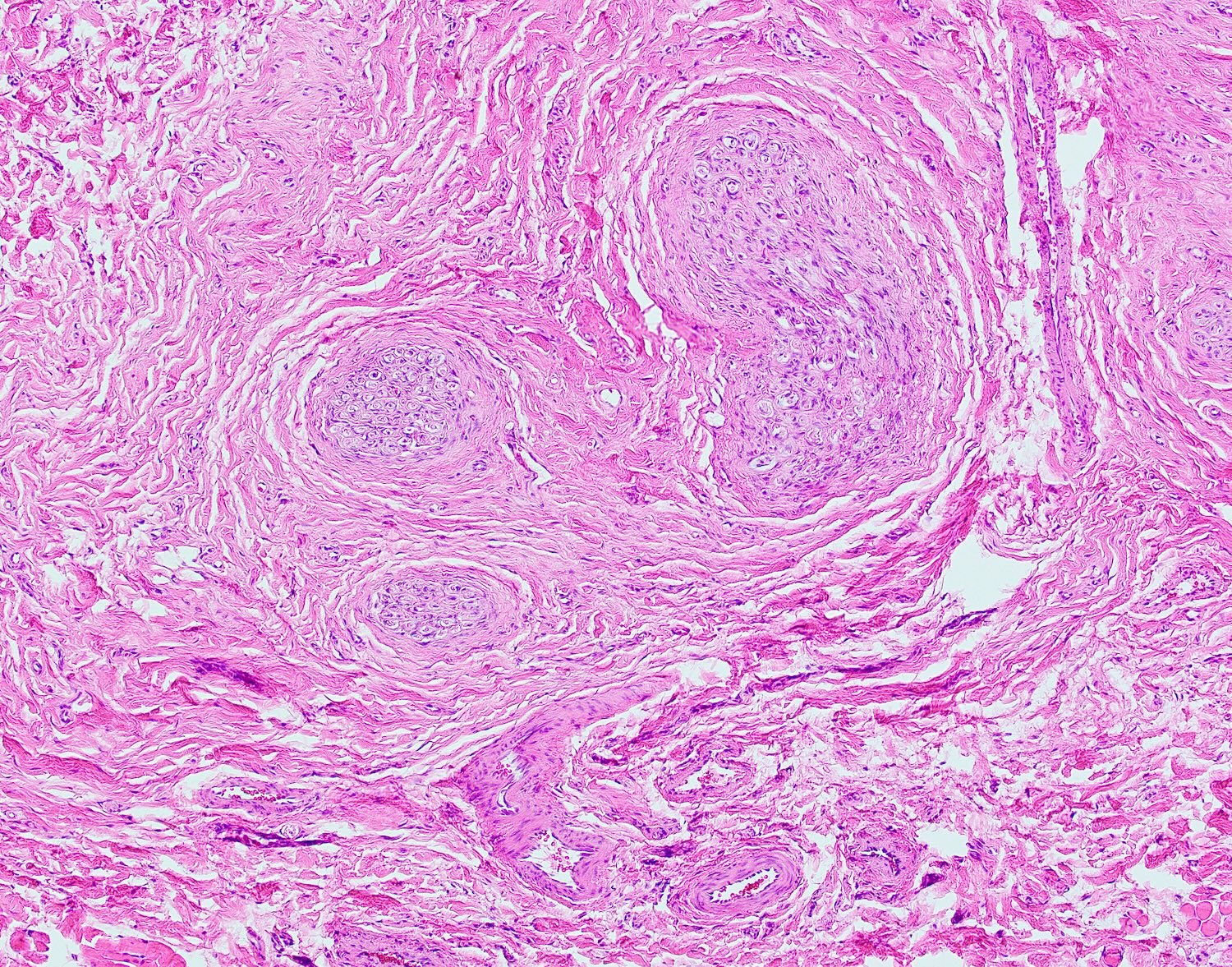
- Oral pseudoperineurioma: nerves with perineural thinning or perineurial cells growing within the nerve as pseudo-onion bulbs (Head Neck Pathol 2013;7:334)
Microscopic (histologic) images
Contributed by Benjamin Wilkins, M.D., Ph.D., Isabella Tondi Resta, M.D. and Molly Housley Smith, D.M.D.
Negative stains
Molecular / cytogenetics description
- RET proto-oncogene mutations in the setting of MEN2B syndrome
- PIK3CA mutations in the setting of PROS
Sample pathology report
- Oral cavity, right tongue, excision:
- Mucosal neuroma, 1.0 cm (see comment)
- Comment: The lesion demonstrates a benign neural proliferation with haphazard growth that has been completely excised. These lesions have been associated with certain genetic syndromes (such as MEN2B) and further evaluation may be considered in the appropriate clinical context.
- Oral cavity, right tongue, excision:
- Disorganized proliferation of nerves, consistent with traumatic neuroma
Differential diagnosis
- Neurofibroma:
- Composed of Schwann cells, fibroblasts and perineurial cells with intermixed collagen fibers and stroma
- CD34+
- Schwannoma:
- Most often occurs in adults within the fourth to sixth decade in the absence of trauma
- Histologically is encapsulated and demonstrates hypercellular and hypocellular areas (Antoni A and B, respectively); frequent Verocay bodies / palisading of the nuclei in Antoni A / hypercellular areas
- Lingual papillae:
- Filiform papillae: often not prominent nodules, prominent keratinization at the location of the rete ridges without taste buds
- Fungiform: often rounded projections with associated lamina propria and embedded taste buds into the epithelium
- Circumvallate: often located at the terminal sulcus in the posterior aspect of the tongue, mushroom shaped and embedded taste buds into the epithelium with prominent clefts ending in serous secreting glands (von Ebner glands)
- Fibroma:
- Demonstrates prominent collagen bundles with scattered fibroblasts
Practice question #1
Practice answer #1
C. Neuroma. Neural proliferation with irregular growth is consistent with a neuroma. Answers A and B are incorrect because of the absence of collagen within the lesion. Answer D is incorrect because this entity is not composed of a neural proliferation. Answer E is incorrect because no evident Antoni A or Antoni B areas can be identified.
Comment Here
Reference: Oral mucosal neuroma
Comment Here
Reference: Oral mucosal neuroma
Practice question #2
A 1 year old boy presents to the pediatrician's office with his mother for an annual physical exam and the mother states that numerous new small nodules are growing on her son's tongue. The pediatrician biopsies one of the nodules, which shows an unencapsulated proliferation of benign nerves with thickened perineurium. No collagen is noted within the proliferation. Which of the following germline gene mutations is the patient most likely to have?
- Menin
- NF1
- PRKAR1A
- RET
- TSC
Practice answer #2
D. RET. RET germline mutations are associated with MEN2B, which is associated with mucosal neuromas, along with Marfanoid habitus and pheochromocytoma. Answer A is incorrect because germline menin mutations are associated with multiple endocrine neoplasia type 1 (MEN1) syndrome, which does not typically manifest with mucosal neuromas. Answer B is incorrect because germline NF1 mutations are associated with neurofibromatosis type 1, which is more likely to develop neurofibromas. Answer C is incorrect because germline PRKAR1A mutations are associated with Carney complex, which does not typically manifest with mucosal neuromas. Answer E is incorrect because germline TSC mutations are associated with tuberous sclerosis, which does not typically manifest with mucosal neuromas.
Comment Here
Reference: Oral mucosal neuroma
Comment Here
Reference: Oral mucosal neuroma