Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2 | Practice question #3 | Practice answer #3 | Practice question #4 | Practice answer #4Cite this page: Rani A, Fatima S. Neurofibroma-general. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissueneurofibroma.html. Accessed September 13th, 2025.
Definition / general
- Neurofibroma is a benign peripheral nerve sheath tumor comprised of neuronal and fibrous components
- It is composed of Schwann cells, perineurial cells, fibroblasts, mast cells and interspersed myelinated and unmyelinated axons within a myxoid and collagenous extracellular matrix
Essential features
- Benign, unencapsulated, low cellularity, spindle cell neoplasm
- Stroma varies from myxoid to a shredded carrot collagenous appearance and contains interspersed mast cells
- S100 positive Schwannian cell population
- CD34 positive stromal component
Terminology
- Neurofibroma
ICD coding
Epidemiology
- All demographic groups are affected
- M = F
- 90% of cases occur sporadically, while the remaining cases are associated with neurofibromatosis type 1 (StatPearls: Neurofibroma [Accessed 24 December 2024])
- In both sporadic and syndromic cases, neurofibromas are a result of biallelic genetic inactivation of the tumor suppressor gene NF1 with complete loss of function of the NF1 gene product, neurofibromin (J Neurosci Res 2011;89:1451)
- In sporadic cases, only the lesional cells carry the NF1 mutation (J Neurosci Res 2011;89:1451)
- In syndromic cases, neurofibromas are the result of a germline mutation in NF1, encoding the tumor suppressor protein neurofibromin, on chromosome 17q11.2 (Handb Clin Neurol 2013;115:939)
- Majority of solitary lesions are sporadic
- Localized lesions most commonly occur in 20 - 40 year old adults (StatPearls: Neurofibroma [Accessed 24 December 2024])
- Multiple lesions are inherited in individuals with neurofibromatosis type 1 (NF1)
- Diffuse and plexiform types occur more frequently in children with neurofibromatosis type 1 (StatPearls: Neurofibroma [Accessed 24 December 2024])
Sites
- Most common site of involvement is the skin, where the tumors are solitary, localized and associated with small nerves
- Tumors of the diffuse and plexiform types show less frequent involvement of deeply situated medium sized nerves, nerve plexuses or major nerve trunks
- Localized neurofibromas can occur anywhere on the body, with a predilection for the trunk, head / neck and extremities
- Diffuse neurofibromas most commonly present on the head / neck (Int J Trichology 2010;2:60)
- Diffuse neurofibroma involves the skin and subcutaneous tissues in a plaque-like manner and infiltrates the muscle without destroying the overall morphologic features of the muscle
- Plexiform neurofibromas most commonly occur on the head / neck, trunk, extremities and spinal nerve roots that develop from cranial and large peripheral nerve sheaths (Annu Rev Pathol 2012;7:469)
Pathophysiology
- Subpopulation of Schwann cells is considered neoplastic (Am J Pathol 2001;159:57)
- NF1 gene encodes neurofibromin, a large protein with RAS GTPase activating (RAS GAP) activity
- Neurofibromin negatively regulates RAS signaling by promoting the conversion of the active GTP bound form of RAS (i.e., RAS GTP) to the inactive guanosine diphosphate (GDP) bound form (J Invest Dermatol 2023;143:1358)
- Complete loss of function of the NF1 gene product, neurofibromin (NF1), is considered prerequisite for tumor development
- Loss of NF1 results in increased RAS signaling → tumor development (Oncogene 2022;41:1235)
- RAS functions as part of a signal transduction pathway that is activated by growth factors and their receptors, including epidermal growth factor (EGF), nerve growth factor and platelet derived growth factor V
- Increased RAS GTP leads to increased signaling through RAF kinase
- RAF activates a kinase cascade involving MEK kinase and the Erkl and Erk2 isoforms of mitogen activated protein (MAP) kinase resulting in cell proliferation
- Increased RAS GTP protects cells from apoptosis by activating protein kinase B / Akt via phosphoinositide 3-OH kinase (PI3K) or by activation of NFκB
- Inflammatory signals mediated by various components of the microenvironment, such as mast cells, macrophages, lymphocytes and dendritic cells as well as Schwann cell interactions with axons are important for tumor development (J Clin Invest 2018;128:2848)
- Neurofibromin deficient Schwann cells secrete 5 times the normal kit ligand, which serves as a chemoattractant for mast cells expressing c-kit receptor
- Mast cells secret a variety of factors, including immunomodulatory factors (such as histamine) as well as profibrotic factor TGFβ, to induce fibroblasts to proliferate and deposit collagen (Oncogene 2021;40:5781)
Etiology
- According to WHO, etiology is unknown
Diagrams / tables
Clinical features
- Localized lesions: painless, violaceous papule, nodule or subcutaneous mass < 2 cm
- Have a characteristic buttonhole sign, where on palpation, the lesion retracts into the subcutis and reappears on the release of pressure (Annu Rev Pathol 2012;7:469)
- Diffuse lesions: ill defined, indurated plaques with thickened skin; mild numbness or tingling may occur if the lesion is large (Int J Trichology 2010;2:60)
- Plexiform neurofibromas
- Superficially presents as a skin colored or hyperpigmented nodular swelling
- Deep lesions arise from spinal nerve roots and present with pain, numbness, paresthesia, mass effect and sequelae of spinal nerve compression (Annu Rev Pathol 2012;7:469)
- Inherited lesions have close associations with neurofibromatosis type 1
- Clinical findings of neurofibromatosis type 1 include pigmented cutaneous macules, axillary or inguinal freckling, Lisch nodules, optic pathway gliomas and bone dysplasia
Diagnosis
- Physical examination
- Biopsy of lesion demonstrating classic histologic features
- Magnetic resonance imaging (MRI) or positron emission tomography (PET) / computed tomography (CT) may be utilized based on the size and location of the lesion
- 18F-FDG PET / CT: used to differentiate between benign and malignant tumors in neurofibroma patients (PLoS One 2015;10:e0143305)
Laboratory
- Melanoma inhibitory activity (MIA) in patients with neurofibromatosis type 1 with plexiform neurofibromas and cutaneous or subcutaneous neurofibromas
- Patients with plexiform neurofibromas had significantly higher levels of sAXL, midkine (MK) and fibroblast growth factor 2 (FGF2) (Neurology 2016;87:S40, Am J Transl Res 2022;14:3180)
Radiology description
- Ultrasound (Pan Afr Med J 2021;39:178)
- Shows mixed sonographic appearance
- Superficial subcutaneous portion is hyperechoic with small irregular hypoechoic areas
- Deep intramuscular masses appear hypoechoic
- CT: intense enhancement (Pan Afr Med J 2021;39:178)
- MRI
- T1: isointense or mildly hyperintense
- T2: hyperintense
- Target sign: a hyperintense rim and central area of low signal may be seen
- Fascicular sign: multiple small ring-like structures with peripheral hyperintensity representing the fascicular bundles within the nerves
- T1 C+ (Gd): heterogeneous enhancement (Radiopaedia: Neurofibroma [Accessed 24 December 2024])
- Superficial plexiform neurofibromas likely to be homogeneous (35%) or heterogeneous without targets
- Deep plexiform neurofibromas typically exhibit a target-like appearance on T2 weighted MR images, characterized by a central area of low signal intensity surrounded by a peripheral ring of high signal intensity (AJR Am J Roentgenol 2005;184:962)
Radiology images
Prognostic factors
- Localized cutaneous neurofibromas are consistently benign
- Atypical neurofibromatous neoplasms of uncertain biological potential (ANNUBP) are premalignant tumors, with the CDKN2A / CDKN2B deletion as the first step in the progression toward malignant peripheral nerve sheath tumor (MPNST) (Genes Chromosomes Cancer 2011;50:1021)
- Plexiform neurofibroma, ANNUBP and solitary intraneural neurofibroma arising in sizeable nerves are precursor lesions of MPNST
- Diffuse type neurofibroma rarely show transformation to MPNST (Am J Surg Pathol 2015;39:1234)
- Neurofibromatosis type 1 associated tumors carry a ~9 - 13% lifetime risk of developing an MPNST (Clin Sarcoma Res 2012;2:17)
Case reports
- 8 year old boy with pigmented neurofibroma and hypertrichosis (Bol Med Hosp Infant Mex 2023;80:57)
- 34 year old man with solitary giant neurofibroma of inguinal region (Sci Prog 2021;104:368504211004269)
- 65 year old woman with tracheal neurofibroma treated by repeated flexible bronchoscopic cryotherapy (Medicine (Baltimore) 2022;101:e29739)
- 68 year old man with palpebral tarsal solitary neurofibroma (Turk J Ophthalmol 2019;49:224)
- 78 year old man with hybrid neurofibroma / schwannoma of the orbit (Rev Esp Patol 2023;56:140)
Treatment
- Sporadic lesions not associated with neurofibromatosis type 1
- Surgical removal being the primary intervention for symptomatic cases
- Sometimes the lesion is inseparable from the parent nerve, which may require sacrificing the parent nerve by means of a complete excision
- Surgery is the mainstay treatment; however, complete resection is not possible in many cases, leading to incomplete resection with frequent recurrence
- MEKi selumetinib is FDA approved for the treatment of inoperable, symptomatic plexiform neurofibroma in pediatric neurofibromatosis type 1 patients (Clin Cancer Res 2021;27:4142)
- Investigation and trials for exploring the potential of targeting various cellular signaling pathways (such as Hippo, JAK / STAT, MAPK) or the tumor microenvironment (nerve cells, macrophages, mast cells, T cells) as future therapeutic strategies for neurofibromatosis are in process (Br J Cancer 2020;123:178)
- Destructive lasers, such as CO2 laser, are effective for treating multiple cutaneous neurofibromas simultaenously (Neurooncol Adv 2019;2:i107)
Clinical images
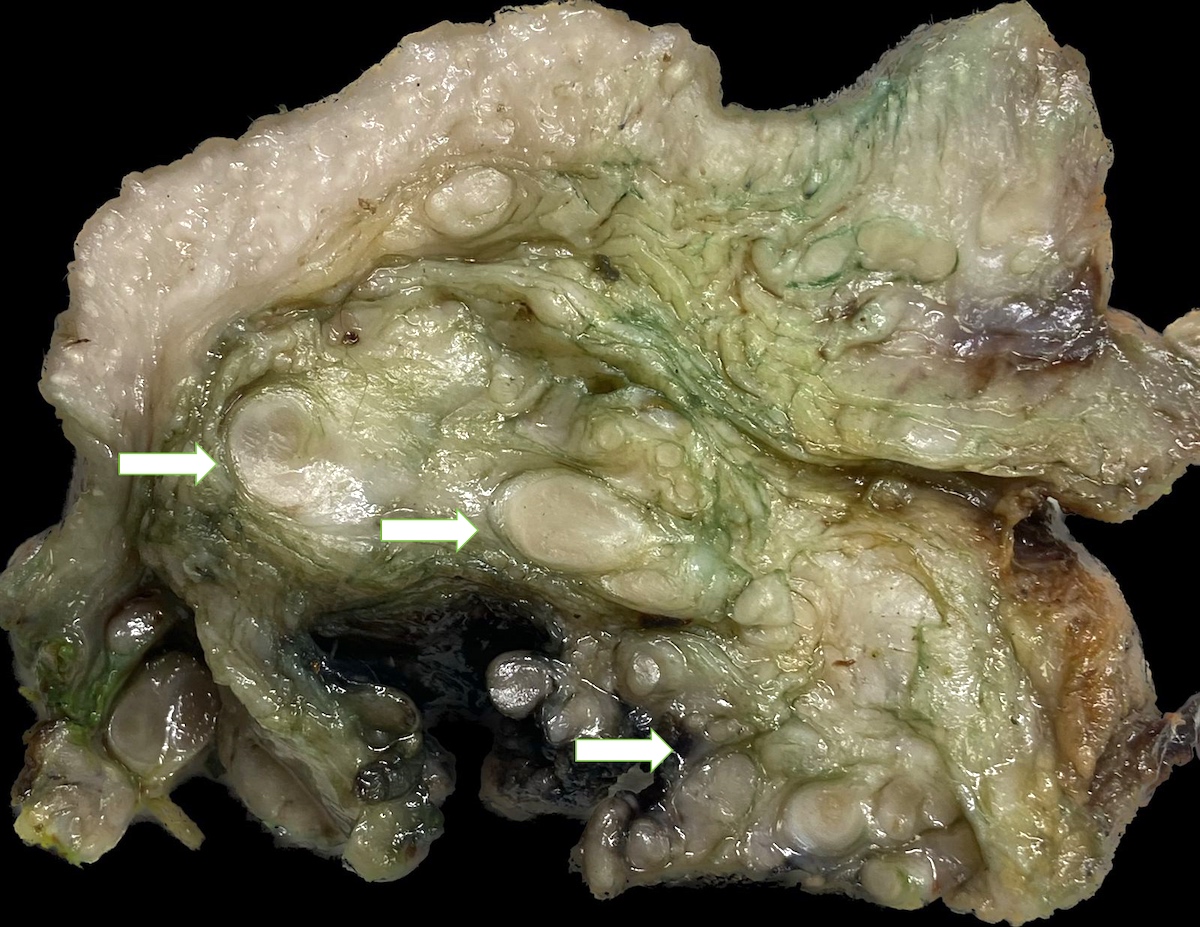
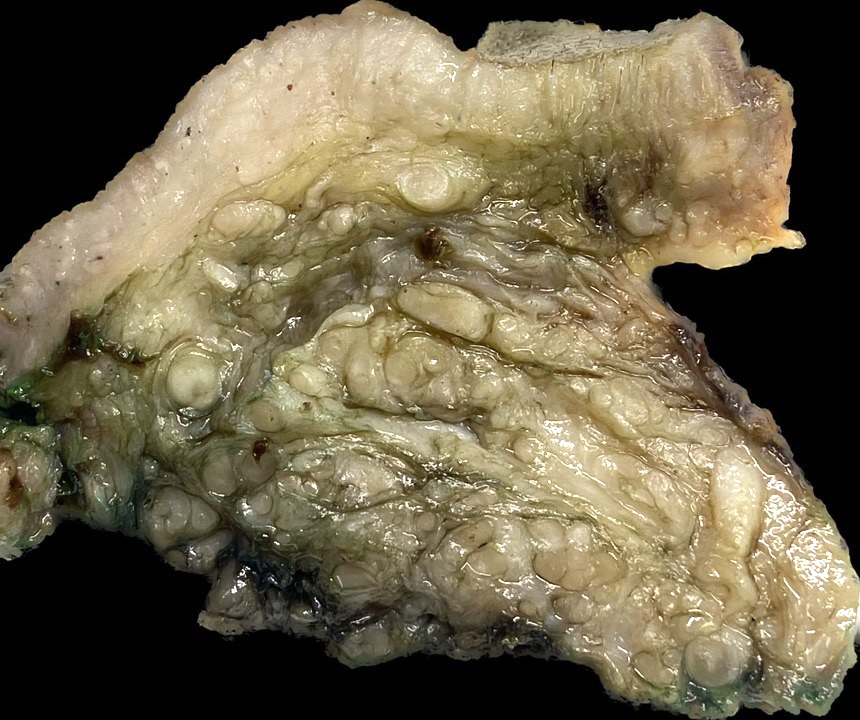
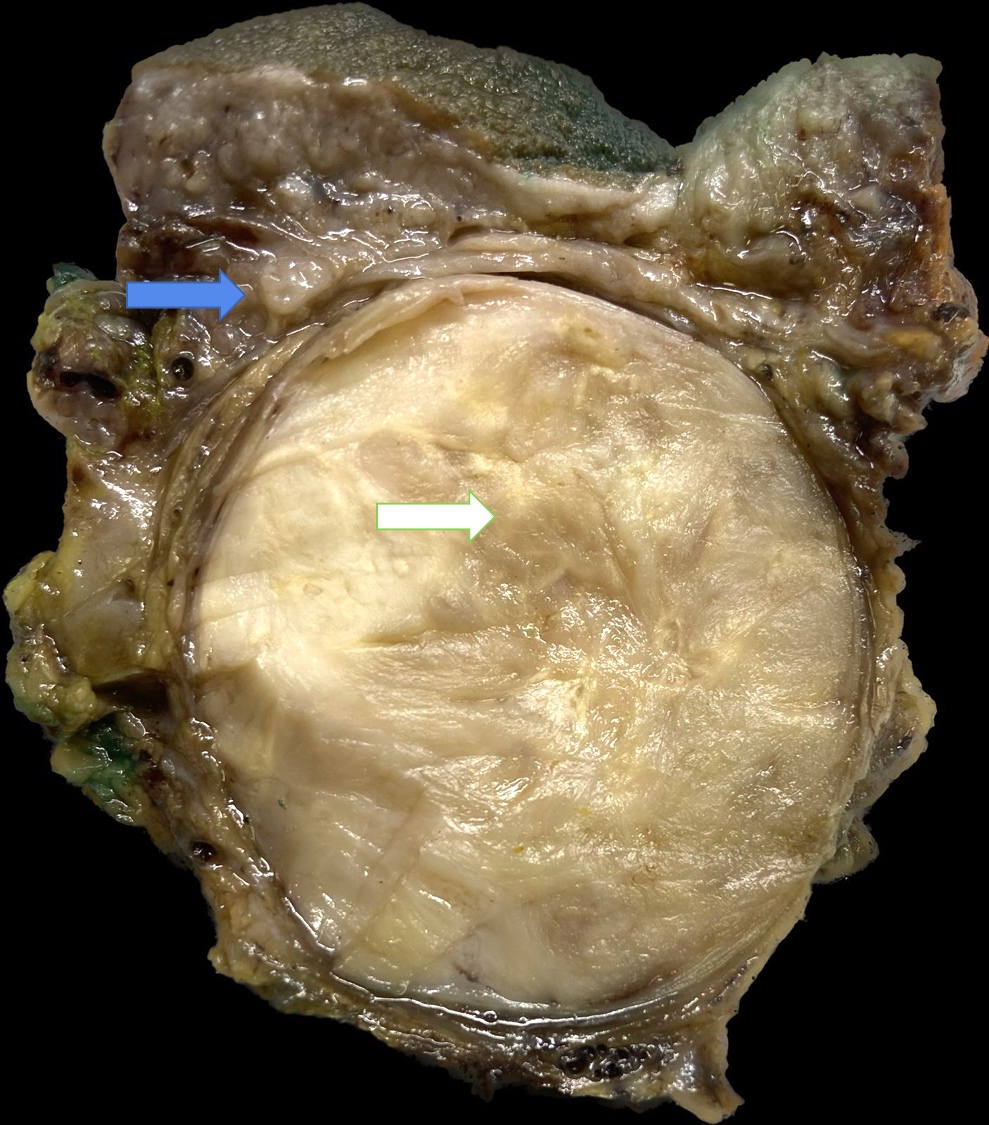
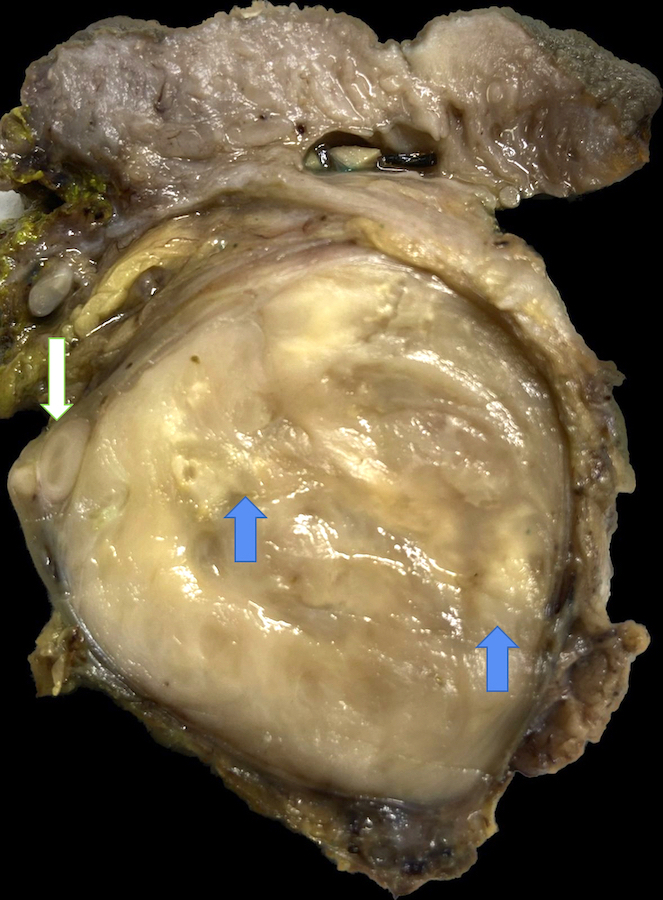
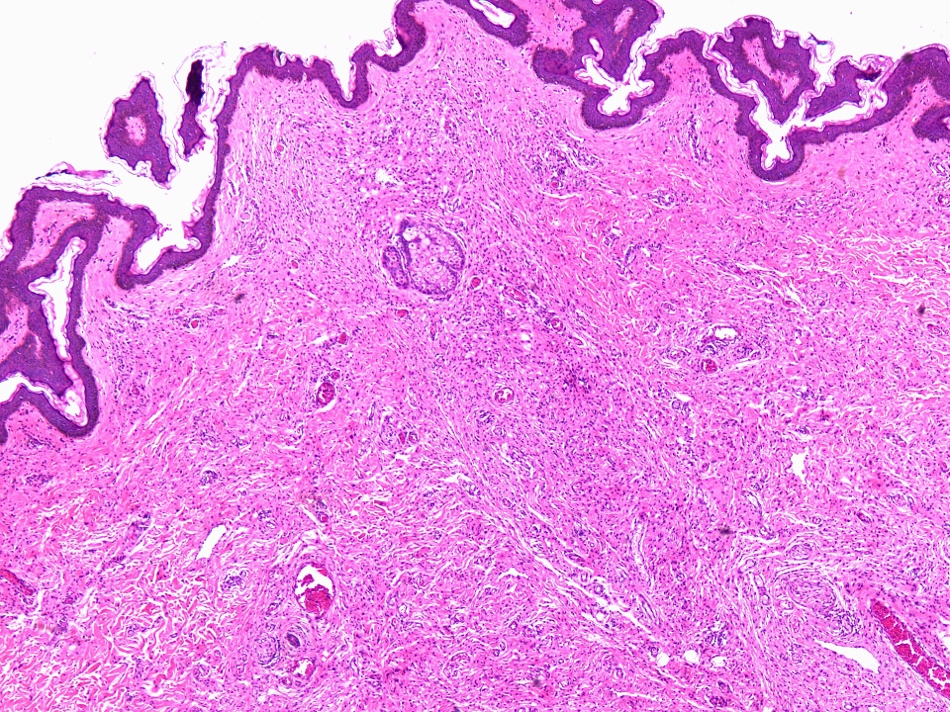
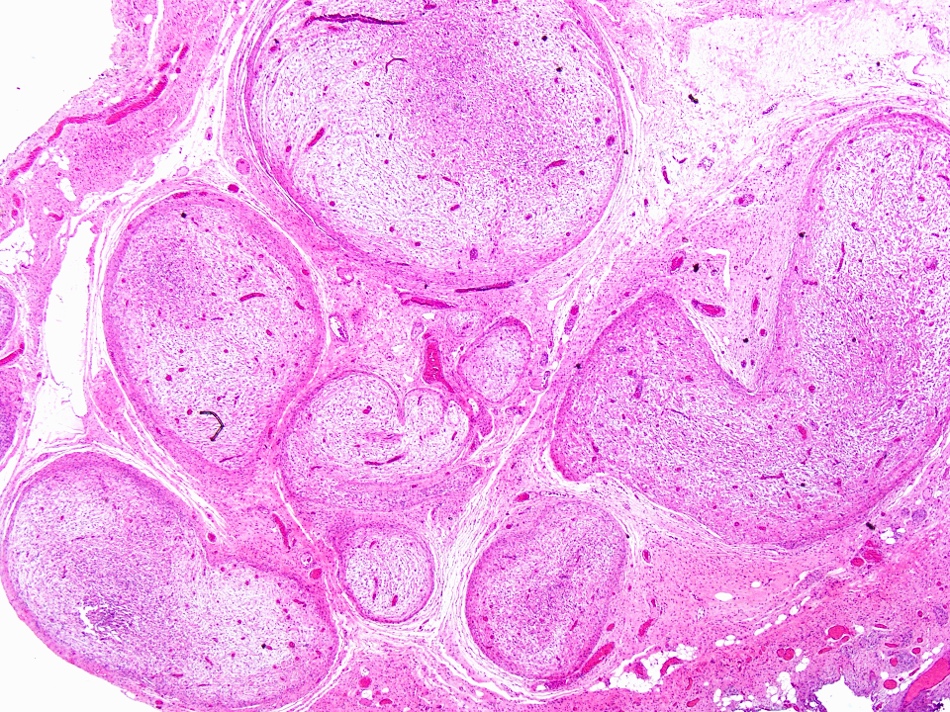
Gross description
- 5 macroscopic forms are distinguished: localized cutaneous, diffuse cutaneous, localized intraneural, plexiform intraneural and massive diffuse soft tissue tumor
- Localized cutaneous neurofibromas are nodular or polypoid lesions with homogenous, shiny, tan or grayish tan myxoid and translucent cut surface (Dermatopathology (Basel) 2022;10:1)
- Diffuse cutaneous neurofibromas can be flat, sessile, globular and pedunculated
- Intraneural neurofibromas present as solitary fusiform masses or as ropy to worm-like growths when plexiform
- Massive soft tissue neurofibromas range in shape from a relatively uniform regional soft tissue enlargement to pendulous bag-like masses
Gross images
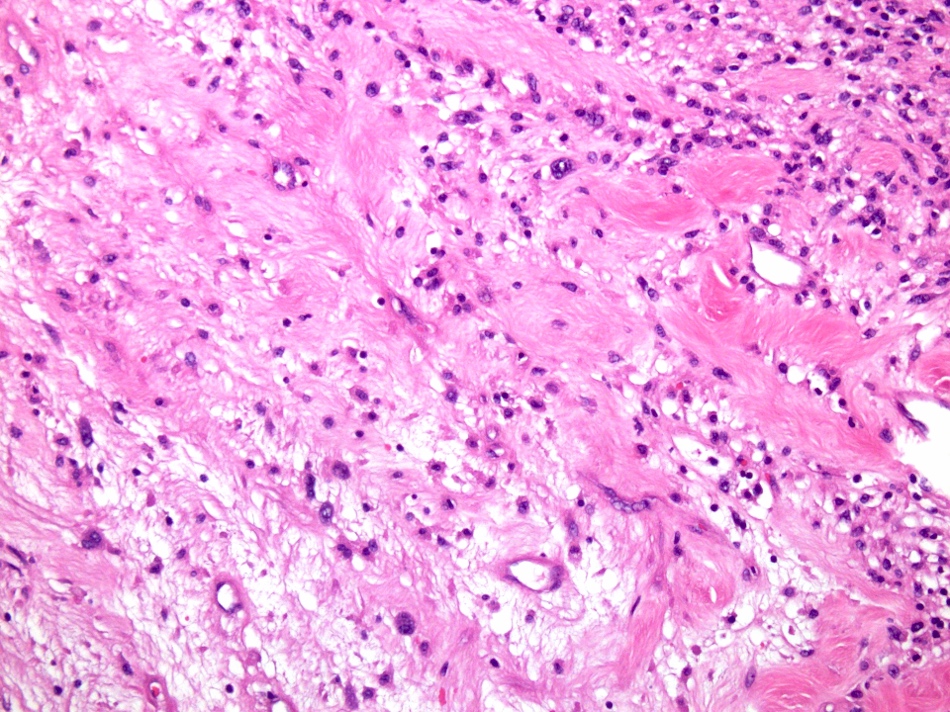
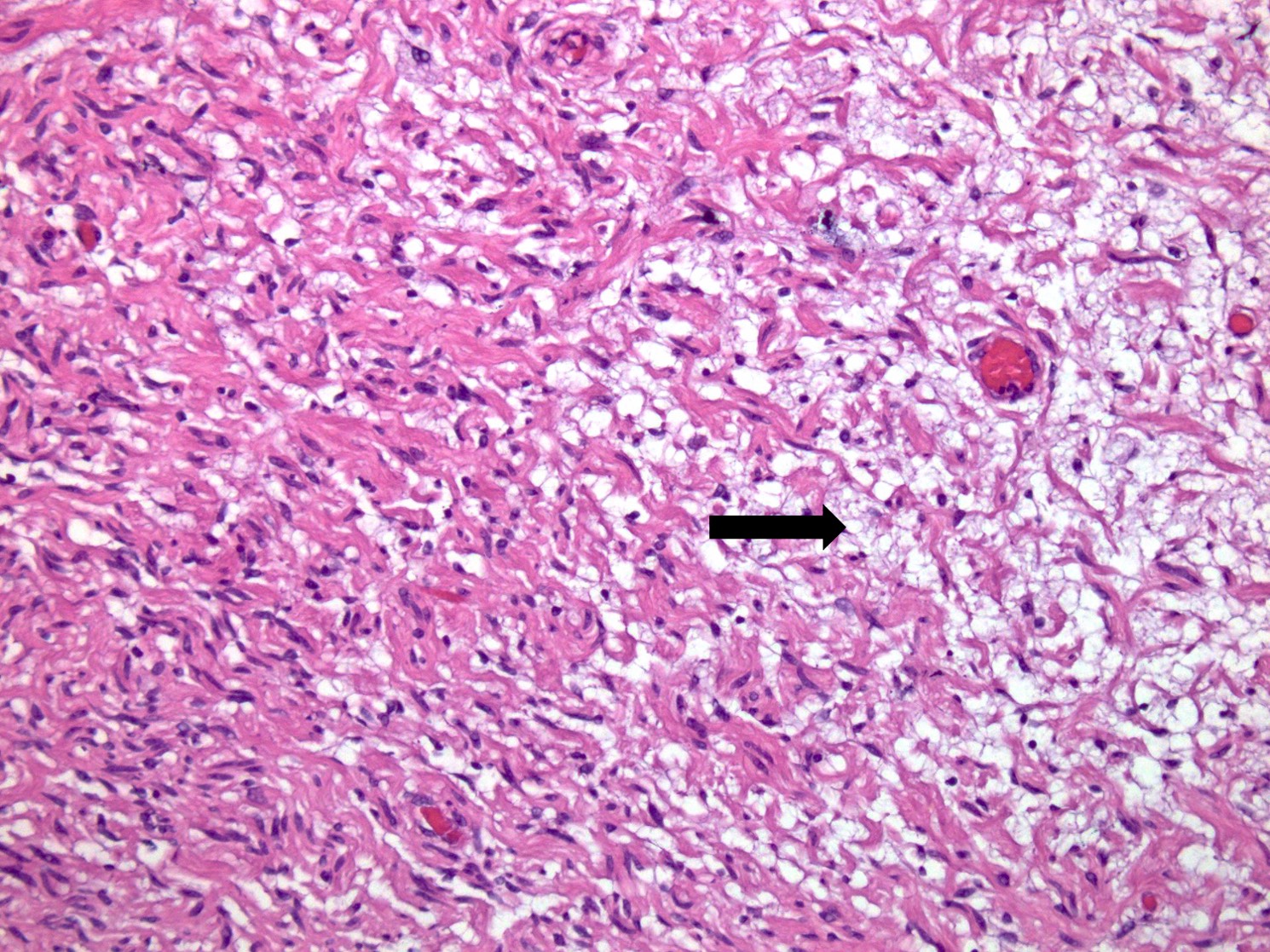
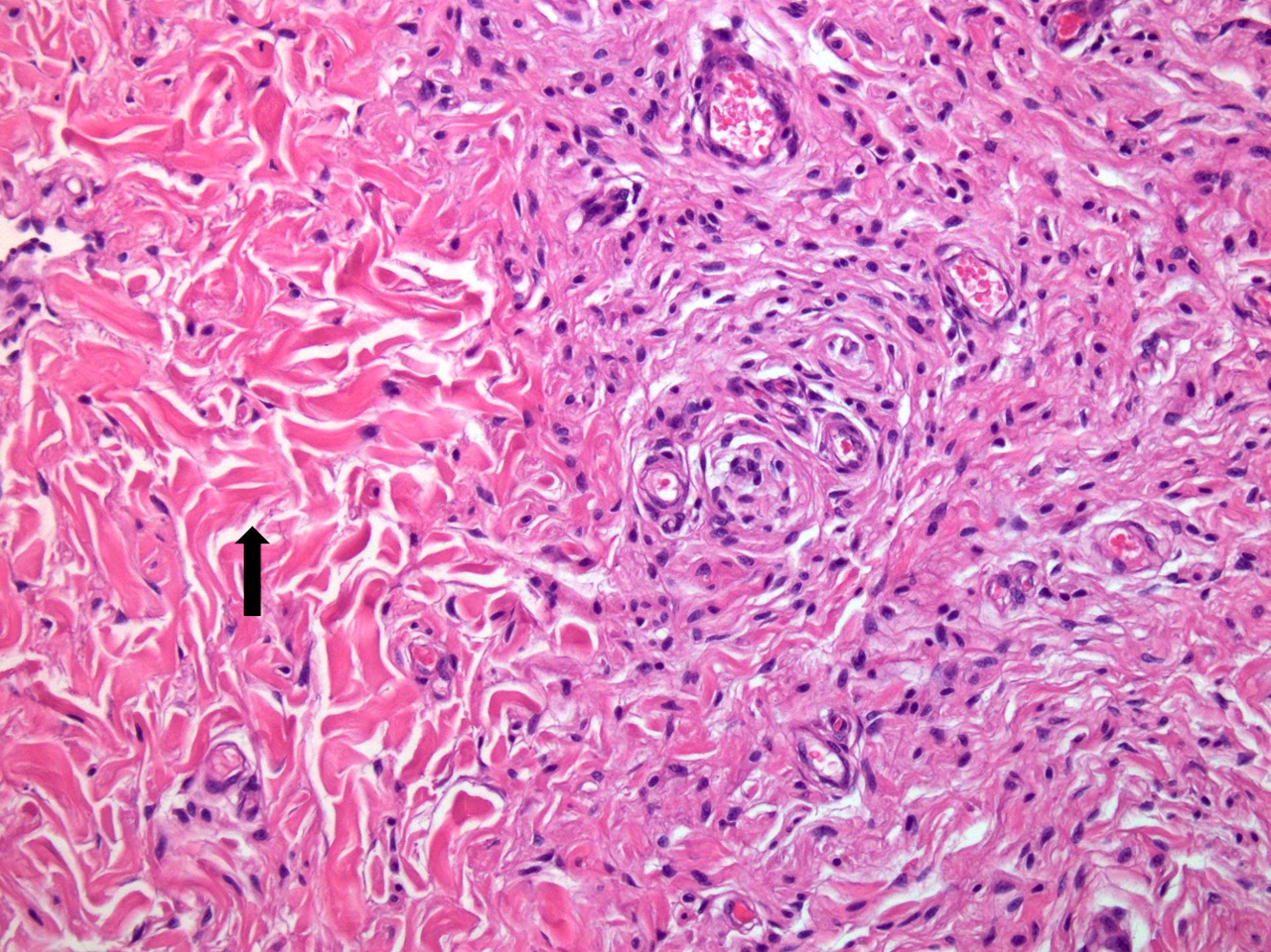
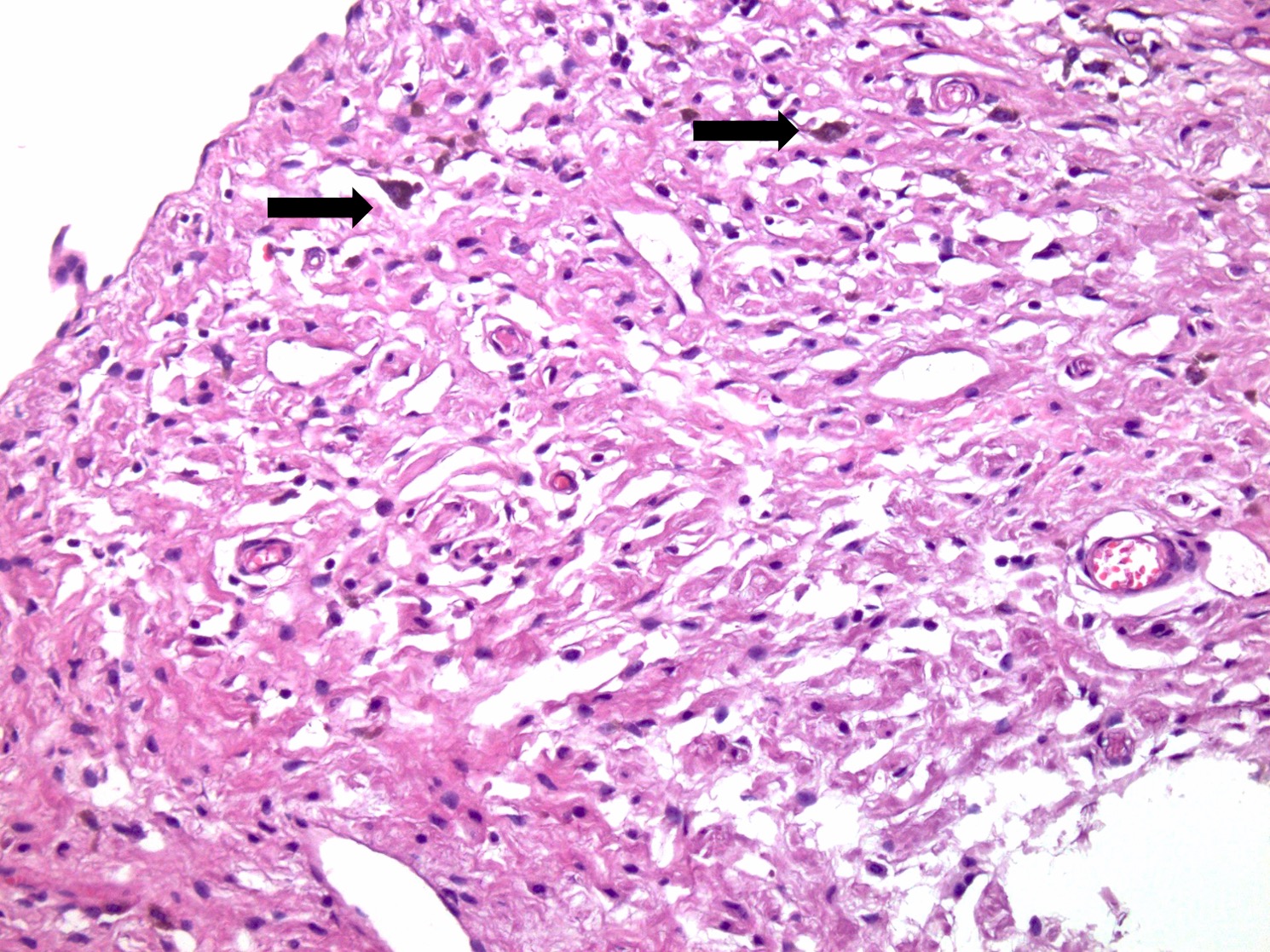
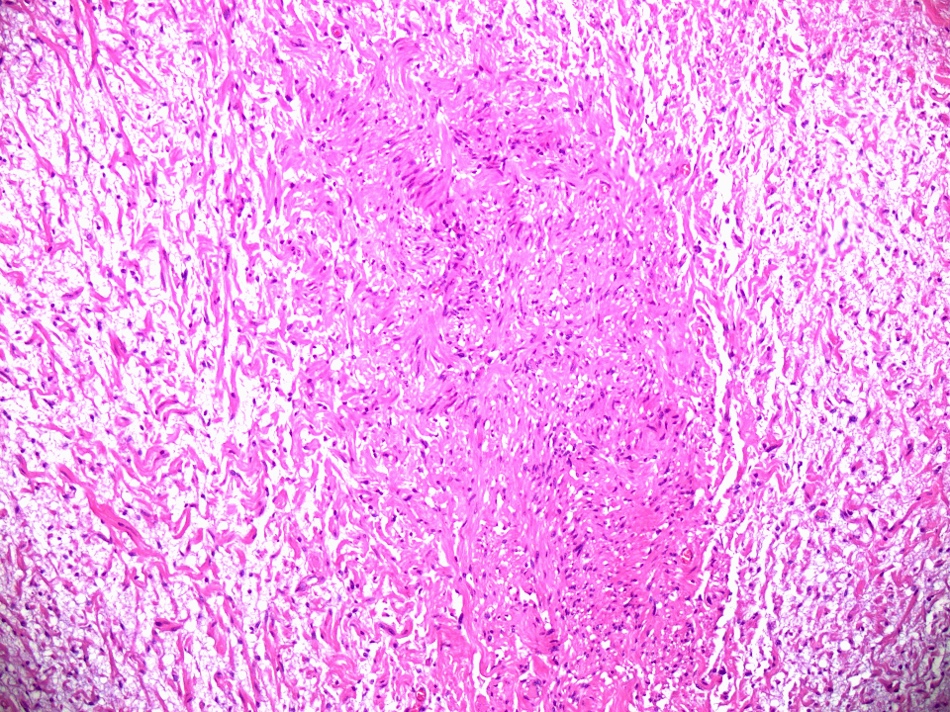
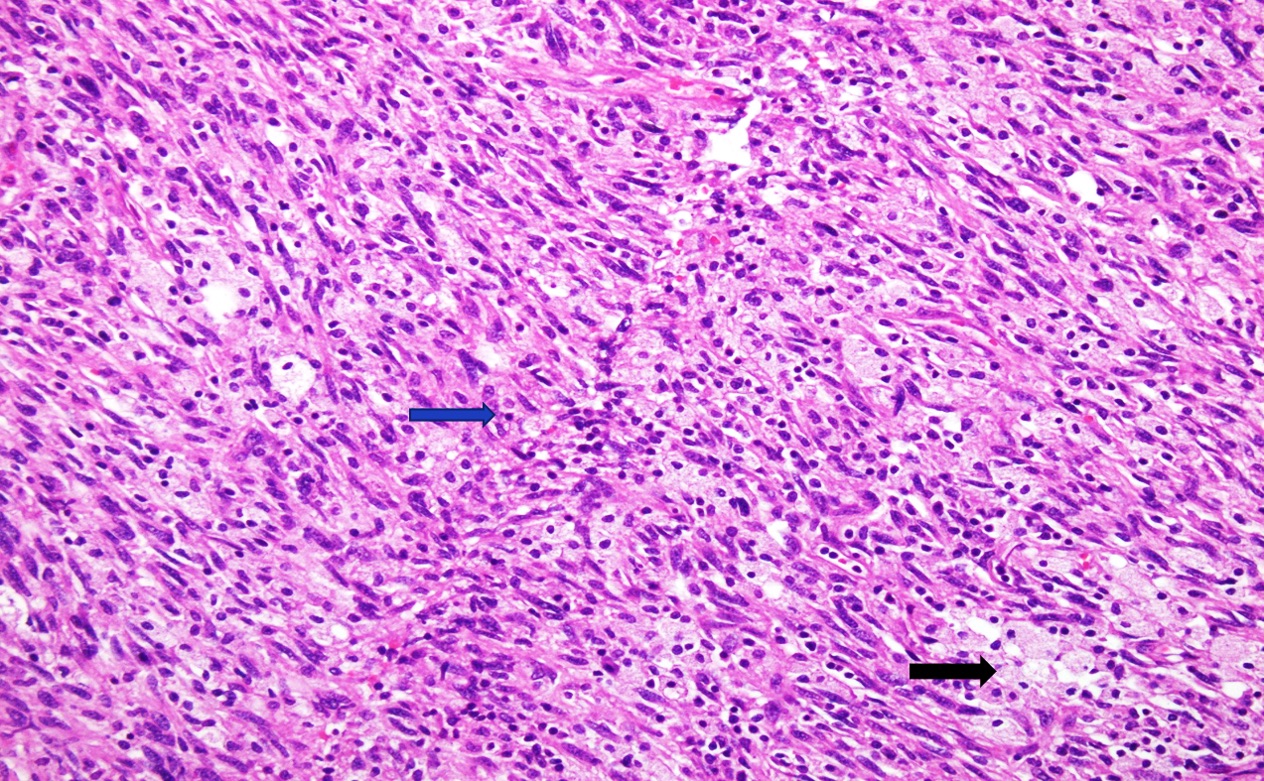
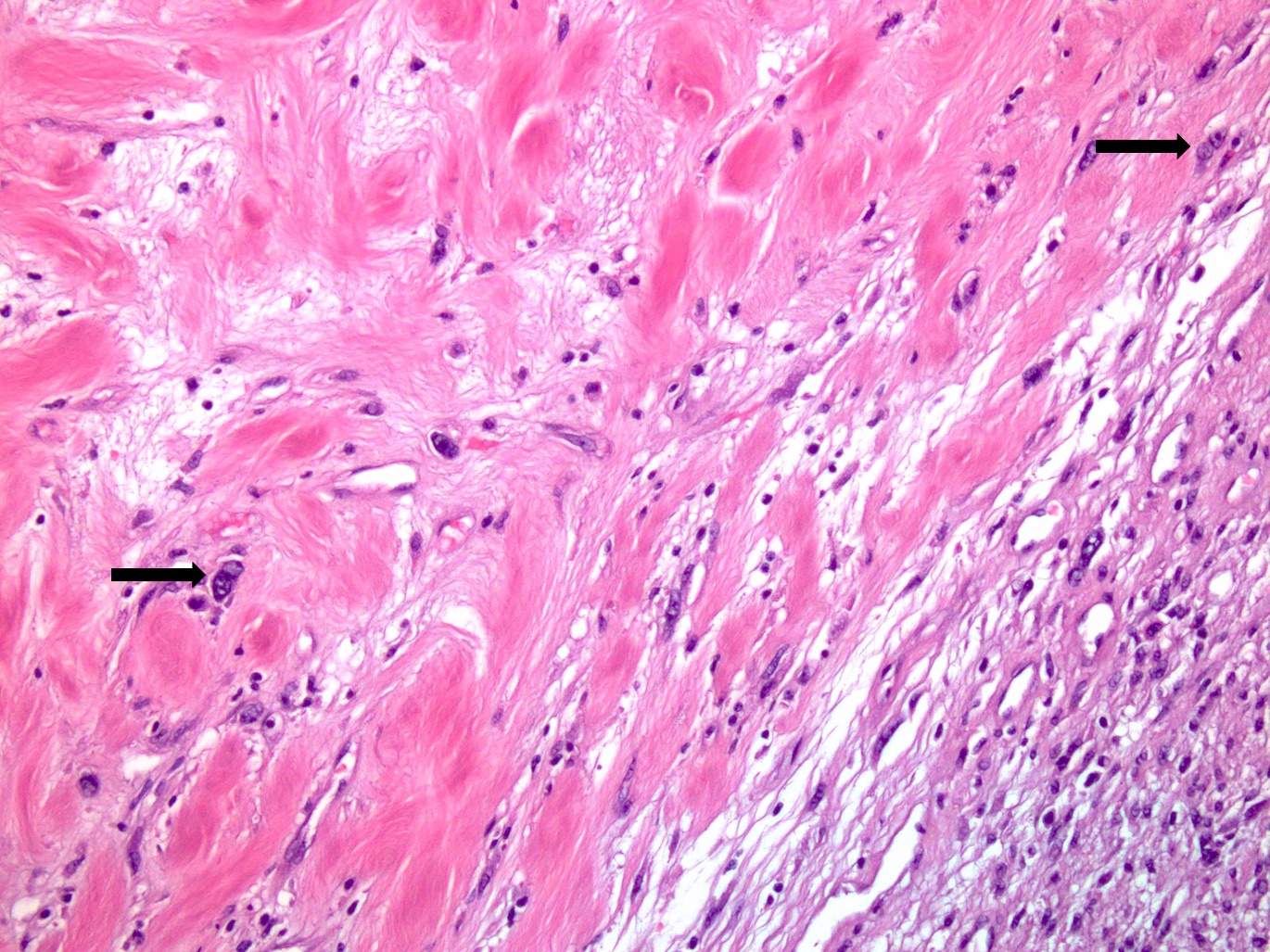
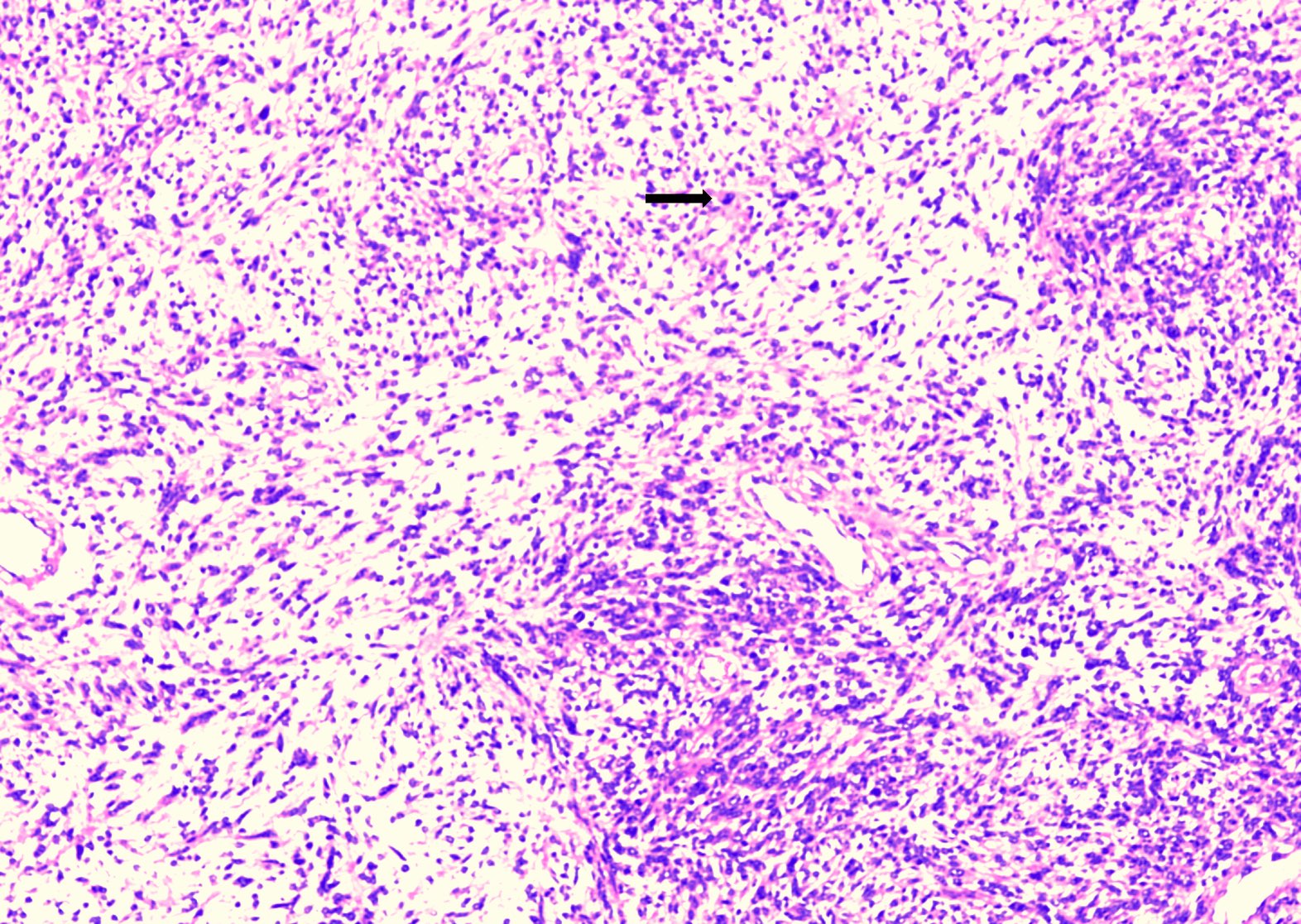
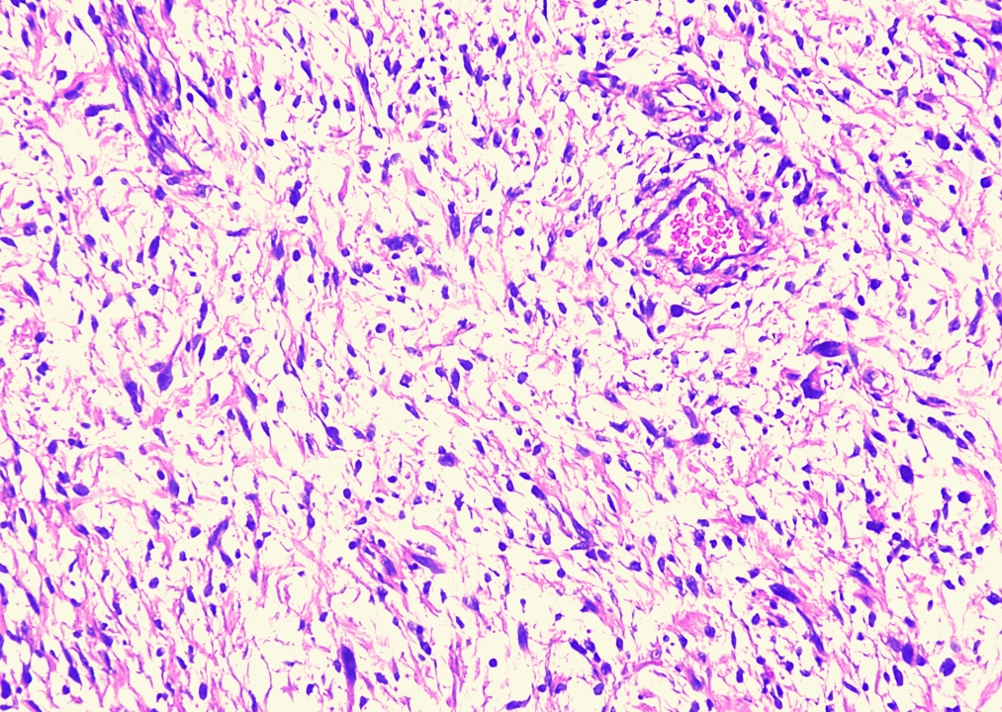
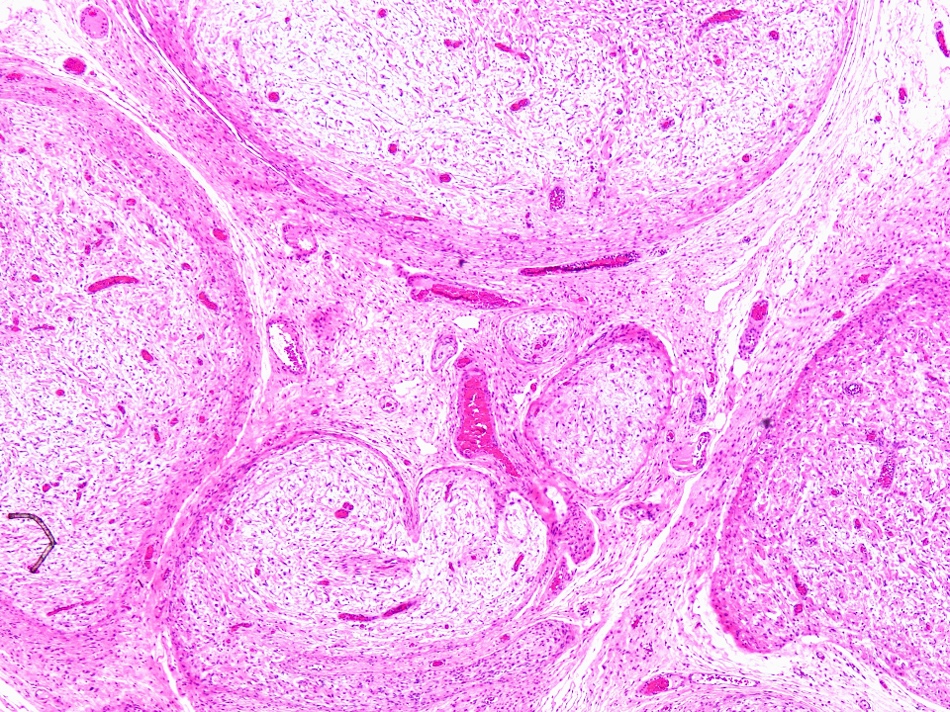
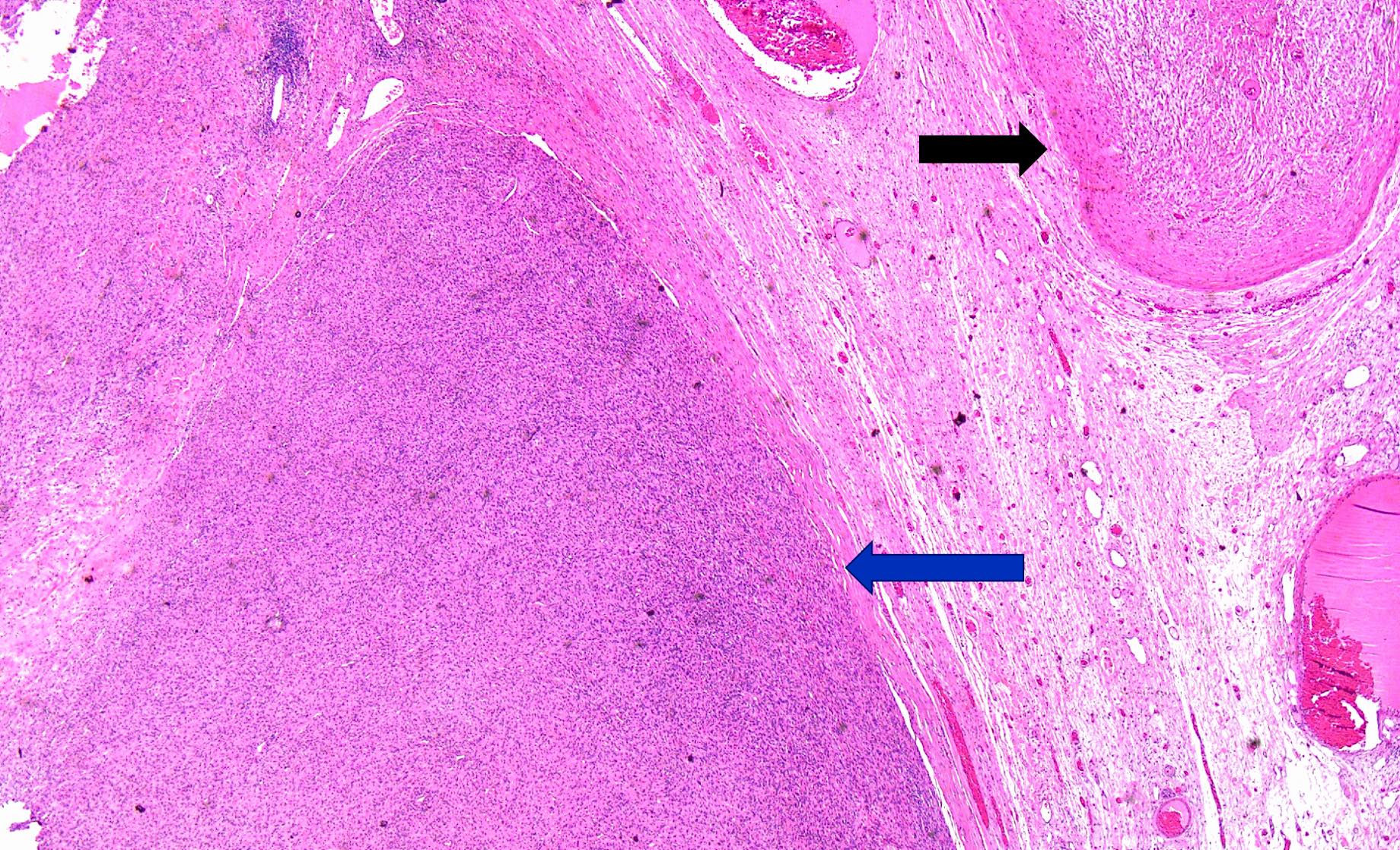
Microscopic (histologic) description
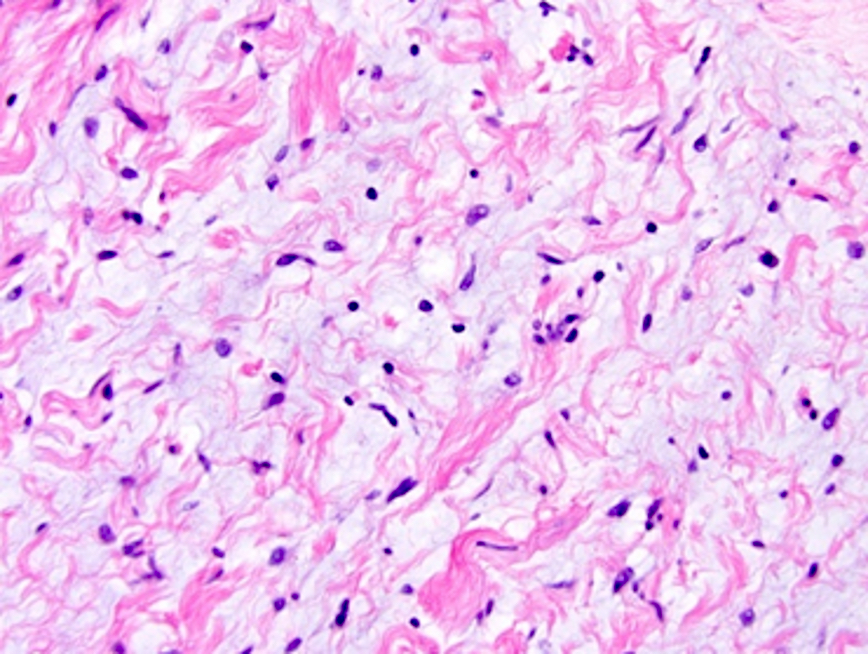
- Infiltrative, spindle cell neoplasm associated with a variably myxoid to collagenous stroma
- Neoplastic Schwann cells are represented by bland spindle shaped cells with thin, wavy nuclei (BMJ Case Rep 2021;14:e239887)
- Stromal collagen has a characteristic appearance resembling shredded carrots
- Other components include perineurial-like cells, fibroblasts and mast cells (Blood 2010;116:157)
- Histological characteristics may include Schwann cell nodules, onion bulbs, melanin pigment, metaplastic bone, epithelioid change and overt glandular differentiation (WHO)
- Nerve fibers are easily identifiable in intraneural subtypes
- Pseudomeissnerian bodies / corpuscles (round layered structures) are a typical feature of diffuse and plexiform neurofibromas
- Individual fascicles are enveloped by perineurium that is composed of EMA positive cells
- Subtypes
- Ancient neurofibroma: scattered atypical or bizarre nuclei with no increased mitoses
- Cellular neurofibroma: hypercellularity shows a fascicular growth pattern and lacks cytological atypia and mitotic activity
- Plexiform neurofibroma: multinodular, tortuous bundles of bland spindle cells consistent with expanded nerve branches, associated with neurofibromatosis type 1
- Refined consensus integrated diagnostic approach (histopathologic and genomic) for classification of NF1 associated peripheral nerve sheath tumors was proposed by multi-institutional expert pathology working group in 2024 (see Table) (Neuro Oncol 2025;27:616)
Microscopic (histologic) images
Virtual slides
Cytology description
- Often paucicellular
- Cellular cluster of small spindled cells with thin wavy nuclei
- Mucin rich background
- Fibrillar and collagenous stroma
- Reference: Int J Res Med Sci 2015;3:475
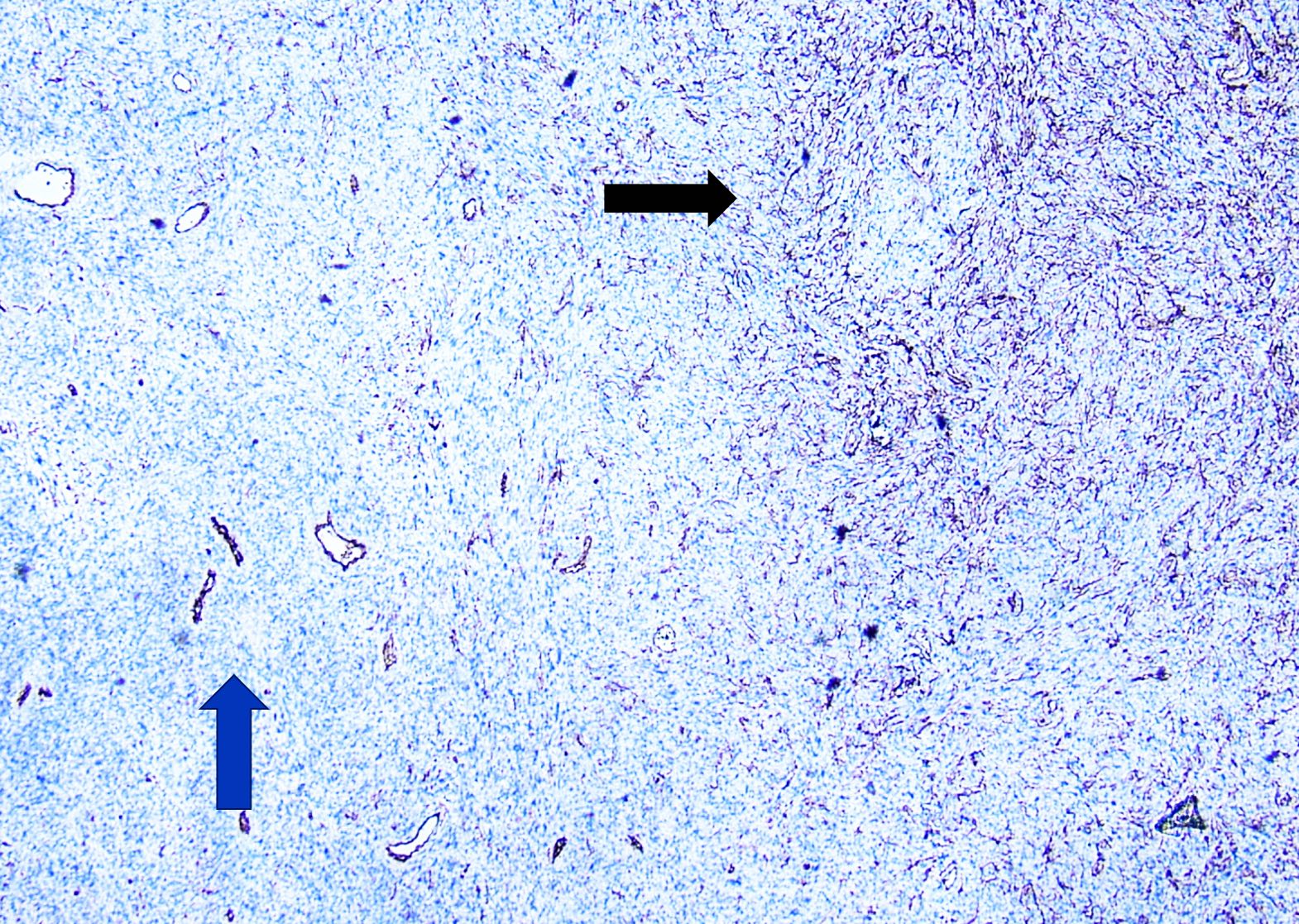
Positive stains
- S100, SOX10 and collagen type IV in scattered cells (unlike strong staining in schwannoma)
- CD34 (usually) lattice-like network
- Collagen type IV shows strong positivity, low Ki67
- Perineurial cells are EMA and GLUT1+ in plexiform but not in ordinary neurofibromas
- p16 (loss of p16 expression raises the possibility of ANNUBP in the setting of neurofibromatosis type 1) (Am J Pathol 1999;155:1879)
- H3K27me3 retained nuclear expression
Negative stains
- Cytokeratin, SMA, desmin, MelanA / MART1
- p53: as neurofibroma is a benign tumor, p53 is negative (p53 will be positive in MPNST)
Electron microscopy description
- Tumor contains neuronal axons, Schwann cells, fibroblasts (J Histochem Cytochem 2006;54:53)
- Peripheral nerves with mucinous degeneration
Electron microscopy images
Molecular / cytogenetics description
- Neurofibromas are the result of a germline mutation in NF1, encoding the tumor suppressor protein neurofibromin, on chromosome 17q11.2
- ANNUBP is strongly associated with deletions of the CDKN2A / CDKN2B locus encoding cell cycle regulators p16 (p16INK4a) and p14ARF (both encoded by CDKN2A) and p15 (p15INK4b; encoded by CDKN2B) (Neuro Oncol 2018;20:818)
- In animal models, loss of p53 and homozygous deletions CDKN2A gene in addition to NF1 is required to generate MPNSTs (Neurosurgery 2006;58:1)
Videos
Neurofibroma with floret cells
Neurofibroma
Sample pathology report
- Thigh mass, excision:
- Neurofibroma (see comment)
- Tumor size: 3.5 cm in greatest dimension
- Comment: Histologic sections contain an infiltrative neoplasm composed of differentiated Schwann cells, perineurial / perineurial-like cells, fibroblasts and mast cells, embedded in a myxoid and collagenous extracellular (shredded carrots) matrix. No histologic features of malignancy are identified.
- S100 positivity in the Schwannian cells, whereas CD34 highlights the stromal component.
Differential diagnosis
- Schwannoma:
- Peak incidence in the fourth to sixth decades
- Composed of Schwann cells
- Associated with somatic and germline mutations in NF2
- Histologically often more cellular, circumscribed, with Verocay bodies and Antoni A and B areas
- Immunohistochemistry: diffuse, uniform staining with S100 (Brain Pathol 2014;24:205)
- CD34 expression is seen in neurofibroma, highlighting a significant population of positive stromal cells (endoneurial fibroblasts) at the peripheral and within the fibrotic and myxoid areas, giving characteristic fingerprint pattern of staining; however, schwannoma is usually negative or shows only focal positivity in the peripheral zone (J Pathol Transl Med 2011;45:30)
- Malignant peripheral nerve sheath tumor:
- Most common locations are the trunk and extremities
- Seen in 20 - 50 year old patients
- Infiltrative growth, arising from peripheral nerve or pre-existing nerve sheath tumor
- Hypercellular, pleomorphic nuclei, high mitotic activity and necrosis
- Can show divergent differentiation
- Patchy S100 or negative (Oncogene 2022;41:2405)
- Loss of nuclear H3K27me3 in high grade tumor
- Dermatofibrosarcoma protuberans (DFSP):
- Most commonly on the trunk and the proximal extremities
- Young to middle aged adults
- Mesenchymal neoplasm with fibroblastic differentiation
- Lower mitotic activity, greater cellularity
- Interdigitation among lobules of fat yields a honeycomb pattern
- CD163-, CD34+ and factor XIIIa+
- COL1A1::PDGFB gene fusions (J Clin Med 2020;9:1752)
- Perineurioma:
- Most commonly arise on the lower limbs
- Slightly more common in females, with a peak in middle aged adults
- Storiform, whorled and lamellar architecture
- Composed of perineural cells which are typically slender, fibroblast-like in appearance with long, delicate cytoplasmic processes
- No definitive association with neurofibromatosis
- Expression of EMA; variable claudin1, GLUT1 and CD34 (Adv Clin Path 2000;4:25)
- Desmoplastic malignant melanoma:
- Sun exposed skin, most frequently in the head and neck region
- Males are more often affected
- Malignant neoplasm of spindled melanocytes encased in dense collagenous stroma, cytologic atypia and evidence of mitotic activity
- Associated with melanoma in situ
- Peripheral lymphoid aggregates (Head Neck Pathol 2023;17:143)
- Negative for melanocytic markers (e.g., HMB45, MelanA, tyrosinase)
- Positive for S100 protein and SOX10
- Dermal neurotized melanocytic nevus:
- Benign nevus with melanocytic nests and loose neurotized stroma
- Immunohistochemistry: positive for melanocytic markers (J Cutan Pathol 2005;32:45, Indian J Dermatol 2015;60:46)
- Nerve sheath myxoma:
- Young and middle aged adults
- Small superficial lesions in the distal extremities
- Myxoid neoplasm with multilobulated growth
- Unencapsulated, composed of bland spindle and epithelioid Schwann cells
- Immunopositivity for S100 (Int J Surg Case Rep 2020;73:183)
- Spindle cell lipoma:
- Subcutis of the posterior neck, back and shoulders
- Commonly affects 45 - 60 year old men
- Bland spindle cells, myxoid matrix, mature fat, ropy collagen
- Loss of RB1 by IHC staining (Am J Surg Pathol 2012;36:1119)
Additional references
Practice question #1
A 44 year old woman presented with a discrete, large, well defined homogenous tumor measuring 8.0 × 3.5 cm in the anteromedial compartment of the thigh. On histology, the lesion is composed of bland spindle cells with thin, wavy nuclei, immersed in a variably loose myxoid stroma as depicted in the above image. Immunohistochemical results showed positivity for CD34 and S100 protein. What is the diagnosis?
- Dermatofibrosarcoma protuberans
- Neurofibroma
- Schwannoma
- Traumatic neuroma
Practice answer #1
B. Neurofibroma. The histology in the description, morphology in the image and immunohistochemical profile are characteristic of neurofibroma.
Answer C is incorrect because the lesion lacks hypercellular and hypocellular areas and Verocay bodies. Also, schwannoma shows strong and diffuse positivity for only the S100 immunohistochemical stain.
Answer A is incorrect because the lesion lacks hypercellular neoplasm with fibroblastic differentiation, interdigitation into adipose tissue and COL1A1::PDGFB gene fusions.
Answer D is incorrect as the lesion lacks disorganized proliferation of nerve fascicles in a collagenous stroma.
Comment Here
Reference: Neurofibroma-general
Comment Here
Reference: Neurofibroma-general
Practice question #2
This type of neurofibroma is characterized by multinodularity involving multiple nerve fascicles, each surrounded in perineurium. It typically involves a large nerve or plexus, imparting a bag of worms or ropy appearance. This type is associated with which of the following?
- Cowden syndrome
- Gardner syndrome
- Neurofibromatosis 1
- Neurofibromatosis 2
Practice answer #2
C. Neurofibromatosis 1. The diagnosis in this case is plexiform neurofibroma and it has an association with neurofibromatosis 1. Answer A is incorrect because benign hamartomatous growth is associated with Cowden syndrome. Answer B is incorrect because colonic adenomatous polyps are associated with Gardner syndrome. Answer D is incorrect because schwannoma is associated with neurofibromatosis 2.
Comment Here
Reference: Neurofibroma-general
Comment Here
Reference: Neurofibroma-general
Practice question #3
Other than S100, which immunohistochemical stain is positive in neurofibroma?
- CD34
- CK5/6
- EMA
- HMB45
Practice answer #3
A. CD34. Neurofibroma shows CD34 positive stromal cells, which form a lattice-like network. Answers B, C and D are incorrect because these markers are negative in neurofibroma.
Comment Here
Reference: Neurofibroma-general
Comment Here
Reference: Neurofibroma-general
Practice question #4
Which of the following immunohistochemical stains best differentiates neurofibroma from schwannoma?
- Calretinin
- CD34
- CK5/6
- S100
Practice answer #4
B. CD34. In contrast to schwannoma, neurofibroma shows positive stromal cells, which form a lattice-like network. Answers A and C are incorrect because both neurofibroma and schwannoma are negative for calretinin and CK5/6. Answer D is incorrect because both are positive for S100.
Comment Here
Reference: Neurofibroma-general
Comment Here
Reference: Neurofibroma-general