Table of Contents
See also | Definition / general | Essential features | Terminology | Staging anatomy | Surgical margins | ICD coding | HPV mediated oropharyngeal primary squamous cell carcinoma (pT) | HPV mediated regional lymph nodes (pN) | AJCC clinical prognostic stage grouping for HPV mediated oropharyngeal squamous cell carcinoma | p16- oropharynx primary tumor (pT) | p16- hypopharynx primary tumor (pT) | p16- oropharynx and hypopharynx pathologic regional lymph nodes (pN) | Distant metastasis (pM) | AJCC clinical prognostic stage grouping for HPV unrelated oropharyngeal and hypopharyngeal squamous cell carcinoma | Registry data collection variables | Histologic grade | Histopathologic type | Diagrams / tables | Practice question #1 | Practice answer #1Cite this page: Magliocca K. Staging-oropharynx & hypopharynx. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/oralcavitystagingoropharynx.html. Accessed September 10th, 2025.
See also
Definition / general
- AJCC 8th edition staging has introduced a separate staging system for HPV mediated (p16+) squamous cell carcinomas of the oropharynx and HPV unrelated (p16-) squamous cell carcinoma of the oropharynx (AJCC: Cancer Staging [Accessed 20 September 2018], CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018])
- Testing with p16 immunohistochemistry is mandatory for all oropharyngeal squamous carcinomas but not for hypopharyngeal cancers
- If p16 testing is not performed on oropharyngeal carcinoma, that case is staged according to the system for p16- cancers
- AJCC level of evidence: II
- Cancers staged using the oropharynx (p16-) and hypopharynx staging system include
- p16- squamous cancers of the oropharynx
- Oropharyngeal cancers without a p16 immunostain performed
- All cancers of the hypopharynx
- Minor gland salivary cancers of the oropharynx and hypopharynx
- Neuroendocrine carcinoma of the oropharynx and hypopharynx
- Cancers staged using the oropharynx (p16+) staging system include
- HPV related squamous cell carcinoma of the oropharynx
- Note: p16 immunohistochemistry assessment is necessary only for squamous carcinomas
- Unknown primary (T0) with nodal positive disease should be staged using this section if a node is p16+ / HPV+ and no primary site is identified
- HPV related squamous cell carcinoma of the oropharynx
- Staging protocols, such as those of CAP, are to document procedure, tumor site, tumor laterality, tumor focality, tumor size, histologic type, histologic grade where applicable, margin status, lymphovascular invasion, perineural invasion, regional lymph node findings and summarize these pathologic findings using TNM system (CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018])
Essential features
- AJCC 7th edition staging was sunset on December 31, 2017; as of January 1, 2018, use of the 8th edition is mandatory
- Use of the CAP protocol is not required for recurrent tumors or for metastatic tumors that are resected at a different time than the primary tumor
- Use of this protocol is also not required for pathology reviews performed at a second institution (i.e. secondary consultation, second opinion or review of outside case at second institution) (CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018])
- Alternatively for providers practicing in different geographic regions, there may be interest in the International Collaboration on Cancer Reporting (ICCR) guidelines:
Terminology
- Synonyms for HPV mediated oropharyngeal carcinoma:
- HPV+ oropharyngeal carcinoma
- p16+ oropharyngeal carcinoma
- Nonkeratinizing oropharyngeal squamous cell carcinoma
Staging anatomy
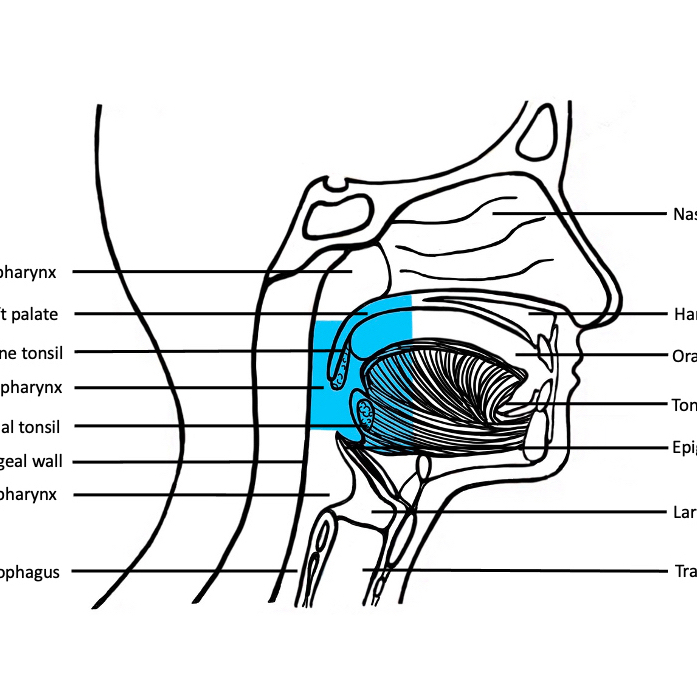
- Anatomic boundaries and primary site(s) of the pharynx: divided into 3 parts including the oropharynx, nasopharynx and hypopharynx
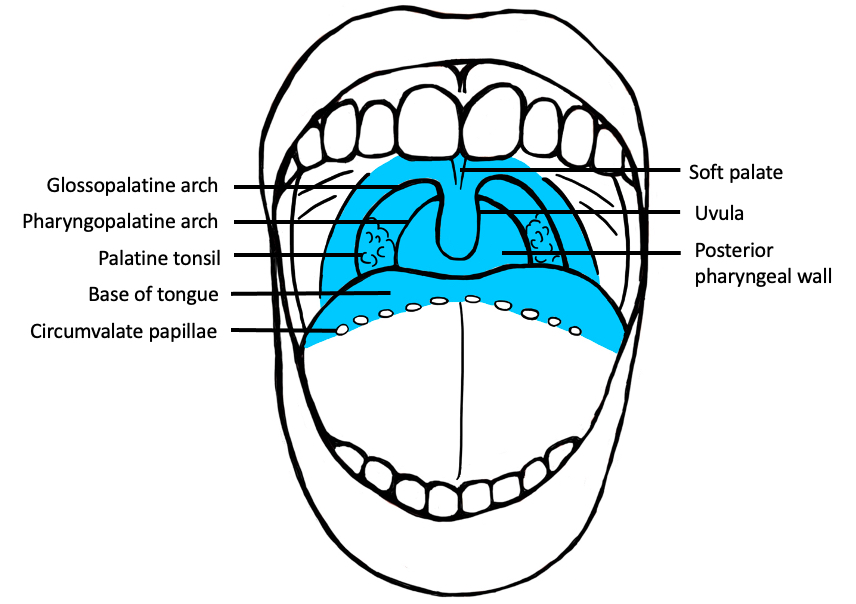
- Oropharynx (see figure 1 in Diagrams / tables) (CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018]):
- Portion of the continuity of the pharynx extending from the plane of the superior surface of the soft palate to the superior surface of the hyoid bone or floor of the vallecula
- Contents include:
- Soft palate
- Palatine tonsils
- Anterior and posterior tonsillar pillars
- Tonsillar fossa and tonsillar (faucial) pillars
- Uvula
- Base of tongue, including the lingual tonsils
- Vallecular
- Posterior oropharyngeal wall
- Nasopharynx (see figure 1 in Diagrams / tables) (CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018]):
- Situated behind the nasal cavity and above the soft palate; it begins anteriorly at the posterior choana and extends along the plane of the airway to the level of the free border of the soft palate
- Contents include:
- Nasopharyngeal tonsils (adenoids) lie along the posterior and lateral of the nasopharynx
- Orifice of Eustachian tube lies along the lateral aspects of the nasopharyngeal wall
- Fossa of Rosenmüller
- Hypopharynx (see figure 1 in Diagrams / tables) (CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Pharynx [Accessed 20 September 2018]):
- Portion of the pharynx extending from the plane of the superior border of the hyoid bone (or floor of the vallecula) to the plane corresponding to the lower border of the cricoid cartilage
- Contents include:
- Pyriform sinus (right and left): represents part of the hypopharynx which expands bilaterally and forward around the sides of the larynx and lies between the larynx and the thyroid cartilage
- Lateral and posterior hypopharyngeal walls
- Postcricoid region extending from the level of the arytenoid cartilage and connecting folds to the inferior border of the cricoid cartilage; it connects the 2 piriform sinuses, thereby forming the anterior wall of the hypopharynx
- Waldeyer ring:
- Formed by a ring or group of extranodal lymphoid tissues about the upper end of the pharynx (see figure 2 in Diagrams / tables) which consists of the:
- Palatine tonsils
- Pharyngeal tonsils (adenoids)
- Base of tongue / lingual tonsils
- Adjacent submucosal lymphatics
- Formed by a ring or group of extranodal lymphoid tissues about the upper end of the pharynx (see figure 2 in Diagrams / tables) which consists of the:
Surgical margins
- Historically, documentation of margin status for many oropharyngeal and hypopharyngeal tumors was not possible, as they were not oncologically resected but rather treated with chemotherapy and radiation
- With the advent of transoral robotic and laser surgery, however, intact resections have become increasingly common
- Limited evidence suggests that at the very minimum, a positive margin consists of invasive carcinoma present at the inked margin
- Akin to other sites, there is no standard definition of a "close" margin and definitions have ranged from 2 - 5 mm
- Despite the paucity of data, in keeping with other sites, the distance from the nearest margin should be recorded
- For hypopharyngeal and HPV- oropharyngeal tumors, in situ disease and high grade dysplasia is plausible and if present at a margin, the margin is considered positive in line with other sites
- When such lesions are identified in pharyngeal sites, they usually occur in association with an invasive carcinoma
- In this setting, the same criteria detailed in the oral cavity and laryngeal protocols apply (see CAP: Protocol for the Examination of Specimens from Patients With Cancers of the Lip and Oral Cavity [Accessed 20 September 2018] and CAP: Protocol for the Examination of Specimens From Patients With Cancers of the Larynx [Accessed 20 September 2018])
- For HPV+ oropharyngeal carcinoma, in situ disease for practical purposes is nonexistent, likely given its derivation from the specialized "lymphoepithelium" of tonsillar crypt; this has resulted in the elimination of pTis staging (AJCC: Cancer Staging [Accessed 20 September 2018])
ICD coding
- C01.9: Base of tongue, NOS
- C02.4: Lingual tonsil
- C05.1: Soft palate, NOS
- C05.2: Uvula
- C09.0: Tonsillar fossa
- C09.1: Tonsillar pillar
- C09.8: Overlapping lesion of tonsil
- C09.9: Tonsil, NOS
- C10.0: Vallecula
- C10.2: Lateral wall of oropharynx
- C10.3: Posterior pharyngeal wall
- C10.8: Overlapping lesion of oropharynx
- C10.9: Oropharynx, NOS
- C11.1: Pharyngeal tonsils
- C12.9: Pyriform sinus
- C13.0: Postcricoid region
- C13.1: Hypopharyngeal aspect of aryepiglottic fold
- C13.2: Posterior wall of hypopharynx
- C13.8: Overlapping lesion of hypopharynx
- C13.9: Hypopharynx, NOS
HPV mediated oropharyngeal primary squamous cell carcinoma (pT)
- pT0: no primary identified
- pT1: tumor ≤ 2 cm in greatest dimension
- pT2: tumor > 2 cm but ≤ 4 cm in greatest dimension
- pT3: tumor > 4 cm in greatest dimension or extension to lingual surface of epiglottis
- pT4: tumor of any size invading adjacent organ(s), such as larynx, extrinsic muscle of tongue, medial pterygoid, hard palate or mandible
Notes:
- Mucosal extension to lingual surface of epiglottis from primary tumor of the base of tongue and vallecular does not constitute invasion of the larynx
HPV mediated regional lymph nodes (pN)
- pNX: regional lymph nodes cannot be assessed
- pN0: no regional lymph node metastasis
- pN1: metastasis in ≤ 4 lymph nodes
- pN2: metastasis in > 4 lymph nodes
Notes:
- Per AJCC 8th edition, for pN, a selective neck dissection ordinarily will include 10+ lymph nodes and a comprehensive neck dissection (radical or modified radical neck dissection) ordinarily will include 15+ lymph nodes
- Negative pathologic examination of a smaller number of nodes still mandates a pN0 designation
AJCC clinical prognostic stage grouping for HPV mediated oropharyngeal squamous cell carcinoma
| Stage I: | T0 - 2 | N0 - 1 | M0 |
| Stage II: | T0 - 2 | N2 | M0 |
| T3 - 4 | N0 - 1 | M0 | |
| Stage III: | T3 - 4 | N2 | M0 |
| Stage IV: | Any T | Any N | M1 |
HPV unrelated (p16-) oropharyngeal and hypopharyngeal squamous cell carcinoma
p16- oropharynx primary tumor (pT)
- pTX: primary tumor cannot be assessed
- pTis: carcinoma in situ
- pT1: tumor ≤ 2 cm in greatest dimension
- pT2: tumor > 2 cm but ≤ 4 cm in greatest dimension
- pT3: tumor > 4 cm in greatest dimension or extension to lingual surface of epiglottis
- pT4a: tumor of any size invading adjacent organ(s), such as larynx, extrinsic muscle of tongue, medial pterygoid, hard palate or mandible
- pT4b: tumor of any size invading adjacent organ(s), such as lateral pterygoid muscle, pterygoid plates, lateral nasopharynx, skull base or encases carotid artery
Notes:
- Mucosal extension to lingual surface of epiglottis from primary tumor of the base of tongue and vallecular does not constitute invasion of the larynx
p16- hypopharynx primary tumor (pT)
- pTX: primary tumor cannot be assessed
- pTis: carcinoma in situ
- pT1: tumor limited to one subsite of hypopharynx or ≤ 2 cm in greatest dimension
- pT2: tumor invades > 1 subsite of hypopharynx or an adjacent site or tumor > 2 cm but ≤ 4 cm in greatest dimension without fixation of hemilarynx
- pT3: tumor > 4 cm in greatest dimension or with fixation of hemilarynx or extension to esophageal mucosa
- pT4a: tumor of any size invading thyroid / cricoid cartilage, hyoid bone, thyroid gland, esophageal muscle or central compartment soft tissue (central compartment soft tissue includes prelaryngeal strap muscles and subcutaneous fat)
- pT4b: tumor of any size invading prevertebral fascia, encases carotid artery or involves mediastinal structures
p16- oropharynx and hypopharynx pathologic regional lymph nodes (pN)
- pNX: regional lymph nodes cannot be assessed
- pN0: no regional lymph node metastasis
- pN1: metastasis in a single ipsilateral lymph node, ≤ 3 cm and extranodal extension (ENE)-
- pN2: metastasis in a single ipsilateral lymph node, ≤ 3 cm in greatest dimension and ENE+; or > 3 cm but ≤ 6 cm in greatest dimension and ENE-; or metastases in multiple ipsilateral lymph nodes, none > 6 cm in greatest dimension and ENE-; or in bilateral or contralateral lymph node(s), none > 6 cm in greatest dimension and ENE-
- pN2a: metastasis in either
- Single ipsilateral lymph node that is ≤ 3 cm and ENE+ or
- Single ipsilateral lymph node that is > 3 cm but ≤ 6 cm in greatest dimension and ENE-
- pN2b: metastasis in multiple ipsilateral lymph nodes, none > 6 cm in greatest dimension and ENE-
- pN2c: metastasis in bilateral or contralateral lymph node(s), none > 6 cm in greatest dimension and ENE-
- pN2a: metastasis in either
- pN3: metastasis in a lymph node > 6 cm in greatest dimension and ENE-; or in a single ipsilateral node > 3 cm in greatest dimension and ENE+; or multiple ipsilateral, contralateral or bilateral nodes, any with ENE+; or a single contralateral node of any size and ENE+
- pN3a: metastasis in a lymph node that is > 6 cm in greatest dimension and ENE-
- pN3b: metastasis in either
- Single ipsilateral lymph node, > 3 cm and ENE+ or
- Multiple ipsilateral, contralateral or bilateral lymph nodes, any with ENE+ or
- Single contralateral lymph node of any size and ENE+
Notes:
- Designation of "U" or "L" may be used for any N category to indicate metastasis above the lower border of the cricoid (U) or below the lower border of the cricoid (L)
- Per AJCC 8th edition, for pN, a selective neck dissection ordinarily will include 10+ lymph nodes and a comprehensive neck dissection (radical or modified radical neck dissection) ordinarily will include 15+ lymph nodes
- Negative pathologic examination of a smaller number of nodes still mandates a pN0 designation
- Midline nodes are considered ipsilateral nodes
Distant metastasis (pM)
- pM0: no distant metastasis
- pM1: distant metastasis
Registry data collection variables
- ENE clinical (present versus absent)
- ENE pathological (present versus absent)
- Extent of microscopic ENE (distance of extension from the native lymph node capsule to the farthest point of invasion in extranodal tissue)
- Perineural invasion
- Lymphovascular invasion
- p16 / HPV status
- Performance status
- Tobacco use and pack year
- Alcohol use
- Depression diagnosis
Histologic grade
- GX: cannot be assessed
- G1: well differentiated
- G2: moderately differentiated
- G3: poorly differentiated
Notes:
- No grading system exists for HPV mediated oropharyngeal carcinoma
- For histologic types of carcinomas that are amenable to grading, 3 histologic grades are suggested, as shown below
- For conventional squamous cell carcinoma, histologic grading as a whole does not perform well as a prognosticator
- Nonetheless, it should be recorded when applicable, as it is a basic tumor characteristic
- Selecting either the most prevalent grade or the highest grade for this synoptic protocol is acceptable
- Variants of squamous cell carcinoma (i.e. verrucous, basaloid, etc.) have an intrinsic biologic potential and currently do not appear to require grading
- Histologic (microscopic) grading of salivary gland carcinomas has been shown to be an independent predictor of behavior and plays a role in optimizing therapy
- However, most salivary gland carcinoma types have an intrinsic biologic behavior and attempted application of a universal grading scheme is merely a crude surrogate
- Thus a generic grading scheme is no longer recommended for salivary gland carcinomas
- Carcinoma types for which grading systems exist and are relevant are incorporated into histologic type
- 3 major categories that are amenable to grading include adenoid cystic carcinoma, mucoepidermoid carcinoma and adenocarcinoma, not otherwise specified
- In some carcinomas, histologic grading may be based on growth pattern, such as in adenoid cystic carcinoma, for which a histologic high grade variant has been recognized based on the percentage of solid growth
- Those adenoid cystic carcinomas showing ≥ 30% of solid growth pattern are considered to be histologically high grade carcinomas
- Histologic grading of mucoepidermoid carcinoma includes a combination of growth pattern characteristics (e.g. cystic, solid, neurotropism) and cytomorphologic findings (e.g. anaplasia, mitoses, necrosis)
- Adenocarcinomas, not otherwise specified, do not have a formalized grading scheme and are graded intuitively based on cytomorphologic features
Histopathologic type
- Carcinoma of the oropharynx and hypopharynx
- Squamous cell carcinoma
- Human papillomavirus (HPV) mediated (positive) squamous cell carcinoma (oropharynx only)*
- HPV unrelated (negative) squamous cell carcinoma (oropharynx and hypopharynx)*
* Modification based on separation of HPV mediated (positive) and HPV unrelated (negative) oropharyngeal squamous cell carcinoma in the AJCC 8th edition and WHO 4th edition
- Variants of squamous cell carcinoma
- Keratinizing
- Nonkeratininizing
- Acantholytic squamous cell carcinoma
- Adenosquamous carcinoma
- Basaloid squamous cell carcinoma
- Papillary squamous cell carcinoma
- Spindle cell squamous cell carcinoma
- Verrucous squamous cell carcinoma
- Lymphoepithelial carcinoma
- Squamous cell carcinoma
- Carcinoma of minor salivary gland
- Acinic cell carcinoma
- Adenoid cystic carcinoma
- Adenocarcinoma, NOS
- Basal cell adenocarcinoma
- Carcinoma ex pleomorphic adenoma
- Carcinoma type cannot be determined
- Carcinosarcoma
- Clear cell adenocarcinoma
- Cystadenocarcinoma
- Epithelial myoepithelial carcinoma
- Mammary analogue secretory carcinoma
- Mucoepidermoid carcinoma
- Mucinous carcinoma
- Myoepithelial carcinoma
- Oncocytic carcinoma
- Polymorphous adenocarcinoma
- Salivary duct carcinoma
- Neuroendocrine carcinoma
- Small cell neuroendocrine carcinoma, HPV-
- Small cell neuroendocrine carcinoma, HPV+
- Large cell neuroendocrine carcinoma, HPV-
- Large cell neuroendocrine carcinoma, HPV+
Diagrams / tables
Practice question #1
With respect to HPV mediated oropharyngeal squamous cell carcinoma, which of the following is not a recognized pT stage under AJCC 8th edition?
- pTis
- pT0
- pT1
- pT2
- pT3
Practice answer #1