Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Medeiros F. Placenta accreta, increta and percreta. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/placentaplacentaaccreta.html. Accessed September 27th, 2025.
Definition / general
- Abnormal placental adherence to the uterine wall
- Placenta accreta: villi implant on the myometrial surface without intervening decidua
- Placenta increta: villi extend into the myometrium
- Placenta percreta: villi penetrate the entire myometrial thickness and through the uterine serosa
Essential features
- Patients with previous cesarean sections and placenta previa are at high risk for the development of abnormal placental implantation, which includes
- Placenta accreta: villi implant on the myometrial surface without intervening decidua
- Placenta increta: villi extend into the myometrium
- Placenta percreta: villi penetrate the entire myometrial thickness and through the uterine serosa
Terminology
- Placenta creta
- Morbidly adherent placenta (MAP)
ICD coding
Epidemiology
- 1/731 births (Obstet Gynecol 2015;125:683)
- 75% accreta
- 18% increta
- 7% percreta
Sites
- In order of frequency: uterus, lower uterine segment and cervix
- Placenta percreta may extend to bladder, ureters and bowel
Pathophysiology
- Poorly understood (Dis Markers 2018;2018:1507674)
- Paucity or absence of decidualized endometrium in nearly all cases
- Impaired extravillous trophoblast function may be an important factor (Pediatr Dev Pathol 2016;19:320)
Etiology
- Previous cesarean sections (a greater number of cesarean sections means a greater risk for accreta) (Pediatr Dev Pathol 2017;20:387)
- Placenta previa
- Prior uterine instrumentation
- Submucosal leiomyoma
- Asherman syndrome (scar tissue within uterine cavity)
Clinical features
- Severe peripartum hemorrhage can occur if the placenta cannot be separated from the uterus at delivery (J Matern Fetal Neonatal Med 2016;29:1795)
- Massive peripartum hemorrhage may lead to disseminated intravascular coagulation (DIC) and shock
- Placenta percreta may damage adjacent organs, including bladder, ureters and bowel
Diagnosis
- Often suspected on prenatal imaging studies and operative findings
- Diagnosis is made upon examination of the hysterectomy specimen
- Histologic confirmation is required
- On rare occasions, diagnosis of placenta accreta can be made on the delivered placenta
Radiology description
- Ultrasound: loss of normal hypoechoic retroplacental zone, increased subplacental vascularity, abnormal interface between uterus and bladder, retroplacental myometrial thickness < 1 mm, multiple vascular lacunae within the placenta (J Matern Fetal Neonatal Med 2016;29:1795)
- MRI may be helpful, particularly < 30 weeks gestation
- Prenatal imaging is more sensitive at detecting severe cases of accreta and tends to not identify mild forms
Radiology images
Prognostic factors
- Delayed placental separation or manual removal increases the risk for accreta in future pregnancies
- Presence of extensive myometrial fibers adherent to the basal plate in a delivered placenta has been shown to increase the risk of placenta accreta in subsequent pregnancies (BJOG 2016;123:2140)
Case reports
- 26 year old woman with pernicious placenta previa / placenta percreta (J Int Med Res 2019;47:6365)
- 38 year old woman with placenta increta (N Engl J Med 2016;375:1382)
- 38 year old woman with placenta accreta in the second trimester (Cureus 2018;10:e2904)
- 38 year old woman with placenta accreta and massive life threatening bleeding (Medicine (Baltimore) 2019;98:e15025)
- 40 year old woman with placenta accreta following hysteroscopy for Asherman syndrome (Case Rep Obstet Gynecol 2018;2018:6968382)
Treatment
- Massive peripartum hemorrhage needs immediate treatment with blood transfusions and management of disseminated intravascular coagulation and shock
- Emergent hysterectomy is required if bleeding cannot be controlled
- Elective hysterectomy may be planned if imaging studies are concerning for severe forms of abnormal placental implantation
- Conservative options include uterine artery ligation, balloon tamponade, uterotonics and hysteroscopic resection for mild forms (Am J Obstet Gynecol 2015;213:755)
Clinical images
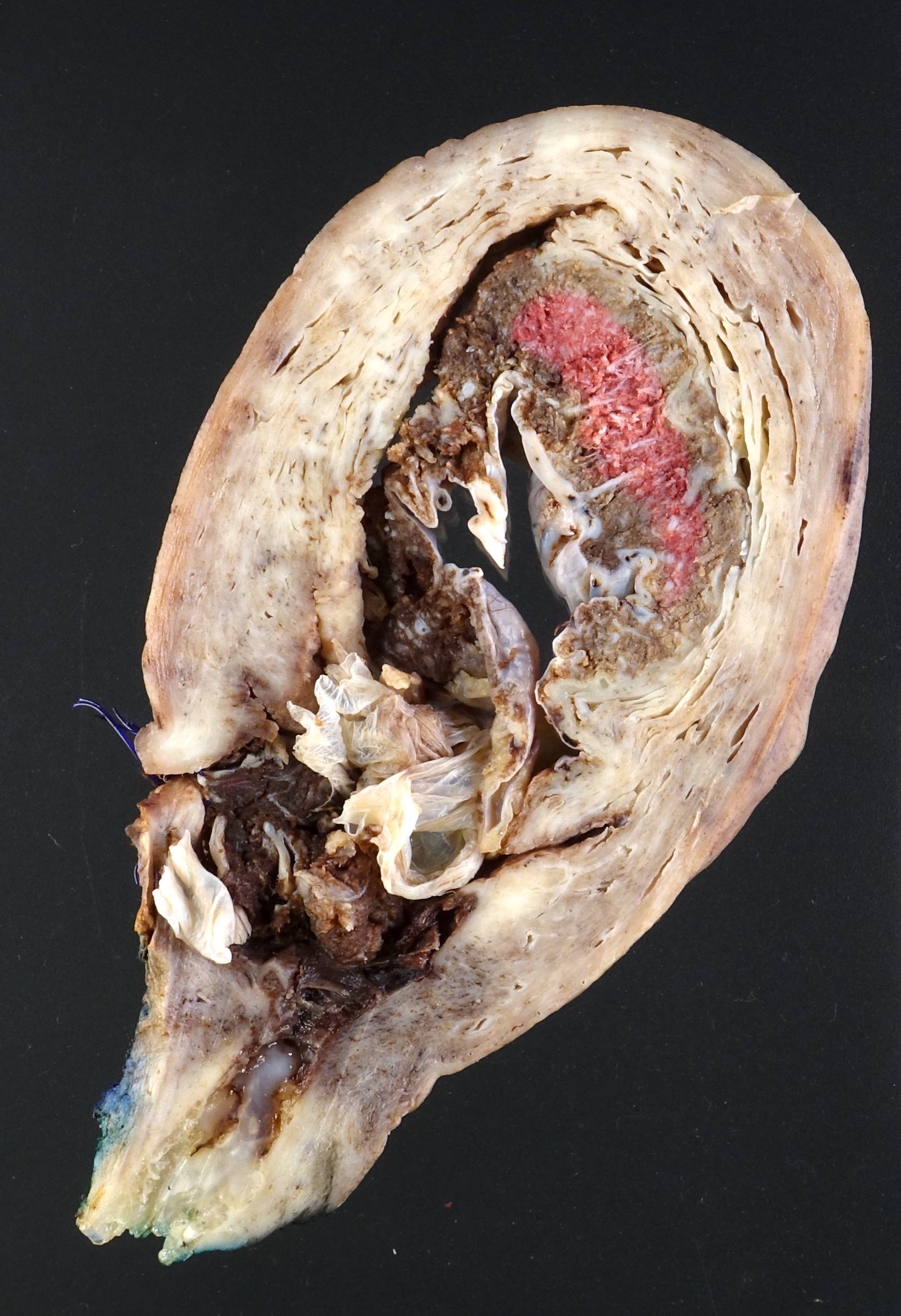
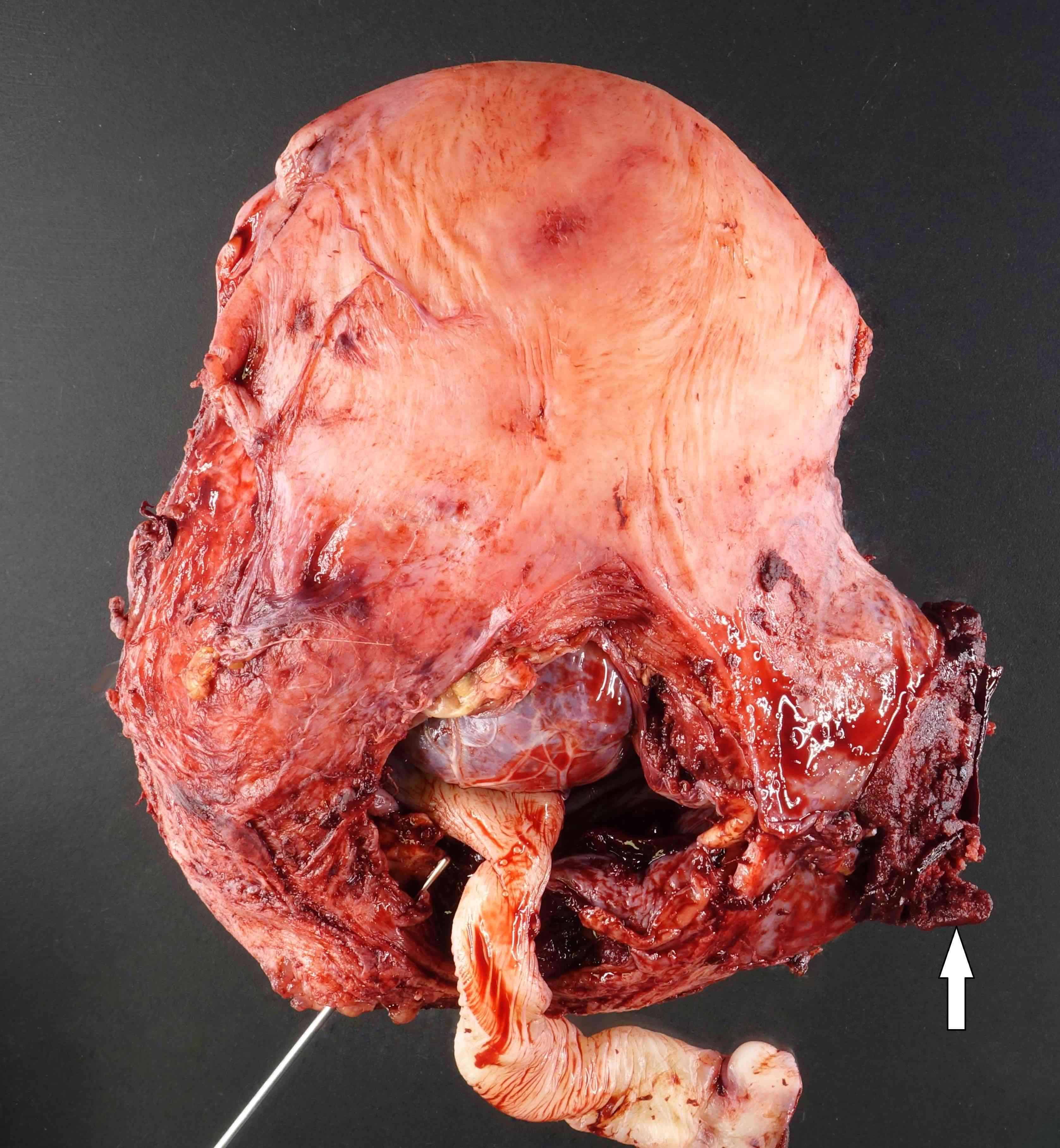
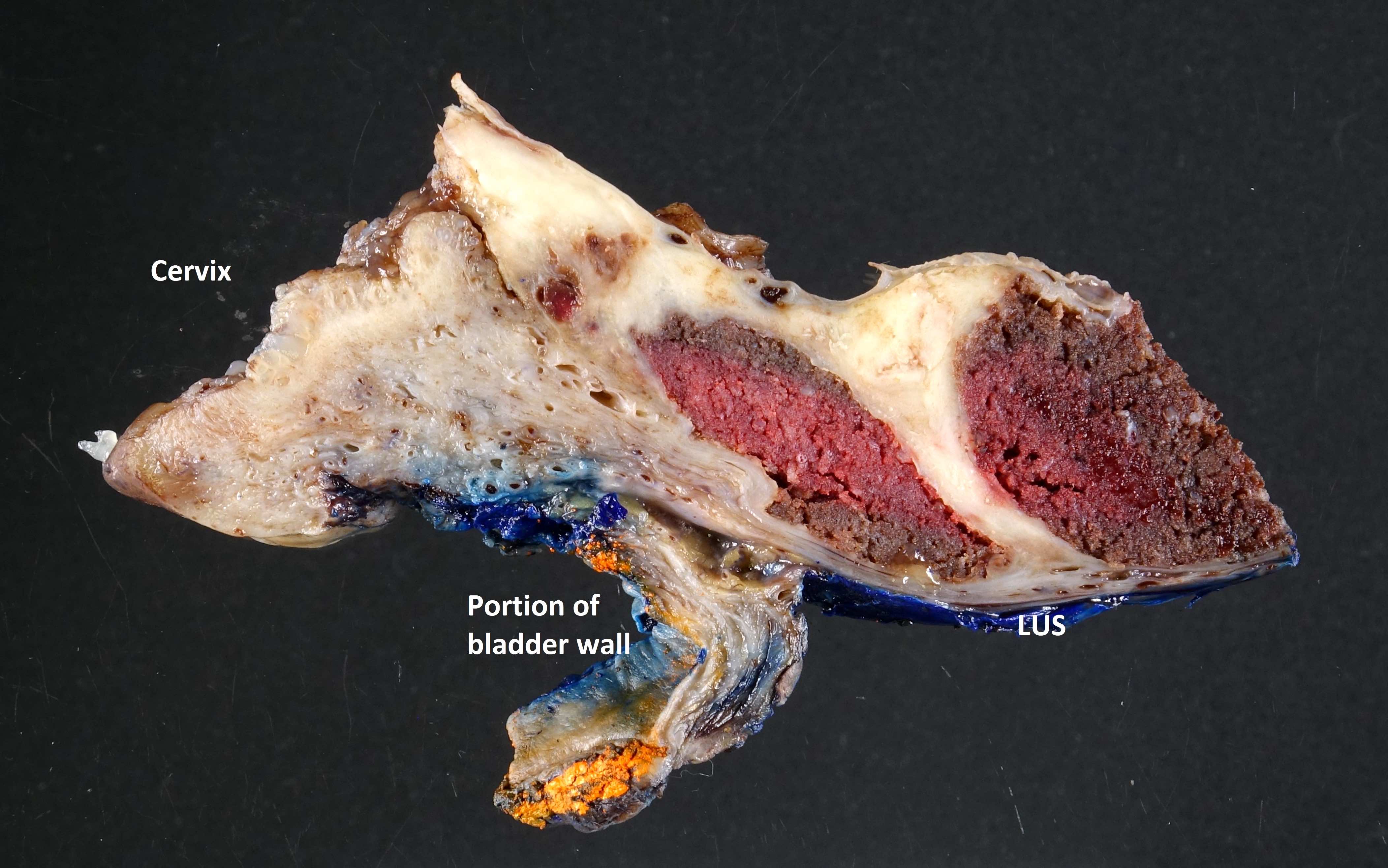
Gross description
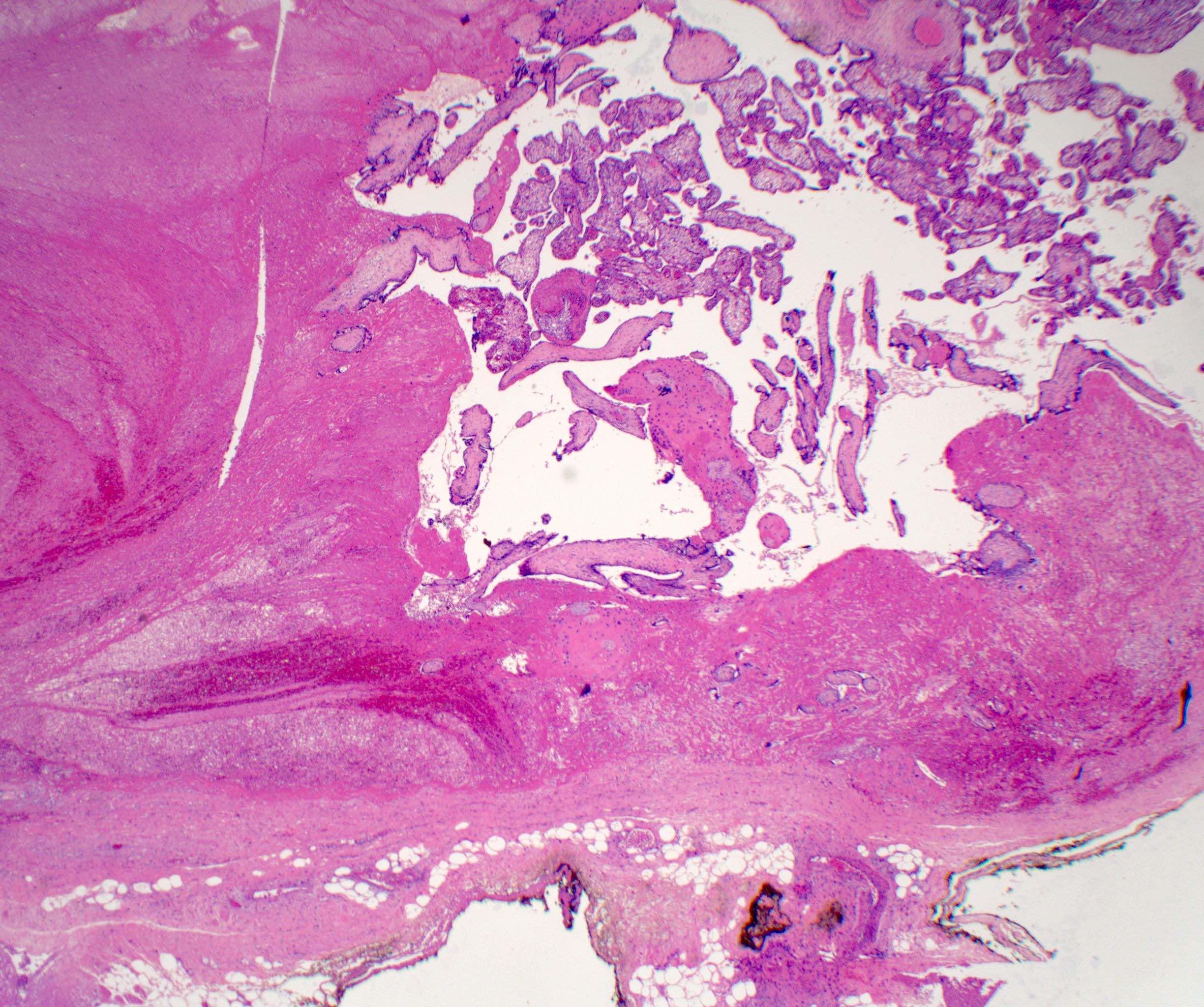
- Hysterectomy specimen:
- With placenta in situ:
- Placenta accreta: placenta adherent to the uterine wall; myometrium not thinned
- Placenta increta: placenta extends into the uterine wall, usually in a blunt manner; myometrium thinned
- Placenta percreta: placenta penetrates through the uterine or lower uterine segment wall; protruding placental tissue on external surface (should be inked) and adherent structures (bladder, bowel)
- Note where the placenta is implanted (lower uterine segment implantation / placenta previa is common)
- With separate placenta:
- Placental implantation site may or may not be visible
- Increased vascularity with ectatic vessels on superficial myometrium provide a clue for the placental implantation site
- If visible, this area should be sampled
- If not visible, check medical records for site of placental implantation and sample the area indicated
- Refer to published guidelines on how to perform gross examination and sampling (Arch Gynecol Obstet 2016;293:951)
- With placenta in situ:
- Delivered placenta:
- Disruption of basal plate
- Missing cotyledons in some cases
- Higher yield of identifying adherent myometrial fibers microscopically by sampling the intact basal plate adjacent to disrupted areas
Gross images
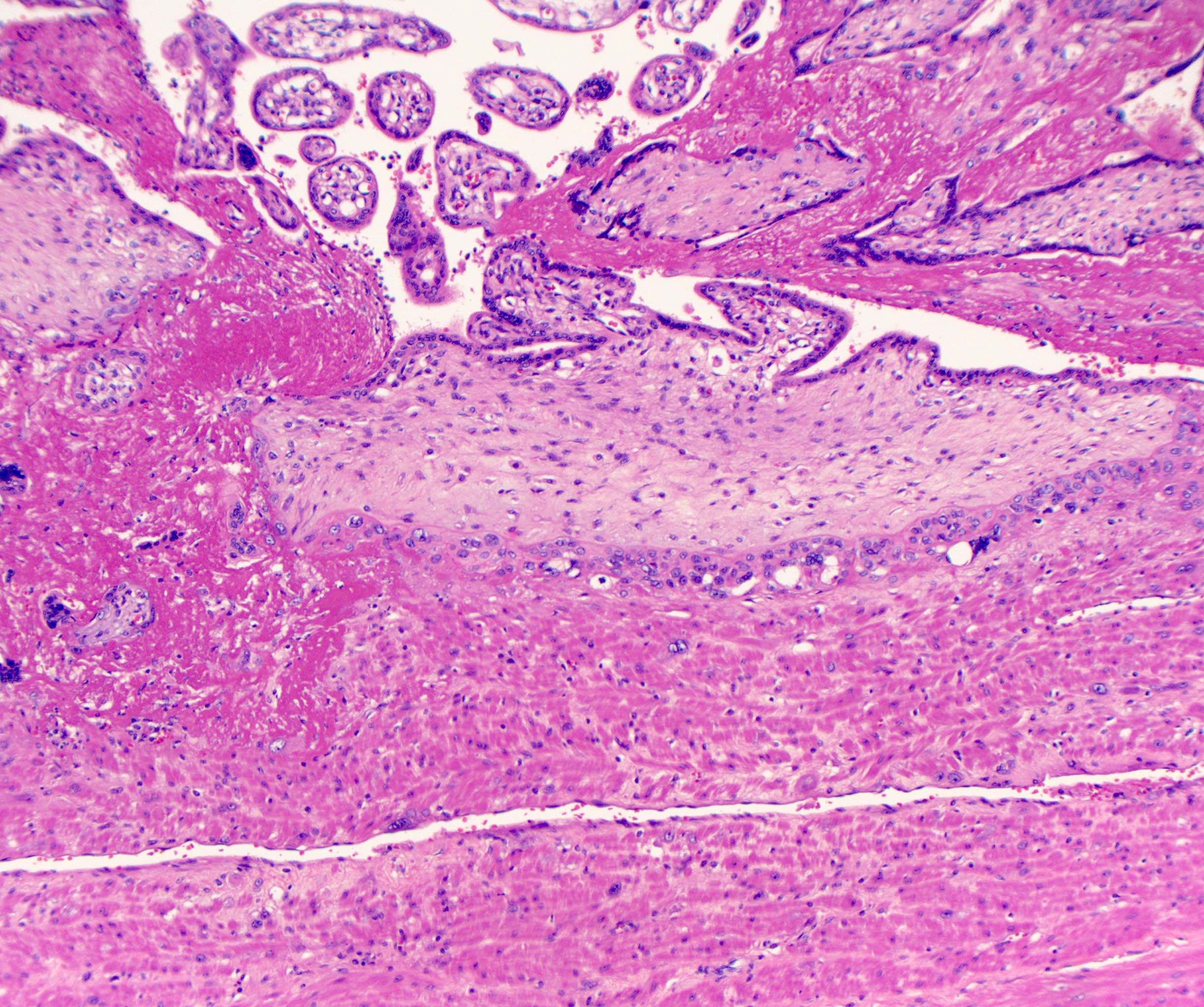
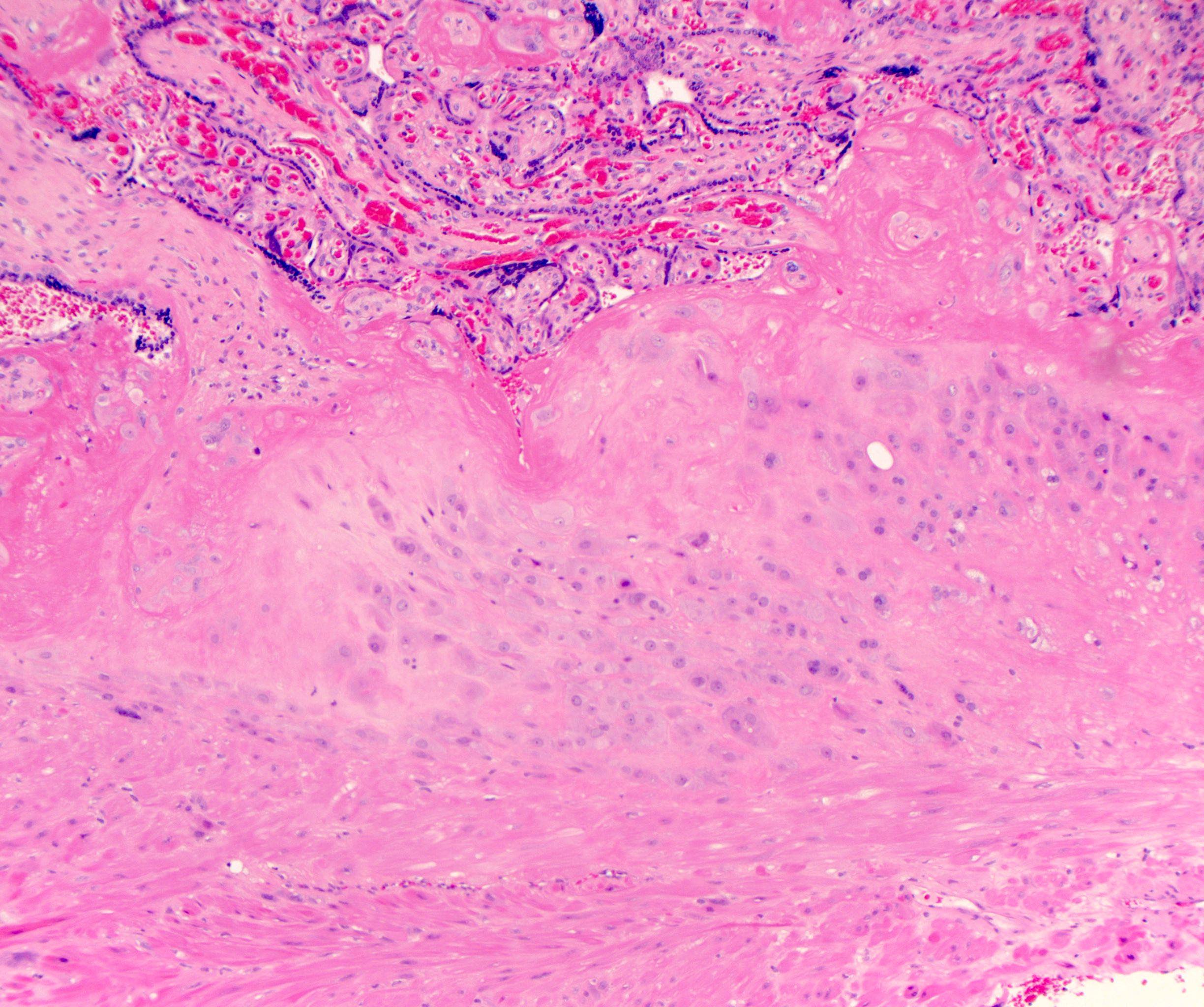
Microscopic (histologic) description
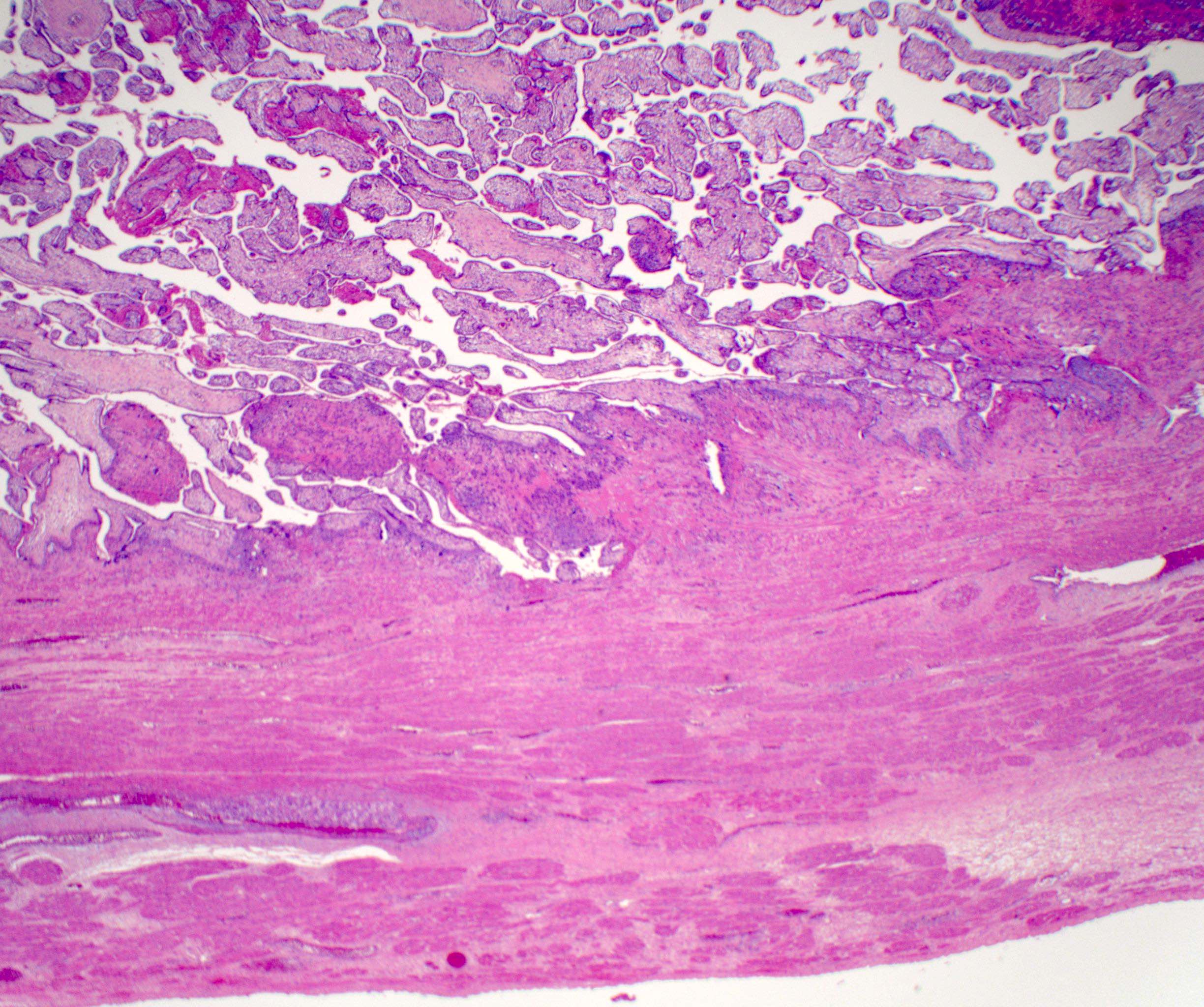
- Diagnosis traditionally made on hysterectomy specimen
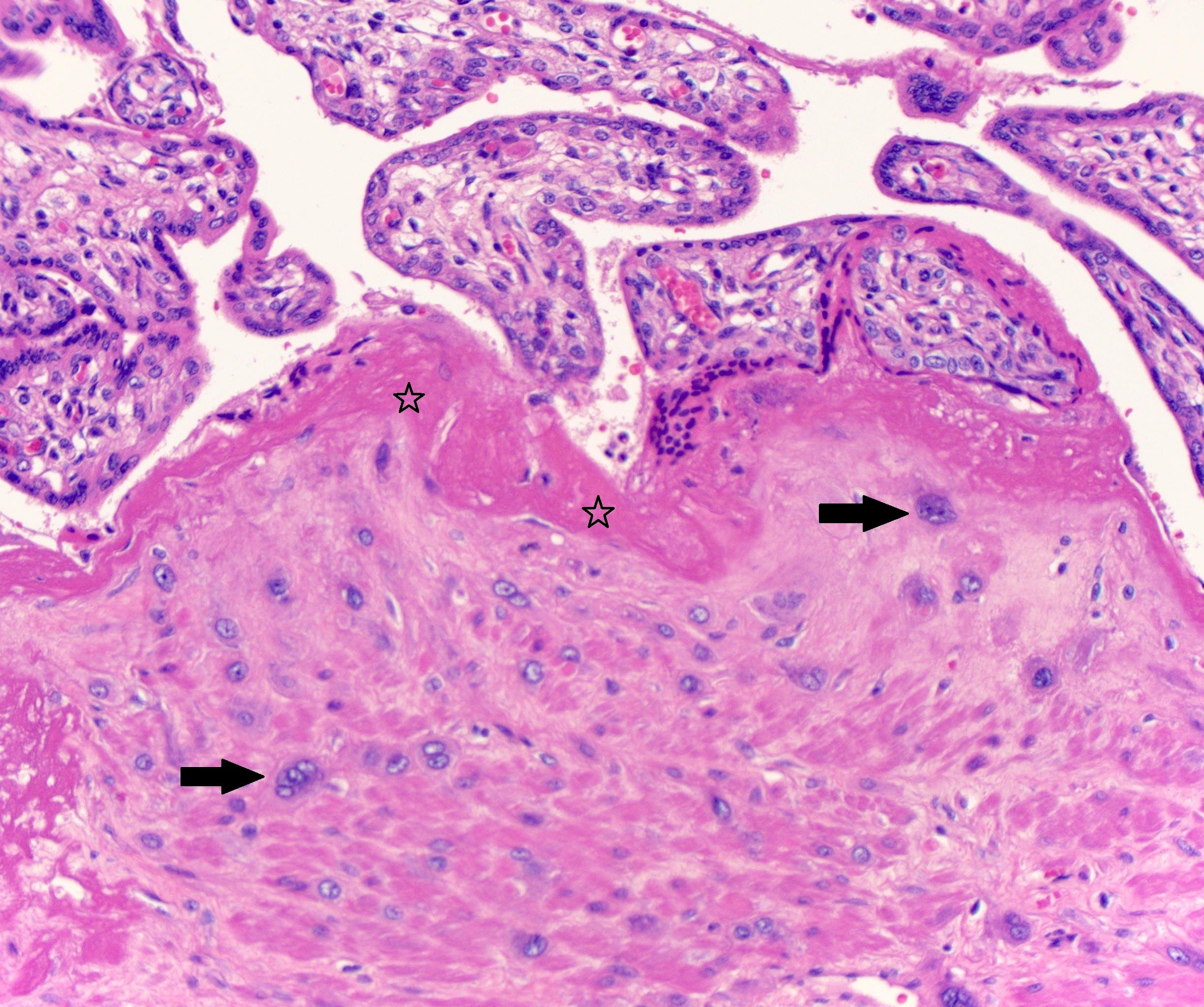
- Placenta accreta:
- Chorionic villi implant directly on the surface of the myometrium without intervening decidua
- Fibrin and extravillous trophoblast (EVT) are often present between the villi and myometrial fibers, in which case a diagnosis of accreta should still be made, given that intervening decidua is not present
- Differentiating decidual cells and extravillous trophoblastic cells may be difficult
- Myometrium is not thinned
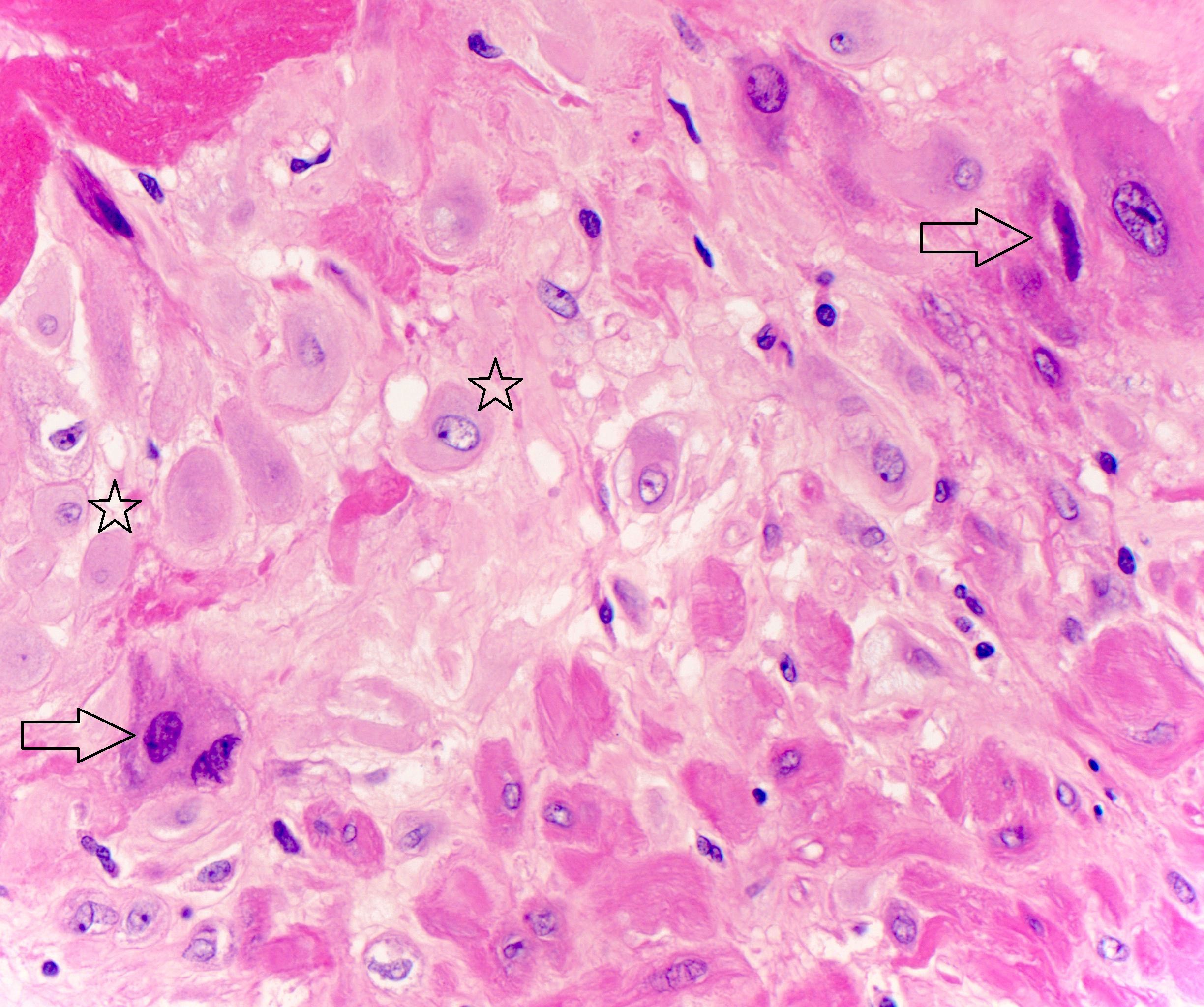
- Placenta increta:
- Chorionic villi identified within the myometrium
- Fibrin and extravillous trophoblast can be present between the villi and myometrial fibers
- Myometrium is thinned
- Presence of extravillous trophoblast within the myometrium is not a diagnostic feature of placenta increta
- Placenta percreta:
- No residual myometrium
- Ink present on villous tissue obtained from area suspicious for placenta percreta grossly
- It is critical that invasion through the myometrial wall is identified in this area to exclude the possibility that the protruding placental tissue was displaced during surgery through the cesarean section incision
- Villous tissue adjacent to adipocytes or in extrauterine structures, such as bladder, is seen in some cases and is diagnostic of percreta
- Placenta accreta:
- Diagnosis uncommonly made on delivered placenta (occult placenta accreta)
- Myometrial fibers attached to the basal plate with complete lack of intervening decidua between the myometrial fibers and the basal chorionic villi, with or without intervening fibrin / extravillous trophoblast (BJOG 2016;123:2140)
- A staging system has been proposed but is not currently used in most practices (Placenta 2015;36:1419)
Microscopic (histologic) images
Positive stains
Videos
Introduction to placenta accreta
Sample pathology report
- Uterus and placenta, postcesarean supracervical hysterectomy:
- Placenta accreta
- Placental parenchyma, fetal membranes and trivascular cord with no significant histopathologic abnormalities
- Myometrium and uterine serosa with no significant abnormalities
- Endocervix with no significant abnormalities, no ectocervix identified
- Uterus, cervix and placenta, postpartum total hysterectomy:
- Placenta previa and percreta
- Placenta adherent to serosa of urinary bladder but no involvement of bladder mucosa / muscular wall
- Very preterm placenta (30 4/7 weeks), fetal membranes and trivascular umbilical cord
Differential diagnosis
- Placenta protruding through the cesarean section defect versus placenta percreta:
- Careful gross examination reveals that the protruding placental tissue is at the site of the cesarean section
- Look for sutures at the site
- Not true percreta
- Correlate with operative note
- Normally thinned myometrium at lower uterine segment versus placenta increta:
- Compare the thickness of the lower uterine segment at the side suspicious for increta with the thickness of the lower uterine segment on the opposite side
- If the myometrium of both sides has a similar thickness throughout, it is not increta
- Physiologic invasion of extravillous trophoblast into the myometrium versus placenta accreta:
- Extravillous trophoblast normally infiltrates the inner third of the myometrium and this is not accreta
- In accreta, only extravillous trophoblast without decidual cells are present between villi and myometrium
- Extravillous trophoblast versus decidual cells:
- Both are large polygonal cells with abundant eosinophilic cytoplasm
- Decidual cells have uniformly bland nuclei with smooth nuclear membranes, homogenous open chromatin and small nucleoli
- Extravillous trophoblast cells have atypical nuclei with irregular nuclear membranes, variation in nuclear shape and size and often hyperchromatic or irregular chromatin
Practice question #1
A 38 year old woman G3 P2 underwent a peripartum hysterectomy for life threatening uncontrollable vaginal bleeding. On gross examination, the placenta was in situ and the thickness of the myometrium was markedly decreased at the placental implantation site. The uterine serosa and lower uterine segment were grossly unremarkable. Microscopic examination revealed villi juxtaposed to myometrial fibers. What is the most appropriate diagnosis?
- Placenta accreta
- Placenta increta
- Placenta percreta
- Subinvolution of the placental site
- Uterine atony
Practice answer #1
Practice question #2
Which of the following is required for a diagnosis of placenta accreta?
- Absence of intervening decidua between villi and myometrium
- Invasive extravillous trophoblast into the myometrium
- Myometrial fibers adherent to the basal plate
- Placenta grossly adherent to the uterine wall
- Villous invasion through the myometrium and serosa
Practice answer #2
A. Absence of intervening decidua between villi and myometrium
Comment Here
Reference: Placenta accreta, increta and percreta
Comment Here
Reference: Placenta accreta, increta and percreta