Table of Contents
Definition / general | Sites | Clinical features | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosisCite this page: Handra-Luca A. Adenocarcinoma, NOS. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/salivaryglandsadenocarcinomaNOS.html. Accessed May 4th, 2024.
Definition / general
- Invasive tumor, often aggressive, with glandular or ductal differentiation but no features characteristic of other specific types (Arch Pathol Lab Med 2004;128:1385)
- Common, 5 - 10% of salivary gland tumors
- 6 - 10% of salivary gland malignancies, 17% of parotid gland malignancies, 15% of minor salivary gland malignancies
Sites
- Parotid gland, submandibular gland, palate, buccal mucosa
Clinical features
- Mean age 58 years (median 67 years), range 10 - 93 years
- Usually asymptomatic
- Often fixed to skin or deep tissues
- Palatal lesions often ulcerated and involve bone
- Gender predominance debated, recent reports show male predominance
- Cervical lymph node metastases in 23%, distant metastases in 37%
- Diagnosis of exclusion (not metastatic, not another salivary gland carcinoma)
- 5 year disease specific survivals is 57%
Case reports
- 49 year old man with parotid mass (Arch Pathol Lab Med 2004;128:487)
Treatment
- Complete surgical excision
Gross description
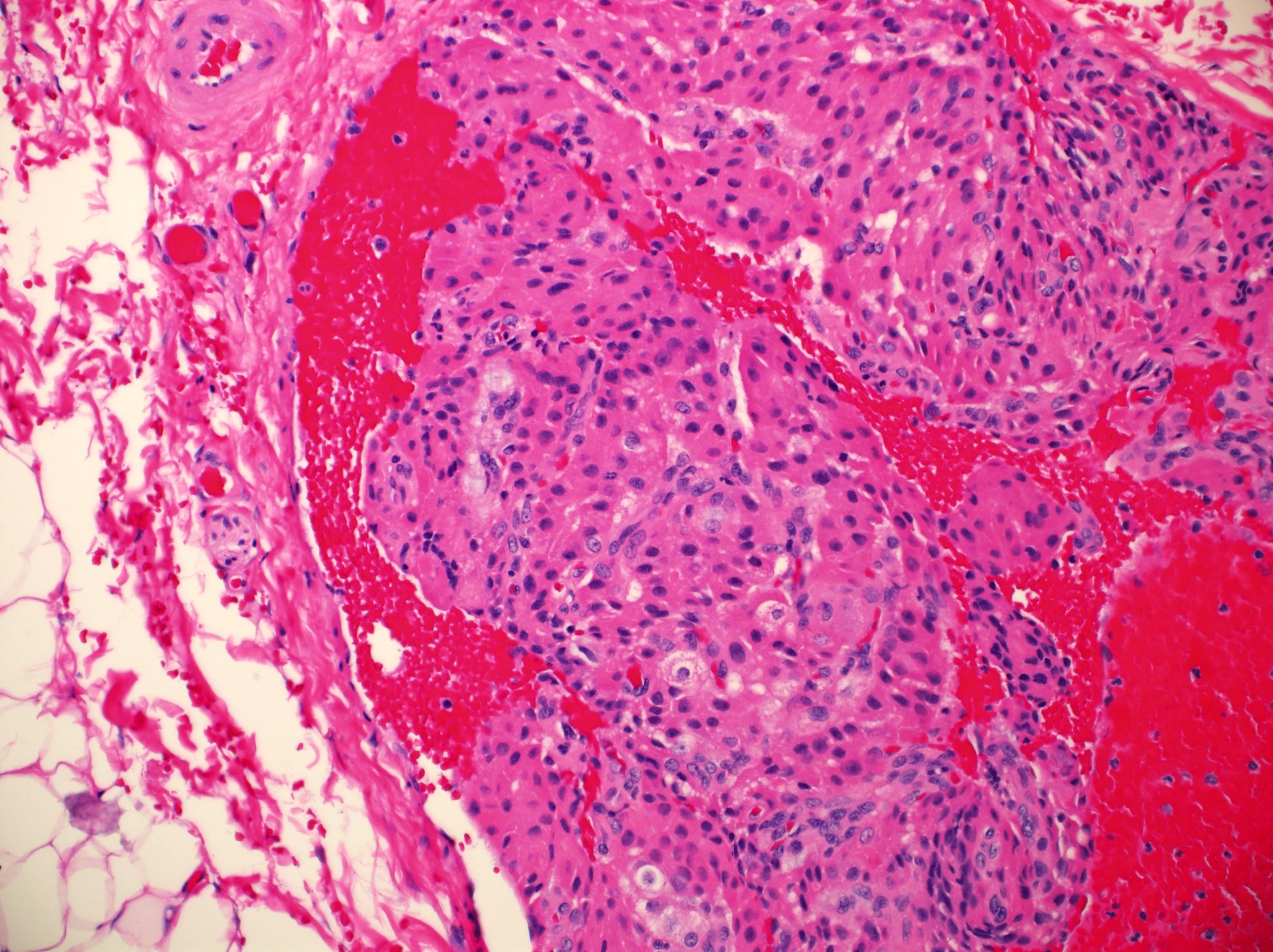
- Poorly circumscribed with infiltrative borders
- Solid tan cut surface with hemorrhage and necrosis
Microscopic (histologic) description
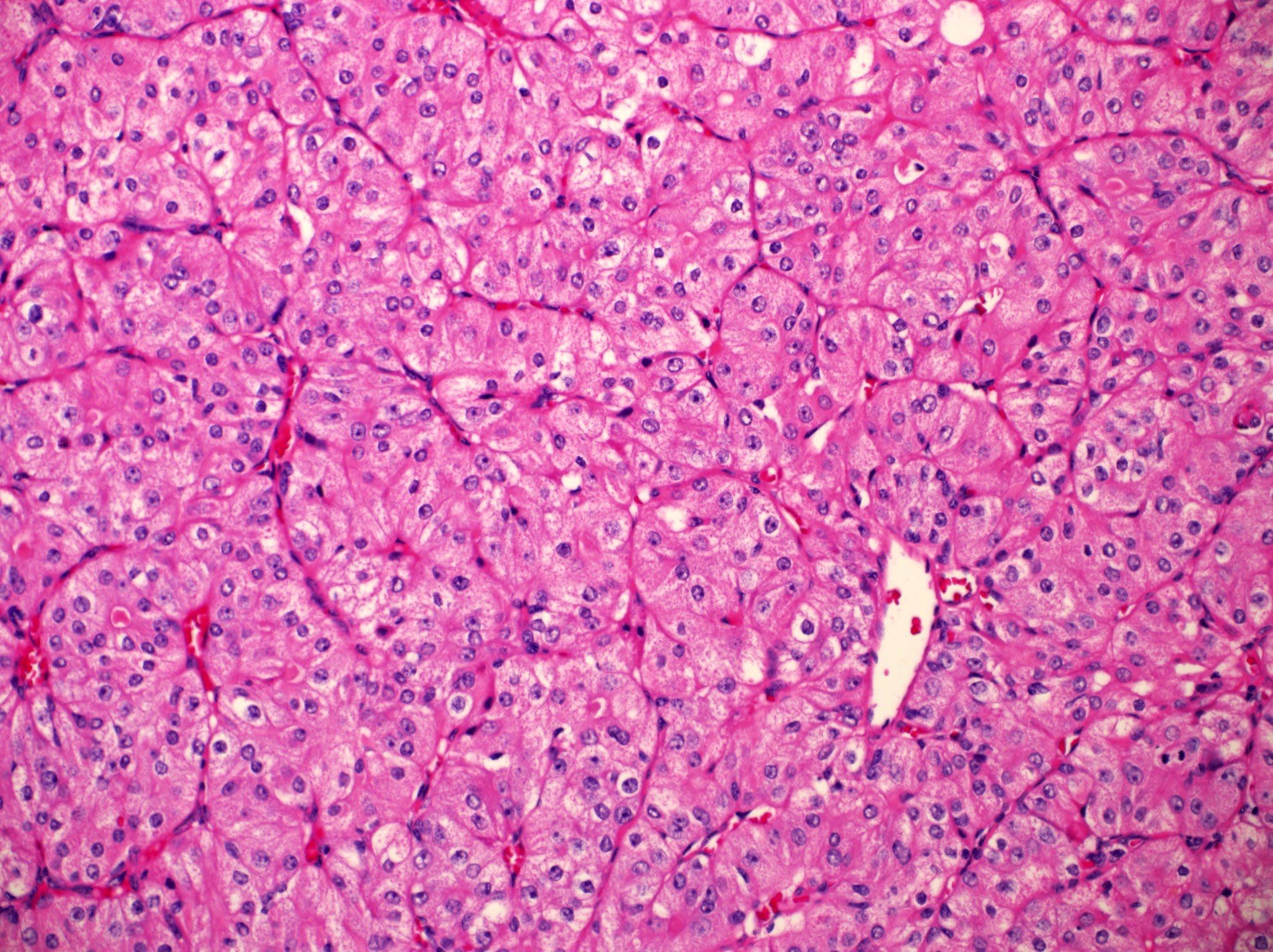
- Invasive with glandular or ductal differentiation but no features characteristic of other specific types
- Patterns include glandular spaces with cyst formation, papillary formation, solid sheets, comedonecrosis, hyalinized "shadow" nodules
- Small clusters of cuboidal, round or ovoid cells with distinct borders and abundant cytoplasm
- May have clear cell or oncocytic features
- Low, intermediate or high grade based on cytomorphic features
- In situ component in 68% (Virchows Arch 2006;449:159)
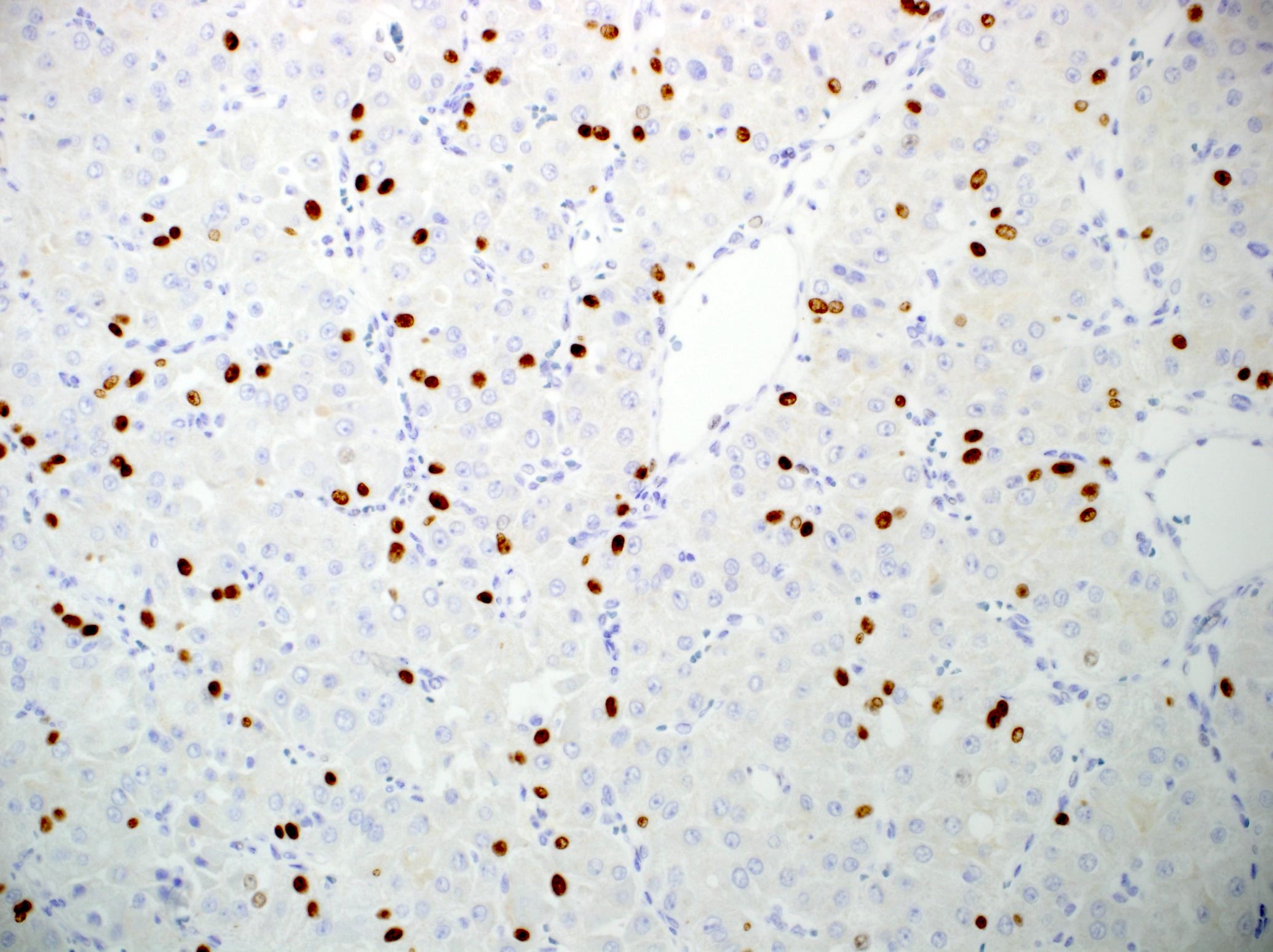
Positive stains
- CK7+ / CK20- (Mod Pathol 2004;17:407), positive for EGFR, survivin, phospho-STAT3, CK18, HER2
- Uniform periductal staining of reactive myofibroblastic cells with calponin, smooth muscle actin, smooth muscle myosin heavy chain (Arch Pathol Lab Med 1999;123:801)
Negative stains
Molecular / cytogenetics description
- EGFR gene amplification, increased EGFR gene copy number
- HER2 amplification, high HER2 gene copy number
- KRAS mutation rarely (Arch Pathol Lab Med 2000;124:836)
Differential diagnosis
- Hybrid carcinoma
- Membranous adenoma
- Metastatic adenocarcinoma
- Polymorphous low grade adenocarcinoma
- Undifferentiated carcinoma