Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Immunofluorescence description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Siatecka H, Gottesman SP. Graft versus host disease. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorGVHD.html. Accessed April 26th, 2024.
Definition / general
- Graft versus host disease (GVHD) is a multisystem immunologic disorder following an allogenic hematopoietic cell transplant and rarely after solid organ transplant or transfusion
- It can be acute or chronic and can affect many organ systems, including the skin, gastrointestinal tract, liver and lungs
Essential features
- GVHD refers to multiorgan syndromes of tissue inflammation or fibrosis that primarily affect skin
- Donor (graft) T cells attack and destroy recipient (host) cells
- 2 types: acute or chronic
- Histologically, acute GVHD presents with vacuolar interface dermatitis with necrotic keratinocytes surrounded by lymphocytes and chronic GVHD shows either lichenoid or sclerodermoid changes
Terminology
- GVHD: graft versus host disease
- aGVHD: acute graft versus host disease
- cGVHD: chronic graft versus host disease
ICD coding
Epidemiology
- GVHD affects patients who are exposed to blood products, bone marrow and solid organs containing T cells that recognize the host as foreign and proceed to attack the host tissue and organs
- Cutaneous GVHD occurs in ~30 - 60% of allogenic hematopoietic stem cell transplant recipients (An Bras Dermatol 2016;91:336, Malays J Pathol 2021;43:361)
- Incidence of chronic GVHD after allogeneic hematopoietic cell transplant is ~40% with reported incidence rates between 6 - 80% (Biol Blood Marrow Transplant 2005;11:945, Bone Marrow Transplant 1998;22:755, Blood 1990;75:2459, Bone Marrow Transplant 1994;13:455)
- Exact incidence of acute GVHD after allogenic hematopoietic stem cell transplant is unknown with reported incidence rates from 9% to 50% in patients who receive transplant from genotypically HLA identical sibling (Biol Blood Marrow Transplant 2005;11:945, Blood 2012;119:296, Bone Marrow Transplant 2013;48:587)
- Increased risk for chronic and acute GVHD is associated with HLA mismatch, older donor age, sex disparity between donor and recipient, history of pregnancy or blood transfusion in the donor, prior donor lymphocyte infusion, CMV and EBV seropositivity, prior acute GVHD (risk factor for chronic GVHD) (Blood 2011;117:3214)
Sites
- Acute GVHD usually affects skin: ears, palms, soles, lateral neck, cheeks and upper back
- Acute extracutaneous GVHD involves liver, gastrointestinal tract, lungs and lymphoid tissue (Australas J Dermatol 2010;51:1)
- Chronic GVHD affects primarily the skin; however, nearly all organ systems can be involved (mucous membranes, liver, lung, eye, joints and fascia, gastrointestinal tract, genitalia) (Blood 2012;120:2545)
Pathophysiology
- GVHD can develop in different clinical scenarios when tissues containing T cells (blood products, bone marrow and solid organs) are transferred from one person to another and the T cells are not able to be removed (Lancet 2009;373:1550)
- Immune cells transferred from a nonidentical donor (graft) into the recipient (host) recognize the host cells as foreign and initiate a graft versus host reaction (N Engl J Med 2017;377:2167)
- There are 3 pathophysiologic phases of acute GVHD (Semin Hematol 2006;43:3, Dermatol Clin 2019;37:569)
- Host tissue damage from the radiation and chemotherapy that precede the transplant
- Activation and multiplication of donor T cells as a result of interaction with antigens from the host
- These activated T cells lead to tissue damage once target organs are reached
- There are also 3 pathophysiologic phases of chronic GVHD (N Engl J Med 2017;377:2565)
- Activation of innate immune cells, endothelial cells and fibroblasts resulting from tissue cytotoxic injury, infections and acute GVHD
- Increased response of the adaptive immune system and decrease in immune cell regulators (upregulation of Th1, Th2 and Th17 cells and downregulation of T regulatory cells)
- Activation of macrophages resulting in production of transforming factor b and platelet derived growth factor, which activate fibroblasts leading to abnormal tissue repair
Etiology
- Allogeneic hematopoietic cell transplant, solid organ transplant or transfusion of blood products
Clinical features
- Previously GVHD was classified as acute and chronic based on a 100 day cutoff
- Current NIH consensus criteria use clinical findings to differentiate between acute and chronic GVHD (Biol Blood Marrow Transplant 2015;21:389)
- Acute GVHD (Australas J Dermatol 2010;51:1)
- Affects skin, gastrointestinal tract, liver and hematopoietic system
- Skin involvement is often the earliest and presents as macular and papular eruption, which may resemble a sunburn; may be pruritic or painful and can become confluent
- Smooth or hyperkeratotic papules and postinflammatory hyperpigmentation may occur
- In severe GVHD, rash can form bullous lesions with epidermal necrosis mimicking SJS / TEN
- Staging of skin involvement is based on severity
- Stage 1: maculopapular rash involving < 25% of body area
- Stage 2: rash involving 25 - 50% of body area
- Stage 3: generalized erythroderma
- Stage 4: generalized erythroderma with bullous formation
- Chronic GVHD (Biol Blood Marrow Transplant 2003;9:215, Australas J Dermatol 2010;51:1)
- Skin is the most common site of involvement; all organs can be affected
- Either isolated to one organ / site or widespread disease
- Can occur with or without history of acute GVHD
- Major cause of morbidity and mortality after transplant
- Onset is usually > 3 months after transplantation
- 3 diagnostic clinical features: lichen planus-like lesions, sclerotic skin lesions and poikilodermatous changes (Biol Blood Marrow Transplant 2005;11:945)
- Lichen planus-like lesions: erythematous, violaceous papules or plaques, usually on dorsal hands and feet, forearms and trunk; can occur in a follicular distribution masquerading keratosis pilaris
- Sclerosis: morphea-like GVHD (involves dermis, presents as hyperpigmented, hypopigmented or skin colored plaques), lichen sclerosus-like (typically plaques on the upper back with epidermal atrophy and superficial dermal fibrosis), deep sclerosis / eosinophilic fasciitis-like (usually medial arms and thighs, subcutaneous sclerosis) (J Am Acad Dermatol 2005;53:591)
- Poikiloderma: patches with pigmentation and telangiectasia showing a mixture of atrophy, hypo and hyperpigmentation
- Hair disorders following allogenic hematopoietic stem cell transplantation: scarring alopecia (LPP / FFA) and nonscarring alopecia (alopecia areata)
- Nail disorders: dystrophy, anonychia, longitudinal ridging, splitting or brittle nails, onycholysis, pterygium
- Acute GVHD (Australas J Dermatol 2010;51:1)
Diagnosis
- Combination of clinical and pathologic findings
- Acute and chronic GVHD: skin punch biopsy
- In chronic GVHD, deep incisional biopsy can be useful in evaluating fascial involvement
- MRI can help to diagnose subcutaneous disease and fasciitis (Arch Dermatol 2009;145:918)
Prognostic factors
- Associated with lower survival for acute GVHD (Bone Marrow Transplant 2013;48:587)
- Advanced disease status
- Increasing age of patients
- Associated with higher survival for acute GVHD (Bone Marrow Transplant 2013;48:587)
- Late onset
- Involving skin only
- Associated with lower survival for chronic GVHD (Ann Hematol 2015;94:1727)
- Low platelet counts < 100,000/μl at the time of diagnosis
- Female donor
- IgG levels above normal at the time of diagnosis
- Hyperbilirubinemia and small intestinal / colonic involvement
- No impact of prior acute GVHD on outcome of patients with chronic GVHD (Ann Hematol 2015;94:1727)
Case reports
- 54 year old man underwent liver transplantation for alcohol use disorder related cirrhosis and presented with dermatitis, bone marrow failure and enteritis (Sci Prog 2022;105:368504221117070)
- 57 year old man status post-kidney transplant with sudden onset diarrhea and skin rash (Medicine (Baltimore) 2017;96:e7333)
- 62 year old man underwent allogenic bone marrow transplantation for acute myeloid leukemia and few years later developed sclerodermatous GVHD involving the trunk and limbs (J Cutan Pathol 2022;49:373)
- 72 year old man with a history of recent cadaveric liver transplantation presented with fever, generalized skin rash and hemorrhagic lesions in the oropharynx (Hepatol Forum 2022;3:30)
Treatment
- Prophylaxis: calcineurin inhibitors (cyclosporine and tacrolimus) (Bone Marrow Transplant 2017;52:357)
- Topical or systemic glucocorticoids, topical tacrolimus, ruxolitinib (Br J Haematol 2012;158:30, N Engl J Med 2020;382:1800)
- Mycophenolate mofetil, etanercept, pentostatin, alpha-1 antitrypsin, sirolimus, extracorporeal photopheresis (Bone Marrow Transplant 2009;44:739, Bone Marrow Transplant 2006;37:1143)
- Glucocorticoid resistant acute GVHD: ruxolitinib (N Engl J Med 2020;382:1800)
Clinical images
Contributed by Pooja Rambhia, M.D. and Adele Shenoy, M.D.
Images hosted on other servers:
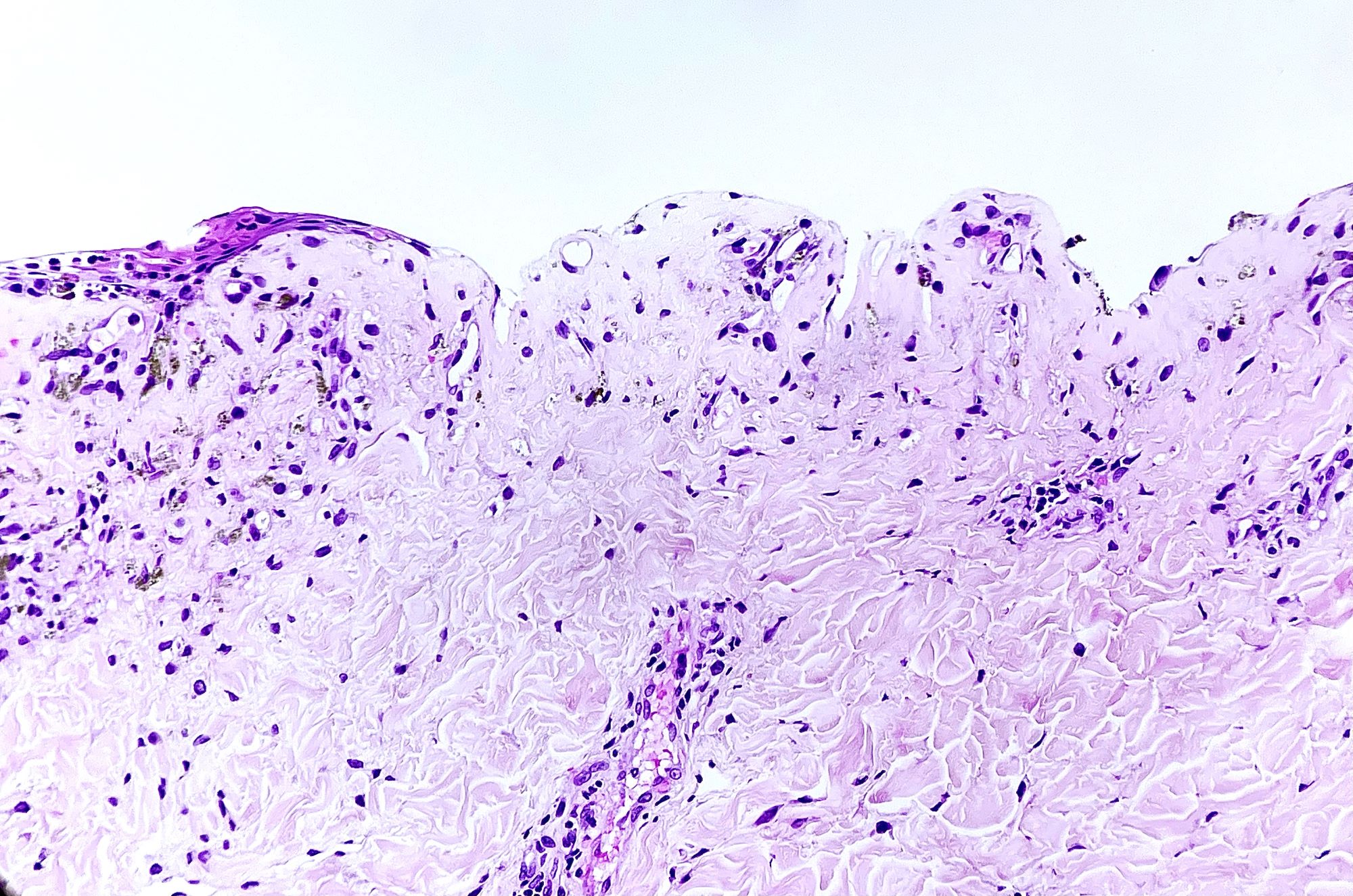
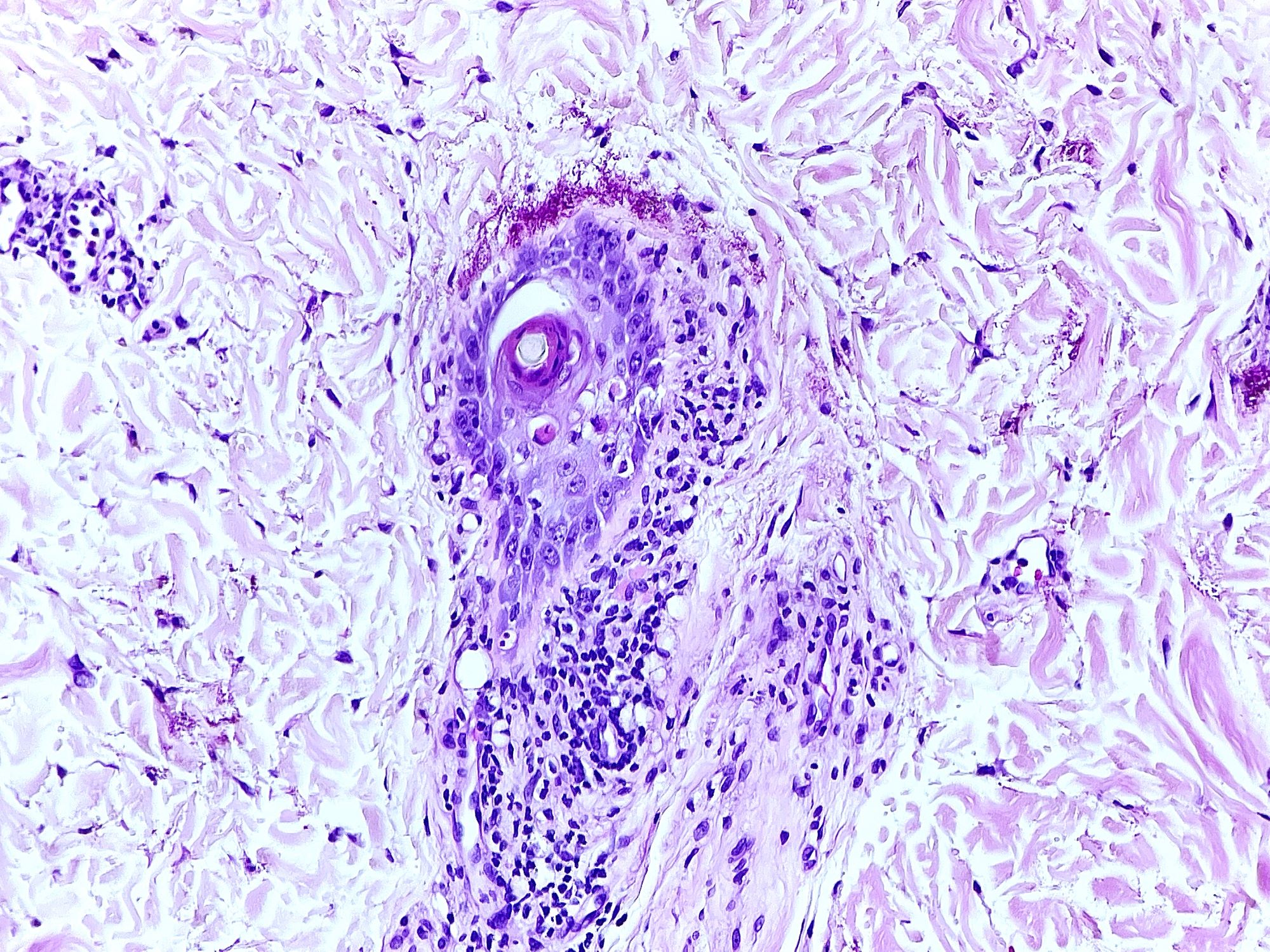
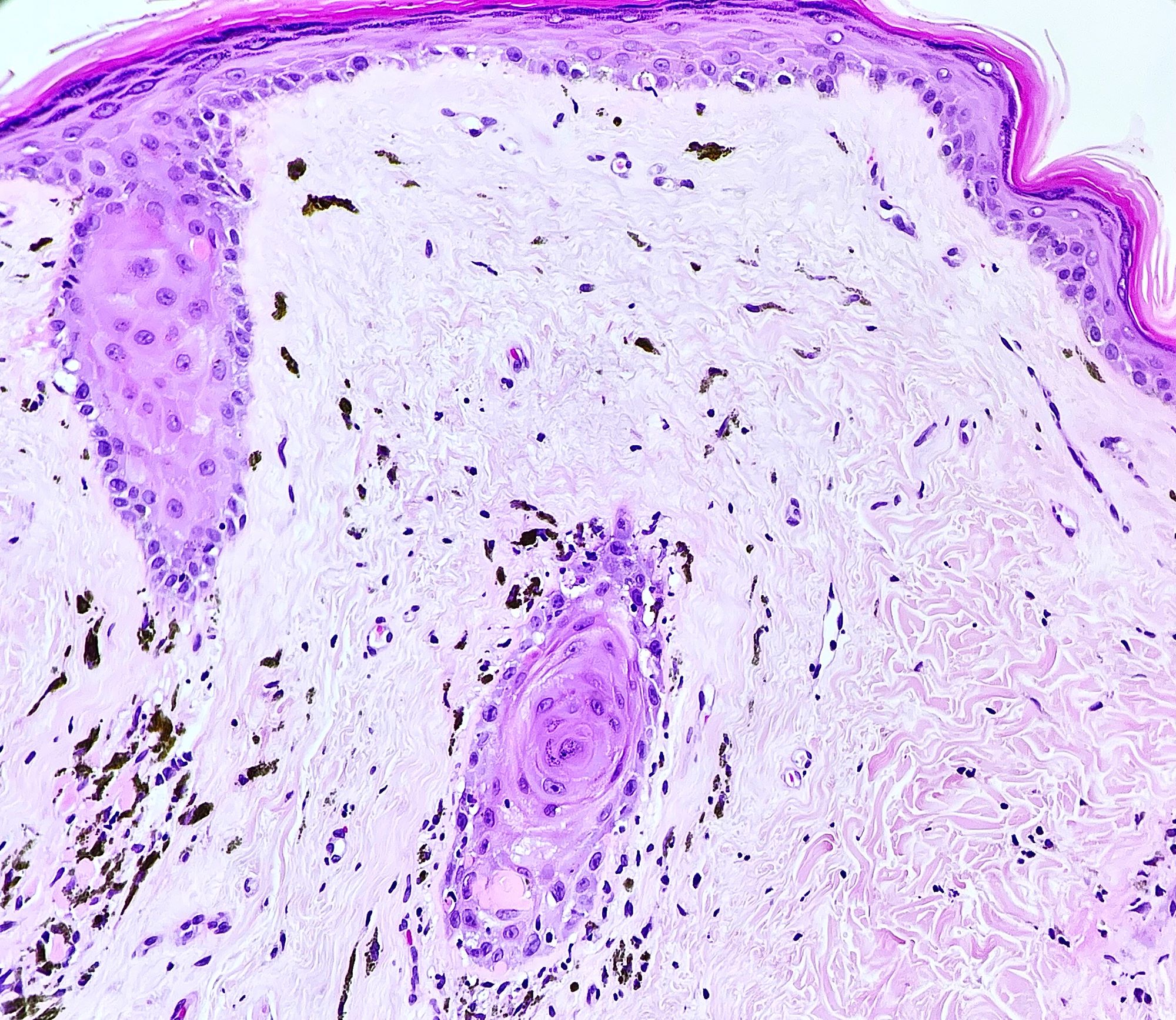
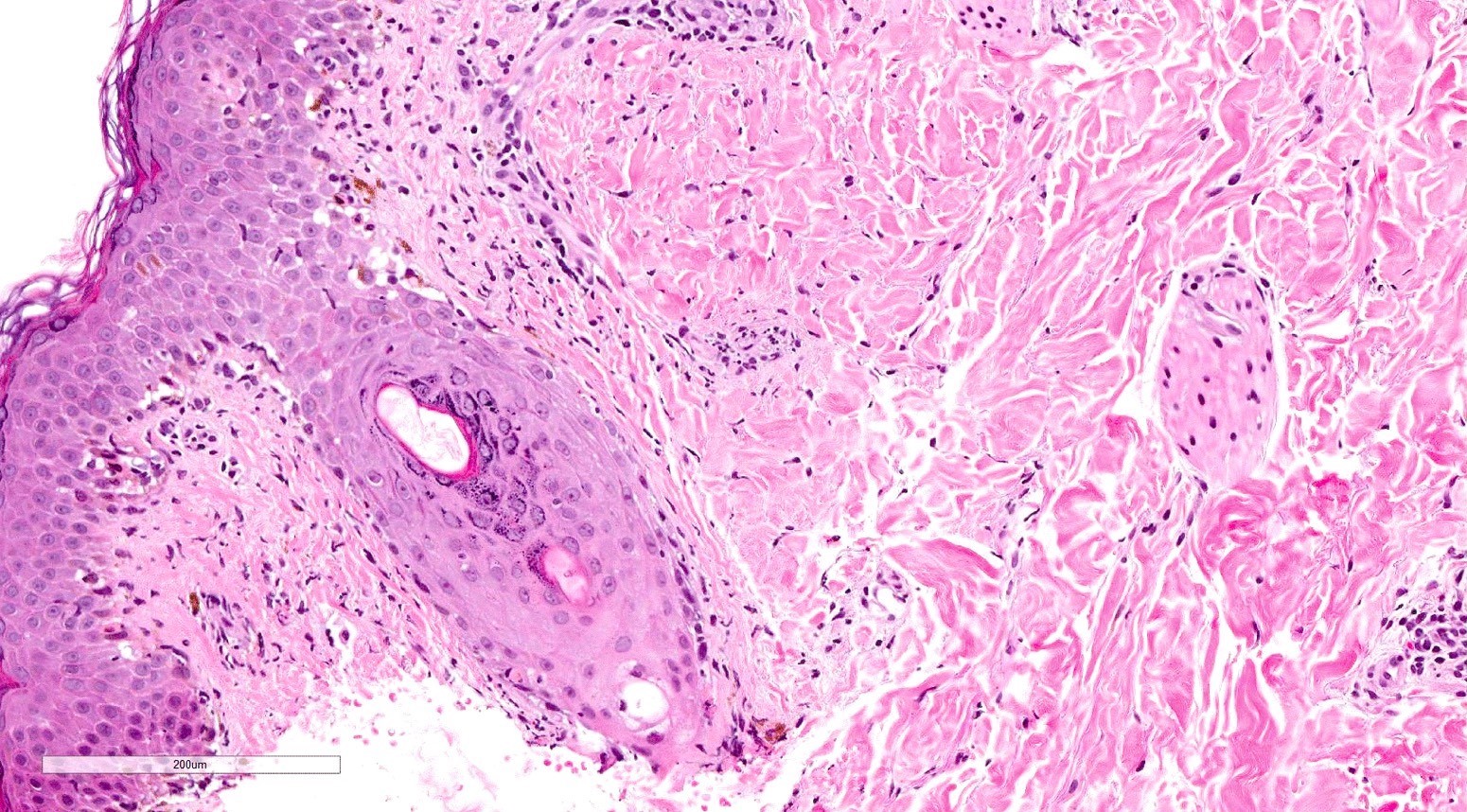
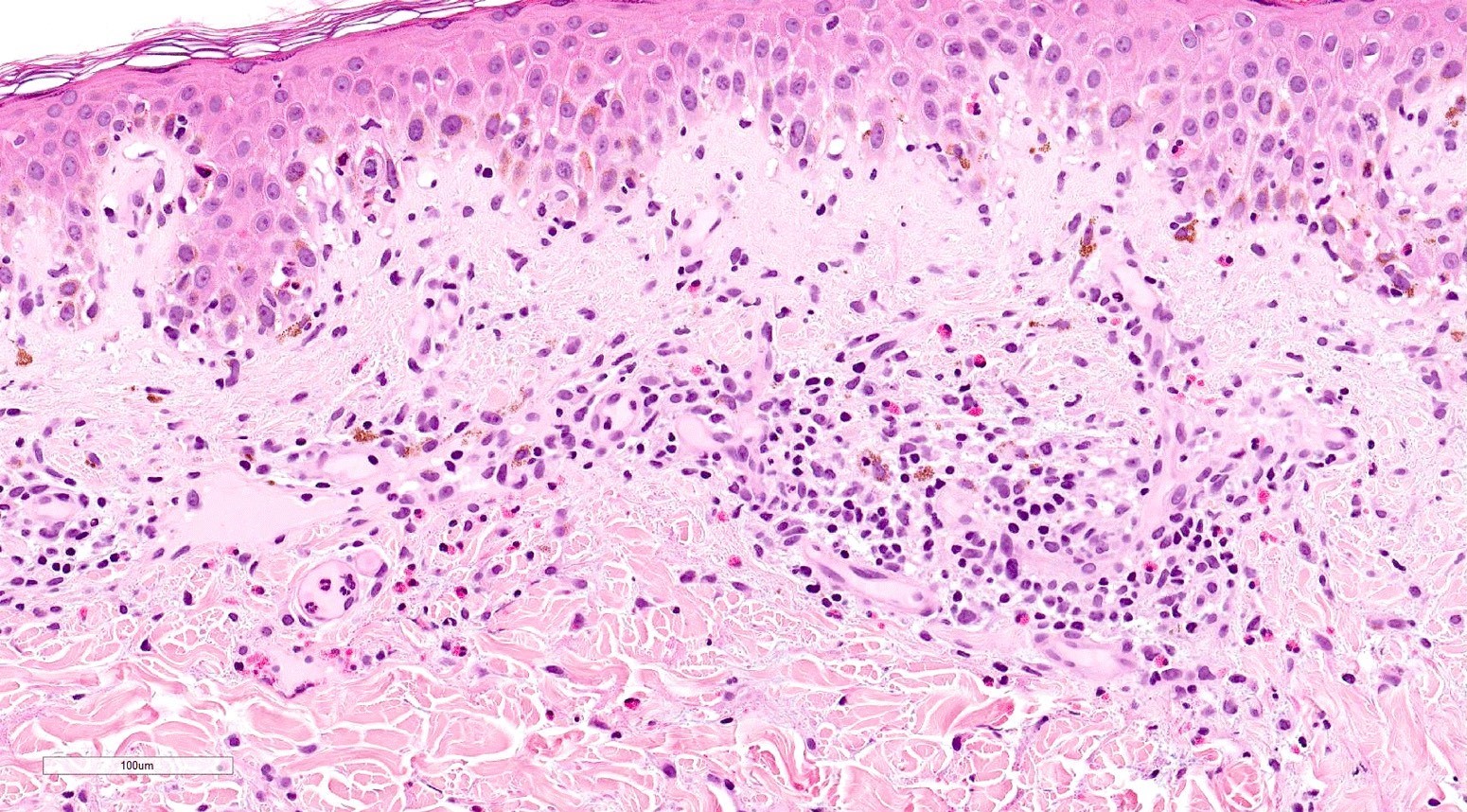
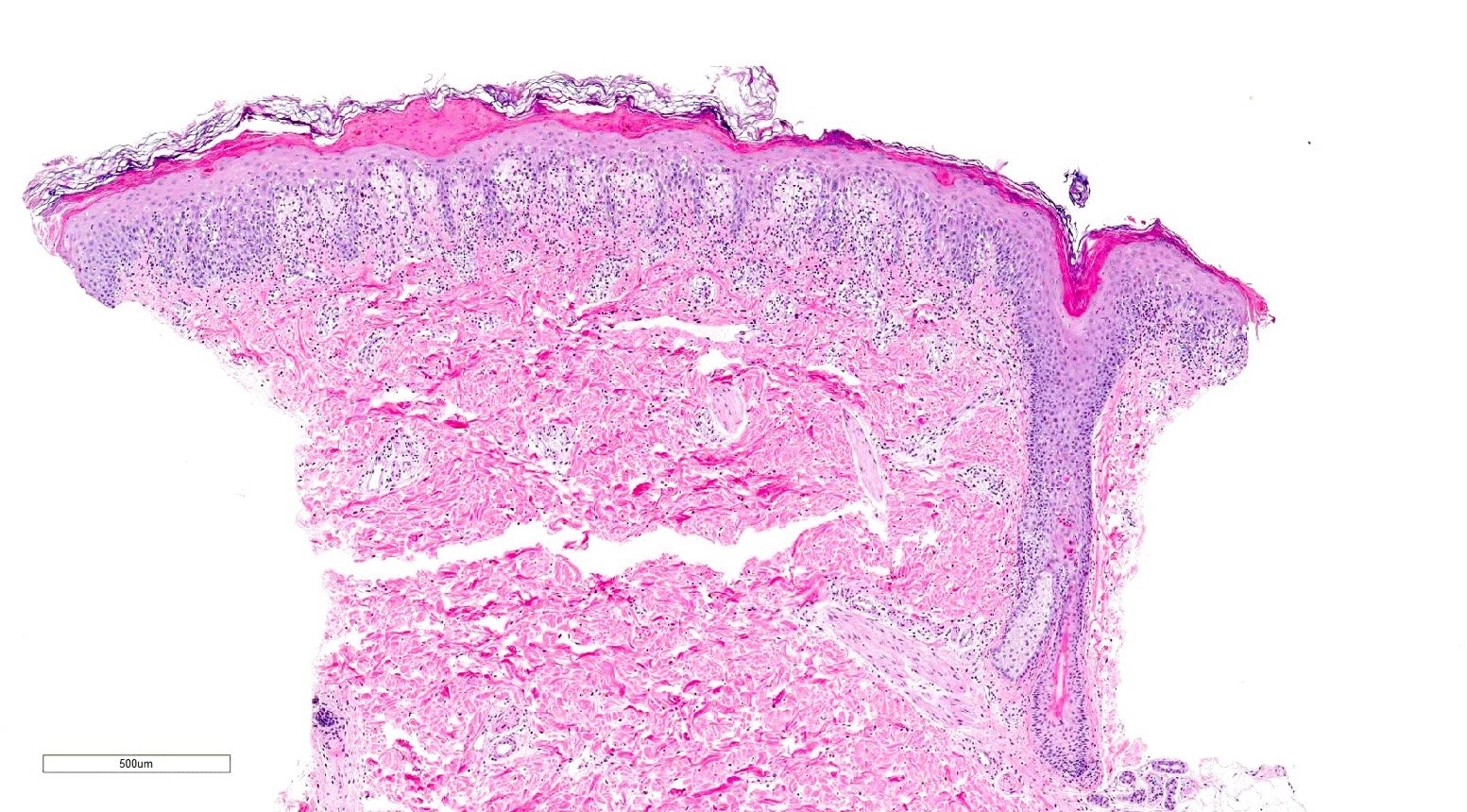
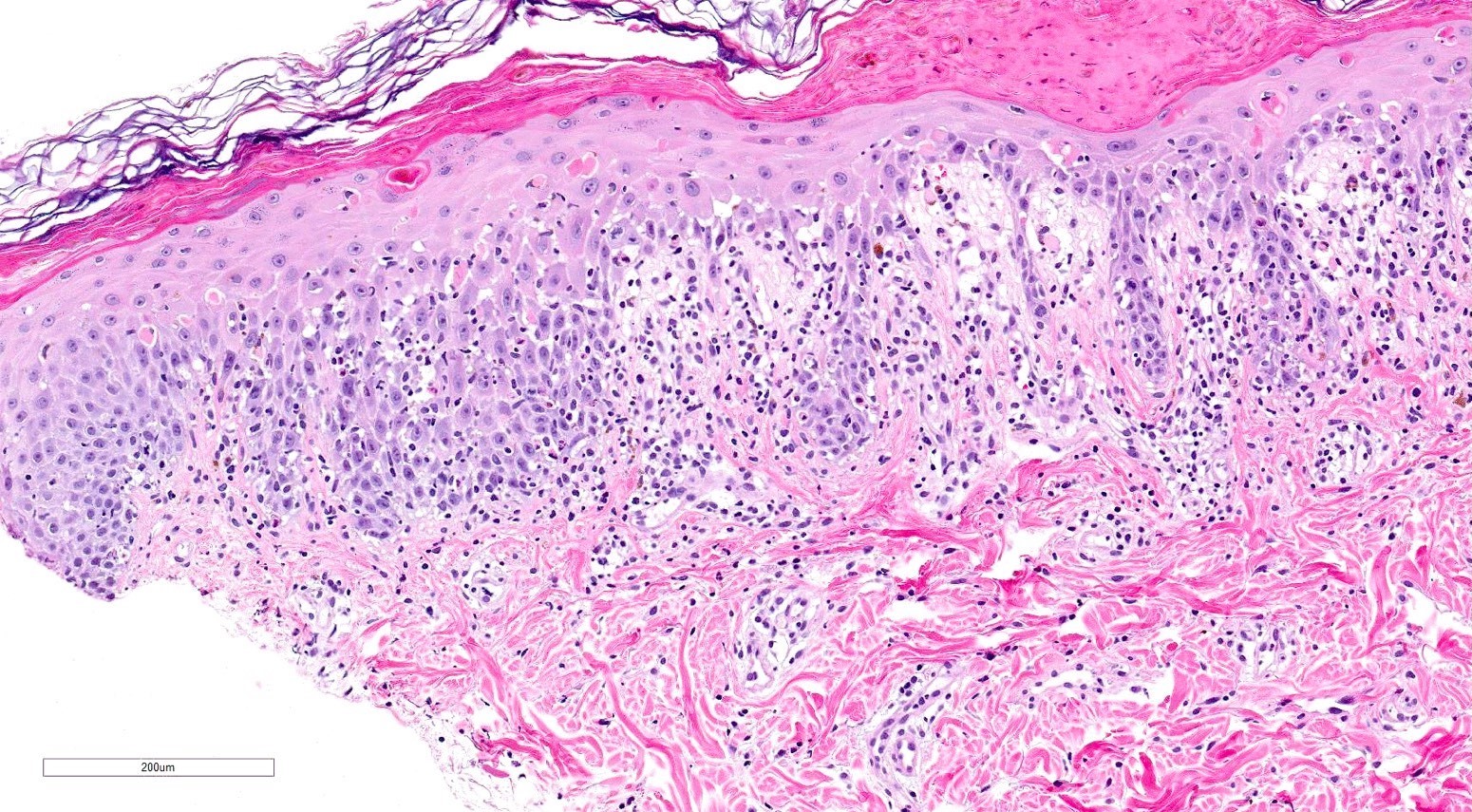
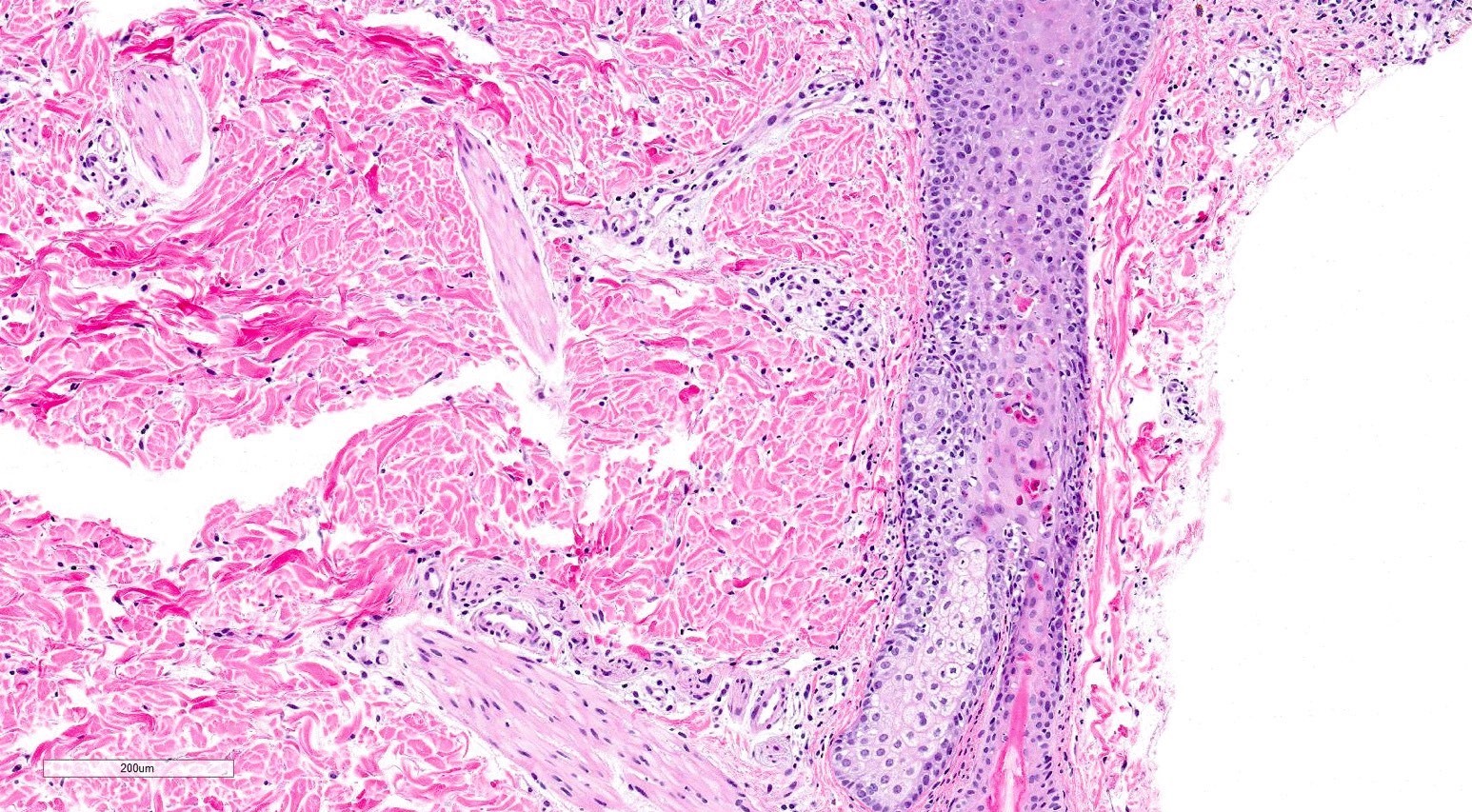
Microscopic (histologic) description
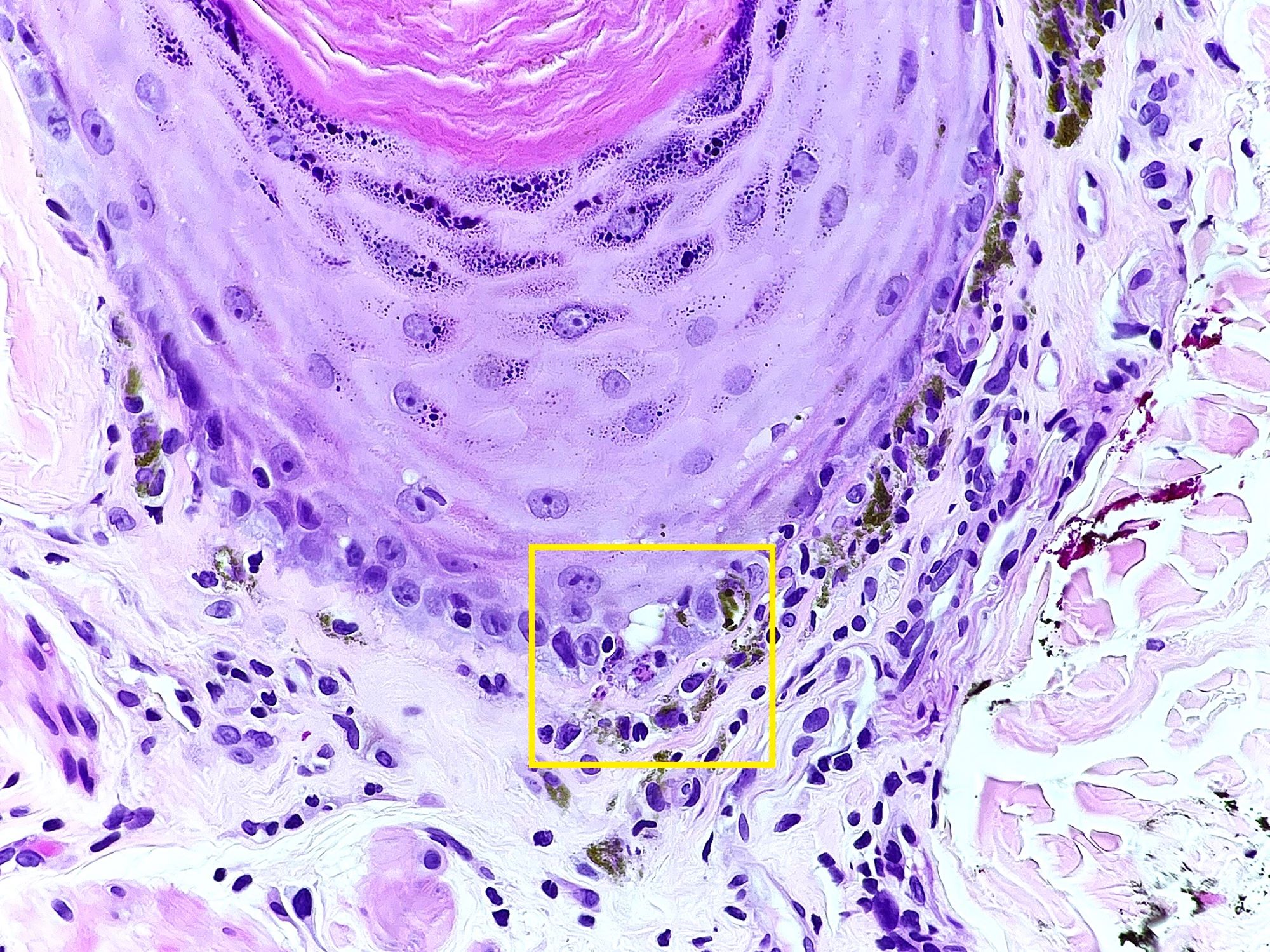
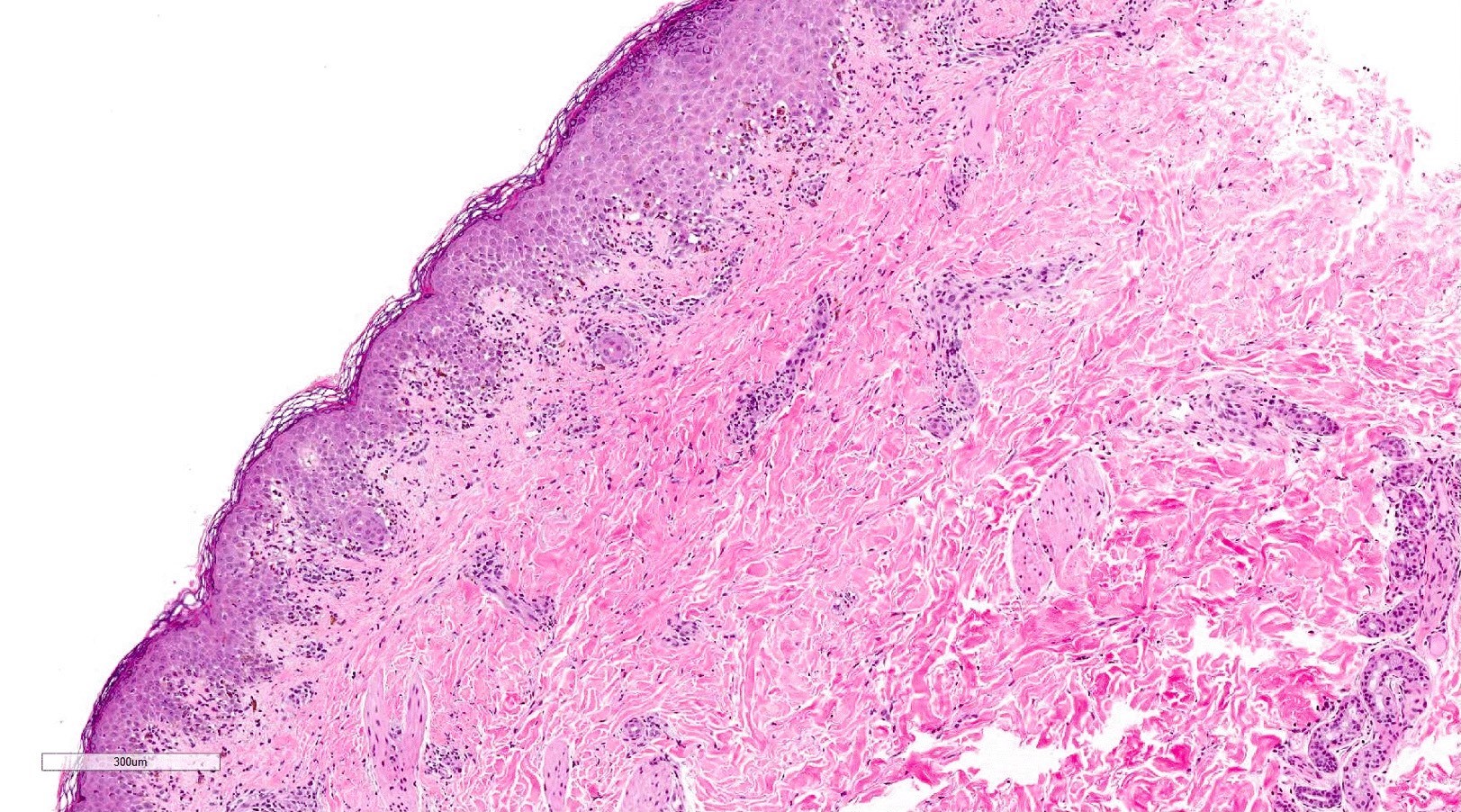
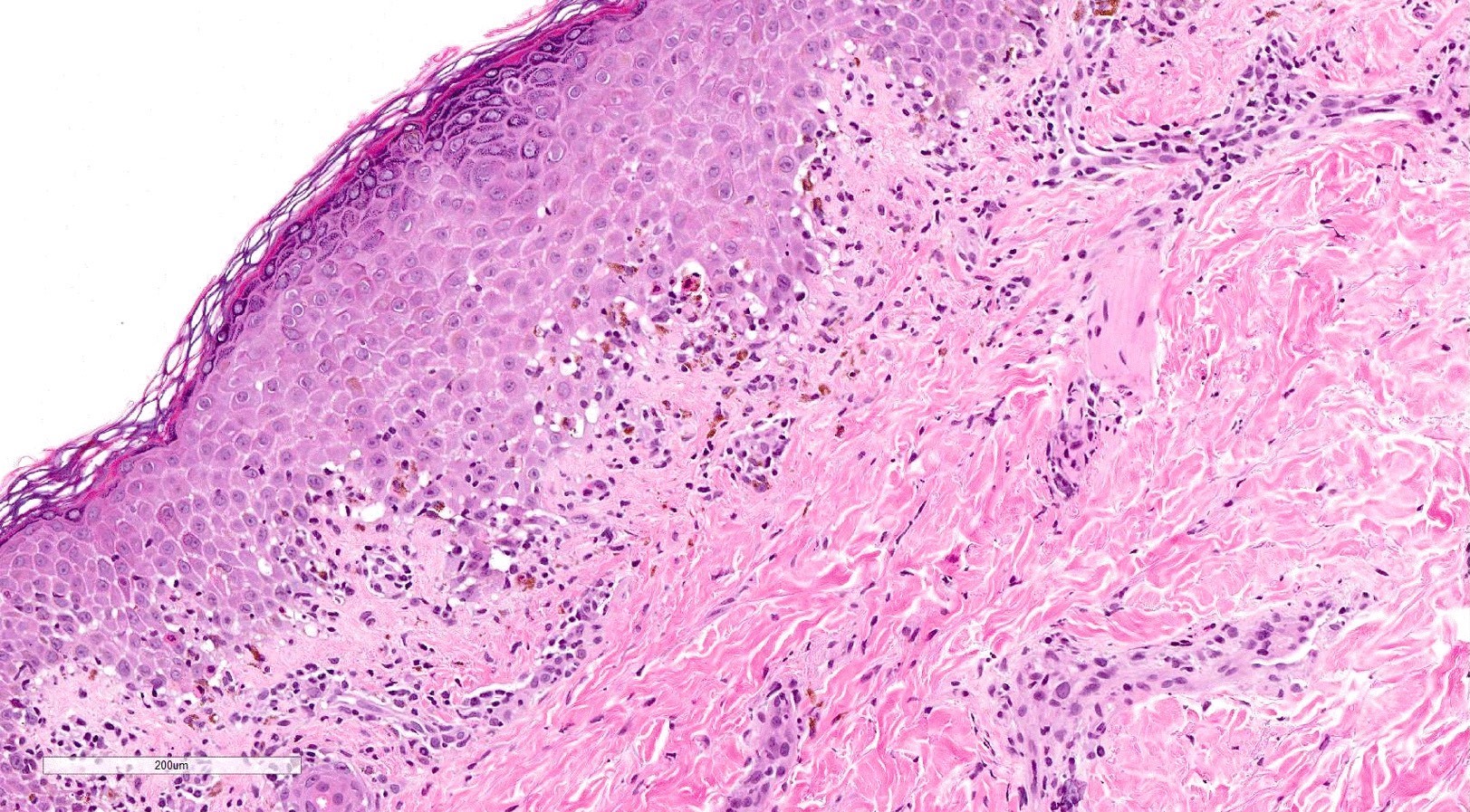
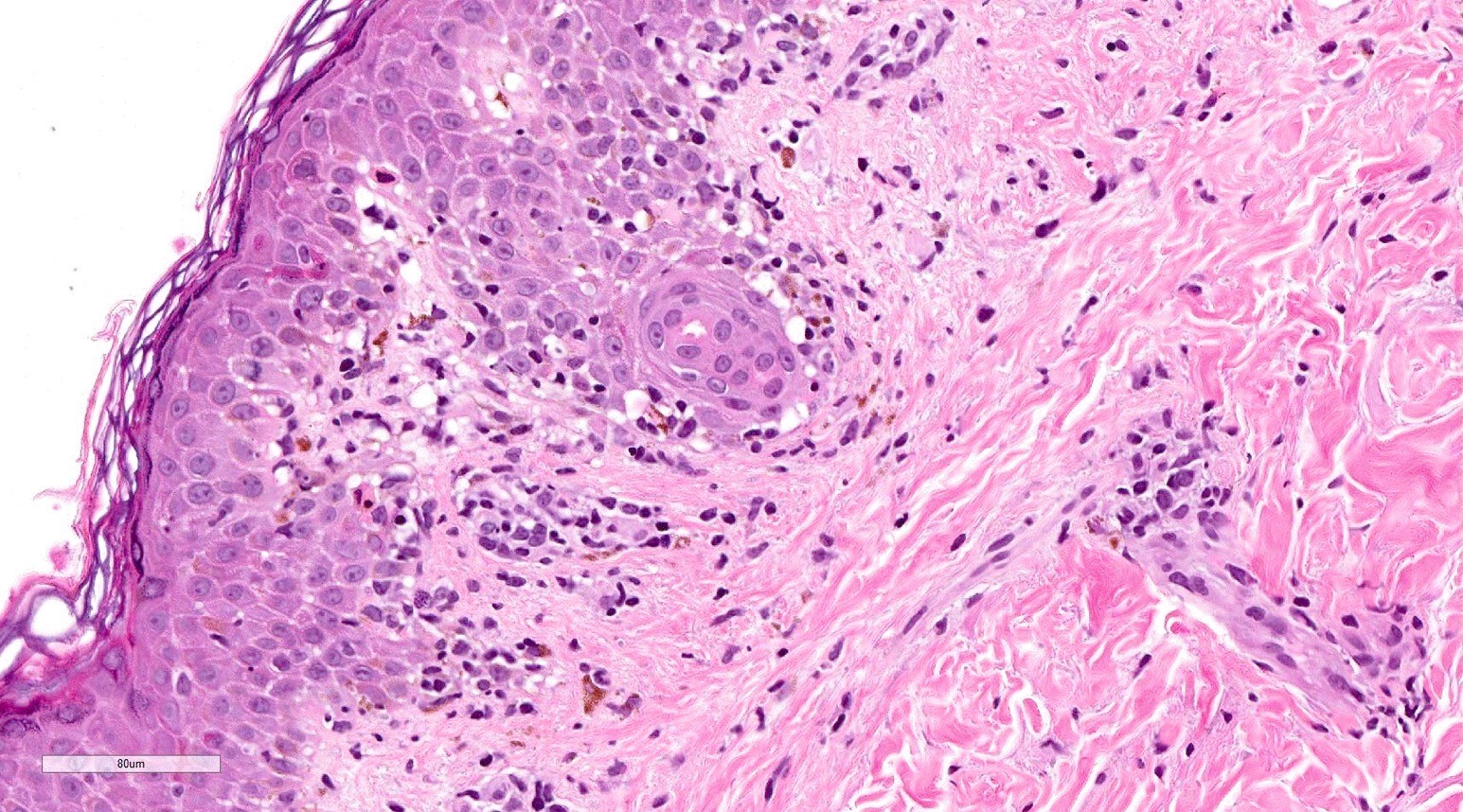
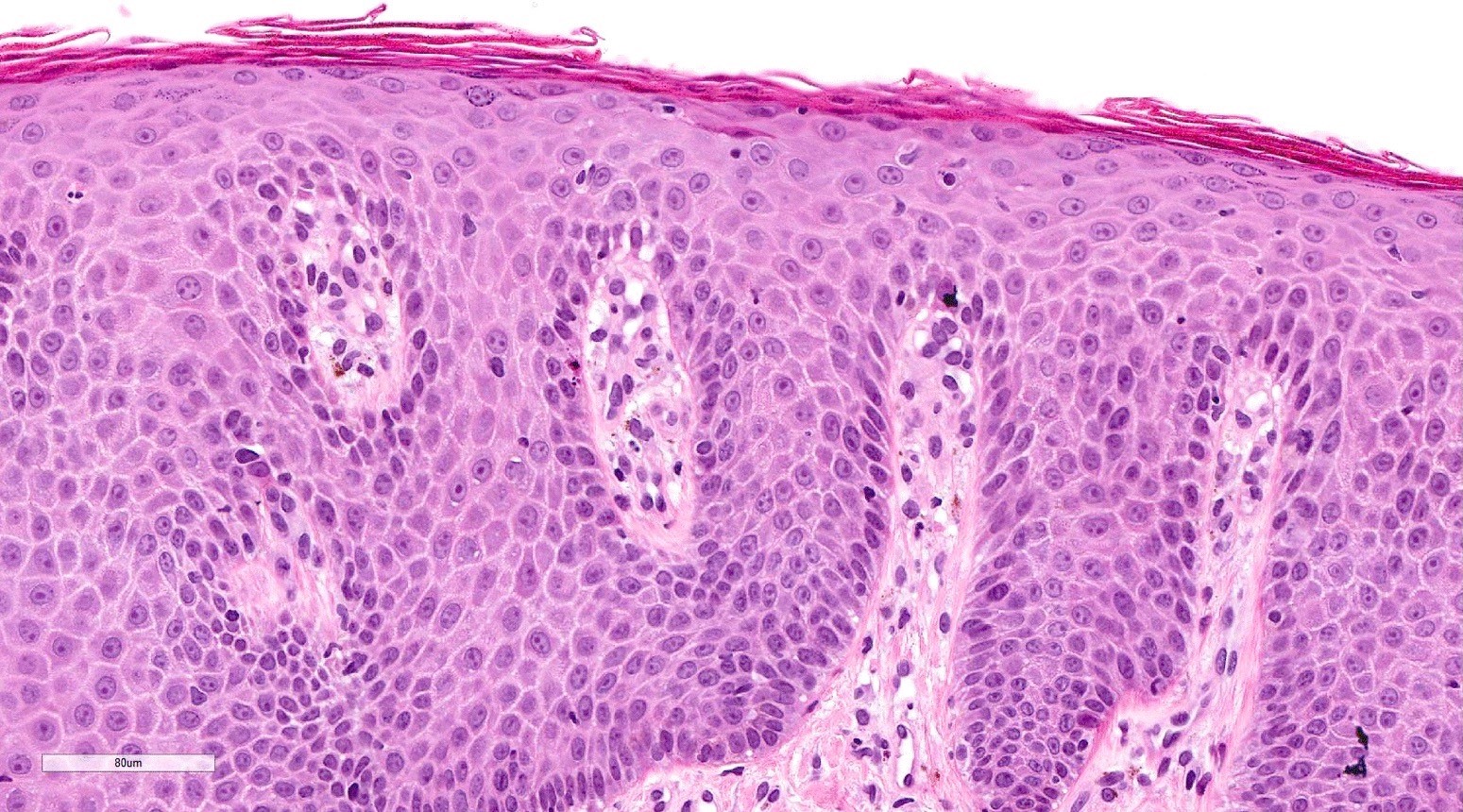
- Acute GVHD (Patterson: Weedon's Skin Pathology, 4th Edition, 2015)
- Mild to moderate superficial perivascular lymphocytic infiltrate with exocytosis of inflammatory cells into the epidermis and basal vacuolation, interface dermatitis
- Scattered, shrunken, eosinophilic keratinocytes with pyknotic nuclei, at all levels of the epidermis; often accompanied by 2 or more lymphocytes, producing the satellite cell necrosis - lymphocyte associated apoptosis
- Occasionally, rare eosinophils can be present; melanin incontinence is prominent in patients with darker skin types
- If severe, subepidermal microvesicles, subepidermal blisters and epidermal necrosis
- Lymphocytic infiltrate in GVHD after solid organ transplantation is usually brisk in comparison to the sparser inflammation following bone marrow transplantation
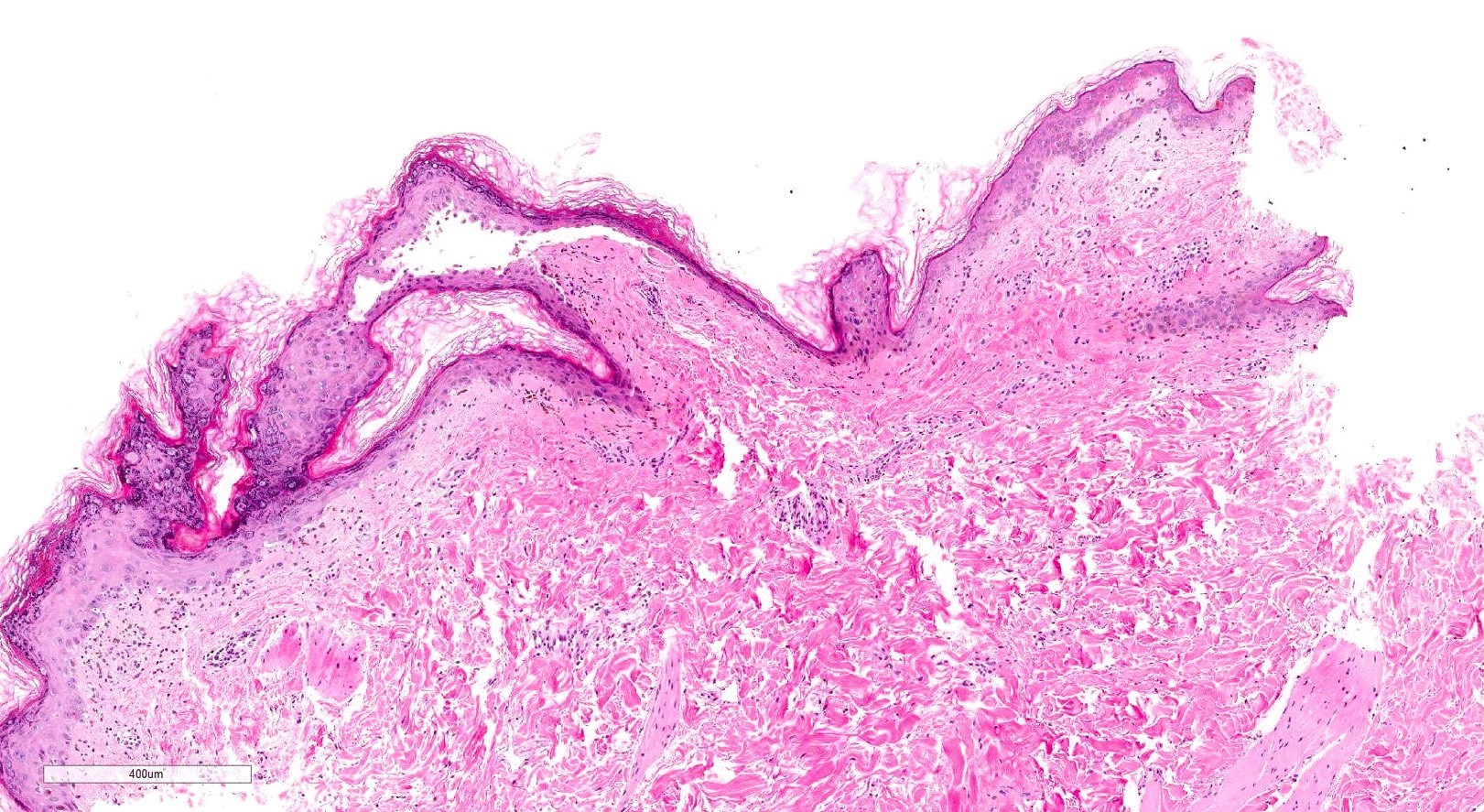
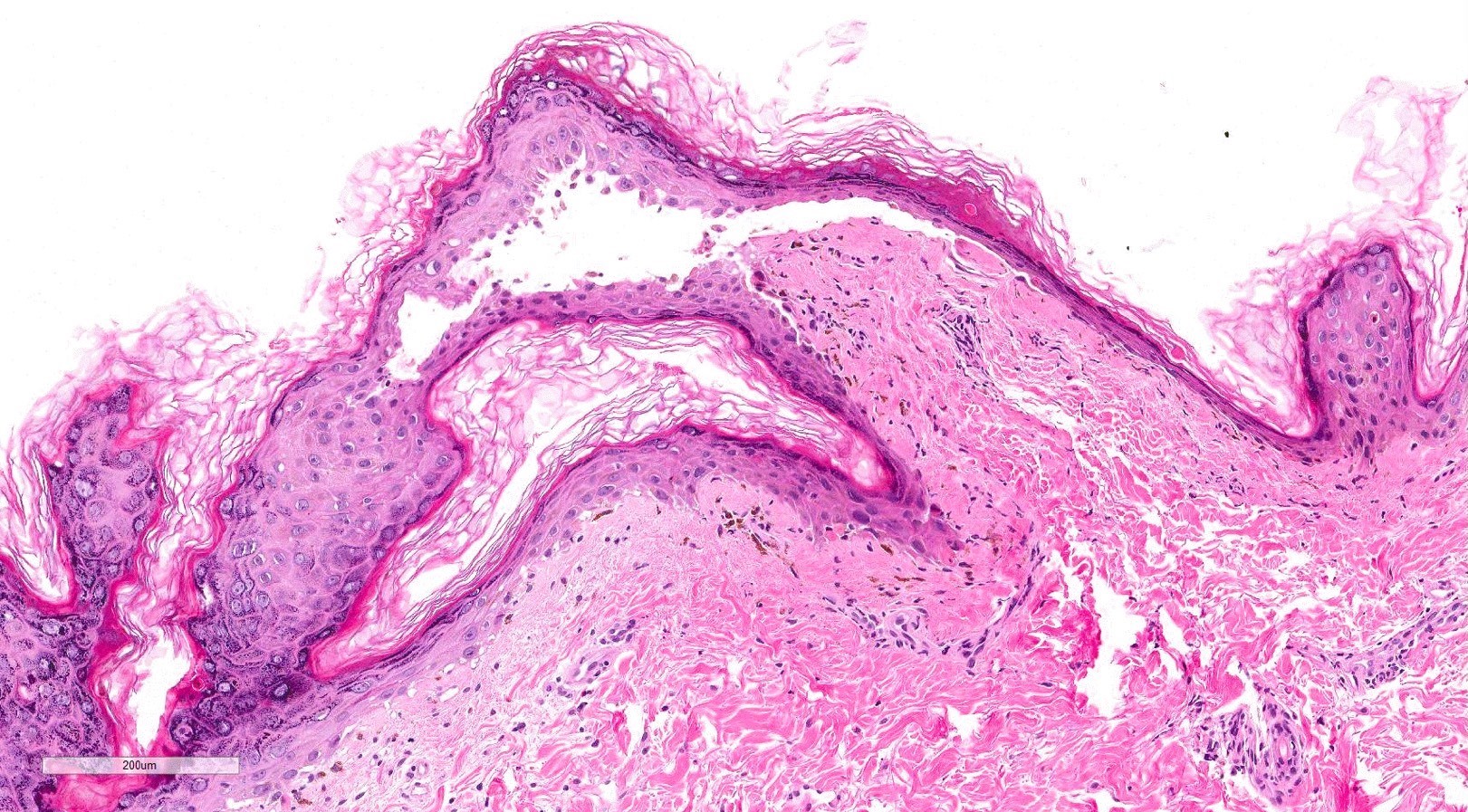
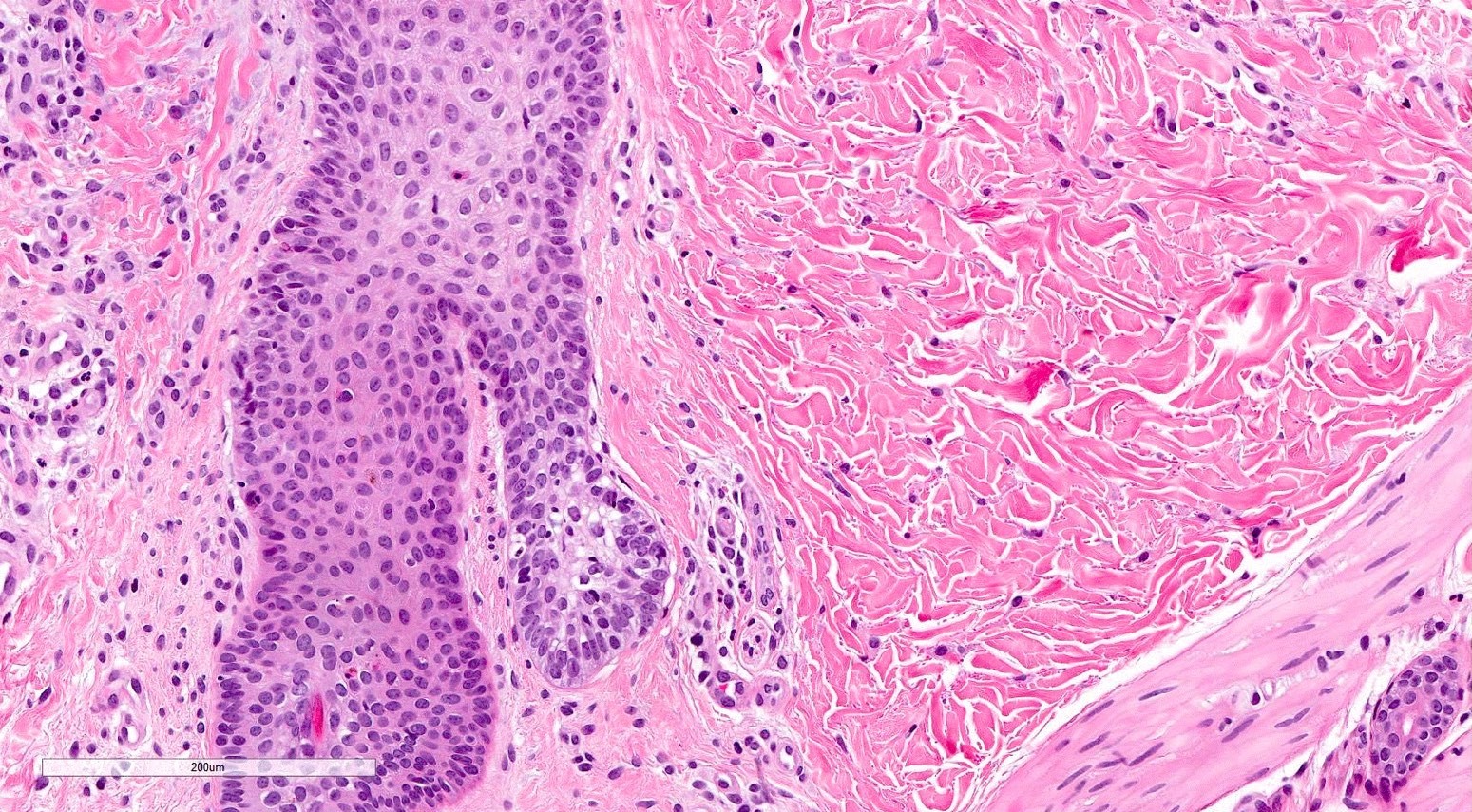
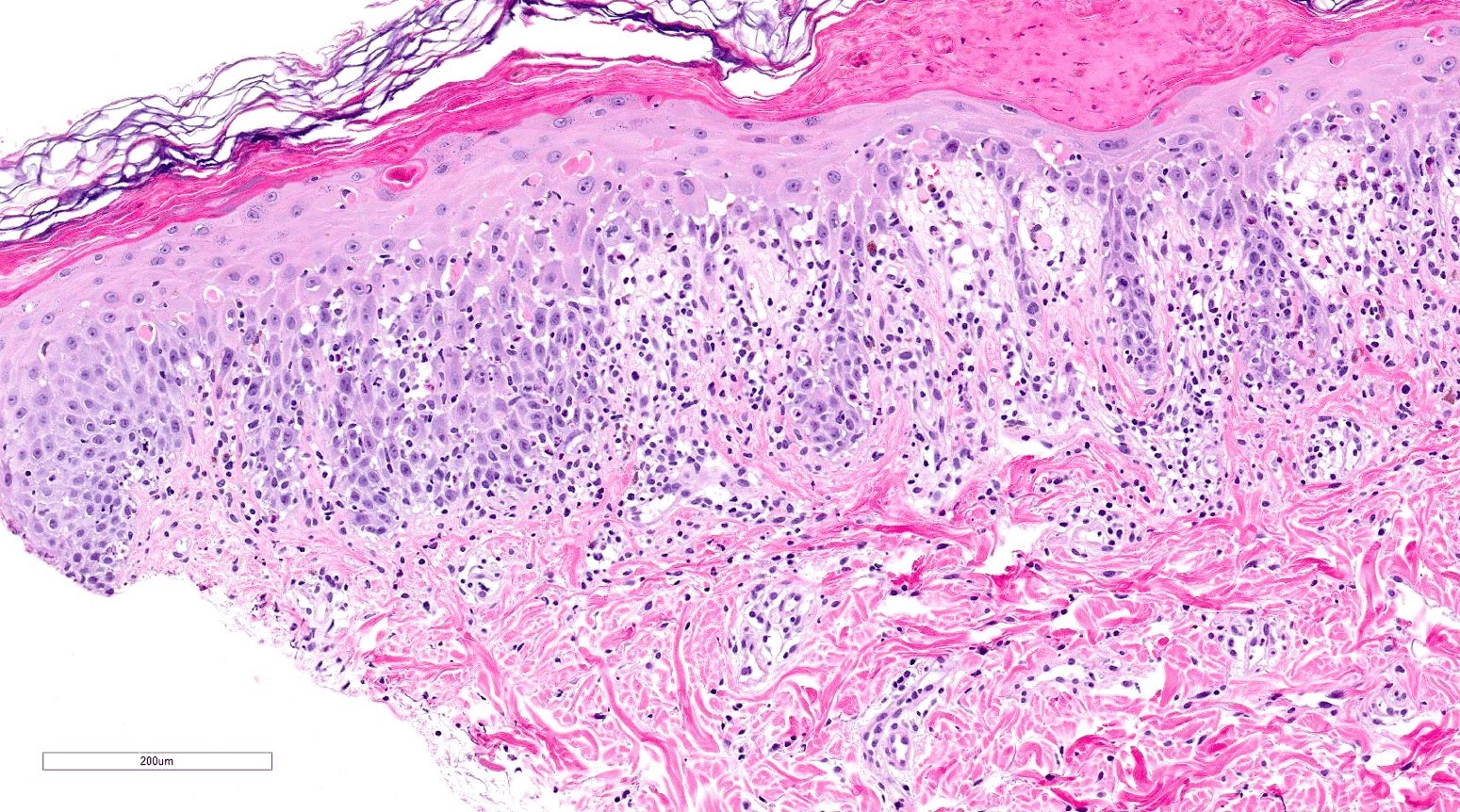
- Chronic GVHD (Biol Blood Marrow Transplant 2015;21:589, Patterson: Weedon's Skin Pathology, 4th Edition, 2015)
- Chronic lichenoid GVHD
- Acanthosis, orthohyperkeratosis, parakeratosis with hypergranulosis
- Underlying band-like lymphocytic infiltrate with basal layer vacuolization and apoptotic keratinocytes
- Periadnexal inflammation can be present
- May be difficult to distinguish from lichen planus without clinicopathologic correlation; satellite cell necrosis is the most helpful clue in GVHD biopsies to distinguish it from lichen planus
- Chronic sclerodermoid GVHD
- Dermal sclerosis (thickened compact collagen with loss of periadnexal fat)
- Manifests with localized morphea-like features, diffuse sclerosis or lichen sclerosus-like features
- Localized morphea-like features and diffuse sclerosis are largely confined to the reticular dermis or subcutaneous septa with little or no epidermal involvement
- Lichen sclerosus-like GVHD: collagen alteration is confined to the papillary dermis (hyalinzation of the papillary dermis), often with residual interface changes characterized by the presence of mild vacuolar alteration, melanophages and sparse superficial perivascular lymphocytic infiltrate
- In the fasciitis variant, biopsy specimens show only fibrous thickening of the fascia with adjacent inflammation without epidermal or dermal involvement
- Rare variants: psoriasiform
- Psoriasiform epithelial hyperplasia
- Subtle vacuolar interface changes
- Satellite cell necrosis (Am J Dermatopathol 2018;40:511)
- Chronic lichenoid GVHD
Microscopic (histologic) images
Contributed by Silvija P. Gottesman, M.D. and Ohoud Aljarbou, M.D.
Immunofluorescence description
- Acute GVHD: immunofluorescence testing is not indicated but can show nonspecific IgM and complement deposits at the basement membrane zone (J Immunol 1978;120:1485)
Sample pathology report
- Skin, forearm, punch biopsy:
- Vacuolar interface dermatitis (see comment)
- Comment: Subtle basilar vacuolar changes with scattered dyskeratotic keratinocytes are seen involving the epidermis and follicular epithelium. In foci, lymphocyte associated apoptosis of keratinocytes (satellite cell necrosis) is noted. There is sparse superficial perivascular lymphocytic infiltrate and absence of eosinophils. Melanin incontinence is noted in the superficial dermis. In the correct clinical setting, these findings are compatible with graft versus host disease. Clinical correlation is recommended.
Differential diagnosis
- Acute GVHD
- Drug reaction (J Am Acad Dermatol 2011;65:726):
- Fewer or less conspicuous eosinophils than are seen in acute drug reaction
- Viral infections (HHV6, HHV7, CMV) (Semin Cutan Med Surg 2007;26:155):
- Look for viral inclusions (CMV) and other clinical clues
- Eruption of lymphocyte recovery (Arch Dermatol 1989;125:1512):
- Self limited; associated with transient fever
- Unlike GVHD, no gastrointestinal or hepatic abnormalities
- Histologically similar to acute GVHD
- Acral erythema (palmoplantar erythrodysesthesia):
- Complication of chemotherapy; affects palms and soles
- Painful symmetrical edema and erythema, blistering and desquamation can happen
- Toxic epidermal necrolysis (J Cutan Pathol 2017;44:857):
- Very challenging to distinguish between this and severe GVHD - clinical correlation
- Engraftment syndrome (Bone Marrow Transplant 2001;27:893):
- Difficult to distinguish from GVHD; there is significant clinical and pathophysiologic overlap - clinical correlation is necessary
- Radiation dermatitis (acute):
- Cutaneous erythema, desquamation, blistering or necrosis
- Histologically similar to acute GVHD - clinical correlation
- Erythema multiforme:
- Clinical picture: target and targetoid lesions are helpful to make a diagnosis
- Histologically similar to acute GVHD
- Drug reaction (J Am Acad Dermatol 2011;65:726):
- Chronic GVHD
- Lichen planus (Clin Dermatol 2005;23:285):
- Lichenoid inflammatory infiltrate is not as dense
- Flexural wrists and shins are classic locations for lichen planus
- Lichenoid drug eruptions (J Cutan Pathol 2021;48:1480):
- Features that are more predictive of a cutaneous drug eruption over GVHD included spongiosis, confluent parakeratosis and numerous eosinophils
- Satellite cell necrosis is more common in GVHD
- Pityriasis lichenoides chronica:
- Overlapping histologic features - clinical correlation
- Eosinophils are rare to absent in both conditions (J Cutan Pathol 2012;39:413)
- Lichen sclerosus (Arch Dermatol 2002;138:924):
- Overlapping histologic features - clinical correlation
- Morphea / systemic sclerosis:
- Distal to proximal progression of cutaneous sclerosis on the extremities is usually not seen in chronic GVHD
- Eosinophilic fasciitis:
- Clinical correlation
- Chronic GVHD presenting as eosinophilic fasciitis is histologically indistinguishable from classic eosinophilic fasciitis (J Clin Rheumatol 2015;21:86)
- Poikiloderma (dermatomyositis, systemic lupus erythematosus) (Lupus 2008;17:591):
- Systemic lupus erythematosus and dermatomyositis may show dermal mucin, which is usually not present in GVHD
- Lichen planus (Clin Dermatol 2005;23:285):
Board review style question #1
A 40 year old woman with a history of AML and status post-bone marrow transplant 2 months ago presented with fever and pruritic maculopapular eruption on palms and soles. Physical exam showed smooth and hyperkeratotic papules. Patient shares that at times she is noncompliant with taking her prescribed medications. Lately she has started using herbal supplements recommended by a friend. Punch biopsy from the foot was taken and microscopic exam showed mild vacuolar interface dermatitis with superficial perivascular lymphocytic infiltrate in the dermis and no eosinophils. Focally in the epidermis, eosinophilic degenerated keratinocytes surrounded by lymphocytes were noted. What is the most likely diagnosis?
- Acute graft versus host disease
- Chronic graft versus host disease
- Drug reaction
- HHV6 infection
Board review style answer #1
A. Acute graft versus host disease. The patient has a history of bone marrow transplant, medication noncompliance and presents with a rash. Biopsy shows vacuolar interface dermatitis with superficial perivascular lymphocytic infiltrate in the dermis, no eosinophils and rare dyskeratotic keratinocytes. The combined clinical and morphologic features listed above are most consistent with acute graft versus host disease. Answer B is incorrect because chronic graft versus host disease would show lichenoid or sclerodermoid features. Answer C is incorrect because drug eruption would present with tissue eosinophilia. Answer D is incorrect because HHV6 infection shows nonspecific microscopic features.
Comment Here
Reference: Graft versus host disease
Comment Here
Reference: Graft versus host disease
Board review style question #2
A 30 year old man with a history of hematologic malignancy and bone marrow transplant 1 year prior presents to the dermatology clinic with erythematous and violaceous papules and plaques on the trunk, dorsal hands and forearms. Punch biopsy from the forearm showed vacuolar interface dermatitis with associated lichenoid inflammation in the papillary dermis, pigment incontinence and absence of eosinophils. Interface changes extend down follicular epithelia. What is the most likely diagnosis?
- Chronic lichenoid graft versus host disease
- Chronic sclerodermoid graft versus host disease
- Lichenoid drug eruption
- Lichen planus
Board review style answer #2
A. Chronic lichenoid graft versus host disease. The patient presents with a rash and has a history of bone marrow transplant. Biopsy shows vacuolar interface dermatitis associated with lichenoid inflammation in the papillary dermis, pigment incontinence and absence of eosinophils. The combined clinical and morphologic features listed above are most consistent with chronic lichenoid graft versus host disease. Answer B is incorrect because chronic sclerodermoid graft versus host disease would show dermal sclerosis, which is absent in this case. Answer C is incorrect because lichenoid drug eruption would show prominent eosinophils, which are not appreciated here. Answer D is incorrect because lichen planus has characteristic clinical presentation of intensely pruritic papules and the inflammatory infiltrate is more prominent than in GVHD.
Comment Here
Reference: Graft versus host disease
Comment Here
Reference: Graft versus host disease
Board review style question #3
Board review style answer #3
B. Graft versus host disease. Biopsy shows epidermis with basal vacuolization and dyskeratotic keratinocytes. There is mild superficial dermal and perivascular lymphocytic infiltrate. The given clinical history along with the pathological findings support the diagnosis of graft versus host disease (GVHD). Answer A is incorrect because while discoid lupus erythematosus histologically can resemble GVHD (basal vacuolar interface change), it shows dermal mucin, which is usually absent in GVHD. Answer C is incorrect because while pityriasis lichenoides chronica and GVHD show similar histologic features, clinical correlation favors GVHD in this case. Answer D is incorrect because viral exanthem has nonspecific histologic findings, including spongiosis, perivascular lymphocytic infiltrate and sometimes lymphoexocytosis and necrotic keratinocytes in epidermis; eosinophils are usually absent. Clinically presents as a morbilliform rash. Clinical correlation and history of bone marrow transplant favors GVHD.
Comment Here
Reference: Graft versus host disease
Comment Here
Reference: Graft versus host disease