Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Vanderbeck K, Torres-Cabala CA. Scleromyxedema. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorscleromyxedema.html. Accessed September 22nd, 2025.
Definition / general
- Dermal fibroblast proliferation with increased collagen and mucin (J Scleroderma Relat Disord 2019;4:118, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Localized (lichen myxedematosus / papular mucinosis), generalized (scleromyxedema) and atypical forms (J Am Acad Dermatol 2001;44:273)
Essential features
- Dermal fibroblastic proliferation with deposition of mucin and increased collagen (J Scleroderma Relat Disord 2019;4:118, Postepy Dermatol Alergol 2013;30:122, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Older lesions may demonstrate flattened or thinned epidermis, atrophy of dermal adnexal structures with mild superficial pervascular lymphocytic infiltrate
- Progressive skin thickening (Postepy Dermatol Alergol 2013;30:122)
Terminology
- Lichen myxedematosus / papular mucinosis: diffuse or focal mucin deposition in upper dermis
- Fibroblast proliferation is less evident
- Progressive skin thickening not seen
- In general, lichen myxedematosus demonstrates less skin involvement and is more localized than scleromyxedema (An Bras Dermatol 2019;94:462, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Lichen myxedematosus, papular mucinosis and scleromyxedema have been used interchangeably in literature
ICD coding
Epidemiology
- There is no gender or race predilection (J Scleroderma Relat Disord 2019;4:118, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Most common in middle aged adults (J Scleroderma Relat Disord 2019;4:118)
Sites
- Scleromyxedema: face, neck, upper limbs, torso, hands; symmetrical distribution (Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011, J Am Acad Dermatol 2001;44:273, An Bras Dermatol 2016;91:48)
- Lichen myxedematosus: any location; most often limbs, acral sites (acral persistent papular mucinosis) and trunk (An Bras Dermatol 2019;94:462, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Visceral sites may be affected (Ann Dermatol 2020;32:168, J Am Acad Dermatol 2013;69:66)
Pathophysiology
- Not clearly understood (J Am Acad Dermatol 2001;44:273, J Scleroderma Relat Disord 2019;4:118)
Etiology
- Unknown; association with plasma cell dyscrasias reported, particularly monoclonal band IgG (lambda) (J Scleroderma Relat Disord 2019;4:118)
Clinical features
- Lichen myxedematosus: skin colored to erythematous papules; may be present in any location with predilection for limbs and trunk (J Am Acad Dermatol 2001;44:273, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Scleromyxedema: waxy, skin colored to erythematous papules
- Often beginning on wrists and hands with spread to forearms, trunk and face
- Facial lesions characterized by linear papules that coalesce into plaques (J Scleroderma Relat Disord 2019;4:118, Postepy Dermatol Alergol 2013;30:122, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- May lead to sclerosis of skin, contractures, tightening of skin around mouth and fingers (sclerodactyly) (Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- May see systemic involvement: esophagus, pulmonary, cardiac, neurologic (J Am Acad Dermatol 1998;38:289, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- IgG lambda gammopathy can be seen with progression to multiple myeloma (rare) (J Scleroderma Relat Disord 2019;4:118, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Donut sign: involvement of the interphalangeal joints
- Central depression seen surrounded by an elevated / thickened skin
- Can lead to sclerodactyly (J Scleroderma Relat Disord 2019;4:118)
- Shar pei sign: deep longitudinal furrowing on trunk or limbs (J Scleroderma Relat Disord 2019;4:118)
- Leonine face: deep furrowing on face, particularly glabellar region with distortion of features (J Scleroderma Relat Disord 2019;4:118)
- Atypical: overlapping features of lichen myxedematosus and scleromyxedema (J Am Acad Dermatol 2001;44:273)
- May involve the entire body
- Visceral involvement noted, contributing to complications and guarded prognosis (J Am Acad Dermatol 2013;69:66, J Scleroderma Relat Disord 2019;4:118, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
Diagnosis
- Presence of clinical features (J Am Acad Dermatol 2001;44:273)
- Histologic analysis (see Microscopic (histologic) description)
Laboratory
- Monoclonal IgG (lambda type) or evidence of other plasma cell dyscrasias (J Scleroderma Relat Disord 2019;4:118, Postepy Dermatol Alergol 2013;30:122)
Prognostic factors
- Scleromyxedema has a worse prognosis than lichen myxedematosus, especially if cardiac or pulmonary involvement (J Am Acad Dermatol 2013;69:66, J Am Acad Dermatol 1998;38:289, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Multiple myeloma is possible but relatively rare (J Scleroderma Relat Disord 2019;4:118, Mayo Clin Proc 2024;99:283)
- Unpredictable course (Postepy Dermatol Alergol 2013;30:122, J Am Acad Dermatol 2013;69:66)
Case reports
- 45 year old woman with scleromyxedema on face, neck, trunk and extremities (Front Immunol 2023;13:1099918)
- 47 year old man with scleromyxedema on face, ears, neck and upper extremities (Case Rep Dermatol 2013;5:168)
- 54 year old man with granulomatous scleromyxedema (Am J Dermatopathol 2015;37:240)
- 73 year old man with scleromyxedema treated with lenalidomide, bortezomib and dexamethasone (Clin Case Rep 2020;8:3043)
Treatment
- Systemic corticosteroids, thalidomide, psoralen plus ultraviolet A radiation (PUVA), photopheresis, electron beam radiation, plasmapheresis, cyclophosphamide (Postepy Dermatol Alergol 2013;30:122, An Bras Dermatol 2016;91:48, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Spontaneous resolution has been reported (J Drugs Dermatol 2020;19:320)
- IVIG with maintenance infusions demonstrate good effect and well tolerated by patients (J Clin Aesthet Dermatol 2014;7:45)
- Lenalidomide, bortezomib and dexathemasone (RVD) therapy has been reported; however, literature is limited (Clin Case Rep 2020;8:3043)
- Stem cell transplantation has been reported to be relatively successful for remission of scleromyxedema (Arch Dermatol 2005;141:1277)
- Treatment of underlying gammopathy
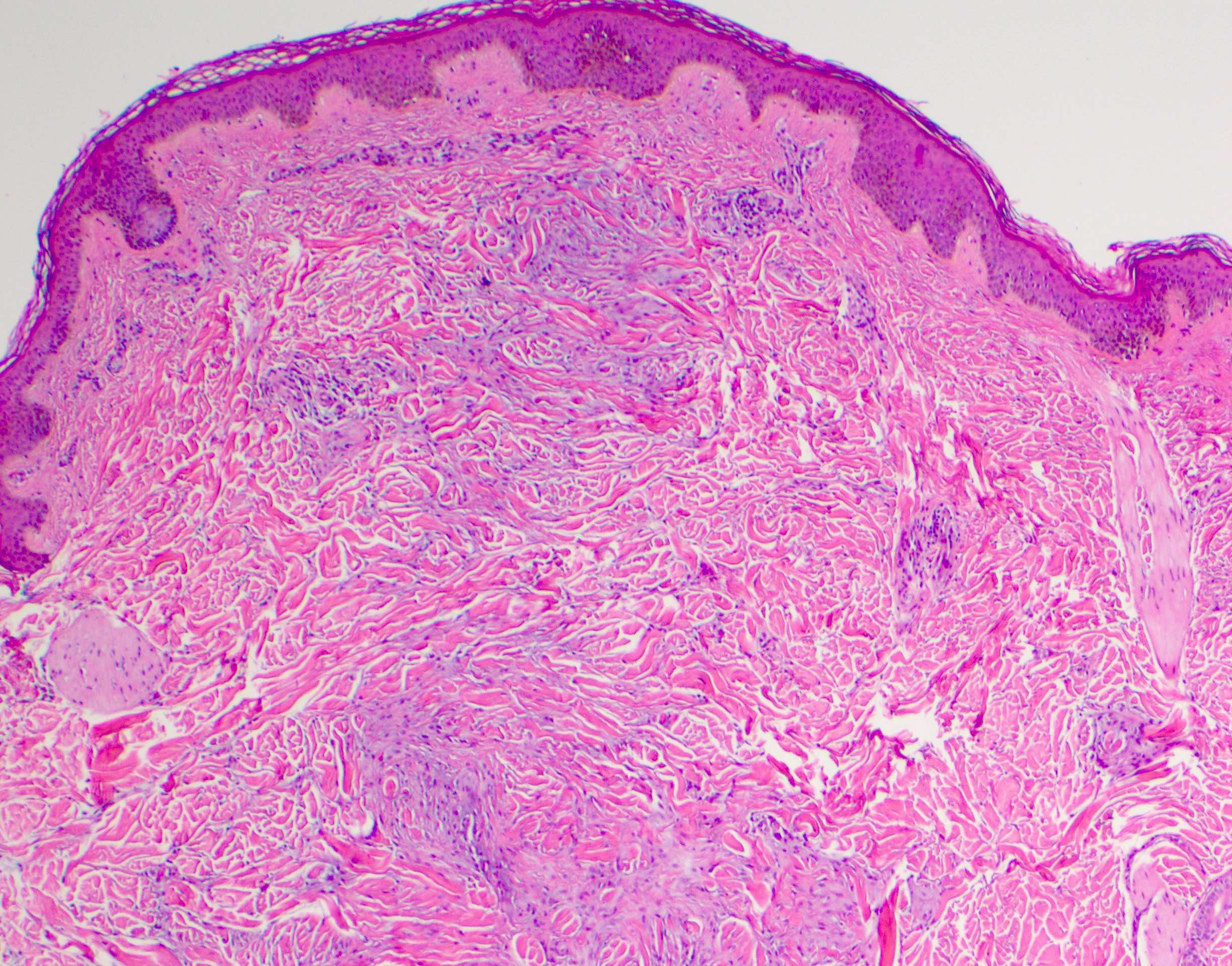
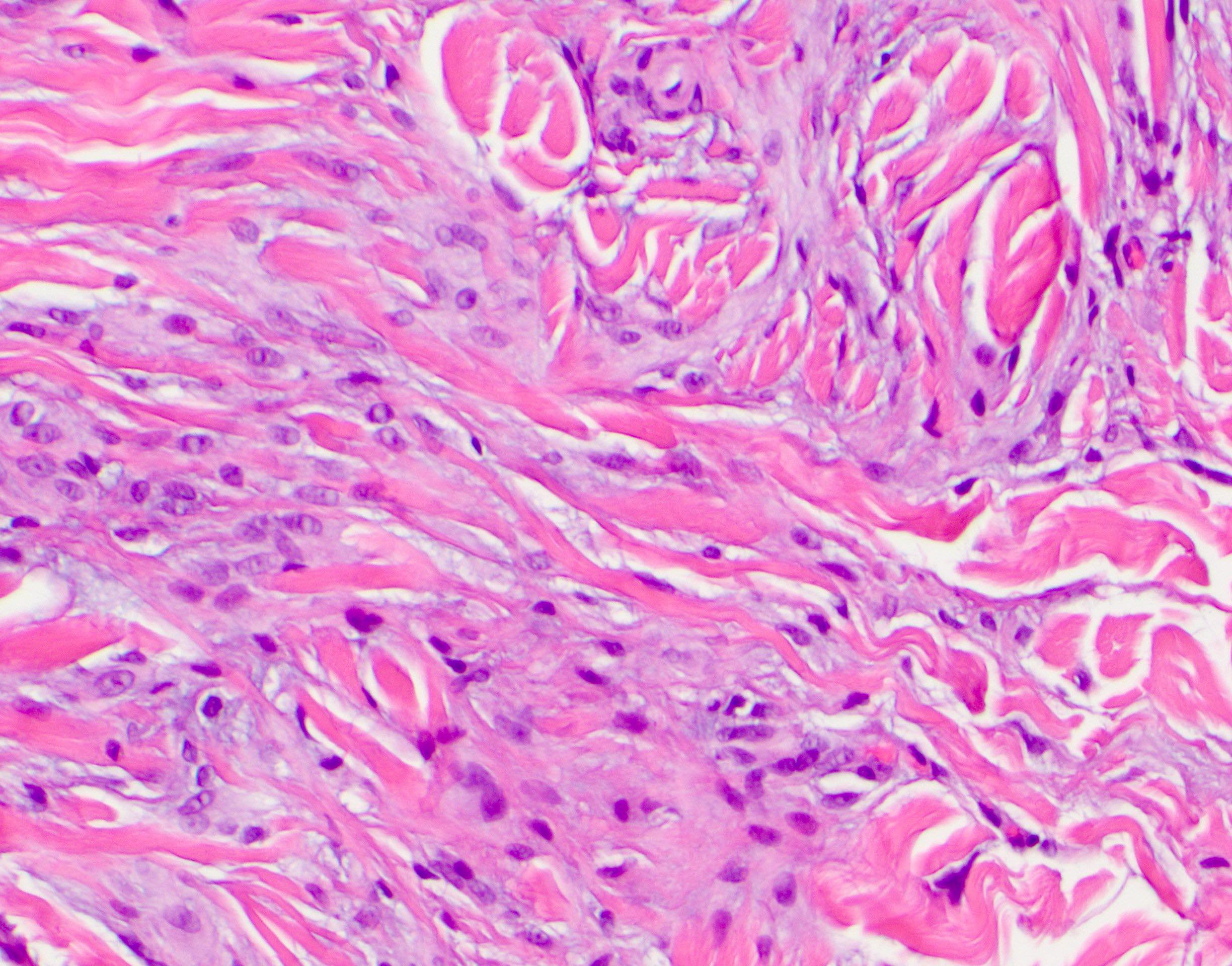
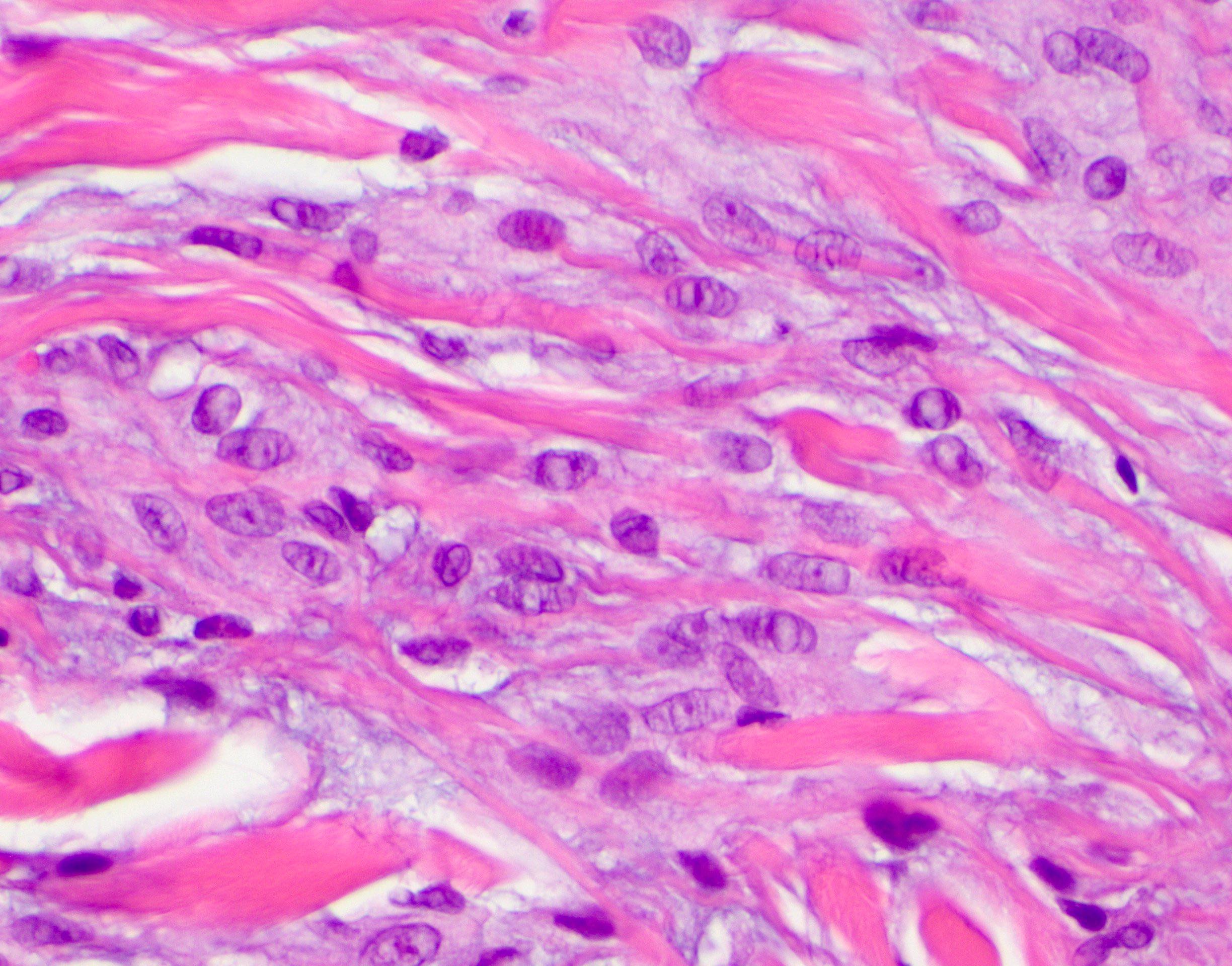
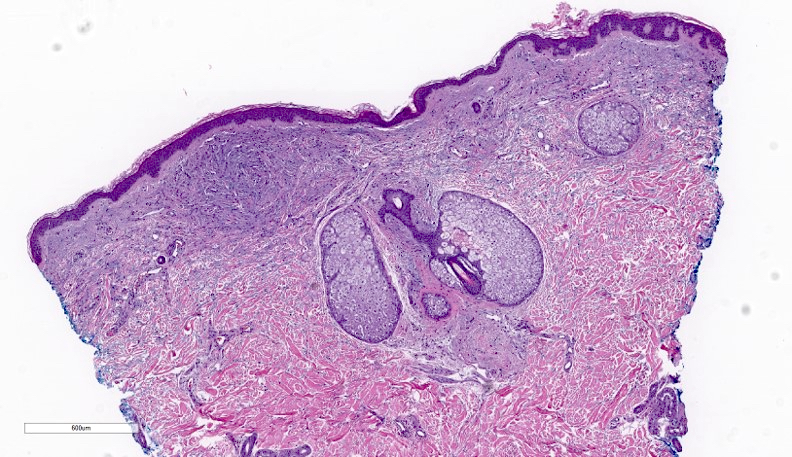
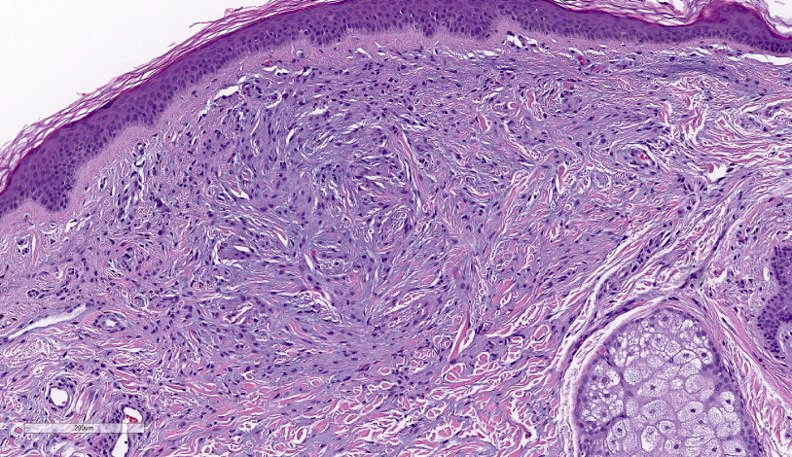
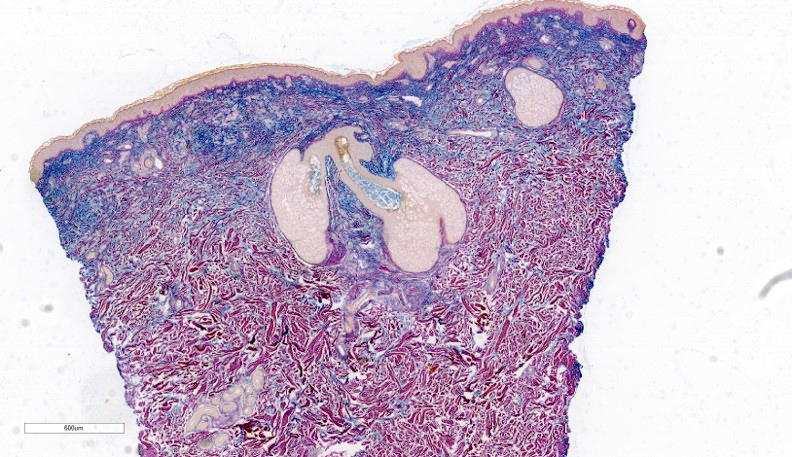
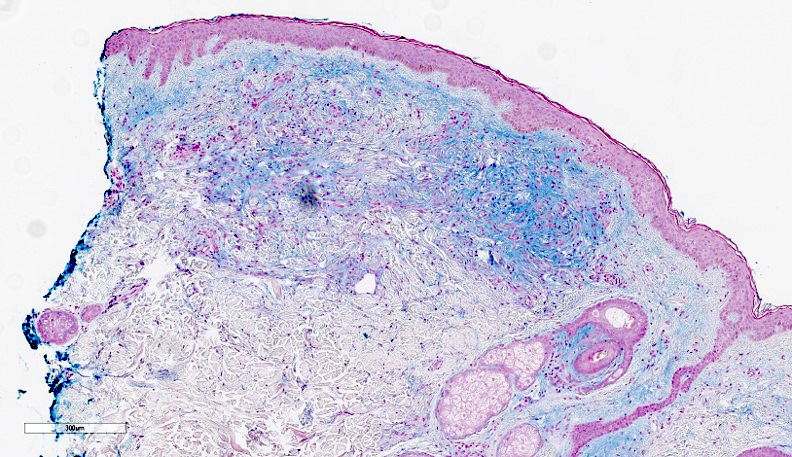
Microscopic (histologic) description
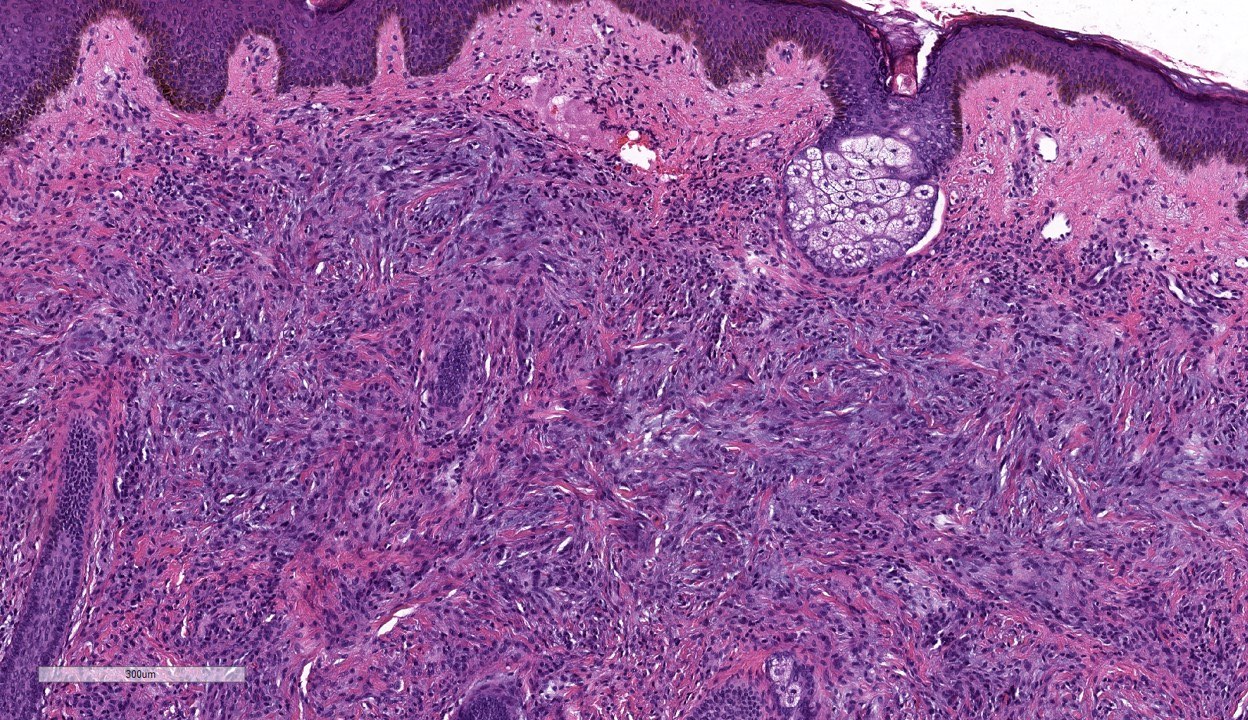
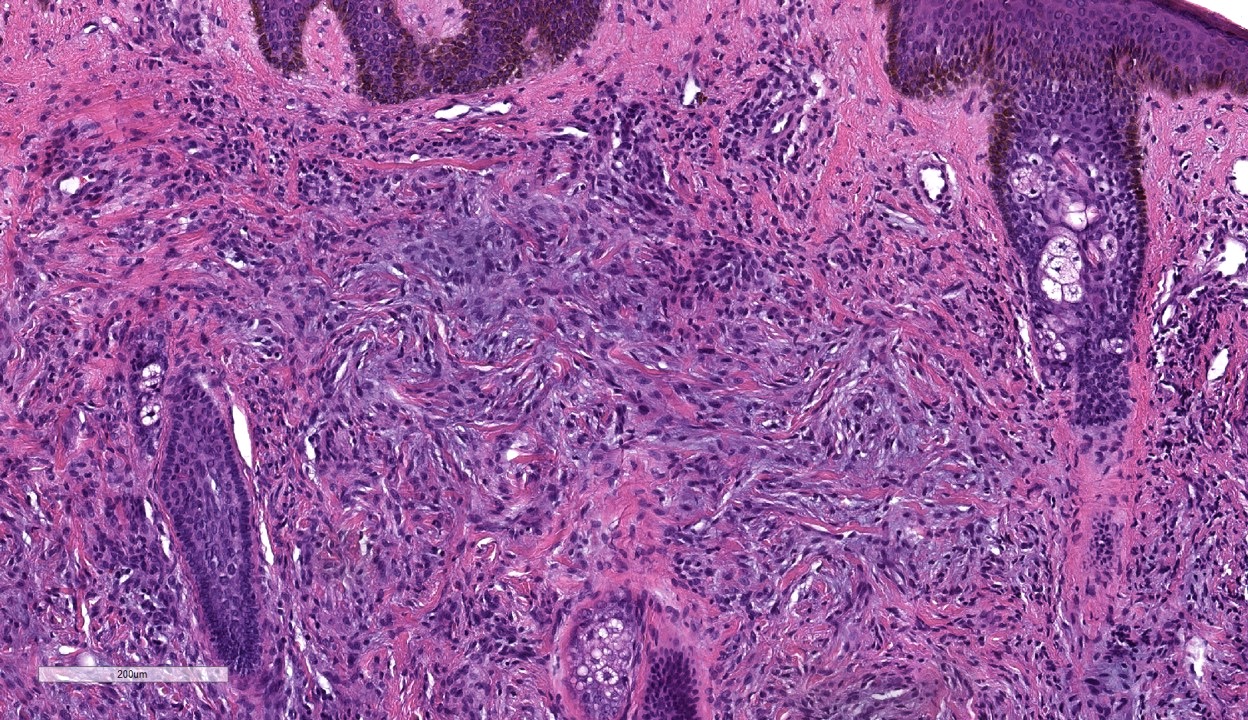
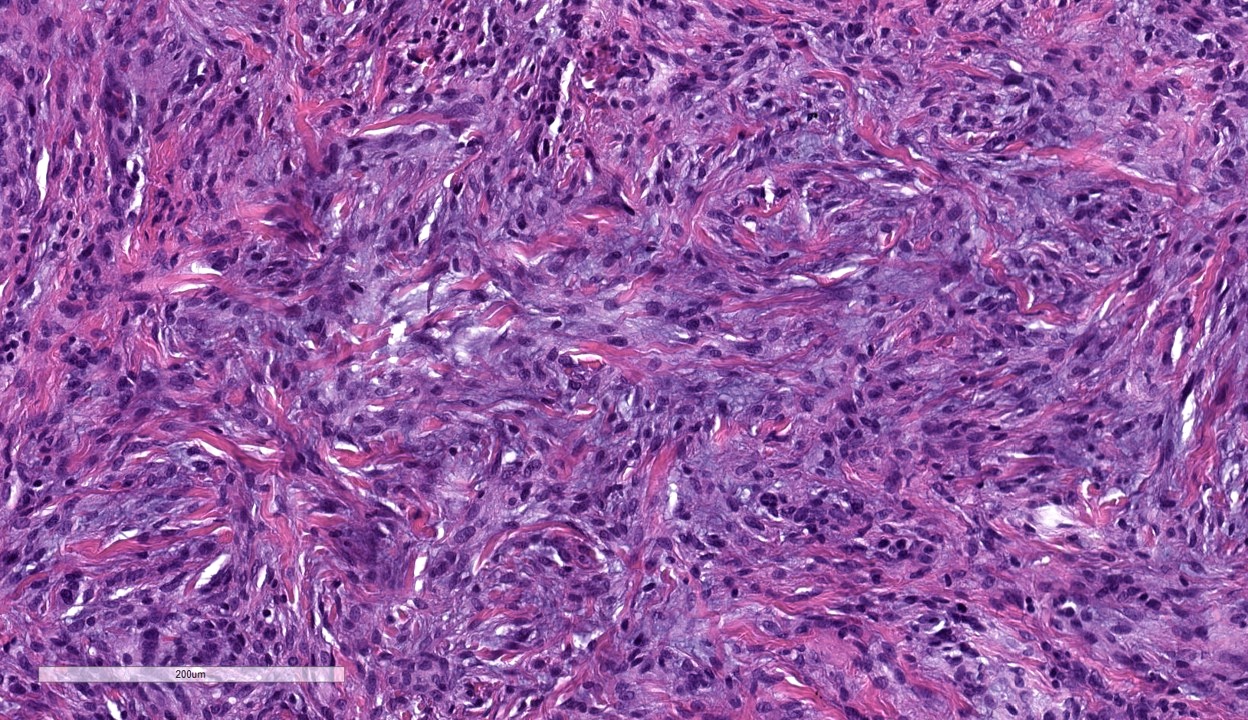
- Lichen myxedematosus and scleromyxedema appear similar (Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Increased number of spindled fibroblasts in reticular dermis (J Scleroderma Relat Disord 2019;4:118, J Am Acad Dermatol 2016;74:1194, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Increased dermal mucin, especially in early disease
- Dermal fibrosis and thickening common in late stage scleromyxedema (J Am Acad Dermatol 2016;74:1194)
- Superficial lymphocyte predominant perivascular infiltrate (mild) (J Scleroderma Relat Disord 2019;4:118)
- Epidermis atrophic to acanthotic (Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Some cases may show loose granulomas and interstitial deposition of mucin, similar to interstitial granuloma annulare (J Cutan Pathol 2010;37:1084)
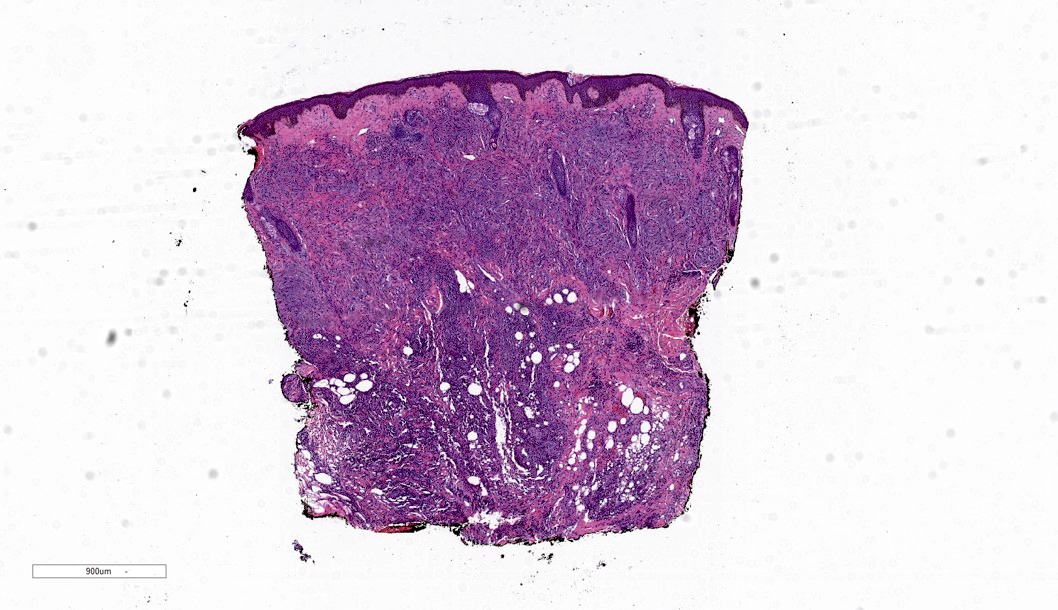
Microscopic (histologic) images
Contributed by Carlos A. Torres-Cabala, M.D.
Immunofluorescence description
- May show scant granular IgG deposition along epidermal basement membrane and focal IgG positivity in connective tissue (J Scleroderma Relat Disord 2019;4:118, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
Positive stains
- Stains for mucin deposition (e.g., colloidal iron special stain) may show increased dermal mucin
Sample pathology report
- Skin, left forearm, punch biopsy:
- Consistent with scleromyxedema (see comment)
- Comment: Sections show skin with atrophic epidermis and increased thickened collagen with spindled fibroblasts within the dermis. There is increased mucin deposition within the dermis, confirmed with colloidal iron special stain. Note is made of the patient’s history and presentation. The findings are in keeping with scleromyxedema. Further clinical correlation is recommended as appropriate.
Differential diagnosis
- Pretibial myxedema:
- Location: anterior lower legs
- No increase in fibroblasts or collagen
- Fragmentation of superficial collagen bundles with increased interstitial mucin
- Association with hypothyroidism (J Scleroderma Relat Disord 2019;4:118, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Nephrogenic systemic fibrosis (NSF):
- Similar histologic features to scleromyxedema; involves deep dermis and subcutis
- Association with renal failure, gadolinium exposure (J Scleroderma Relat Disord 2019;4:118, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Scleredema:
- Scleredema type 1:
- ~55% of cases affecting predominantly young patients (children and young adults)
- Onset begins after febrile infection (streptococcal infection most common) within 2 to 3 weeks following illness (StatPearls: Scleredema [Accessed 9 September 2024])
- Scleredema type 2:
- ~25% of cases and young patients
- Insidious onset with slow progression
- Paraproteinemia is the most commonly associated condition, which develops years after onset of scleredema
- Also associated with monoclonal gammopathy of undetermined significance (MGUS, IgG, IgA), multiple myeloma and amyloidosis (StatPearls: Scleredema [Accessed 9 September 2024])
- Scleredema type 3:
- ~20% of cases
- Seen in diabetic patients (scleredema diabeticorum)
- Complication of poorly controlled insulin dependent diabetes, with severe vascular complications associated (StatPearls: Scleredema [Accessed 9 September 2024])
- Histology
- No increase in fibroblasts, mucin deposition present but less than in scleromyxedema
- Thickened and enlarged collagen fibers within mid and reticular dermis with extension to subcutis
- Adnexal structures present
- Epidermis unremarkable (J Scleroderma Relat Disord 2019;4:118, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011, StatPearls: Scleredema [Accessed 9 September 2024]).
- Interstitial granuloma annulare:
- Granulomatous inflammation with surrounding mucin (interstitial)
- No history of progressive generalized involvement (J Scleroderma Relat Disord 2019;4:118, Hall: Diagnostic Pathology - Nonneoplastic Dermatopathology, 3rd Edition, 2021, Brinster: Dermatopathology - A Volume in the High Yield Pathology Series, 1st Edition, 2011)
- Morphea / scleroderma:
- Localized (morphea, localized scleroderma) and systemic sclerosis
- Early morphea / scleroderma demonstrates lymphocyte predominant perivascular infiltrate within superficial and deep dermis
- This is followed by the development of obliterative sclerosis within dermis and subcutis, with thickened collagen bundles and attenuation or atrophy of adnexal structures
- Scleredema type 1:
Additional references
Practice question #1
Practice answer #1
D. Scleromyxedema. Progressive skin changes starting first with hands and progressing to other sites is characteristic of this disorder. Histologic findings of increased fibrosis, collagen and mucin within dermis are also characteristic. Answer B is incorrect because lymphocyte predominant perivascular infiltrate within superficial and deep dermis in early lesions. Followed by the development of obliterative sclerosis within dermis and subcutis, with thickened collagen bundles and attenuation or atrophy of adnexal structures. Answer C is incorrect because the patient has no history of hypothyroidism. Anterior lower legs are not involved and biopsies show fragmentation of superficial collagen bundles with increased interstitial mucin. Answer A is incorrect because, despite the histologic overlap, there is a history of progressive involvement of multiple body sites. Granulomatous inflammation (interstitial) with associated mucin.
Comment Here
Reference: Scleromyxedema
Comment Here
Reference: Scleromyxedema
Practice question #2
Patients with scleromyxedema may have which associated comorbidity?
- Hypothyroidism
- Multiple myeloma
- Renal failure
- Rosacea
Practice answer #2
B. Multiple myeloma. Scleromyxedema is often associated with plasma cell dyscrasias. Multiple myeloma can be seen with this disorder, although rare. Answer A is incorrect because hypothyroidism is associated with (not a consequence of) pretibial myxedema. Answer C is incorrect because a history of renal failure is seen in nephrogenic systemic fibrosis. Answer D is incorrect because rosacea is not associated with this disorder.
Comment Here
Reference: Scleromyxedema
Comment Here
Reference: Scleromyxedema