Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Asadbeigi SN, Nguyen C. Dysplastic nevus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumormelanocyticdysplasticnevus.html. Accessed September 14th, 2025.
Definition / general
- Controversial topic (J Am Acad Dermatol 2012;67:19.e1)
- Pigmented lesions that share clinical and histological features of both common nevi and melanoma (J Am Acad Dermatol 2012;67:19.e1)
Essential features
- First described by Clark and colleagues in 1978 (Arch Dermatol 1978;114:732)
- Dysplastic nevi are characterized by histological, rather than clinical, criteria
- Although many melanomas arise de novo (without an obvious or detectable precursor lesion), approximately 25% histologically demonstrate an associated melanocytic nevus (J Natl Cancer Inst 2016;108:djw121)
Terminology
- Clark nevus
- Nevus with architectural disorder
- Nevus with architectural disorder and cytologic atypia
- Atypical mole
- B-K mole syndrome (Semin Cutan Med Surg 1999;18:4)
- Dysplastic nevus syndrome (Am J Dermatopathol 1982;4:455)
- Familial atypical multiple mole melanoma syndrome (Can Med Assoc J 1968;99:17l)
Epidemiology
- Common in general population, with incidence of 2 - 18% (StatPearls: Dysplastic Nevi [Accessed 14 April 2022])
- More common in younger patient populations (StatPearls: Dysplastic Nevi [Accessed 14 April 2022])
- Usually becomes clinically apparent after puberty (J Am Acad Dermatol 2012;67:1.e1)
- Higher incidence in patients with skin Fitzpatrick type I or II, compared to III and IV (Am Fam Physician 2015;91:762)
- Predilection in sun exposed areas and in patients with histories of acute sunburn (Am Fam Physician 2015;91:762)
- Higher incidence among patients with history of melanoma (StatPearls: Dysplastic Nevi [Accessed 14 April 2022])
- Higher risk for melanoma development in patients with nevi demonstrating more severe atypia (Mod Pathol 2003;16:764)
- Inherited in autosomal dominant pattern in families with dysplastic nevus syndrome (Melanoma Res 1993;3:15)
Sites
- Skin of any body site can be involved
- More common on trunk and sun exposed skin (Am Fam Physician 2015;91:762)
Pathophysiology
- Pathophysiology is not well understood (StatPearls: Dysplastic Nevi [Accessed 14 April 2022])
- Familial cases:
- Autosomal dominant with incomplete penetrance
- CDKN2A mutation but found less frequently than in melanoma (Melanoma Res 1993;3:15)
- BRAF (most commonly V600E), p53 and p16 mutation (StatPearls: Dysplastic Nevi [Accessed 14 April 2022])
Etiology
- Etiology is not well characterized; it appears that multiple factors, such as genetics and environment, play roles in dysplastic nevus development (StatPearls: Dysplastic Nevi [Accessed 14 April 2022])
- CDKN2A point mutations or deletions are not commonly found in dysplastic nevi (StatPearls: Dysplastic Nevi [Accessed 14 April 2022], Arch Dermatol 2005;141:177)
Clinical features
- Dysplastic nevi are characterized by histologic features; clinically, dysplastic nevi may appear small and banal
- Atypical nevi demonstrate the following clinical features:
- Usually > 5 mm
- Irregular borders
- Some with a pigmented and erythematous rim
- Variegated pigmentation with a mixture of pink, light and dark brown
- Dermoscopy: reticular pattern, dots and clods at the periphery (J Dermatol 2019;46:e76, Dermatol Clin 2016;34:395)
- Classic dysplastic nevus syndrome:
- Patients with 100 or more nevi with at least 1 nevus larger than 8 mm and at least 1 nevus with clinical atypical features
- National Institutes of Health revision: this term should only be used in patients with a positive family history for melanoma (Clinics (Sao Paulo) 2011;66:493)
- Eruptive atypical nevus may develop after chemotherapy or immunotherapy (Pediatr Dermatol 2007;24:135)
Diagnosis
- Diagnosis is heavily dependent on the histologic features and has a relatively poor interobserver correlation (J Am Acad Dermatol 2012;67:1.e1)
- Initial diagnostic biopsy should sample entire lesion (Australas J Dermatol 2005;46:70)
Prognostic factors
- Most dysplastic nevi never progress to melanomas even though they are associated with melanomas
- Several studies suggest that patients with dysplastic nevi demonstrate an increased risk of melanoma, between 4 - 15 fold (J Am Acad Dermatol 2012;67:1.e1)
- Patients with familial dysplastic nevus syndrome have an increased risk of developing other malignancies, particularly pancreatic cancer (Int J Cancer 2000;87:809)
- Patients with dysplastic nevi and 2 or more family members with melanoma have a higher risk of melanoma but patients who have a family history of melanoma and no dysplastic nevi are only at an average risk for melanoma (Clinics (Sao Paulo) 2011;66:493)
- Risk of melanoma increases as the number of dysplastic nevi increase (Melanoma Manag 2016;3:85)
- Superficial spreading type melanoma is more commonly associated with dysplastic nevus compared with lentigo maligna type melanoma (Arch Dermatol 2003;139:1620)
Case reports
- 22 year old man with multiple eruptive dysplastic nevi and postchemotherapy in situ melanomas (Pediatr Dermatol 2007;24:135)
- 24 year old man with pointillist dysplastic nevus (Arch Dermatol 2005;141:763)
- 38 year old woman with dysplastic nevi and pancreatic cancer (Exp Ther Med 2022;23:31)
- 44 year old man with agminated dysplastic nevi and atypical mole syndrome (Arch Dermatol 2001;137:917)
- 49 and 55 year old women with dysplastic nevus and associated sebocyte-like melanocytes in nevi (Am J Dermatopathol 2007;29:566)
Treatment
- Surveillance of skin and pigmented lesion through self skin check and clinical exam; frequency depends on age, sex, family history and activity of the lesion (StatPearls: Dysplastic Nevi [Accessed 14 April 2022])
- Sun protection
- Total body photography and dermoscopy to track the changes or evolution (Cancer Epidemiol Biomarkers Prev 2013;22:528)
- Re-excision: decision to re-excise depends on the clinician's perception and risk assessment
- Severely dysplastic lesions: complete excision due to poor inter-rater concordance in differentiating from melanoma in situ or invasion of superficial dermis (J Am Acad Dermatol 2012;67:1.e1)
- Mildly atypical nevi are considered benign and no additional treatment is necessary
- Lack of consensus on moderate atypia (J Am Acad Dermatol 2017;76:527, JAMA Dermatol 2016;152:1327, JAMA Dermatol 2015;151:212)
Clinical images
Images hosted on other servers:
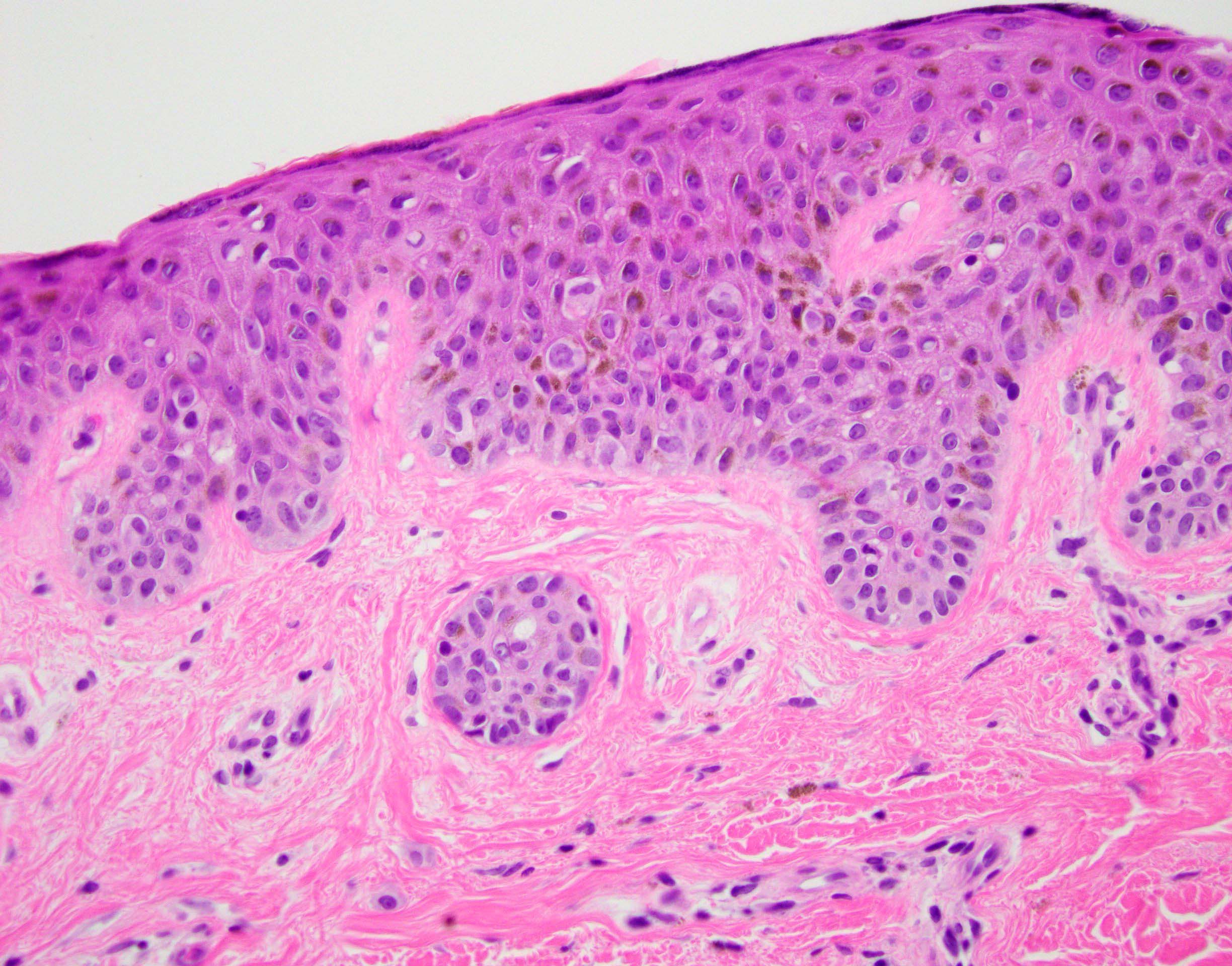
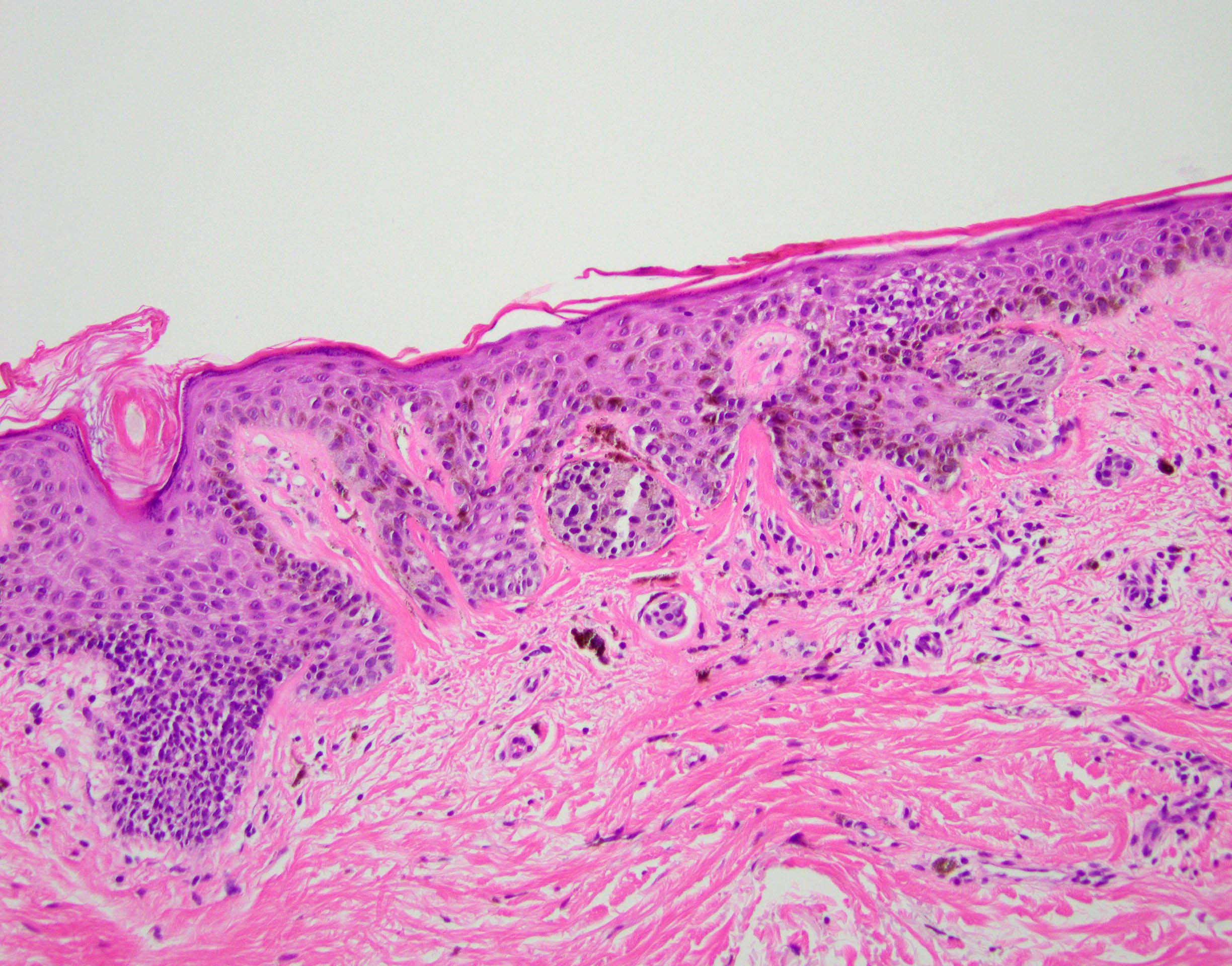
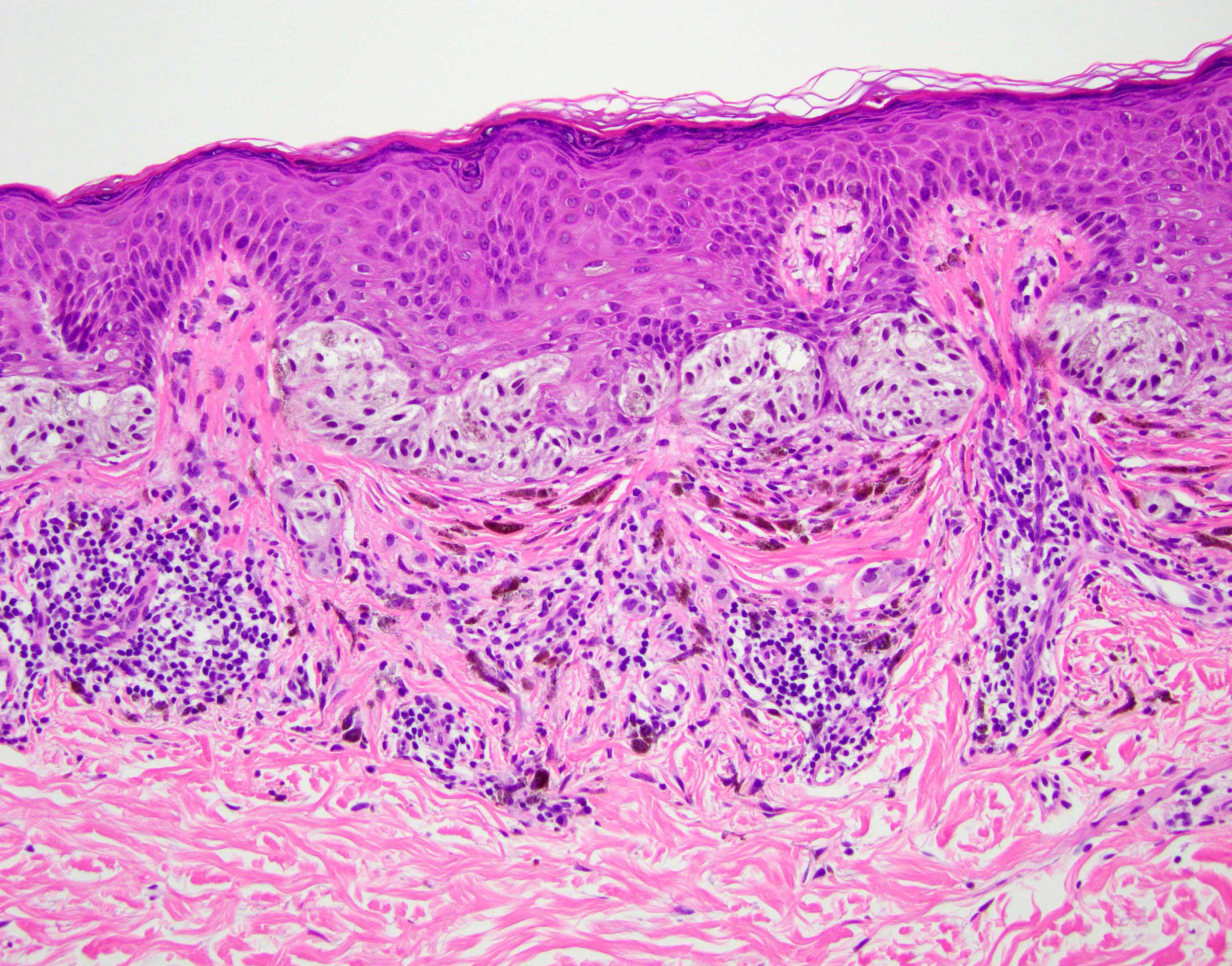
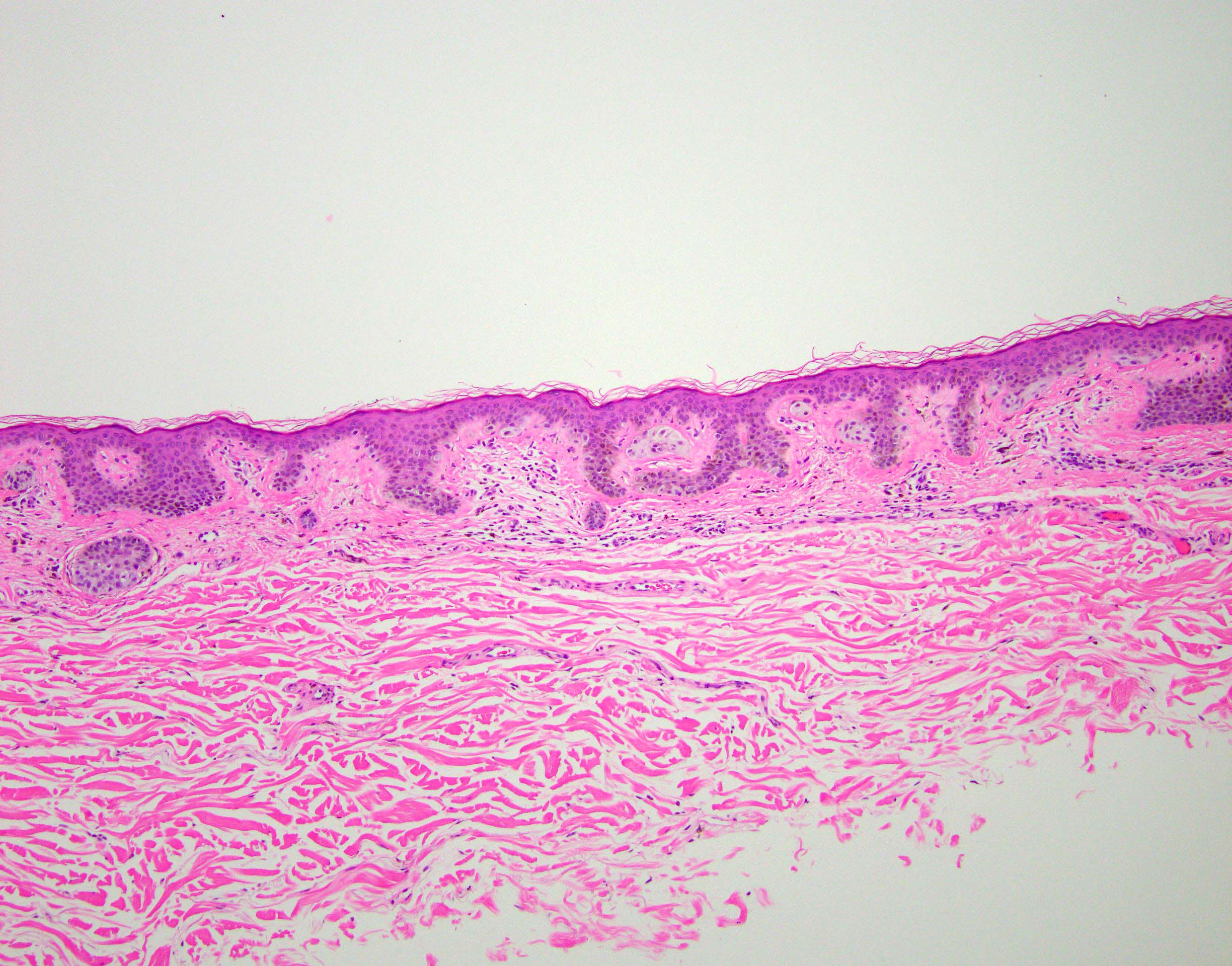
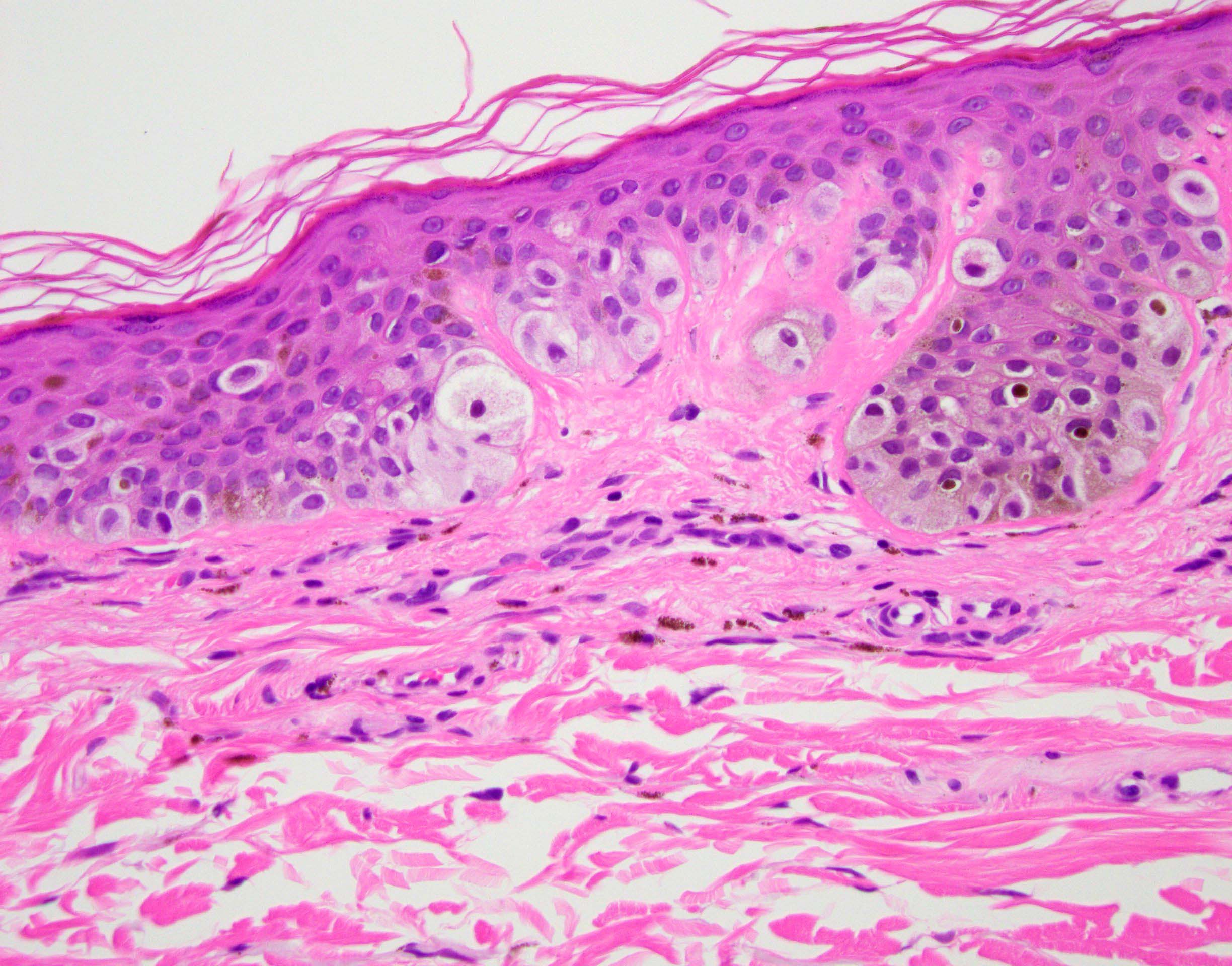
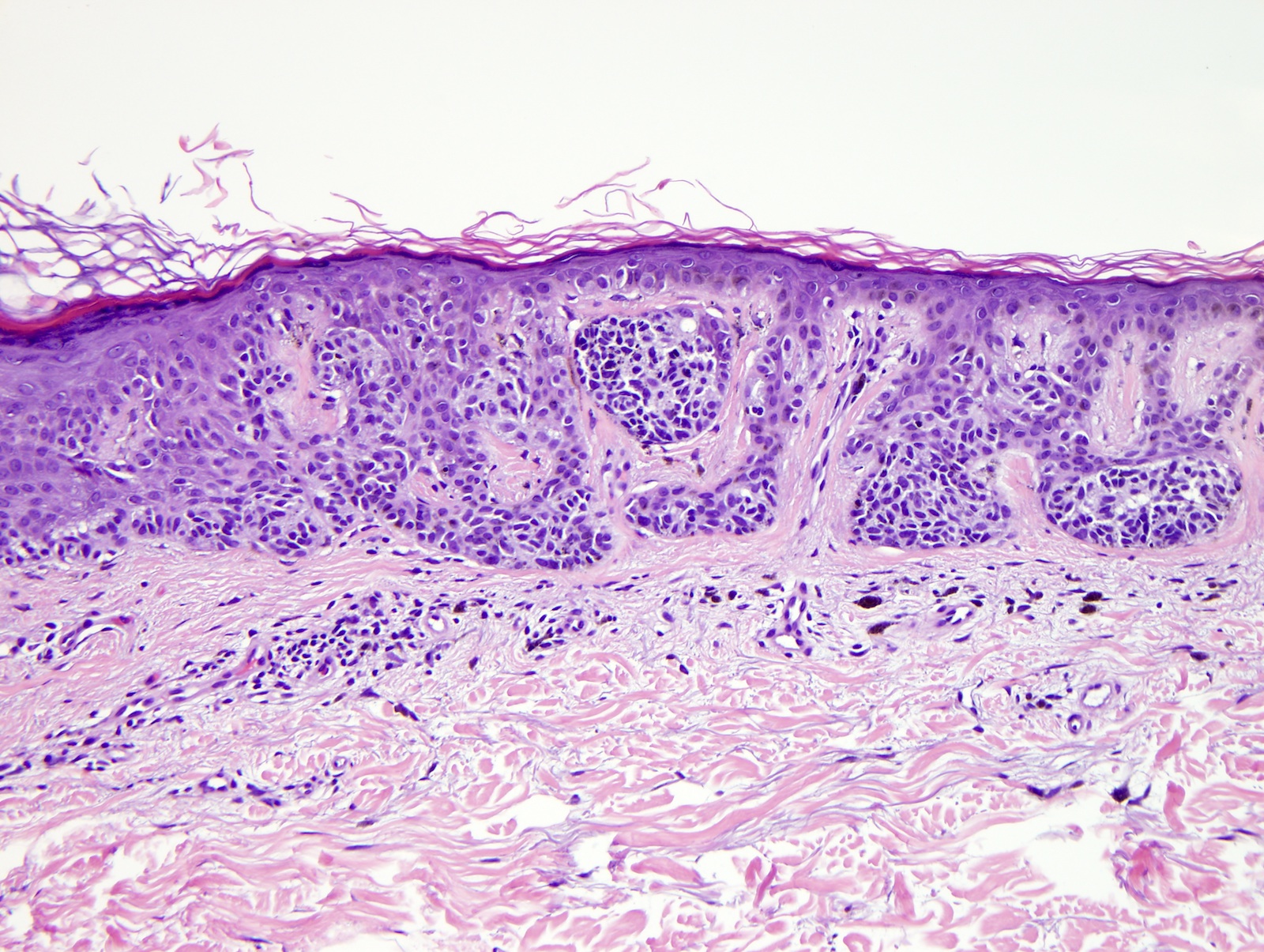
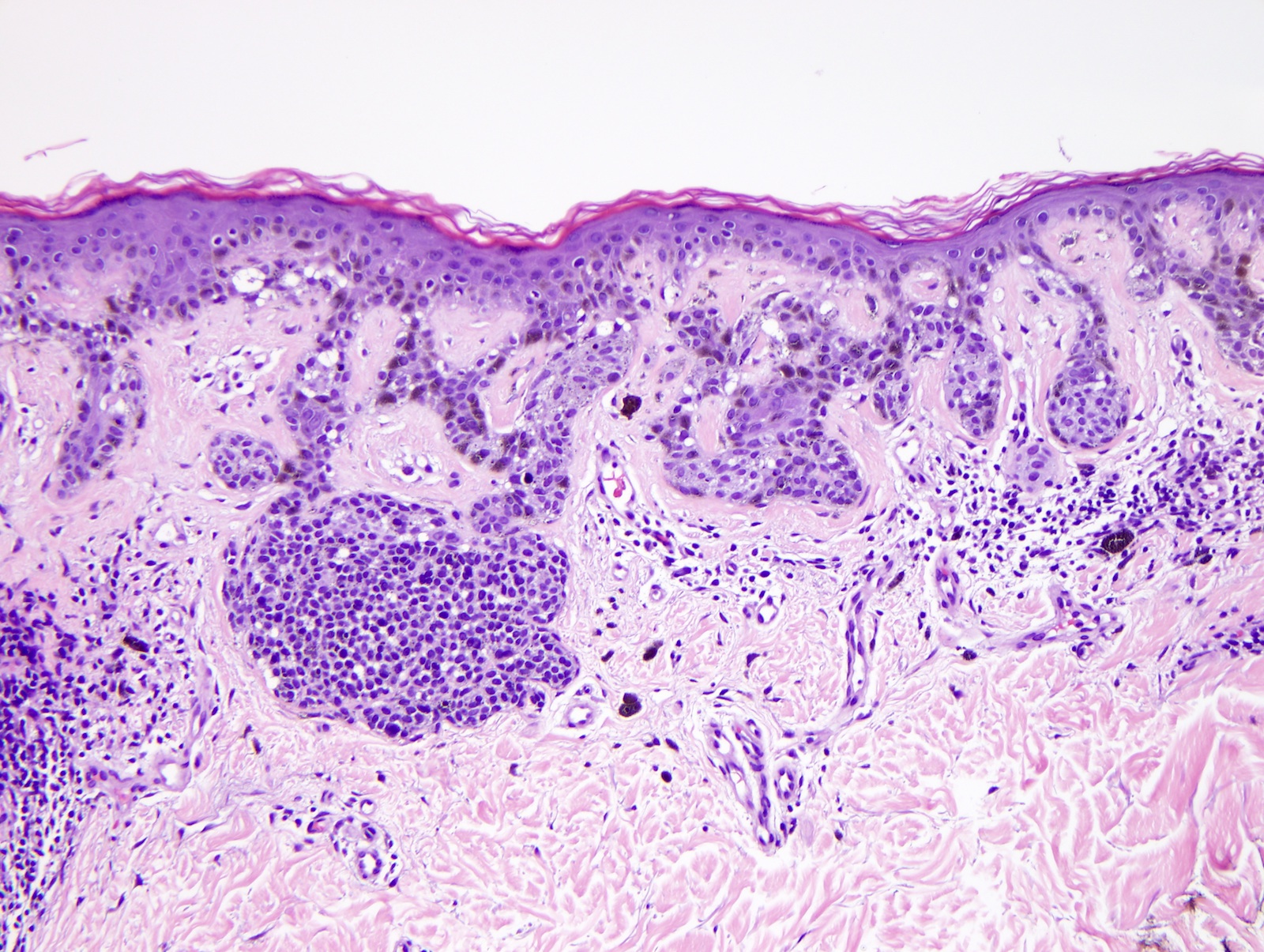
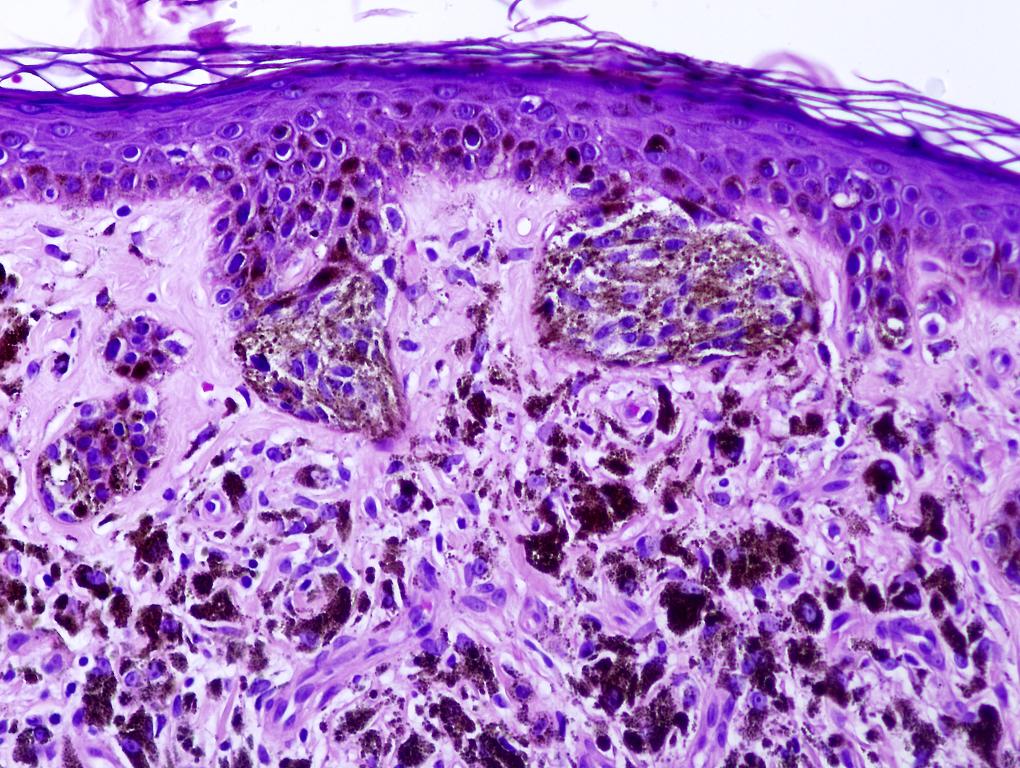
Microscopic (histologic) description
- Familial or sporadic dysplastic nevi show the same features
- Architectural changes:
- Dysplastic nevus should not be diagnosed solely based on architectural atypia; cytologic atypia should also be present
- Shouldering: the epidermal component extends at least 3 rete ridges beyond the lateral margin of the dermal component in compound nevi
- Bridging: connection of the adjacent nests along elongated rete ridges
- Lentiginous hyperplasia
- Irregular nesting: nests show irregular sizes and shapes and are not confined to the tips of rete ridges
- Dysplastic nevus should not be diagnosed solely based on architectural atypia; cytologic atypia should also be present
- Cytological changes:
- Increased nuclear size and hyperchromatic nuclei
- Irregular nuclear membrane
- Prominent nucleoli
- Pleomorphism
- Multivacuolated melanocytes in the dermal component
- Cytologic atypia classified into mild, moderate or severe or simplified to low or high grade
- Stromal changes:
- Lamellar fibroplasia
- Meyerson phenomenon: a subacute spongiotic dermatitis
- Possible epidermal changes: acanthosis, focal parakeratosis, effacement of rete ridges, attenuation of the epidermis; however, the latter 2 features are typically absent in dysplastic nevus and are more characteristic of melanoma (Arch Dermatol Res 2022;314:159)
- Epidermolytic hyperkeratosis may be present but not specific (Am J Dermatopathol 2002;24:23)
- Nevus of special site: flexural, breast, genital and acral nevi can be clinically and histologically atypical and simulate features of a dysplastic nevus or melanoma (Mod Pathol 2006;19:S4)
- The following criteria are not considered to be the typical features of special site nevi and dysplasia should be considered:
- Nevus of genital skin:
- Large and poorly circumscribed
- Extensive shouldering
- Significant epidermal pagetosis
- Necrosis
- Ulceration
- Dermal mitosis
- Nevus of flexural skin:
- Cytologic atypia
- Stromal alterations
- Nevus of acral sites:
- Acral nevi are often more cellular and are arranged in predominantly lentiginous pattern rather than nested patterns
- Dysplastic nevi demonstrate uniform elongation and anastomosis of rete ridges
- Nevus of genital skin:
- The following criteria are not considered to be the typical features of special site nevi and dysplasia should be considered:
Microscopic (histologic) images
Positive stains
- Positive IHC but not useful in separating melanoma and dysplastic nevus:
- SOX10, MART1 / MelanA, MITF
- HMB45: loss of staining with maturation in dysplastic nevus
Molecular / cytogenetics description
- Mutation in BRAF is more common compared to benign nevus (62 - 81%)
- RAS mutation is seen in congenital nevus and rarely in dysplastic nevus
- Mutation / deletion of p16 tumor suppressor gene rarely in dysplastic nevus
- Altered expression of p53
- Increased microsatellite instability in dysplastic nevus; not seen in benign nevus
- Some dysplastic nevi have deletion in p16 encoding chromosomal region 9p21
- Usually diploid
- 24% have high risk mucosal HPV by PCR (Br J Dermatol 2005;152:909)
- Microarray analysis of 4 markers (ING4, Cul1, BRG1 and Bim) may distinguish melanoma from dysplastic nevi (PLoS One 2012;7:e45037)
Videos
Dysplastic nevus by Dr. Jerad Gardner
Compound Clark nevus
Dr. Clay Cockerell's approach to dysplastic nevi
Sample pathology report
- Skin, left arm, shave biopsy:
- Compound nevus with architectural disorder and severe cytologic atypia (see comment)
- Comment: The process extends to lateral margins. A complete excision is recommended.
- Microscopic description: Sections reveal junctional and dermal melanocytes arranged in irregular nests and single units. The lesion is poorly circumscribed and has some focal upward migration of melanocytes. The melanocytes show significant pleomorphism and hyperchromasia. Lamellar fibroplasia and a scattered lymphohistiocytic infiltrate are noted in the dermis.
Differential diagnosis
- Banal nevus:
- Minor architectural abnormalities can be present but cytological atypia is absent
- Lentigo maligna:
- Epidermal atrophy and effacement instead of epidermal hyperplasia
- Dermis shows significant solar elastosis in lentigo maligna
- Melanoma in situ, superficial spreading type:
- Severely dysplastic nevi and early melanoma are difficult to distinguish and the diagnosis may be subjective
- Recurrent nevus:
- Scar of the previous biopsy or excision is present
- Extension of the junctional component beyond the margins of scar may be a more concerning feature
Practice question #1
Which of the following favors a diagnosis of melanoma rather than dysplastic nevus?
- Bridging of the rete ridges
- Focal pagetosis of melanocytes
- Lamellar fibroplasia
- Mitotic activity in dermal melanocytes
Practice answer #1
Practice question #2
Practice answer #2