Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Mohamed KS, Omman RA. Melanotic macule. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumormelanocyticmelanoticmacule.html. Accessed August 4th, 2025.
Definition / general
- Melanotic macule is a benign hyperpigmented lesion predominantly involving the mucosa or acral (volar) skin
- Due to basilar hyperpigmentation of the mucosa or the epidermis
- Typically no increase in the number of melanocytes (mild melanocytic hyperplasia occasionally)
- No relation to sun exposure (except for ink spot lentigo) (Oral Surg Oral Med Oral Pathol 1976;42:196)
Essential features
- Prominent basal layer melanin hyperpigmentation without an increase / minimal increase in the number of melanocytes
- Sporadic or rarely associated with syndromes or diseases
Terminology
- Mucosal melanotic macule; mucosal lentigo
- Based on location:
- Genital melanotic macule; vulvar melanosis; penile melanotic macule
- Oral melanotic macule; melanotic macule of oral mucosa; labial melanotic macule
- Volar melanotic macule (on the palms and soles)
- Ungual melanotic macule (nails)
- Based on etiology:
- Ink spot lentigo with reticulated pattern on the skin due to sun exposure (Arch Dermatol 1992;128:934)
- PUVA (psoralen and UVA therapy) lentigines / melanotic macules on the skin as a side effect of PUVA treatment (J Am Acad Dermatol 1983;9:47)
ICD coding
Epidemiology
- Genital melanotic macule:
- 0.01% of dermatologic patients
- No racial predilection
- Both sexes (F:M = 3.1:1)
- May affect all ages
- Average age of onset (41 years) is younger than that for genital melanoma (J Am Acad Dermatol 2017;76:836)
- Vulvar melanosis:
- 68% of pigmented vulvar lesions in the reproductive age group
- 67% of lesions occur in premenopausal women (J Am Acad Dermatol 1990;22:104, JAMA Dermatol 2020;156:1185)
- Oral melanotic macule:
- 3% of the general population
- Second most common (30.8%) solitary pigmented lesion of the oral mucosa after amalgam tattoo
- 14% with family history; more common in the white population (60.9%); more common in females (74.1%) (Head Neck 2021;43:3775)
- Congenital melanotic macule of the tongue: rare; might be more frequent in dark skinned patients (Pediatr Dermatol 2015;32:109, Ann Dermatol Venereol 2008;135:567)
Sites
- Vulva:
- Mucosal surfaces more often than skin
- Labia minora is the most common vulvar site (Arch Dermatol 2008;144:1030, JAMA Dermatol 2020;156:1185)
- Penis: the glans is the most common location (J Am Acad Dermatol 2000;42:640, J Cosmet Dermatol 2022;21:3308)
- Oral mucosa: the vermilion border of the lower lip is the most common location, followed by gingiva, then buccal mucosa and palate (Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;112:e21)
- Volar: found on palms, fingers, soles or toes in dark skinned individuals (Am J Dermatopathol 2008;30:612)
- Congenital melanotic macule of the tongue:
- Rare
- Solitary or multiple dark macules present since birth with proportional growth
- On the dorsum of the tongue
- No family history or associated systemic conditions (Pediatr Dermatol 2015;32:109)
Pathophysiology
- Unclear
- Hypermelaninosis (increase in melanin pigmentation) without or occasionally slight increase in melanocyte number
- May be due to increased melanocytic activity (Oral Dis 1999;5:80)
Etiology
- Sporadic
- Post sun exposure
- Ink spot lentigo: rete ridges appear less blunted and more tortuous (eMedicine: Lentigo Workup [Accessed 27 November 2022])
- Postradiotherapy
- PUVA: increased melanocytes, atypia, elongated rete ridges with increased pigmentation in basal cell region (eMedicine: Lentigo Workup [Accessed 27 November 2022])
- Syndromic
- Melanotic macules and multiple lentigines (systemic conditions)
- Addison disease
- Endocrinal disorder, most common cause is autoimmune and tuberculosis (Contemp Clin Dent 2012;3:484)
- Generalized hyperpigmentation, hyperpigmentation of mucosa and skin, hyponatremia, hypokalemia, GI upset, anorexia, nausea, vomiting, diarrhea (J Assoc Physicians India 2001;49:523, The Open Dermatology Journal 2009;3:3, J Clin Endocrinol Metab 2001;86:2909)
- Peutz-Jeghers syndrome
- Inherited condition
- Hamartomatous polyps in GI tract, increased risk of cancer and mucocutaneous hyperpigmentation (Cancer.Net: Peutz-Jeghers Syndrome [Accessed 20 November 2022])
- Carney complex
- Also known as NAME (nevi, atrial myxomas, ephelides) and LAMB (lentigines, atrial myxoma, blue nevi)
- Most common skin lesions are lentigines, epithelioid type blue nevi, combined nevi, café au lait macules and depigmented lesions
- Also associated with myxomas, thyroid cancer, acromegaly, psammomatous melanotic schwannoma, etc. (GeneReviews: Carney Complex [Accessed 28 November 2022])
- LEOPARD syndrome or Noonan syndrome with multiple lentigines
- Lentigines (flat brown macules), electrocardiographic abnormalities, ocular hypertelorism, pulmonary stenosis, abnormalities of genitalia, retardation of growth, deafness
- Autosomal dominant disorder, caused by missense mutation in PTPN11 gene (eMedicine: LEOPARD Syndrome [Accessed 20 November 2022])
- Laugier-Hunziker syndrome (LHS)
- Rare benign acquired condition occurs frequently among middle aged women
- Manifests as single or multiple lenticular hyperpigmented macules (2 - 5 mm) and longitudinal melanonychia (50% of patients)
- Most common sites of macules are labial (particularly the lower lip), oral (especially buccal mucosa), acral and genital (World J Clin Cases 2018;6:322)
- Dermoscopy of labial lesions in LHS: parallel furrow pattern with multiple brown dots; multiple brown or blue-gray granular patterns (Arch Dermatol 2007;143:631, Dermatol Surg 2010;36:152)
- Addison disease
- Melanotic macules and multiple lentigines (systemic conditions)
Clinical features
- Asymptomatic
- Genital:
- Multifocal (> 50%)
- < 5 cm (> 50% are < 1.5 cm)
- Homogenous or irregular pigmentation (brown to black)
- One study (small sample size) showed 15% associated with a personal history of melanoma (Arch Dermatol 2008;144:1030, J Am Acad Dermatol 2017;76:836)
- Oral: solitary; well circumscribed; 6 - 10 mm; brown to black (Head Neck 2021;43:3775)
Diagnosis
- Clinical examination:
- Genital melanosis: a thorough total body skin examination to rule out occult melanoma (J Am Acad Dermatol 2017;76:836)
- Diffuse or multiple mucocutaneous pigmented macules: careful clinical examination and clinically relevant investigations to rule out associated syndromes
- Dermoscopy:
- Labial lesions in LHS: parallel furrow pattern with multiple brown dots; multiple brown or blue-gray granular patterns (Arch Dermatol 2007;143:631, Dermatol Surg 2010;36:152)
- Vulvar melanosis: ring-like, structureless, globular-like, parallel, cobblestone-like and reticular-like or combined patterns (Arch Dermatol 2008;144:1030)
- Biopsy:
- Oral melanotic macule: histological confirmation is necessary as any oral pigmented lesion is considered melanoma until proven otherwise
Laboratory
- Laboratory tests typically not required; in patients with features suggestive of syndromic / systemic disease association, pertinent lab tests should be performed
Prognostic factors
- Excellent with no malignant transformation
Case reports
- Hispanic infant boy with a congenital hyperpigmented macule of the tongue (Cureus 2020;12:e11475)
- 28 year old woman with lingual melanotic macule (An Bras Dermatol 2018;93:310)
- 64 year old woman with a pigmented lesion of the marginal gingiva (Med Buccale Chir Buccale 2017;23:156)
Treatment
- No treatment is required
Clinical images
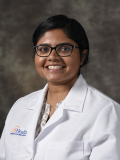
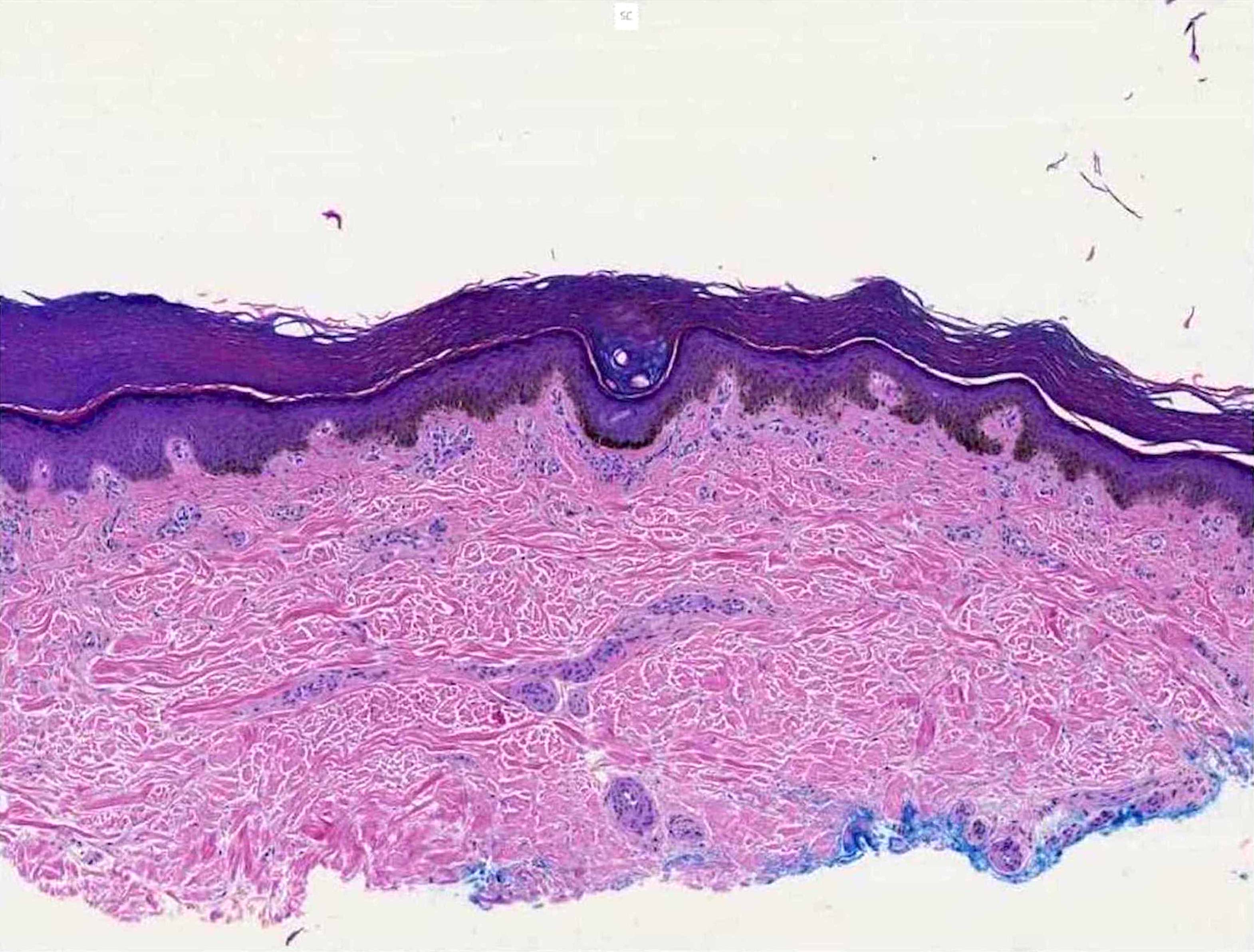
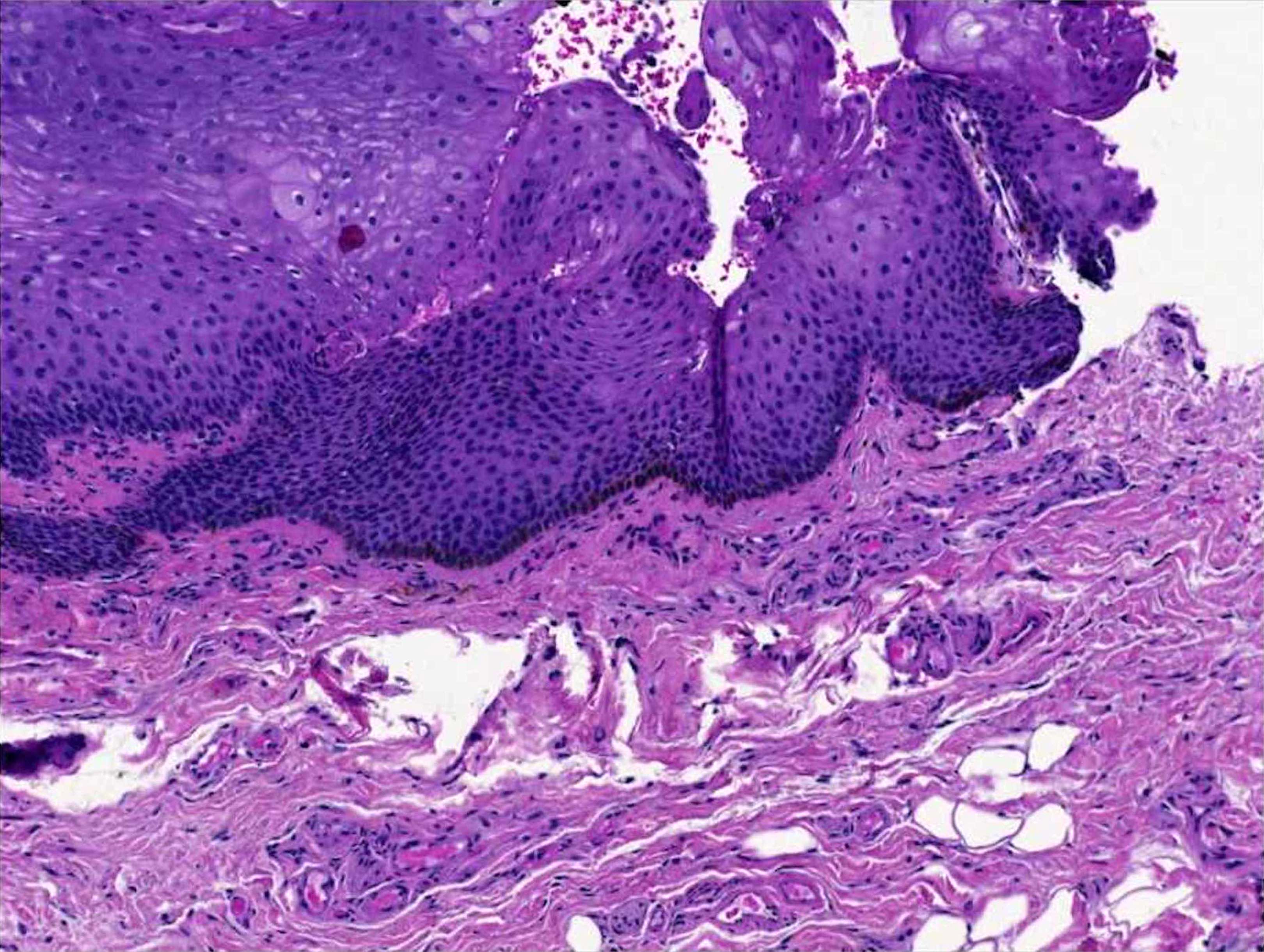
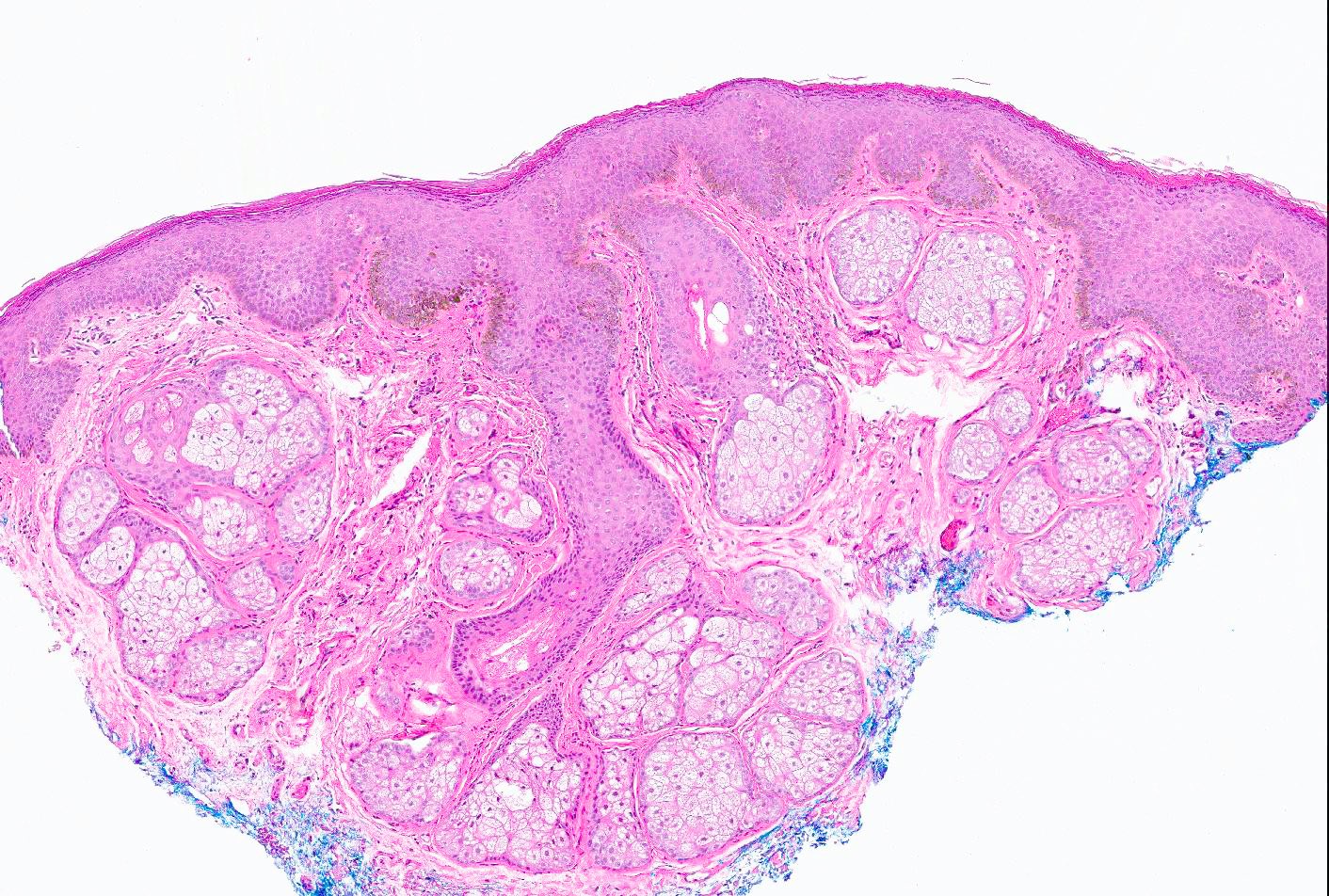
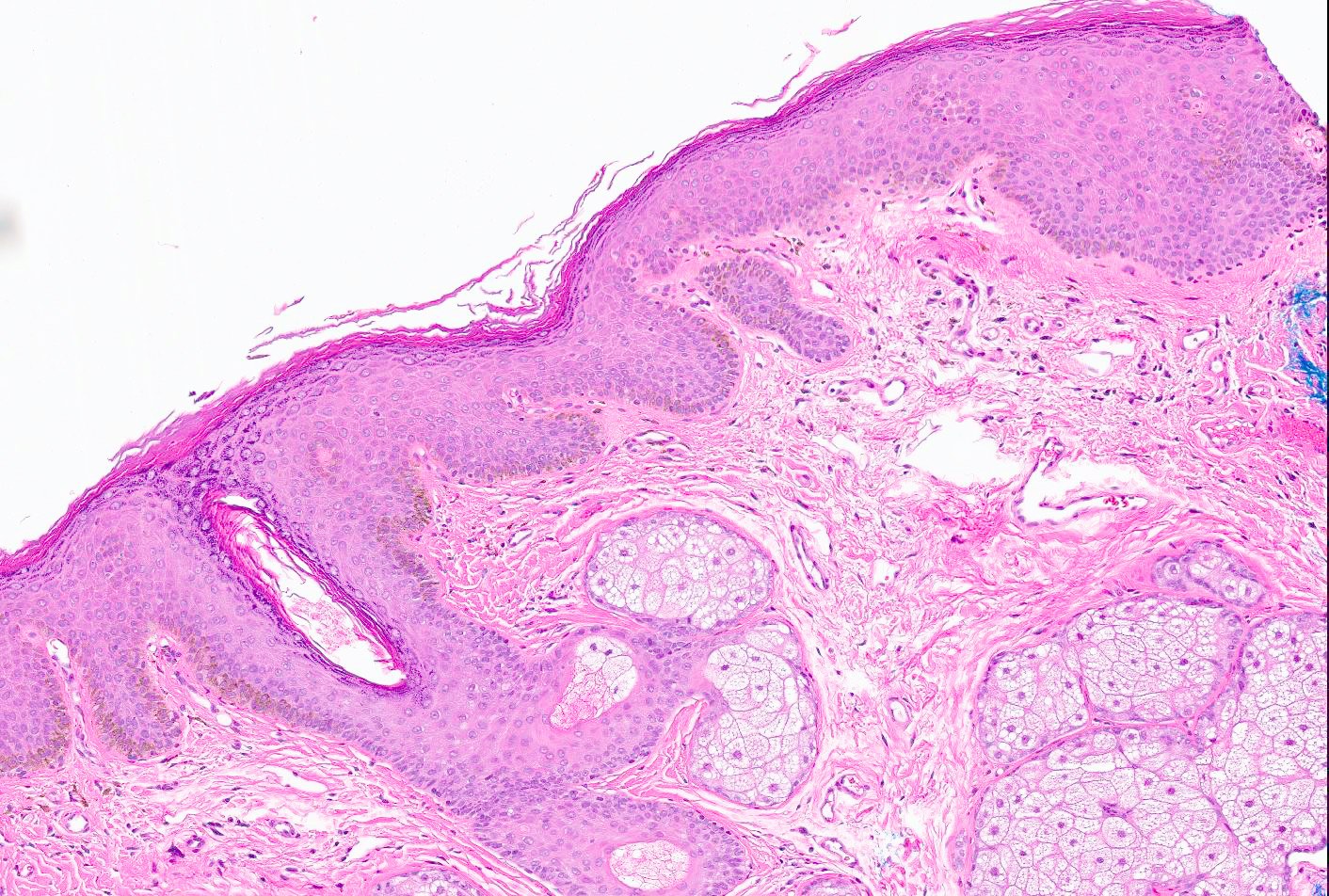
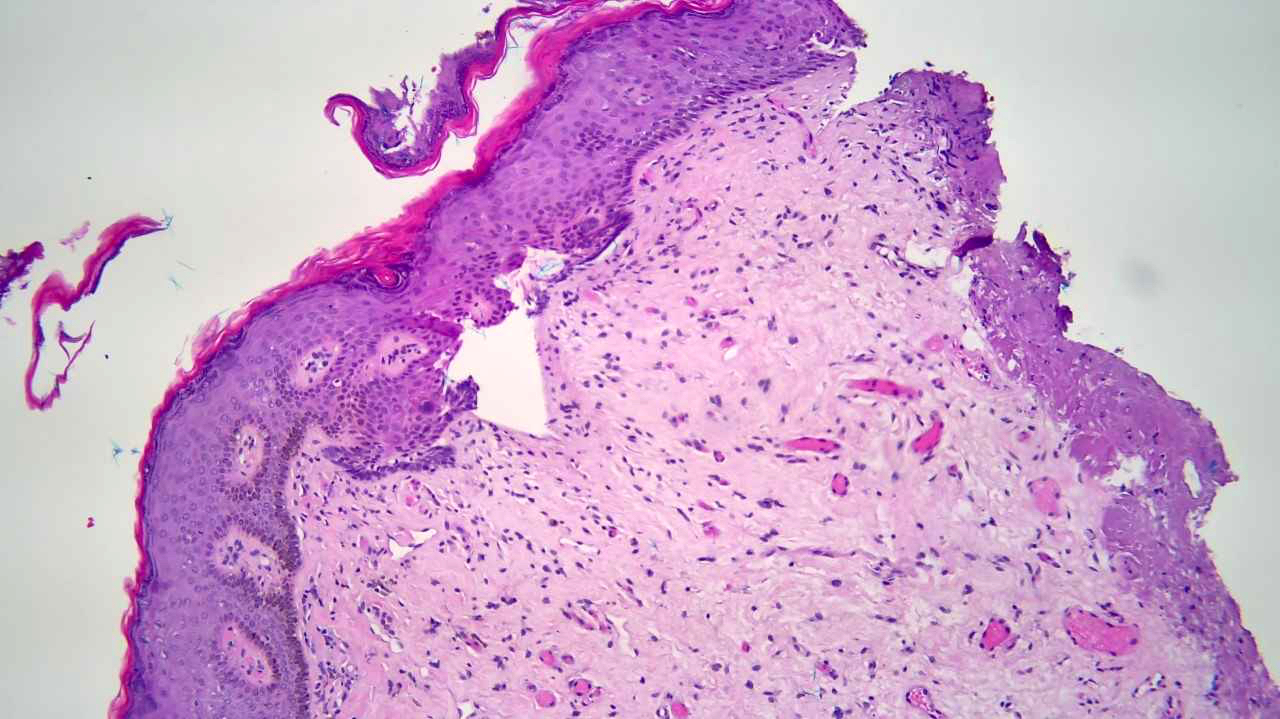
Microscopic (histologic) description
- Increased basal keratinocyte pigmentation
- Mostly restricted to tips of rete ridges
- Dendrites are short and delicate
- Coarse dendrites reaching to the upper epidermis are worrisome for early melanoma in situ
- Melanin pigment incontinence and melanophages in the lamina propria or upper dermis
- No increase in the melanocyte number (occasionally a very mild increase in melanocytes at the dermoepidermal junction may occur but typically have no atypia and lack confluence)
- Rare cells above the DEJ can be seen but only with immunohistochemistry
- More epithelioid and somewhat atypical melanocytes may be seen in vulval and penile melanotic macules (Massi: Histological Diagnosis of Nevi and Melanoma, 2nd Edition, 2014)
- Associated frequent acanthosis, hyperkeratosis, hyperparakeratosis, spongiosis and elongated rete ridges (in nonoral lesions) (World J Clin Cases 2018;6:322)
Microscopic (histologic) images
Positive stains
- SOX10 / S100 / HMB45 / MelanA / MART1 show normal / minimally increased melanocytic density
- PRAME: false positive in rare subungal melanotic macules (Am J Dermatopathol 2022;44:499)
Videos
Labial melanotic macule
(brown spot on lip)
Sample pathology report
- Lip, biopsy:
- Melanotic macule (see comment)
- Comment: Sections show increased basilar pigmentation at the tips of rete ridges. Mild acanthosis and dermal melanophages are present. No significant increase in melanocytes is noted.
Differential diagnosis
- Melanoma in situ:
- Increase in irregularly scattered melanocytes restricted to the epidermis / mucosa
- Confluence of melanocytes or presence of pagetoid spread
- Melanocytes are atypical, epitheliod / spindled, pleomorphic, with eosinophilic or purple nucleoli (Massi: Histological Diagnosis of Nevi and Melanoma, 2nd Edition, 2014)
- Coarse melanin granules may be seen
- Heavy lymphoplasmacytic infiltrate
- Melanoma:
- Prominent atypical lentiginous melanocytes and often nested pattern of melanocytic hyperplasia with the atypical melanocytes invading the dermis
- Dermal mitosis present
- Pigment is not only restricted to basal layer but haphazardly distributed
- Acquired mucosal nevus:
- Has junctional, compound and intramucosal nevi types (BMJ Case Rep 2013;2013:bcr2013010191)
- Presence of nested melanocytes without atypia
- Lentiginous nevus:
- Also known as jentigo
- Rare melanocytic nests and melanocytic hyperplasia towards the edges
- Lentigo simplex:
- Increased melanocytes at the basal layer and epithelial hyperplasia
- Pigmentation of the rete ridges
- Solar lentigo:
- Solar elastosis and bulb-like elongation of the rete ridges
- Mild increase in melanocytes at the tips of rete ridges, giving dirty sock appearance
- Ephelis:
- No increase in melanocytes, diagnosis is usually clinical, appears during summer and fades in winter
- Increased pigmentation (darkness of pigment increases with sun exposure)
- Oral melanoacanthoma:
- Pigmented, spongiosis and interspersed dendritic melanocytes (J Med Case Rep 2009;3:11)
- Lack of melanocytic proliferation at the dermoepidermal junction but proliferation of dendritic melanocytes scattered throughout spinous layer present
- Amalgam tattoo:
- Due to dental silver fillings that may be implanted into the mucosa during dental procedure (PLoS One 2018;13:e0207026)
- Dark brown to black or fine golden to dark brown granules deposited in the dermis
- Smoker's melanosis:
- Benign pigmentation of the oral mucosa, on anterior mandibular gingiva and interdental papillae
- Adult onset and lesion continues to darken (J Periodontol 1991;62:524)
- Racial pigmentation / physiologic pigmentation:
- Macular pigmented areas of varying shapes and sizes
- Shows increased melanin within the basal epithelial layer and melanin incontinence within the superficial lamina propria (Dermatol Ther 2010;23:220)
- Drug induced pigmentation:
- Antineoplastic (imatinib); antimalarials (the second most common); antibiotic (minocycline); antifungal (ketoconazole); antiretroviral; antimycobacterial (clofazimine) (Patient Prefer Adherence 2020;14:1961)
- Patterns of histologic abnormalities are drug specific
- Features such as hyperpigmentation of the basal cell layer, pigment incontinence within the dermis and accumulation of pigment laden macrophages around blood vessels and eccrine glands often seen (eMedicine: Drug-Induced Pigmentation Workup [Accessed 20 November 2022])
- Antineoplastic (imatinib); antimalarials (the second most common); antibiotic (minocycline); antifungal (ketoconazole); antiretroviral; antimycobacterial (clofazimine) (Patient Prefer Adherence 2020;14:1961)
- Postinflammatory hyperpigmentation:
- Acquired excess of pigment in various conditions (infection, drugs, inflammatory diseases and others)
- Epidermal postinflammatory hyperpigmentation: increased melanin pigment in the basal cell layer of the epidermis
- Dermal postinflammatory hyperpigmentation: melanin pigment in the upper dermis, with pigment incontinence
- Increased numbers of melanophages in the papillary dermis (eMedicine: Postinflammatory Hyperpigmentation Workup [Accessed 20 November 2022])
Additional references
Practice question #1
A biopsy of the vulvar pigmented macule of a 42 year old patient shows basilar hyperpigmentation with no nest formation. SOX10 immunostain was performed and shows no increase in melanocytes. What is the best classification for this lesion?
- Invasive melanoma
- Melanoma in situ
- Melanotic macule
- Mucosal nevus
Practice answer #1
Practice question #2
Which of the following syndromes has associated melanotic macules?
- Brooke-Speigler syndrome
- Laugier-Hunziker syndrome
- Netherton syndrome
- Nevoid basal cell carcinoma syndrome
Practice answer #2