Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Swaney M, Patel KS. Ischemia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/smallbowelischemia.html. Accessed October 4th, 2025.
Definition / general
- Decreased blood flow or lack of oxygen to the bowel that causes necrosis or damage
Essential features
- Numerous arterial or venous causes of small bowel ischemia
- Early histologic findings: mucosal surface damage with hemorrhagic necrosis and lamina propria hyalinization
- Late histologic findings: necrosis, inflammation, loss of base crypts, crypt distortion
- Important to examine the vessels for evidence of thromboembolic disease or vasculitis
- Reference: Greenson: Diagnostic Pathology - Gastrointestinal, 3rd Edition, 2019
Terminology
- Necrosis / necrotic bowel
- Mesenteric ischemia
ICD coding
Epidemiology
- Mean age of 70 years old; less common before age 60
- M:F = 1:1
- Rare condition but high mortality rates (24 - 94%) (StatPearls: Bowel Ischemia [Accessed 9 August 2023])
- Decrease in mesenteric arterial blood flow is the most common cause
Sites
- Small bowel (duodenum, jejunum, ileum)
- Often has transmural infarction due to occlusion of superior mesenteric artery
Pathophysiology
- Decrease or lack of blood flow deprives the tissue of oxygen
- Lack of oxygen leads to cell death and necrosis
- Ischemia injury causes the release of toxic byproducts, production of free radicals and activation of neutrophils (StatPearls: Bowel Ischemia [Accessed 9 August 2023])
- Thrombosis can lead to full thickness infarction
Etiology
- Artery occlusion: thrombosis, embolism, atherosclerosis, vasculitis, compression (adhesions, volvulus, tumor), radiation
- Venous occlusion: thrombosis (oral contraceptives, hypercoagulable states), compression (adhesions, volvulus, tumor)
- Low flow states: shock (blood loss, postsurgery), dehydration, heart failure, vasospasm (medications, drugs like cocaine)
- Intestinal obstruction: masses (neoplasms, diverticular disease), ileus, motility disorders
- Infection: enterohemorrhagic E. coli (E. coli O157:H7), cytomegalovirus
- Drugs / medications: nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, chemotherapy, digoxin, vasoconstrictors (cocaine, amphetamines, decongestants, ergot alkaloids)
- Reference: Am J Surg Pathol 1998;22:773
Clinical features
- Abdominal pain (usually sudden onset), nausea / vomiting, hematochezia and fever
Diagnosis
- History and physical is most important
- Some patients have leukocytosis
- Computed tomography (CT) of abdomen with or without contrast (Curr Gastroenterol Rep 2019;21:27)
- Findings of underlying cause: CT angiography of abdomen, magnetic resonance angiography (MRA) of abdomen, infectious causes
- Endoscopic findings: edema and erythema, geographic ulcers, strictures (Greenson: Diagnostic Pathology - Gastrointestinal, 3rd Edition, 2019)
Laboratory
- Some patients present with leukocytosis or other complete blood count (CBC) abnormalities (if bleeding)
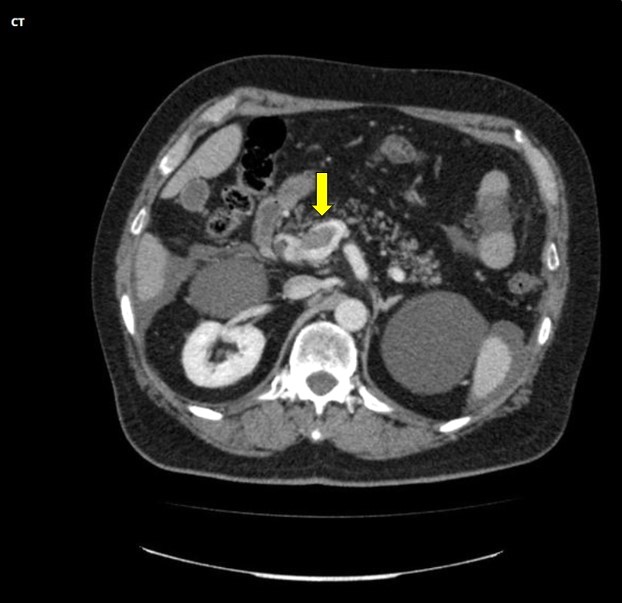
Radiology description
- CT of abdomen with and without contrast shows evidence of intestinal ischemia by bowel wall thickening, dilatation of bowel lumen, mesenteric fat stranding and ascites, bowel wall attenuation and possibly pneumatosis
Prognostic factors
- Depends on the underlying cause
- 90% mortality for mesenteric artery thrombosis, 10% mortality for nonocclusive disease (Turk J Surg 2017;33:104)
Case reports
- 33 year old man presented with acute abdominal pain following amphetamine use (Radiol Case Rep 2020;15:2183)
- 34 year old man with history of right hepatectomy presented with diffuse abdominal pain, bloating and nausea (World J Gastrointest Pathophysiol 2019;10:29)
- 59 year old woman with history of peritonectomy (Int J Surg Case Rep 2020;76:247)
Treatment
- Supportive treatment, hemodynamic stability and oxygen
- Surgical treatment if necessary
Gross description
- Infarcted bowel mucosa and wall described as dusky, which is a dark red-brown color
- Bowel wall can be thin and friable, may contain bloody contents
- Geographic (sharp demarcation) between infarcted bowel and normal bowel
- Ulcers and pseudomembranes may be present (Greenson: Diagnostic Pathology - Gastrointestinal, 3rd Edition, 2019)
Gross images
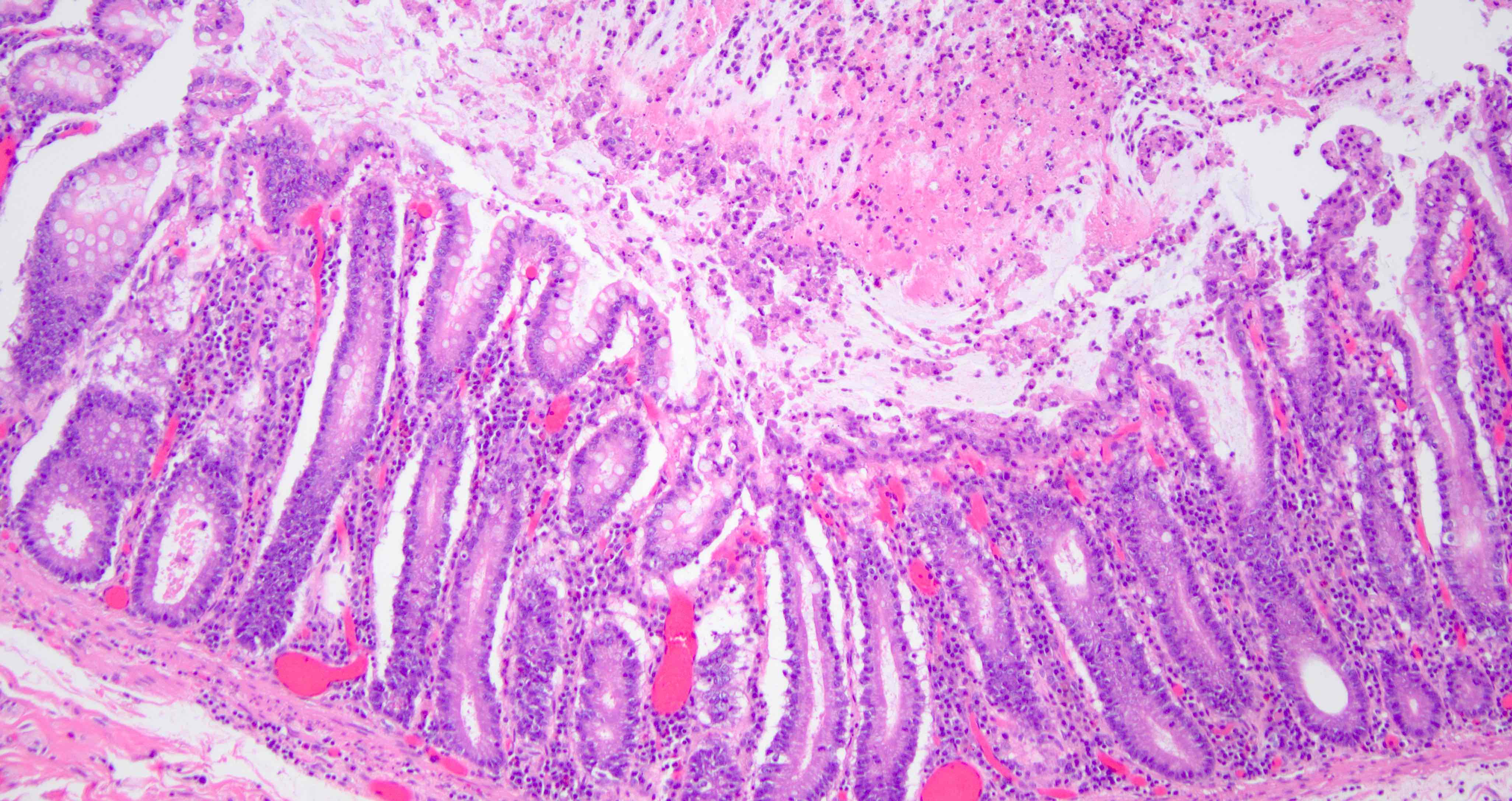
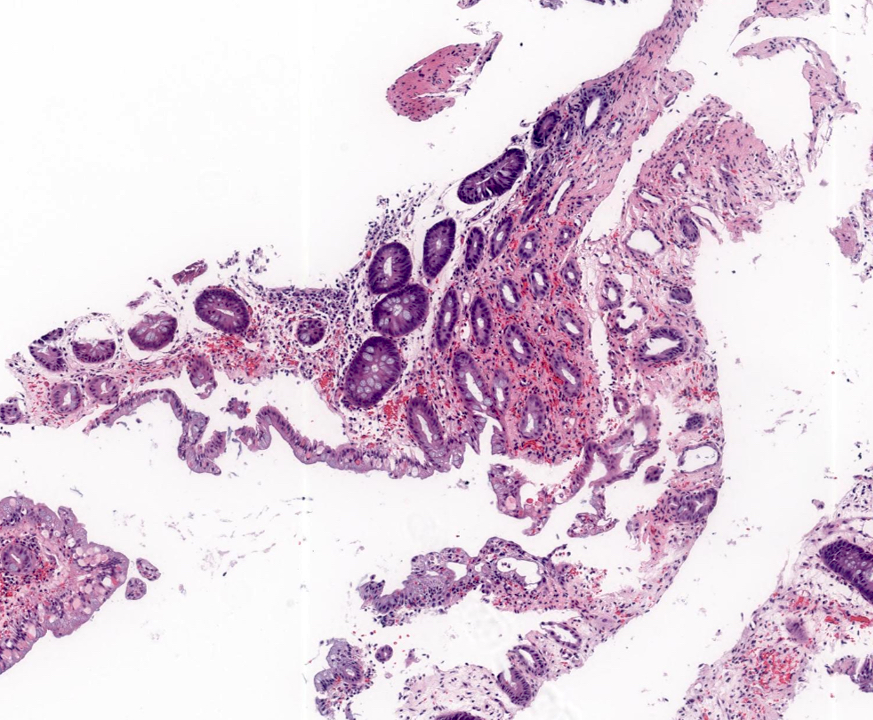
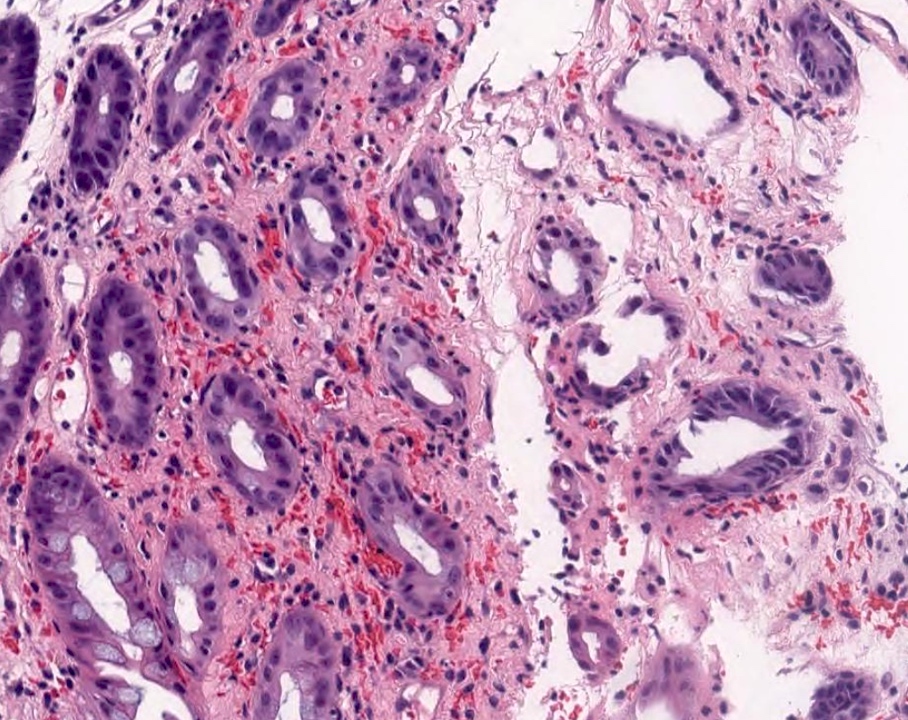
Microscopic (histologic) description
- Early histologic findings
- Mucosal surface with hemorrhagic necrosis and loss of surface crypts
- Base of crypts can remain intact but are atrophic and withered with marked regenerative atypia
- Lamina propria hyalinization with smudgy appearance
- Edematous submucosa, edema and subsequent splaying of muscularis mucosae
- Little inflammation
- Pseudomembranes may be present
- Later histologic findings
- Inflammation progresses with crypt distortion
- Hemosiderin laden macrophages
- Can have giant cells in areas of ulceration
- Vessels
- Evidence of thrombi, emboli or vasculitis; most commonly in resection specimens
- Do not overinterpret thrombi or inflammation in ulcer bed
- Reference: Greenson: Diagnostic Pathology - Gastrointestinal, 3rd Edition, 2019
Microscopic (histologic) images
Sample pathology report
- Small bowel, biopsy:
- Enteric mucosa with changes consistent with ischemic type mucosal injury (see comment)
- Comment: Possible etiologies for this ischemic type mucosal injury include true ischemic colitis, infection (such as E. coli 0157:H7) and a drug reaction (including oral contraceptives, NSAIDs, digoxin and ergotamine derivatives). Clinical and endoscopic correlation is recommended.
- Small bowel, resection:
- Ischemic enteritis with transmural necrosis / hemorrhage / perforation
- Resection margins are viable
Differential diagnosis
- Enterohemorrhagic E. coli infection:
- History of eating undercooked meat
- Fibrin thrombi are characteristic but not specific for E. coli
- Chronic inflammatory bowel disease:
- Chronic ischemia with stricture formation may look identical to quiescent Crohn's disease
- Presence of hemosiderin laden macrophages favors ischemia
- Presence of fistulae and granulomas favors Crohn's disease
- Nonsteroidal anti-inflammatory drug damage:
- Can be histologically similar to ischemia
- Clinical history is important
- Dysplasia:
- Should appear top heavy; ischemia is bottom heavy
- Typically has more branched and complex architecture
- Regenerative crypts in ischemia are usually small and round
- Behçet disease:
- Scattered, punched out ulcers in the gastrointestinal (GI) tract, no intervening normal mucosa
- Patients have urogenital and ocular manifestations, which are required for diagnosis
- Clostridium difficile colitis:
- Usually, a more diffuse process than ischemia (geographic)
- Hyalinized lamina propria or withered crypts are not usually seen with C. difficile
- Reference: Greenson: Diagnostic Pathology - Gastrointestinal, 3rd Edition, 2019, Am J Surg Pathol 1998;22:773
Practice question #1
Practice answer #1
A. Atrophic crypts with lamina propria hyalinization.
Features of ischemic colitis vary depending on the extent and timing of the ischemic event. This biopsy shows features of withered and atrophic crypts and lamina propria hyalinization in the absence of acute inflammation or other significant architectural distortion. The withered crypts are a feature of ischemic pattern colitis, the etiology of which includes both ischemia and infection. Answer B is incorrect because crypt abscesses and granulomatous inflammation are typically seen in inflammatory bowel disease and are not features of ischemic colitis. Answer C is incorrect because mast cells and eosinophils are not typically seen in small bowel ischemia. These features can be seen in eosinophilic gastroenteritis, parasitic infections, mastocytosis or Langerhans histiocytosis. Answer D is incorrect because pseudomembrane formation is typically seen with C. difficile colitis.
Comment Here
Reference: Ischemia
Comment Here
Reference: Ischemia
Practice question #2
Which of the following are clinicopathologic features that distinguish ischemic enteritis from other causes of enteritis?
- Branched and complex architecture in crypts
- Evidence of thrombi, emboli or vasculitis
- History of eating undercooked meat
- Scattered ulcers in the GI tract, ocular, oral and genital manifestations
Practice answer #2
B. Evidence of thrombi, emboli or vasculitis, most commonly in resection specimens, can be seen in ischemic small bowel. Answer C is incorrect because E. coli infection is associated with history of eating undercooked meat. Answer A is incorrect because small bowel dysplasia is associated with branched and complex architecture in crypts. Answer D is incorrect because scattered ulcers in the GI tract, ocular, oral and genital manifestations are commonly associated with Behçet disease.
Comment Here
Reference: Ischemia
Comment Here
Reference: Ischemia