Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Potterveld S, Clay MR. Myxoid liposarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuemyxoidliposarcoma.html. Accessed September 18th, 2025.
Definition / general
- Malignant tumor composed of primitive nonlipogenic mesenchymal cells, signet ring lipoblasts and prominent myxoid stroma with a highly characteristic branching vascular pattern
Essential features
- Prominent myxoid stroma with branching vasculature (so called chicken wire vasculature)
- Majority of the tumor can be nonlipogenic with only scattered lipoblasts that often have a characteristic signet ring morphology
- Recurrent molecular alteration with either t(12;16)(q13;p11.2) FUS::DDIT3 or very rarely (~2%) t(12;22)(q13;q12) EWSR1::DDIT3 rearrangements
- Includes a spectrum of disease including high grade lesions, which were formerly regarded as round cell liposarcoma (see Terminology)
- Has an unusual propensity to present with a first metastasis to another soft tissue or bony site (such as from one leg to the contralateral leg or to the retroperitoneum or spine)
Terminology
- Although myxoid liposarcoma and round cell liposarcoma were initially described separately, both tumors have identical molecular alterations and clear evidence of cases with transition between the 2 morphologic patterns are easily found
- Both tumors are now classified as myxoid liposarcoma with a secondary designation of high or low grade
- Percent of round cell component needed for this distinction is debated in the literature with most pathologists using either > 25% or > 5% indicating a high grade lesion
- WHO currently lists 5%
- Cases with borderline round cell component (< 5%) are regarded as having areas of transition, a designation of unclear diagnostic significance
ICD coding
- ICD-O: 8852/3 - myxoid liposarcoma
- ICD-11: 2B59.Y & XH3EL0 - liposarcoma, other specified primary site & myxoid liposarcoma
Epidemiology
- Peaks in the fourth and fifth decades and represents ~5% of adult sarcomas (Int J Surg Oncol 2018;2018:8928706)
- M = F
- May occur in children or very rarely in the elderly
Sites
- Usually in the extremities, proximal thigh is quite common
- Primary retroperitoneal involvement is rare, although metastasis to the retroperitoneal soft tissue is not uncommon
- Propensity to present with multifocal disease, seemingly from hematogenous spread that has spared the lungs (J Surg Oncol 2002;80:89)
- Primary subcutaneous tumors have been reported (J Cutan Pathol 2014;41:907)
Diagnosis
- Core needle biopsy is minimally invasive and can provide sufficient tissue sampling for definitive diagnosis, although it may not allow for accurate tumor grading due to sampling bias
- Surgical resection is the gold standard procedure for ensuring accurate diagnosis and prognostication
Radiology description
- Vague foci of fat in a lacy or linear pattern on MRI (Radiographics 2000;20:1007)
- May appear cystic on nonenhanced MRI, although they enhance like other solid masses, often as T1 hyperintense fatty septa (Radiographics 2000;20:1007, Radiol Case Rep 2017;12:811)
- Other features include encapsulation, lobulated fat and diffuse, globular or nodular intense enhancement (Radiol Case Rep 2017;12:811)
Radiology images
Prognostic factors
- Predilection for metastasis, especially when there is a significant round cell component
- Metastases can occur decades later, necessitating continued long term follow up (World J Surg Oncol 2008;6:62)
- Pure low grade tumors have less aggressive behavior but still share a propensity for recurrence and can metastasize in 5 - 10% of cases
- Unfavorable outcome has been associated with TP53 and CDKN2A gene mutations, although this seems rare (Tumori 1998;84:571)
- Some evidence suggests that high grade components can be identified via MRI and that metastases can be identified very early with imaging studies (Acta Radiol 2014;55:952, Skeletal Radiol 2018;47:369)
Case reports
- 35 and 44 year old men with multicentric tumors (World J Surg Oncol 2007;5:139)
- 51 year old man with thyroidal metastases from a right thigh myxoid liposarcoma (J Laryngol Otol 2006;120:511)
- 66 year old woman with solitary breast metastasis from a right thigh myxoid liposarcoma (BMC Cancer 2014;14:482)
- 71 year old man with supraclavicular fossa mass (Chest 2000;117:1518)
- Review of patients with skeletal metastases (Ann Surg Oncol 2007;14:1507)
Treatment
- Surgical resection with negative margins is the treatment of choice
- Trabectedin may be useful in nonresectable tumors
- Neoadjuvant or adjuvant radiation therapy may be considered since myxoid liposarcoma has been found to be more radiosensitive than many other soft tissue tumor types (Cancer 2009;115:3254)
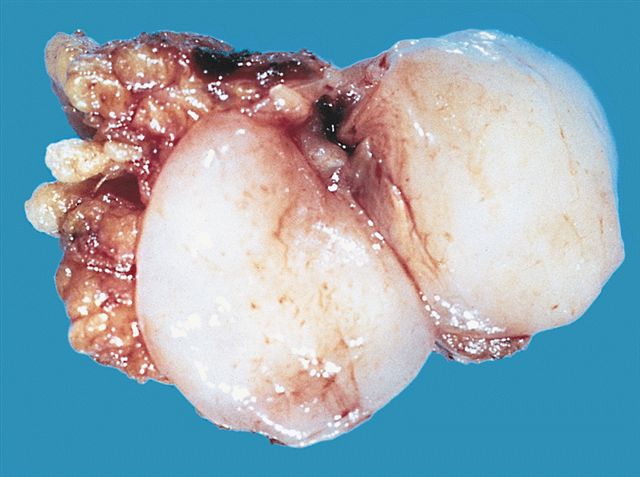
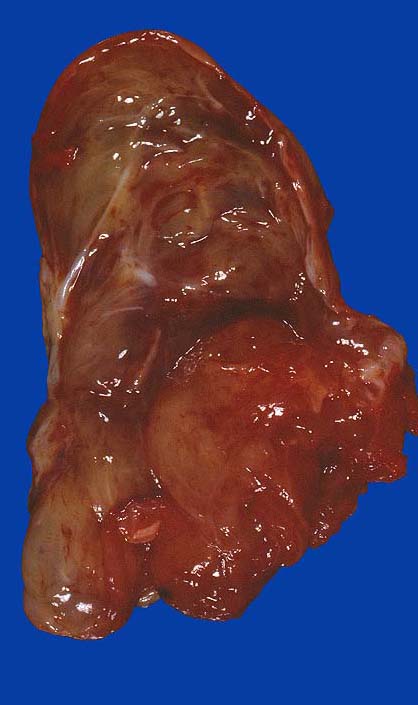
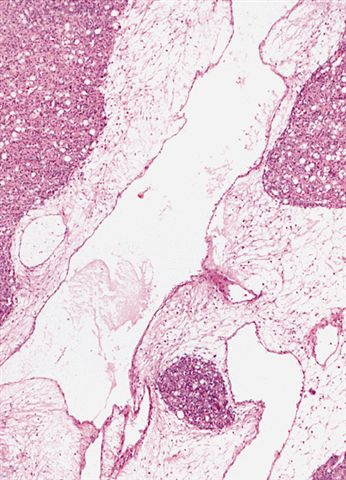
Gross description
- Typically these lesions are well circumscribed and multinodular
- Low grade tumors will have a gelatinous cut surface, with higher grade tumors showing a more solid fleshy appearance
Gross images
Microscopic (histologic) description
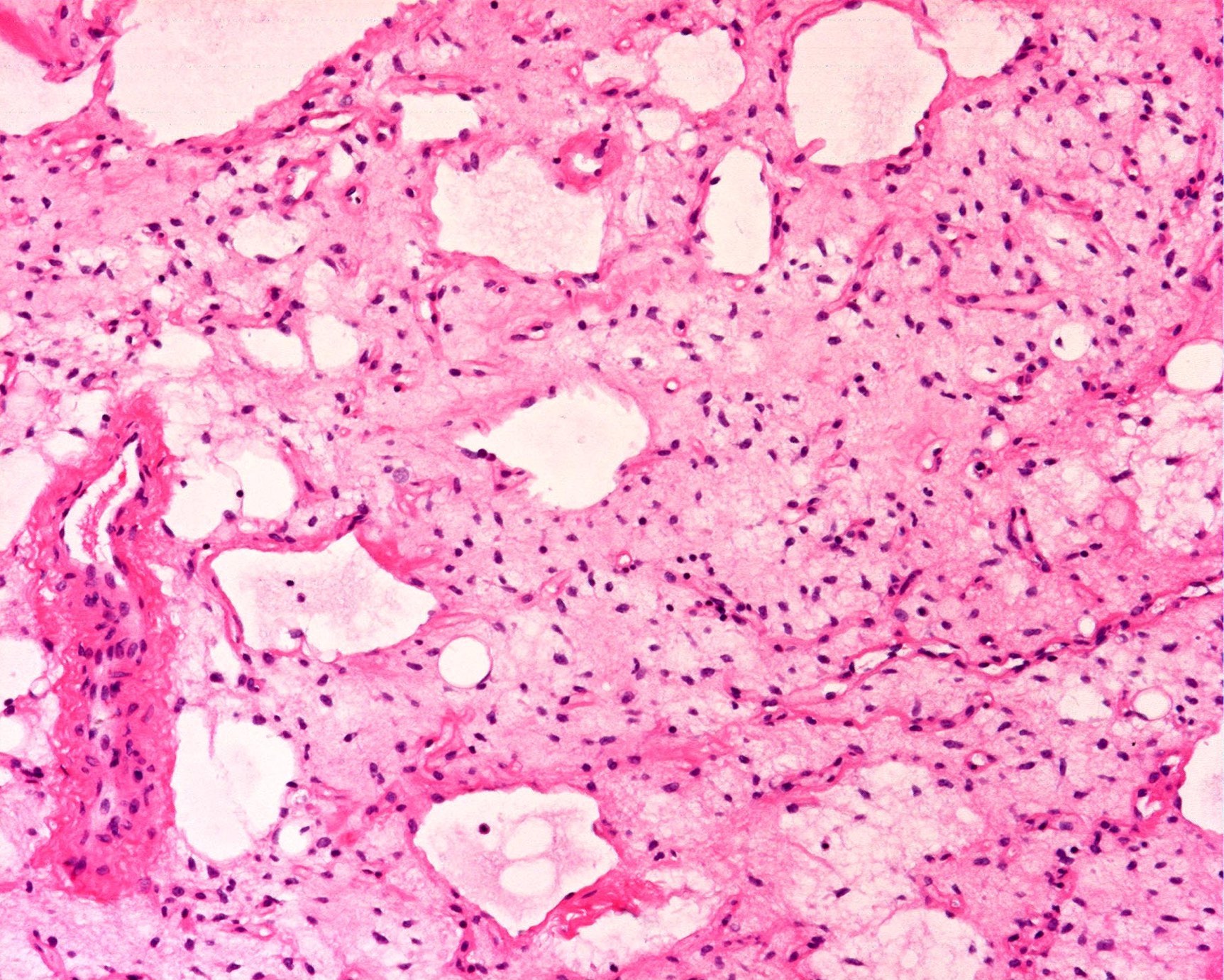
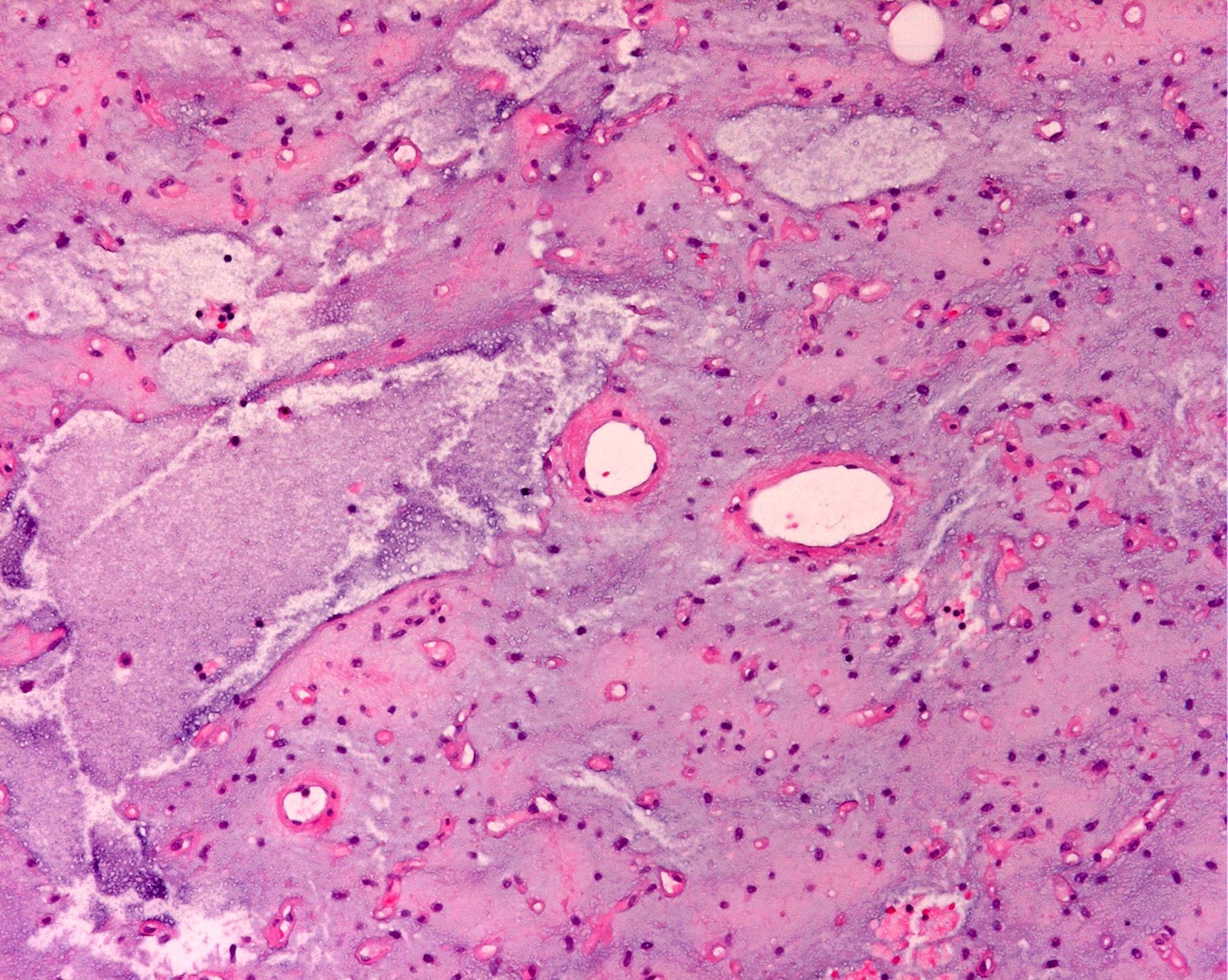
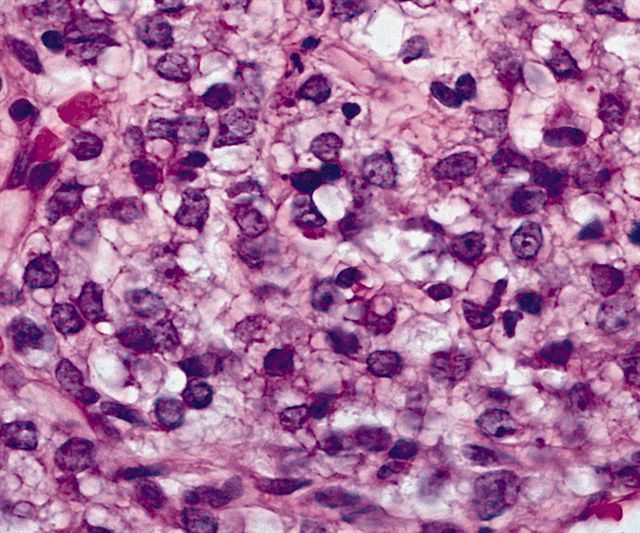
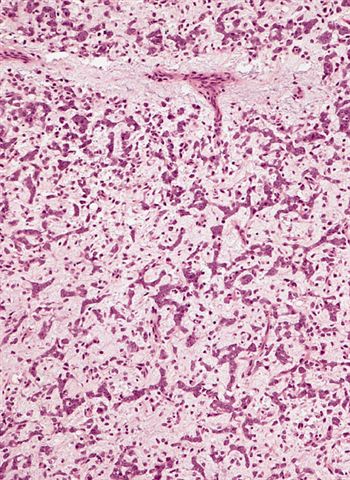
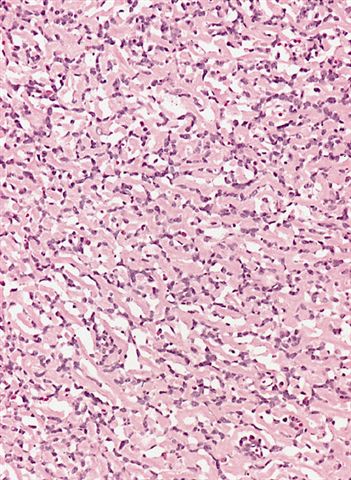
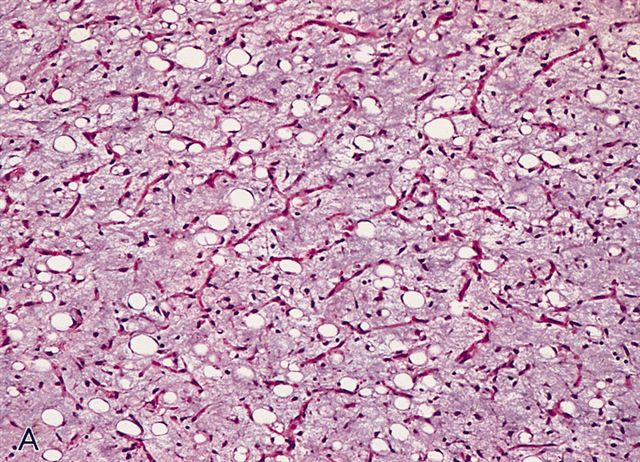
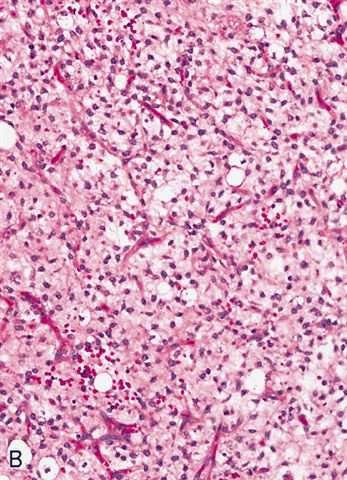
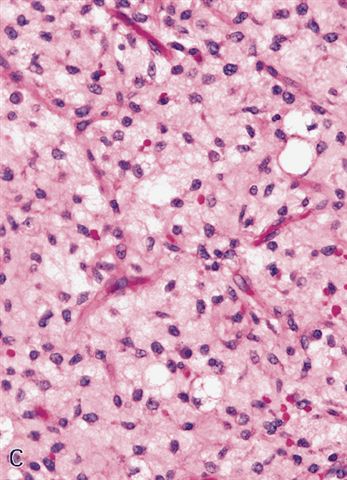
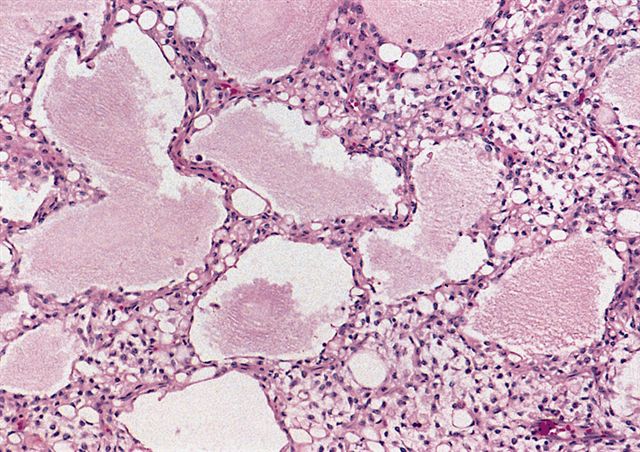
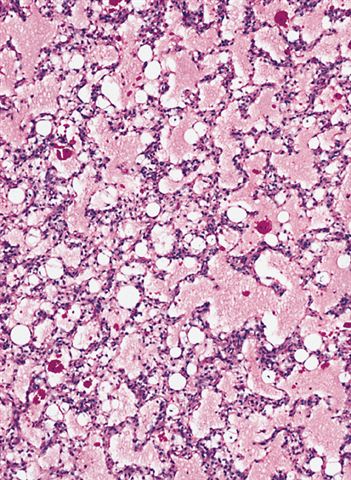
- Low grade
- Paucicellular with monomorphic, stellate or fusiform shaped cells without atypia; striking in their blandness, so much so that any significant pleomorphism should cause one to pause
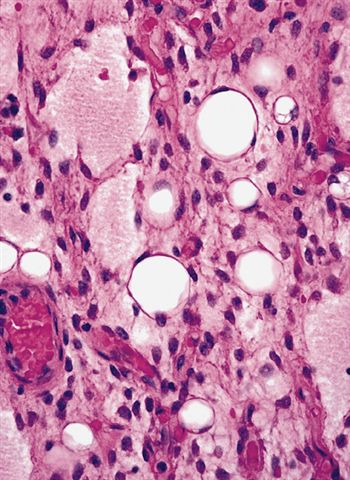
- Prominent plexiform vasculature (delicate thin walled arborizing and curving capillaries that form a network reminiscent of chicken wire fencing)
- These are striking because of the overall background paucicellularity and are still present in high grade tumors but are much less obvious
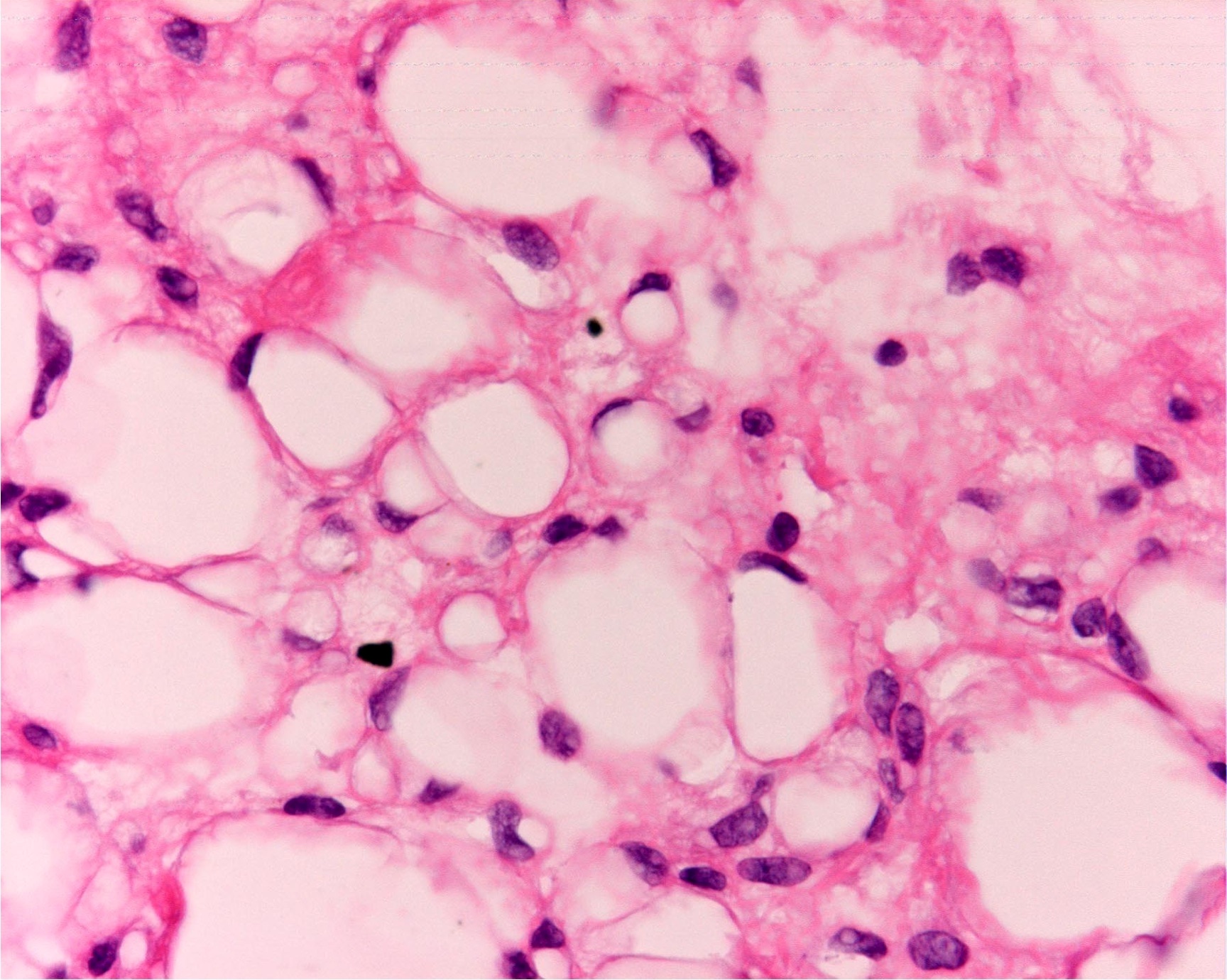
- Numerous signet ring lipoblasts, particularly at periphery of lobules
- This imparts a lipoblastoma-like appearance (see Differential diagnosis)
- Mucoid matrix is rich in hyaluronic acid that may form large mucoid pools (so called pulmonary edema pattern)
- Will be positive for stromal mucin stains such as Alcian blue (see Microscopic (histologic) images)
- Metaplastic cartilage or bone can rarely be seen
- Metaplastic components retain the same molecular alteration without progressive molecular change (no support that these foci represent dedifferentiation) (J Clin Oncol 2018;36:151, Appl Immunohistochem Mol Morphol 2007;15:477)
- Typically there is no significant mitotic activity
- There are many rare morphologic variants (Am J Clin Pathol 2012;137:229)
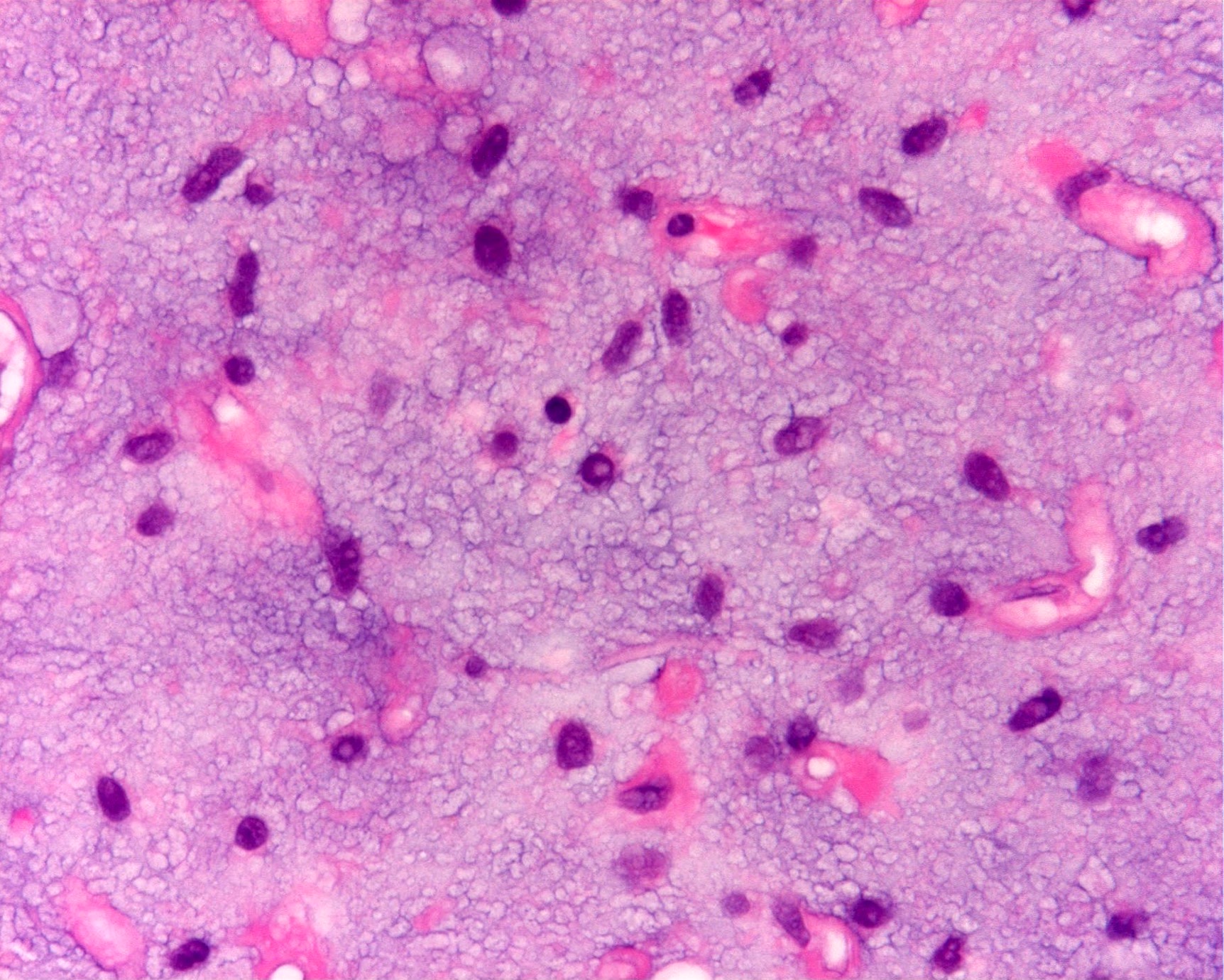
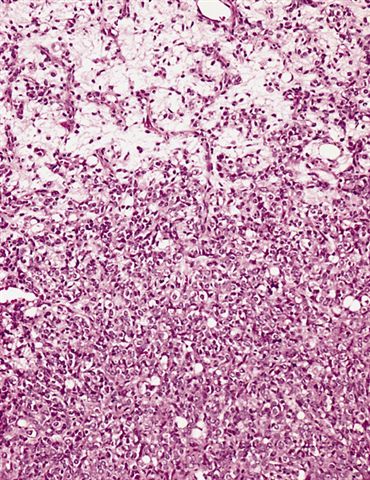
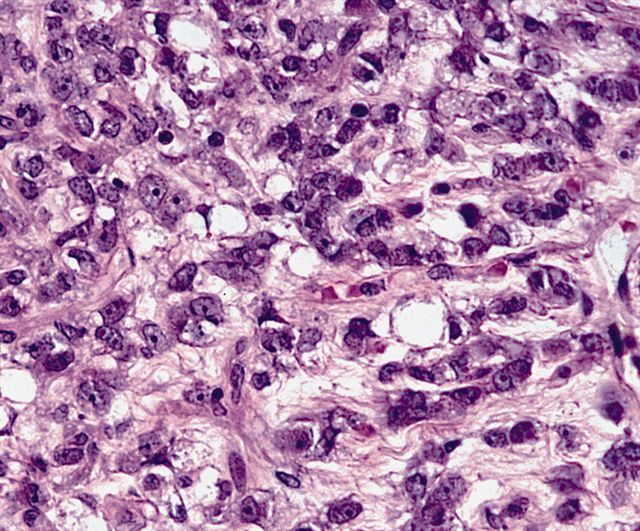
- High grade
- Hypercellular solid sheets of back to back cells with round cell or primitive cytomorphology in > 5% of the sampled tumor
- Cells can have a small amount of hypereosinophilic cytoplasm, a finding of no clinical significance but of significant diagnostic confusion, especially in a limited sample
- Pitfalls and tips
- High grade tumors are so cellular that you can typically walk across nuclei in a high power field without stepping in matrix
- When in doubt, especially in a small sample, pursue molecular testing (typically fluorescent in situ hybridization) for FUS gene rearrangement
- If no FUS gene rearrangement is detected and your suspicion is high that the lesion represents myxoid liposarcoma, proceed to EWSR1 fusion testing, as EWSR1::DDIT3 fusions are detected in rare cases (see Molecular / cytogenetics description)
- Sample these tumors extensively; you likely will not see small amounts of round cell progression grossly
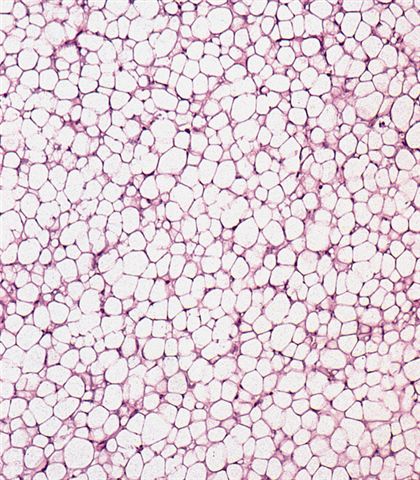
- Can contain large areas of mature adipocytic differentiation
- If the clinical or radiologic picture is concerning, sample additional tumor or do molecular testing
- Location (e.g., extremity) and age of the patient (e.g., young adult) can be helpful clues in the differential diagnosis
- Most of the diagnostic clues are helpful in the appropriate context but individually can be seen in many other tumor types
- Plexiform vasculature and cells that look like signet rings can be found in a diverse variety of tumors
- Combination of a number of clinical, radiologic, histologic and if needed, molecular features will make the diagnosis
Virtual slides
Cytology description
- Myxoid material with arborizing blood vessels and lipoblasts (Acta Cytol 2007;51:456)
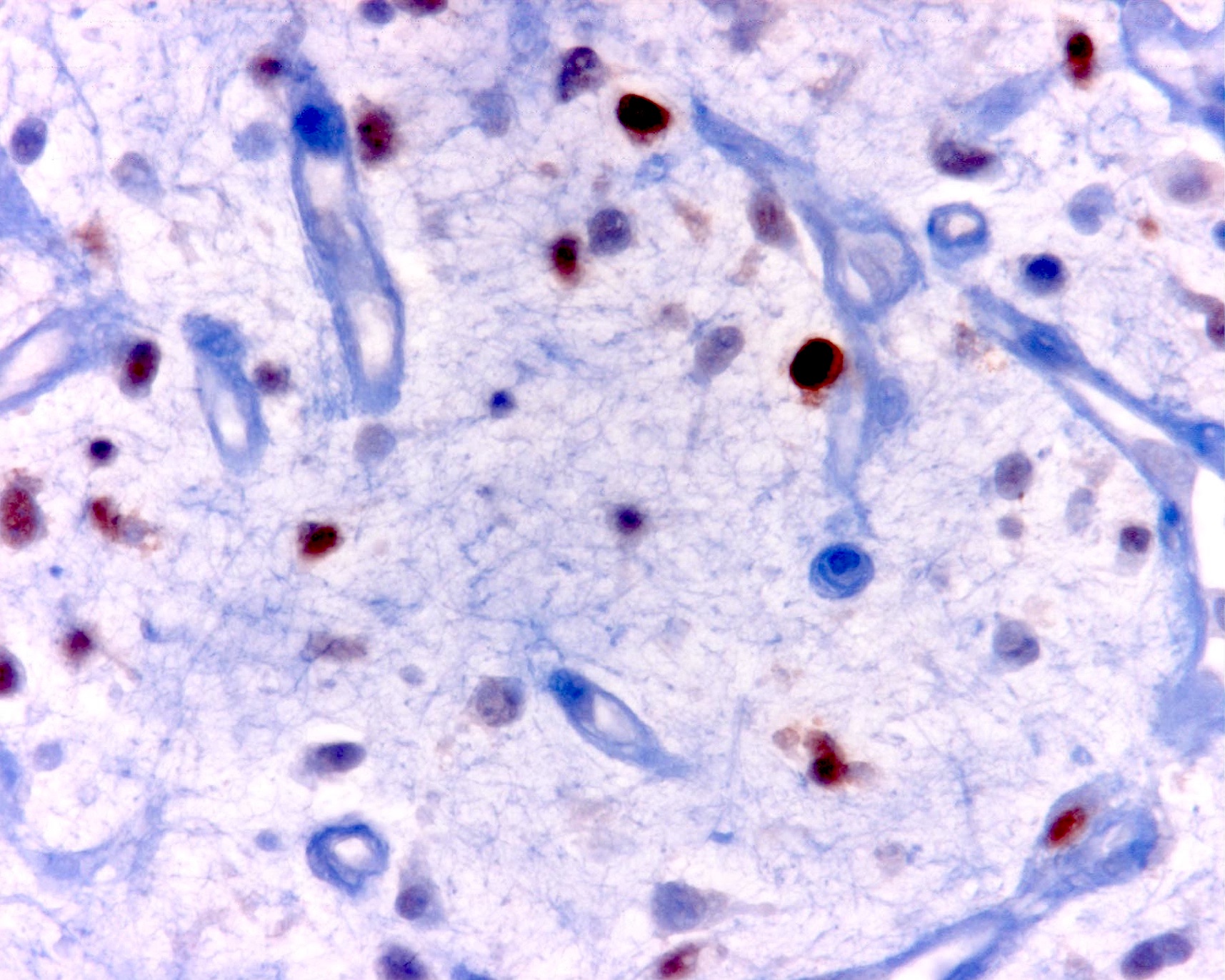
Positive stains
Molecular / cytogenetics description
- t(12;16)(q13;p11.2) FUS::DDIT3 in most cases
- t(12;22)(q13;q12) EWSR1::DDIT3 very rarely (2 - 5%)
- Rearrangements can be complex and involve other chromosomes (Am J Clin Pathol 1995;103:20)
- DDIT3 was formerly known as CHOP (early literature will use the terminology FUS::CHOP)
- Can be identified via FISH, PCR, classic cytogenetics and sequencing
Videos
Myxoid liposarcoma
High grade myxoid liposarcoma
Sample pathology report
- Soft tissue mass, left thigh, resection:
- Myxoid liposarcoma, low grade (5.5 cm) (see comment)
- Surgical resection margins are negative for tumor
- Comment: Histologic sections of this soft tissue mass demonstrate a hypocellular lesion composed of bland round to stellate cells evenly dispersed in a myxoid stroma with delicate arborizing vasculature. No areas of high grade disease are identified. FISH studies are positive for a DDIT3 gene rearrangement, supporting the diagnosis.
Differential diagnosis
- Low grade:
- Atypical lipomatous tumor / well differentiated liposarcoma (ALT / WDL):
- Can be myxoid and focally indistinguishable from myxoid liposarcoma
- Usually has some degree of stromal atypia, however, and will lack the plexiform vasculature
- Has amplification of chromosome 12q14 (including the MDM2 gene) versus the FUS rearrangement seen in myxoid liposarcoma
- Myxoid liposarcomas are also more likely to show a predilection for signet ring lipoblasts
- Extraskeletal myxoid chondrosarcoma (EMC):
- Composed of cords of epithelioid malignant cells set in a similar chondromyxoid matrix
- No cytoplasmic fat vacuoles and less prominent vasculature
- Immunohistochemical staining is not helpful (both are S100 positive)
- Cytogenetics can be helpful but care must be taken
- EMC has t(9;22)(q22;q12) gene rearrangements in most cases that result in an EWSR1::NR4A3 fusion
- EWSR1 FISH will be positive but can lead to confusion with the 2 - 5% of myxoid liposarcomas that rarely have EWSR1 rearrangements
- PCR applications can be particularly helpful in this setting
- In the lung, primary pulmonary myxoid sarcoma should be considered (Pathology 2017;49:792)
- Lipoblastoma / lipoblastomatosis:
- Can show similar histology but usually are present in patients < 5 years old
- Will have PLAG1 gene rearrangements instead of FUS or EWSR1 rearrangements
- Lipoblastoma-like tumor of the vulva:
- Recently described entity that occurs in the vulva and shares remarkable histologic overlap with lipoblastoma and myxoid liposarcoma
- These lesions have been shown to have Rb loss like the spindle cell lipoma family of tumors
- Does not have PLAG1 or FUS rearrangements (Int J Gynecol Pathol 2019;38:204, Am J Surg Pathol 2015;39:1290)
- There is a significant difference in treatment and clinical outcome (only a limited ability to locally recur) and these lesions should be distinguished when possible
- Myxoid dermatofibrosarcoma protuberans (DFSP):
- Typically these are located superficially, which is uncommon in myxoid liposarcoma
- Look carefully to distinguish between entrapped fat versus true signet ring lipoblasts
- Immunohistochemical staining and molecular testing can help
- DFSP will be CD34 positive, S100 negative, with the inverse seen in myxoid liposarcoma and DFSP will harbor the t(17;22)(q22;q13) COL1A1::PDGFB gene fusion
- Some large reference labs offer PDGFB as a break apart FISH assay
- Myxoma:
- Extremely paucicellular, lacks a prominent vascular component and no lipoblasts are found
- Associated with GNAS mutations (Mod Pathol 2009;22:718)
- Atypical lipomatous tumor / well differentiated liposarcoma (ALT / WDL):
- High grade:
- Myxofibrosarcoma:
- Older adults, often superficial, infiltrative and with no true cytoplasmic fat vacuoles (although they can contain pseudolipoblasts)
- Significantly more nuclear atypia, thicker curvilinear vessels and frequent mitotic figures
- Pleomorphic liposarcoma (PLS):
- Entirely different entity that shares similarity in name only
- High grade pleomorphic sarcoma with scattered atypical lipoblasts
- Atypia far in excess of what is seen in round cell liposarcoma, which retains its monotony (a clue to a tumor driven by a translocation)
- Typically has a complex karyotype
- Round cell sarcomas (Ewing, BCOR::CCNB3, CIC::DUX4, etc.):
- Numerous round cell sarcomas that may morphologically resemble high grade myxoid liposarcoma
- Low grade areas and lipoblasts can be particularly informative
- Immunohistochemical and molecular differences can also be exploited (Ewing sarcoma has different partner genes than does myxoid liposarcoma, a feature that can be taken advantage of via sequencing or PCR)
- Myxofibrosarcoma:
Additional references
Practice question #1
The microscopic image above depicts the histologic appearance of a soft tissue mass resected from the thigh of a 37 year old man and is representative of the entire lesion. Which of the following is true regarding the diagnosis?
- Immunohistochemical studies for MDM2 will show strong diffuse positive nuclear staining in the tumor cells
- Majority of cases harbor t(7;16) FUS::CREB3L2 gene fusion
- Majority of cases harbor t(9;22) EWSR1::NR4A3 gene fusion
- Majority of cases harbor t(12;16) FUS::DDIT3 gene fusion
- The lesion is classified as high grade if hypercellular solid sheets of back to back cells with round cell cytomorphology compose > 1% of the sampled tumor
Practice answer #1
D. Majority of cases harbor t(12;16) FUS::DDIT3 gene fusion. The microscopic image depicts a low grade myxoid liposarcoma characterized by a proliferation of bland stellate tumor cells embedded in a myxoid matrix with a prominent plexiform capillary network and scattered signet ring lipoblasts. There is no mitotic activity or pleomorphism. The majority of cases of myxoid liposarcoma harbor a t(12;16) FUS::DDIT3 gene fusion. Answers B and C are incorrect because the t(9;22) EWSR1::NR4A3 gene fusion is characteristic of extraskeletal myxoid chondrosarcoma and the t(7;16) FUS::CREB3L2 gene fusion is characteristic of low grade fibromyxoid sarcoma. Answer E is incorrect because classification of myxoid liposarcoma as high grade requires > 5% of the sampled lesion to consist of a hypercellular round cell component according to the WHO. Cases with borderline round cell component (< 5%) are regarded as having areas of transition, a designation of unclear diagnostic significance. Answer A is incorrect because immunohistochemistry for MDM2 is negative in myxoid liposarcomas.
Comment Here
Reference: Myxoid liposarcoma
Comment Here
Reference: Myxoid liposarcoma
Practice question #2
Which of the following features is characteristic of myxoid liposarcomas?
- Hyalinized, thick walled vessels
- Poor response to radiation therapy
- Primary tumor in the retroperitoneum
- Propensity to skip the lung and metastasize to other soft tissue sites
- Marked nuclear atypia
Practice answer #2
D. Propensity to skip the lung and metastasize to other soft tissue sites. Myxoid liposarcomas have a unique propensity to metastasize to other soft tissue sites. Answers A and E are incorrect because these tumors tend to have bland nuclear features and arborizing plexiform vasculature. Answer B is incorrect because they have been found to be more radiosensitive than many other soft tissue tumor types. Answer C is incorrect because although myxoid liposarcomas can commonly metastasize to the retroperitoneum, primary retroperitoneal tumors are quite rare.
Comment Here
Reference: Myxoid liposarcoma
Comment Here
Reference: Myxoid liposarcoma