Table of Contents
Definition / general | Essential features | Terminology | Clinical features | Diagnosis | Case reports | Cytology description | Cytology images | Explanatory notes | Management | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Suzuki A. AUS. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidatypia.html. Accessed September 23rd, 2025.
Definition / general
- Bethesda category III, atypia of undetermined significance (AUS) is used for cases with a minor degree of atypia, primarily cytologic or architectural in nature, insufficient to qualify for either of the indeterminate categories (category IV - V) and higher
Essential features
- AUS includes cases with few cells that have distinct but mild nuclear atypia or with more extensive but very mild nuclear atypia
- Frequency: 1 - 20%
- Resection rate: 43.0 - 64.7%
- Risk of malignancy (ROM): 13 - 30%
- Repeat fine needle aspiration (FNA) results in a more definitive cytologic interpretation (70 - 90%)
Terminology
- AUS can be subdivided into AUS with nuclear atypia (AUS-N) and other atypia (AUS-O)
- AUS-N: a low level of concern for papillary thyroid carcinoma (PTC) or noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP)
- AUS-O: nonnuclear features result in an AUS interpretation
- Follicular lesion of undetermined significance (FLUS), previously considered synonymous with AUS or often used as a synthetic term AUS / FLUS, was removed in the third edition to avoid confusion
Clinical features
- Frequency: 8% in meta analysis (Expert Rev Endocrinol Metab 2014;9:97)
- AUS is considered as the last resort after excluding all the rest of the Bethesda categories
- Goal is to have 7 - 10% and ideally AUS:malignant ratio should not exceed 3:1 (used as quality control criteria in the individual laboratory) (Cancer Cytopathol 2015;123:713, Cancer Cytopathol 2012;120:111)
- Architectural atypia (41%) > nuclear atypia (32%) > oncocytic atypia (17%)
- Resection rate: 43.0 - 64.7% (Thyroid 2014;24:832, Arch Pathol Lab Med 2013;137:1664)
- Risk of malignancy: 13 - 30% (Ali: The Bethesda System for Reporting Thyroid Cytopathology, 3rd Edition, 2023, Cancer Cytopathol 2012;120:111)
- Nuclear atypia (36 - 44%) > other atypia (15 - 23%) (Acta Cytol 2011;55:518)
- 16% when NIFTP is implicated (Ali: The Bethesda System for Reporting Thyroid Cytopathology, 3rd Edition, 2023, Cancer Cytopathol 2012;120:111)
Diagnosis
- Aspirates containing cells (follicular, lymphoid or other) with architectural or nuclear atypia that is not sufficient to be classified as follicular neoplasm (FN), suspicious for malignancy or malignant (Ali: The Bethesda System for Reporting Thyroid Cytopathology, 3rd Edition, 2023)
Case reports
- 10 year old girl with multifocal NIFTP (F1000Res 2020;9:645)
- 43 year old man with follicular thyroid carcinoma with large sternal metastasis (Int J Surg Case Rep 2023;112:108973)
- 59 year old man with intrathyroid thyroglossal duct cyst (Cureus 2021;13:e20399)
- 65 year old man with synchronous papillary - medullary thyroid microcarcinoma (AME Case Rep 2022;6:27)
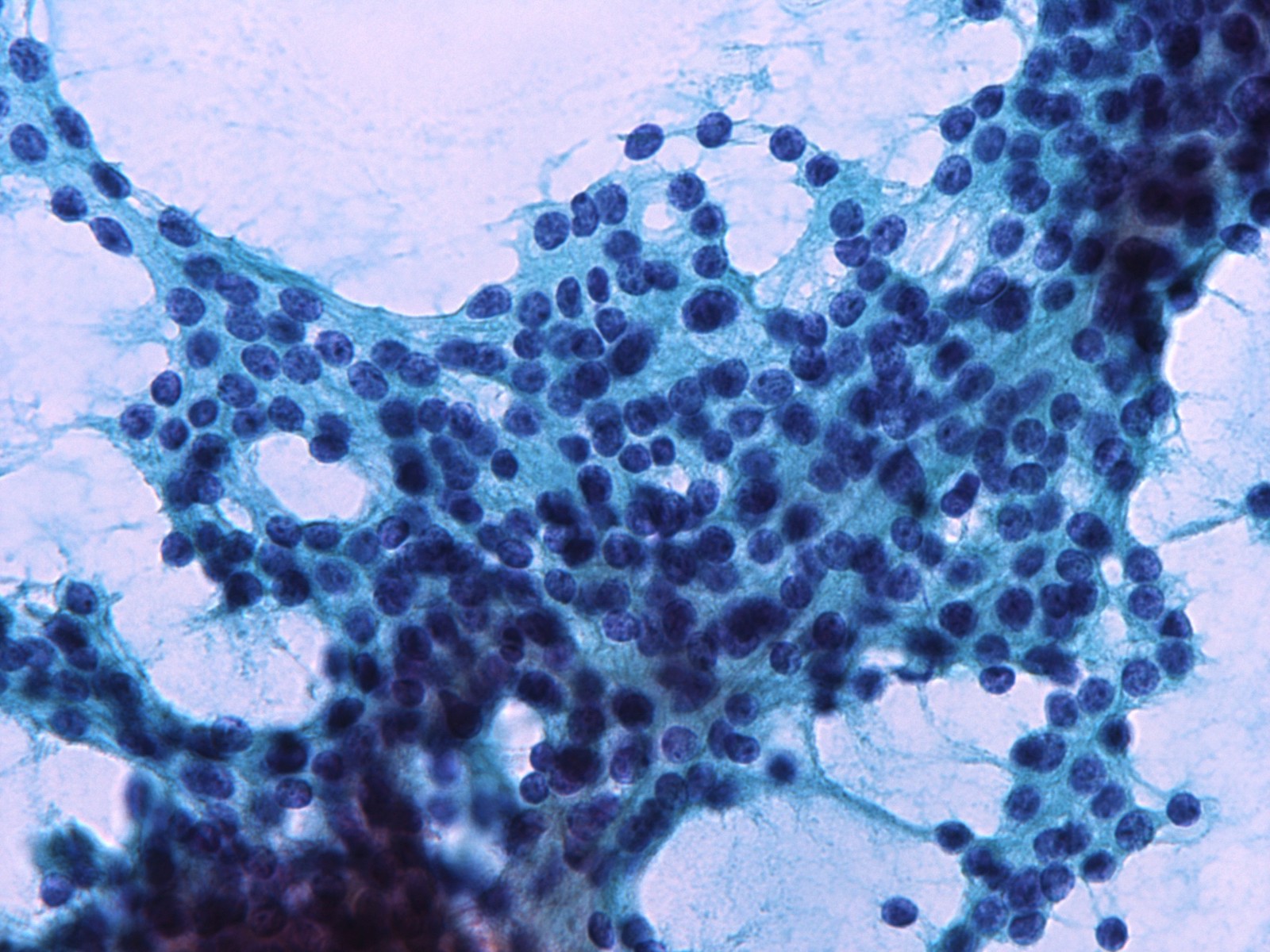
Cytology description
- AUS-N
- Can be focal or can show most cells with mild nuclear atypia
- Most of the aspirate appears benign but rare cells have
- Nuclear enlargement
- Pale chromatin
- Irregular nuclear contours
- No nuclear pseudoinclusions
- Reference: Thyroid 2023;33:1039
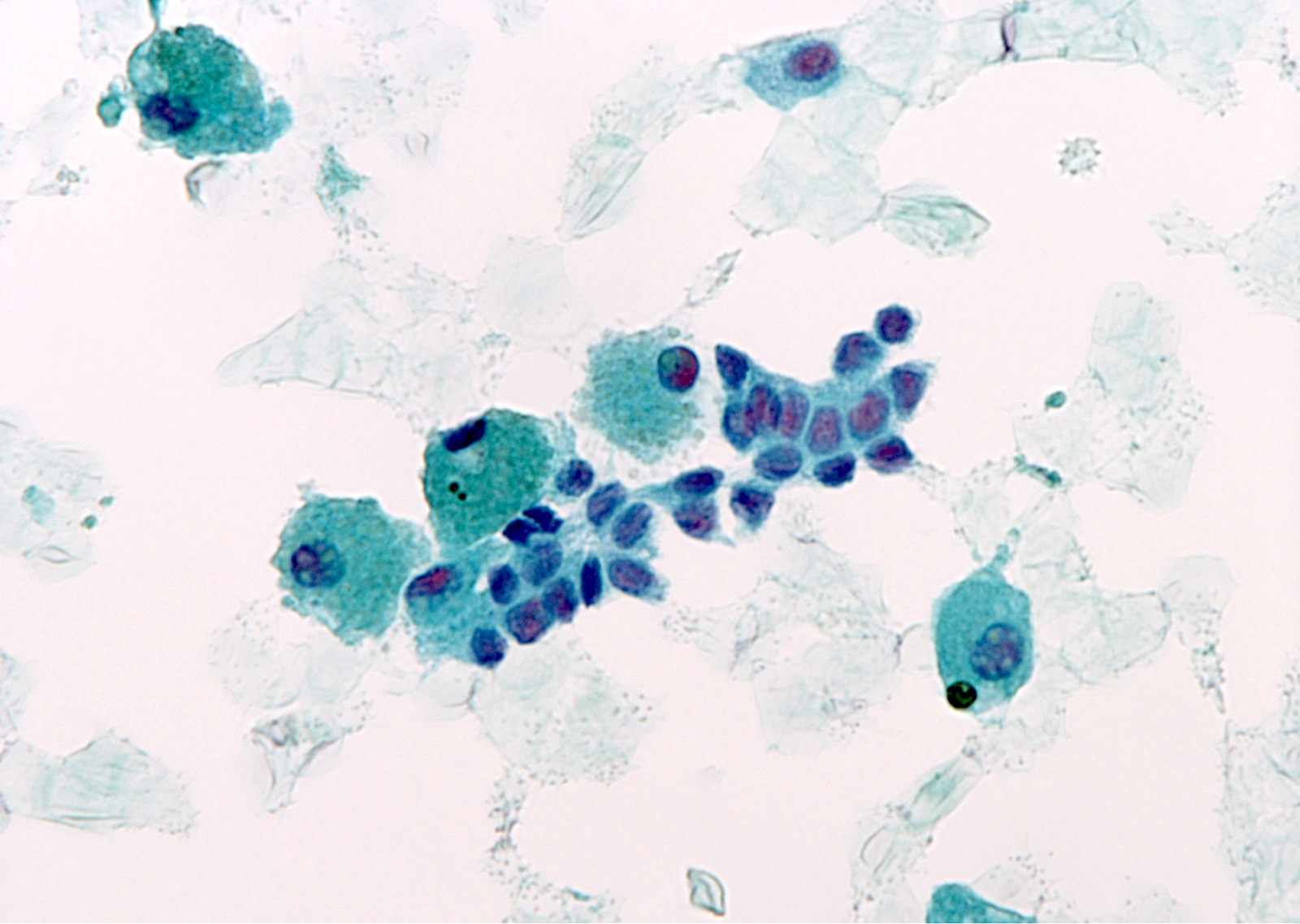
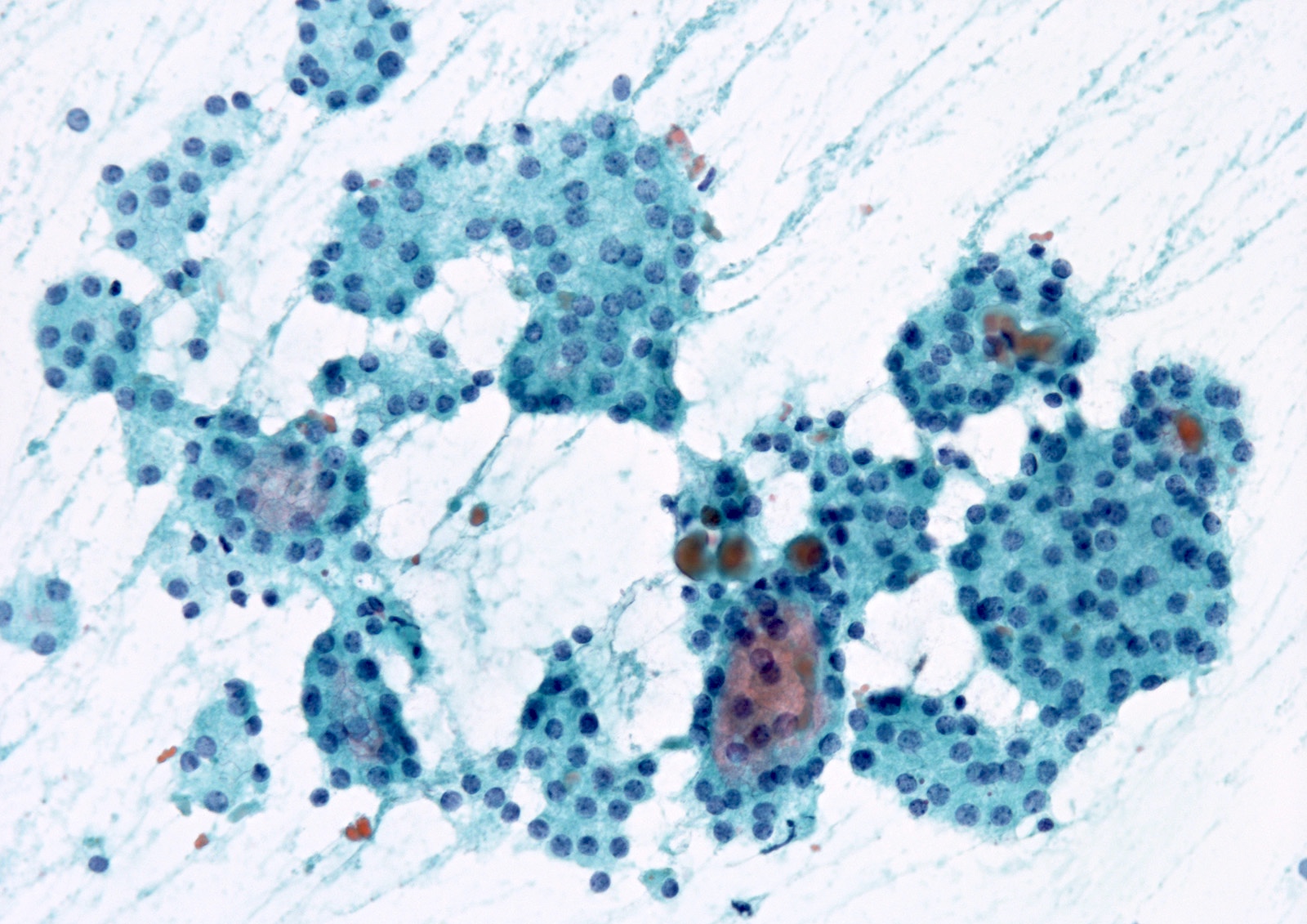
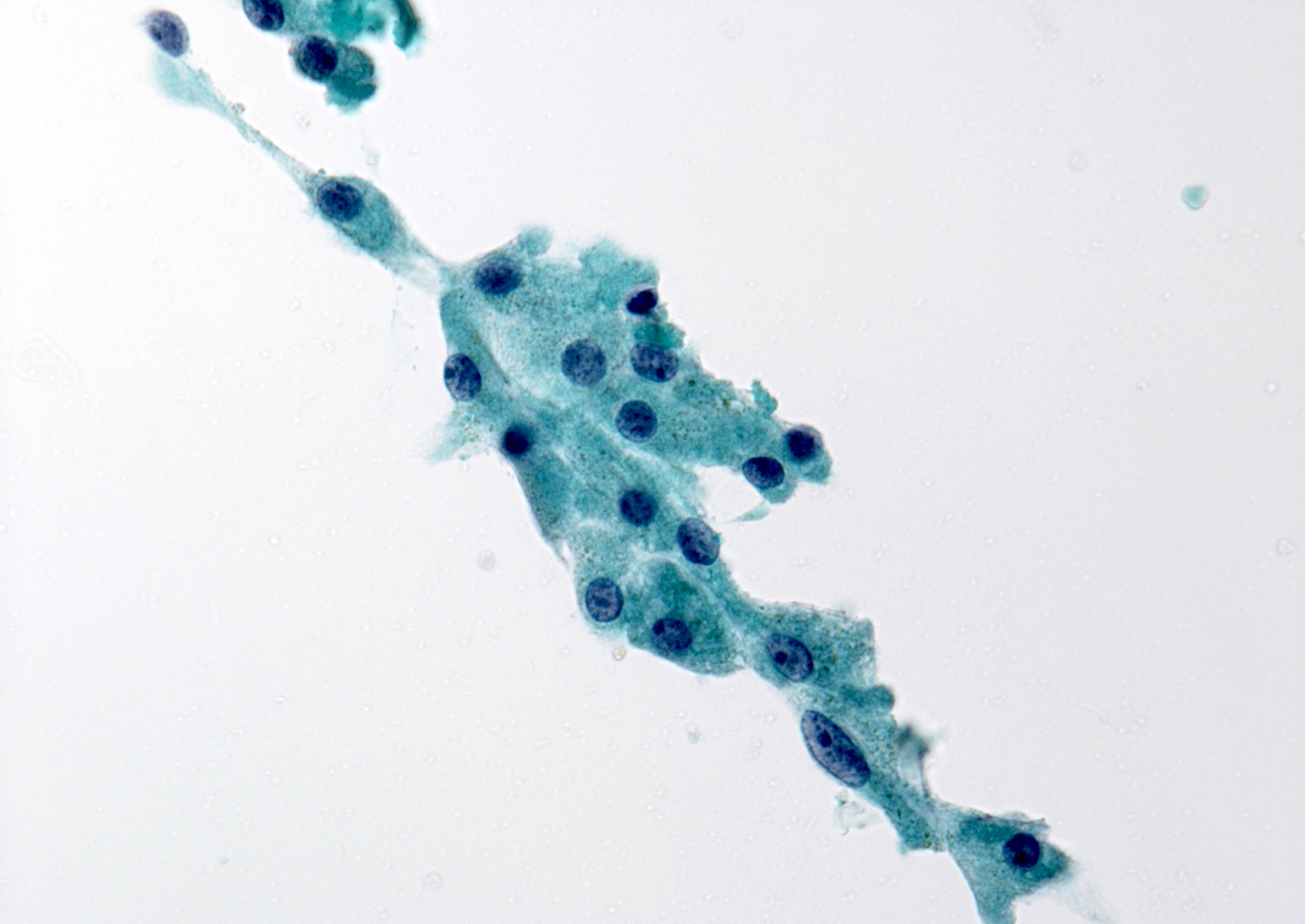
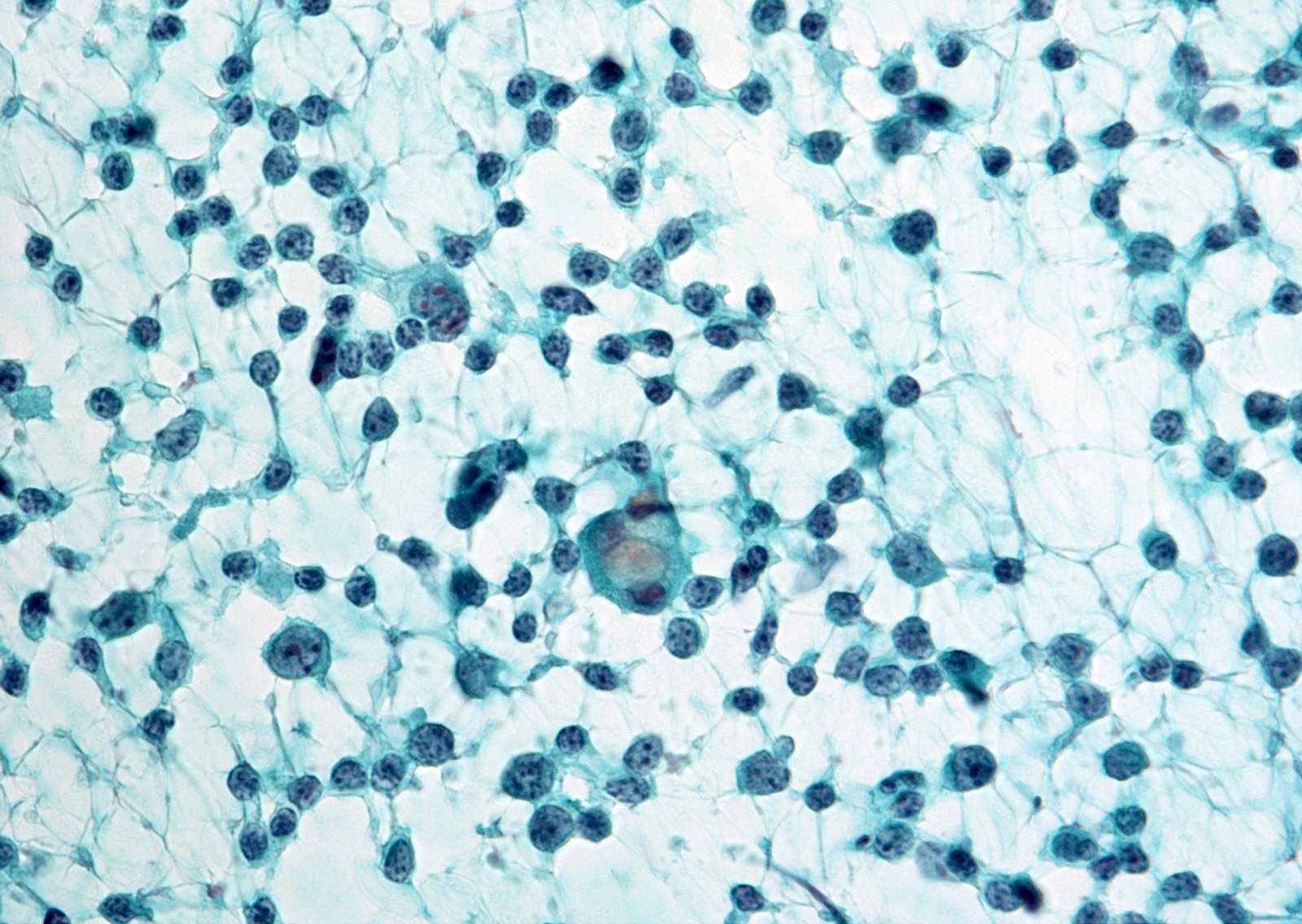
Cytology images
Contributed by Ayana Suzuki, Ph.D.
Images hosted on other servers:
Explanatory notes
- AUS is an interpretation of last resort and should be used judiciously
- Specimen preparation artifacts may potentially raise concern for AUS
- AUS with nuclear atypia is associated with papillary thyroid carcinoma (28 - 56%) (Am J Clin Pathol 2011;136:572, Diagn Cytopathol 2012;40:410)
- Rare cells (< 20 cells) with enlarged, often overlapping nuclei, pale chromatin, irregular nuclear outlines and nuclear grooves
- Well defined, intranuclear pseudoinclusions or psammomatous calcifications (more suspicious) (Acta Cytol 2008;52:320)
- AUS subclassification in children also provides further risk stratification, similar to adults
Management
- 2015 American Thyroid Association Management Guidelines recommend either repeat FNA or molecular testing (Thyroid 2016;26:1)
- Molecular testing of AUS nodules can reduce the need for diagnostic surgery
- 65 - 87% of AUS cases have a negative molecular testing result (architectural atypia > cytologic atypia)
- Oncocytic AUS has a lower rate of gene expression classifier (GEC) benign results despite its very low risk of malignancy (Thyroid 2015;25:789)
- Surgery versus continued observation is based on a synthesis of cytologic, molecular, clinical and radiologic findings as well as clinical risk factors and patient preference
- NIFTP will diminish the overall risk of malignancy for AUS (Thyroid 2015;25:987, Cancer Cytopathol 2016;124:181)
Videos
Atypical thyroid FNA
Head and tail of the Bethesda system for thyroid
Thyroid cytology - Bethesda classification
How to observe thyroid FNA
Sample pathology report
- Thyroid, ultrasound guided FNA:
- AUS-O (see comment)
- Sparsely cellular aspirate comprised of follicular cells with microfollicular pattern colloid is absent
- Comment: Repeat FNA or molecular testing may be helpful if clinically indicated.
- Thyroid, ultrasound guided FNA:
- AUS-N (see comment)
- Follicular cells with mild nuclear irregularity
- Comment: Repeat FNA or molecular testing may be helpful if clinically indicated.
- Thyroid, ultrasound guided FNA:
- AUS-N (see comment)
- Follicular cells, predominantly benign appearing, with focal nuclear atypia
- Comment: Repeat FNA or molecular testing may be helpful if clinically indicated.
- Thyroid, ultrasound guided FNA:
- AUS-O (see comment)
- Numerous relatively monomorphic lymphoid cells
- Comment: An additional aspiration, with apportioning of needle washout fluid for flow cytometry, may be helpful if clinically indicated.
Differential diagnosis
- AUS-N
- Extensive but mild cytologic atypia:
- Many if not most cells have mildly enlarged nuclei with
- Slightly pale chromatin
- Only limited nuclear contour irregularity
- No nuclear pseudoinclusions
- Many if not most cells have mildly enlarged nuclei with
- Atypical cyst lining cells:
- Cyst lining cells may appear atypical (rare cases), such as
- Nuclear grooves
- Prominent nucleoli
- Elongated nuclei and cytoplasm
- Rare intranuclear pseudoinclusions
- Associated with hemosiderin laden macrophages
- Reactive follicular or mesenchymal cells associated with cystic degeneration of thyroid nodules
- Most cases are benign (Cancer 2005;105:71)
- Cyst lining cells may appear atypical (rare cases), such as
- Histiocytoid cells:
- Compared with histiocytes
- Larger
- Rounder nuclei
- Higher N:C ratio
- Harder (glassier) cytoplasm
- Larger, discrete vacuoles without the hemosiderin or microvacuolization of histiocytes
- Characteristic of cystic papillary thyroid carcinoma (Cancer 2002;96:240)
- Immunostaining: keratins (papillary thyroid carcinoma cells), CD68 (histiocytes)
- Compared with histiocytes
- Extensive but mild cytologic atypia:
- AUS-O
- Architectural atypia:
- Rare clusters with microfollicles or crowded 3 dimensional groups with scant colloid
- Low risk
- Follicular neoplasm diagnosis if the specimen were more cellular
- 50 - 70% of follicular cells exhibit microfollicles but without a marked predominance
- DICER1 mutated nodules may be associated with this pattern in pediatric samples
- Focally prominent microfollicles with minimal nuclear atypia
- More prominent than usual population of microfollicles but not sufficient for a diagnosis of follicular neoplasm
- Should not be confused with an overall mixed but predominantly macrofollicular aspirate (benign)
- Rare clusters with microfollicles or crowded 3 dimensional groups with scant colloid
- Oncocytic atypia:
- Sparsely cellular aspirate comprised of oncocytes with minimal colloid
- Very low risk
- Oncocytic follicular neoplasm diagnosis if the specimen were highly cellular
- Markedly cellular sample composed of oncocytes with sparse colloid, yet the clinical setting suggests benign
- Clinically suggesting lymphocytic thyroiditis or a multinodular goiter
- More highly predictive of a hyperplastic oncocytic nodule than usual (Am J Clin Pathol 2011;135:139)
- Specimens with oncocytes in cohesive flat sheets without nuclear atypia and abundant colloid indicate benign (if high risk clinical or radiologic findings are absent)
- Sparsely cellular aspirate comprised of oncocytes with minimal colloid
- Atypia, not otherwise specified (NOS):
- Minor population of follicular cells with nuclear enlargement and prominent nucleoli
- Does not raise concern for papillary thyroid carcinoma and best classified as NOS
- Specimens from patients with a history of radioactive iodine, carbimazole or other pharmaceutical agents can usually be diagnosed as benign
- Psammomatous calcifications in the absence of follicular cells with nuclear features of papillary thyroid carcinoma
- Psammoma bodies raise concern for papillary thyroid carcinoma and should prompt careful scrutiny of papillary thyroid carcinoma cells
- Lamellar bodies of inspissated colloid may be indistinguishable from true psammomatous calcifications
- Minor population of follicular cells with nuclear enlargement and prominent nucleoli
- Atypical lymphoid cells, rule out lymphoma:
- There is an atypical lymphoid infiltrate but the degree of atypia is insufficient for suspicious for malignancy
- Repeat aspirate for flow cytometry is desirable
- Parathyroid lesion:
- Triangular cell clusters with 1 sharp corner (wedge pattern), salt and pepper chromatin and no colloid (Head Neck 2002;24:157, Acta Cytol 2004;48:133, Diagn Cytopathol 2021;49:70)
- 25 - 30% of parathyroid lesions can be recognized
- Immunohistochemistry (especially GATA3 antibody) and ancillary studies (parathyroid hormone assays, molecular studies) can confirm the diagnosis (Diagn Cytopathol 2021;49:70, Endocr J 2016;63:621)
- Architectural atypia:
Practice question #1
Which case belongs to architectural atypia?
- Atypical lymphoid infiltration
- Focally prominent microfollicles with minimal nuclear atypia
- Most of the aspirate appears benign but rare cells have irregular nuclear contours
- Psammomatous calcifications in the absence of nuclear features of papillary thyroid carcinoma
- Sparsely cellular aspirate comprised of oncocytes with minimal colloid
Practice answer #1
B. Focally prominent microfollicles with minimal nuclear atypia. Microfollicles are architectural atypia, suggesting follicular neoplasm. Answer A is incorrect because atypical lymphoid infiltration belongs to atypical lymphoid cells. Answer C is incorrect because most of the aspirate appearing benign but rare cells having irregular nuclear contours belongs to nuclear atypia. Answer D is incorrect because psammomatous calcifications in the absence of nuclear features of papillary thyroid carcinoma (PTC) belongs to atypia, not otherwise specified. Answer E is incorrect because sparsely cellular aspirate comprised of oncocytes with minimal colloid belongs to oncocytic atypia.
Comment Here
Reference: AUS
Comment Here
Reference: AUS
Practice question #2
Practice answer #2
B. GATA3. The lesion shown in the image is an intrathyroidal parathyroid adenoma. Answer A is incorrect because calcitonin is a marker for medullary thyroid carcinoma. Answers C, D, and E are incorrect because PAX8, thyroglobulin and TTF1 are markers for follicular cells.
Comment Here
Reference: AUS
Comment Here
Reference: AUS