Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Xu B. Papillary thyroid carcinoma - classic. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidpapillaryclassic.html. Accessed September 15th, 2025.
Definition / general
- Classic variant of papillary thyroid carcinoma is characterized by 2 cardinal features:
- The presence of true papillae defined as papillae with a central vascular core
- Nuclear features in the overlying epithelial cells defined by nuclear enlargement, nuclear membrane irregularity and a distinct chromatin pattern
Essential features
- Defined by 2 cardinal features: true papillae with a fibrovascular core and nuclear features of papillary carcinoma
- One of the most common types of papillary carcinoma
- Tendency to spread to regional lymph nodes
- High frequency of BRAF V600E mutation
Terminology
- Papillary carcinoma, conventional type (variant)
- Papillary carcinoma, usual type (variant)
ICD coding
Epidemiology
- One of the most common variants of papillary thyroid carcinoma (J Clin Endocrinol Metab 2014;99:E276)
- Previously was most common type of papillary thyroid carcinoma but now papillary microcarcinoma and papillary thyroid carcinoma, follicular variant are more common
- Female predominance; F:M ratio = ~3:1
- Median age of diagnosis in 50s
Sites
- Most commonly affects the thyroid gland
- May also occur in thyroglossal duct, lingual thyroid, ectopic thyroid and struma ovarii (Endocr Pathol 2015;26:75, Endocrine 2016;51:189, Am J Surg Pathol 2007;31:1337)
Etiology
- Ionizing radiation is the best established risk factor, including:
- Iatrogenic (e.g., radiation for head and neck cancer)
- Post Chernobyl nuclear accident (Endocr Pathol 2006;17:307)
- Post atom bomb
- Can be familial in 4.5% of cases (Surgery 2009;145:100)
Clinical features
- Painless palpable thyroid mass
Diagnosis
- Typically, the diagnosis is first rendered on ultrasound guided preoperative fine needle aspiration cytology
- Surgical pathology report of a resected specimen provides further information about the subtyping (i.e., variant) and microstaging
Radiology description
- Diagnostic thyroid ultrasound with survey of cervical lymph nodes is the recommended imaging modality for patients with thyroid nodule(s) (Thyroid 2016;26:1)
- The following ultrasound findings are associated with thyroid carcinoma, in particular papillary thyroid carcinoma (Thyroid 2016;26:1):
- Hypoechogenicity compared with surrounding thyroid or strap muscles
- Irregular border
- Microcalcification
- Tall shape (i.e., a nodule that is taller than wide measured on a transverse view)
Prognostic factors
- AJCC pathologic staging and the American Thyroid Association (ATA) initial risk stratification provide prognostic information (Amin: AJCC Cancer Staging Manual, 8th Edition, 2018, Thyroid 2016;26:1)
- Pathologic parameters included in the risk stratification for a classic variant of papillary thyroid carcinoma are:
- ATA intermediate risk: microscopic invasion into perithyroidal soft tissue, lymphovascular invasion and > 5 pathologically positive lymph nodes with all involved lymph nodes < 3 cm in size
- ATA high risk: gross extrathyroidal extension, incomplete resection, distant metastasis and pathologic nodal metastasis ≥ 3 cm in greatest dimension
Case reports
- 7 year old girl with sporadic papillary thyroid carcinoma, classic variant harboring ETV6-NTRK3 fusion (J Pediatr Endocrinol Metab 2018;31:461)
- 12 and 16 year old boys with papillary thyroid carcinoma arising within thyroglossal duct cyst (Head Neck Pathol 2017;11:442)
- 48 year old woman with synchronous papillary thyroid carcinoma and non-Hodgkin lymphoma (Medicine (Baltimore) 2018;97:e9831)
- 61 year old man with papillary thyroid carcinoma metastatic to axillary lymph node (J Med Case Rep 2015;9:181)
- 72 year old man with metastatic papillary thyroid carcinoma into a clear cell renal cell carcinoma (J Otolaryngol Head Neck Surg 2017;46:17.)
Treatment
- Commonly treated with surgical resection (e.g., total thyroidectomy, subtotal thyroidectomy, hemithyroidectomy or lobectomy)
- Post operative radioactive iodine treatment may be considered if the tumor exhibits aggressive features (ATA intermediate or high risk) (Thyroid 2016;26:1)
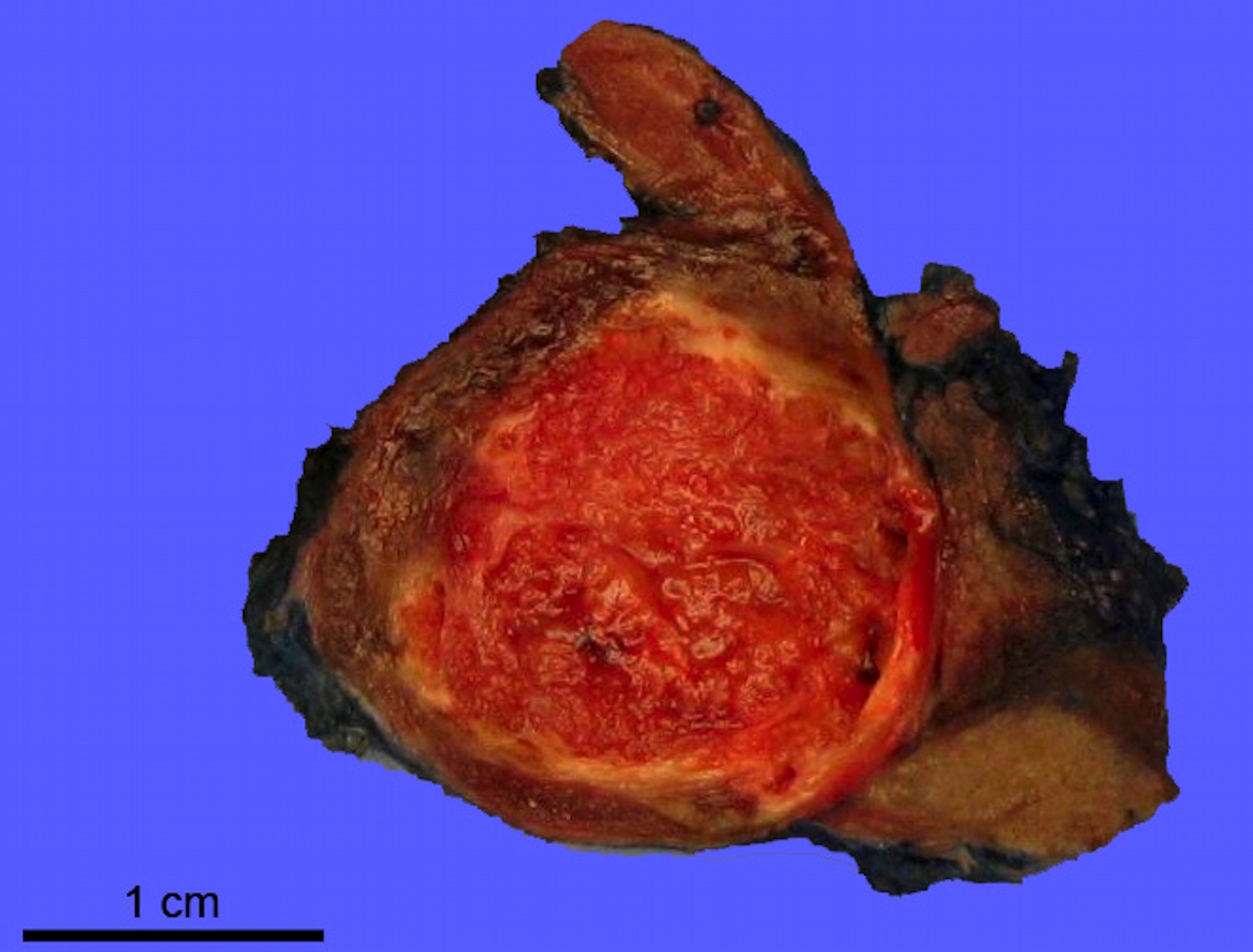
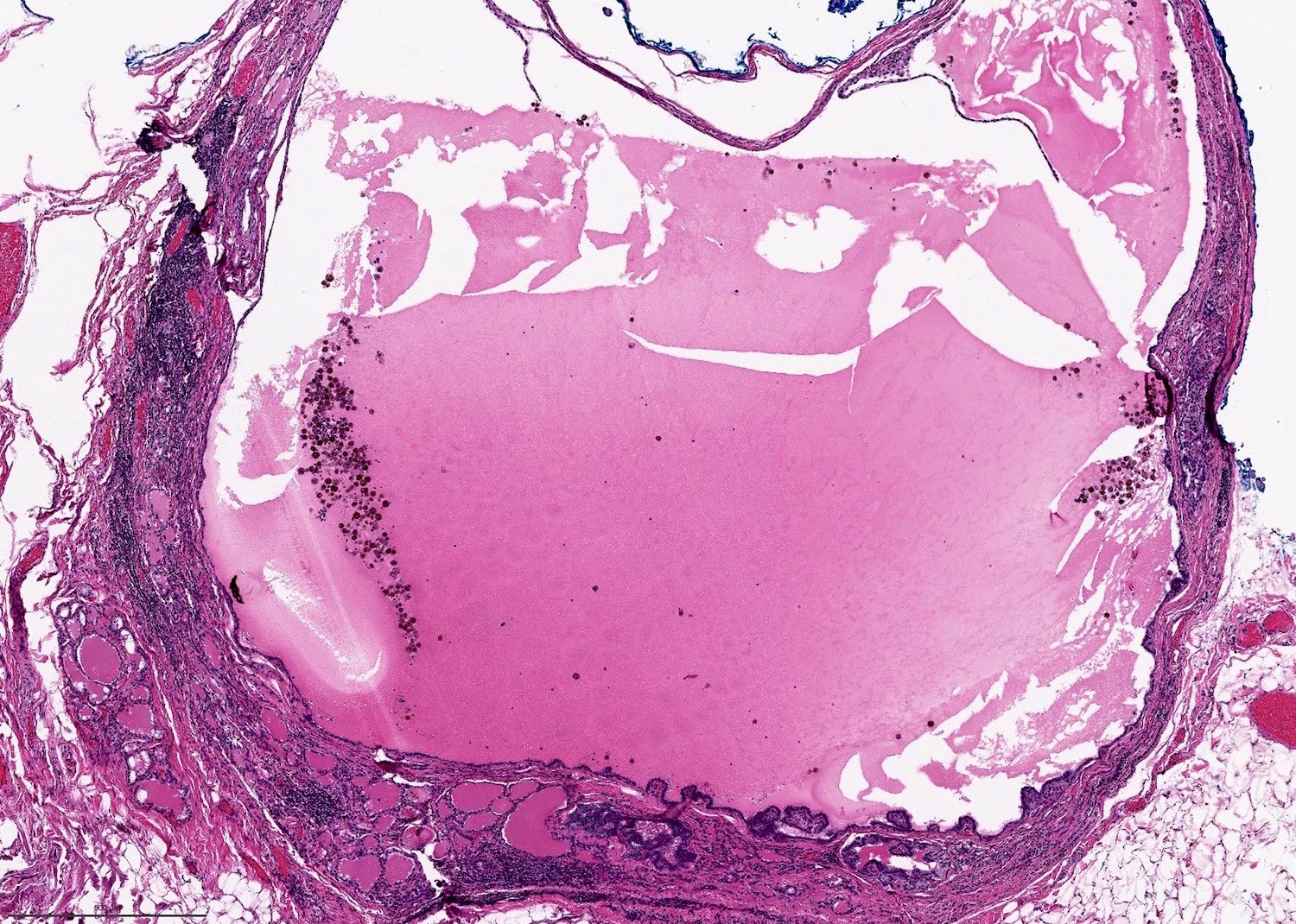
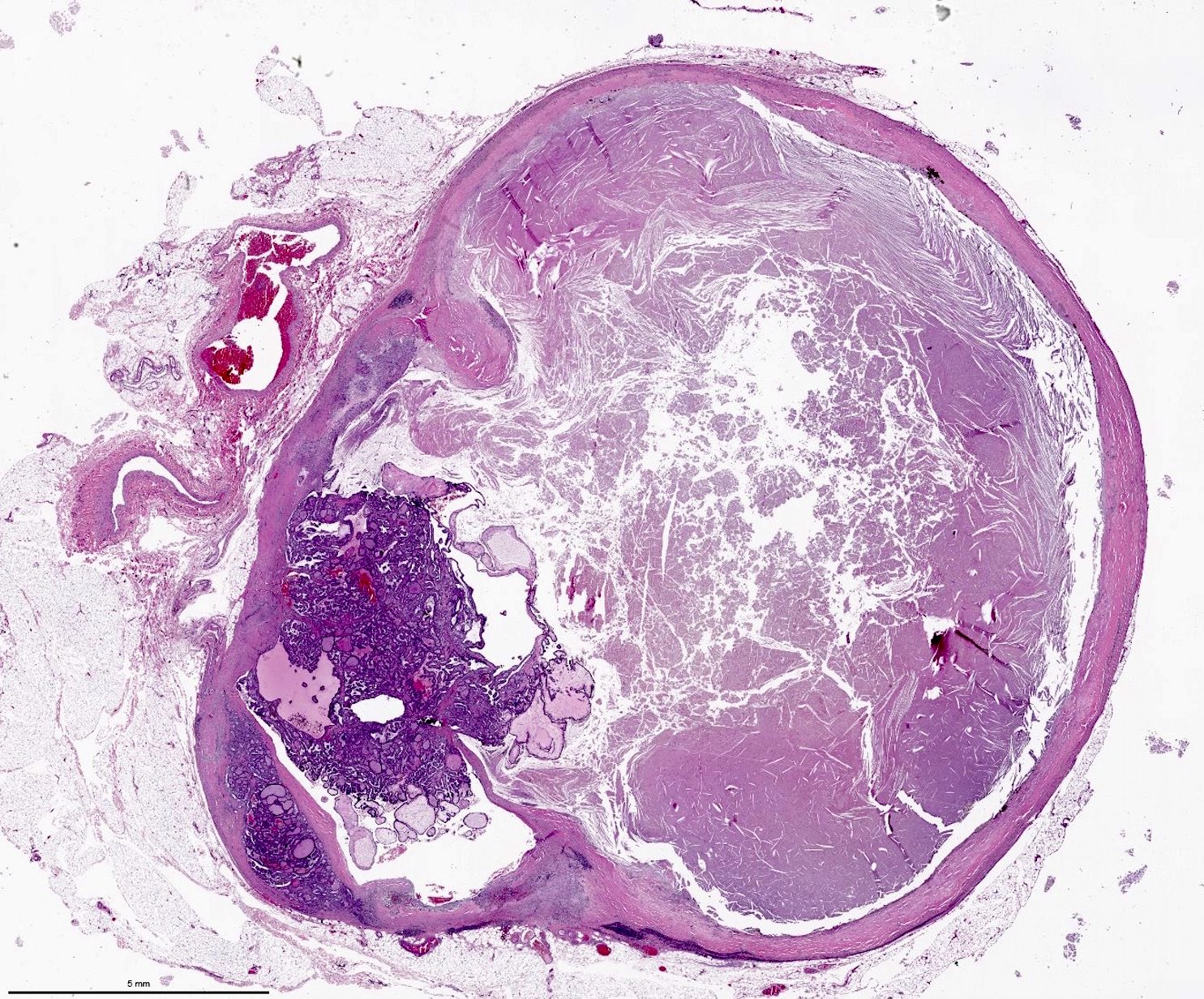
Gross description
- Solid or cystic mass with papillary projections
Frozen section description
- Frozen section of papillary thyroid carcinoma is strongly discouraged as frozen artifacts distort the nuclear features necessary for diagnosis
- The standard care is to perform preoperative fine needle aspiration to establish the diagnosis and to determine the most appropriate surgical procedure
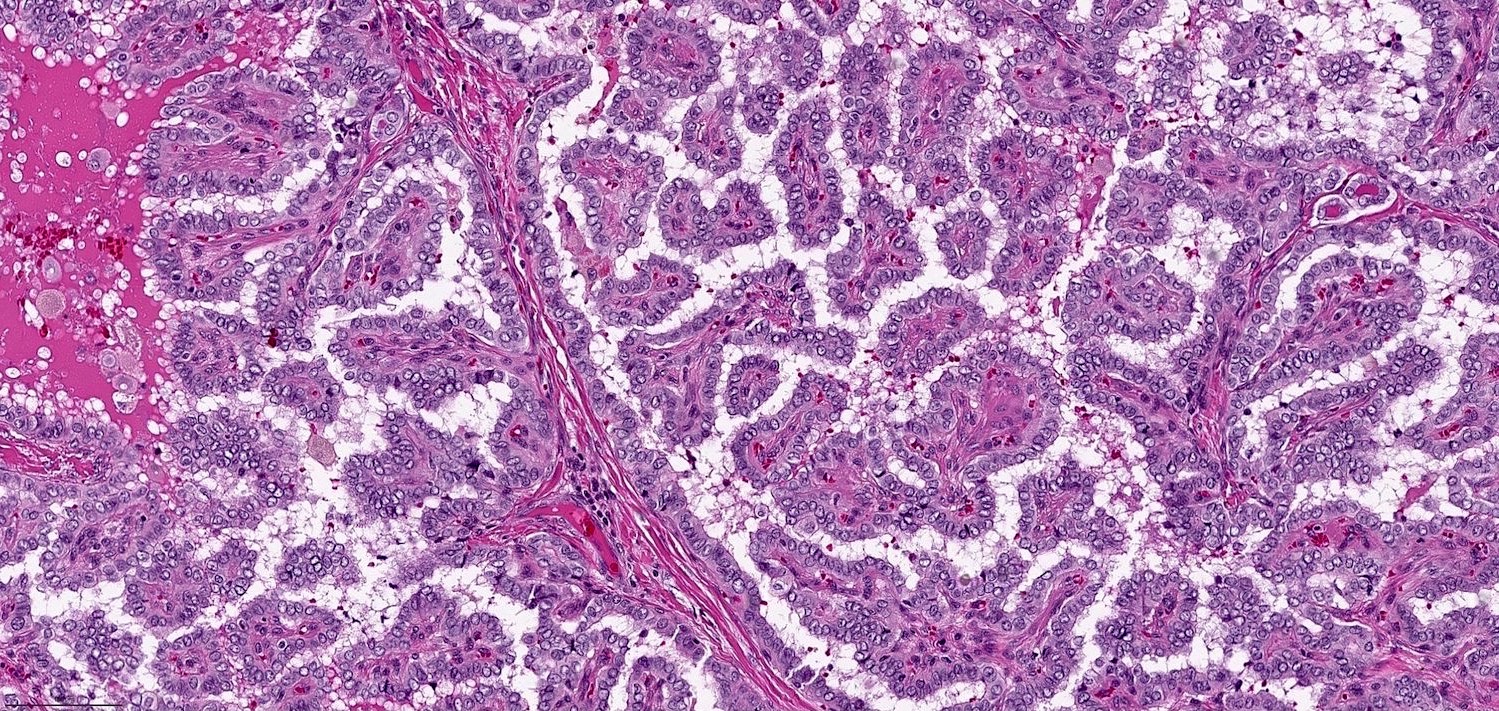
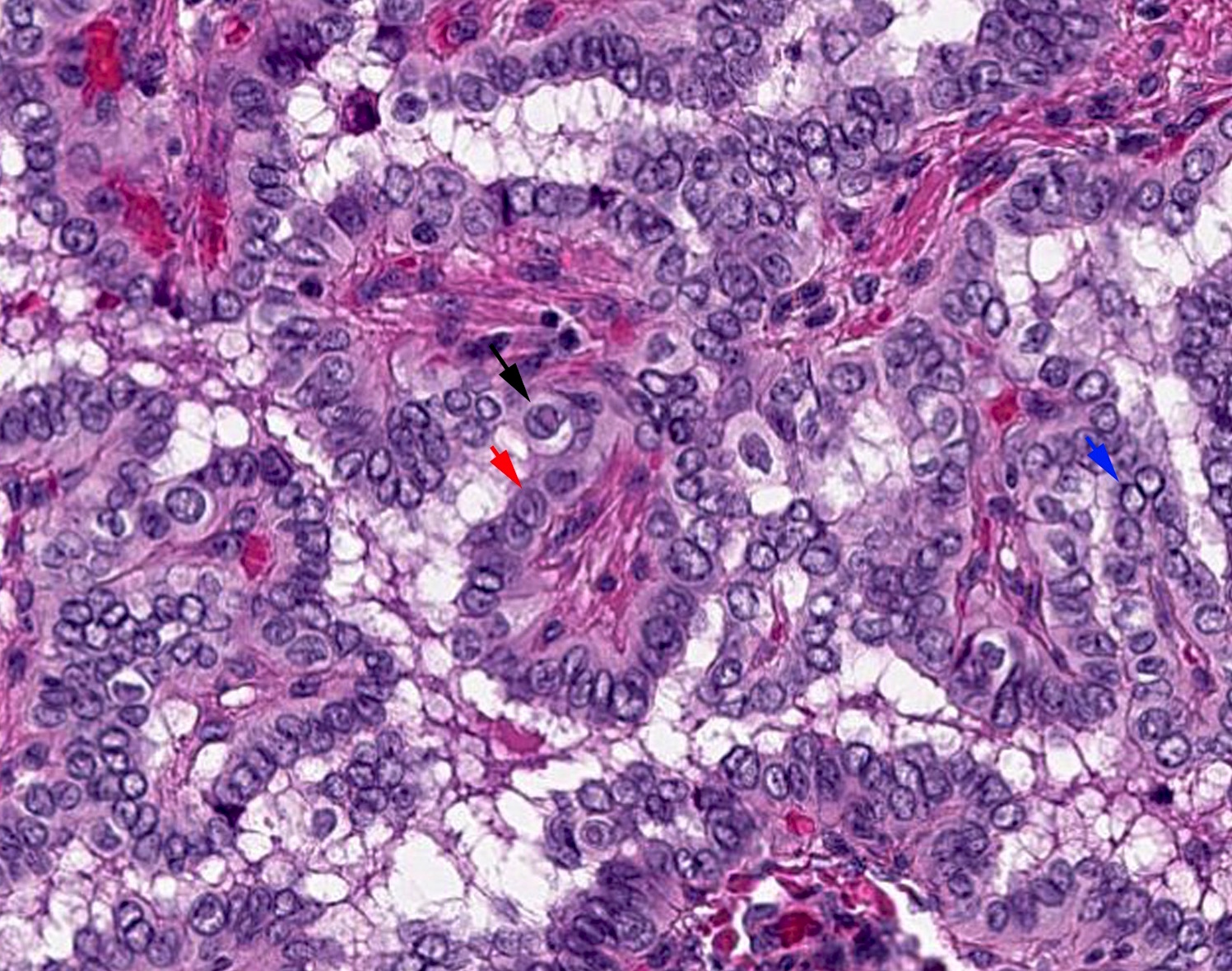
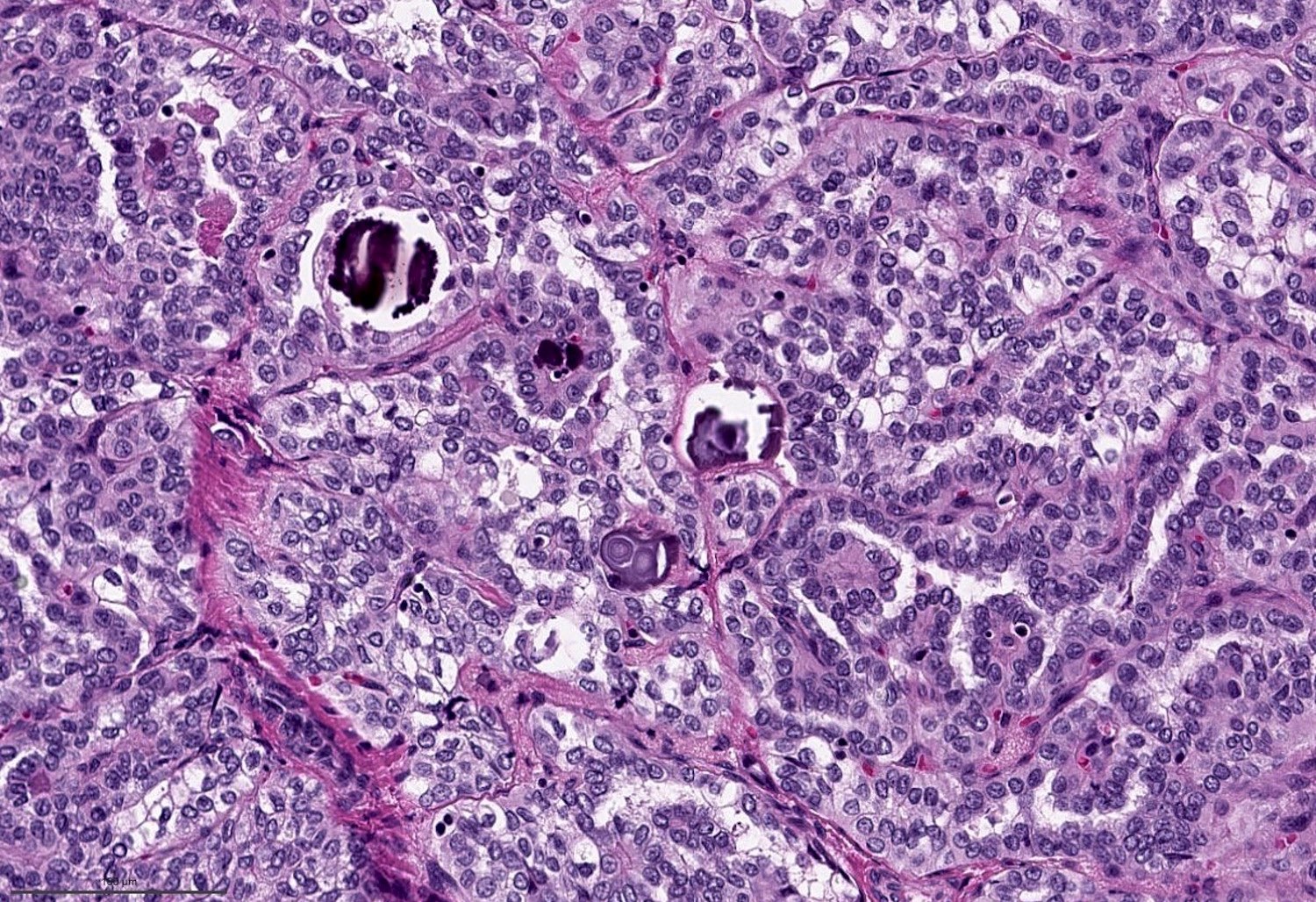
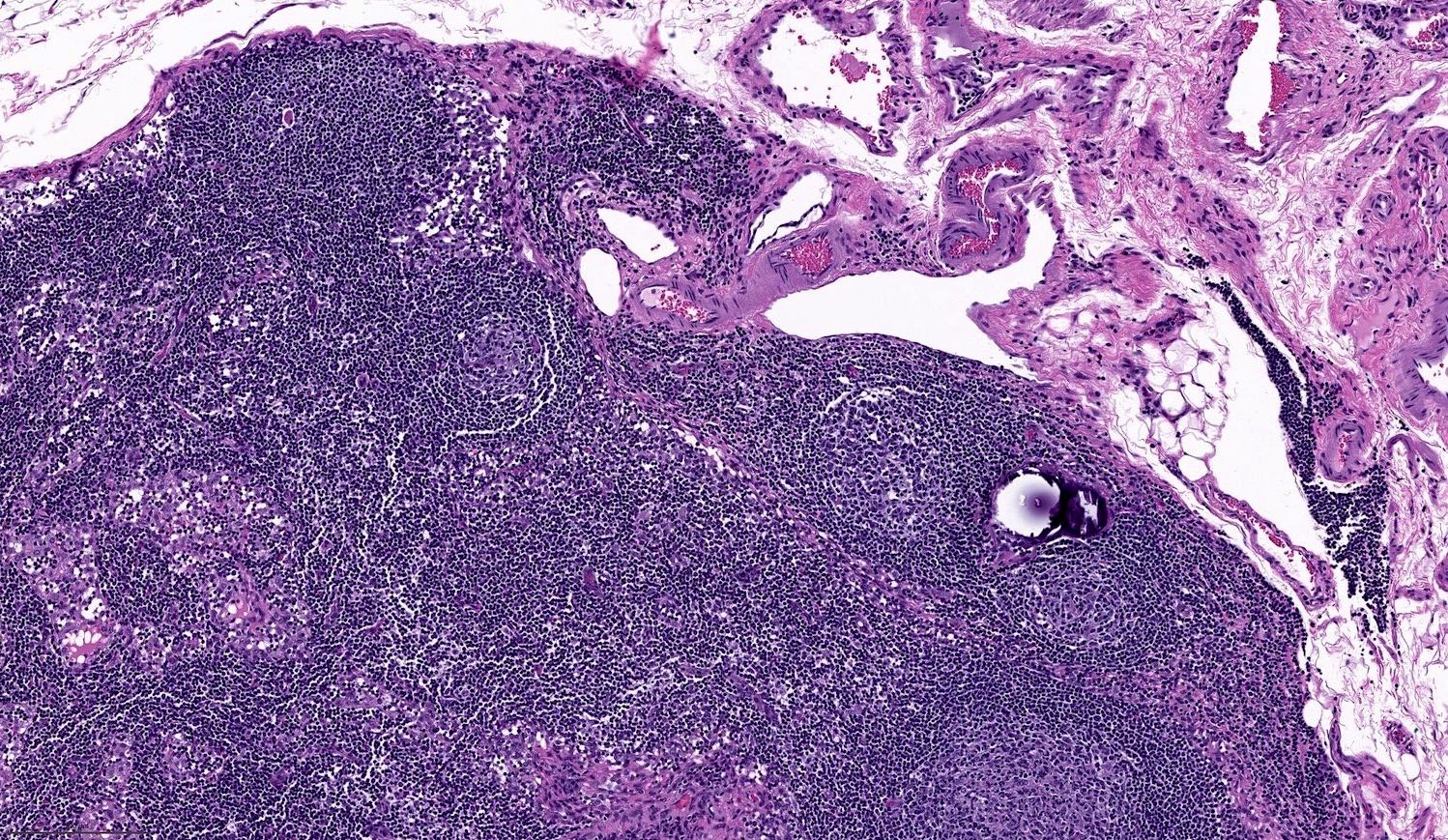
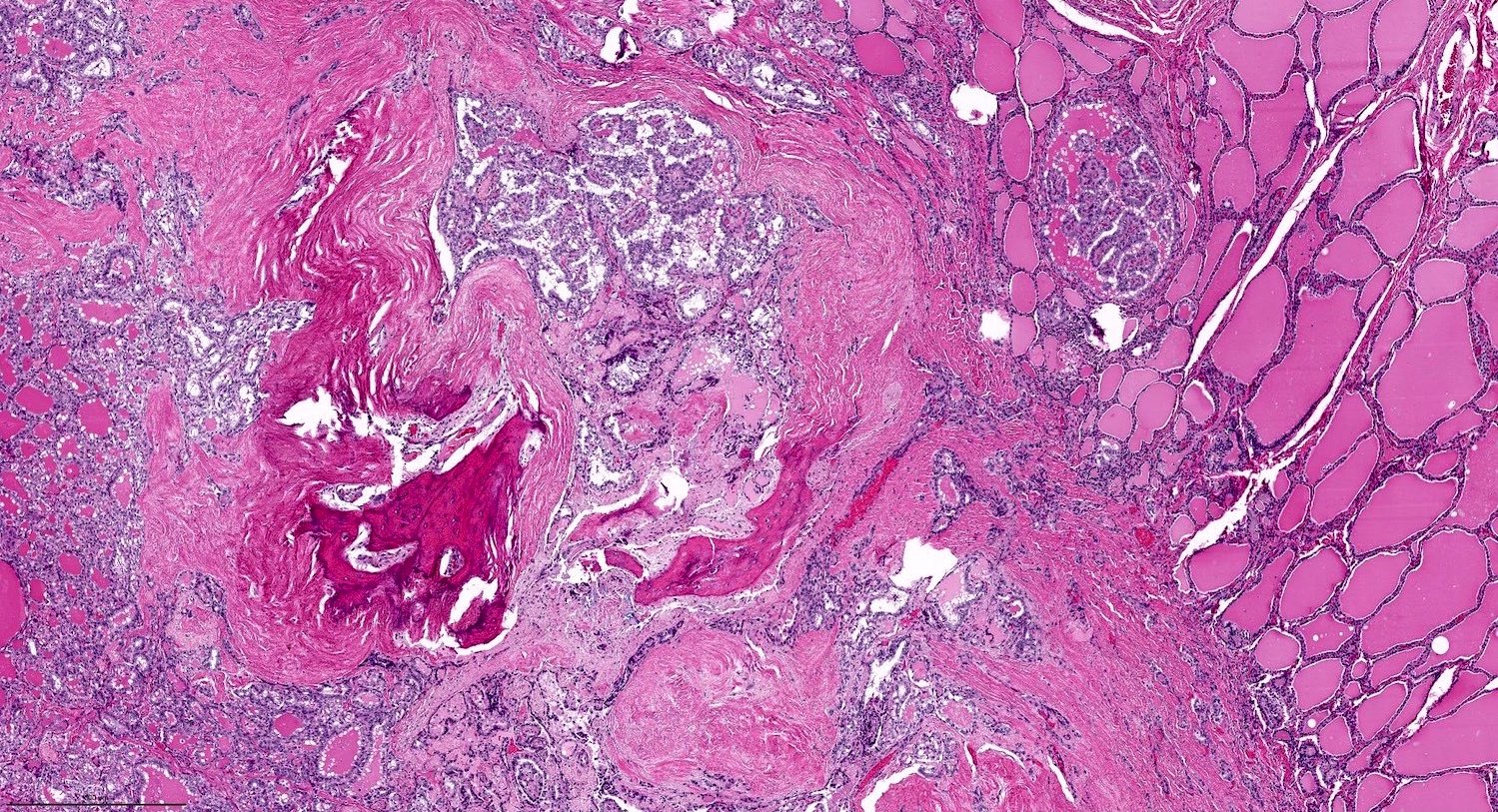
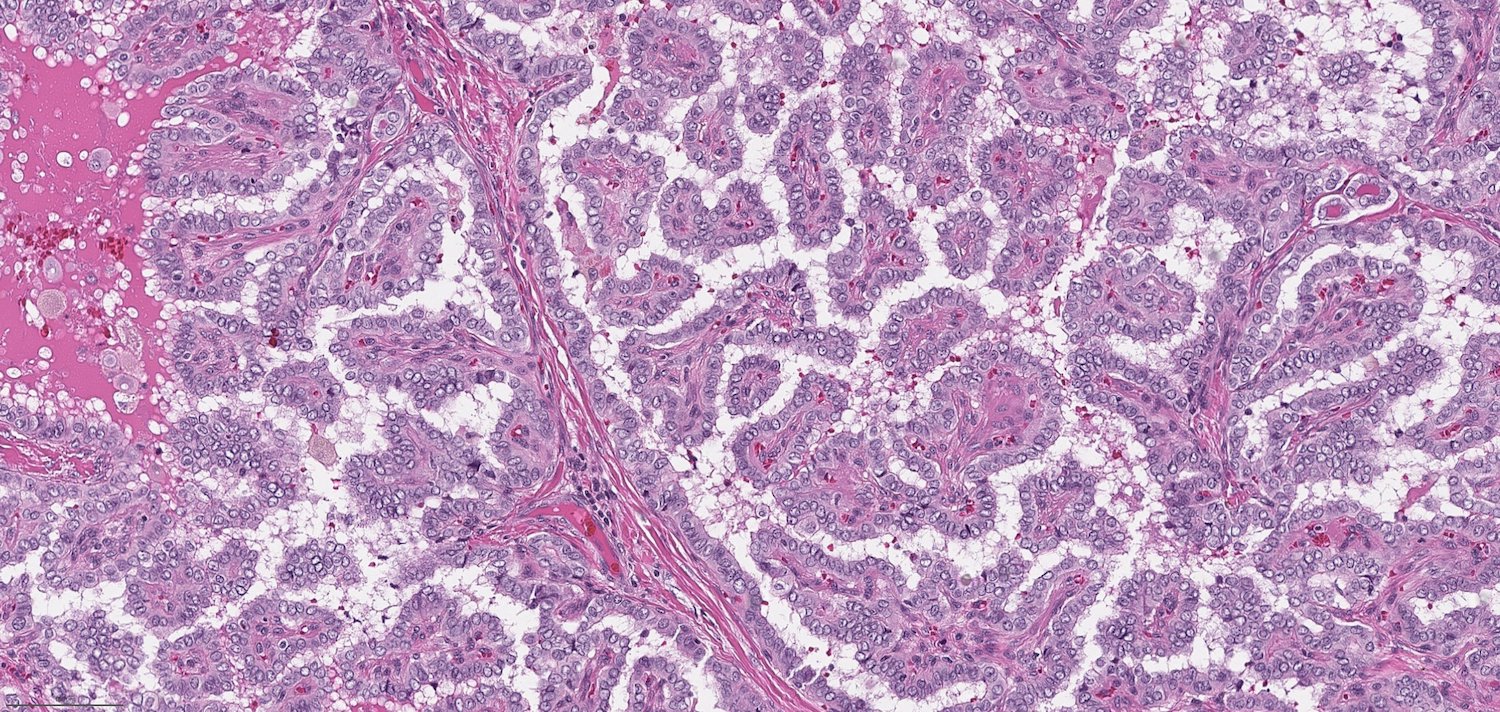
Microscopic (histologic) description
- Characterized by 2 cardinal features:
- The presence of true papillae defined as finger-like projection with a fibrovascular core
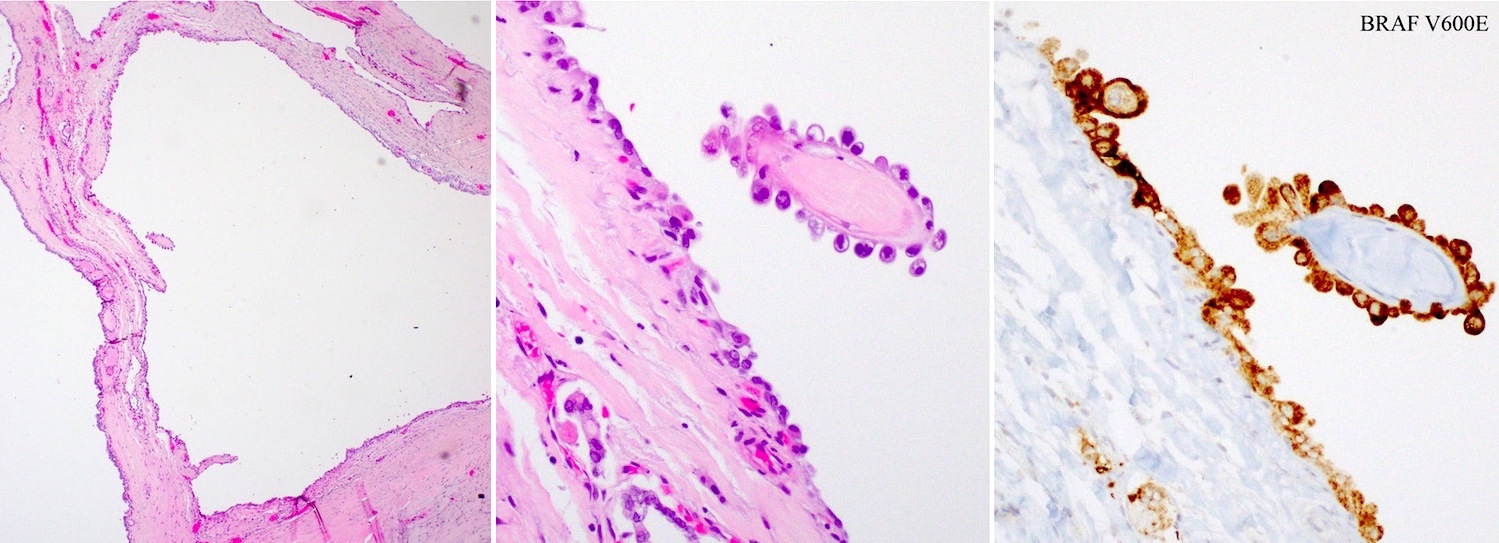
- The lining cells show nuclear features of papillary carcinoma, defined as 1) nuclear enlargement, 2) nuclear membrane irregularity and 3) chromatin clearing
- Lack diagnostic features of other aggressive variants (e.g., tall cell variant, columnar variant and hobnail variant)
- Other histologic findings that may be present include:
- Psammoma bodies: laminated microcalcification, common in classic variant
- Prominent cystic degeneration / cystic change
- Ossification or dystrophic calcification
Microscopic (histologic) images
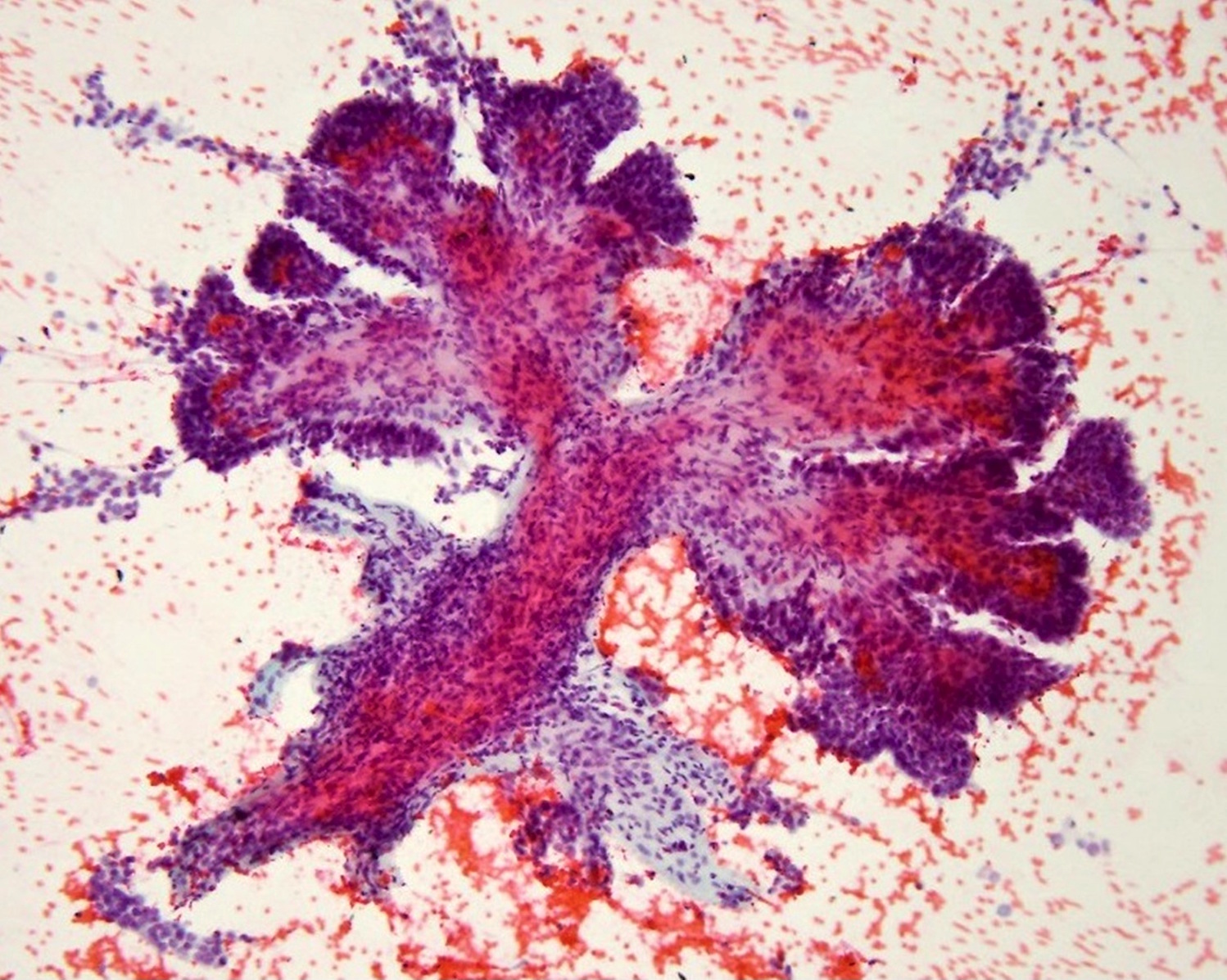
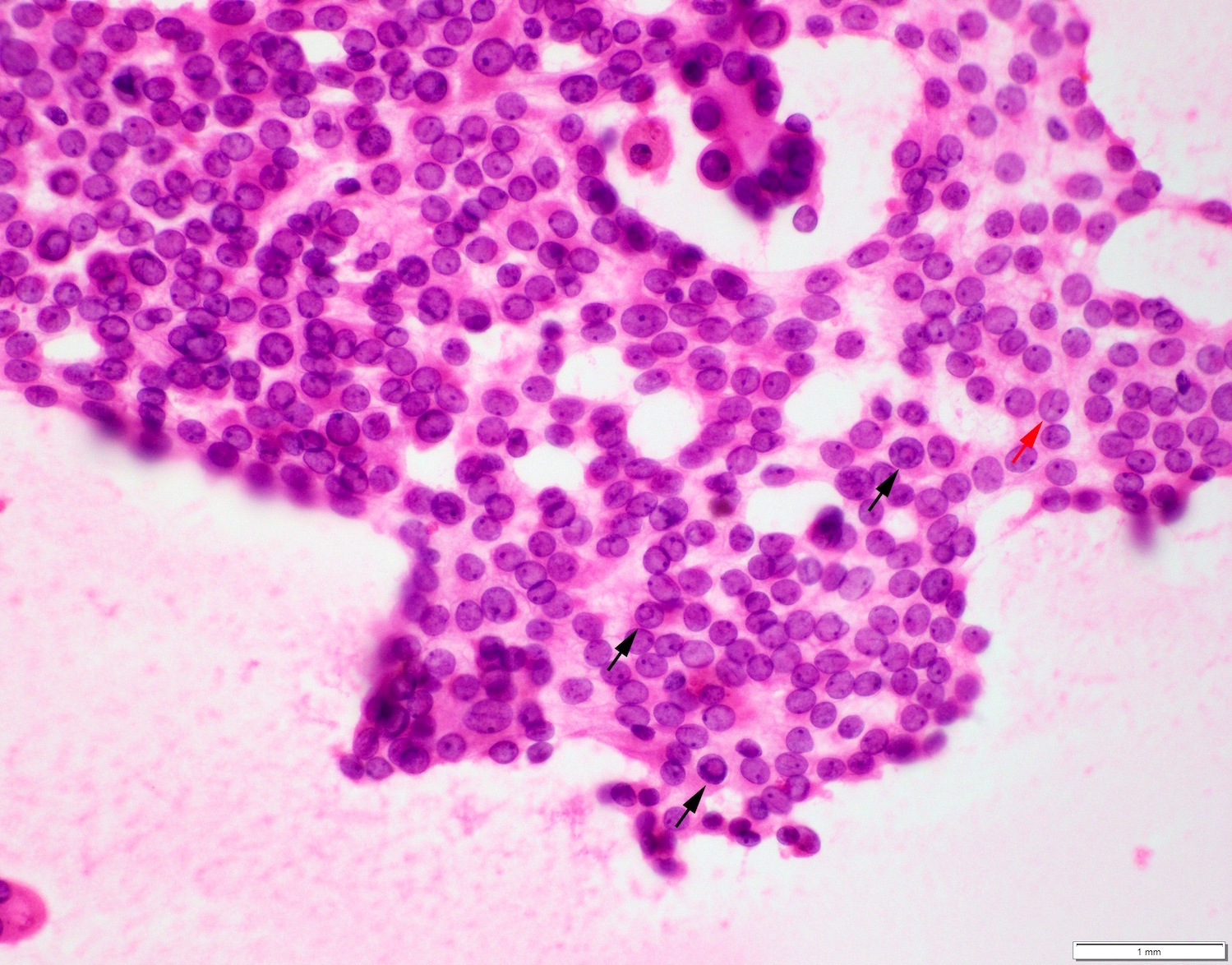
Cytology description
- Cytology sample shows nuclear features of papillary thyroid carcinoma: oval nuclei, nuclear overlapping, nuclear membrane irregularity, powdery chromatin, chromatin margination, nuclear grooves and nuclear pseudoinclusions
- In classic variant, large papillary projections may be seen in cytology samples
Positive stains
- Thyroid follicular cell lineage markers: TTF1, thyroglobulin and PAX8
- Mutation specific protein: BRAF V600E (VE1 antibody) (Thyroid 2019;29:1792, J Clin Endocrinol Metab 2013;98:E1414)
Negative stains
Molecular / cytogenetics description
- 50 - 77% harbor BRAF mutation, in particular BRAF V600E (J Clin Endocrinol Metab 2014;99:E276, Cell 2014;159:676)
- Absence or low frequency (6.3%) of RAS mutation (J Clin Endocrinol Metab 2014;99:E276, Cell 2014;159:676)
- 8% with RET-PTC rearrangement (Cell 2014;159:676)
- Other rare fusions in classic variant include: NTRK3 fusion in 2%, NTRK1 fusion in 1.4%, ALK fusion in 1.1% and PAX8-PPARgamma fusion in 0.8% (Cell 2014;159:676)
- TERT promoter mutation is rare; present in < 1% of cases
Sample pathology report
- Thyroid, left lobe and isthmus, left hemithyroidectomy:
- Papillary carcinoma, classic type, 2.3 cm (see synoptic report)
Differential diagnosis
- Papillary foci of Graves disease or other papillary hyperplasia
- May have abundant papillary infoldings and the cytoplasm may be tall or columnar
- However, the nuclei are small and round and lack nuclear clearing
- Medullary thyroid carcinoma, papillary variant
- May occasionally contain true papillary architecture (so called papillary variant)
- Lesional cells show nuclear features of neuroendocrine tumors with salt and pepper nuclei
- Positive for calcitonin, synaptophysin and chromogranin
Practice question #1
Practice answer #1
A. BRAF V600E mutation. This is papillary thyroid carcinoma, classic type.
Comment Here
Reference: Classic papillary thyroid carcinoma
Comment Here
Reference: Classic papillary thyroid carcinoma
Practice question #2
Which of the following histologic findings is a feature of classic type of papillary thyroid carcinoma?
- Composed entirely of follicles
- Nuclei of the lesional cells are small and round without nuclear membrane irregularity
- Contains well formed papillae with a fibrovascular core
- Lesional cells have a cell height at least 2 - 3 times of the cell width
Practice answer #2
C. Contains well formed papillae with a fibrovascular core
Comment Here
Reference: Classic papillary thyroid carcinoma
Comment Here
Reference: Classic papillary thyroid carcinoma