Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Huvila J, Gilks CB. Lichen sclerosus. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/vulvalichensclerosus.html. Accessed September 4th, 2025.
Definition / general
- Immune mediated chronic fibroinflammatory condition of vulvar skin
- Most commonly postmenopausal at onset; rarely can occur in children
Essential features
- Lichenoid interface inflammatory reaction
- Hyalinization and homogenization of the superficial dermal collagen with displacement of inflammatory cells downward, below the abnormal collagen layer
- Epidermis is usually thin (atrophic)
Terminology
- Lichen sclerosus et atrophicus
- Alternative spelling: lichen sclerosis
Epidemiology
- Typically seen in postmenopausal women (Climacteric 2017;20:339)
- Associated with other autoimmune disorders (J Eur Acad Dermatol Venereol 2010;24:1031)
Sites
- Vulvar skin
- Can involve perianal skin
- Typically does not involve vaginal mucosa but focal extension from vulvar skin onto the adjacent mucosa may be seen
Pathophysiology
- Cell mediated immune response with associated degenerative changes of the basal keratinocytes
- Secondary fibrosis of the superficial dermis, leading to a subepithelial hypocellular band of homogenous appearing collagen
Etiology
- Autoimmune (Int J Biol Sci 2019;15:1429)
- May be familial (J Eur Acad Dermatol Venereol 2010;24:1031)
Clinical features
- Intensely pruritic
- May become excoriated
- Associated with increased risk of developing human papillomavirus (HPV) independent vulvar intraepithelial neoplasia (VIN) and squamous cell carcinoma (Int J Cancer 2017;140:1998)
- Vulvar skin becomes thinned (cigarette paper appearance), with destruction of normal anatomic landmarks as the disease progresses
Diagnosis
- Characteristic clinical findings are highly suggestive but a biopsy can provide a definitive diagnosis if there is diagnostic uncertainty and also rule out neoplasia (e.g., VIN or Paget disease)
Prognostic factors
- Early diagnosis and treatment may prevent disease progression
Case reports
- 44 year old woman with bullous lichen sclerosus (Dermatol Online J 2018;24:13030)
- 50 year old woman with lichen sclerosus undergoing treatment with nivolumab (Dermatol Online J 2020;26:13030)
- 60 and 61 year old women with lichen sclerosus with vaginal involvement (Facts Views Vis Obgyn 2017;9:171)
- 66 year old woman with lichen sclerosus after treatment for vulvar squamous cell carcinoma (Gynecol Oncol Rep 2017;20:73)
Treatment
- Topical corticosteroids (first line), with topical calcineurin inhibitor therapy as second line (Am J Clin Dermatol 2013;14:27)
Clinical images
Gross description
- Diagnosis is made based on small biopsy specimens
- May be an incidental finding in a resection specimen (e.g., for vulvar squamous cell carcinoma)
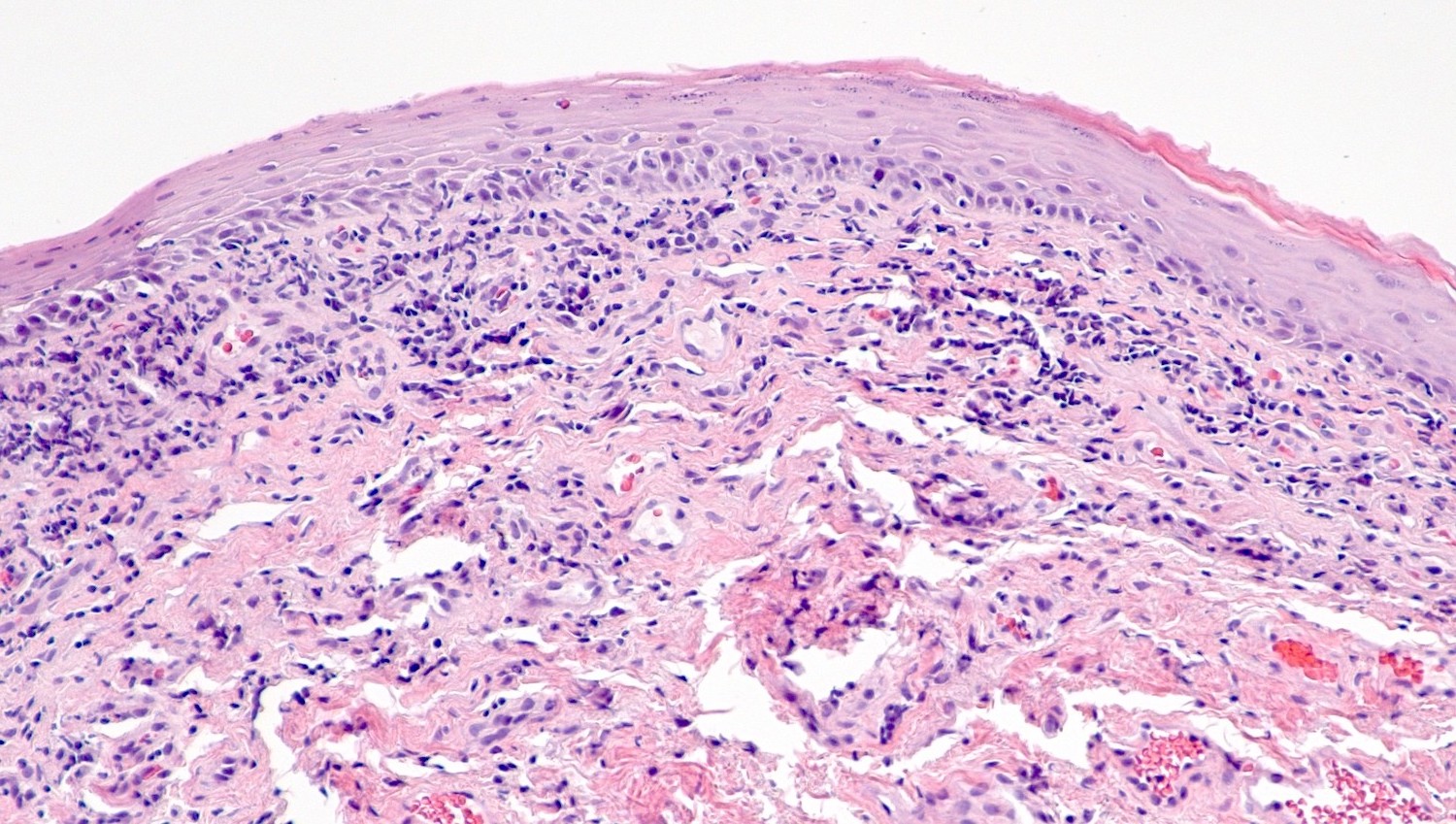
Microscopic (histologic) description
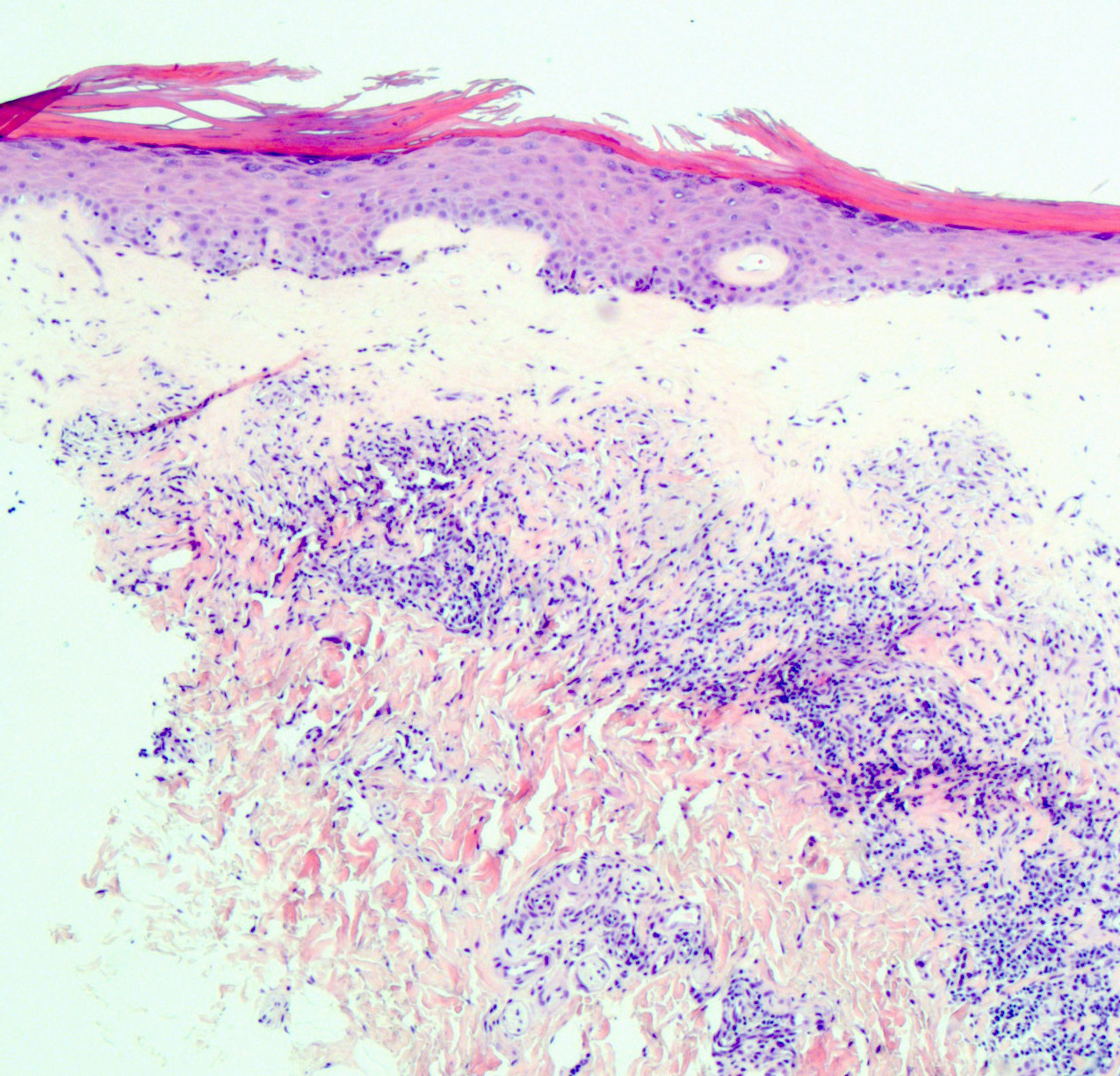
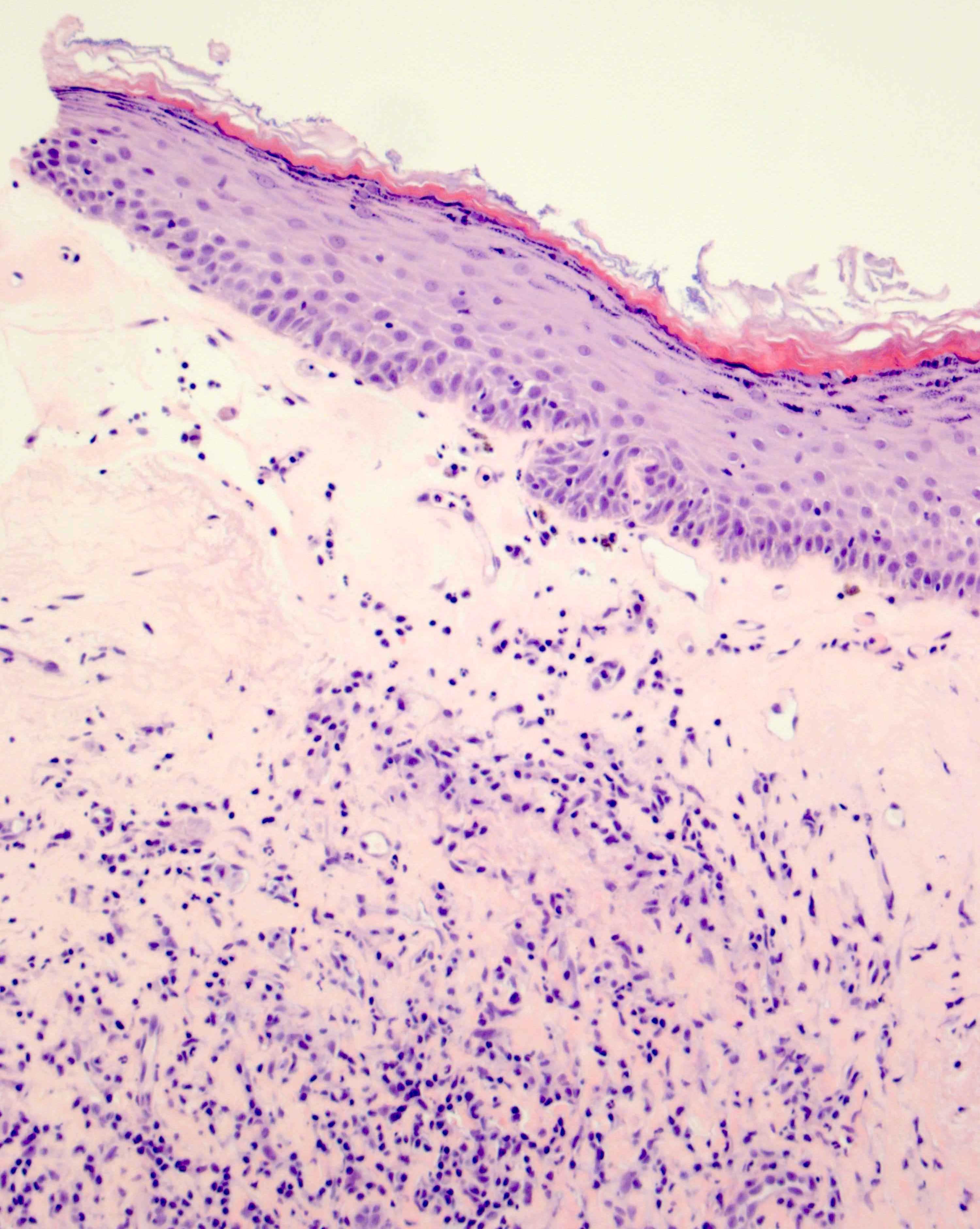
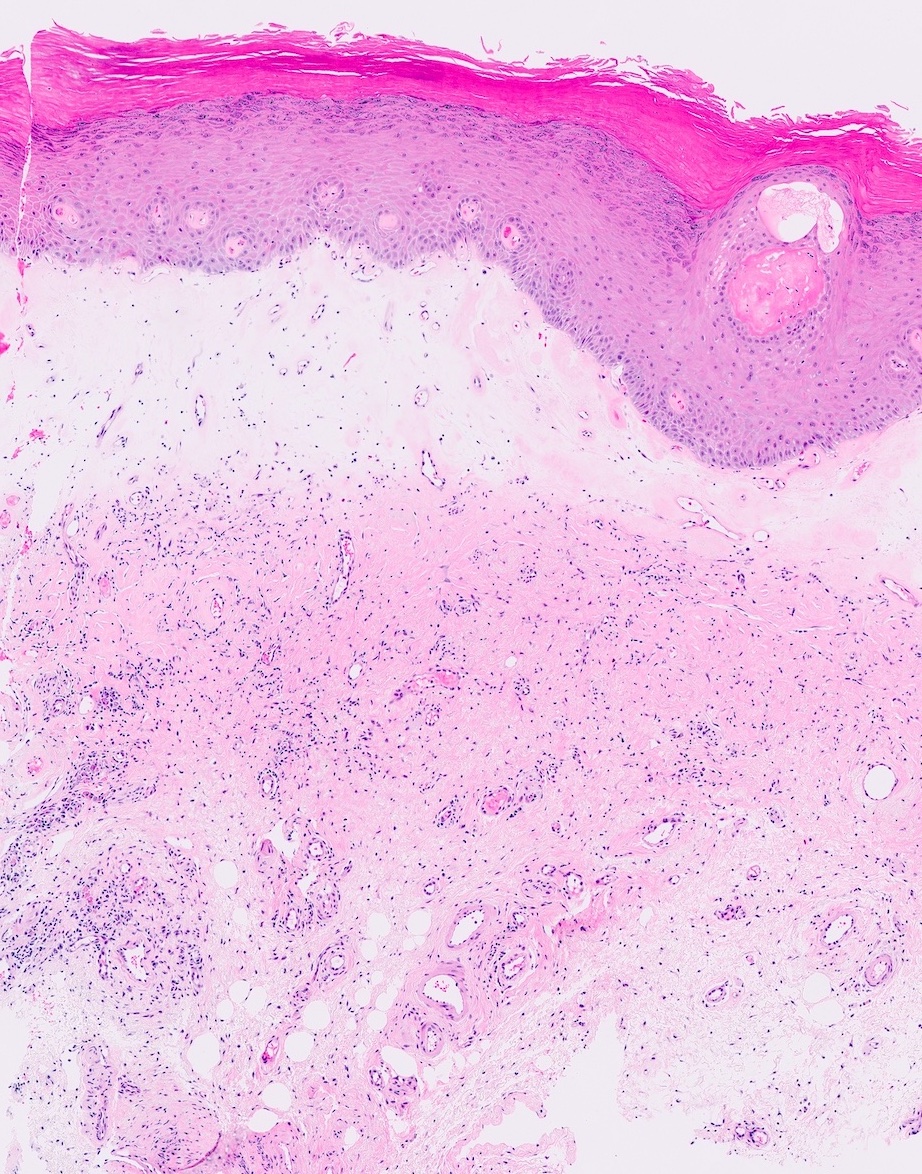
- Vacuolar interface reaction pattern in conjunction with dermal sclerosis (homogenized and hyalinized eosinophilic collagen bundles) of any thickness intervening between inflammatory infiltrate and epithelium or vessel walls (Mod Pathol 1998;11:844)
- Early lesions show only the inflammation and no or minimal fibrosis (inflammatory phase); the histopathological findings at this stage of disease development are not diagnostic
- Severe hyperkeratosis; thin epidermis, loss of rete pegs, basal cell degeneration, homogenized band of dense fibrosis at papillary dermis, upper dermal edema, band-like chronic inflammation
- In early stages, findings are subtle and often more prominent in adnexal structures than in interfollicular skin; adnexal structures show acanthosis, luminal hyperkeratosis and hypergranulosis
- Early dermal changes are homogenized collagen and wide ectatic capillaries in dermal papillae immediately beneath basement membrane
- Superficial dermal collagen may be wire-like with lymphocyte entrapment (J Cutan Pathol 2015;42:510)
- Lymphocytic infiltrate can be sparse or dense, lichenoid or interstitial with epidermal lymphocyte exocytosis
- Erosions or ulceration can occur (J Low Genit Tract Dis 2021;25:255)
Microscopic (histologic) images
Negative stains
- Wild type pattern staining for p53
Videos
Introduction to lichen sclerosus
Sample pathology report
- Right labium majus, biopsy:
- Lichen sclerosus (see comment)
- Comment: This vulvar biopsy shows established lichen sclerosus. Negative for dysplasia or malignancy.
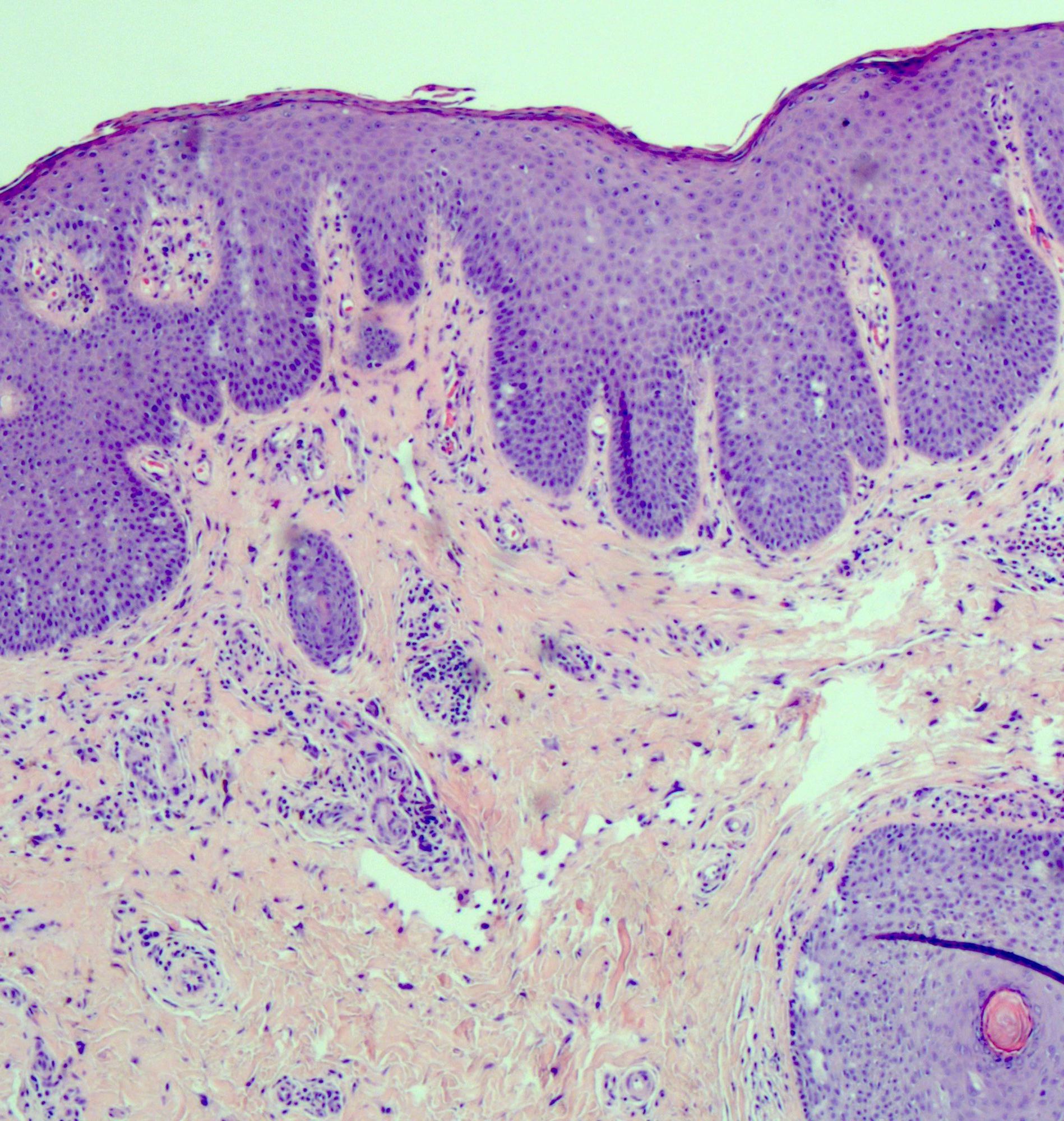
Differential diagnosis
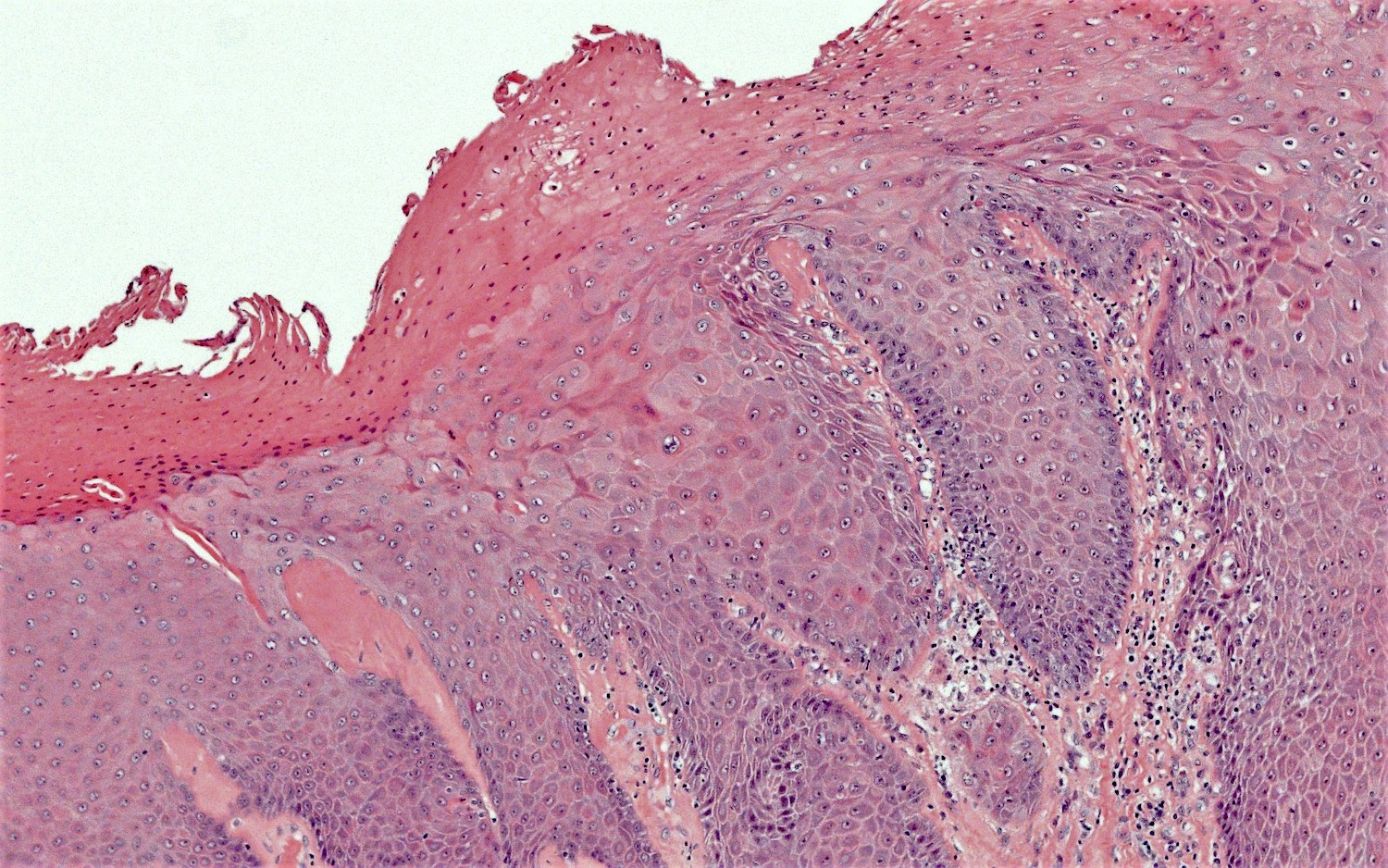
- HPV independent vulvar intraepithelial neoplasia (VIN):
- Other terminology: differentiated VIN (dVIN), differentiated exophytic vulvar intraepithelial lesion (DEVIL), vulvar acanthosis with altered differentiation (VAAD), vulvar altered maturation (VAM)
- Shows epithelial hyperplasia and loss of normal maturation; often shows significant basal atypia and may show mutant pattern p53 immunostaining (Mod Pathol 2011;24:297)
- Lichen planus:
- Clinically, the presence of erosions, oral involvement, a burning sensation or a hyperkeratotic lesional margin favor a diagnosis of lichen planus over lichen sclerosus (Australas J Dermatol 2020;61:324)
- Typically involves mucosa or nonhair bearing skin
- Subepithelial band-like inflammatory infiltrate is directly under the squamous epithelium, without a separating area of fibrosis / sclerosis
- Pointed rete ridges are more common in lichen planus, while the presence of epidermal atrophy or basal lamina thickening favor lichen sclerosus (Am J Surg Pathol 1998;22:473)
- Early lesions of lichen sclerosus, before the fibrosis becomes established, can be difficult or impossible to distinguish from lichen planus; such cases can be signed out descriptively, indicating that follow up, with or without rebiopsy, should allow for definitive diagnosis
- Lichen planus can coexist with lichen sclerosus (J Low Genit Tract Dis 2017;21:204)
- Lichen simplex chronicus:
- Common; spares the vaginal mucosa (Dermatol Clin 2010;28:669)
- Epidermal hyperplasia is present, rather than atrophic changes, with no degenerative changes of the basal epithelial layer and no superficial subepidermal sclerosis
- Excoriation is common and may lead to subepidermal scarring but with variably sized collagen bundles and not the homogenized sclerotic band of lichen sclerosis
- Spongiosis / spongiotic dermatitis may be present but is not necessary for diagnosis (Int J Womens Dermatol 2017;3:58)
- Hypergranulosis is common
Additional references
Practice question #1
Practice answer #1
Practice question #2
There is an association between lichen sclerosus of the vulva and
- High grade squamous intraepithelial lesion (HSIL / VIN3)
- Human papillomavirus (HPV) independent vulvar intraepithelial neoplasia (VIN)
- Lichen planus
- Psoriasis
Practice answer #2
B. Human papillomavirus (HPV) independent vulvar intraepithelial neoplasia (VIN)
Comment Here
Reference: Lichen sclerosus
Comment Here
Reference: Lichen sclerosus