Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Classification | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Immunohistochemistry & special stains | Molecular / cytogenetics description | Differential diagnosis | Additional referencesCite this page: Martinez A. Osteosarcoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mandiblemaxillaosteosarcoma.html. Accessed May 13th, 2024.
Definition / general
- Osteosarcoma (OS) is a malignant, high grade tumor of bone in which the tumor cells produce osteoid (bone)
Essential features
- Craniofacial osteosarcomas represent about 6.5% - 7% of all osteosarcomas
- Patients with osteosarcomas of the jaw are generally 10 to 20 years older than those with osteosarcomas of long bones
- Chondroblastic OS may be difficult to distinguish from chondrosarcoma due to sampling bias or OS that have large cartilaginous component
- The cartilaginous component of a chondroblastic OS is usually high grade
- Chondroblastic OS should be accompanied by osteoid production from the sarcomatous stromal cells
- Many chondrosarcomas have IDH1 and IDH2 mutations, whereas chondroblastic OS do not
- Low grade central osteosarcoma may demonstrate histologic overlap with benign fibro-osseous lesions
- Complete surgical resection with wide margins has been reported as the most significant prognostic factor
Terminology
- Osteosarcoma (OS)
- Osteogenic sarcoma
- Osteosarcoma of the jawbones
- Conventional osteosarcoma
- Chondroblastic osteosarcoma
- Osteoblastic osteosarcoma
- Secondary osteosarcoma
Epidemiology
- Most common nonhematopoietic bone malignancy
- Second most common bone malignancy after myeloma
- Conventional OS has a bimodal age distribution
- Most (~60%) seen in second decade
- Second peak after 50 years
- Usually in setting of radiation or other secondary causes such as Paget disease
- Craniofacial osteosarcomas represent about 6.5% - 7% of all osteosarcomas
- Conventional osteosarcomas are most common
- Approximately 25% of craniofacial OS are of the chondroblastic subtype
- Patients with osteosarcomas of the jaw are generally 10 to 20 years older than those with osteosarcomas of long bones
- Males are affected more frequently than females
Classification
2013 WHO Classification for osteosarcoma is as follows:
- Low grade central osteosarcoma
- Conventional osteosarcoma
- Osteoblastic
- Chondroblastic
- Fibroblastic
- Secondary
- Small cell osteosarcoma
- Telangiectatic osteosarcoma
- Parosteal osteosarcoma
- Periosteal osteosarcoma
Sites
- Mandibular tumors are more frequent in the posterior body and ramus
- Maxillary lesions are more common along the alveolar ridge, sinus floor and palate than the zygoma or orbital rim
- For other sites, please see osteosarcoma of long bones
Etiology
- It usually occurs de novo
- Primary osteosarcoma is associated with genetic syndromes
- Li-Fraumeni
- Hereditary retinoblastoma
- Rothmund-Thomson
- May also be associated with radiation therapy, Paget disease of bone or fibrous dysplasia
Clinical features
- Variable but can include pain, swelling, paresthesia and ulceration
Diagnosis
- Diagnosis dependent on clinical, radiologic and pathologic correlation
Radiology description
- Can show radiopaque, radiolucent or mixed appearances on plain radiographs
- May be destructive with permeative margins
- May break through cortex and elevate periosteum
- Sunburst pattern due to new bone formation in soft tissue
Prognostic factors
- Complete surgical resection with wide margins has been reported as the most significant prognostic factor
- 70% overall 5 year survival with surgery alone
- Better than extragnathic OS
- 70% overall 5 year survival with surgery alone
- ~50% of mandibular osteosarcomas recur locally after resection
- Recurrence rate is even higher with maxillary and skull lesions (80% and 75%, respectively)
- Metastases are less frequent than local recurrence and occur in about 1/3 of patients with craniofacial osteosarcomas
- Typically occur within 2 years of initial treatment
- Radiotherapy in addition to surgery improves overall survival, disease specific survival and local control in craniofacial osteosarcoma with positive / uncertain resection margins (Cancer 2009;115:3262)
Case reports
- 18 year old woman with a slow growing asymptomatic swelling in the left upper buccal vestibule for 2 months (J Maxillofac Oral Surg 2009;8:290)
- 20 year old man with pain and swelling in the left zygomatic region (J Oral Maxillofac Pathol 2014;18:281)
- 27 year old woman with facial asymmetry caused by the a swelling in the premaxillary region with upper lip protrusion (J Oral Maxillofac Pathol 2014;18:464)
- 27 year old woman with maxillary mass (Case of Week #350)
- 59 year old woman with osteosarcoma developing from fibrous dysplasia of the sphenoid bone (Head Neck Pathol 2015;9:100)
Treatment
- Radical surgery with adjuvant chemotherapy
- Radiation can be added if tumor cannot be fully removed surgically
Clinical images
Images hosted on other servers:
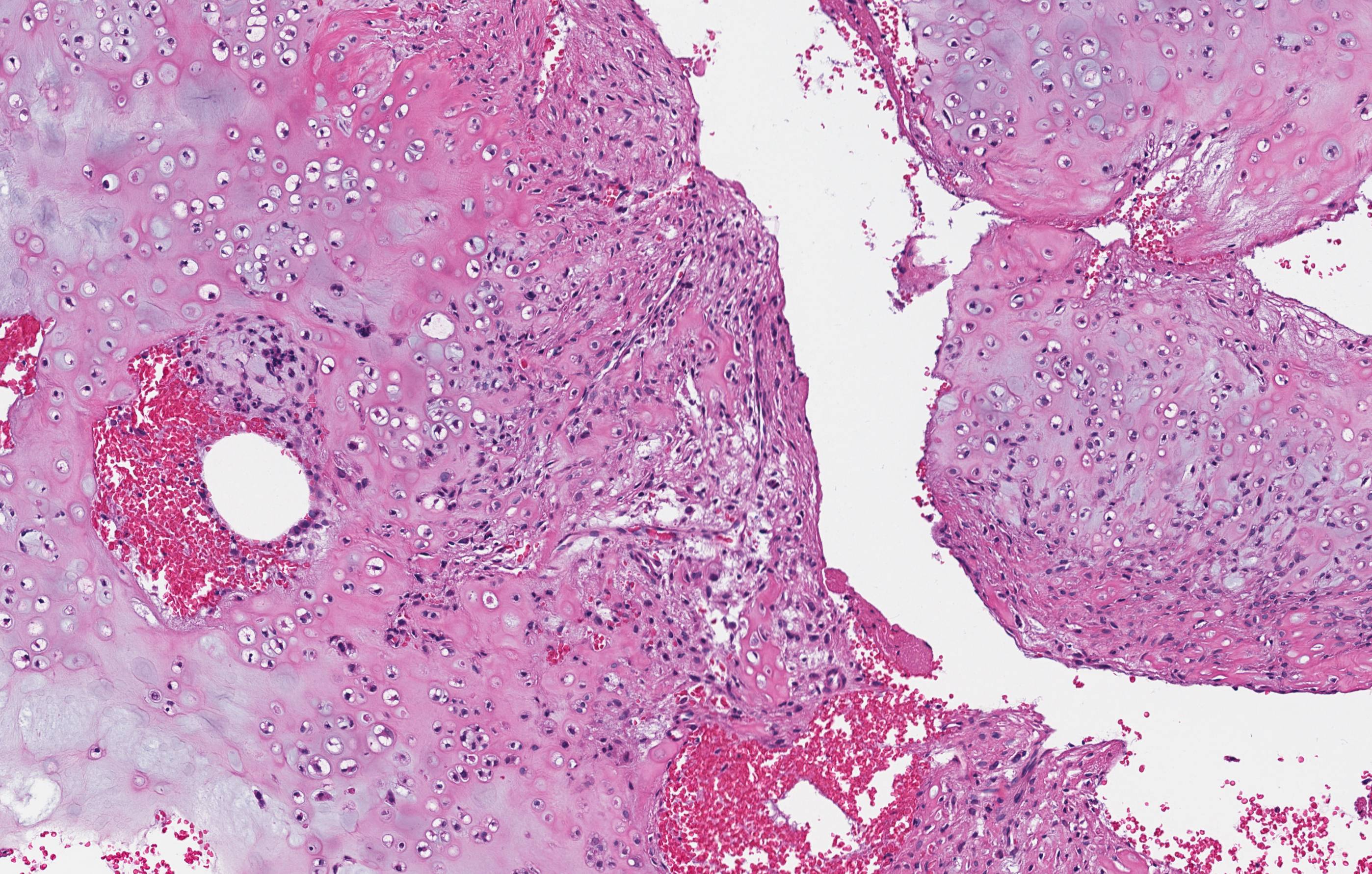
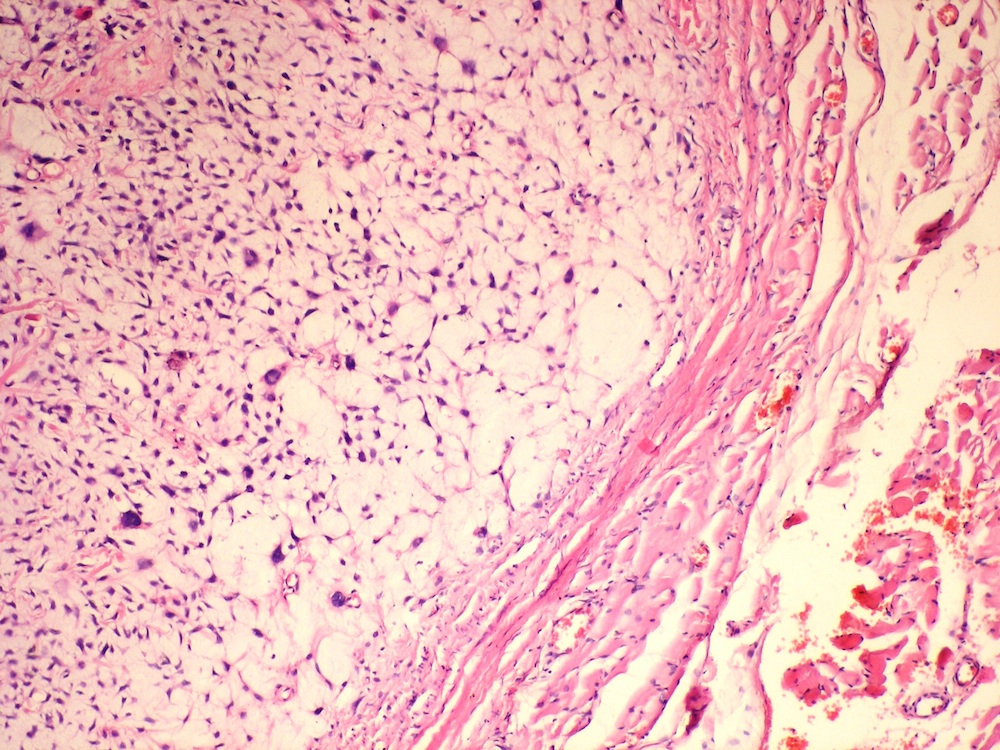
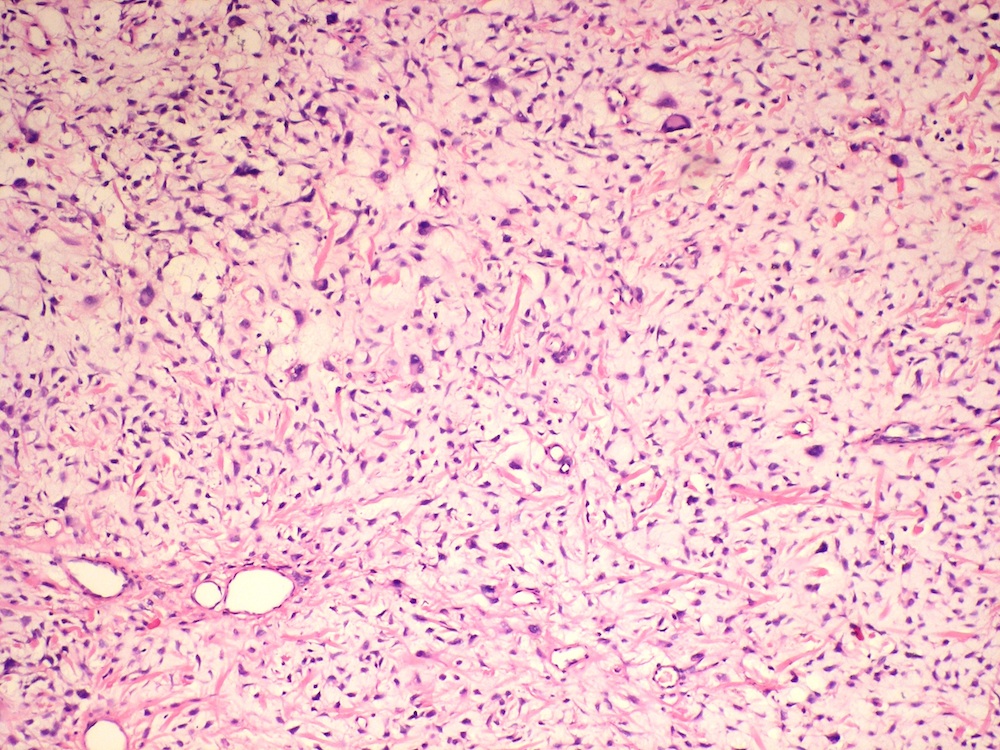
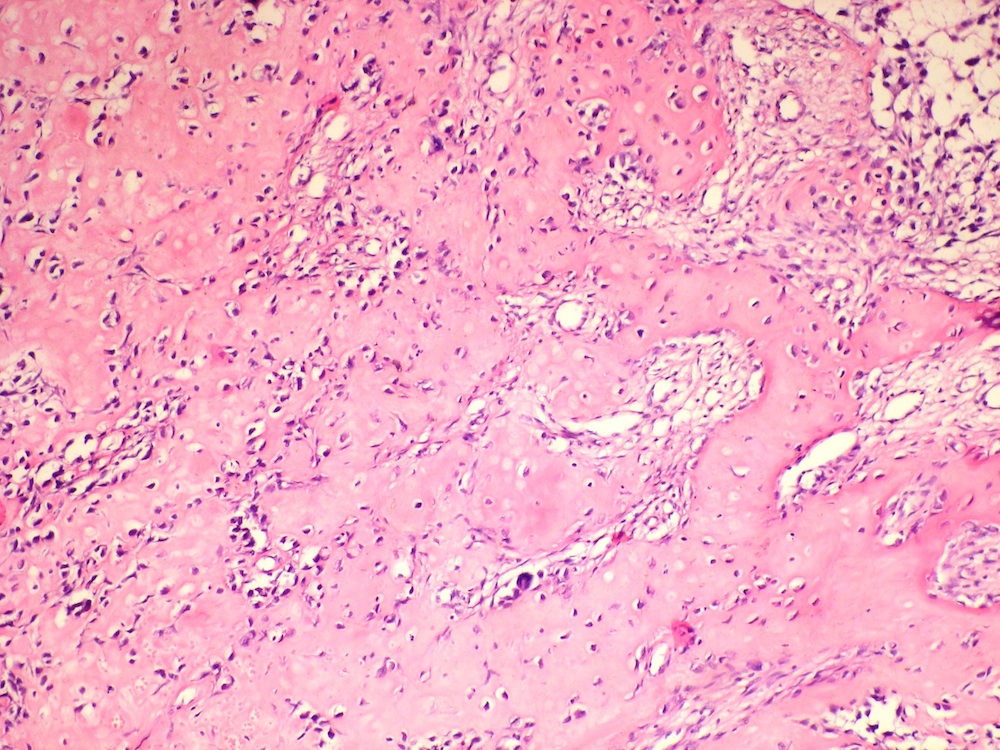
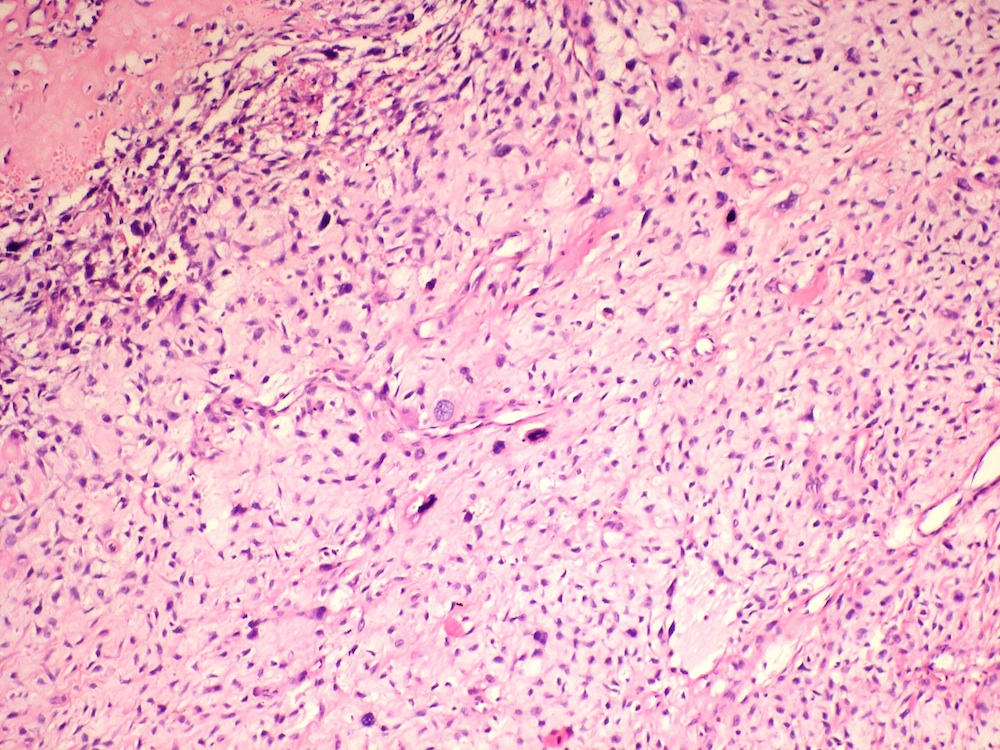
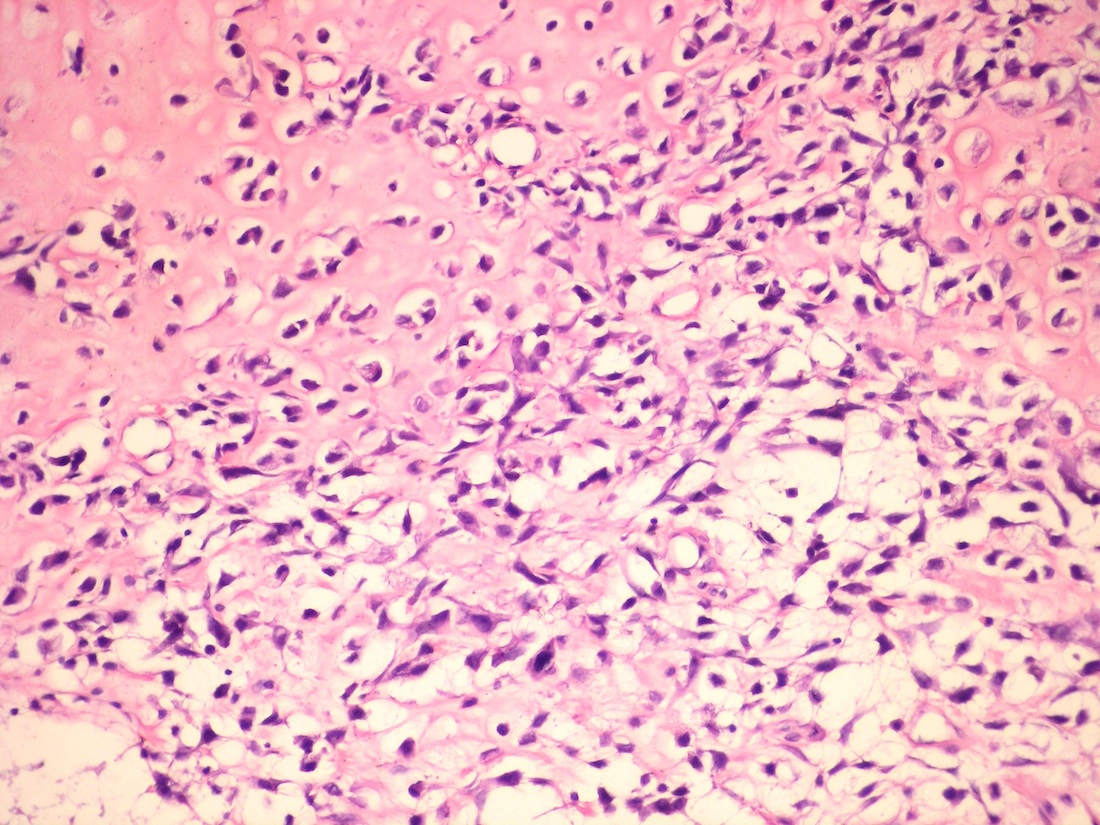
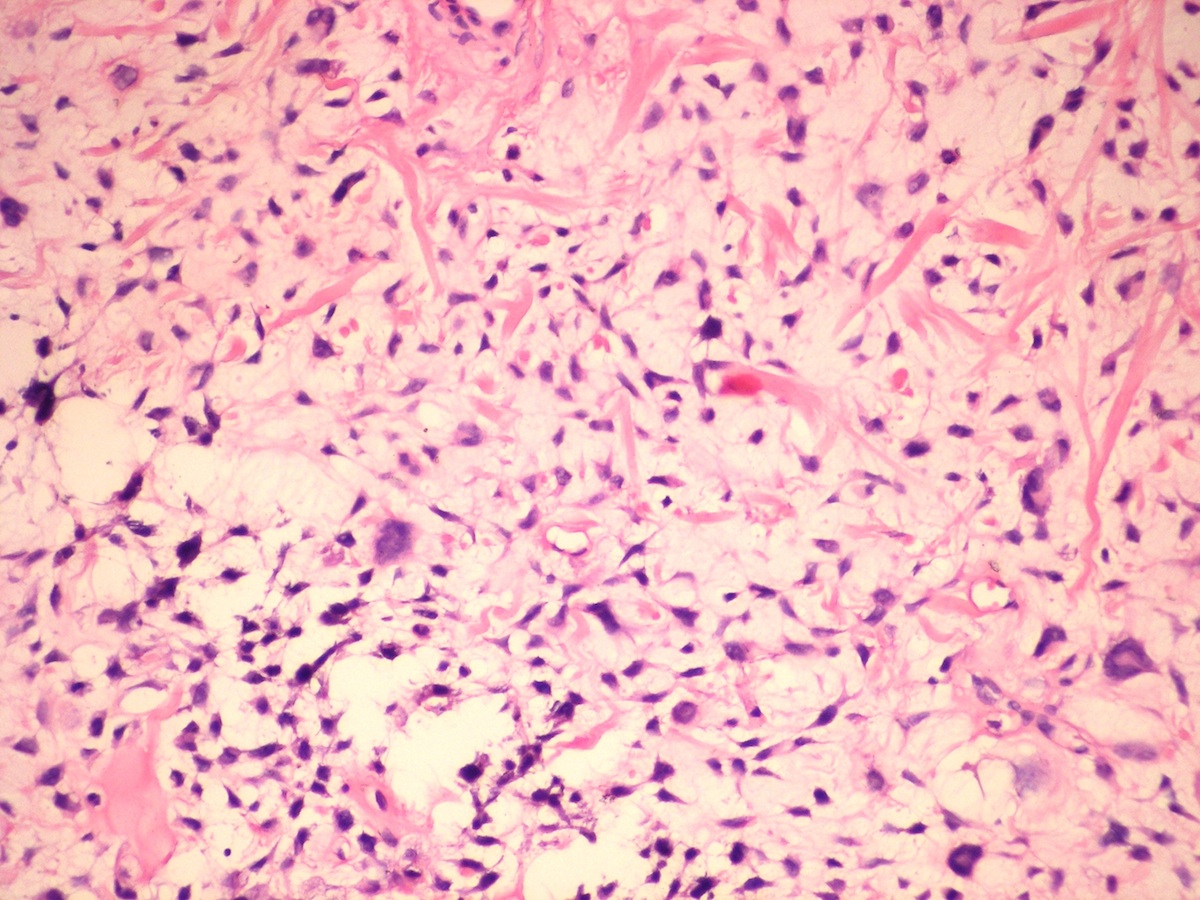
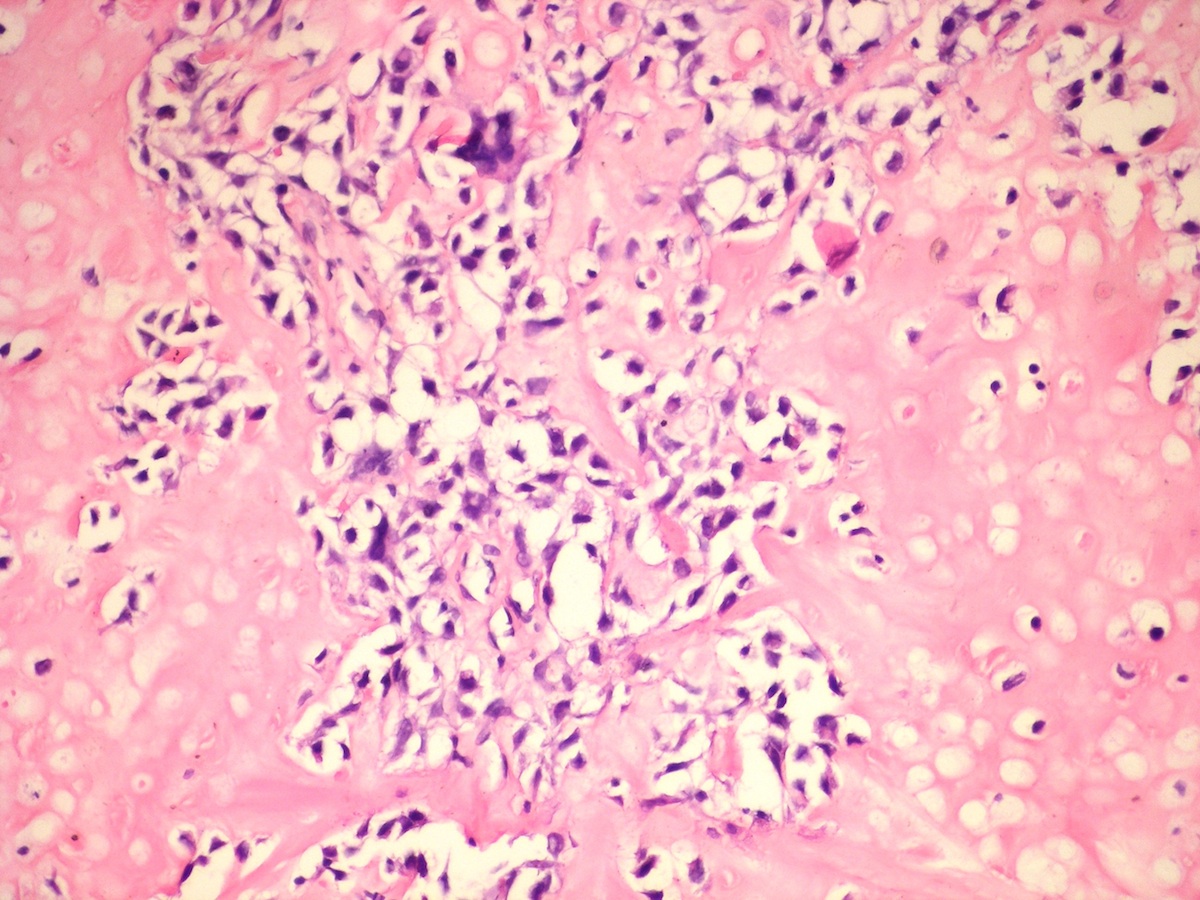
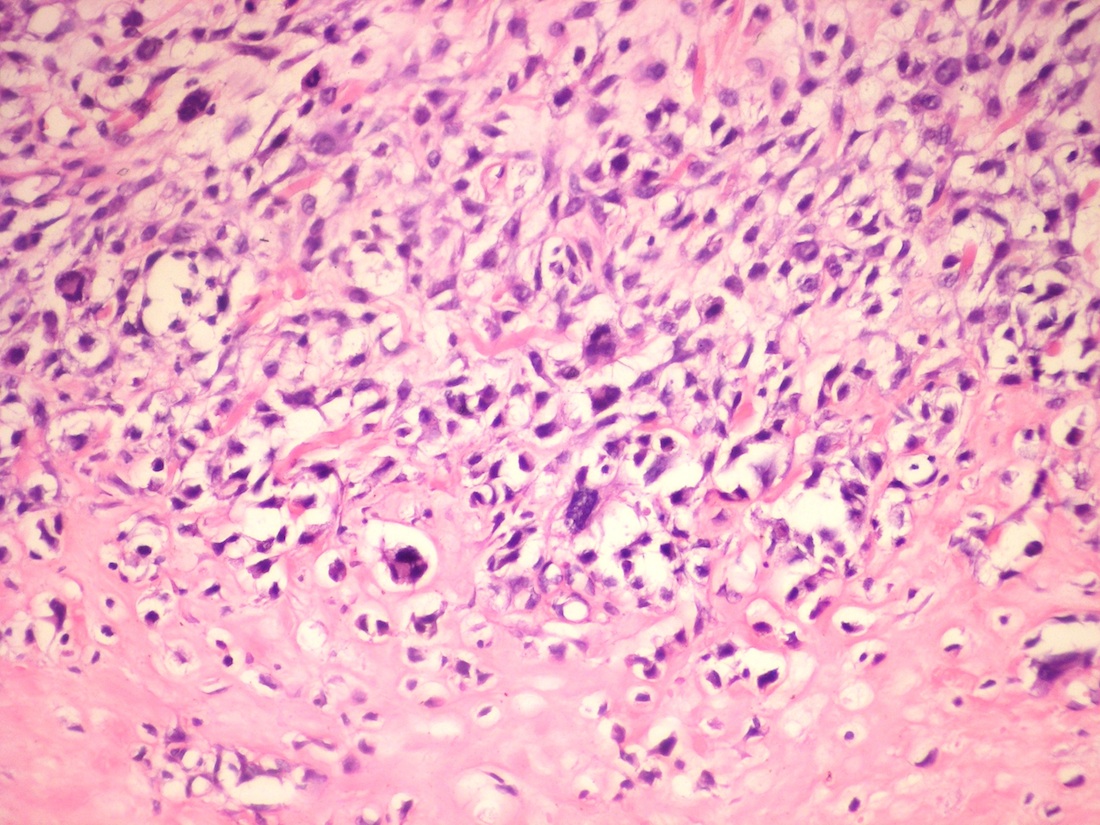
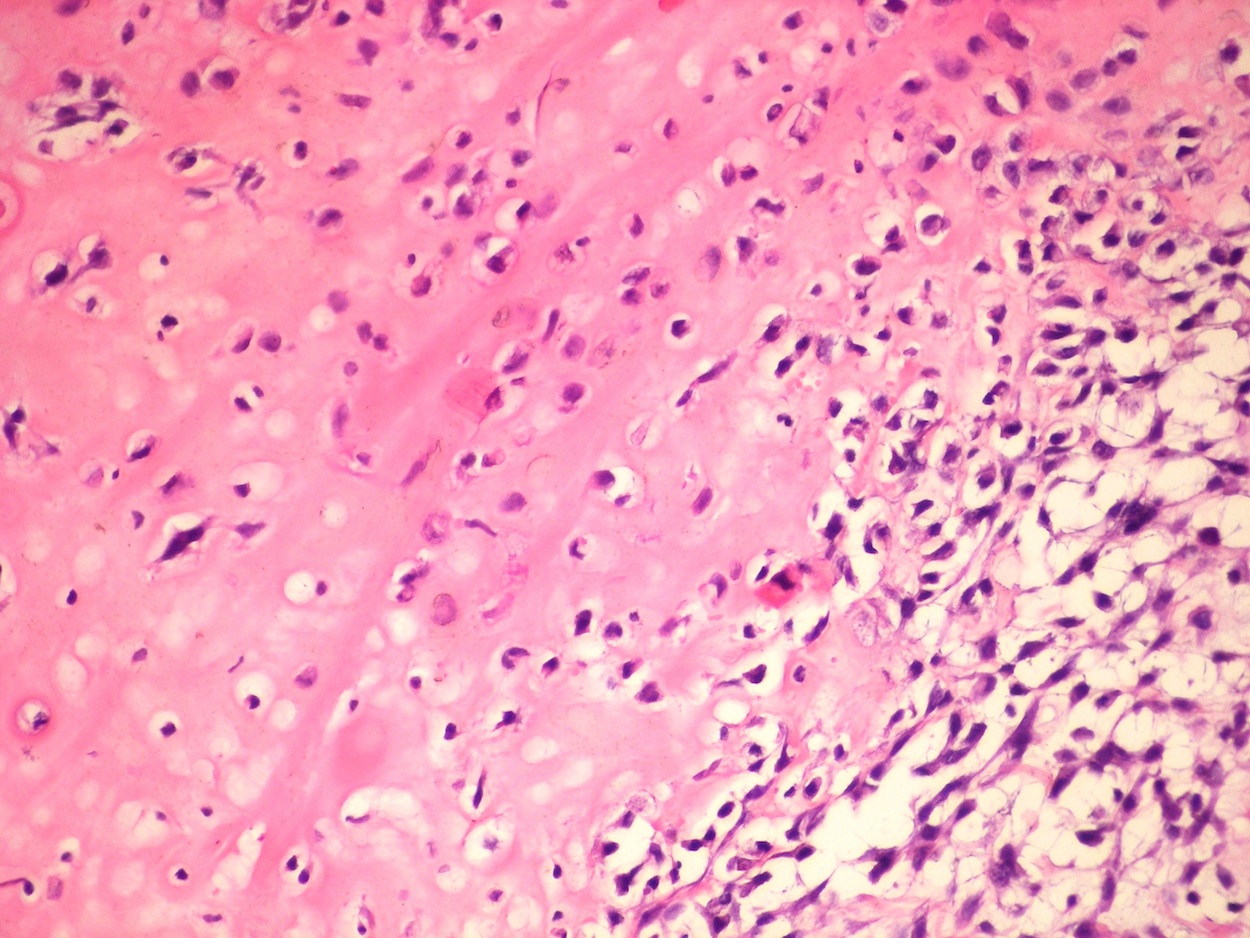
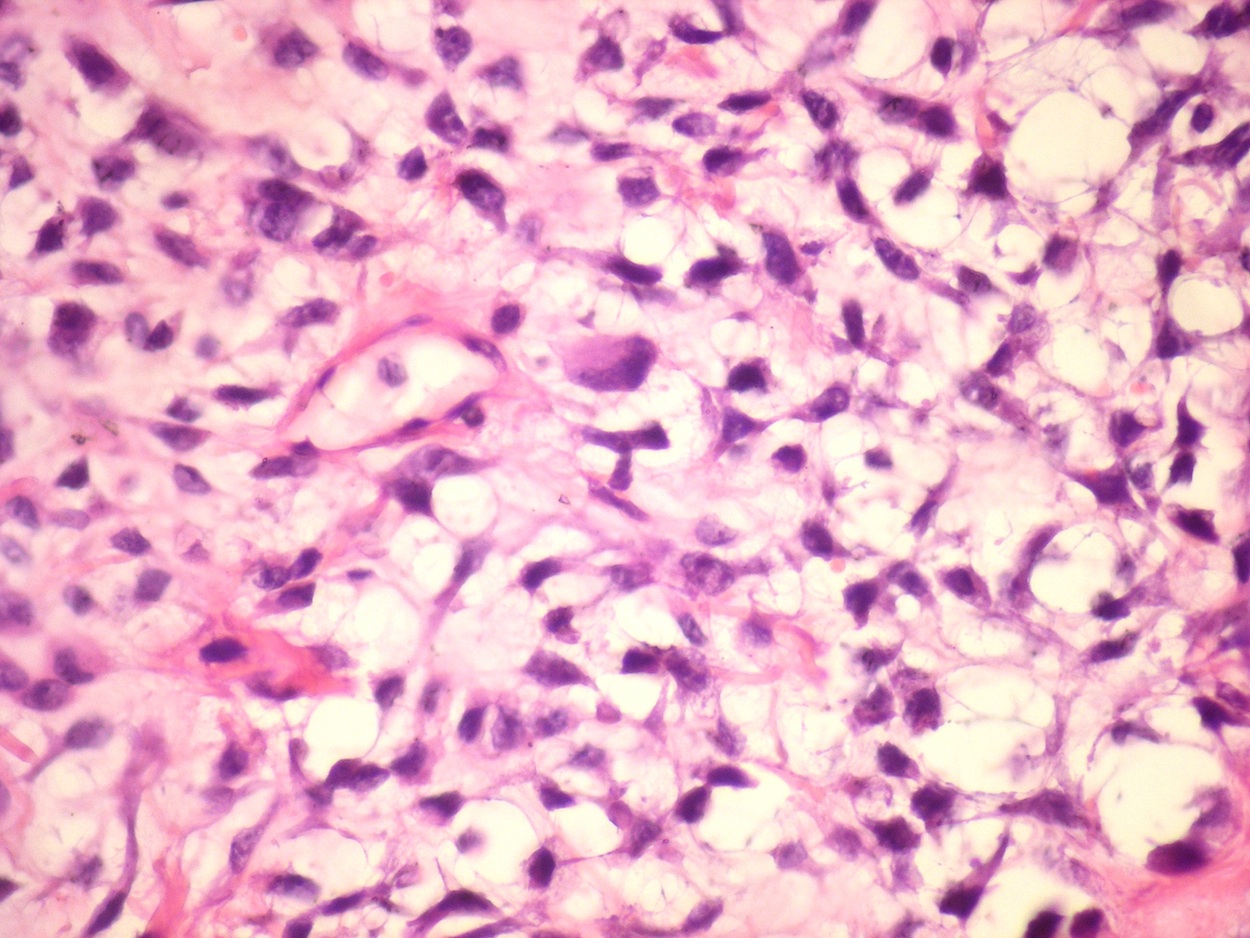
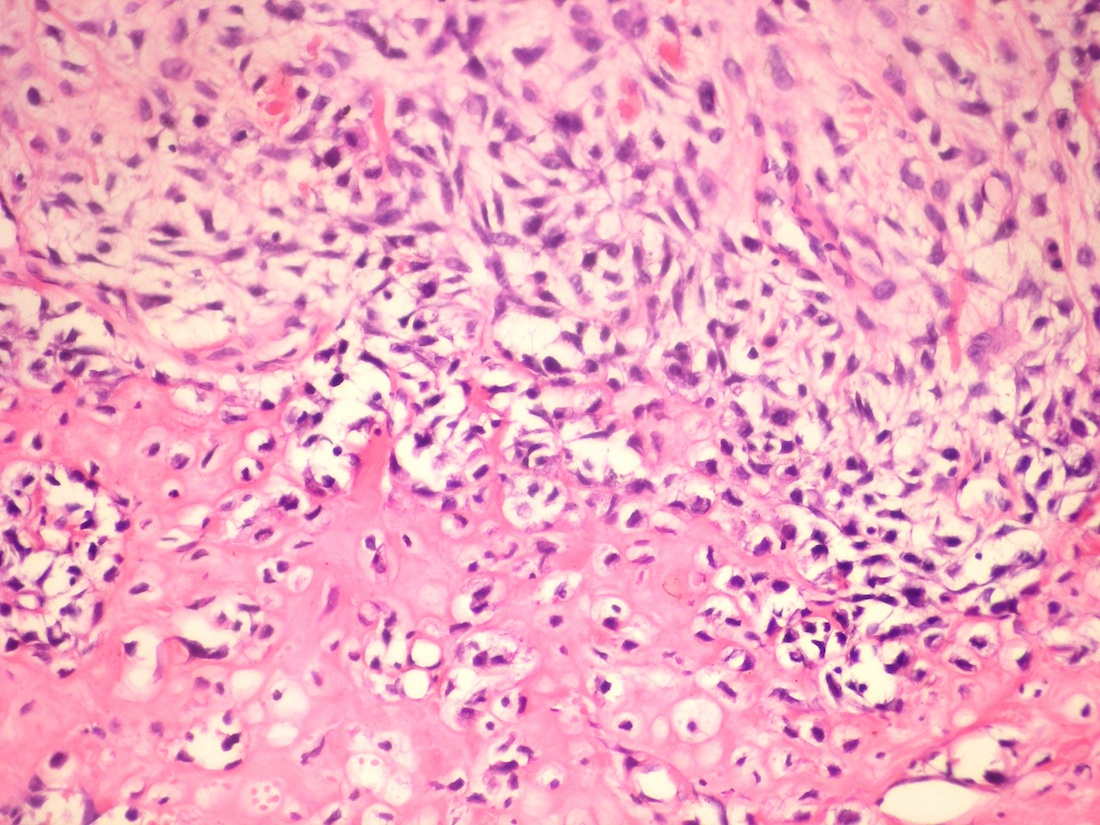
Microscopic (histologic) description
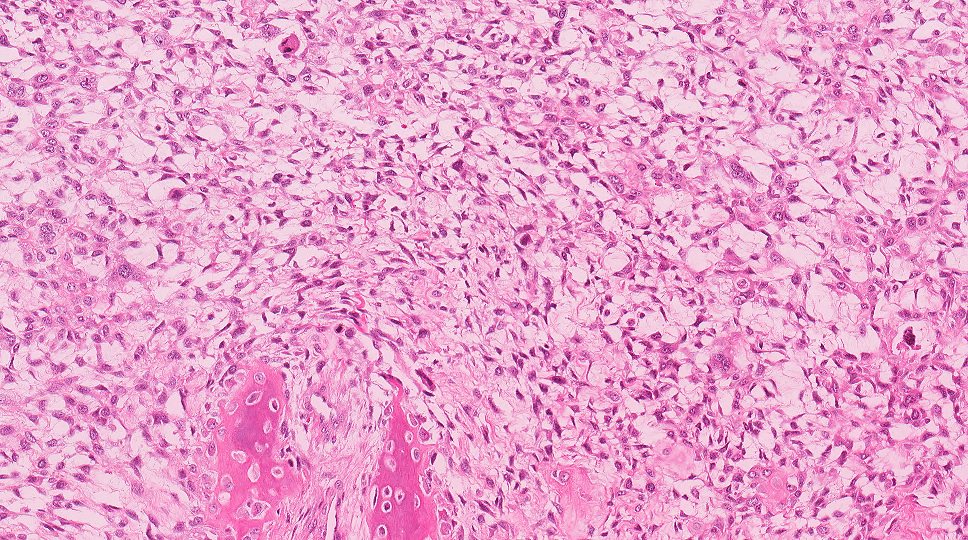
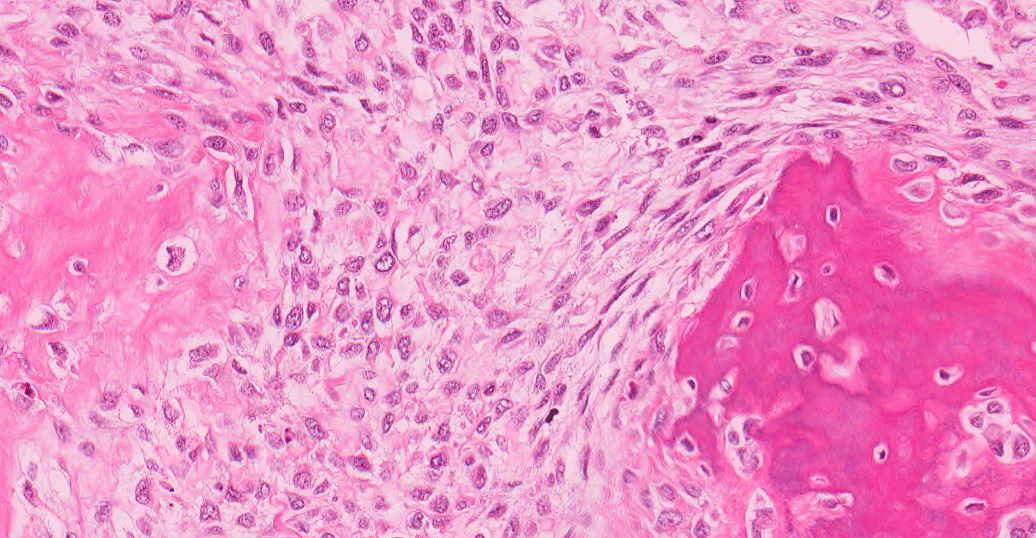
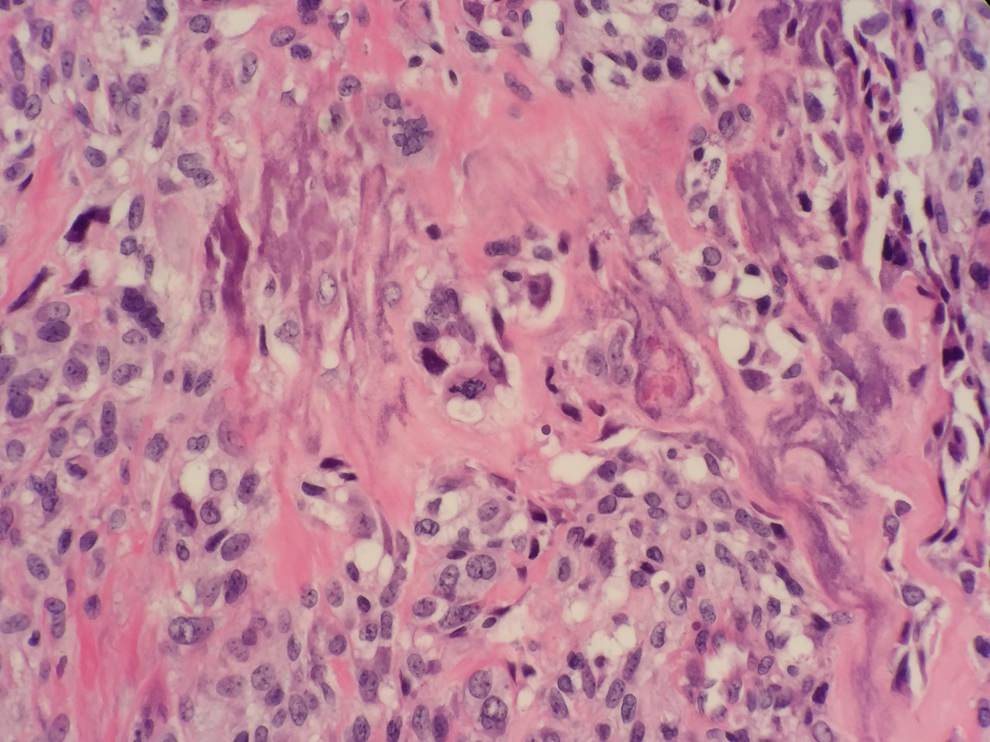
- Osteosarcomas are composed of sarcomatous tumor cells that produces malignant bone or osteoid
- The tumor cells may have densely eosinophilic cytoplasm resembling osteoblasts but often are larger than normal osteoblasts and vary in size with nuclear atypia
- The osteoid may be thin, lace-like (some say it resembles fungal hyphae) or or it may consist of broad, irregular trabeculae
- The osteoid may be variable in amount
- For craniofacial OS, conventional OS are most common so morphology would include:
- Variably amounts of osteoblastic, fibroblastic (pure spindle cell growth with minimal matrix) or chondroblastic (malignant appearing cartilage with peripheral spindling and osteoid production)
Microscopic (histologic) images
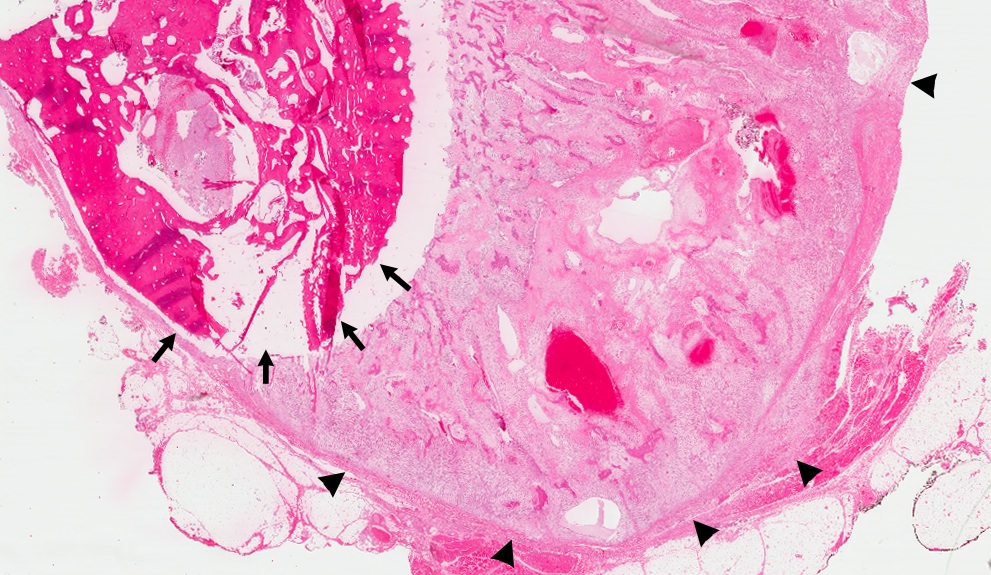
Contributed by Kelly Magliocca, D.D.S., M.P.H.
Case of the Week #350: chondroblastic osteosarcoma of maxilla
Contributed by Dr. Kelly Magliocca and Dr. Anthony Martinez:
Images hosted on other servers:

a) Large osteosarcoma involv-
ing mandible ramus and body
b) Classic chondroblastic
osteosarcoma of the jaw
Immunohistochemistry & special stains
- IHC is of limited value in the diagnosis of osteosarcoma
- Can be positive for osteoblastic lineage biomarkers, including bone morphogenetic proteins, osteocalcin and osteopontin
- S100 protein can be seen in the areas that exhibit cartilaginous differentiation
- Occasional focal positivity for keratins, epithelial membrane antigen and muscle markers (smooth muscle actin and desmin)
Molecular / cytogenetics description
- Conventional osteosarcomas have complex karyotype with numerous aberrations
- Chromothripsis is a genetic mechanism where a single cataclysmic event results in tens to hundreds of genomic rearrangements
Differential diagnosis
- Chondrosarcoma
- Can usually be distinguished from osteosarcoma on clinical, radiologic and pathologic grounds
- More difficult to distinguish when osteosarcomas have large cartilaginous component such as chondroblastic OS
- The cartilaginous component of a chondroblastic OS is usually high grade
- Chondroblastic OS should be accompanied by osteoid production from the sarcomatous stromal cells
- Many chondrosarcomas have IDH1 and IDH2 mutations
- Fibrous dysplasia
- Benign fibro-osseous lesion that may involved one or more bones
- Curvilinear trabeculae (Chinese letters) of metaplastic woven bone (never matures) in hypocellular, fibroblastic stroma
- Fibrous dysplasia is caused by mutations in GNAS gene
- Malignant transformation rarely occurs
- Can be secondary osteosarcoma
- Ossifying fibroma
- Benign fibro-osseous neoplasm that is composed of fibrous tissue that contains a variable amount of bony trabeculae or cementum-like spherules
- Bony trabeculae may be lined by osteoblasts
- Osteoblasts should not be atypical like the sarcomatous cells of osteosarcoma that produce osteoid
- Some larger osteoblastomas may show prominent periosteal new bone formation and may mimic osteosarcoma radiographically
- May also involve the craniofacial bones
- Similar to osteoid osteoma with a nidus containing an interlacing network of bone trabeculae distributed in a loose fibroblastic stroma with a prominent vasculature
- Prominent rimming osteoblasts and multinucleated osteoclast-like giant cells can be seen
- The mitotic rate can be high, but atypical mitoses are not seen
Additional references