Table of Contents
Definition / general | Essential features | Terminology | Physiology | Diagrams / tables | Laboratory | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Videos | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Nguyen TPX. Anatomy & histology-parathyroid. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/parathyroidanatomy.html. Accessed April 28th, 2024.
Definition / general
- Endocrine organs composed of 4 glands, located in close relationship to the posterior aspects of the thyroid lobes
- Superior glands are usually located at the cricothyroid junction, derived from the fourth branchial pouches, together with thyroid
- Inferior glands are close to the point where the inferior parathyroid artery crosses the recurrent laryngeal nerve, derived from fourth branchial pouches, together with the ultimobranchial bodies (Kierszenbaum: Histology and Cell Biology - An Introduction to Pathology, 4th Edition, 2016)
- Number varies from 2 to 12, including ectopic (39.3%) and supernumerary (6.5%) glands (World J Surg 2011;35:1260)
- Ectopic parathyroid glands may be found anywhere along pathway of descent of branchial pouches: thymus (30%), anterior mediastinum (20%), thyroid (20%) or thyrothymic ligament (15%) (Exp Clin Endocrinol Diabetes 2012;120:604, Am J Surg 2006;191:418)
- Discovered in 1880 by Ivar Sandström, a Swedish medical student (Am J Surg Pathol 1996;20:1123)
Essential features
- 4 tiny glands located on the posterior surface of the thyroid
- Histologically composed of a parenchyma of chief cells, oxyphils and transitional cells, and stromal fat
- Regulate calcium homeostasis through synthesis and secretion of parathyroid hormone (PTH)
Terminology
- Glandulae parathyroidae (by Ivar Sandström, 1880), Epithelkörperchen (by Kohn, 1895)
Physiology
- Genes involved in differentiation and growth of parathyroid glands
- Transcription factors: Hoxa3, Pax9, Pax1, Tbx1, Gcm2, Eya1, GATA3, SOX3, AIRE1
- Growth factors and their signaling pathways (Fgf8, BMPs, Chordin, TGFβ, Shh, Tbce) regulate migration of the pharyngeal pouch endoderm, its interaction with the mesenchyme and the balance between proliferation and apoptosis (Dev Biol 1998;195:1, Genes Dev 1998;12:2735, Endocrinol Metab Clin North Am 2018;47:733)
- Synthesis and secretion of parathyroid hormone (PTH), an 84 amino acid peptide derived from a large precursor of 115 amino acids (preproPTH); only the 34 N terminal amino acids have biologic activity (J Endocrinol 2005;187:311)
- Main function of PTH is regulation of serum calcium which mediated by the calcium sensing receptor (CaSR); hypocalcemia activates CaSR, inducing increased PTH synthesis and secretion (Biochem Biophys Res Commun 1995;214:524, Proc Natl Acad Sci USA 1995;92:131)
- PTH acts by increasing calcium resorption into blood from bone, kidney and the gut
- Acting on the PTH receptor (PTHR1) that stimulates renal tubular reabsorption of calcium
- Enhances calcitriol formation in kidney by stimulating 1α vitamin D hydroxylase to convert 25(OH) vitamin D to 1α25(OH)2 vitamin D, resulting in increased gut absorption of calcium
- Prolong life and increase activity of osteoblast, while osteoblast signaling activates osteoclasts, indirectly causing bone resorption; PTH activates osteocytes, causing lysis of perilacunar bone (Mills: Histology for Pathologists, 5th Edition, 2020)
Diagrams / tables
Laboratory
- Serum intact PTH concentration is 23 (15 - 31.6) pg/mL (Horm Res Paediatr 2015;84:124)
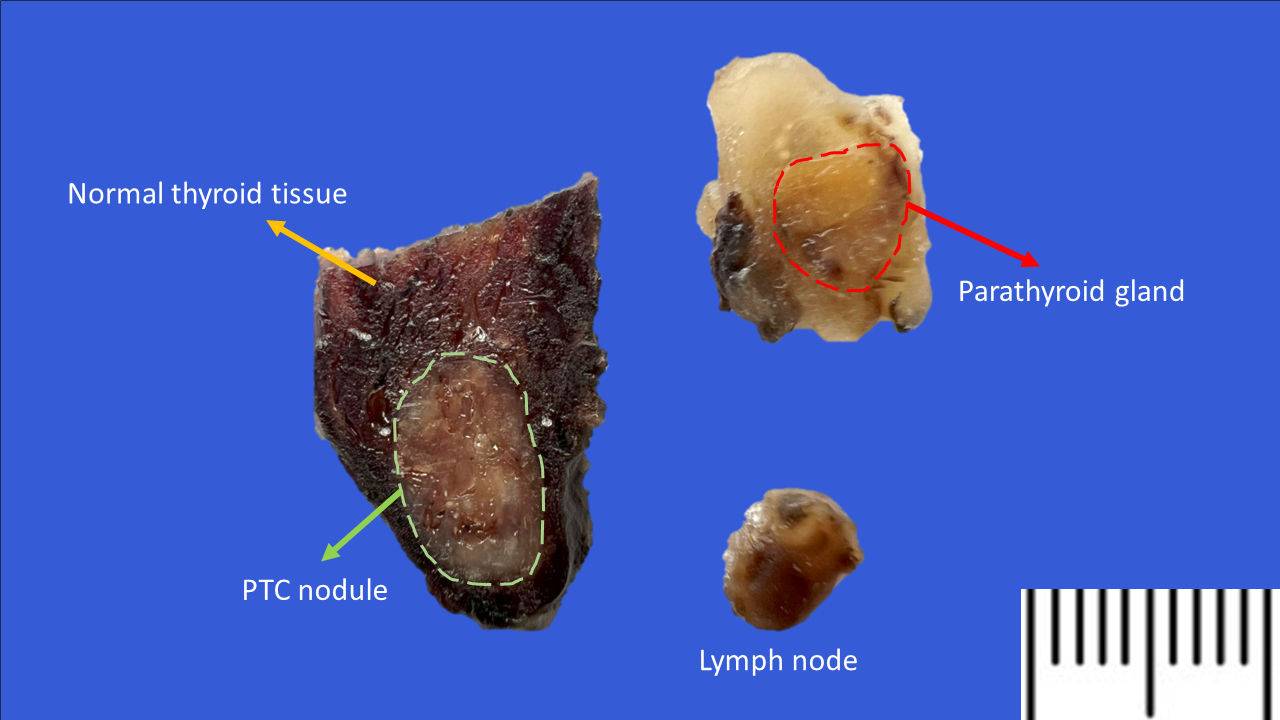
Gross description
- Small, smooth, soft, flattened ovoid or bean shaped structures (4 - 6 mm long, 3 - 4 mm wide, 1 - 2 mm thick), yellow-tan
- Each gland weighs ~30 - 40 mg but can also extremely variable; inferior glands are slightly larger
- 60 mg is the upper limit of normal weight for a parathyroid gland, although weight > 40 mg can be considered abnormal (J Am Coll Surg 2006;203:758)
- Parenchyma is yellow to orange-tan depending on the amount of stromal fat, percent of oncocytic cells and vascularity
- Reference: Lindberg: Diagnostic Pathology - Normal Histology, 3rd Edition, 2022
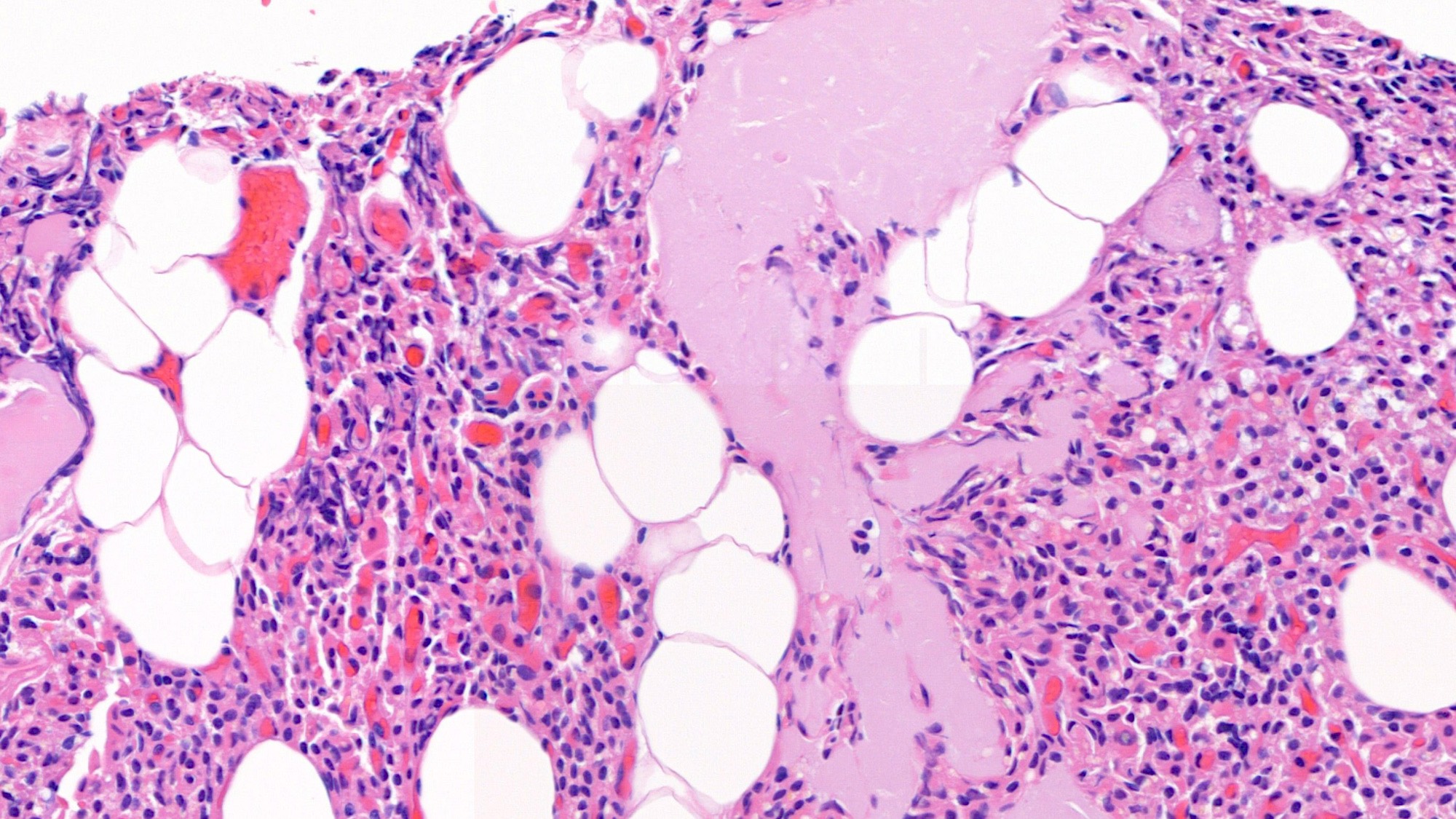
Frozen section description
- Parathyroids often sent for intraoperative consultation: 1) identification of parathyroid tissue to preserve the glands in situ or for autotransplantation to avoid postoperative hypoparathyroidism and 2) evaluation during surgery for primary hyperparathyroidism to verify abnormal glands
- Parathyroid to be differentiated from fat, lymph nodes, thymus, thyroid and other tissue (Arch Pathol Lab Med 2005;129:1575)
- Parathyroid consists of a mixture of parenchymal cells (chief, oxyphil) and fat
- Near infrared fluorescence imaging with indocyanine green imaging is a useful tool for intraoperative detection of parathyroid by surgeon (In Vivo 2020;34:23)
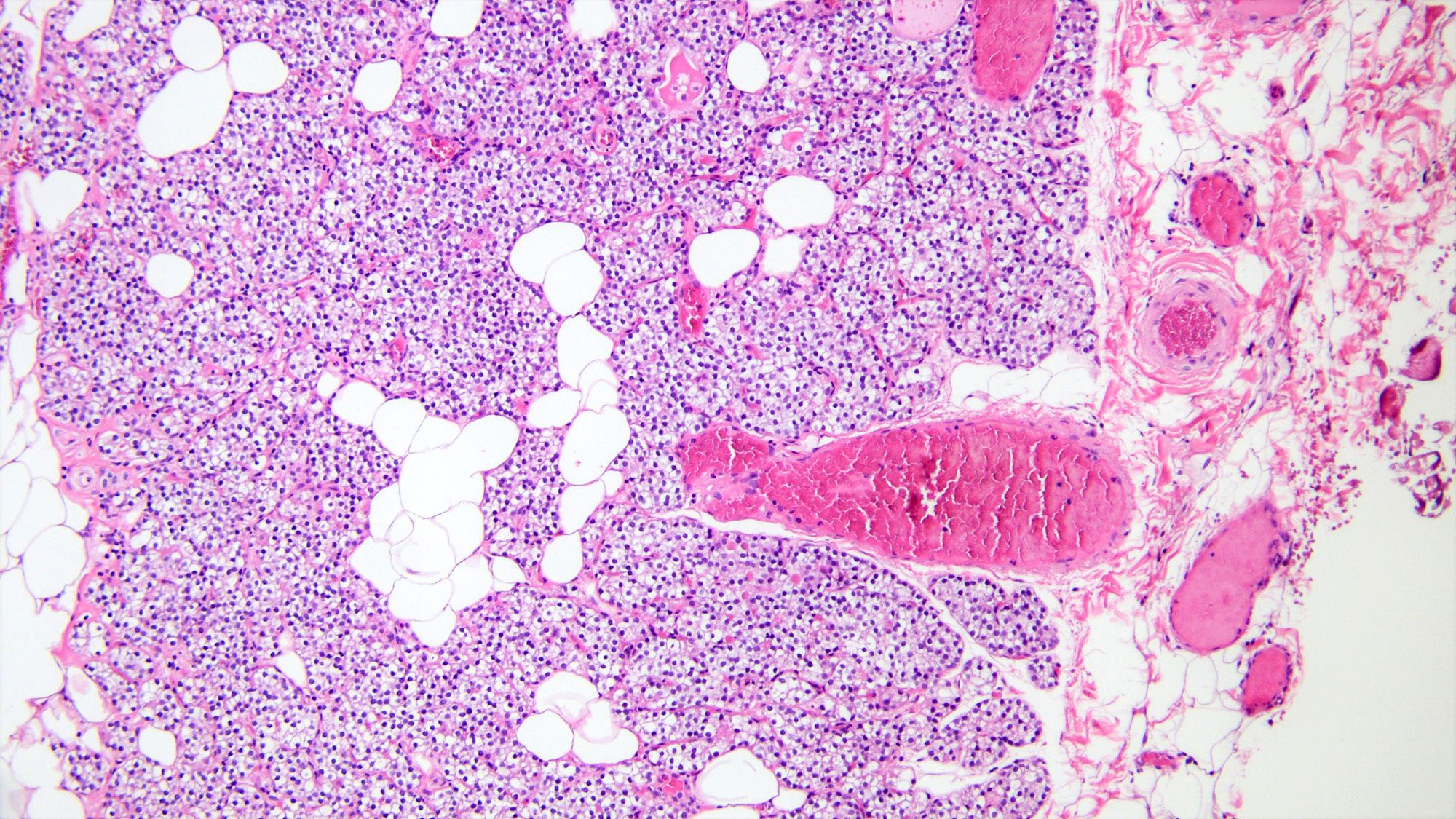
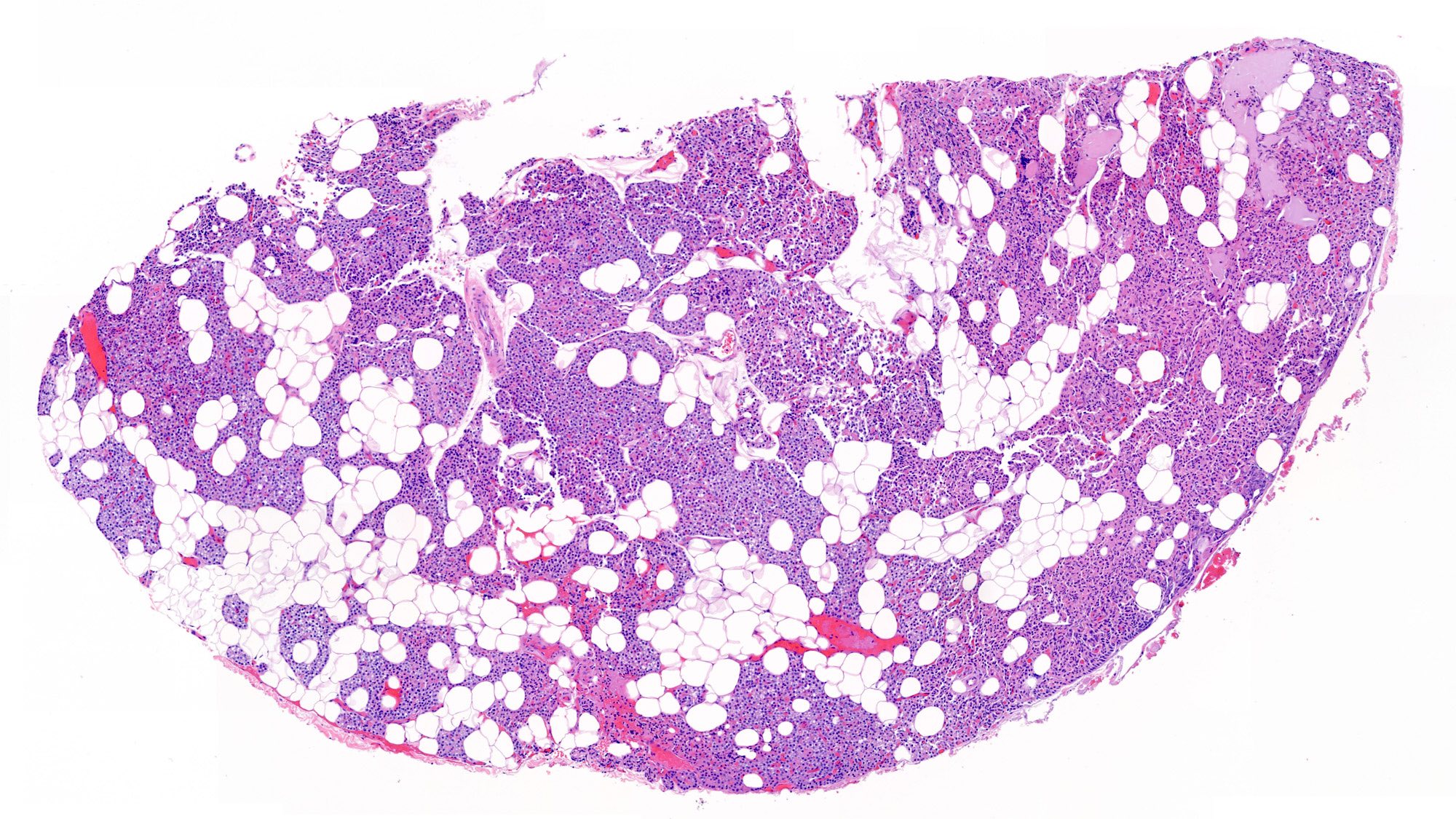
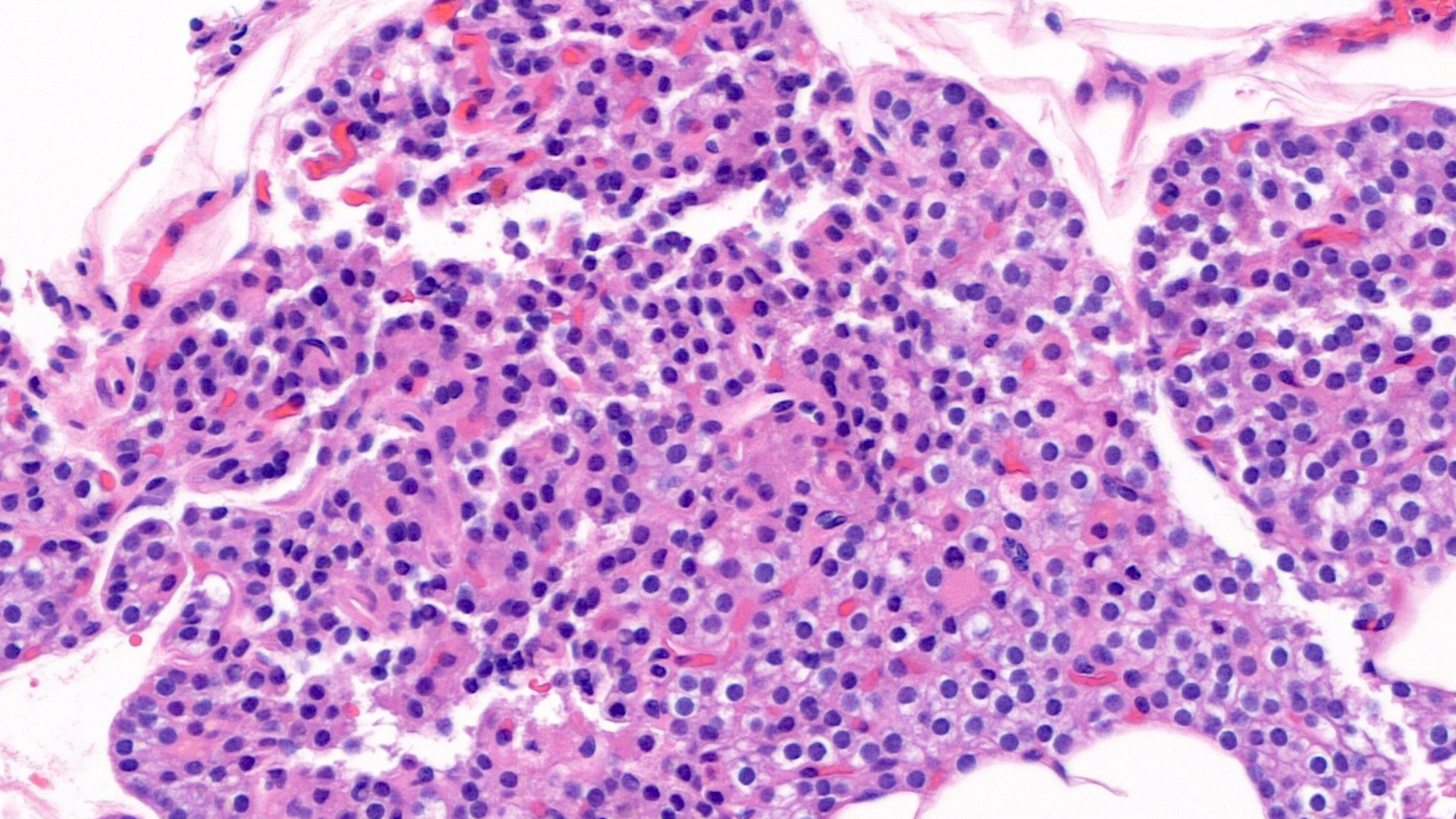
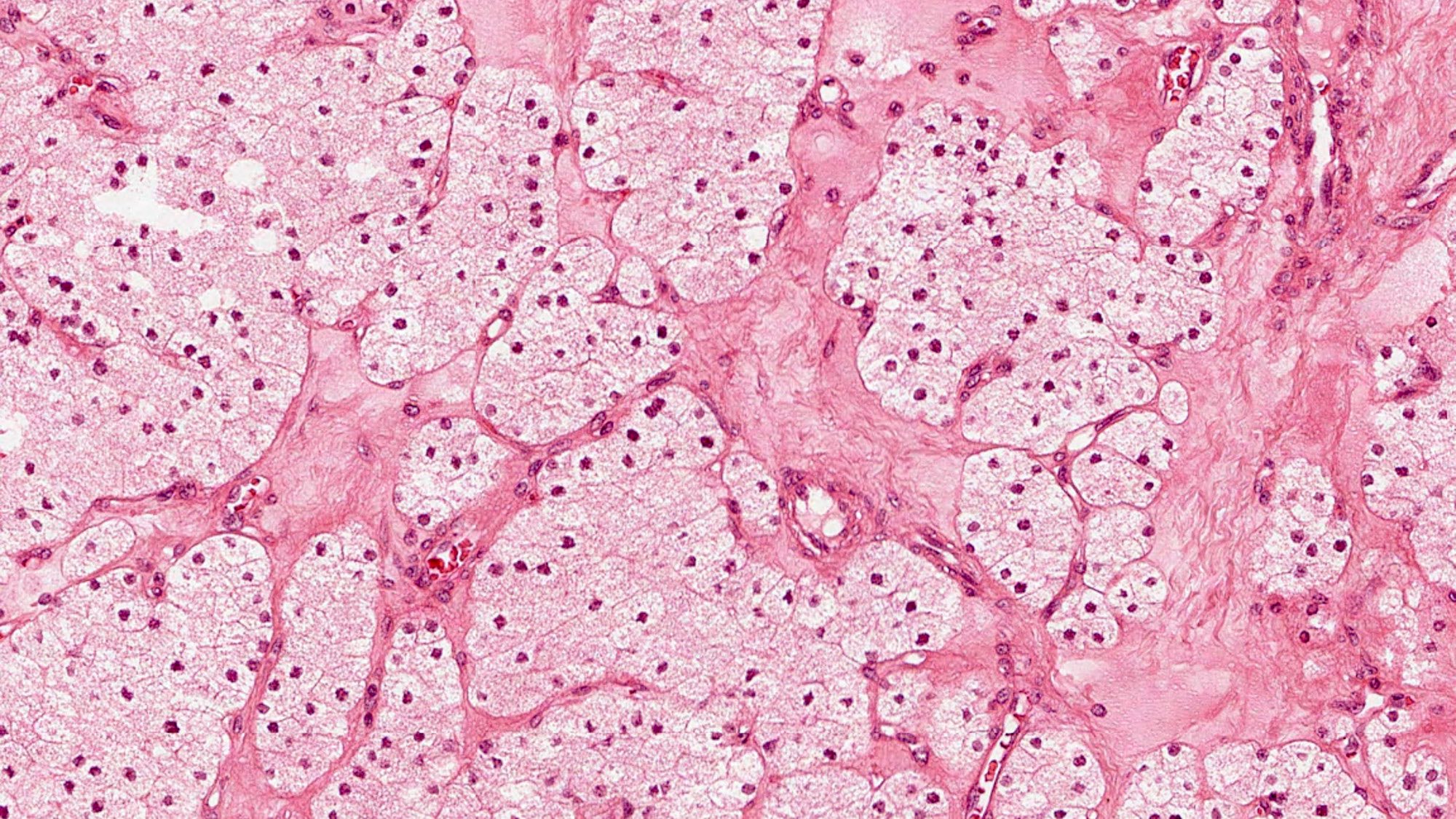
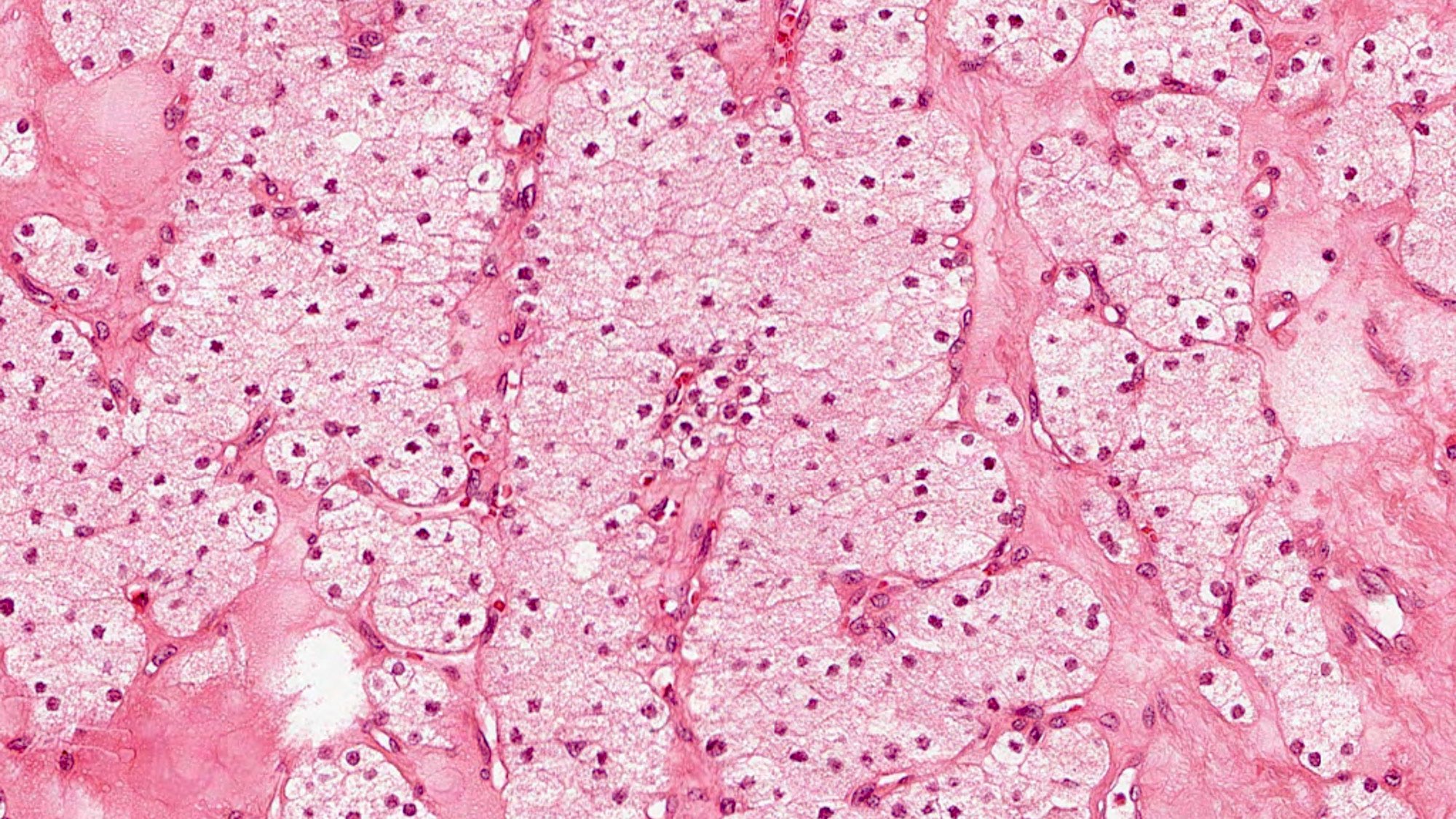
Microscopic (histologic) description
- Thinly encapsulated with fibrous septa extending into parenchyma dividing gland into vague lobules
- Parenchyma has 3 cell types: chief cells, oxyphils and transitional cells; these are all variants of the chief cells that have differing degrees of oncocytic change
- Parenchymal cells arranged in nests and cords
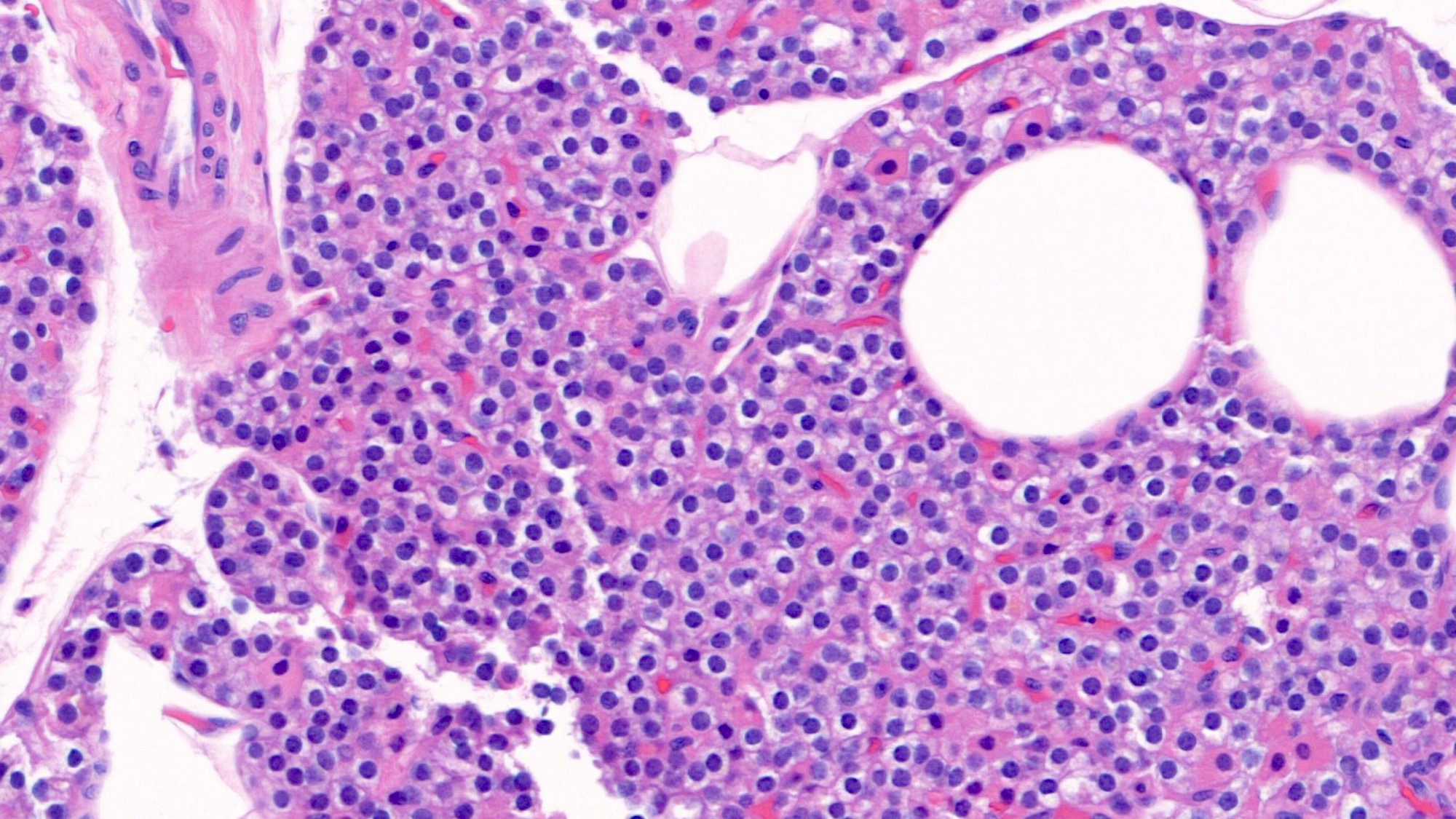
- Chief cells
- Functional cells, responsible for the synthesis and secretion of PTH
- 8 - 12 μm in diameter, round to polygonal with centrally located nuclei, coarse chromatin and small nucleoli
- Cytoplasm varies from clear to amphophilic or faintly eosinophilic
- Clear vacuolated appearance is due to accumulation of glycogen or lipid
- Arranged in small nests and thin cords and separated by stromal adipose tissue
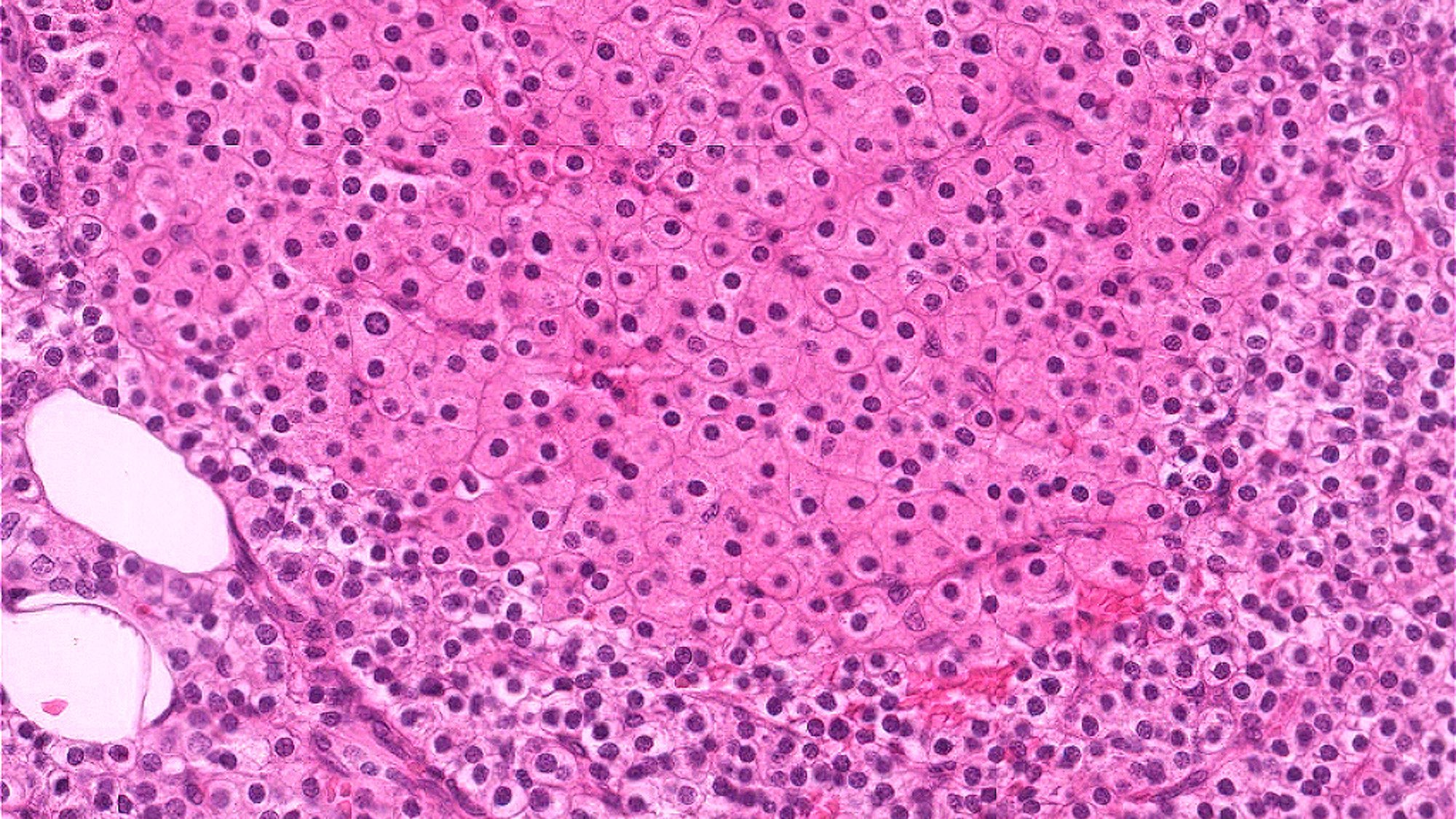
- Oxyphil cells
- Typically appear at puberty and increase in number with age
- Larger than chief cells, measuring 12 - 20 μm in diameter
- Singly, in small clusters or as large nodules and sheets
- Abundant granular eosinophilic cytoplasm due to the accumulation of numerous mitochondria
- Transitional cells
- Intermediate forms that have features of chief cells and partial oncocytic change
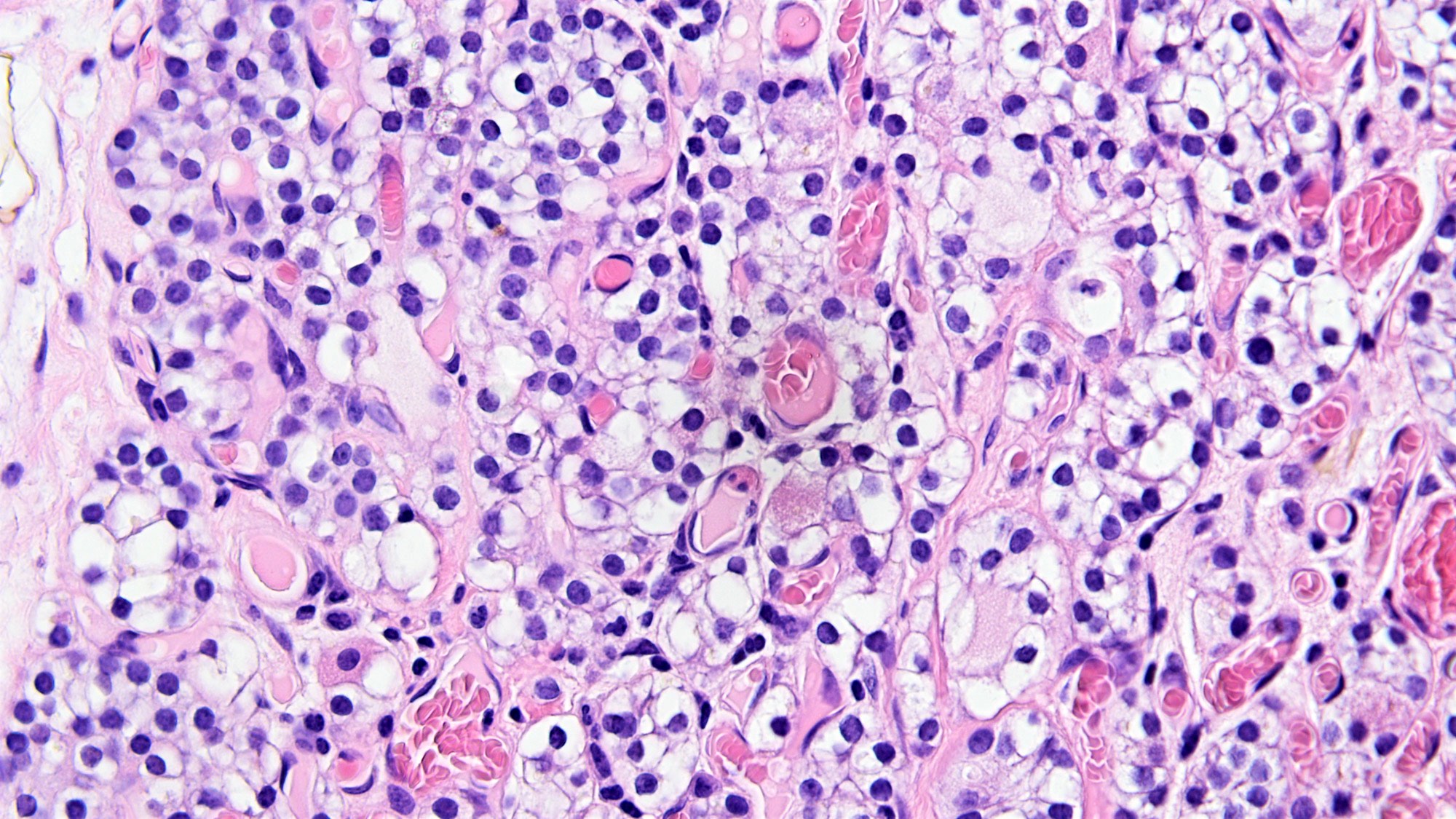
- Water clear cell
- Found in the fetal gland but are not present in normal adult glands
- Found usually only in pathologic states (hyperplasia and adenoma)
- Very large, measuring 15 - 20 μm and up to 40 μm
- Represent chief cells with excessive cytoplasmic glycogen
- May have cysts and follicles filled with proteinaceous material that resembles colloid of the thyroid gland
- Positive with periodic acid-Schiff (PAS)
- Do not contain birefringent calcium oxalate crystals (polarized light)
- Stroma comprised of stromal fat cells and fibroconnective tissue with rich vascular supply
- Amount of stromal fat tends to be higher in women (Mills: Histology for Pathologists, 5th Edition, 2020)
- Age related changes: increased stromal fat cells, accumulation of fibroconnective tissue, more oxyphils
- Reference: Lindberg: Diagnostic Pathology - Normal Histology, 3rd Edition, 2022
Microscopic (histologic) images
Positive stains
- Histochemistry
- Immunohistochemistry
- Neuroendocrine lineage: synaptophysin (cytoplasmic), chromogranin A (cytoplasmic)
- GATA3 (nuclear), GCM2 (nuclear), PTH (cytoplasmic) (distinguish parathyroid cells from other neuroendocrine cells) (Endocr Pathol 2018;29:113)
- Polyclonal PAX8 (nuclear), CK AE1 / AE3, CK7, CK8/18, CK19 (cytoplasmic)
Negative stains
- Thyroid specific markers: TTF1, thyroglobulin (Endocr Pathol 2018;29:113)
- Calcitonin and calcitonin gene related peptide (usually) (Endocr Patho 2019;30:168)
- Monoclonal PAX8, PGP9.5, neurofilaments
Electron microscopy description
- Chief cells: contain relatively few secretory granules
- Oxyphil cells: the cytoplasm is filled with numerous mitochondria
- Transitional cells: have fewer mitochondria than fully developed oncocytic cells but more than chief cells
- Reference: Mills: Histology for Pathologists, 5th Edition, 2020
Videos
Histology of parathyroid
Board review style question #1
Which cell type of parathyroid glands is round to polygonal with centrally located nuclei, coarse chromatin, small nucleoli and cytoplasm that ranges from clear to amphophilic or faintly eosinophilic?
- Chief cell
- Oxyphil cell
- Transitional cell
- Water clear cell
Board review style answer #1
A. Chief cell. These features are suitable for the chief cell's function of producing and releasing PTH hormone.
Answer B is incorrect because oxyphil cells have granular eosinophilic cytoplasm.
Answer C is incorrect because transitional cells have partial features of chief cells and oxyphil cells.
Answer D is incorrect because water clear cell has foamy cytoplasm.
Comment Here
Reference: Anatomy & histology - parathyroid
Comment Here
Reference: Anatomy & histology - parathyroid
Board review style question #2
Board review style answer #2
B. Fetal glands. Water clear cells are usually found in fetal parathyroid glands with excessive cytoplasmic glycogen.
Answers A, C and D are incorrect because they only comprise 3 cell types (chief cells, oxyphil cells and transitional cells) of normal adult parathyroid glands.
Comment Here
Reference: Anatomy & histology - parathyroid
Comment Here
Reference: Anatomy & histology - parathyroid