Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lamiaa H, Abbas O. Juvenile xanthogranuloma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticjuvenilexantho.html. Accessed April 29th, 2024.
Definition / general
- Rare, sporadic, benign disorder which results from the proliferation of factor XIIIa positive dendritic cells
- Most common form of non-Langerhans cell histiocytosis
- Typically a disorder of early childhood
Essential features
- Juvenile xanthogranuloma (JXG) is a rare, benign proliferative non-Langerhans cell histiocytic proliferation
- Occurs predominantly in young children
- Clinically, it presents as a solitary red-brown, yellowish papule or nodule, most often on the head and neck area
- Systemic JXG is rare and may involve any organ system
- Histologically characterized by the presence of histiocytes, foam cells and Touton giant cells
- Generally follows a benign course with spontaneous resolution over a period of a few years
- Cutaneous JXG is usually self limited
- Cases of ocular JXG should be referred to an ophthalmologist
- Symptomatic systemic JXG may require treatment
Terminology
- Nevoxanthoendothelioma, xanthoma multiplex, juvenile xanthoma, multiple eruptive xanthoma in infancy, congenital xanthoma tuberosum, xanthoma neviforme and juvenile giant cell granuloma
ICD coding
- ICD-10: D76.3 - Other histiocytosis syndromes
Epidemiology
- Incidence is unknown
- Between 40 - 70% of cases arise in the first year of life
- More than 15 - 20% of patients have lesions at birth
- Adult onset accounts for 10% of cases
- M:F = ~1.4:1 (Actas Dermosifiliogr 2020;111:725)
- Has been associated with juvenile chronic myelogenous leukemia and neurofibromatosis type I (Br J Dermatol 2017;176:481)
Sites
- Presents as a solitary cutaneous nodule on the head, neck or trunk
- Occasionally extracutaneous presentation of nodules occurs within the eye (most common), soft tissues or visceral organs
- Ocular JXG is usually unilateral and most often develops before the age of 2
- Hyphema and glaucoma are serious complications of ocular JXG
- Systemic involvement is rare, occurring in less than 5% of cases
- Reference: Actas Dermosifiliogr 2020;111:725
Pathophysiology
- Unknown at this time
Etiology
- Cause is unknown
- Suggested that histiocytes possibly react to a traumatic or infectious stimuli by progressive lipidation
Clinical features
- 2 clinical variants have been described: a small and a large nodular form; both present as red-brown, dome shaped papules
- Small nodular form usually consists of multiple 2 - 5 mm sized papules, whereas the large nodular form is characterized by 1 or a few nodules 1 - 2 cm in diameter; these 2 forms can coexist
- Has been associated with insulin dependent diabetes mellitus, aquagenic pruritus, urticaria pigmentosa and cytomegalovirus infection
- Most adult patients have solitary lesions
- Reference: Actas Dermosifiliogr 2020;111:725
Diagnosis
- Diagnosis is made clinically based on the typical appearance of lesions on physical examination in most cases
- On dermoscopy, the setting sun sign is described, which corresponds to a yellow-orange, central area surrounded by a peripheral border with branched, linear telangiectasias (An Bras Dermatol 2018;93:138)
- In older lesions, white and yellow globules are most commonly seen on dermoscopy because of the more lipidized cells (An Bras Dermatol 2018;93:138)
Prognostic factors
- Has a good prognosis; lesions usually regress spontaneously
- Cases of liver or central nervous system involvement may rarely be fatal
Case reports
- 31 week preterm newborn with multiple skin lesions whose clinical, histological and immunohistochemical findings were consistent with juvenile xanthogranuloma (Rev Paul Pediatr 2019;37:257)
- 14 month old and 14 year old girls with oral JXG affecting the lower lip and the soft palate, respectively (Pediatr Dent 2017;39:238)
- 12 year old girl with a slowly growing yellowish polypoid lesion on the posterior scalp (Am J Dermatopathol 2017;39:773)
Treatment
- Self limited
- No treatment is usually required
- Excision can be done for cosmetic concerns
- Reference: Actas Dermosifiliogr 2020;111:725
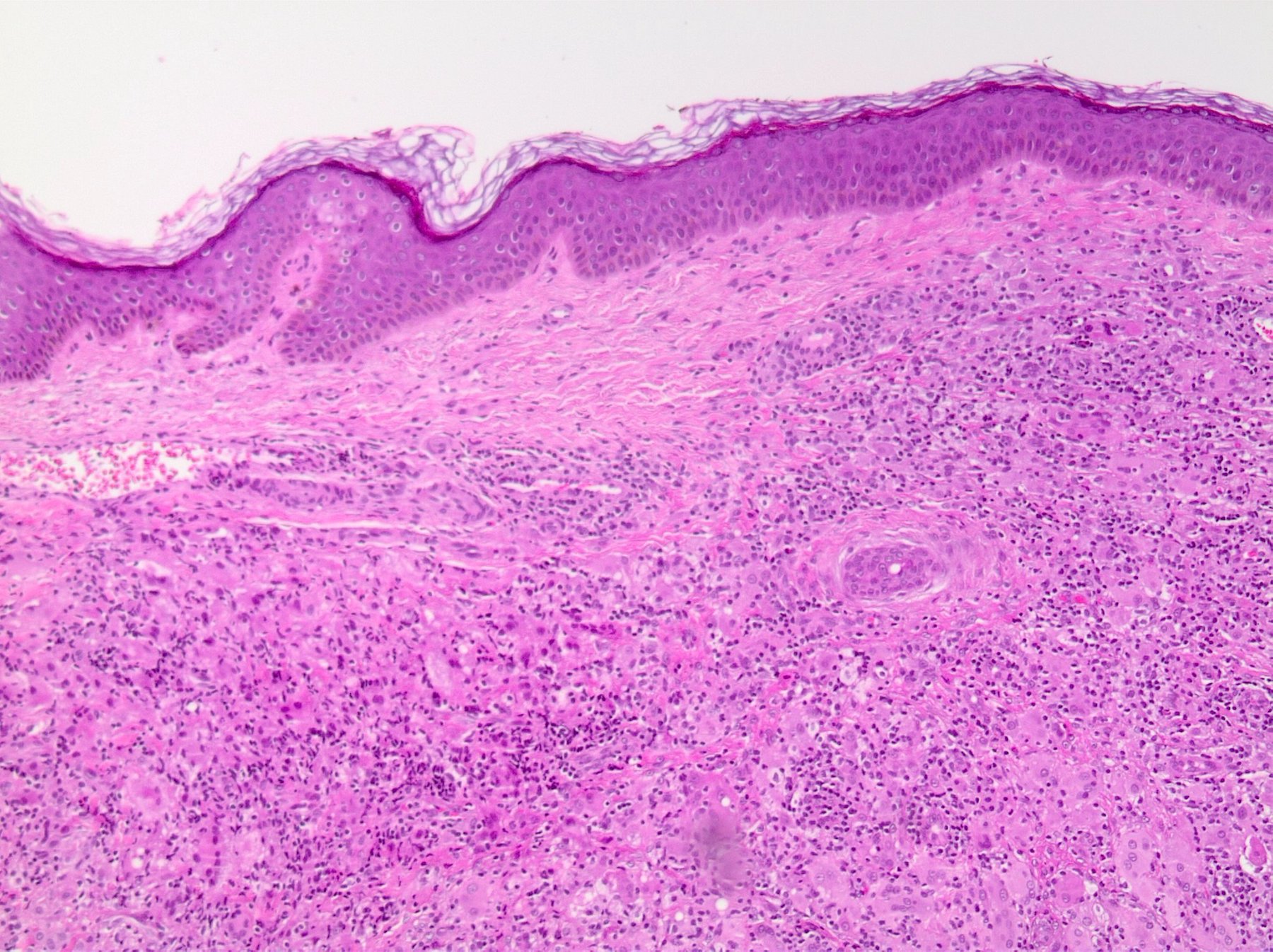
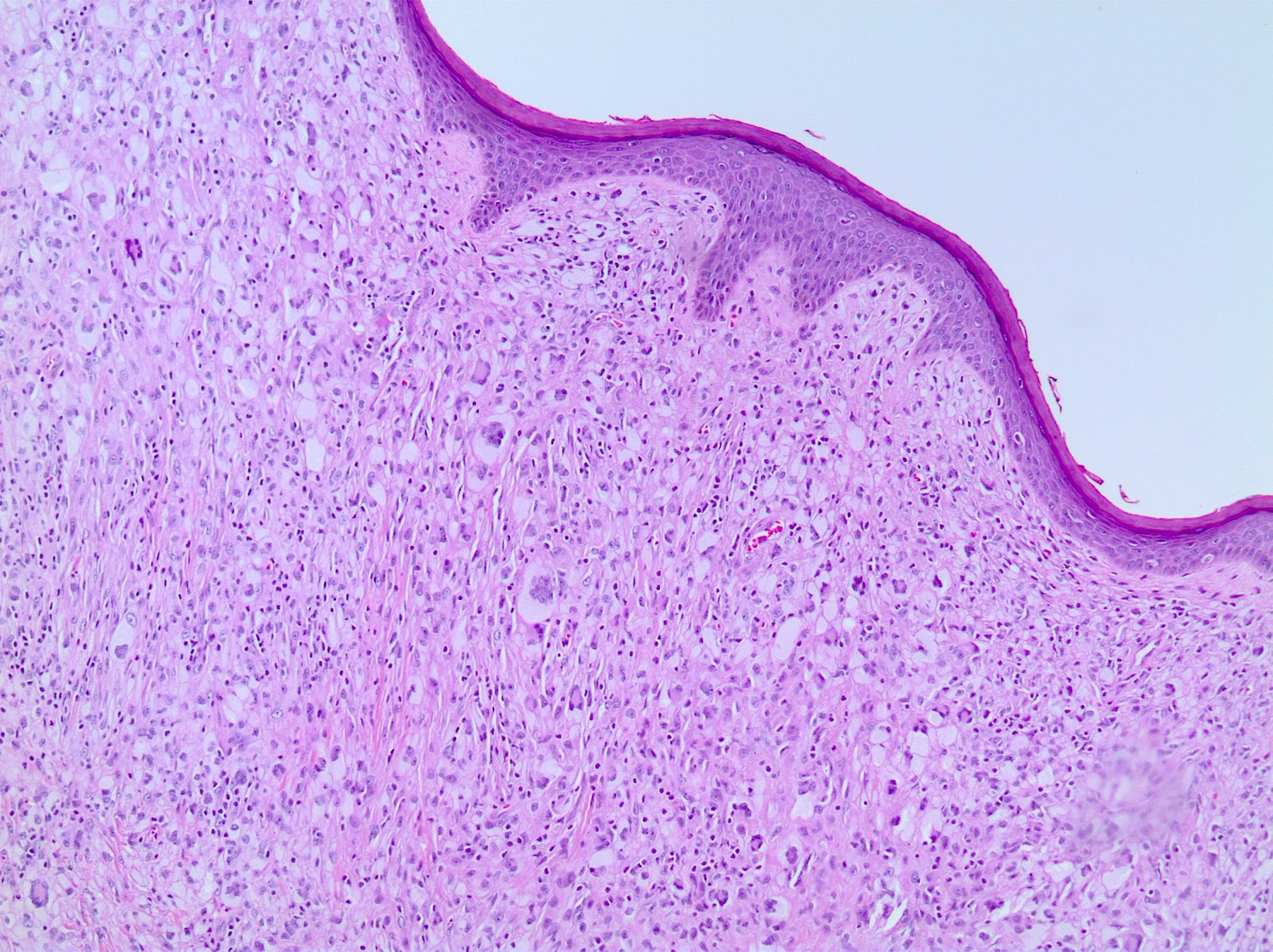
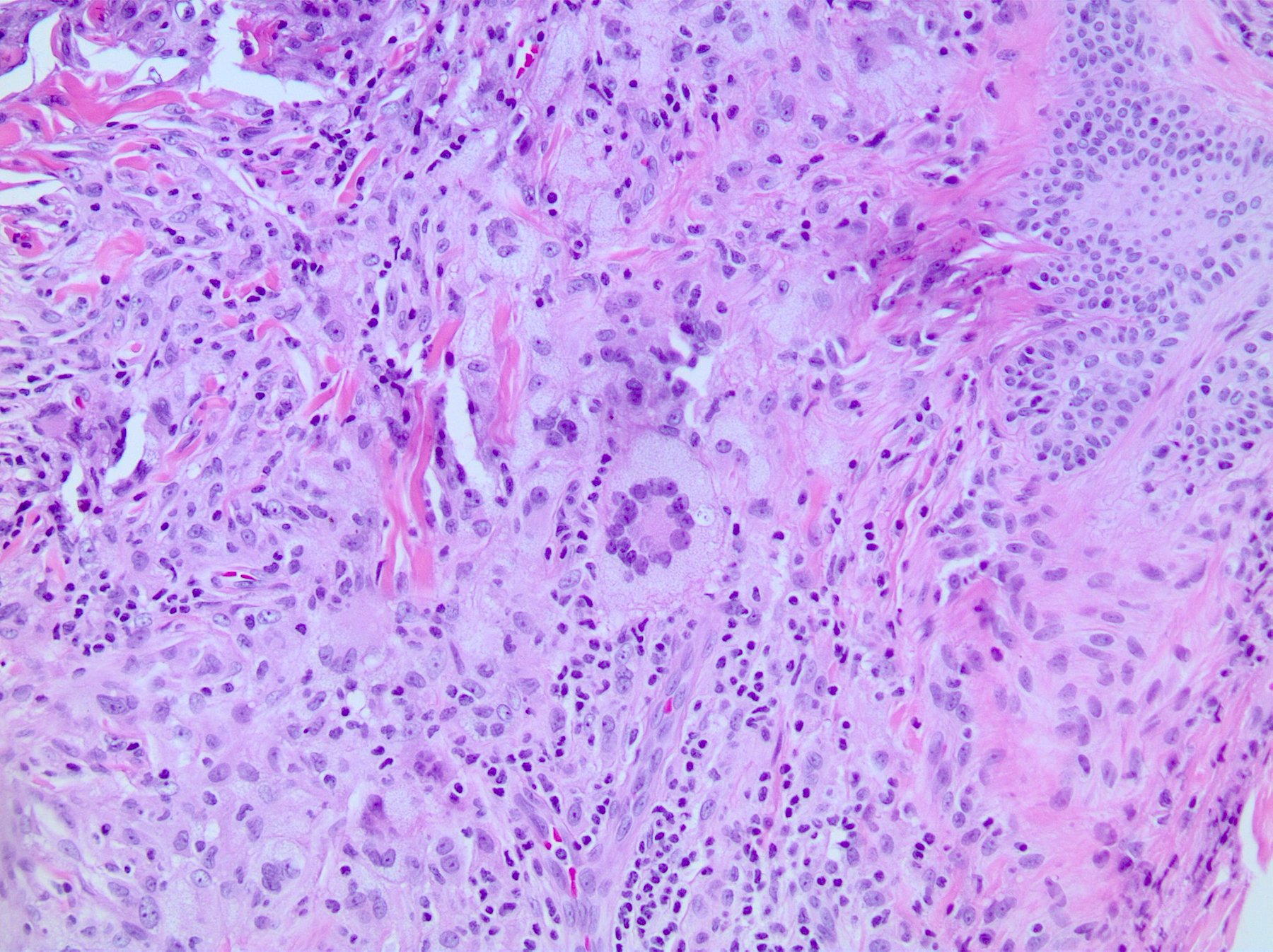
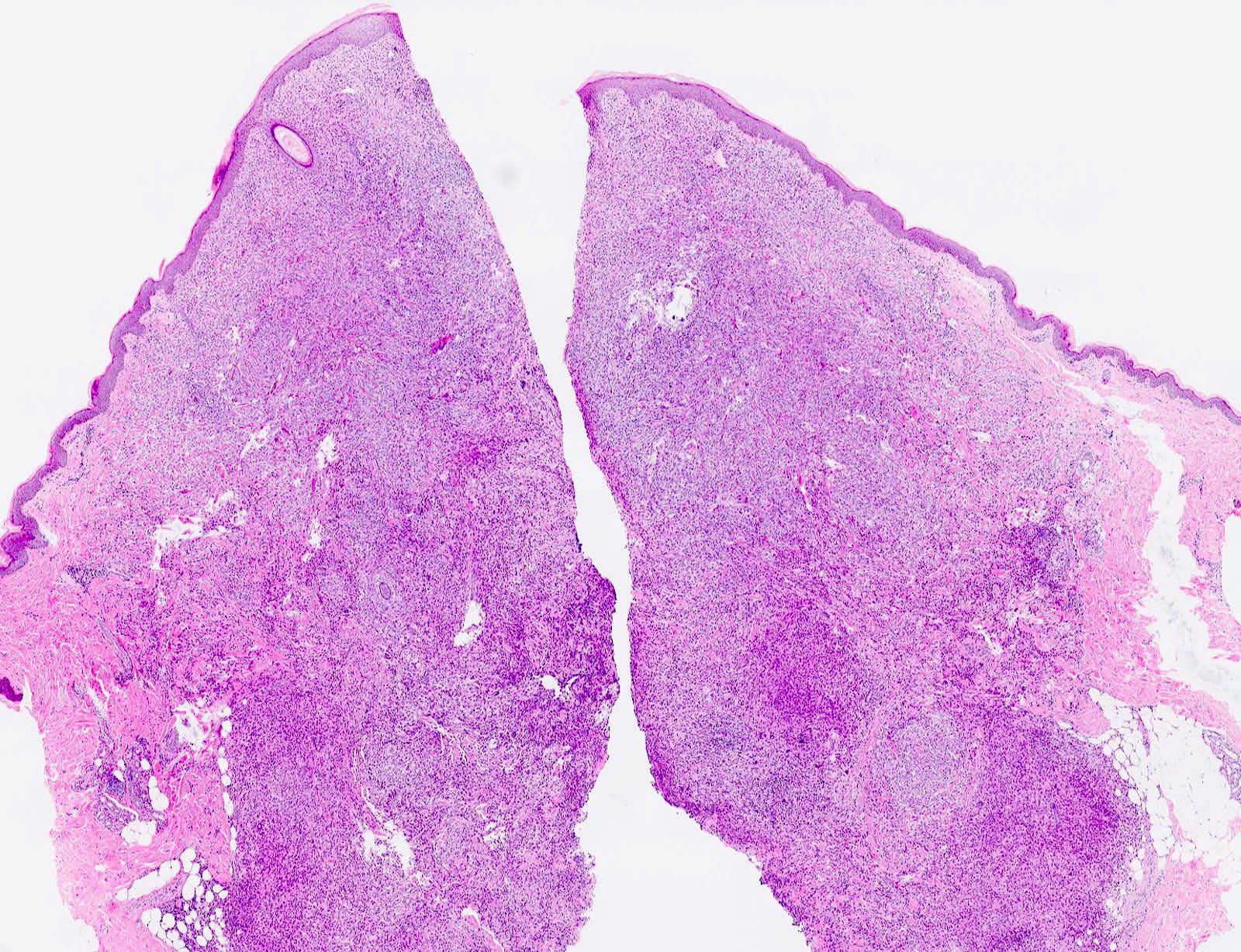
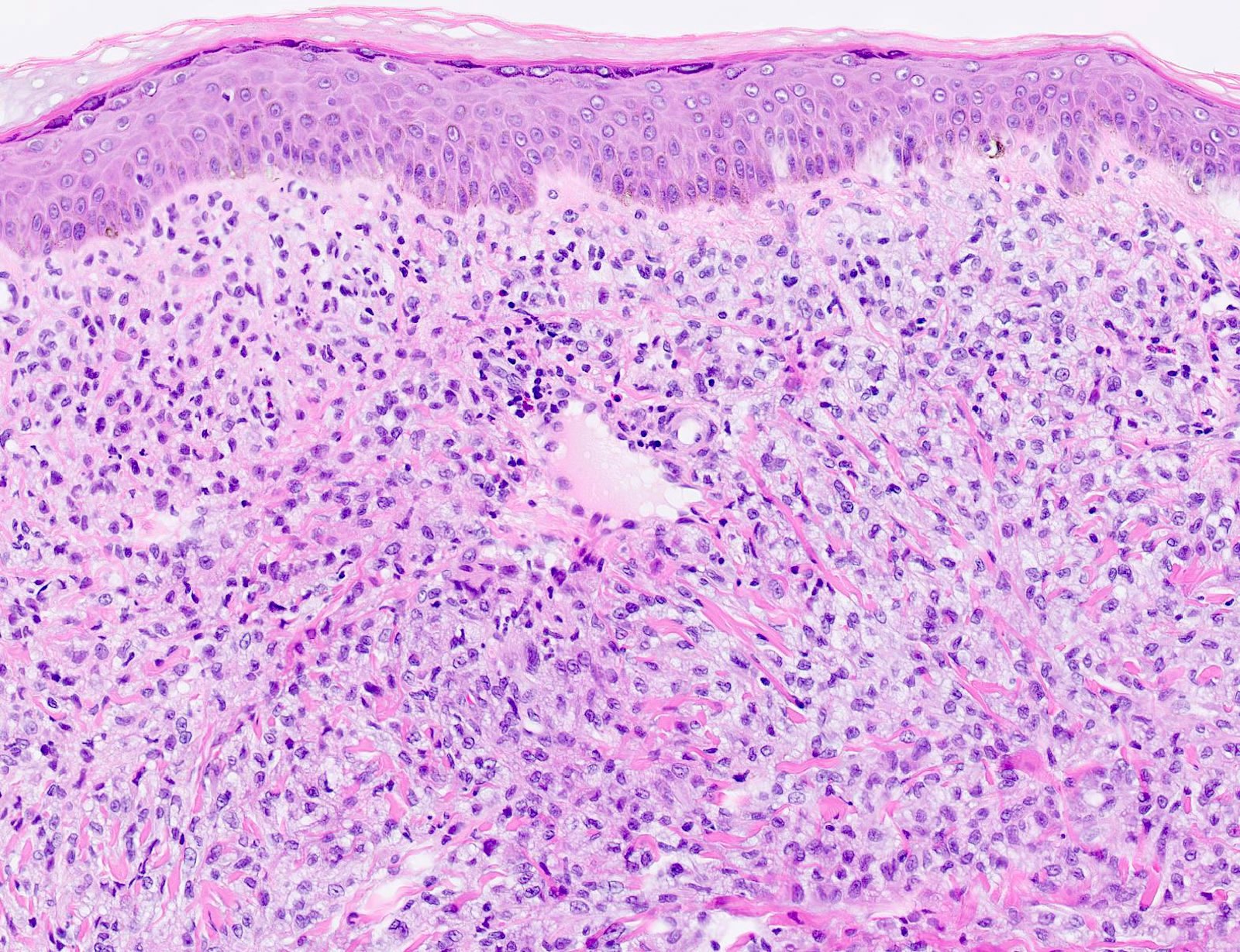
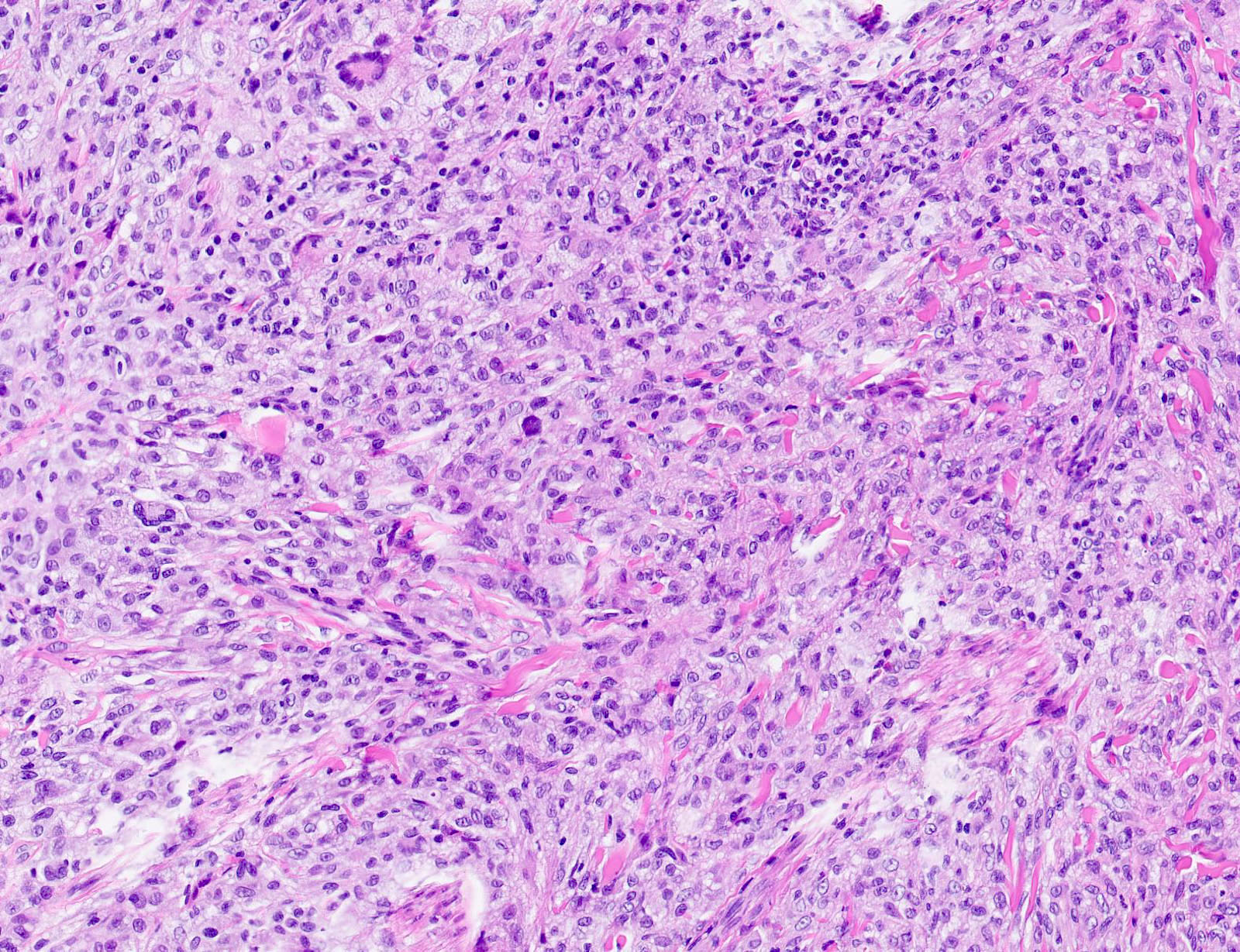
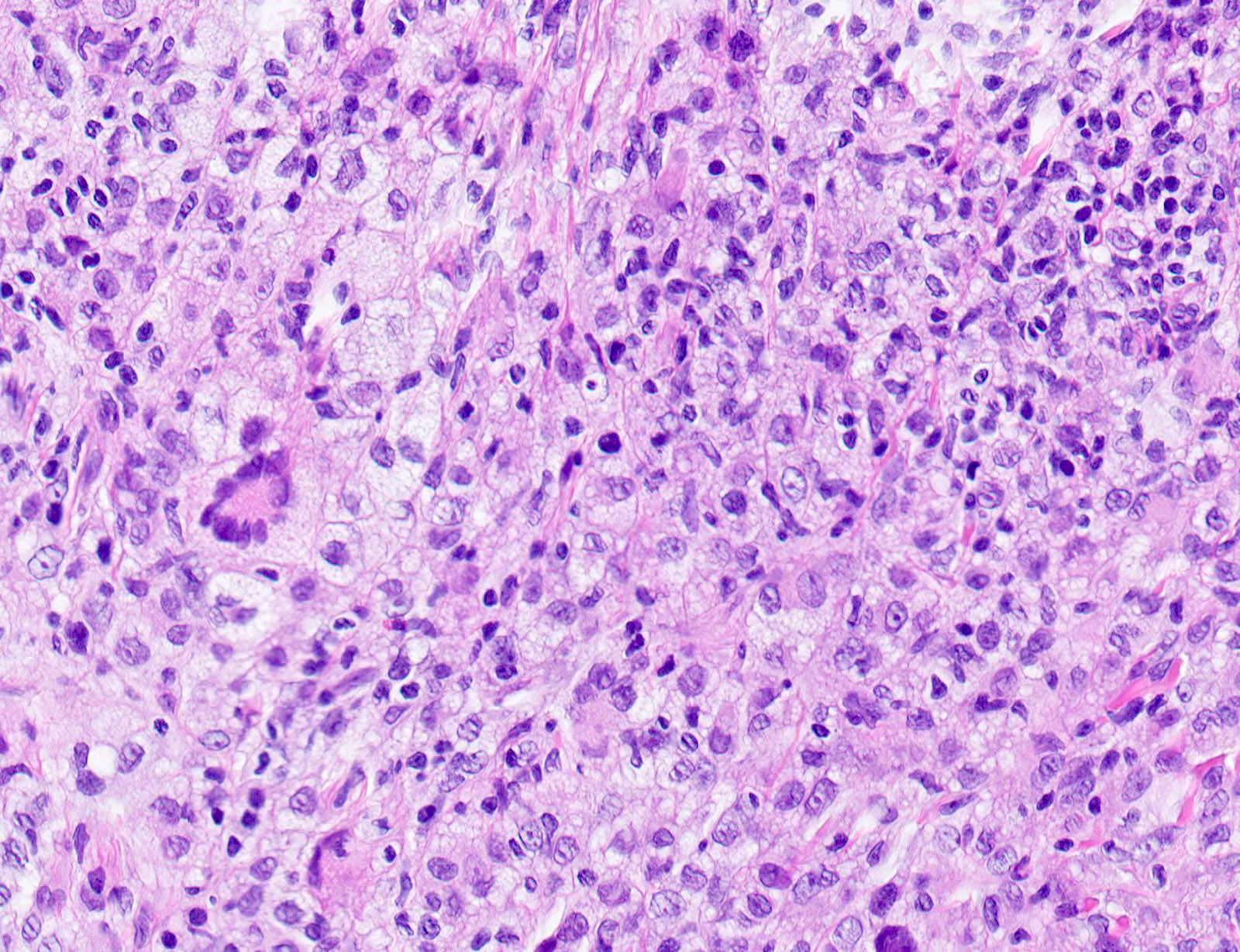
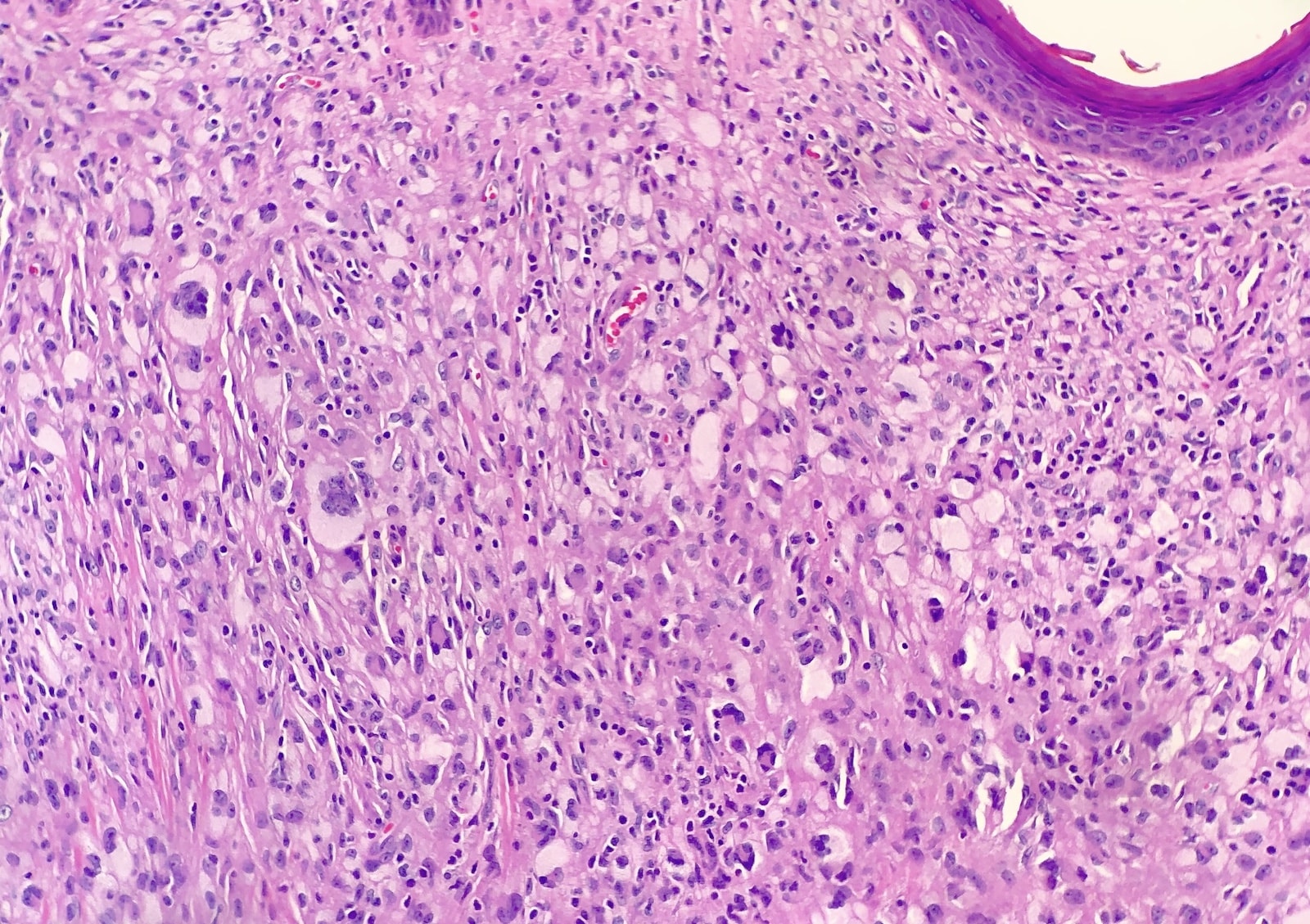
Microscopic (histologic) description
- Demarcated dense dermal infiltrate of foamy histiocytes that can extend to the subcutis in large lesions
- Scattered Touton giant cells are characteristic
- Can have loss of the rete ridges and ulceration
- Lymphocytes, plasma cells, eosinophils and some neutrophils can be observed
- Early lesions usually have monomorphous histiocytes with abundant eosinophilic cytoplasm
- In older lesions, the histiocytes become more xanthomatous by developing lipid in their cytoplasm, creating a foamy appearance
- Reference: Actas Dermosifiliogr 2020;111:725
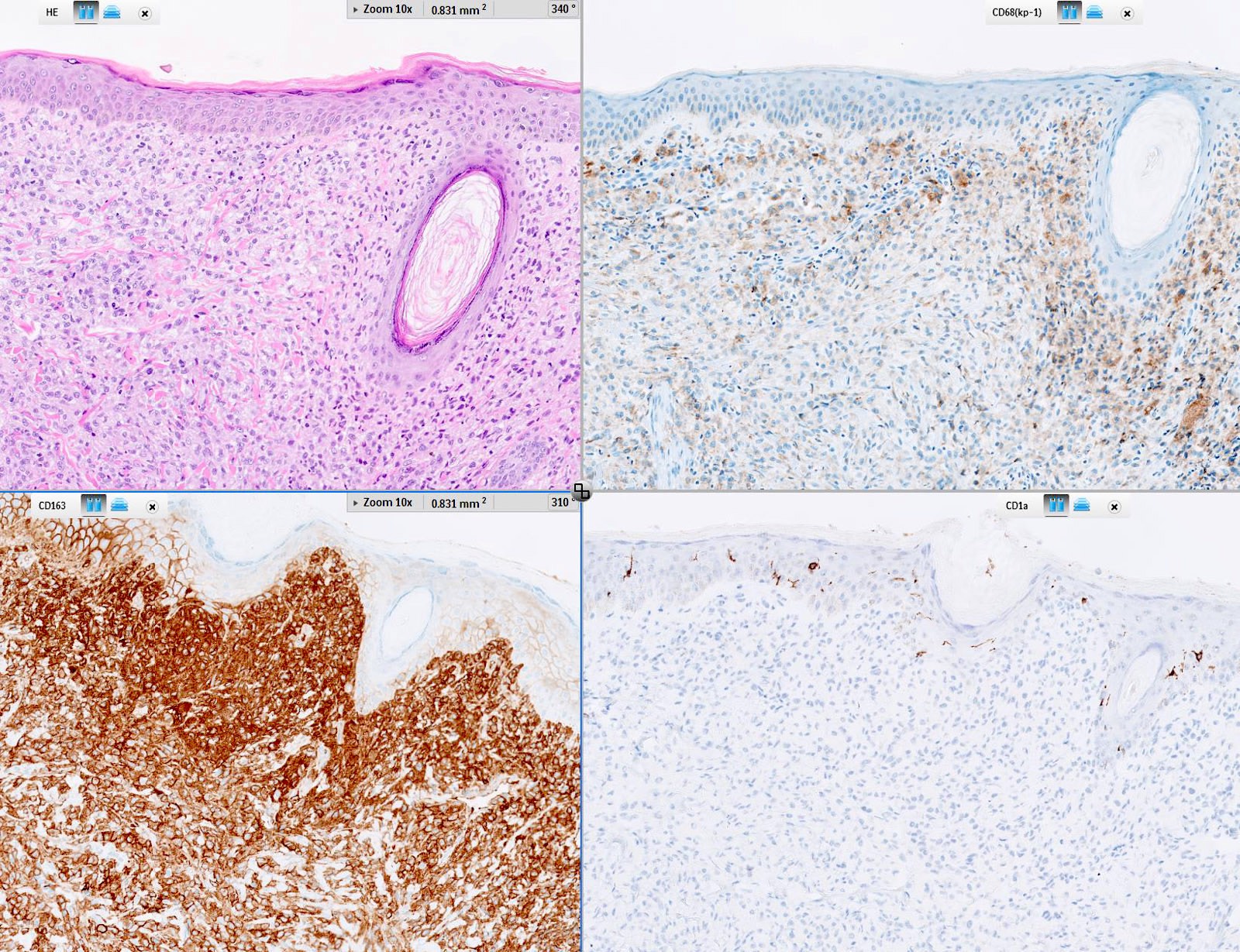
Microscopic (histologic) images
Contributed by Lamiaa Hamie, M.D., M.Sc. and Ossama Abbas, M.D.
Contributed by Jijgee Munkhdelger, M.D., Ph.D. and Andrey Bychkov, M.D., Ph.D.
Virtual slides
Positive stains
- HAM56
- CD68
- Factor XIIIa
- CD163
- Reference: Actas Dermosifiliogr 2020;111:725
Negative stains
- Langerin (CD207)
- CD1a
- S100 (not always)
- Reference: Actas Dermosifiliogr 2020;111:725
Videos
Brief review of JXG
Sample pathology report
- Right arm, excision:
- Xanthogranuloma (see comment)
- Comment: Dense sheets of histiocytes infiltrating the dermis and the upper portion of the subcutaneous fat. Numerous multinucleated giant cells of the Touton cell type. In addition, clinicopathologic correlation may be helpful.
Differential diagnosis
- Langerhans cell histiocytosis:
- LCH cells are positive for S100 protein, CD1a and langerin (CD207)
- Intracytoplasmic Birbeck granules are seen on electron microscopy
- Systemic manifestations include osteolytic bone lesions, diabetes insipidus, hepatosplenomegaly and lymphadenopathy
- Papular xanthoma:
- Multiple yellow-red papules
- Mainly on the trunk
- Fewer Touton cells than JXG
- Factor XIIIa is more likely to be negative
- Tuberous xanthoma:
- Occurs in areas of pressure
- Associated with hypercholesterolemia and high LDL
- Consists of dermal aggregates of foam cells, no Touton cells or inflammatory cells
- Spitz nevus:
- Nests of spindle and epithelioid cells within a uniformly hyperplastic epidermis
- Melanocytic immunostaining with S100, MelanA (MART1) and tyrosinase
- Mastocytoma:
- Reddish golden-brown papules
- Can display Darier sign
- Can be pruritic
- Mast cells in the papillary dermis
- Dermatofibroma:
- Brownish papules
- Mainly on the extremities
- May arise after trauma
- Older age group
- Dermal spindle shaped proliferation with collagen trapping
- Reticulohistiocytoma:
- More prominent nucleoli
- Few to no Touton giant cells
- More likely to be punctuated by inflammatory foci
- Ground glass cytoplasm (can be seen in some JXGs)
- Erdheim-Chester disease:
Additional references
Board review style question #1
Board review style answer #1
A. This is a juvenile xanthogranuloma. Its most common site of extracutaneous presentation is the eyes.
Comment Here
Reference: Juvenile xanthogranuloma
Comment Here
Reference: Juvenile xanthogranuloma
Board review style question #2
A 2 year old girl was brought to the clinic for an asymptomatic red-yellow papule of a few months' duration on the arm. On histological examination, there was a dermal infiltrate of foamy histiocytes and multinucleated giant cells with a ring of nuclei surrounded by a foamy cytoplasm. Which of these markers would be negative on immunohistochemical staining?
- HAM56
- CD207
- Factor XIIIa
- CD163
- CD68
Board review style answer #2
B. This is a juvenile xanthogranuloma, which is negative for CD207 (Langerin).
Comment Here
Reference: Juvenile xanthogranuloma
Comment Here
Reference: Juvenile xanthogranuloma