26 August 2005 - Case #17
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Osama M. Al-Agha, SUNY Downstate Medical Center, Brooklyn, New York, USA and Dr. Jotica Talwar, Staten Island University Hospital, Staten Island, New York, USA.
Case #17
Clinical history:
A 61 year old woman presented with chest tightness, intermittent shortness of breath and right supraclavicular lymph node enlargement. Radiologic studies revealed an anterosuperior mediastinal mass measuring 5 x 4 x 4 cm with mediastinal lymphadenopathy. The patient underwent CT guided needle biopsy for the mediastinal mass.
Microscopic description:
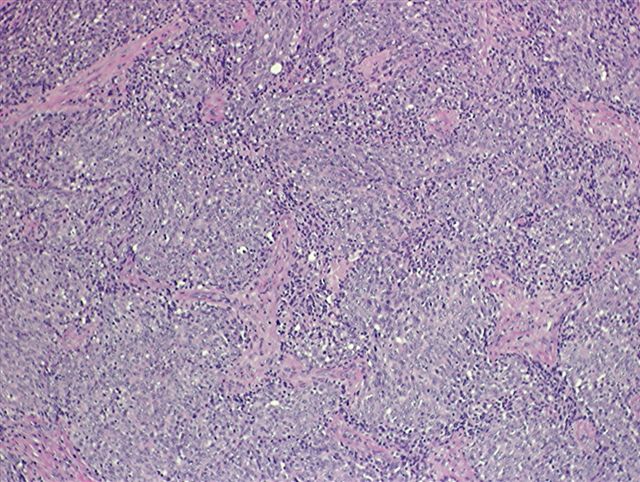
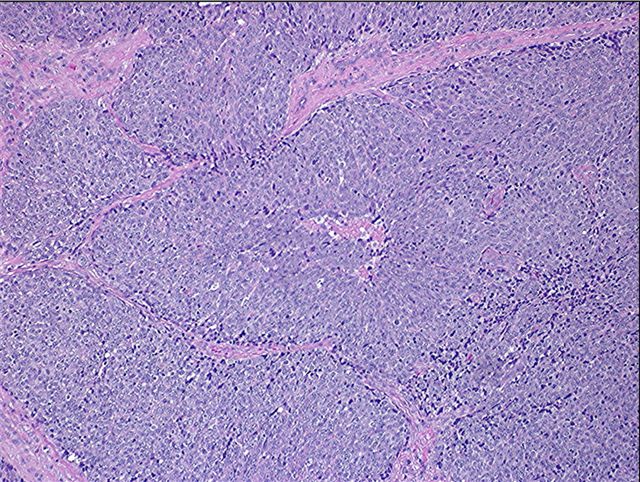
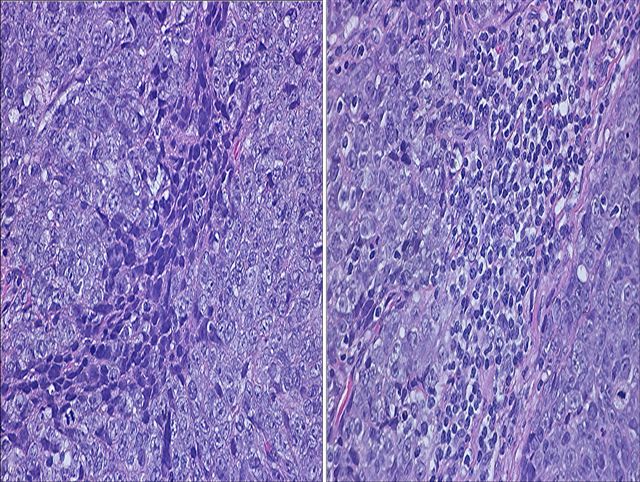
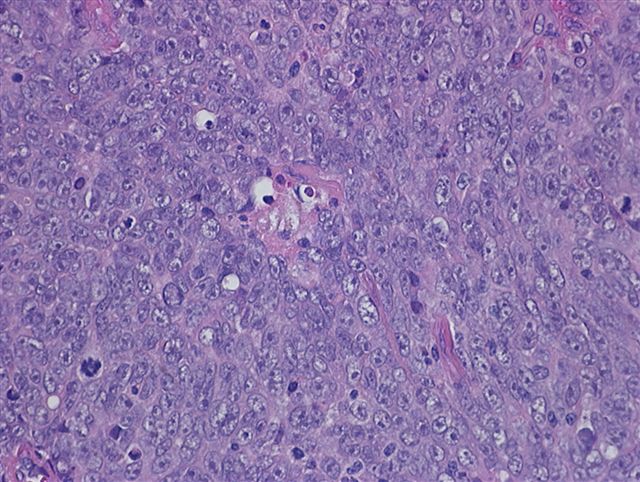
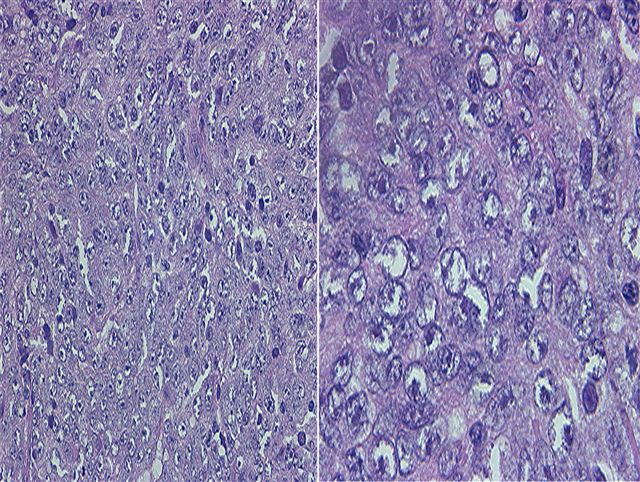
Microscopic examination revealed a neoplastic process that was composed of solid nests or islands of round or polygonal neoplastic epithelial cells encased within a dense narrow fibrous stroma (Figures 1 and 2). A few patches of lymphocytes were dispersed between the islands and admixed with the neoplastic epithelial cells (Figure 3). The epithelial tumor cells showed overt atypia, manifested by pleomorphism, nuclear enlargement, hyperchromasia and nucleolar prominence with increased mitotic activity (Figures 4 and 5).
Immunohistochemistry description:
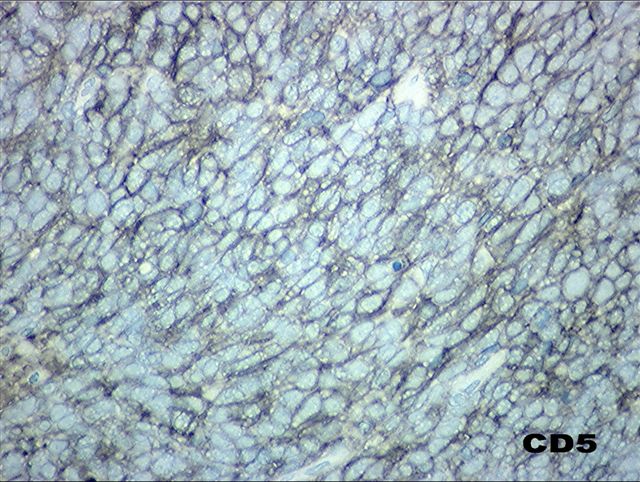
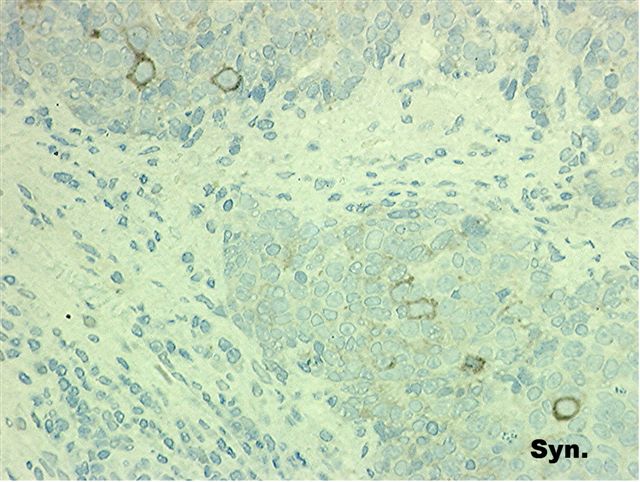
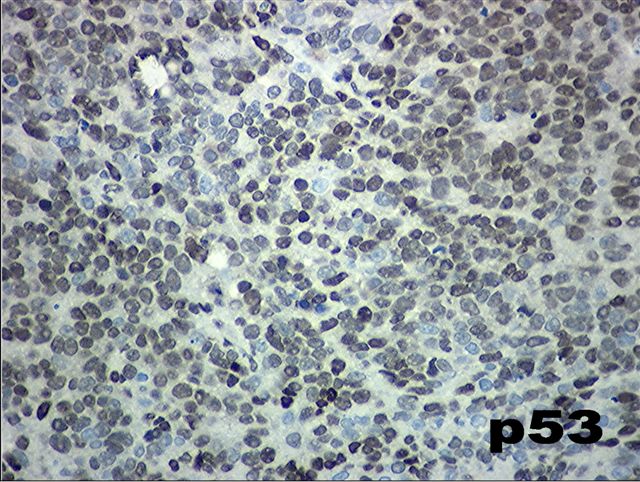
Immunohistochemical staining showed that the tumor cells were diffusely positive for CD5 (Figure 6). Scattered single cells were reactive to synaptophysin (Figure 7). More than 60% of the tumor cells overexpressed p53 (Figure 8). The tumor cells were not immunoreactive for cytokeratin 7, cytokeratin 20 and thyroid transcription factor 1 (TTF1). Excisional biopsy of the supraclavicular lymph node revealed a neoplastic process that was morphologically and immunohistochemically identical to the tumor in the mediastinal mass.
Microscopic images:
What is your diagnosis?
Diagnosis: Thymic carcinoma (type C thymoma), nonkeratinizing squamous cell carcinoma type
Immunohistochemistry images:
Negative immunostains (images not available):
CK7, CK20, TTF1
Discussion:
Thymic carcinoma is a rare tumor, account for only 0.06% of all thymic neoplasms. Most patients are age 40 through 60 years. 90% occur in the anterosuperior mediastinum. It may be associated with elevated parathyroid hormone levels and hypercalcemia, as well as pulmonary sarcoidosis. It is typically not associated with paraneoplastic syndromes such as myasthenia gravis or pure red cell aplasia.
Histologically, it is an epithelial tumor that exhibits marked cytologic atypia and features that are not specific to the thymus. Lymphocytes are the nonneoplastic component and often exhibit the phenotype of mature T cells (i.e., CD5+).
In 1999, the World Health Organization (WHO) classified epithelial thymic tumors into 6 types: A, AB, B1, B2, B3 and C, which correlate with clinical features (Am J Surg Pathol 2001;25:103, Am J Surg Pathol 2002;26:1605). Thymic carcinoma is included in this classification system as type C thymoma and it should be differentiated from other types. Type A thymoma is composed of medullary type thymic epithelial cells accompanied by few, if any, nonneoplastic lymphocytes. Features suggestive of medullary differentiation may also be present, including rosette-like structures and abortive Hassall corpuscles. Type AB thymoma has the features of type A thymoma but with numerous lymphocytes. Type B1 thymoma contains areas resembling thymic cortex with cortical type epithelial cells (plump and rounded) and areas resembling thymic medulla with medullary type epithelial cells (spindle shaped), all admixed with numerous lymphocytes. Type B2 thymoma resembles type B1 thymoma in its predominance of lymphocytes but foci of medullary differentiation are less conspicuous or absent. Type B3 thymoma has a sheet-like growth of round or polygonal epithelial cells that exhibit no or mild atypia, admixed with a minor component of lymphocytes.
Type C thymoma or thymic carcinoma exhibits clear cut cytologic atypia and histologic features observed in carcinomas of other organs but not specific to the thymus. These include keratinizing squamous cell, nonkeratinizing squamous cell, lymphoepithelioma-like, sarcomatoid, clear cell, basaloid squamous, mucoepidermoid, mucinous, neuroendocrine and anaplastic carcinomas. The differential diagnosis of thymic carcinoma includes metastases from the lung, trachea, bronchi, esophagus or other sites, which are much more common. It also includes other mediastinal tumors, such as lymphoma and germ cell tumor. CD5 and CD70 immunoreactivity are present in most thymic versus nonthymic carcinomas (Am J Surg Pathol 1997;21:936 - CD5, Am J Surg Pathol 2000;24:742 - CD70 tested on frozen tissue). In addition, thymic carcinomas have higher p53 expression, although this is not specific. Most thymic carcinomas exhibit focal neuroendocrine differentiation.
Thymic carcinomas have aggressive behavior. They are typically invasive and advanced at diagnosis with higher recurrence rates and worse prognoses than thymomas. Metastatic sites of thymic carcinoma include mediastinal lymph nodes and less commonly other thoracic lymph nodes. Extrathoracic metastasis is rare. Treatment of thymic carcinoma depends on tumor stage and includes radiation therapy and chemotherapy, with or without surgery (Ann Hematol 2003;82:69, Cancer 2002;94:3115).
In the current case, the patient presented with an advanced stage of thymic carcinoma, nonkeratinizing squamous cell carcinoma type that has aggressive behavior. The tumor in this patient was surgically incurable and therefore radiotherapy was considered.
Reference: Rosai: Histological Typing of Tumours of the Thymus, 2nd Edition, 1999
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Osama M. Al-Agha, SUNY Downstate Medical Center, Brooklyn, New York, USA and Dr. Jotica Talwar, Staten Island University Hospital, Staten Island, New York, USA.
Website news:
(1) This week's case is sponsored by Invitrogen. Invitrogen offers Zymed total system solution for pathology reagents and automation. From antibodies, kits and probes for IHC and CISH to immunostainers for automation, you can be confident that Zymed products will always deliver high quality staining results and offer the cutting edge pathology solutions you need. (Note: sponsors do NOT have access to email addresses or other personal information in the possession of PathologyOutlines.com.)
Visit and follow our Blog to see recent updates to the website.
(1) This week's case is sponsored by Invitrogen. Invitrogen offers Zymed total system solution for pathology reagents and automation. From antibodies, kits and probes for IHC and CISH to immunostainers for automation, you can be confident that Zymed products will always deliver high quality staining results and offer the cutting edge pathology solutions you need. (Note: sponsors do NOT have access to email addresses or other personal information in the possession of PathologyOutlines.com.)
Visit and follow our Blog to see recent updates to the website.
Case #17
Clinical history:
A 61 year old woman presented with chest tightness, intermittent shortness of breath and right supraclavicular lymph node enlargement. Radiologic studies revealed an anterosuperior mediastinal mass measuring 5 x 4 x 4 cm with mediastinal lymphadenopathy. The patient underwent CT guided needle biopsy for the mediastinal mass.
Microscopic description:
Microscopic examination revealed a neoplastic process that was composed of solid nests or islands of round or polygonal neoplastic epithelial cells encased within a dense narrow fibrous stroma (Figures 1 and 2). A few patches of lymphocytes were dispersed between the islands and admixed with the neoplastic epithelial cells (Figure 3). The epithelial tumor cells showed overt atypia, manifested by pleomorphism, nuclear enlargement, hyperchromasia and nucleolar prominence with increased mitotic activity (Figures 4 and 5).
Immunohistochemistry description:
Immunohistochemical staining showed that the tumor cells were diffusely positive for CD5 (Figure 6). Scattered single cells were reactive to synaptophysin (Figure 7). More than 60% of the tumor cells overexpressed p53 (Figure 8). The tumor cells were not immunoreactive for cytokeratin 7, cytokeratin 20 and thyroid transcription factor 1 (TTF1). Excisional biopsy of the supraclavicular lymph node revealed a neoplastic process that was morphologically and immunohistochemically identical to the tumor in the mediastinal mass.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Thymic carcinoma (type C thymoma), nonkeratinizing squamous cell carcinoma type
Immunohistochemistry images:
Negative immunostains (images not available):
CK7, CK20, TTF1
Discussion:
Thymic carcinoma is a rare tumor, account for only 0.06% of all thymic neoplasms. Most patients are age 40 through 60 years. 90% occur in the anterosuperior mediastinum. It may be associated with elevated parathyroid hormone levels and hypercalcemia, as well as pulmonary sarcoidosis. It is typically not associated with paraneoplastic syndromes such as myasthenia gravis or pure red cell aplasia.
Histologically, it is an epithelial tumor that exhibits marked cytologic atypia and features that are not specific to the thymus. Lymphocytes are the nonneoplastic component and often exhibit the phenotype of mature T cells (i.e., CD5+).
In 1999, the World Health Organization (WHO) classified epithelial thymic tumors into 6 types: A, AB, B1, B2, B3 and C, which correlate with clinical features (Am J Surg Pathol 2001;25:103, Am J Surg Pathol 2002;26:1605). Thymic carcinoma is included in this classification system as type C thymoma and it should be differentiated from other types. Type A thymoma is composed of medullary type thymic epithelial cells accompanied by few, if any, nonneoplastic lymphocytes. Features suggestive of medullary differentiation may also be present, including rosette-like structures and abortive Hassall corpuscles. Type AB thymoma has the features of type A thymoma but with numerous lymphocytes. Type B1 thymoma contains areas resembling thymic cortex with cortical type epithelial cells (plump and rounded) and areas resembling thymic medulla with medullary type epithelial cells (spindle shaped), all admixed with numerous lymphocytes. Type B2 thymoma resembles type B1 thymoma in its predominance of lymphocytes but foci of medullary differentiation are less conspicuous or absent. Type B3 thymoma has a sheet-like growth of round or polygonal epithelial cells that exhibit no or mild atypia, admixed with a minor component of lymphocytes.
Type C thymoma or thymic carcinoma exhibits clear cut cytologic atypia and histologic features observed in carcinomas of other organs but not specific to the thymus. These include keratinizing squamous cell, nonkeratinizing squamous cell, lymphoepithelioma-like, sarcomatoid, clear cell, basaloid squamous, mucoepidermoid, mucinous, neuroendocrine and anaplastic carcinomas. The differential diagnosis of thymic carcinoma includes metastases from the lung, trachea, bronchi, esophagus or other sites, which are much more common. It also includes other mediastinal tumors, such as lymphoma and germ cell tumor. CD5 and CD70 immunoreactivity are present in most thymic versus nonthymic carcinomas (Am J Surg Pathol 1997;21:936 - CD5, Am J Surg Pathol 2000;24:742 - CD70 tested on frozen tissue). In addition, thymic carcinomas have higher p53 expression, although this is not specific. Most thymic carcinomas exhibit focal neuroendocrine differentiation.
Thymic carcinomas have aggressive behavior. They are typically invasive and advanced at diagnosis with higher recurrence rates and worse prognoses than thymomas. Metastatic sites of thymic carcinoma include mediastinal lymph nodes and less commonly other thoracic lymph nodes. Extrathoracic metastasis is rare. Treatment of thymic carcinoma depends on tumor stage and includes radiation therapy and chemotherapy, with or without surgery (Ann Hematol 2003;82:69, Cancer 2002;94:3115).
In the current case, the patient presented with an advanced stage of thymic carcinoma, nonkeratinizing squamous cell carcinoma type that has aggressive behavior. The tumor in this patient was surgically incurable and therefore radiotherapy was considered.
Reference: Rosai: Histological Typing of Tumours of the Thymus, 2nd Edition, 1999