Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Practice question #1 | Practice answer #1Cite this page: Pfahl E, Perrino CM, Zynger DL. Ganglioneuroma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/adrenalganglioneuroma.html. Accessed August 26th, 2025.
Definition / general
- Mature, benign neoplasm of the adrenal gland that is composed predominantly of Schwannian stroma with admixed mature ganglion cells
Essential features
- Neural crest cell derived, benign tumor
- Majority are nonfunctional and are thus found incidentally
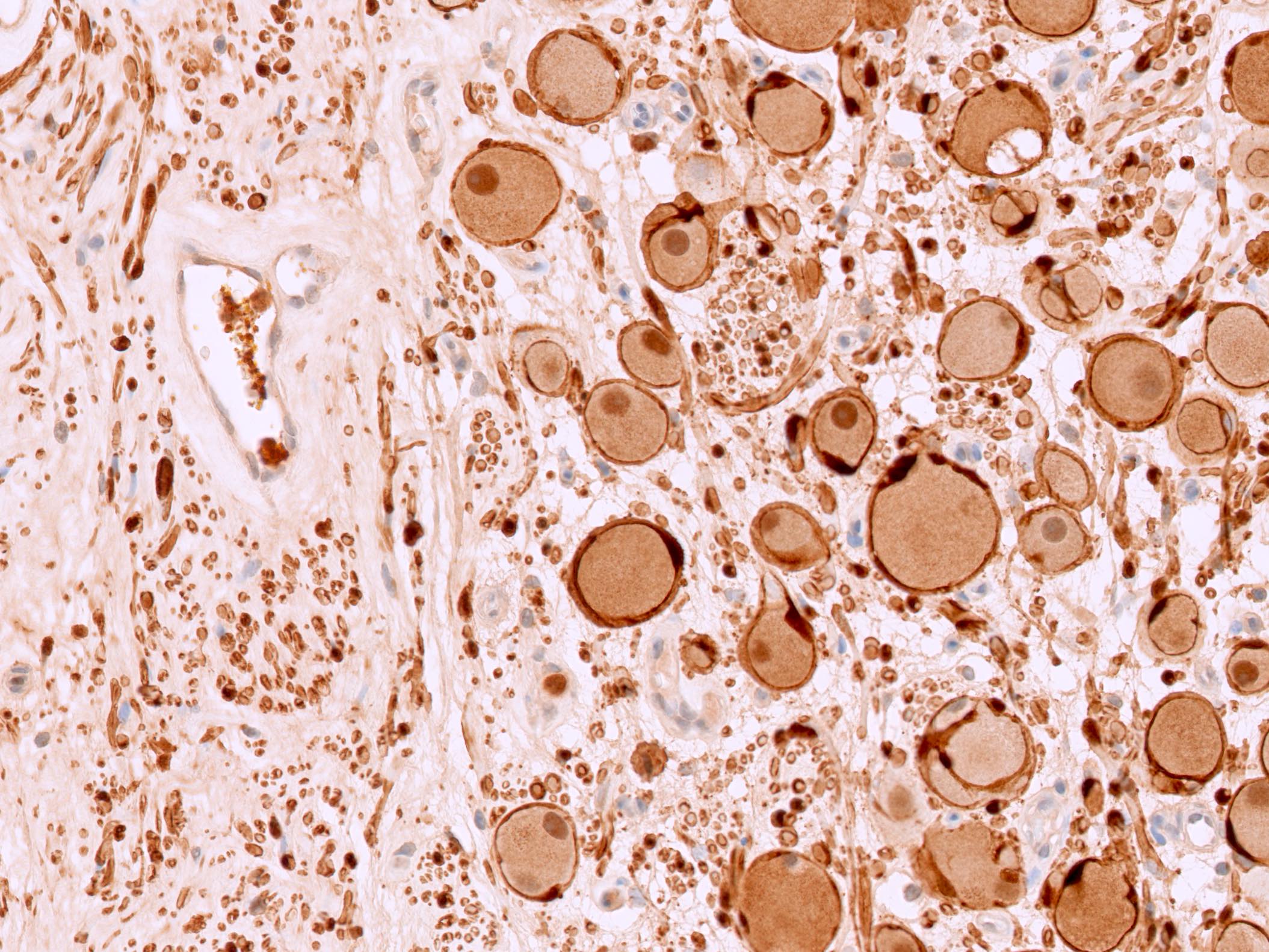
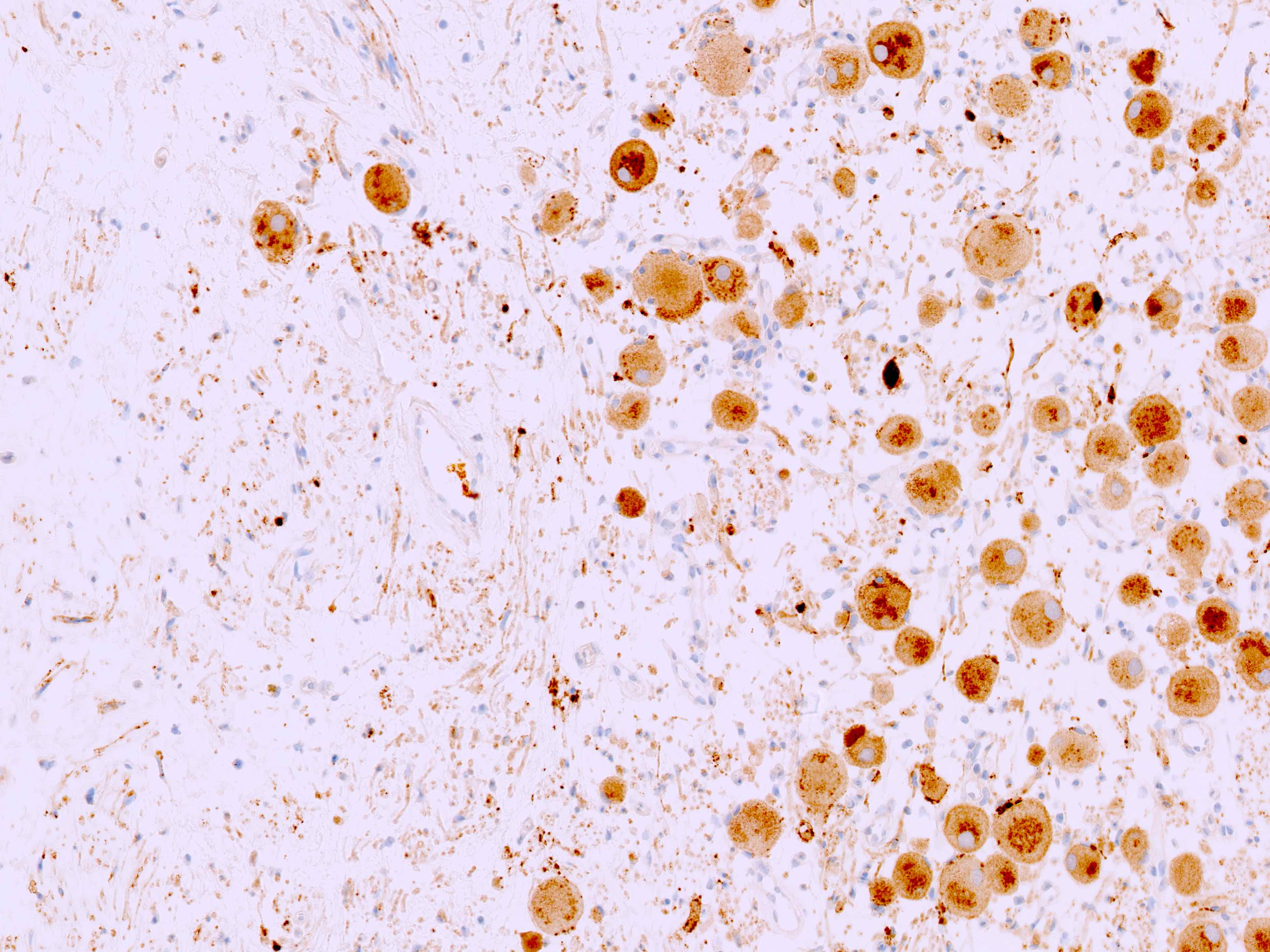
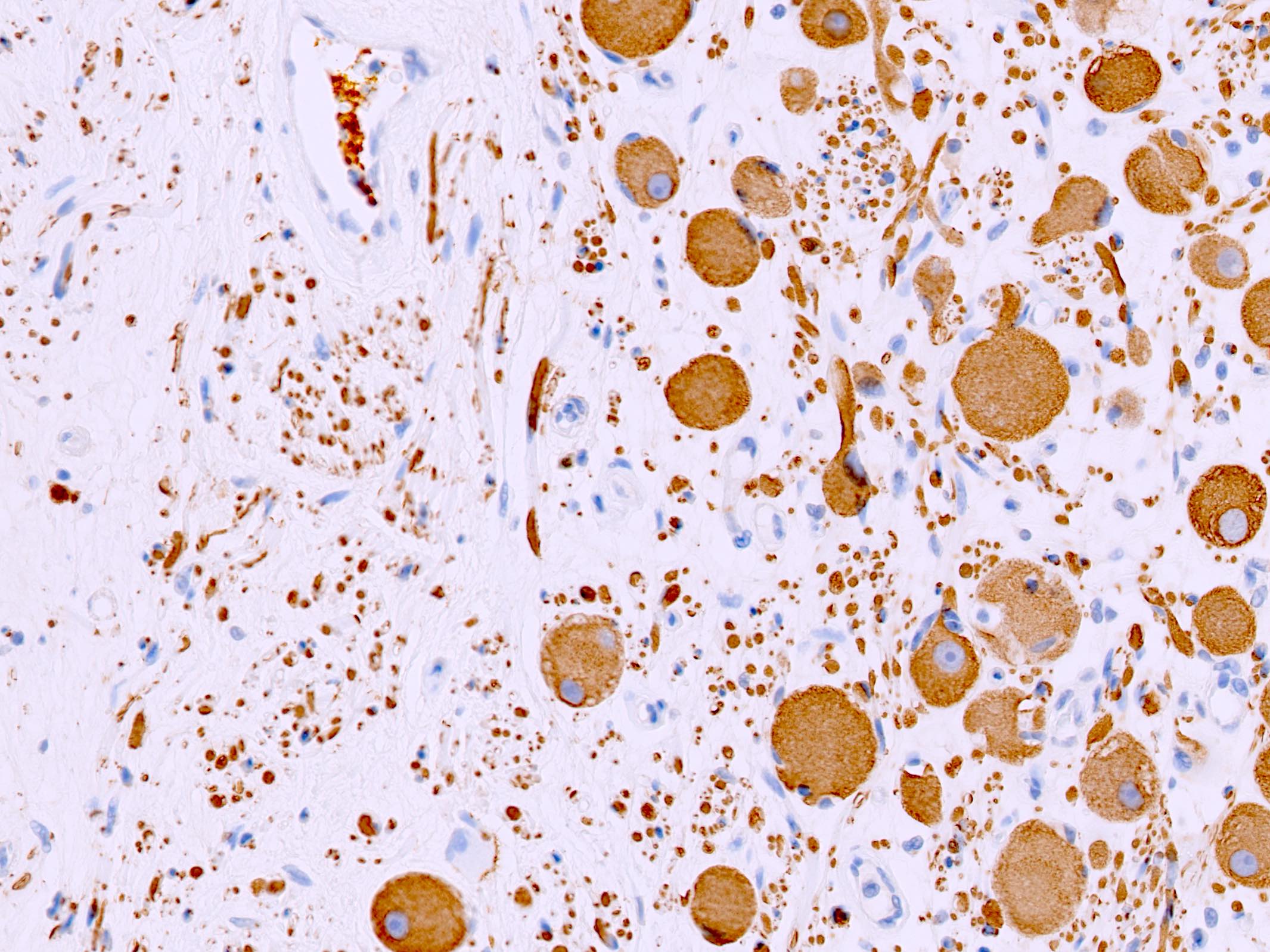
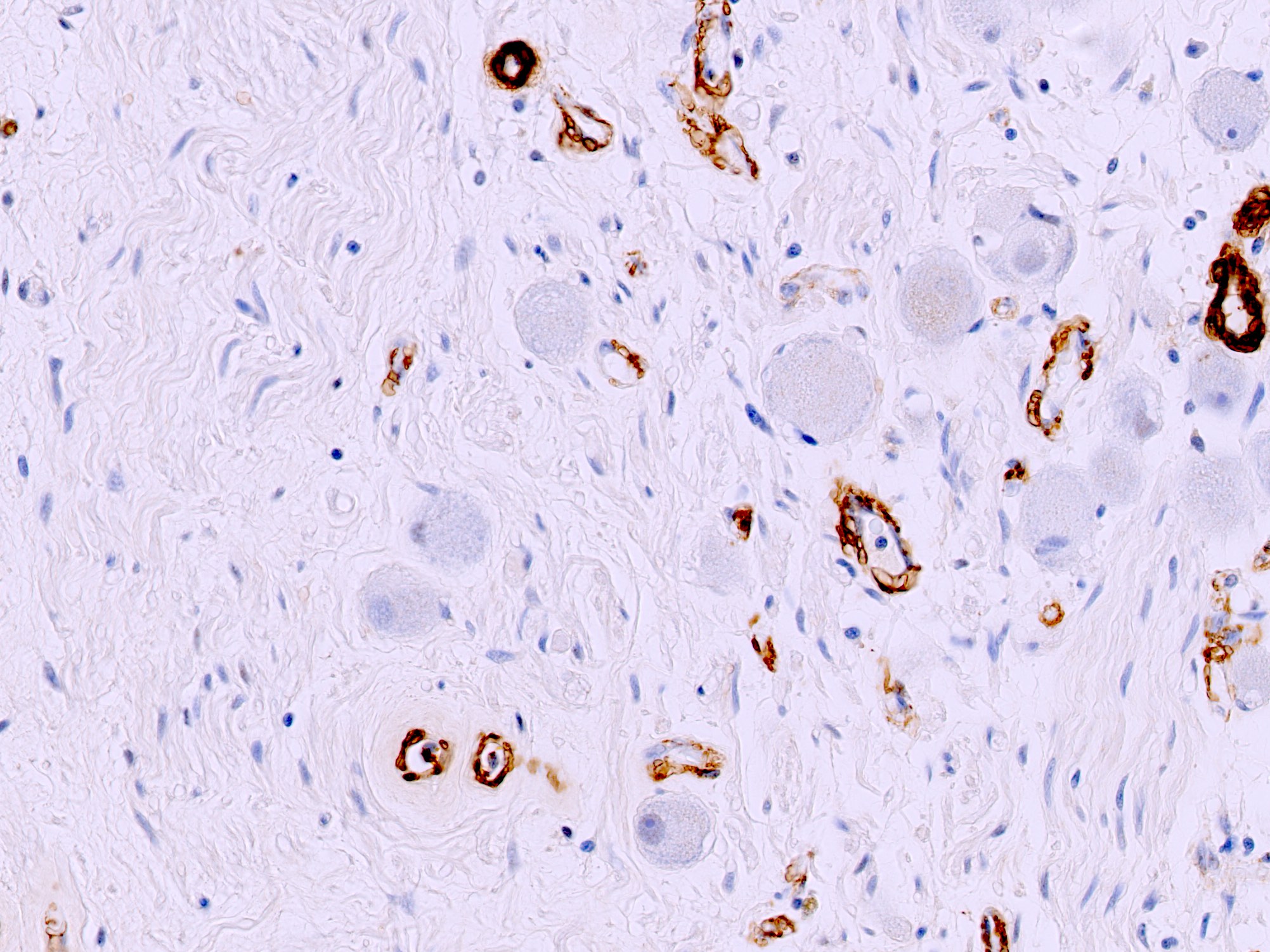
- Admixture of ganglion and Schwann cells on histology, both of which typically stain positive for S100 and synaptophysin, with predominance of Schwannian stroma
- Treatment is adrenalectomy with excellent prognosis
ICD coding
Epidemiology
- 1.5 - 2.9% of all adrenal tumors (J Endocrinol Invest 2015;38:547, Ann Surg Treat Res 2021;101:79, Am J Transl Res 2022;14:7528, Int J Surg 2017;41:S103)
- Incidence: ~1 per 1 million (J Endocrinol Invest 2015;38:547)
- Mean age: 35 - 41 years (median: 35 - 40), in contrast to tumors within the retroperitoneum or posterior mediastinum, which usually occur in a pediatric population (Endocr Pract 2014;20:864, Am J Transl Res 2022;14:7528, Ann Surg Treat Res 2021;101:79, J Endocrinol Invest 2015;38:547, J Int Med Res 2020;48:300060520945510, Int J Surg 2017;41:S103, Eur Rev Med Pharmacol Sci 2013;17:1110)
- Higher frequency in men than women (data from case series in the last decade with at least 30 patients: 69%, 59% and 47% male) (Am J Transl Res 2022;14:7528, World J Surg 2018;42:2469, J Int Med Res 2020;48:300060520945510)
Sites
- Located anywhere along the distribution of sympathetic nervous system, including neck, posterior mediastinum, retroperitoneum, pelvis and adrenal gland / periadrenal adipose (described in this topic) (J Endocrinol Invest 2015;38:547)
- Most commonly in posterior mediastinum and retroperitoneum (Clin Endocrinol (Oxf) 2014;80:342)
- In adrenal, possible higher rate in right adrenal (52 - 72%); rarely bilateral (0 - 4%) (Ann Surg Treat Res 2021;101:79, Am J Transl Res 2022;14:7528, Eur Rev Med Pharmacol Sci 2013;17:1110, World J Surg 2018;42:2469, J Int Med Res 2020;48:300060520945510)
Pathophysiology
- Clonal proliferation of cells of neural crest origin (Ann Surg Treat Res 2021;101:79)
Etiology
- No known risk factors
Clinical features
- 63 - 77% are asymptomatic and are discovered incidentally upon imaging (Am J Transl Res 2022;14:7528, World J Surg 2018;42:2469, J Int Med Res 2020;48:300060520945510)
- Most common nonspecific symptom is abdominal pain (10 - 25%) (Am J Transl Res 2022;14:7528, World J Surg 2018;42:2469, J Int Med Res 2020;48:300060520945510)
- Uncommonly, catecholamine synthesis may cause hypertension (2.4 - 12%) (Endocr Pract 2014;20:864, Am J Transl Res 2022;14:7528, Ann Surg Treat Res 2021;101:79, J Int Med Res 2020;48:300060520945510)
- Very rarely, cases have been reported to secrete testosterone and dopamine with associated symptoms of hormonal overproduction (Gland Surg 2020;9:2204)
Diagnosis
- Adrenalectomy with histopathological examination is the gold standard for diagnosis (J Endocrinol Invest 2015;38:547, Ann Surg Treat Res 2021;101:79, Endocr Pract 2014;20:864)
Laboratory
- Infrequently increased catecholamines or catecholamine metabolites in urine (3.9 - 4.8%) (Am J Transl Res 2022;14:7528, World J Surg 2018;42:2469)
Radiology description
- Ultrasound
- Well defined, homogeneous, hypoechogenic mass (Endocr Pract 2014;20:864)
- Computed tomography (CT)
- Circumscribed and well defined (Am J Transl Res 2022;14:7528)
- Hypodense, homogeneous or slightly heterogeneous lesion (Ann Surg Treat Res 2021;101:79)
- May have fine / punctate calcifications (16 - 33%) (J Int Med Res 2020;48:300060520945510, Am J Transl Res 2022;14:7528, World J Surg 2018;42:2469)
- Magnetic resonance imaging (MRI)
- T1: homogeneous, hypointense signal (Int J Surg 2017;41:S103)
- T2: heterogeneous, high signal intensity (Int J Surg 2017;41:S103)
Radiology images
Prognostic factors
- Benign tumor with excellent prognosis following adrenalectomy (Ann Surg Treat Res 2021;101:79)
- No reported recurrence in any case series published in the last decade (World J Surg 2018;42:2469, Am J Transl Res 2022;14:7528, J Endocrinol Invest 2015;38:547, Ann Surg Treat Res 2021;101:79)
- Rare (< 20) case reports of transformation to malignant peripheral nerve sheath tumor (MPNST), occurring both with and without a history of abdominal radiation (Pathology 2015;47:595)
Case reports
- 18 year old woman presented with abdominal pain and adrenal mass (AACE Clin Case Rep 2020;7:61)
- Woman in her mid 20s presented with adrenal mass and hypertension (Cureus 2023;15:e39977)
- 53 year old man presented with hypochondrial pain and adrenal lesion (Acta Biomed 2023;94:e2023263)
- 70 year old woman with dopamine secreting symptomatic ganglioneuroma (Gland Surg 2020;9:2204)
Treatment
- Complete adrenalectomy, via laparoscopic or open approach (World J Surg 2018;42:2469, Am J Transl Res 2022;14:7528, J Int Med Res 2020;48:300060520945510)
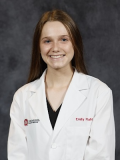
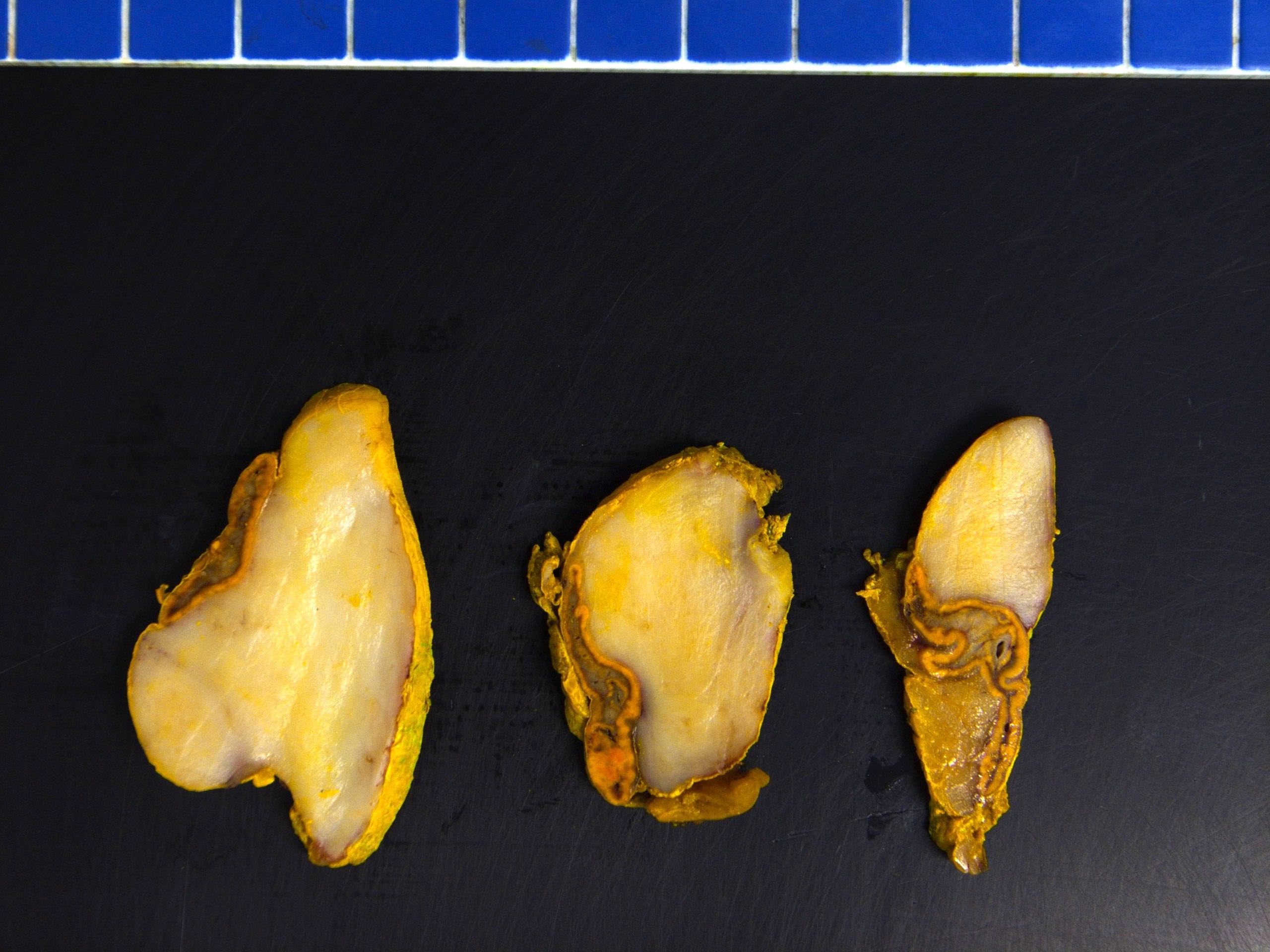
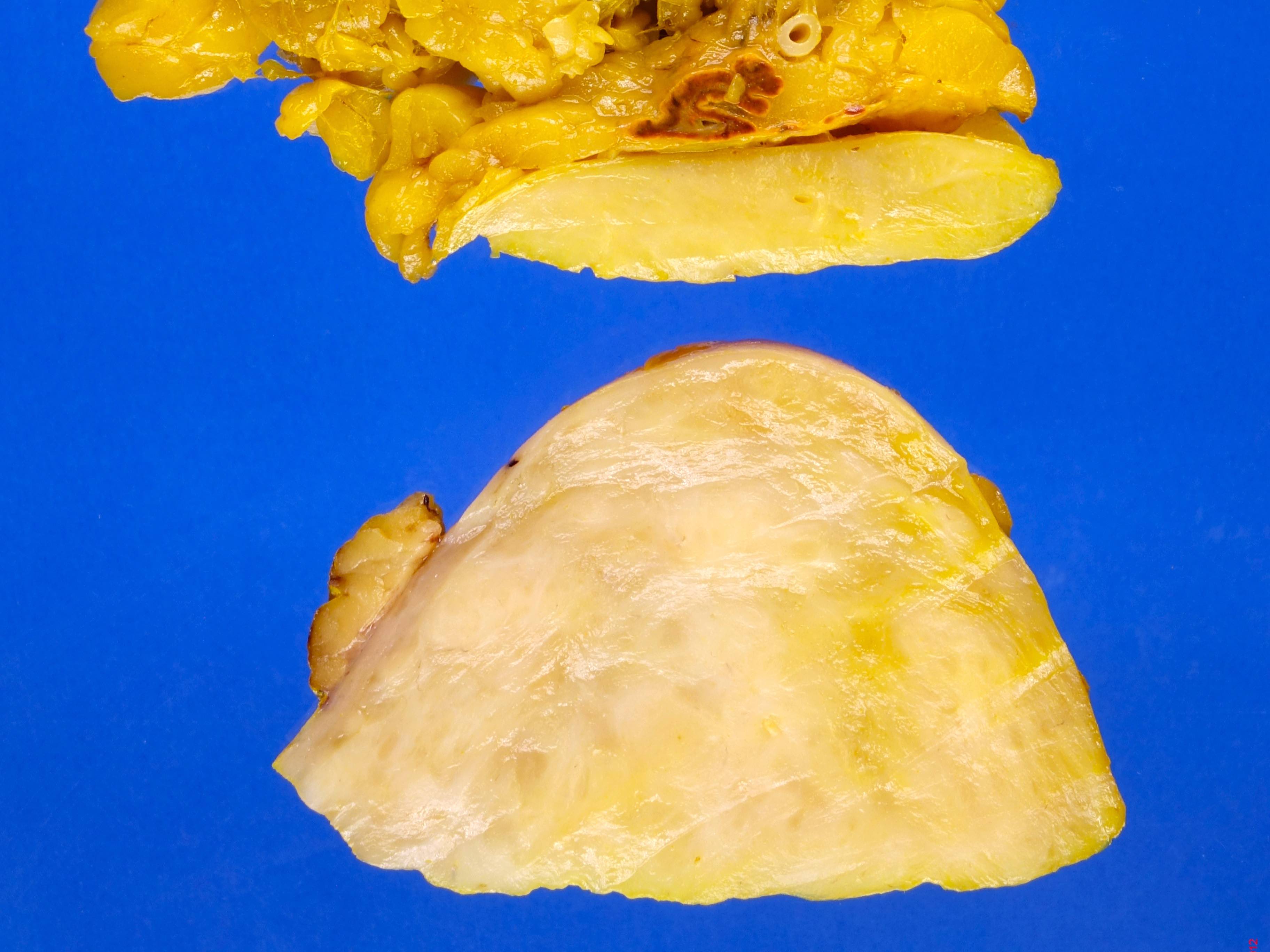
Gross description
- Well circumscribed, firm, encapsulated, gray-white or yellow-brown lesion (Am J Case Rep 2022;23:e936138, Am J Transl Res 2022;14:7528, World J Surg 2018;42:2469)
- Mean tumor size: 6.1 - 7 cm (median: 8 cm) (Ann Surg Treat Res 2021;101:79, Am J Transl Res 2022;14:7528, Endocr Pract 2014;20:864)
- Median weight: 180 - 210 g (Clin Endocrinol (Oxf) 2014;80:342, Am J Transl Res 2022;14:7528)
Gross images
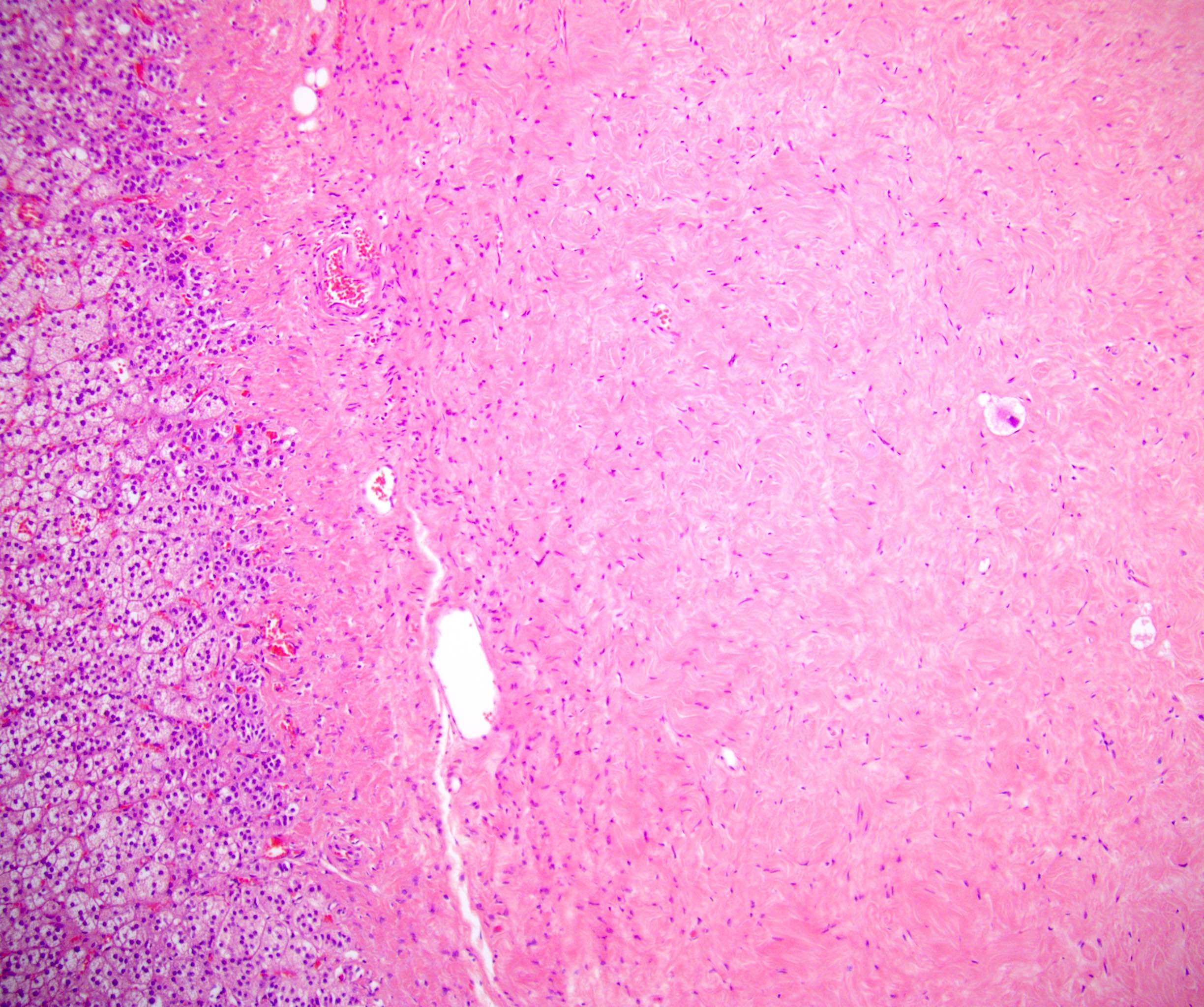
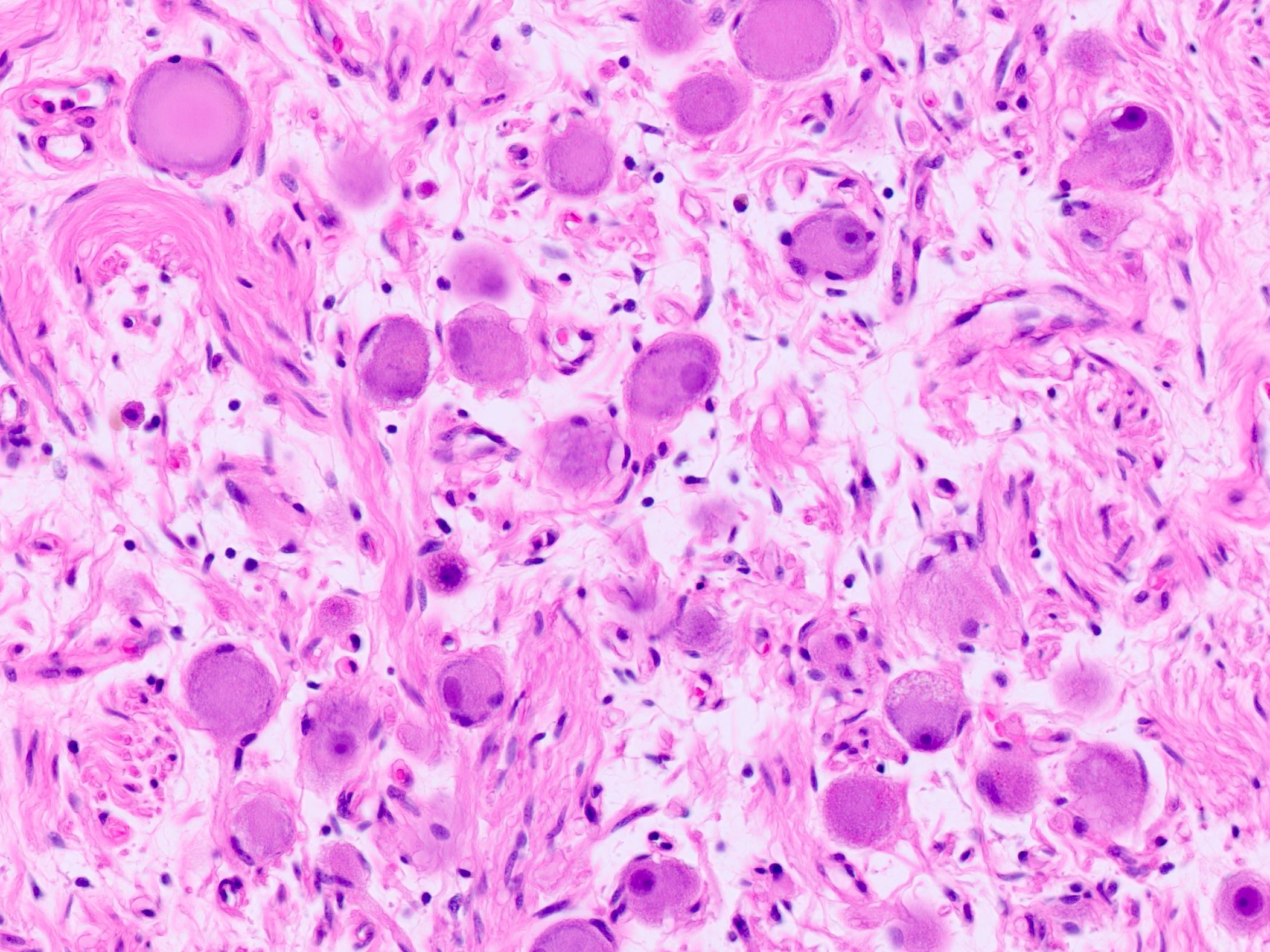
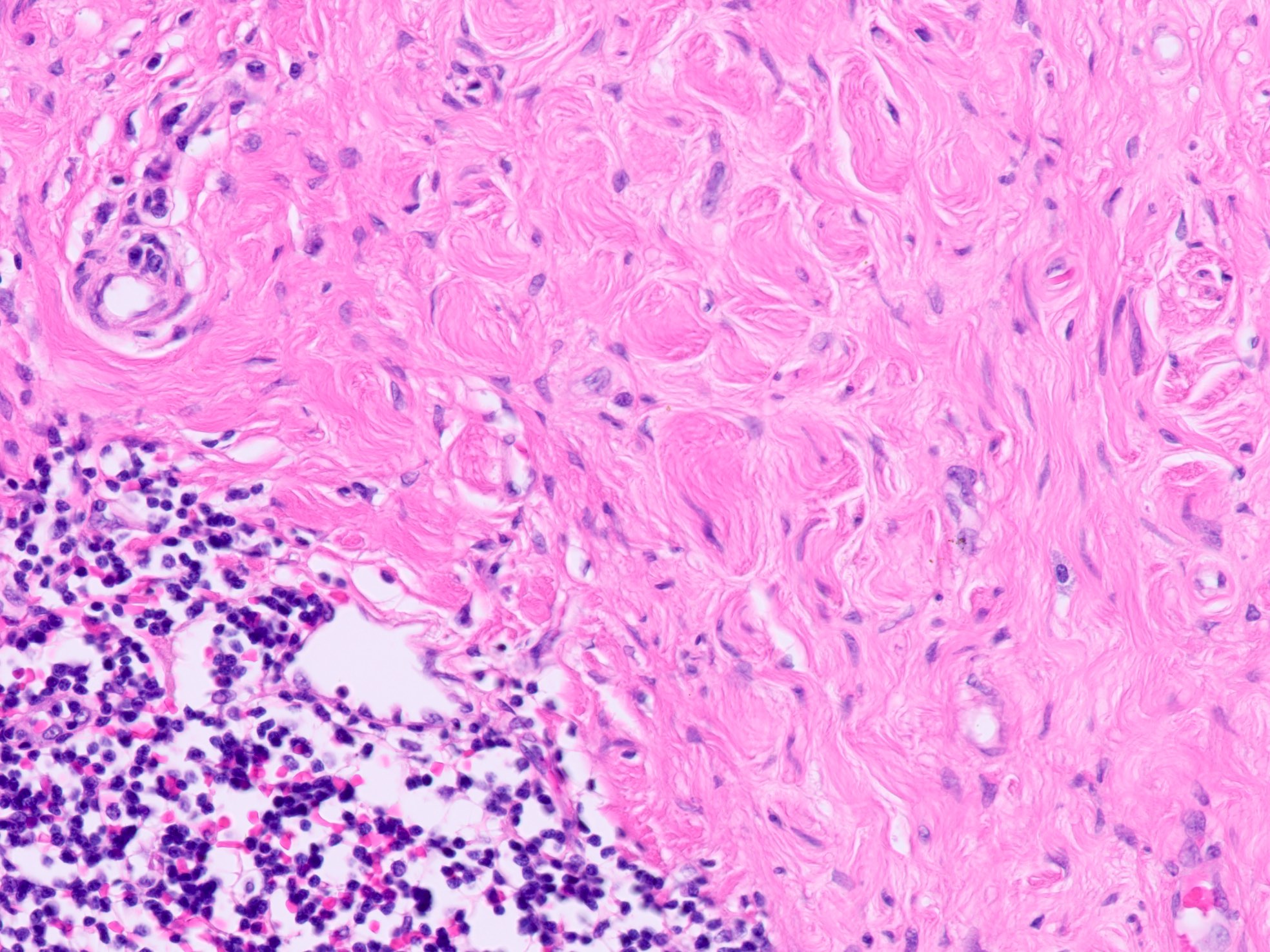
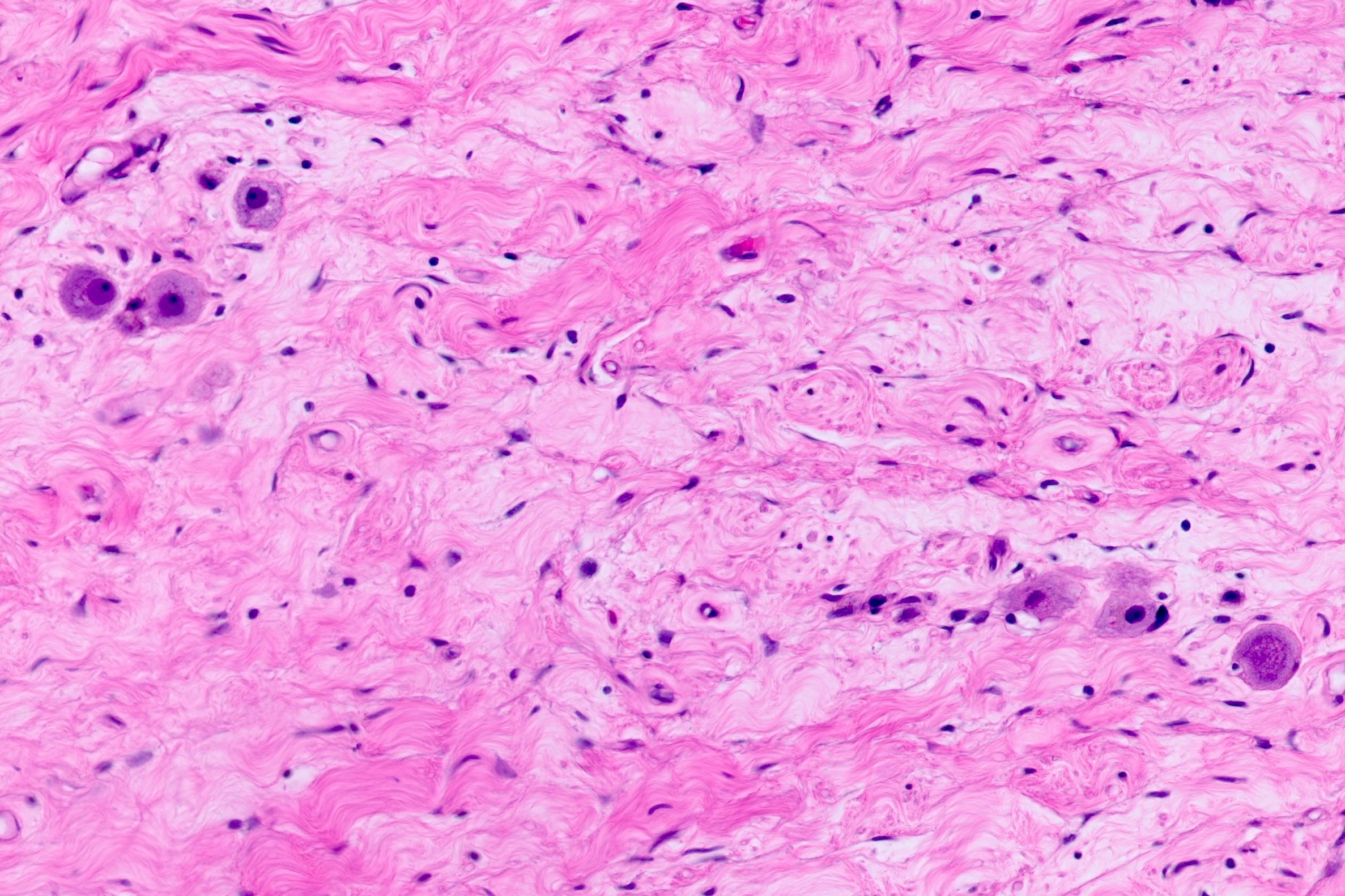
Microscopic (histologic) description
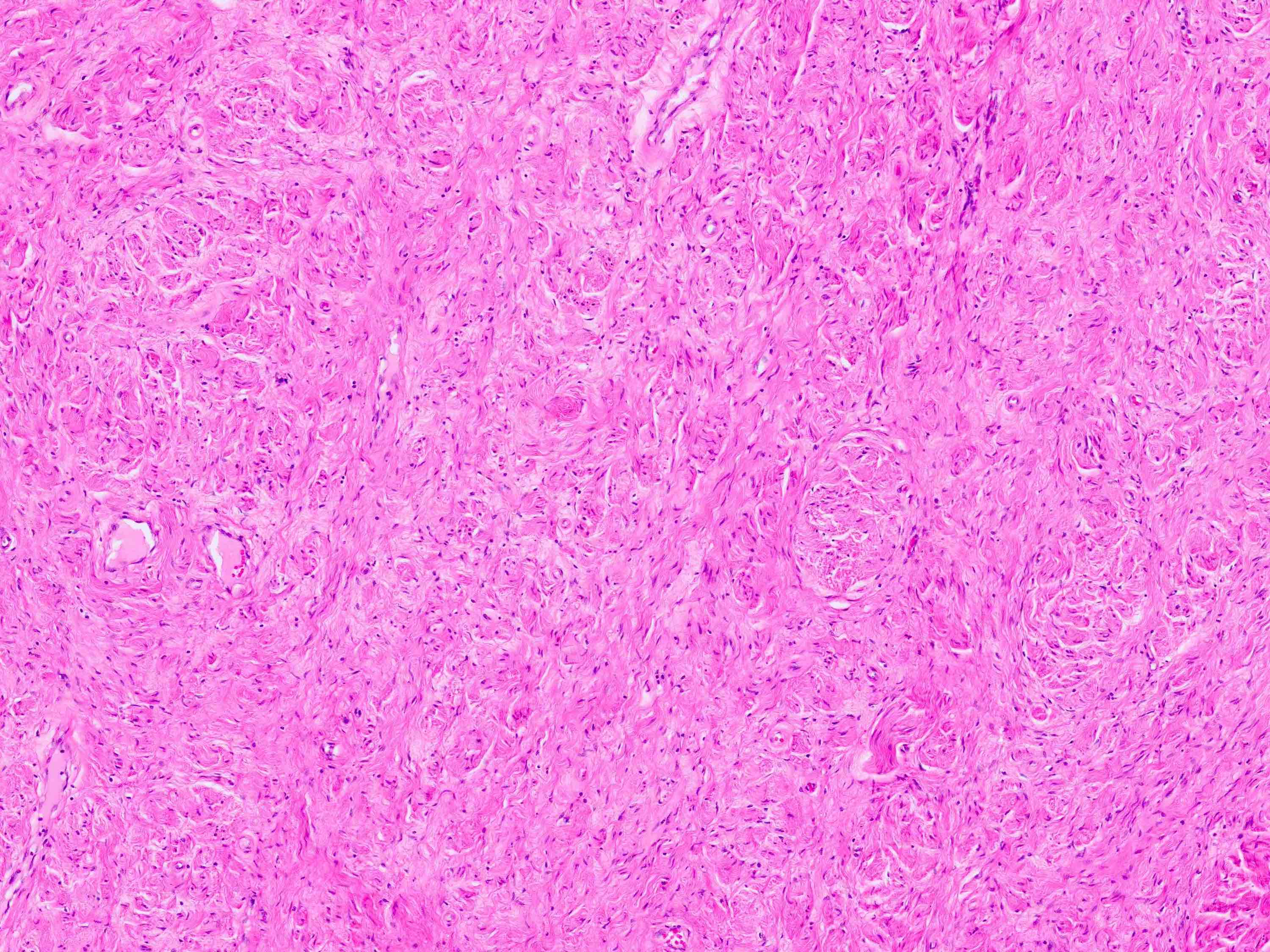
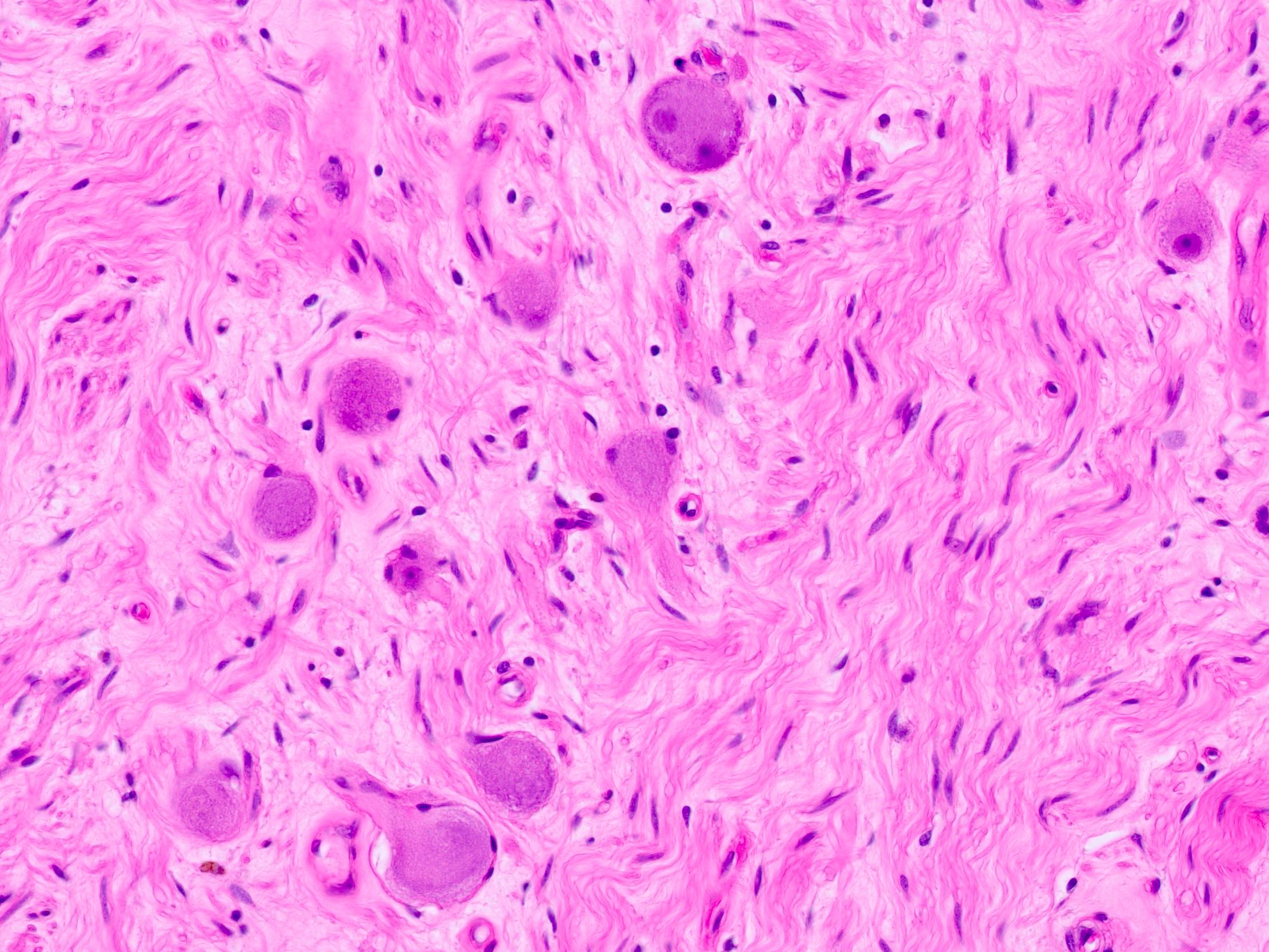
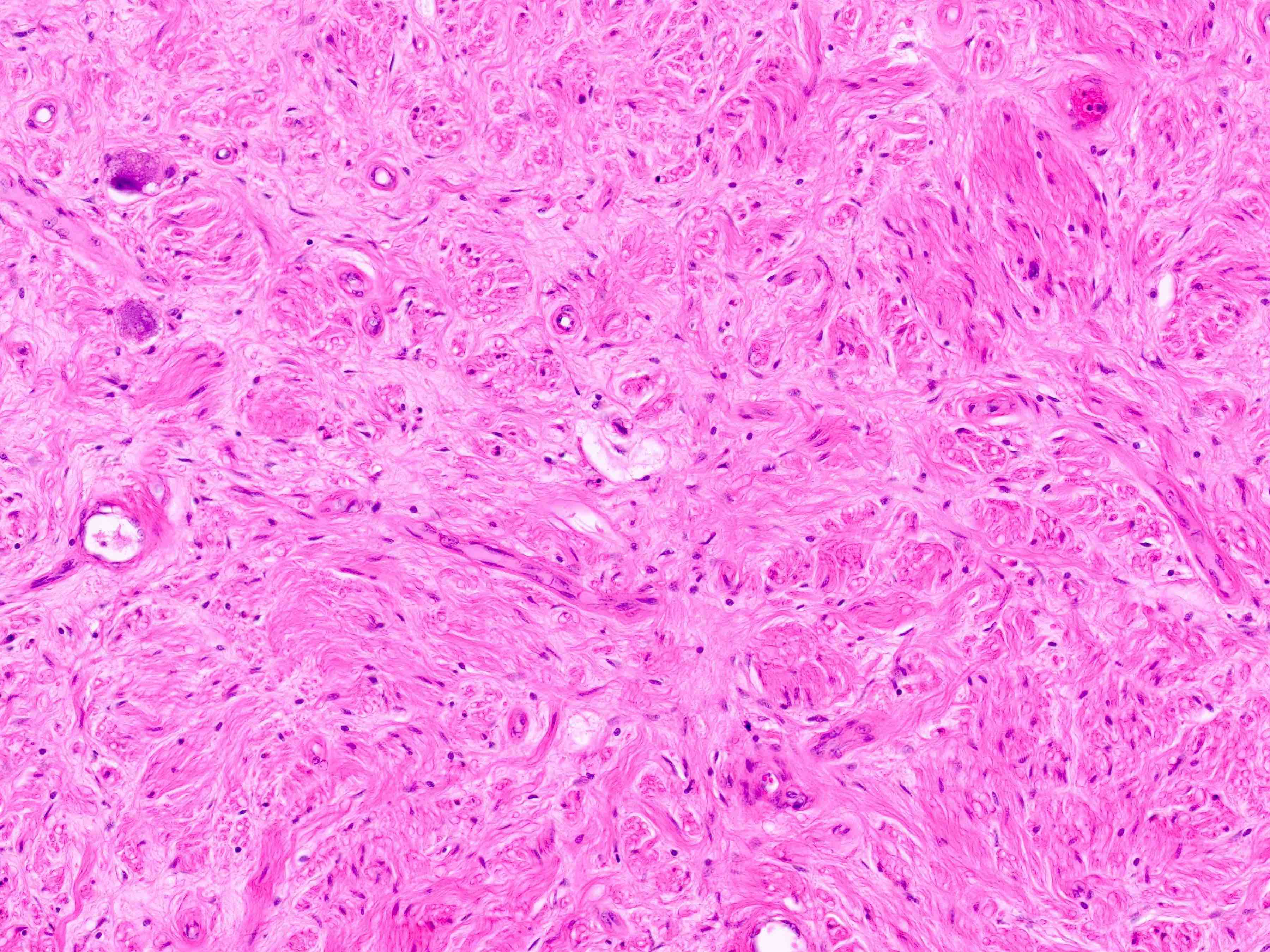
- Admixture of Schwann cells and ganglion cells with predominance of Schwannian stroma (Schwannian stroma dominant)
- No naked neuropil and no neuroblastic foci or nodules (World J Surg 2018;42:2469)
- Schwann cells
- Loose, fibrillary, homogenous, eosinophilic stroma
- Spindle cells with elongated bland nuclei
- Ensheaths neuritic processes
- May be arranged in small intersecting fascicles
- Ganglion cells
- 2 histologic subtypes depending on appearance of ganglion cells
- Mature type: every ganglion cell is mature with compact, granular, eosinophilic cytoplasm that may contain neuromelanin and Nissel substance, distinct cell borders, single, eccentric, round nucleus and prominent nucleolus
- Maturing type: minor component of scattered collections of maturing ganglion cells that do not form discrete nests or nodules
- May contain finely granular, gold to brown pigment (lipofuscin or neuromelanin)
- Background may include lobules of mature adipose tissue (especially at periphery of lesion), mast cells, chronic inflammation and dense collagenized stroma
- Mild variation in cellularity is permitted
- No significant atypia, mitoses or necrosis should be present
- Composite tumor: rare, usually ganglioneuroma with pheochromocytoma (see Composite pheochromocytoma)
Microscopic (histologic) images
Cytology description
- Large, scattered polyhedral ganglion cells with abundant cytoplasm, large nuclei and fibrillary stroma with wavy spindle shaped cells and cigar shaped nuclei (Diagn Cytopathol 2022;50:E146, Acta Cytol 1987;31:33)
Positive stains
Negative stains
- EMA
- WT1 (negative for nuclear staining with cytoplasmic staining seen in ganglion)
- References: Cesk Patol 2012;48:215, J Pediatr Surg 2011;46:326
Molecular / cytogenetics description
- Ganglioneuromas are not usually associated with genetic abnormalities (Clin Endocrinol (Oxf) 2014;80:342)
- Role of RET and relationship with multiple endocrine neoplasia is uncertain
- Mutational analysis negative in 4 cases (1 ganglioneuroma, 3 composite pheochromocytoma with ganglioneuroma) (J Clin Endocrinol Metab 2010;95:3118)
- RET expressed at low level in 1 of 3 ganglioneuromas (J Mol Med (Berl) 1996;74:617)
- 1 patient with medullary thyroid carcinoma, ganglioneuroma and multiple endocrine neoplasia type 2A (MEN2A) had RET codon 634 mutation (Clin Endocrinol (Oxf) 2014;80:342)
- 2 pediatric patients (1 with MEN2A, 1 with MEN2B) had ganglioneuroma and no pheochromocytoma (J Clin Endocrinol Metab 2005;90:4383)
- MEN2A and MEN2B have rarely been associated with composite pheochromocytoma with ganglioneuroma (Am J Surg Pathol 1997;21:102)
- Aberrant methylation in MGMT, TIMP3a and p16INK4a in a few cases (Eur J Cancer 2003;39:1478)
- Allelic loss at chromosome 1p in 1 case (Eur J Cancer 2003;39:1478)
Videos
Microscopic features
Gross features
Sample pathology report
- Right adrenal, total laparoscopic adrenalectomy:
- Ganglioneuroma, mature type, 4.2 cm (see comment)
- Surgical margins negative for tumor
- Comment: The tumor is composed of mostly fibrillary stroma with occasional mature ganglion. The stroma and ganglion cells express S100 and synaptophysin. No naked neuropil is present. No maturing ganglion cells or neuroblastic cells are present.
Differential diagnosis
- Ganglioneuroblastoma:
- Immature neuroblasts present and form a nodule or admixed distinct clusters in a background of Schwannian stroma
- Careful tissue sampling and histologic examination is required for differentiating from maturing ganglioneuroma
- Composite pheochromocytoma with ganglioneuroma:
- Pheochromocytoma component is also present, which is composed of nests of amphophilic to basophilic cells with granular cytoplasm
- Neurofibroma:
- Much more likely to be seen subcutaneous, along a nerve trunk or in the head / neck
- Ganglion cells are absent
- Collagenous stroma
- Schwannoma:
- Most commonly in limbs or in the head / neck
- Ganglion cells are absent
- Hypercellular and hypocellular areas with Verocay bodies
- Peripheral ganglion:
- Ganglion cells admixed with organized nerve fibers rather than haphazard Schwann cells
- Does not form a mass lesion
- May not be able to differentiate in limited biopsy tissue
Practice question #1
Practice answer #1
C. Ganglioneuroma. The histology slide shows scattered mature ganglion cells in a background of bland stroma diagnostic for ganglioneuroma. Answer A is incorrect because ganglion cells are present and large bland adrenal cortical cells are not present. Answer B is incorrect because immature neuroblasts would be seen. Answer D is incorrect because neuroblastomas show small round blue cells with minimal cytoplasm that are not present. Answer E is incorrect because ganglion cells are present and nests of basophilic granular cells are not seen.
Comment Here
Reference: Ganglioneuroma
Comment Here
Reference: Ganglioneuroma