Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Gonzalez RS. Adenocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/anusadenocarcinoma.html. Accessed October 2nd, 2025.
Definition / general
- Rare adenocarcinoma that arises within the anal canal
- Several WHO recognized clinicopathologic subtypes have been described
Essential features
- Rare, primary, gland forming malignancy of the anus
- Subtypes include
- Mucosal
- Extramucosal anal gland
- Extramucosal fistula associated
- Extramucosal non-anal gland non-fistula associated
- Must be distinguished from adenocarcinoma secondarily involving anus (generally rectal carcinoma)
Terminology
- Also known as perianal adenocarcinoma or perianal gland adenocarcinoma
- Anal duct adenocarcinoma is not a recommended term
ICD coding
Epidemiology
- 5% of anorectal malignancies (JCO Oncol Pract 2020;16:635)
- Slightly more common in White men (Cancer Med 2019;8:3855)
Sites
- Anus (by definition; may require clinical confirmation)
Pathophysiology
- Cases deemed mucosal anal adenocarcinomas may arise from transitional mucosa between anus and rectum or may actually arise in the rectum and spread downward (JCO Oncol Pract 2020;16:635)
- Extramucosal cases may arise from anal glands, from congenital anorectal duplications or along a fistula tract (Dis Colon Rectum 1998;41:992)
- Rare, mucosa based cases are linked to high risk human papillomavirus (HPV) infection (Mod Pathol 2020;33:944, Int J Surg Pathol 2021;29:672, Br J Cancer 2018;118:1302)
Etiology
- Proposed etiologic associations include chronic fistula, anal Crohn's disease and anal sexual intercourse (Semin Surg Oncol 1994;10:235)
- Though rare, chronic fistulas in patients with Crohn's disease can become malignant, potentially due to long term injury and repair of the intestinal tract or prolonged immunosuppression (J Gastrointest Surg 2010;14:66)
Clinical features
- Typical symptoms include anal pain, anal bleeding or mass sensation
- For some patients, particularly those with inflammatory bowel disease, the cancer arises in a perianal fistula (Ann Surg Oncol 2023;30:3517)
- Poor prognosis; 5 and 10 year survival rates around 5% in one series (Colorectal Dis 2013;15:1481)
- Early evidence suggests that HPV associated cases may have better prognoses (Mod Pathol 2020;33:944)
Diagnosis
- Gross examination and tissue sampling
Prognostic factors
- Poor prognosis associated with advanced T and N category disease and higher histologic grade (Int J Radiat Oncol Biol Phys 2003;56:1274)
Case reports
- 42 year old man with anal tenderness (Medicine (Baltimore) 2021;100:e27083)
- 70 year old man with firm perianal nodule (BMJ Open Gastroenterol 2021;8:e000661)
- 71 year old man with anal bleeding (Pathol Int 2021;71:715)
- 72 year old man with Crohn's disease and perianal fistula (Cureus 2022;14:e31339)
- 84 year old man with adenocarcinoma arising from an anal gland (Int J Surg Case Rep 2014;5:234)
Treatment
- Standard treatment includes abdominoperineal resection; adding chemotherapy and radiation improves outcome (Int J Radiat Oncol Biol Phys 2003;56:1274)
- National Comprehensive Cancer Network (NCCN) recommends following their guidelines for rectal cancer when treating anal adenocarcinoma (NCCN Guidelines: Anal Carcinoma [Accessed 24 February 2024])
- Therefore, neoadjuvant therapy is often given
Gross description
- Anal canal tumors are nodular, ulcerated and 3 - 4 cm or more; they invade deeply into wall and spread proximally and distally into the submucosa of the distal rectum and proximal anus
Gross images
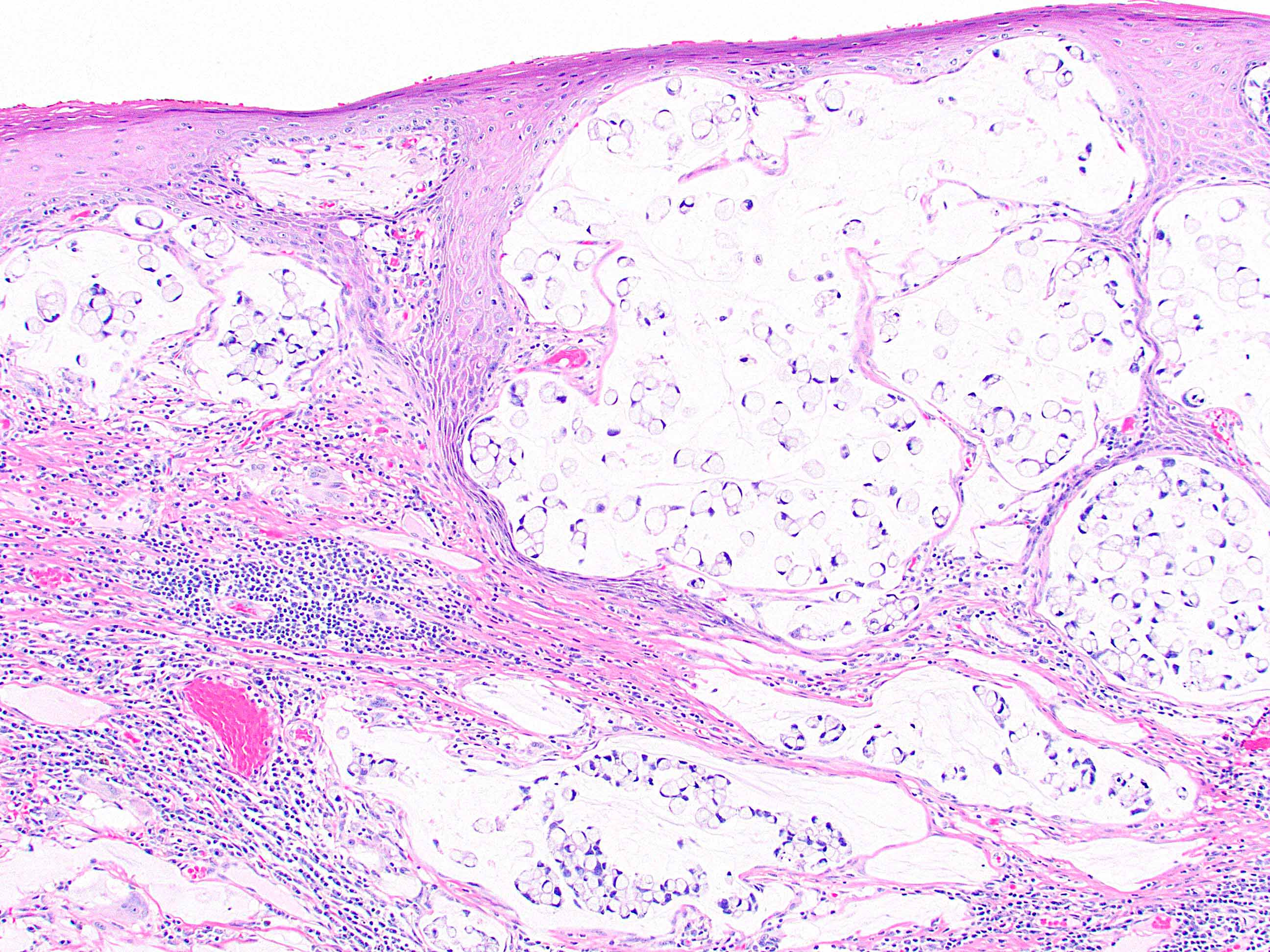
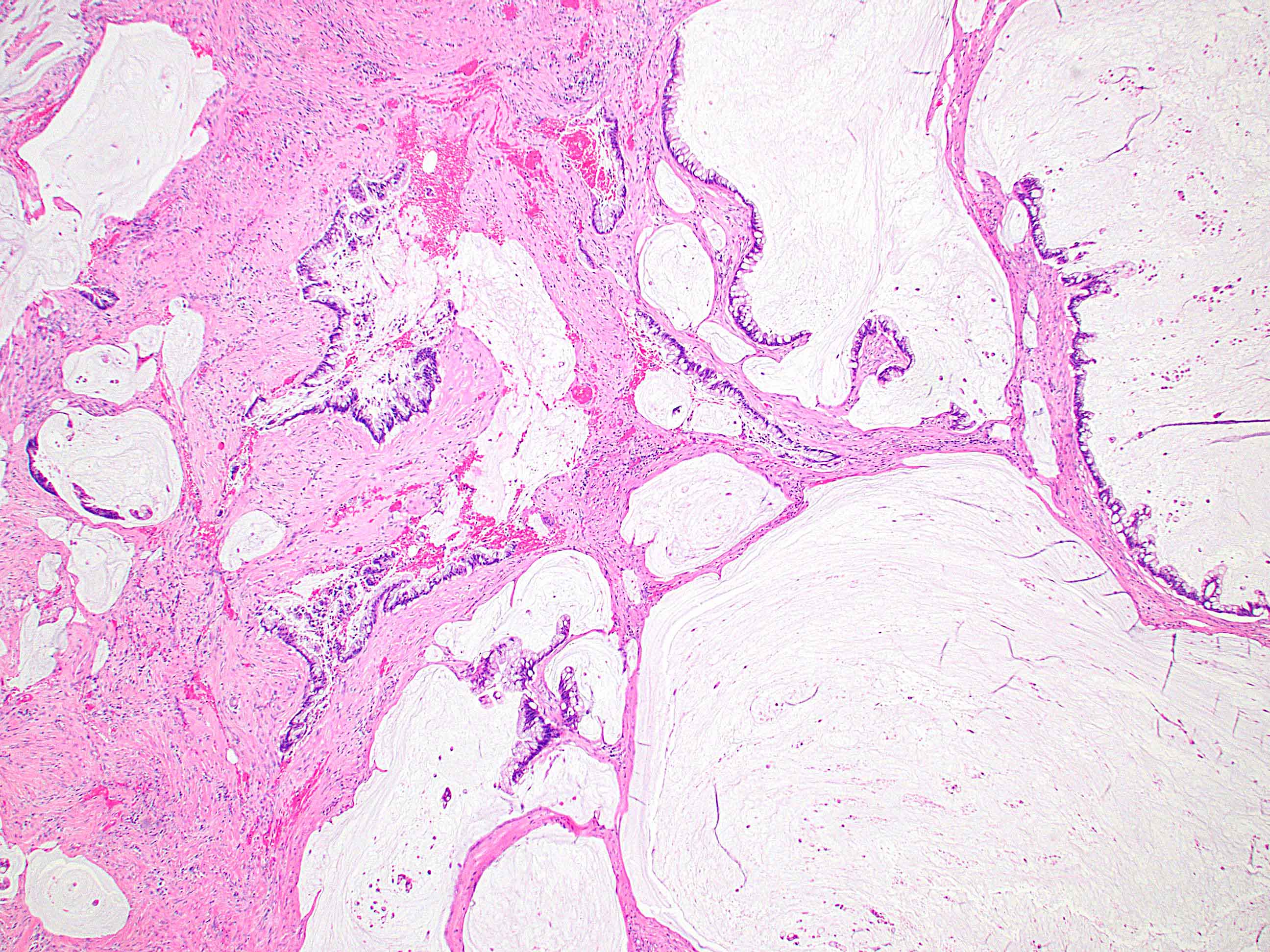
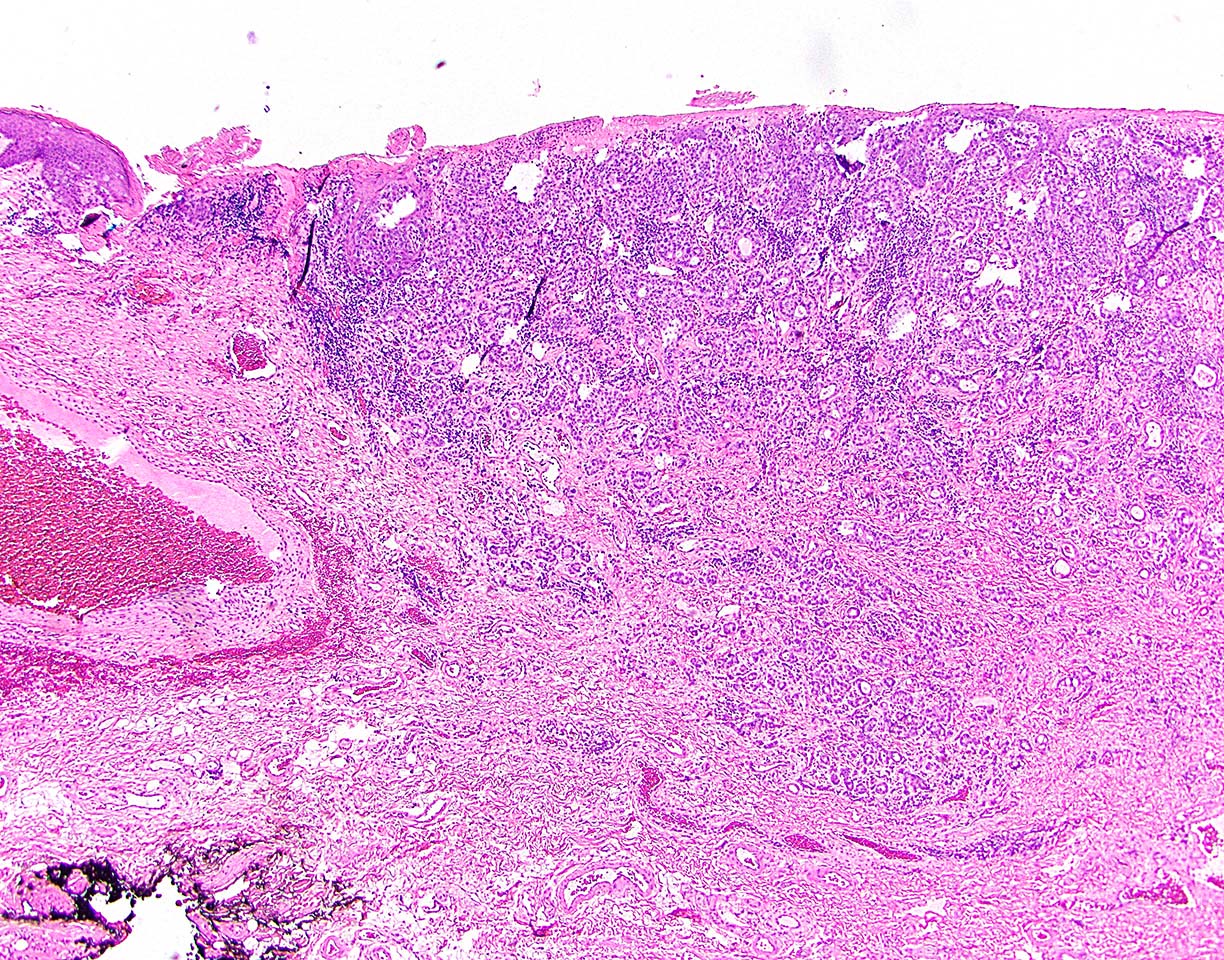
Microscopic (histologic) description
- 4 subtypes have been described based on tumor origin
- Mucosal anal adenocarcinomas arise from the mucosal surface and have an intestinal appearance mimicking rectal adenocarcinoma (e.g., pencillate nuclei, amphophilic cytoplasm, cribriforming, some degree of mucin)
- Some of these are perhaps of rectal origin but may be deemed anal adenocarcinomas clinically
- Extramucosal anal gland adenocarcinomas form haphazardly dispersed small glands with scant mucin production that invade the wall of the anorectal area without an intraluminal component; overlying epithelium may be intact or secondarily involved (Cancer 2001;92:2045)
- Some cases may demonstrate abundant mucin or signet ring cells
- Extramucosal fistula associated adenocarcinomas are often mucinous (> 50% of tumor volume consists of mucin) and generally have an intestinal appearance otherwise
- Extramucosal non-anal gland non-fistula associated adenocarcinomas can vary histologically but often have a somewhat intestinal appearance without involving the mucosal surface
- Mucosal anal adenocarcinomas arise from the mucosal surface and have an intestinal appearance mimicking rectal adenocarcinoma (e.g., pencillate nuclei, amphophilic cytoplasm, cribriforming, some degree of mucin)
- HPV related cases show papillary or villiform structures lined by columnar cells that often contain abundant mucin (Mod Pathol 2020;33:944)
- Single neoplastic cells may colonize the overlying and adjacent squamous mucosa (extramammary Paget disease) (Int J Surg Pathol 2021;29:672)
- These have not yet been strictly assigned to one of the above subtypes
Microscopic (histologic) images
Contributed by Raul S. Gonzalez, M.D. and Xiaoyan Liao, M.D., Ph.D.
Positive stains
- CK7 positive primarily in anal gland type, occasionally in other types (Cancer 2001;92:2045, Hum Pathol 2012;43:216)
- CK20 and CDX2 positive primarily in mucosal type, extramucosal non-anal gland non-fistula type, possibly fistula type (Ann Surg Oncol 2023;30:3517, Histopathology 2018;73:157)
- p16 strongly positive in HPV associated cases (Mod Pathol 2020;33:944)
Negative stains
- CK7 can be negative in mucosal type and extramucosal non-anal gland non-fistula type
- CK20 and CDX2 often negative in anal gland type
- p16 generally negative in cases not associated with HPV (Arch Pathol Lab Med 2007;131:1304)
Molecular / cytogenetics description
- KRAS mutations in 47% of cases and NRAS mutations in 6% of cases (Br J Cancer 2018;118:1302)
- Fistula associated cases show mutations in TP53, among other genes (Ann Surg Oncol 2023;30:3517)
Sample pathology report
- Anus, resection:
- Extramucosal anal gland adenocarcinoma, moderately differentiated (3.1 cm, pT2) (see synoptic report and comment)
- Pagetoid spread focally present in background squamous mucosa
- Margins of resection negative for malignancy
- Lymphovascular invasion present
- Perineural invasion not identified
- No lymph nodes present in specimen
- Comment: Immunostains show the carcinoma is positive for CK7 and negative for CK20 and CDX2.
- Extramucosal anal gland adenocarcinoma, moderately differentiated (3.1 cm, pT2) (see synoptic report and comment)
Differential diagnosis
- Anal mucoepidermoid carcinoma:
- Rare (J Gastroenterol 2001;36:508)
- Composed of mucin producing cells, squamous cells and intermediate cells
- Secondary involvement by rectal adenocarcinoma:
- Squamous cell carcinoma:
- Far more common at this location
- Distinguishable microscopically by morphology and immunoprofile
- Secondary involvement by gynecologic tract adenocarcinoma:
Additional references
Practice question #1
Practice answer #1
D. They can arise in a fistula tract. This may occur in patients with Crohn's disease. Crohn's disease can lead to the development of chronic anal fistulas, which can eventually become malignant and develop into anal adenocarcinoma. Answer A is incorrect because advanced stage indicates a poor prognosis. Answer B is incorrect because anal adenocarcinoma is more common in men. Answer C is incorrect because anal adenocarcinomas are rare and secondary anal involvement by rectal carcinoma is more common.
Comment Here
Reference: Anal adenocarcinoma
Comment Here
Reference: Anal adenocarcinoma
Practice question #2
Extramucosal anal gland adenocarcinoma is usually positive for which of the following immunohistochemical stains?
- CDX2
- CK7
- CK20
- p16
Practice answer #2
B. CK7. Anal gland adenocarcinomas are often positive for CK7, supporting the diagnosis. Answers A and C are incorrect because anal gland adenocarcinomas are generally negative for CDX2 and CK20, unlike mucosal anal adenocarcinomas and fistula associated anal adenocarcinomas. Answer D is incorrect because anal gland adenocarcinoma is not often positive for p16; however, some mucosal based anal adenocarcinomas are strongly positive for p16 and also positive for HPV.
Comment Here
Reference: Anal adenocarcinoma
Comment Here
Reference: Anal adenocarcinoma