Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Kiran N, Mendoza P. Conjunctival intraepithelial neoplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/eyecinconj.html. Accessed August 12th, 2025.
Definition / general
- Spectrum of abnormal growth of atypical squamous epithelial cells of the conjunctiva; graded based on thickness of epithelial involvement
- Noninvasive; epithelial basement membrane remains intact
- Considered to be a premalignant lesion that can progress to invasive squamous cell carcinoma
Essential features
- Dysplastic changes of conjunctiva
- Precursor to squamous cell carcinoma
- Typical clinical presentation is a lesion at the limbus within the interpalpebral fissure
Terminology
- Conjunctival intraepithelial neoplasia (1, 2 or 3)
- Also called conjunctival dysplasia (mild, moderate or severe), conjunctival epithelial dyskeratosis, Bowen disease
- Falls within the broad spectrum of ocular surface squamous neoplasia (OSSN), which encompasses neoplastic squamous abnormalities of the conjunctival, limbal and corneal epithelium, including squamous cell carcinoma
ICD coding
Epidemiology
- Estimated incidence is 17 - 20 cases per 1 million person years (Arch Ophthalmol 1992;110:525)
- Incidence rate varies worldwide; highest rates in Africa (3.4 cases per 100,000 per year in Zimbabwe) (Trop Med Int Health 2013;18:1424)
- Reported incidence of OSSN was 0.53 cases/million/year (conjunctival intraepithelial neoplasia: 0.43 cases/million/year; squamous cell carcinoma: 0.08 cases/million/year) in the United Kingdom (Eye (Lond) 2019;33:283)
- Third most common conjunctival lesion in adults (after pterygium and nevus) (Cornea 1987;6:78)
- 2 disease patterns:
- In northern high latitude areas, mostly affects elderly males
- Close to the equator, males and females are equally affected at a younger age; also associated with HIV
- Occurs at a younger age and with more aggressive clinical course in patients with xeroderma pigmentosum and HIV (Graefes Arch Clin Exp Ophthalmol 2011;249:1217, Ophthalmology 2015;122:1688)
- HIV testing should be considered in patients < 40 years old with no other risk factors
- Risk factors include exposure to UV light, especially in light skinned individuals, human papillomavirus infection (HPV 16 / 18), immunosuppression, tobacco use, vitamin A deficiency, ocular surface injury and exposure to petroleum products (Ophthalmology 1994;101:360, Ophthalmology 2002;109:542, Cornea 2003;22:687)
Sites
- Typically occurs in the bulbar conjunctiva in the interpalpebral fissure (sun exposed area) arising at the limbus (where stem cells reside)
- Can spread onto the cornea
- Occasionally occurs in the forniceal or palpebral conjunctiva
- Reference: Am J Ophthalmol 2017;173:106
Pathophysiology
- Arises from conjunctival epithelial cells that originate from the ocular surface ectoderm
- Preferred limbal location suggests that most cases arise from limbal stem cells; limbal stem cells are sensitive to oncogenic factors and are susceptible to DNA alterations secondary to UV light
- Reference: Exp Eye Res 2014;129:172
Etiology
- Appears to be multifactorial, involving a variety of environmental factors in a susceptible host
- Acquired condition linked to chronic ultraviolet B radiation exposure
- Deficiency of DNA repair in xeroderma pigmentosum confers an increased risk
- Reference: Asia Pac J Ophthalmol (Phila) 2017;6:109
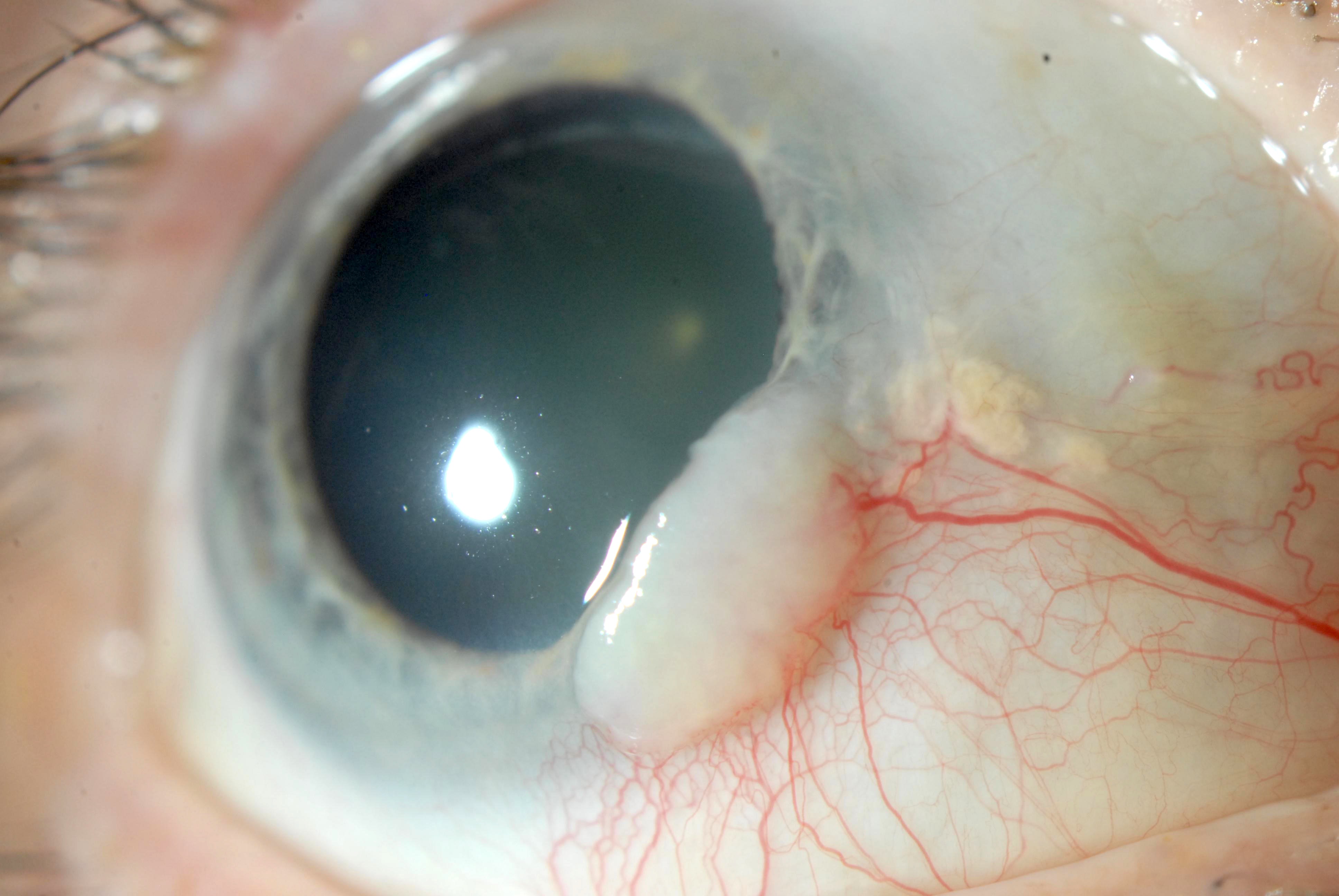
Clinical features
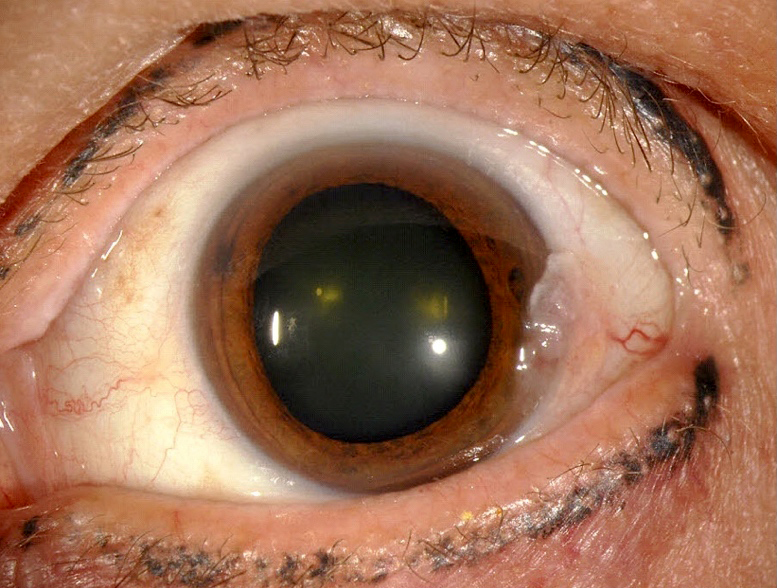
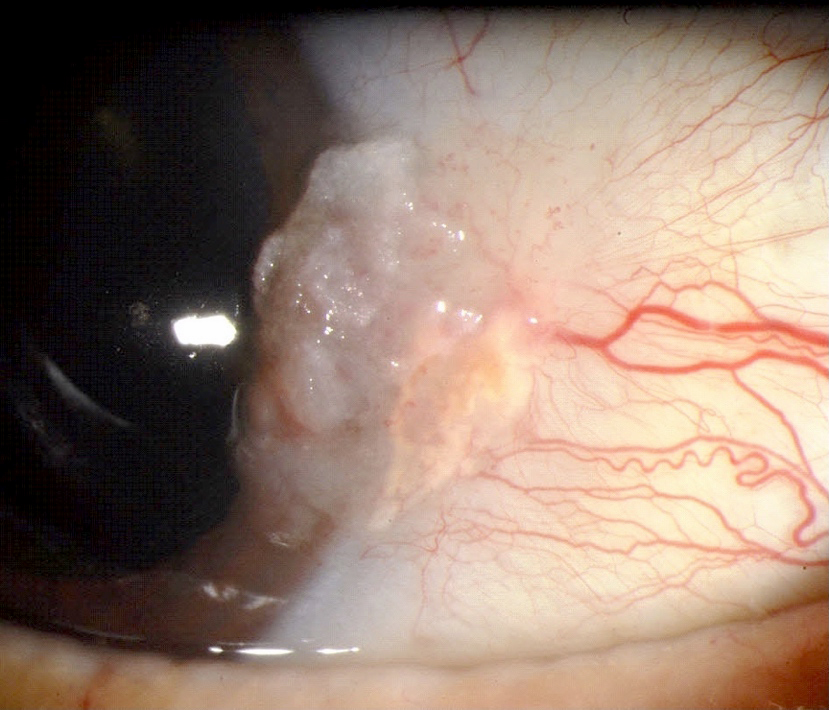
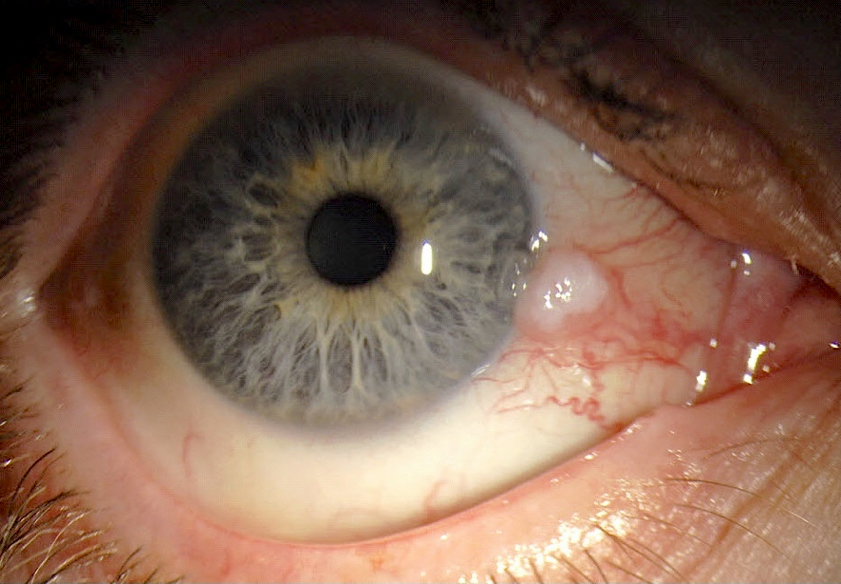
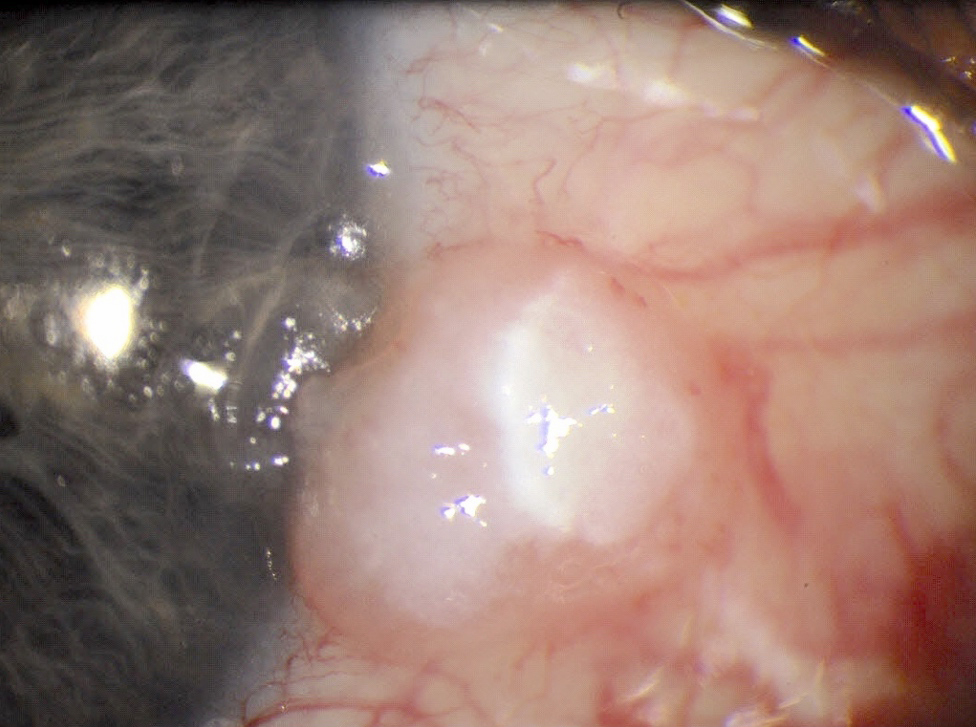
- Fleshy, gray or white conjunctival lesion
- May be elevated or flat
- May appear gelatinous, leukoplakic, papilliform or diffuse (Optometry 2011;82:15)
- Lesions commonly have associated feeder vessels
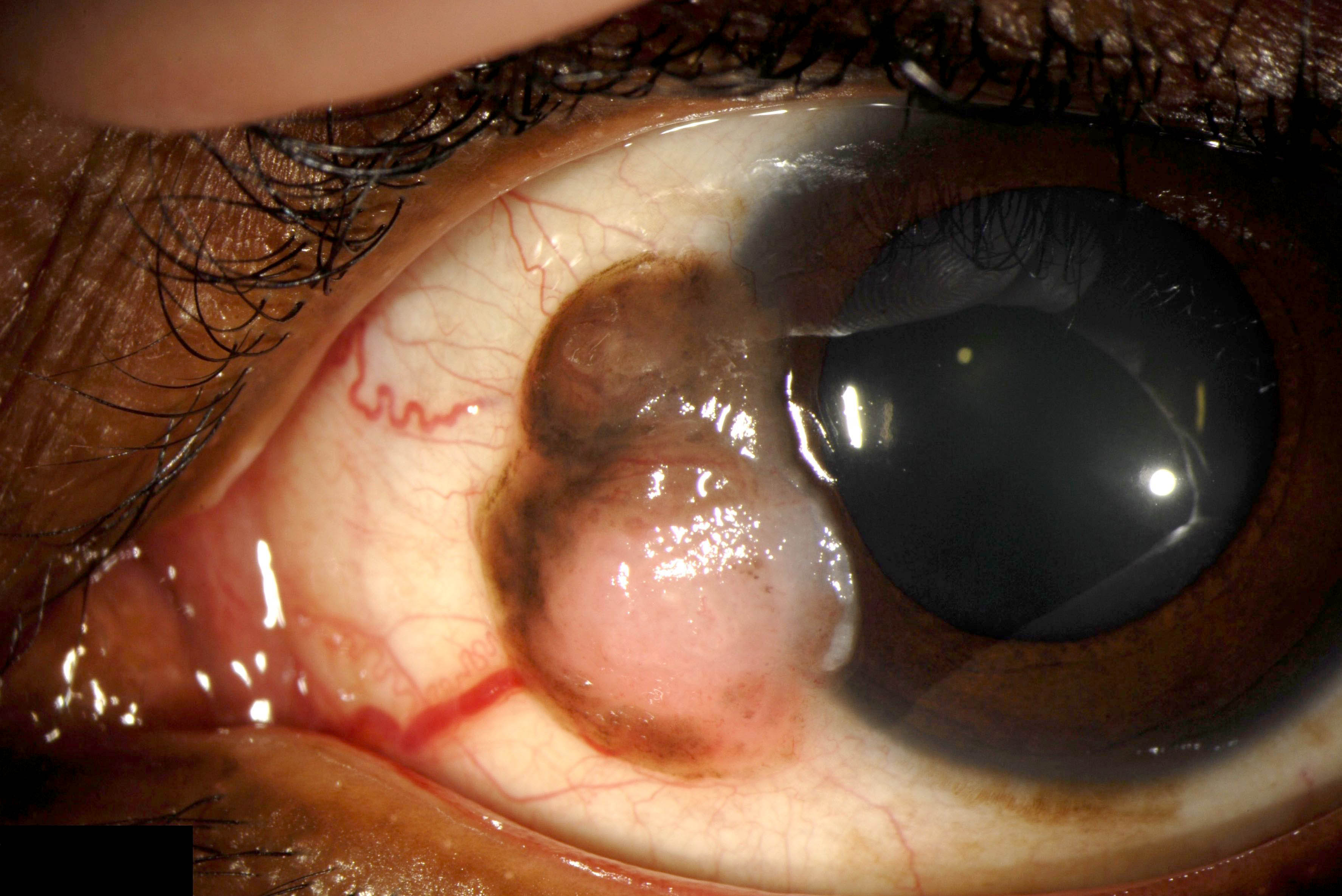
- Lesions may be pigmented and resemble melanoma due to intratumoral pigmented dendritic melanocytes (Ophthalmology 2008;115:1673)
- Moves freely over the underlying episclera, unlike invasive carcinoma, which is fixed (Optometry 2011;82:15)
Diagnosis
- Histopathologic evaluation of excised tissue to confirm the diagnosis
- Exfoliative cytology and in vivo confocal microscopy are safe, noninvasive and effective diagnostic tools (Am J Ophthalmol 2009;148:772, Eye (Lond) 2012;26:781, Am J Ophthalmol 2011;151:238)
Prognostic factors
- Recurrence associated with higher grade lesions, tumors and positive margins (Ophthalmology 2012;119:1974, Ophthalmology 2012;119:233)
- Recurrence rate 5 - 33% with negative margins and 53 - 56% with positive margins (Ophthalmology 1986;93:176, Ophthalmology 1997;104:485)
- Actinic keratosis growth pattern has a good prognosis while diffuse growth pattern has poorer prognosis with more recurrences because tumoral margin is not well defined
Case reports
- 41 year old HIV positive man with low CD4 counts presented with conjunctival epithelial dysplasia and viral retinitis (Indian J Ophthalmol 2019;67:116)
- 45 year old woman with a history of HPV 16 presented with bilateral conjunctival squamous cell carcinoma in situ (Ophthalmic Plast Reconstr Surg 2018;34:e1)
- 48 year old white man with a leukoplakic conjunctival growth 3 months after total body phototherapy for mycosis fungoides (MF) (Am J Ophthalmol Case Rep 2019;14:98)
- 56 year old woman with conjunctival intraepithelial neoplasia presented as a pigmented conjunctival lesion (Case Rep Ophthalmol 2021;12:77)
- Man with conjunctival lesion and history of basal cell carcinoma (Ophthalmology 2015;122:1039)
Treatment
- Surgical excision using a no touch technique with 2 - 4 mm margins, alcohol application and supplemental surgical margin cryotherapy (Arch Ophthalmol 1997;115:808)
- Topical interferon alpha 2b, mitomycin or 5-fluorouracil (Ophthalmology 2008;115:1291, Ophthalmology 2007;114:976, Br J Ophthalmol 2017;101:1094)
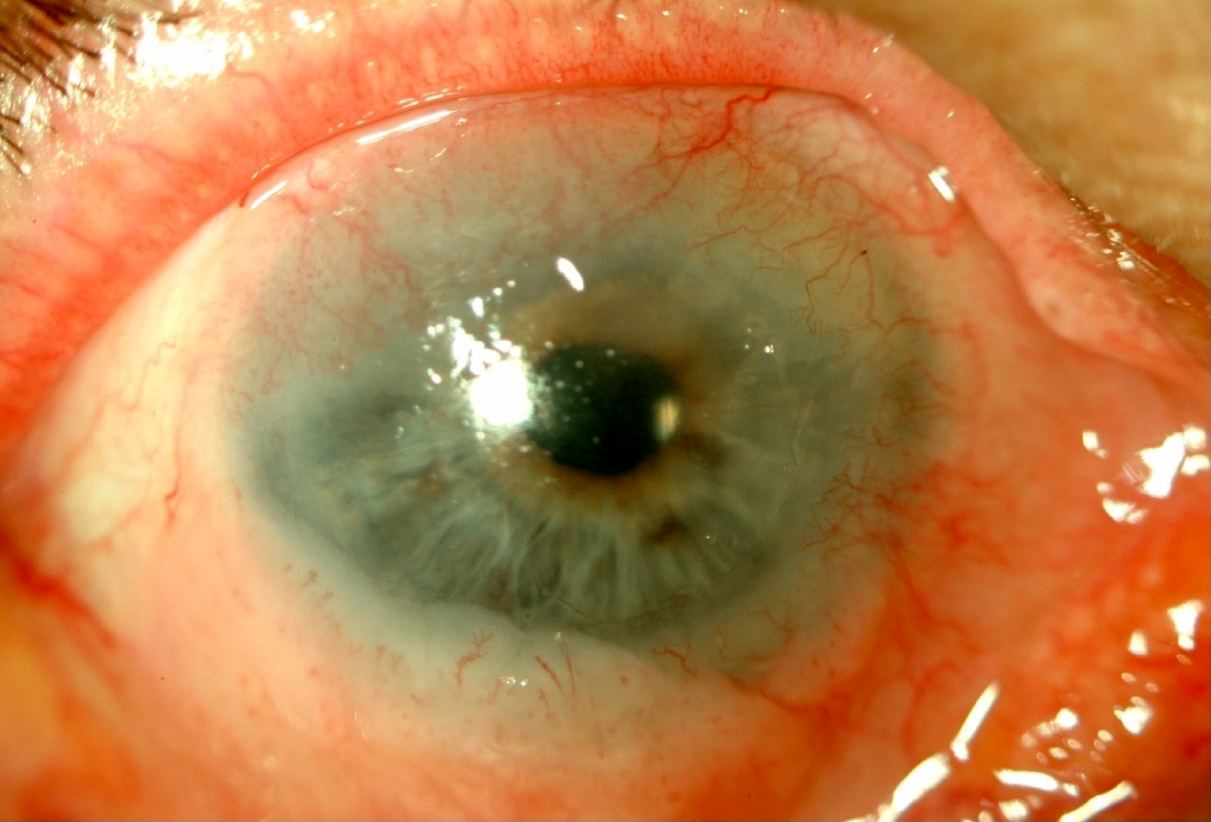
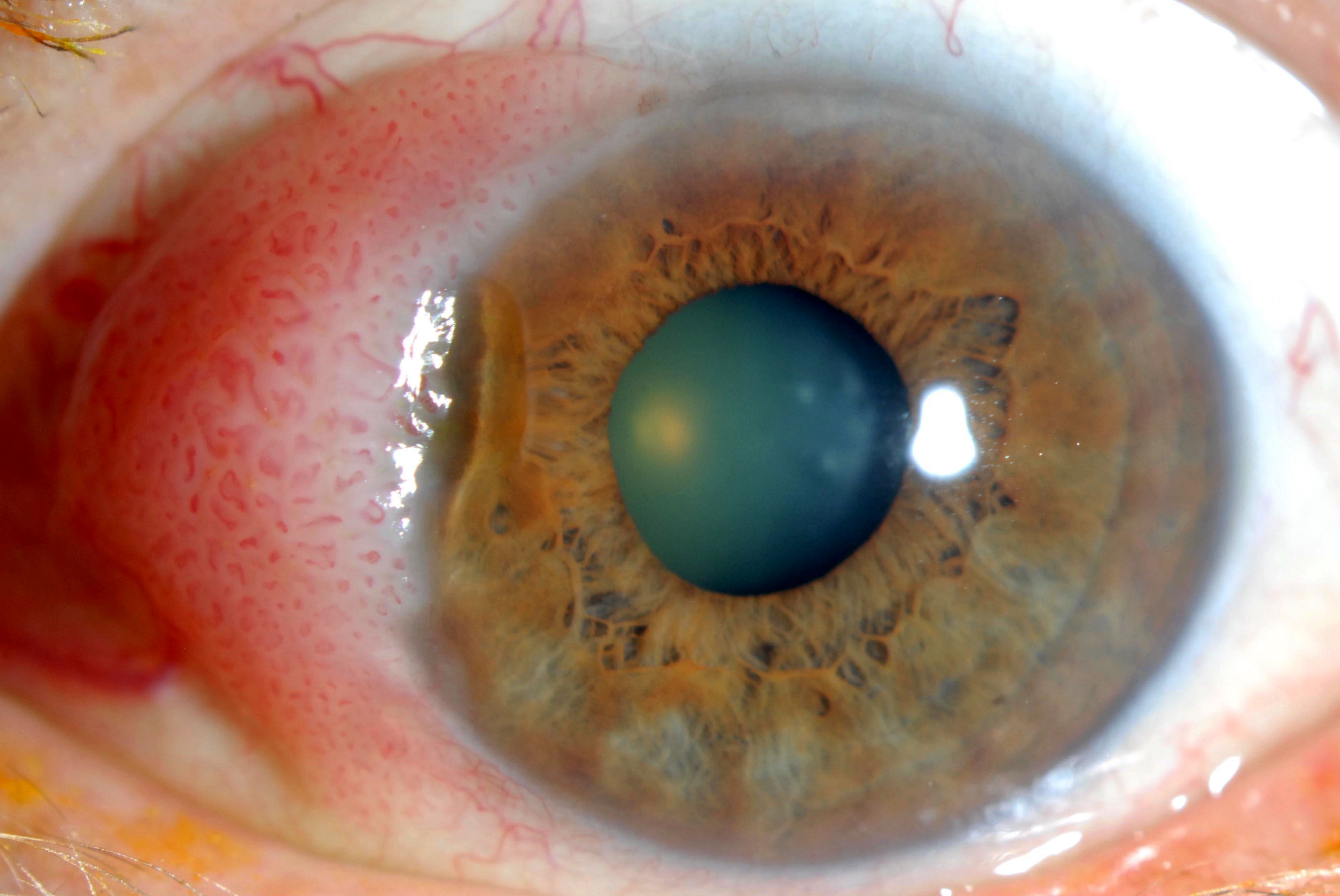
Clinical images
Gross description
- Gelatinous, translucent or granular appearance of conjunctiva
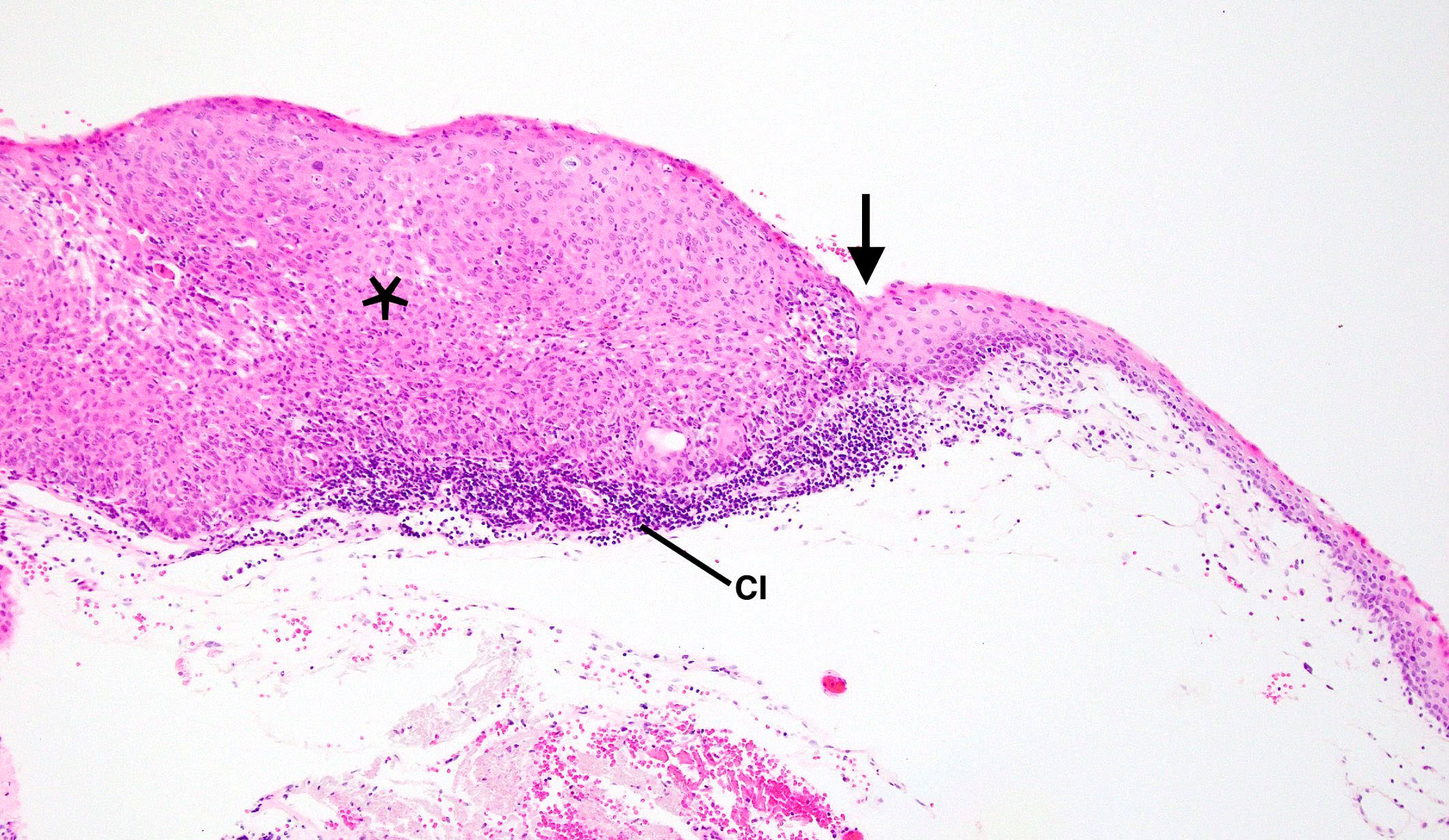
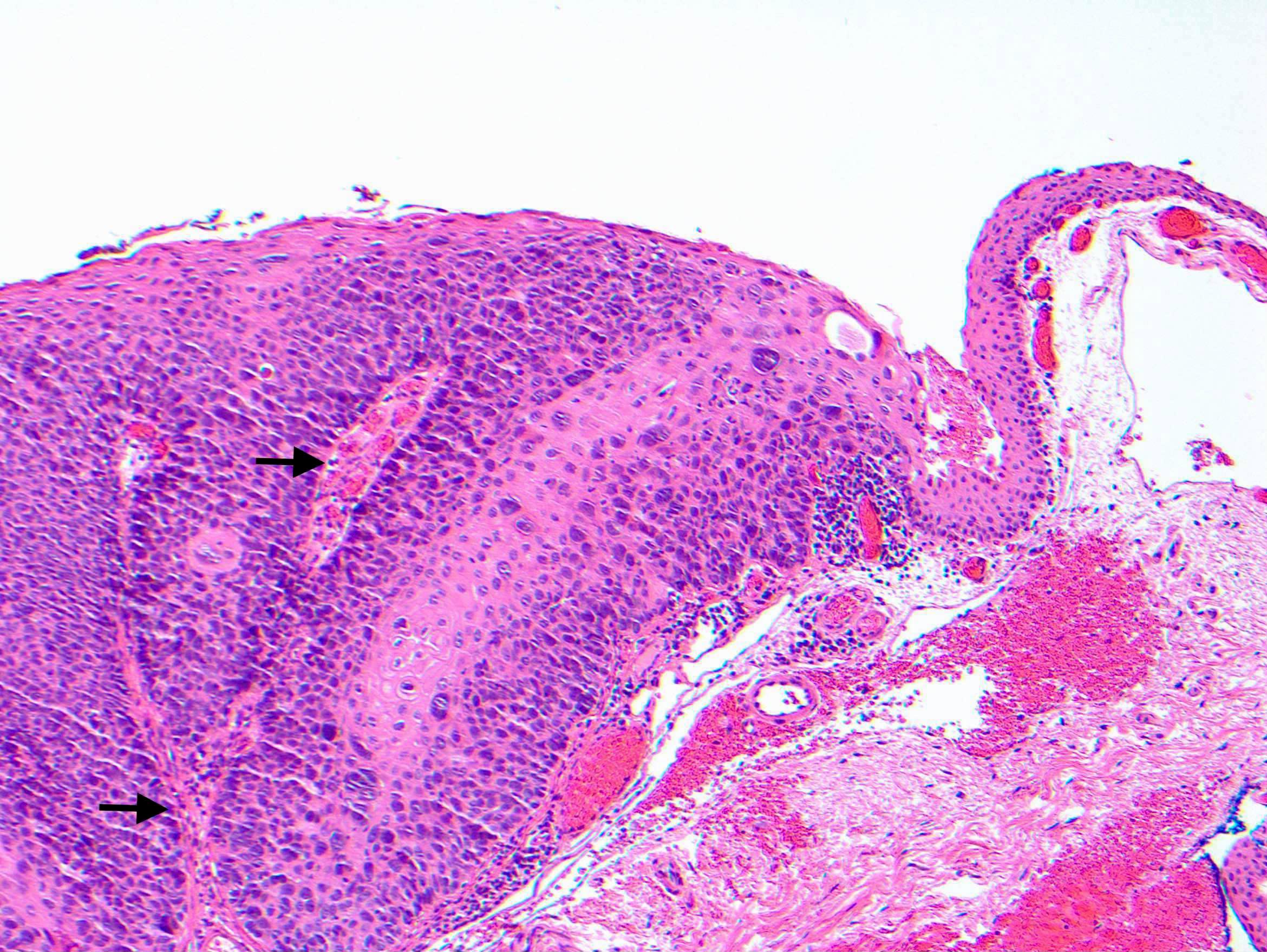
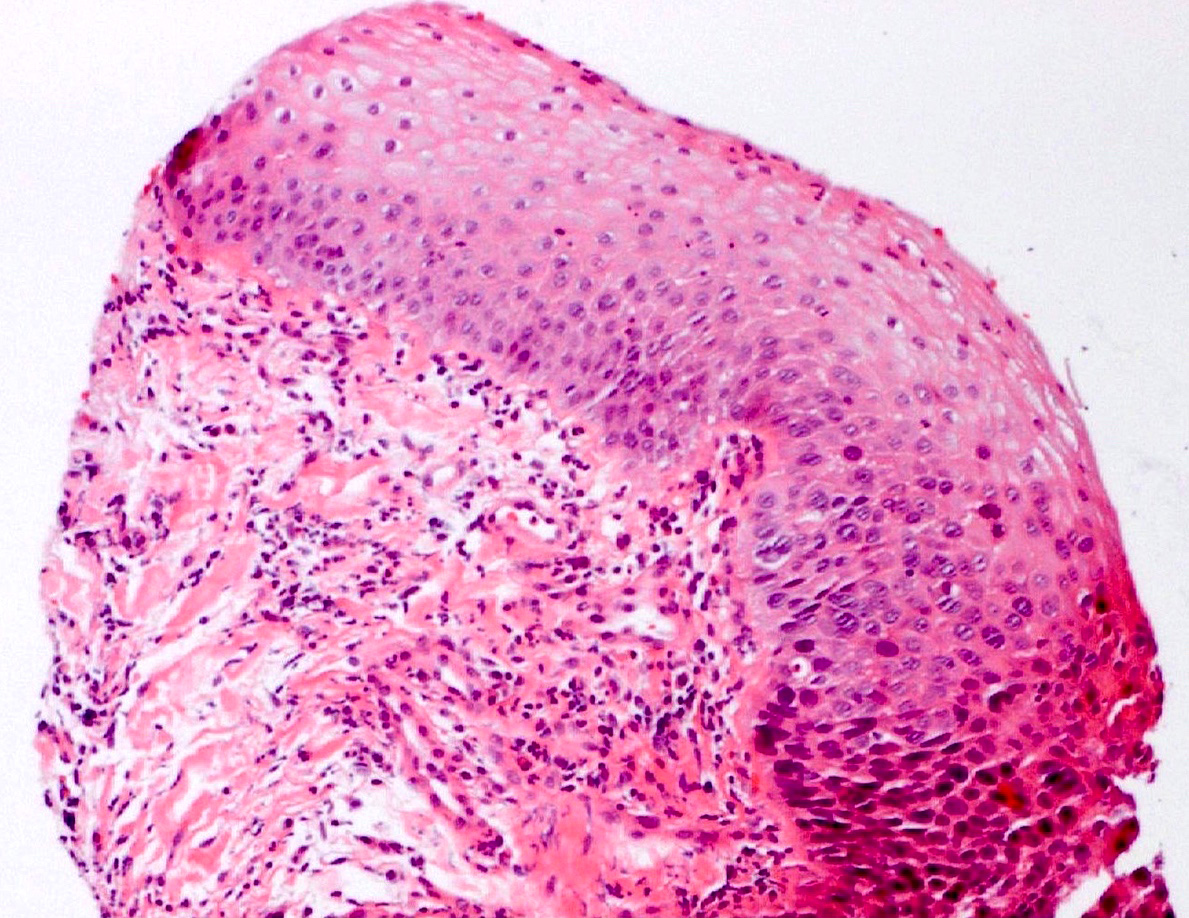
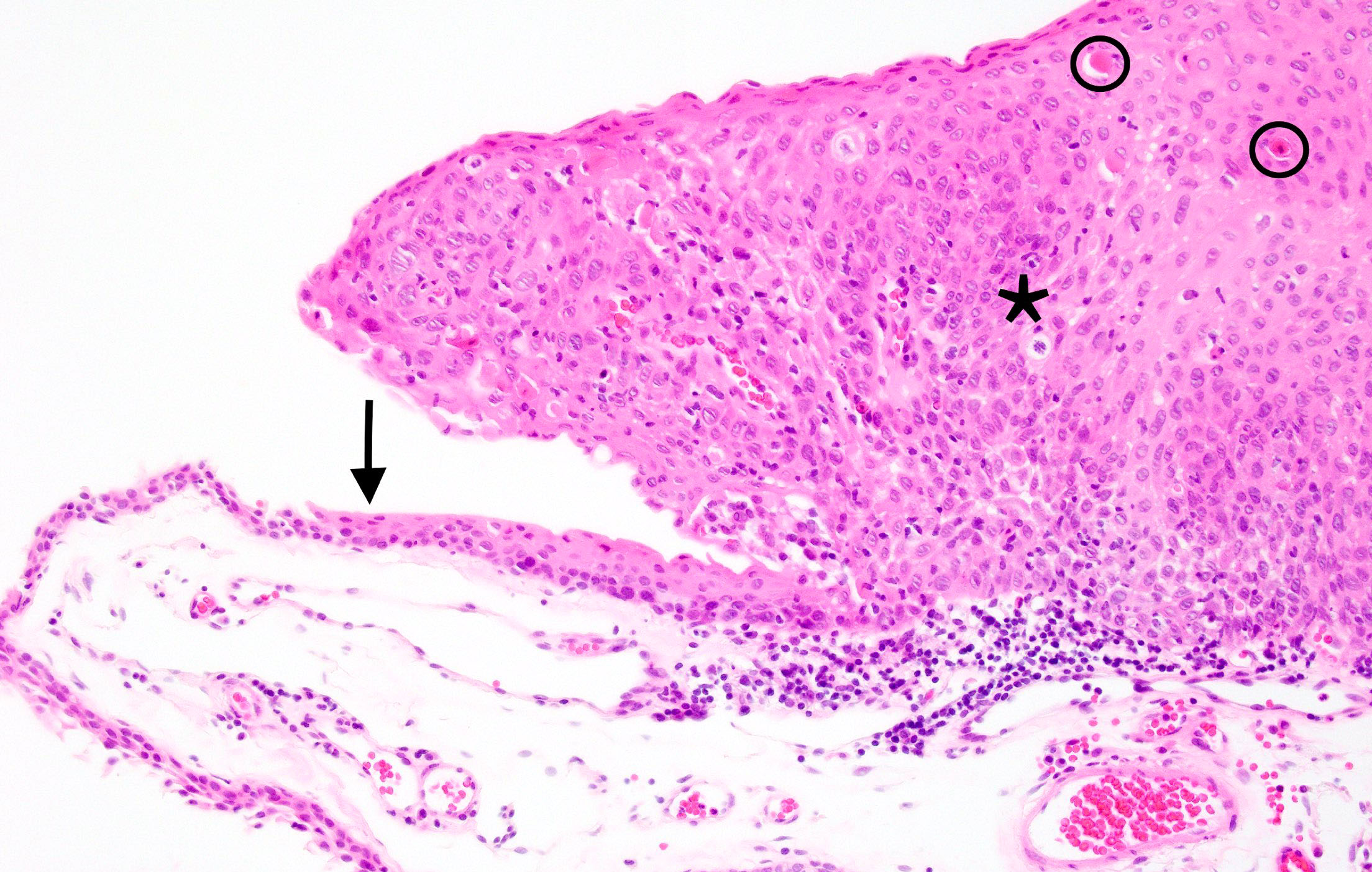
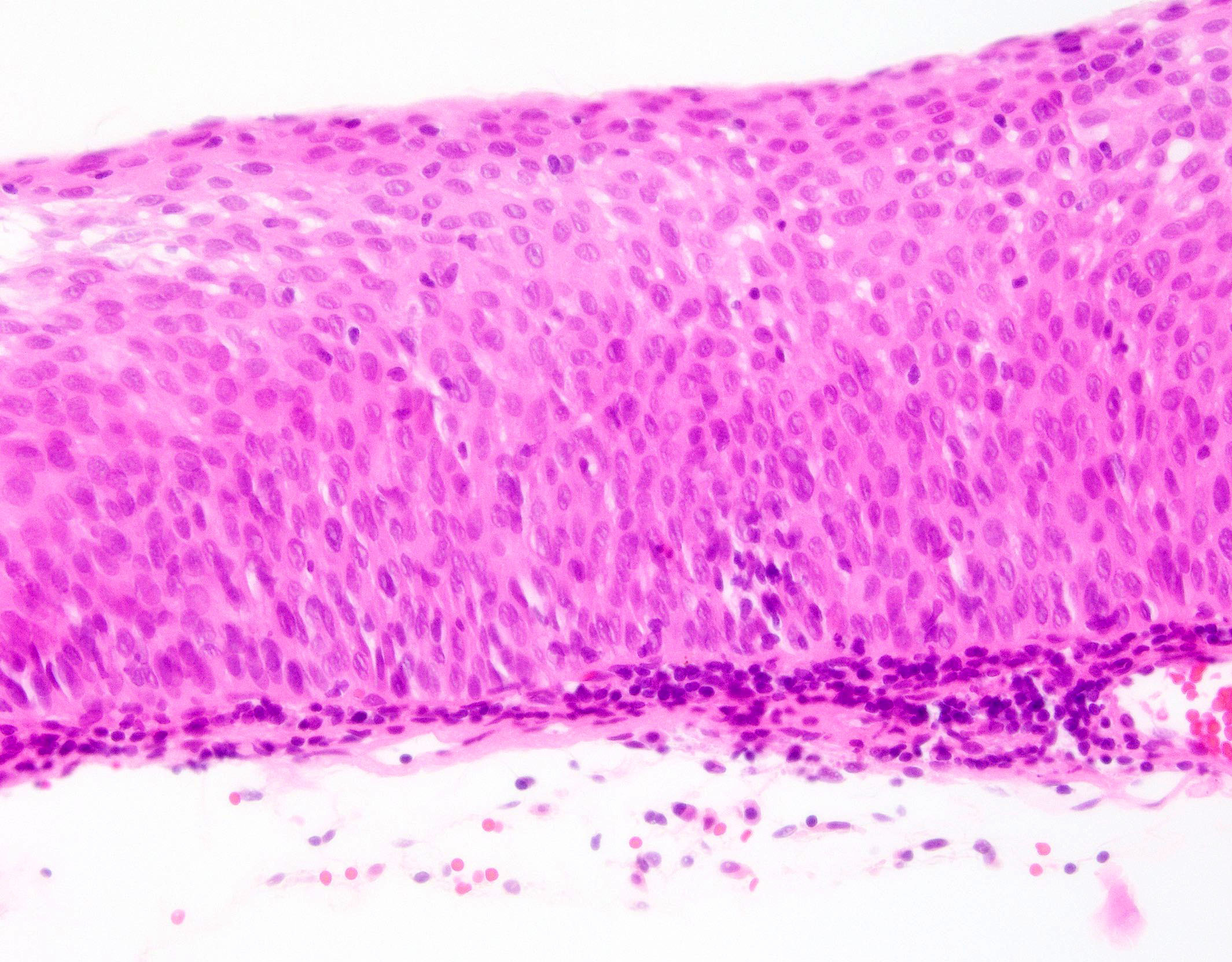
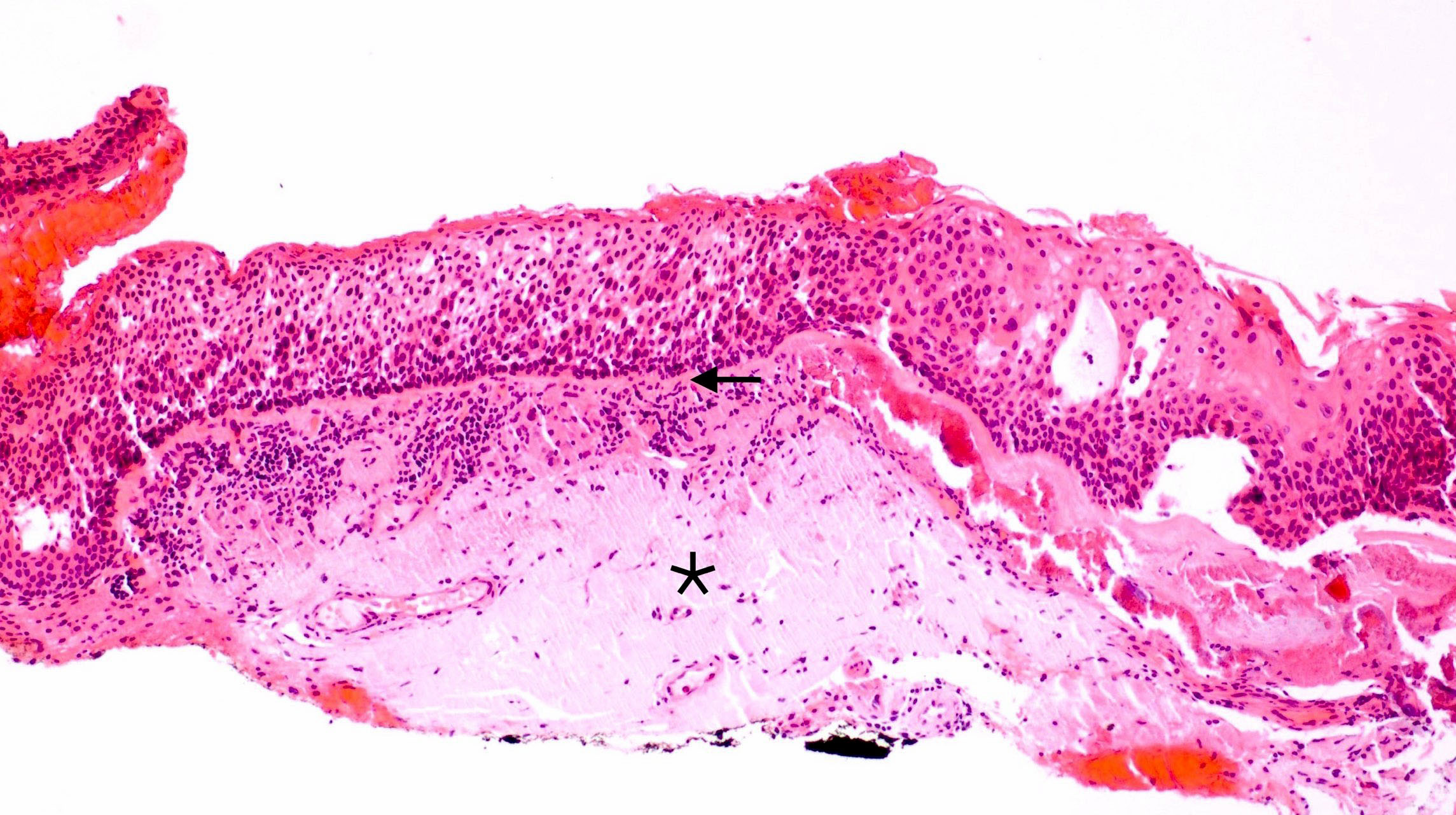
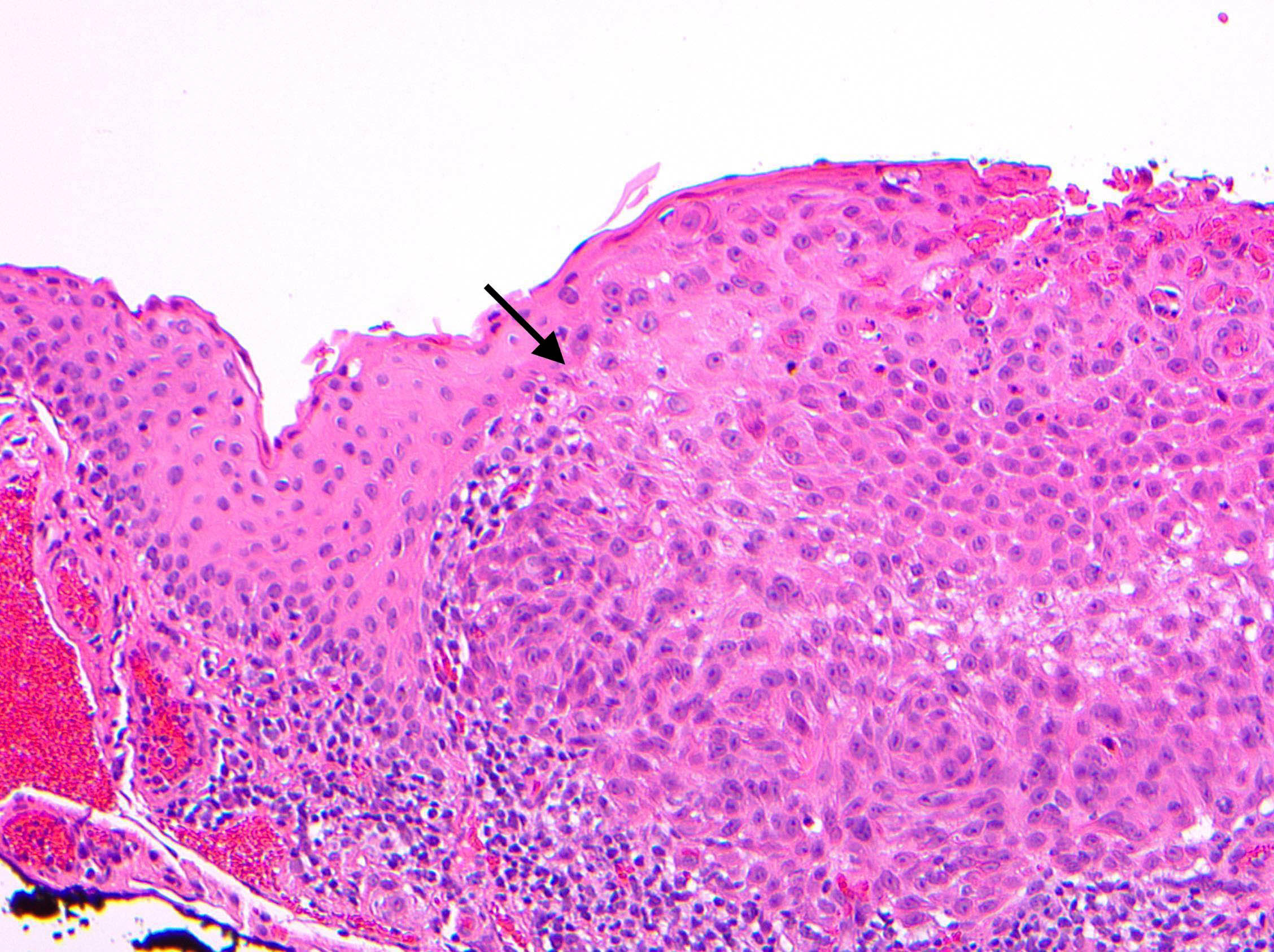
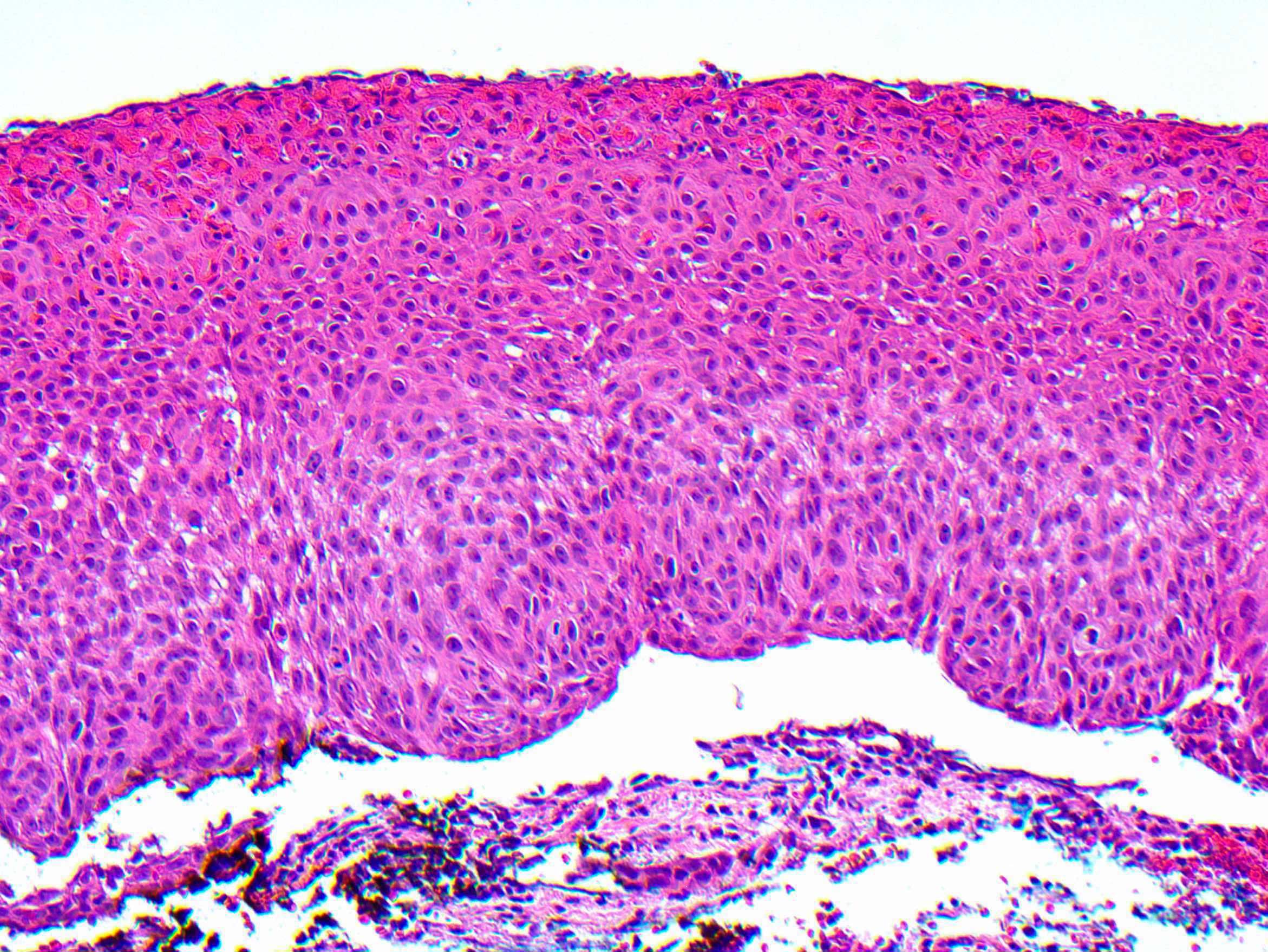
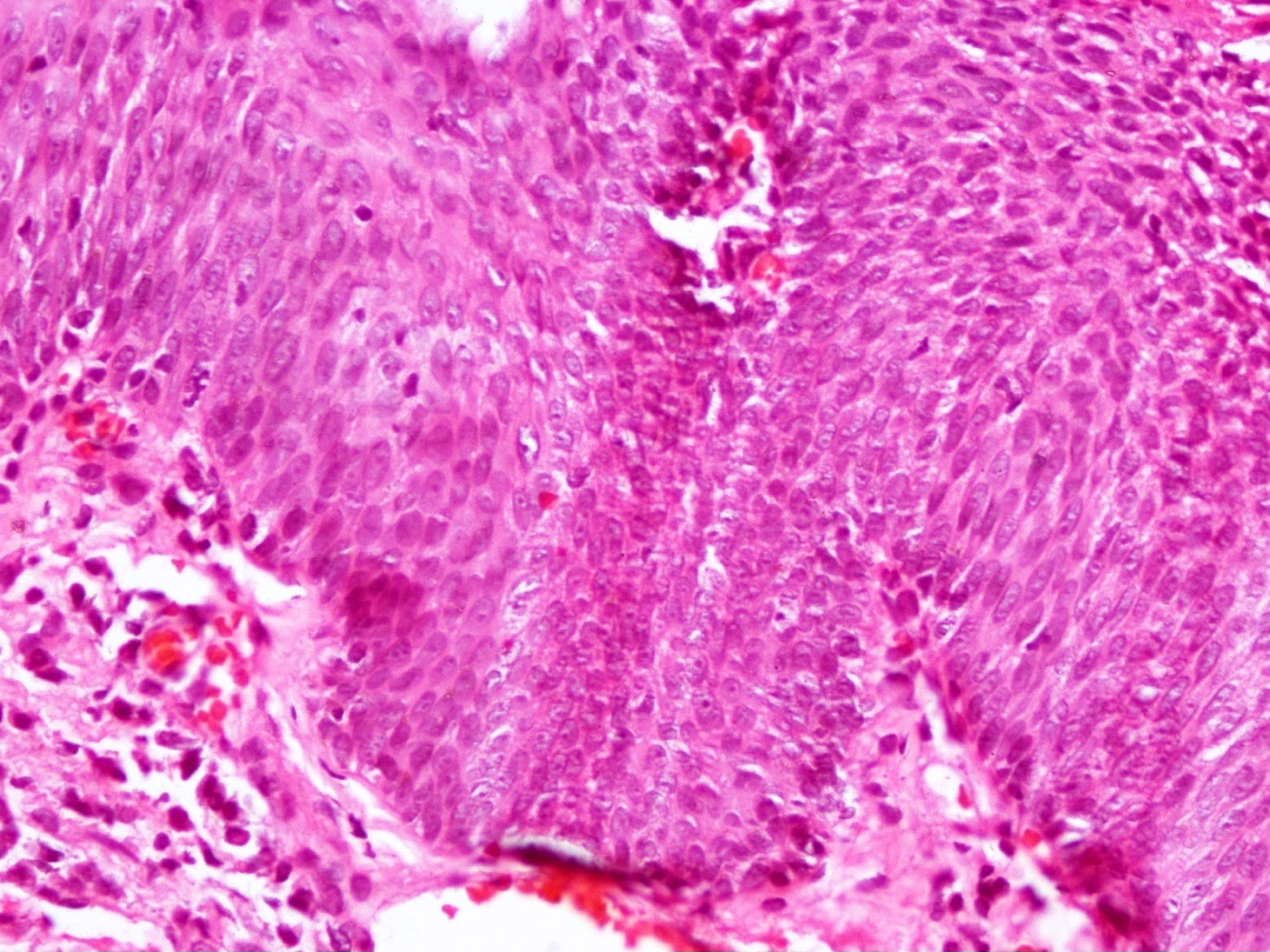
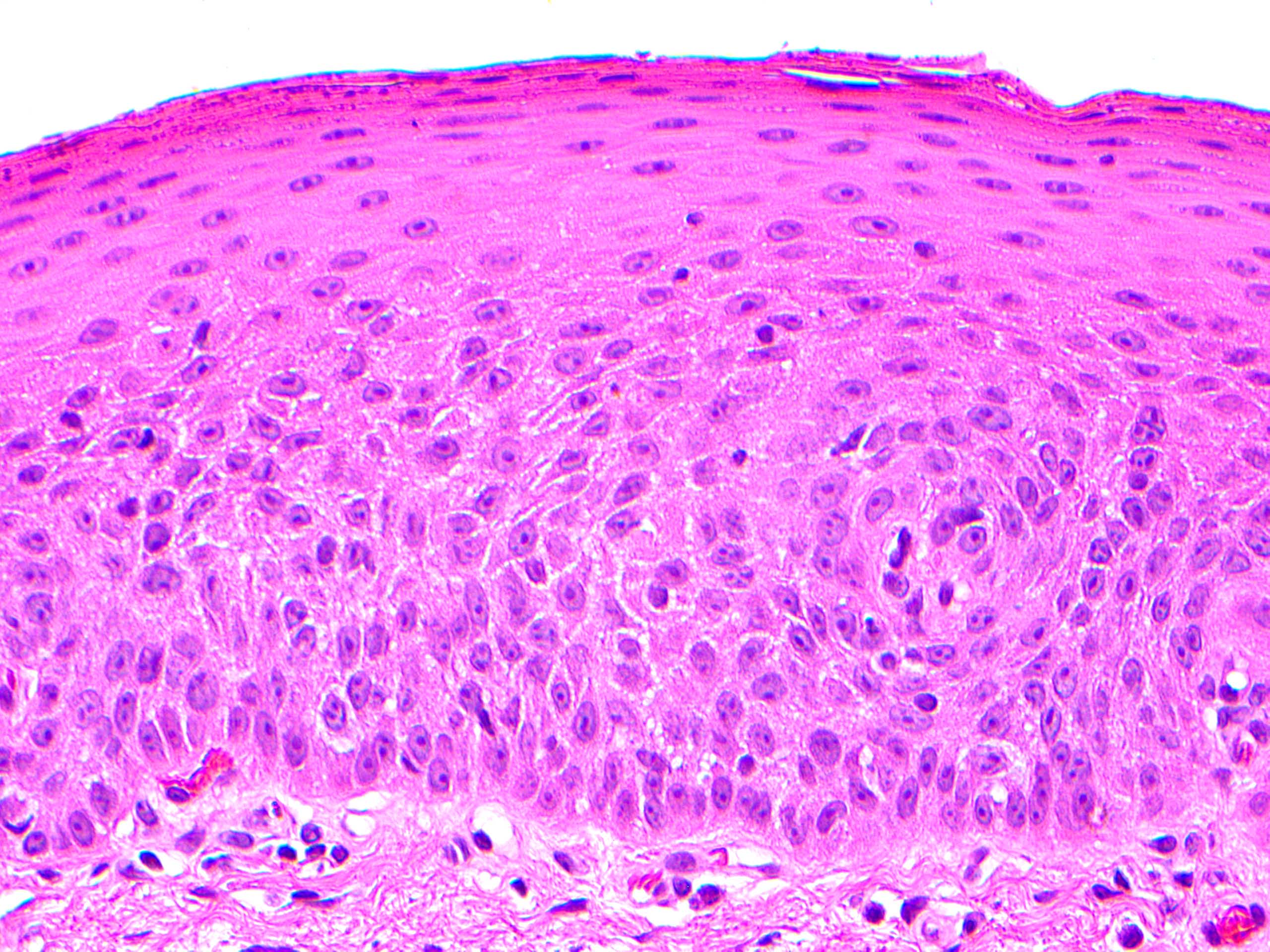
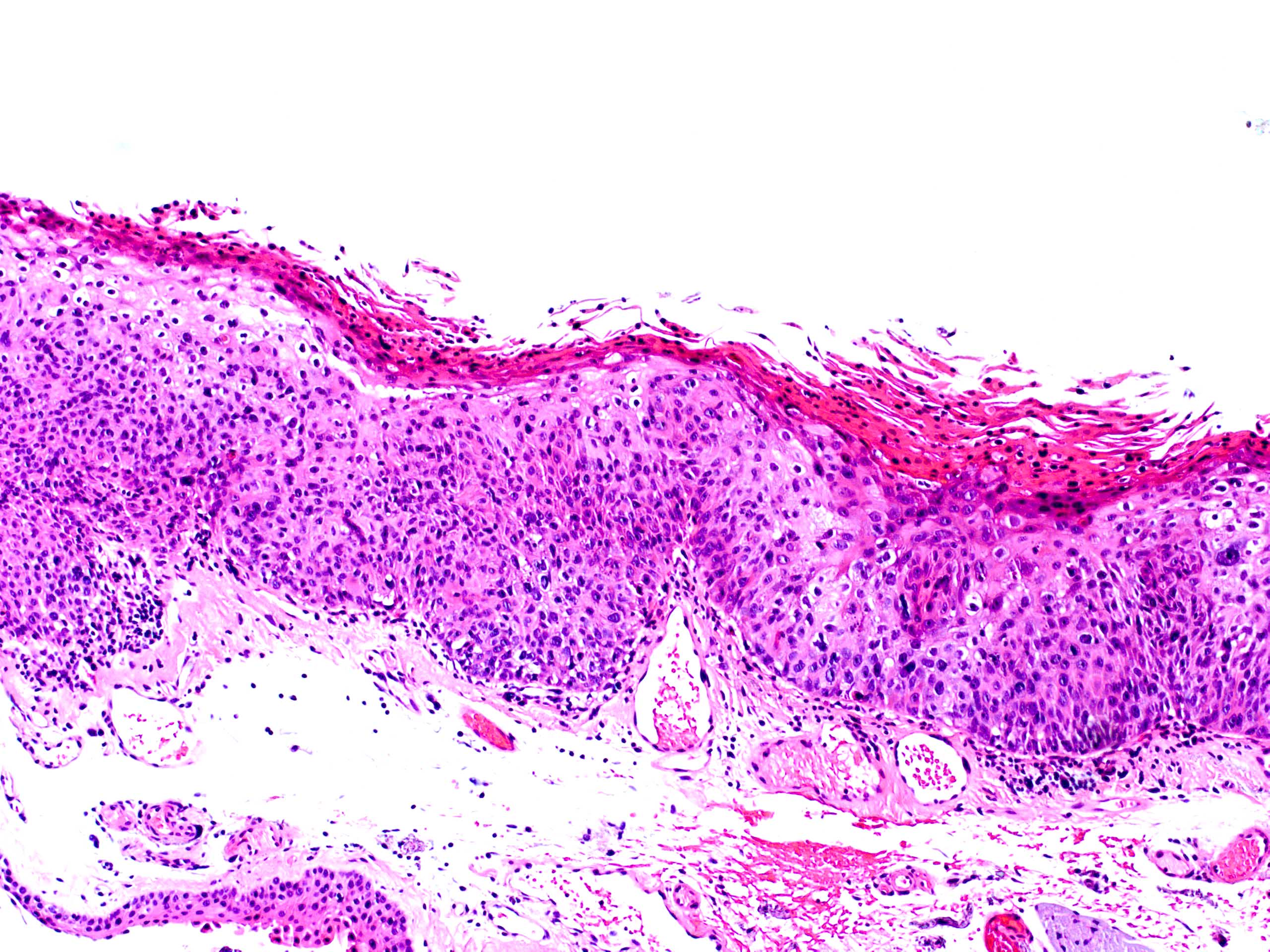
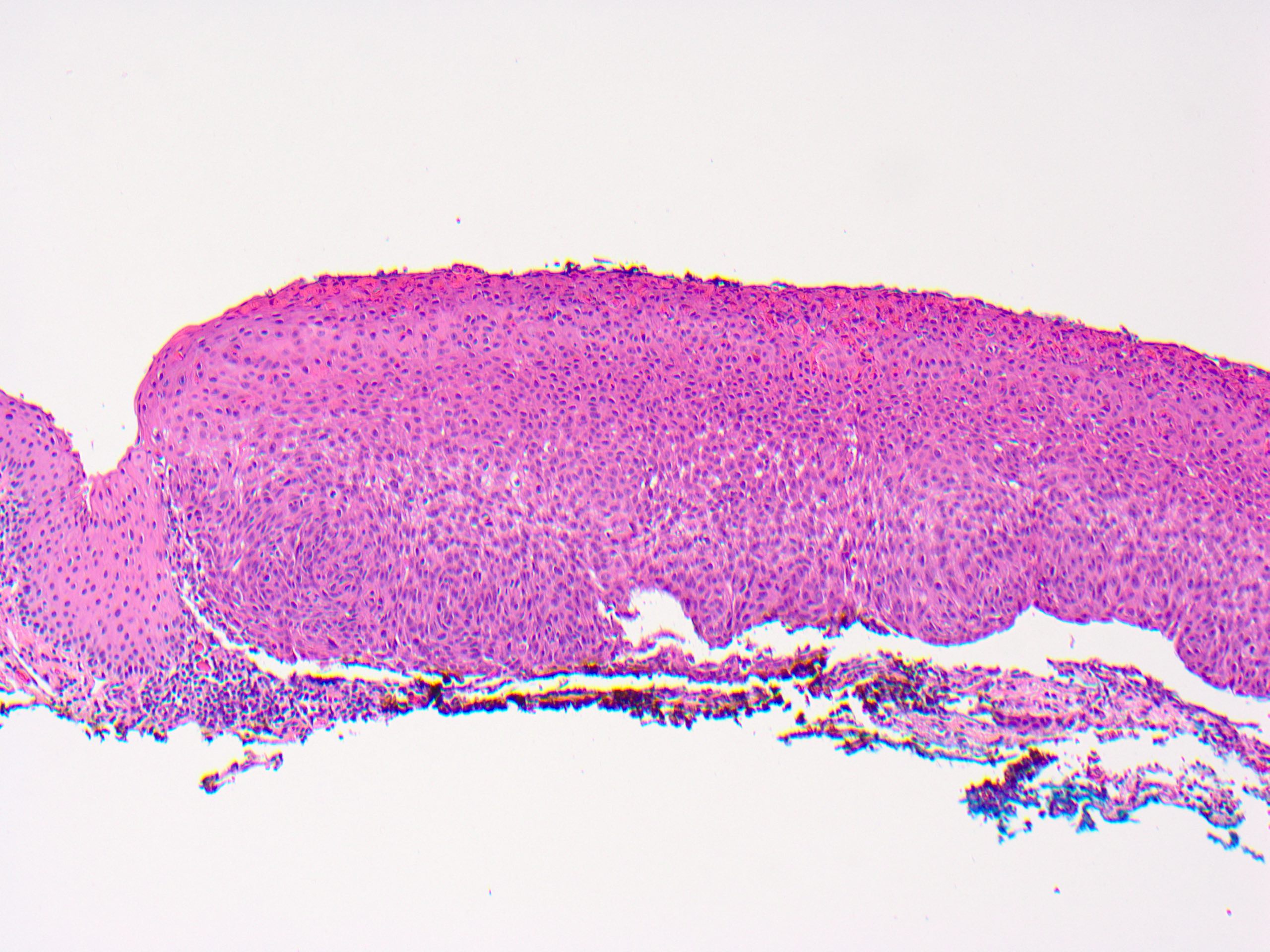
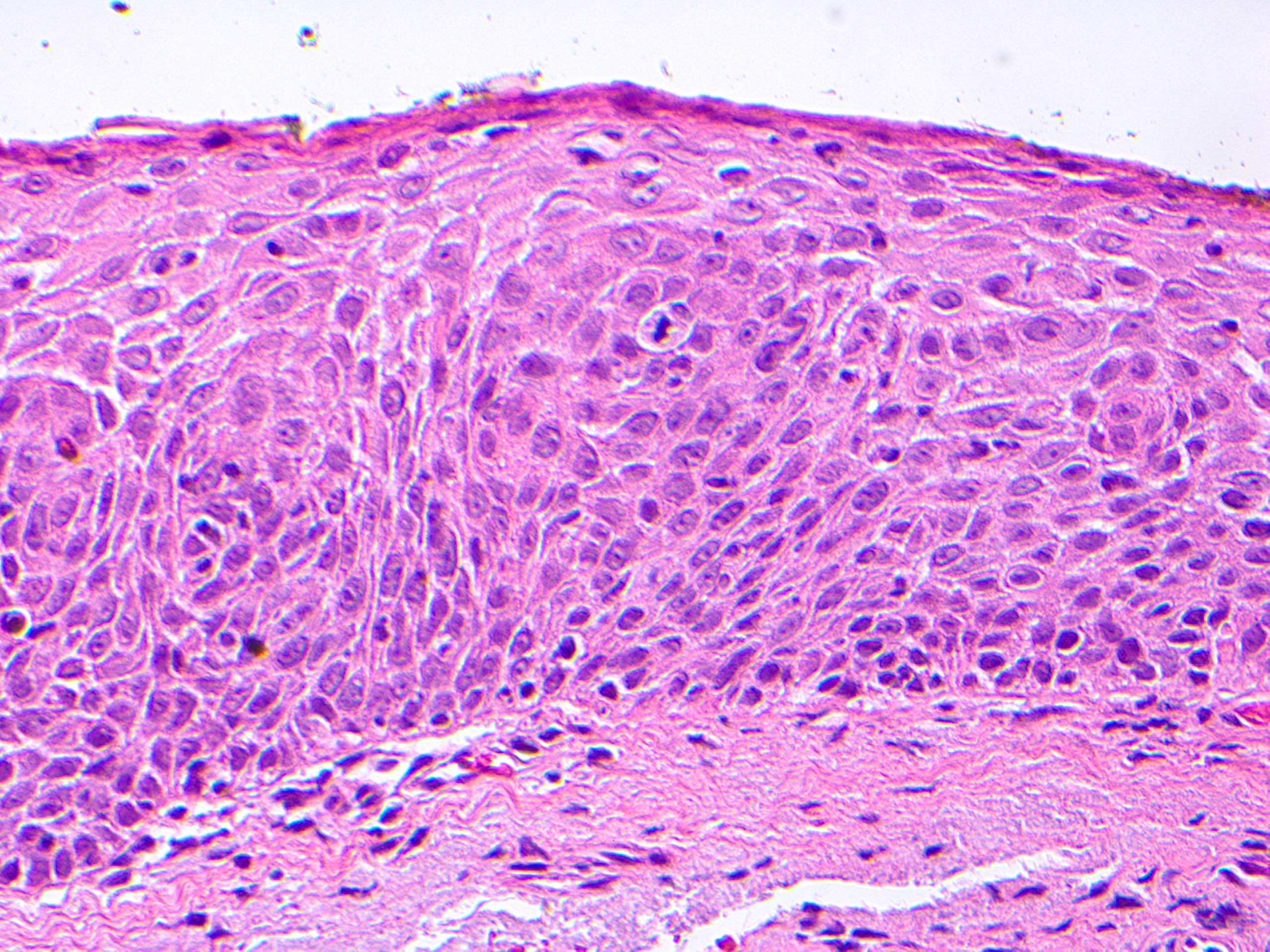
Microscopic (histologic) description
- Grading:
- Depends on thickness of conjunctival epithelial involvement by dysplasia:
- Conjunctival intraepithelial neoplasia 1 (mild dysplasia): involves lower third of epithelial thickness
- Conjunctival intraepithelial neoplasia 2 (moderate dysplasia): involves lower two - thirds
- Conjunctival intraepithelial neoplasia 3 (severe dysplasia): involves > two - thirds of thickness; surface maturation still present
- Carcinoma in situ: involves entire epithelium (full thickness); no more surface maturation (surface epithelium replaced by dysplastic cells)
- Depends on thickness of conjunctival epithelial involvement by dysplasia:
- Architectural features:
- Thickened epithelium (acanthosis); increased cellularity
- Loss of normal maturation sequence; disorganization
- Dysplasia begins in basal layers and extends toward surface
- Noninvasive; epithelial basement membrane is intact
- May have sharp demarcation between normal and abnormal epithelium
- Chronic inflammatory infiltrate in underlying stroma may be present
- Can have surface keratinization
- Papillary configuration with intralesional vessels and occasionally fibrovascular cores
- Intratumoral pigmented dendritic melanocytes can give rise to pigmented lesions resembling melanoma (Ophthalmology 2008;115:1673)
- Varieties (Can J Ophthalmol 1995;30:312):
- Actinic keratosis variety:
- Arises in epithelium covered areas of solar elastosis
- Usually leukoplakic due to surface keratinization
- Focal and well delineated
- Diffuse variety:
- Arises in non sun exposed epithelium
- Usually gelatinous
- Diffuse and poorly delineated
- Actinic keratosis variety:
Microscopic (histologic) images
Contributed by Pia Mendoza, M.D.
Contributed by Frederick A. Jakobiec, M.D., D.Sc., Deepali Jain, M.D. and Hans Grossniklaus, M.D.
Cytology description
- Increased N/C ratio
- Nuclear hyperchromasia
- Pleomorphism
- May have prominent nucleoli
- May have dyskeratosis
- Rarely has HPV related / koilocytic changes
- Reference: Am J Ophthalmol 2009;148:772
Positive stains
- p53: increased immunoreactivity in dysplasia (Am J Ophthalmol 2013;156:830)
- Ki67: increased proliferation rates in suprabasal epithelium in dysplasia (Am J Ophthalmol 2013;156:830)
- p16: greater intensity and percentage staining in high grade dysplasia (Am J Dermatopathol 2018;40:486)
Negative stains
- CK7: loss of expression in dysplasia (expressed in normal conjunctiva and squamous papillomas) (Am J Ophthalmol 2013;156:830)
- Periodic acid Schiff (PAS): negative in dysplasia due to loss of goblet cells (highlights goblet cells in normal conjunctiva and squamous papillomas)
Molecular / cytogenetics description
- Somatic TP53 mutations have been reported (Cornea 2000;19:159)
- Frequent TERT promoter mutations consistent with UV radiation induced damage (Invest Ophthalmol Vis Sci 2015;56:5854)
Sample pathology report
- Right eye, conjunctiva, excision:
- Conjunctival intraepithelial neoplasia 2 / moderate dysplasia (see comment)
- Comment: Surgical margins are negative for intraepithelial neoplasia. Negative for invasive carcinoma.
Differential diagnosis
- Conjunctival squamous papilloma:
- Pterygium:
- Wing-like, fleshy conjunctival lesion
- Epithelium without dysplasia
- Underlying stromal fibrovascular tissue with solar elastosis
- Pyogenic granuloma:
- Lobulated capillary proliferation with acute and chronic inflammation
- Sebaceous gland carcinoma:
- Primarily an eyelid tumor, with extension into the conjunctiva
- Large anaplastic cells with finely vacuolated cytoplasm spreading in pagetoid fashion to the conjunctiva
- Adipophilin+
- Pinguecula:
- Whitish yellow elevated conjunctival lesion in interpalpebral zone near limbus
- Goblet cell containing epithelium with various degrees of acanthosis or keratinizing metaplasia without dysplasia
- Subepithelial solar elastosis
Additional references
Practice question #1
Practice answer #1
A. Conjunctival intraepithelial neoplasia grade 3.
The patient is an older, light skinned man, likely with significant UV exposure, putting him at higher risk for the conditions listed in the choices. The clinical image shows a gelatinous conjunctival lesion with feeder vessels at the limbus in the interpalpebral zone. The biopsy shows thickened conjunctival epithelium with loss of the normal maturation sequence. There is a proliferation of dysplastic squamous cells with high N/C ratios, mitotic activity, hyperchromatic and pleomorphic nuclei involving > two - thirds of the epithelial thickness (conjunctival intraepithelial neoplasia 3 / severe dysplasia). The basement membrane is intact.
Primary acquired melanosis (choice B) is a proliferation of intraepithelial melanocytes that typically grow in a nested pattern. Pterygium (choice C) would present clinically as a wing-like, fleshy conjunctival lesion. Histopathology would show thin epithelium without dysplasia and underlying stromal fibrovascular tissue with solar elastosis. Conjunctival intraepithelial neoplasia is a precursor of squamous cell carcinoma (choice D). In squamous cell carcinoma, dysplastic cells invade beyond the basement membrane.
Comment Here
Reference: Conjunctival intraepithelial neoplasia
Primary acquired melanosis (choice B) is a proliferation of intraepithelial melanocytes that typically grow in a nested pattern. Pterygium (choice C) would present clinically as a wing-like, fleshy conjunctival lesion. Histopathology would show thin epithelium without dysplasia and underlying stromal fibrovascular tissue with solar elastosis. Conjunctival intraepithelial neoplasia is a precursor of squamous cell carcinoma (choice D). In squamous cell carcinoma, dysplastic cells invade beyond the basement membrane.
Comment Here
Reference: Conjunctival intraepithelial neoplasia
Practice question #2
Which of the following is a feature of conjunctival intraepithelial neoplasia?
- Association with HPV 6 and 11
- Goblet cell containing epithelium without dysplasia
- Positivity for CK7 and periodic acid Schiff (PAS)
- Proliferation of atypical squamous cells, which may be a precursor to squamous cell carcinoma
Practice answer #2
D. Proliferation of atypical squamous cells, which may be a precursor to squamous cell carcinoma.
Conjunctival intraepithelial neoplasia is characterized by a proliferation of neoplastic squamous cells showing cellular atypia. It is considered a premalignant lesion that may progress to invasive squamous cell carcinoma.
HPV 6 and 11 (choice A) are associated with squamous papilloma. HPV 16 and 18 are associated with conjunctival intraepithelial neoplasia. Goblet cell containing epithelium without dysplasia (choice B) is seen in other entities that may mimic conjunctival intraepithelial neoplasia, such as pterygium, pingueculae and squamous papilloma. CK7 (choice C) is expressed in normal conjunctiva and squamous papillomas but usually negative in dysplasia. PAS is positive in normal conjunctiva and squamous papillomas due to presence of goblet cells; however, goblet cells are usually lacking in conjunctival intraepithelial neoplasia.
Comment Here
Reference: Conjunctival intraepithelial neoplasia
HPV 6 and 11 (choice A) are associated with squamous papilloma. HPV 16 and 18 are associated with conjunctival intraepithelial neoplasia. Goblet cell containing epithelium without dysplasia (choice B) is seen in other entities that may mimic conjunctival intraepithelial neoplasia, such as pterygium, pingueculae and squamous papilloma. CK7 (choice C) is expressed in normal conjunctiva and squamous papillomas but usually negative in dysplasia. PAS is positive in normal conjunctiva and squamous papillomas due to presence of goblet cells; however, goblet cells are usually lacking in conjunctival intraepithelial neoplasia.
Comment Here
Reference: Conjunctival intraepithelial neoplasia