Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1Cite this page: Venable JG, Windon AL. Hepatic small vessel neoplasm. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/liverhsvn.html. Accessed September 10th, 2025.
Definition / general
- Rare, recently described vascular hepatic neoplasm of uncertain malignant potential that is composed of anastomosing, densely packed, small, thin vessels with infiltrative borders, minimal cytologic atypia and a low proliferative rate
Essential features
- Hepatic small vessel neoplasm that shares similar morphologic and molecular qualities to and is thought to represent anastomosing hemangioma of the liver
- Histologically described as benign, low grade hepatic vascular neoplasm with a mottled, unencapsulated gross appearance with poorly circumscribed borders
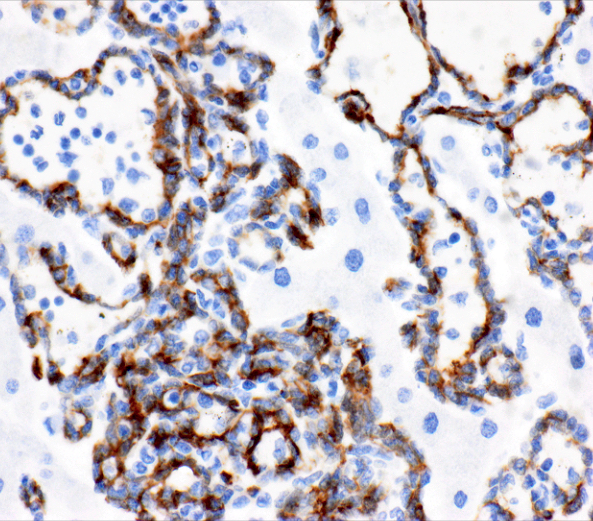
- Positive for vascular markers with frequent GNAQ mutations
Terminology
- Hepatic small vessel neoplasm (HSVN)
- Anastomosing hemangioma (AH)
ICD coding
- ICD-10: D37.6 - neoplasm of uncertain behavior of liver, gallbladder and bile ducts
Epidemiology
- Average patient age: 54 years old (24 - 83 years) and more common in males (Hum Pathol 2016;54:143)
Sites
- Hepatic parenchyma (Hum Pathol 2016;54:143)
- Radiographic evidence of concurrent spleen involvement but not histologically proven (BMJ Case Rep 2022;15:e248785)
Pathophysiology
- Shares GNAQ mutations with anastomosing hemangiomas (Mod Pathol 2017;30:722, Hum Pathol 2016;54:143)
Etiology
- Has morphologic and molecular similarities to and may represent anastomosing hemangioma of the liver
Clinical features
- Usually, an asymptomatic solitary liver lesion that is discovered incidentally (Hum Pathol 2016;54:143)
- Rarely, if large enough, may cause epigastric fullness or back pain (Hum Pathol 2018;78:159)
Diagnosis
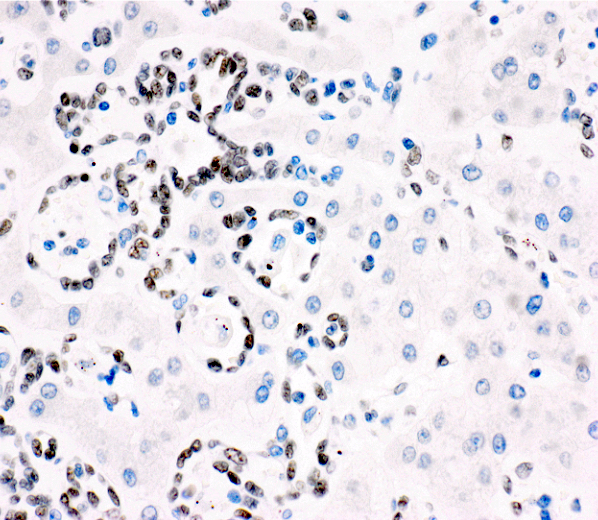
- Histopathologic diagnosis: infiltrative small vessel vascular neoplasm with mild nuclear atypia and low proliferative index
- Diagnosis can be supported by immunohistochemistry and molecular testing
Laboratory
- Normal complete blood count (CBC), serum chemistry, aspartate aminotransferase (AST), alanine aminotransferase (ALT), alpha fetoprotein (AFP), carcinoembryonic antigen (CEA) and CA19-9 (BMJ Case Rep 2022;15:e248785)
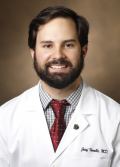
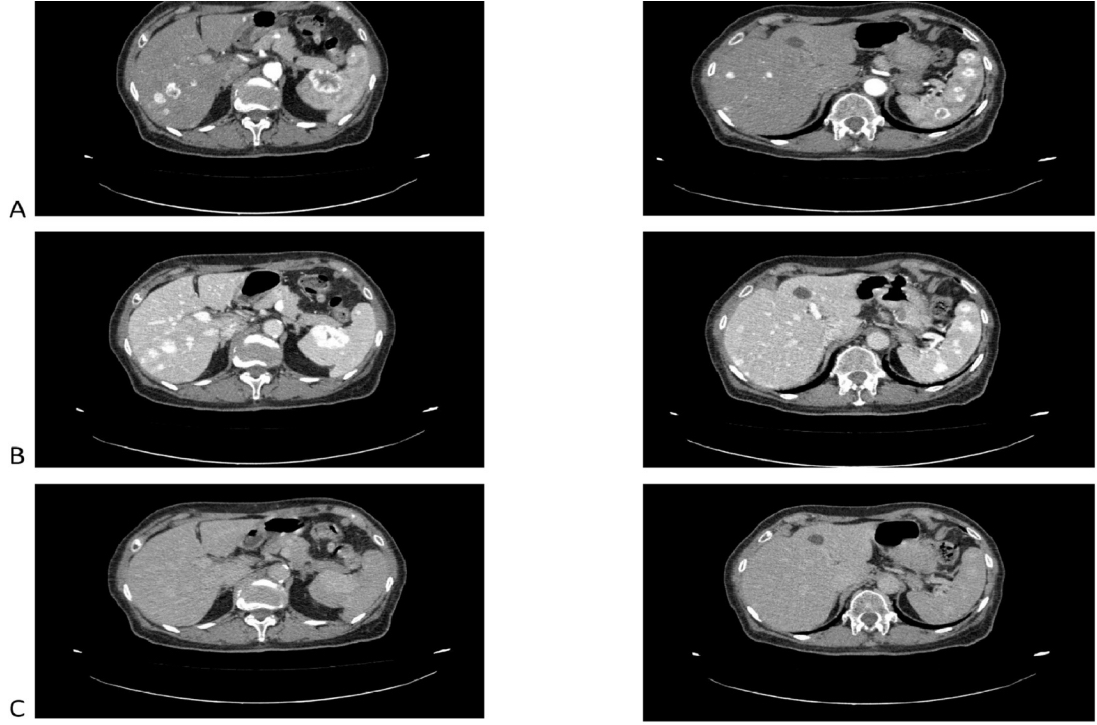
Radiology description
- CT with contrast: hypodense lesions with contrast enhancement in the arterial and portal phase and wash out in the tardive phase
- PET / CT: no evidence of abnormal 18F fluorodeoxyglucose (18F FDG) uptake
- MRI with contrast: atypical vascular tumor with strong and early rim enhancement in arterial phase, with central irregular morphology and gradual enhancement (BMJ Case Rep 2022;15:e248785)
Prognostic factors
- Unknown prognosis and prognostic factors due to scant follow up studies
- Likely low malignant potential (Hum Pathol 2016;54:143)
- Single case report with possible malignant transformation and metastasis (Hum Pathol 2022;29:300671)
Case reports
- 60 year old woman with liver dysfunction and innumerable, diffuse liver nodules (Hum Pathol 2022;29:300671)
- 62 year old man with vague epigastric fullness, 17 cm hepatic lesion (Hum Pathol 2018;78:159)
- Woman in her 70s with concurrent hepatic and splenic lesions (BMJ Case Rep 2022;15:e248785)
Treatment
- Complete resection and close clinical follow up is recommended due to the unknown longterm behavior of this neoplasm (Hum Pathol 2016;54:143)
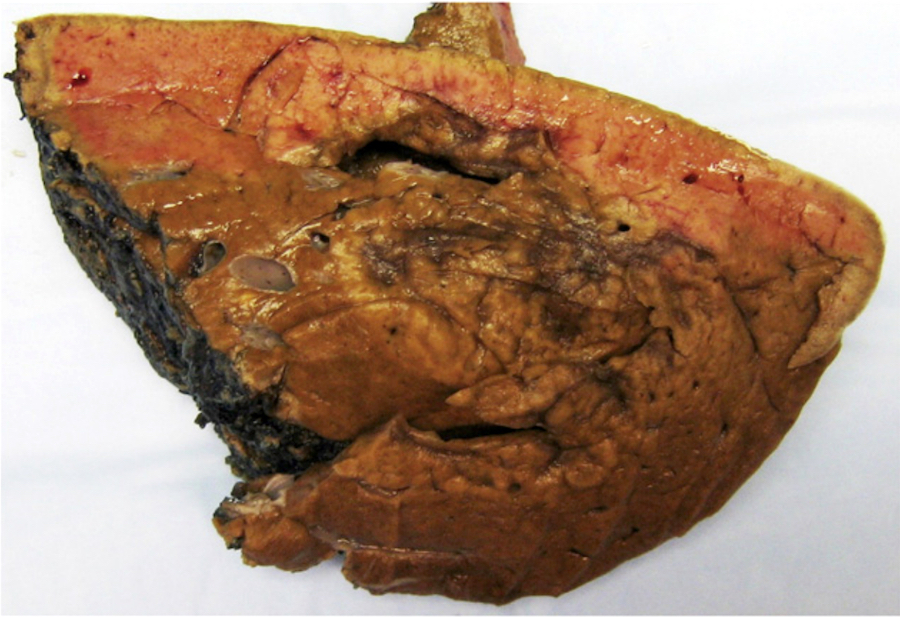
Gross description
- Poorly circumscribed, unencapsulated, pale tan to brown hemorrhagic lesions with ill defined borders
- Size ranges from < 1 cm to > 15 cm
- No grossly apparent cystic spaces or vessels (Hum Pathol 2016;54:143)
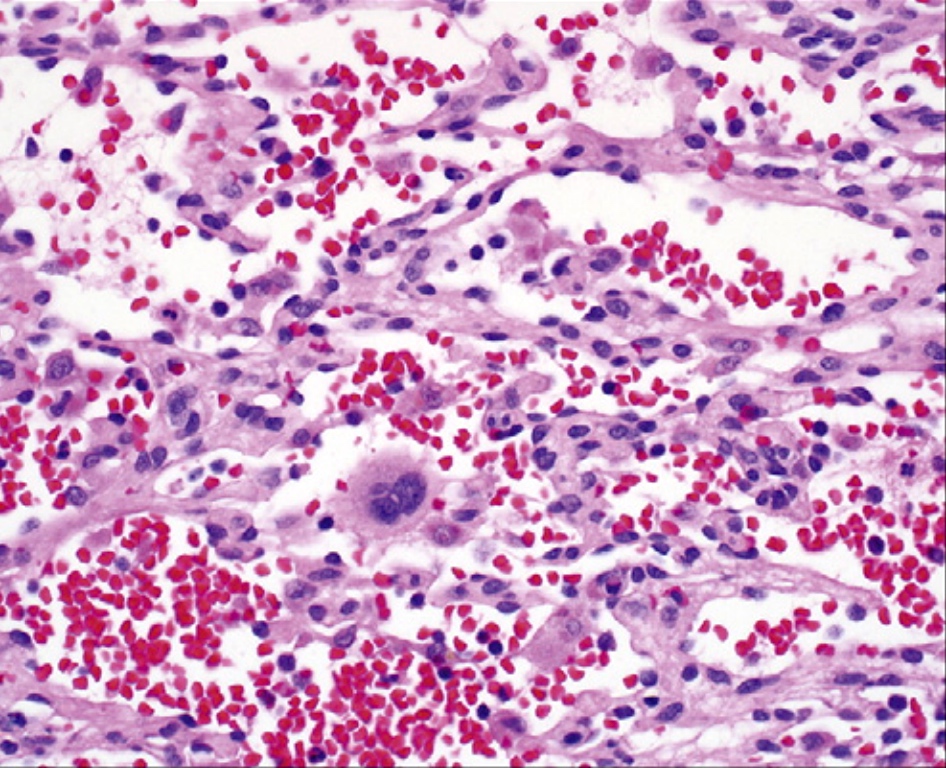
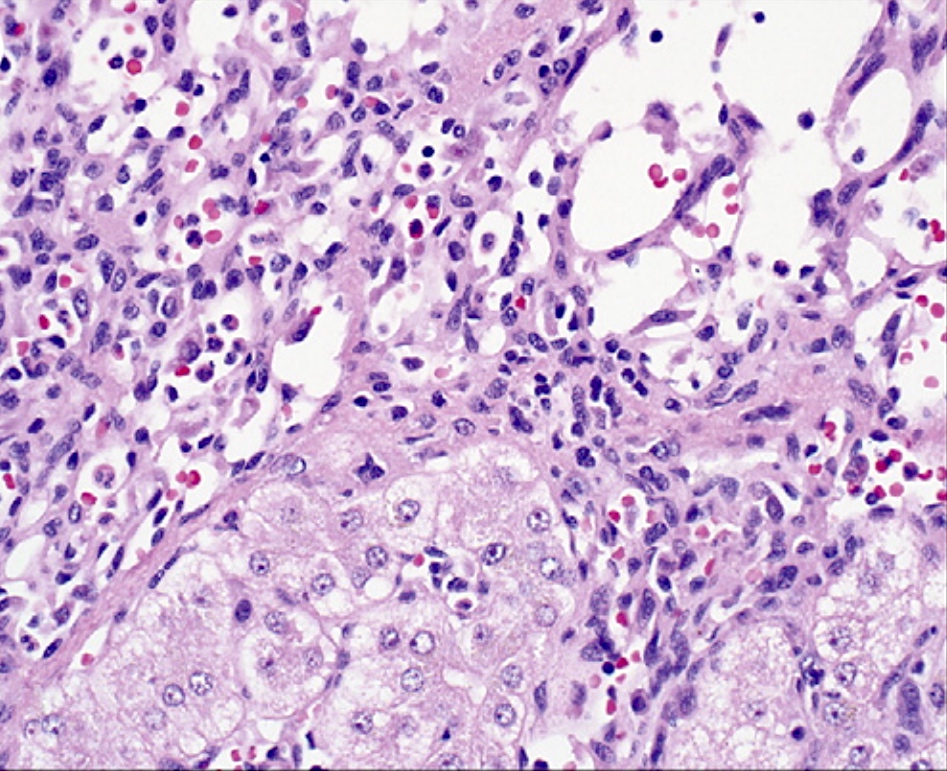
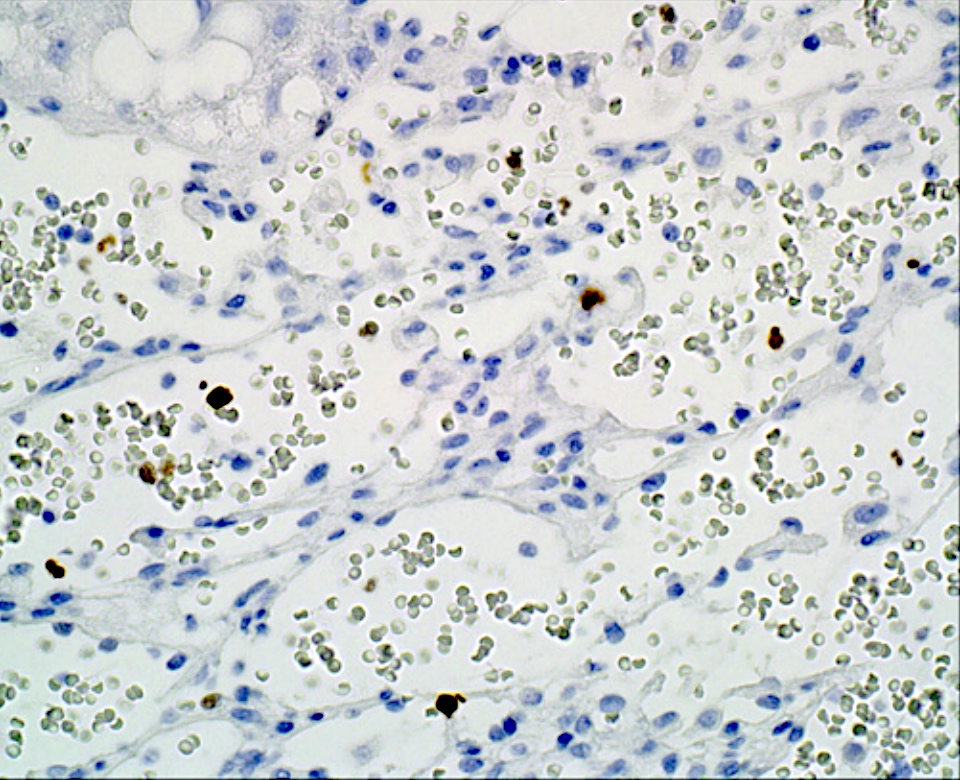
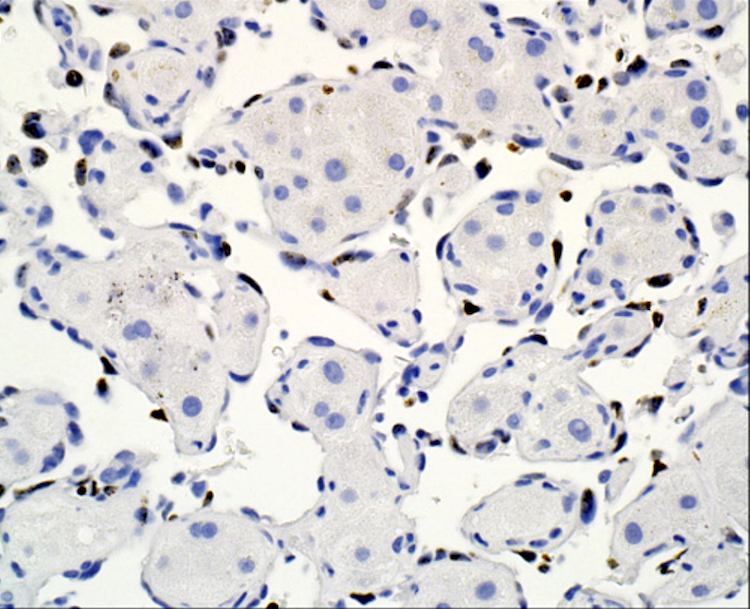
Microscopic (histologic) description
- Anastomosing, closely packed, small thin vascular channels lined by flat to plump endothelial cells with occasional hobnailing
- Infiltrative border with extension between hepatic plates and around portal tracts
- Minimal cytologic atypia
- Absence of necrosis, mitotic activity, prominent nucleoli, nuclear pleomorphism
- Occasional extramedullary hematopoiesis, hyaline globules and vascular thrombi
- Reference: Hum Pathol 2016;54:143
Microscopic (histologic) images
Positive stains
Negative stains
- Pankeratin, HepPar1, p53 (wild type), CD117, S100, c-Myc, GLUT1 (Hum Pathol 2016;54:143)
Molecular / cytogenetics description
- Recurrent activating hotspot mutations of GNAQ, GNA11 and GNA14
- Not found in angiosarcoma
- Recorded in several other vascular lesions: capillary hemangioma, angioma variants, hemangioendothelioma
- Activating hotspot mutation in PIK3CA
- Also found in angiosarcoma
- Reference: Hum Pathol 2016;54:143
Sample pathology report
- Liver, excision:
- Hepatic small vessel neoplasm, 2.5 cm (see comment)
- Comment: The Ki67 proliferative index is approximately 6%. Surgical margins are negative for tumor.
- Liver, biopsy:
- Vascular neoplasm with nuclear atypia (see comment)
- Comment: A neoplastic process consisting of back to back small vessels with mild nuclear atypia is identified. Ki67 immunohistochemical stain highlights ~5% of the endothelial nuclei. Although definitive infiltrative architecture is not present in this sample, these findings are most consistent with the recently described entity hepatic small vessel neoplasm.
Differential diagnosis
- Hepatic angiosarcoma, vasoformative type (more common):
- Marked nuclear pleomorphism, prominent nucleoli, frequent mitoses
- Ki67 proliferative index > 10% (Hum Pathol 2016;54:143)
- Strong and diffuse p53 and c-Myc
- Lacks GNAQ, GNA11, GNA14 mutations
- Epithelioid hemangioendothelioma:
- Lacks zonation pattern, epithelioid morphology, fibromyxoid stroma and intracytoplasmic lumina (Diagn Pathol 2014;9:131)
- Cavernous hemangioma:
- Lacks infiltrative borders
- Large vascular spaces, flat uniform endothelial cells
- Ki67 proliferative index < 1%
Additional references
Practice question #1
A 2.5 cm liver lesion was incidentally identified on a CT scan of a 55 year old man with no significant medical history. No other lesions are identified radiographically. A core biopsy is performed revealing an infiltrative neoplasm pictured above. ERG is positive while HepPar1 and HHV8 are negative and p53 shows wild type staining. What molecular abnormality would most likely be identified in this neoplasm?
- GNAQ hotspot mutation
- KDR mutation
- MYC amplification
- RAS mutation
- TP53 mutation
Practice answer #1
A. GNAQ hotspot mutation. The H&E photomicrograph shows a neoplasm consisting of small vessels with unremarkable endothelial cells, infiltrating between hepatic plates, consistent with a hepatic small vessel neoplasm (HSVN). HSVNs (and benign vascular neoplasms such as hemangiomas) are associated with hotpot mutations in the GNAQ family of genes. The other answer choices are mutations commonly identified in hepatic angiosarcoma (Hum Pathol 2022;29:300671).
Comment Here
Reference: Hepatic small vessel neoplasm
Comment Here
Reference: Hepatic small vessel neoplasm